Академический Документы
Профессиональный Документы
Культура Документы
GA PIB-37 Ovarian Hyperstimulation Syndrome April 2013
Загружено:
goomi0 оценок0% нашли этот документ полезным (0 голосов)
8 просмотров2 страницыcdc
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документcdc
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
8 просмотров2 страницыGA PIB-37 Ovarian Hyperstimulation Syndrome April 2013
Загружено:
goomicdc
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 2
Ovarian Hyperstimulation Syndrome
Patient Information
Womens Health Service, Wellington Hospital
What is Ovarian Hyperstimulation
Syndrome?
As part of their fertility treatment many women
take medication by tablets or injections to
stimulate their ovaries to produce many egg sacs
(follicles). Sometimes there is an excessive
response to fertility drugs and this causes
Ovarian Hyperstimulation Syndrome (OHSS).
Overstimulated ovaries enlarge and release
chemicals into the bloodstream that make the
blood vessels leak fluid into the body. Fluid leaks
into your abdomen, and in severe cases, into the
space around the heart and lungs. OHSS can
affect the kidneys, liver and lungs. A serious but
rare complication is a blood clot (thrombosis).
have had OHSS previously
get pregnant, particularly if it is a multiple
pregnancy (twins or more)
How long does OHSS last?
Most of the symptoms should resolve in a few
days. If you have mild OHSS you can be looked
after at home.
If your fertility treatment does not result in a
pregnancy, OHSS will get better by the time your
period comes.
If your fertility treatment results in a pregnancy,
OHSS can last up to a few weeks or longer.
What should I do if I have mild OHSS?
What are the symptoms of OHSS?
The symptoms include abdominal swelling or
bloating due to the enlarged ovaries, nausea and
as the condition get worse, vomiting.
Mild OHSS - mild abdominal swelling or bloating,
abdominal discomfort and nausea.
Moderate OHSS symptoms of mild OHSS but
the swelling and bloating is worse because fluid
is building up in the abdomen. There is
abdominal pain and vomiting.
Severe OHSS Symptoms of moderate OHSS
plus extreme thirst and dehydration because so
much fluid is building up in the abdomen, passing
very small amounts of concentrated urine,
difficulty breathing because of the build up of
fluid in the chest and a red, hot, swollen and
tender leg due to a clot in the leg or lungs
(thrombosis).
Who gets OHSS?
Mild symptoms are common in women having
IVF treatment. As many as one in three (33%)
women develop mild OHSS. About one in 20
(5%) women develop moderate or severe OHSS.
The risk of OHSS is increased in women
who:
have polycystic ovaries
Make sure you drink clear fluids at regular
intervals. Make sure you do not drink in excess. If
you have pain, take paracetamol or codeine (no
more than the maximum dose).
Even if you are tired, make sure you continue to
move your legs to prevent blood clots.
When should I call for medical help?
Call for medical help if you develop any of the
symptoms of severe OHSS, particularly if you are
in pain despite taking pain relief.
If you start to vomit, have urinary problems, chest
pain or any difficulty breathing.
When will I need to stay in hospital?
There is no specific test that can diagnose OHSS.
A diagnosis is made on the basis of your
symptoms. Your doctor will ask you to describe
your symptoms and will examine you. In addition
your doctor may order:
Blood tests to check your Kidney, Liver
and clotting functions
You will be weighed and your abdomen
measured. This is to confirm if fluid is
building up or reducing.
Page 1 of 2
Fluid intake and output (how much you
drink and how much urine you pass) will
be monitored.
Ultrasound scan of your ovaries to
measure how big they are and whether
there is any fluid build-up in your
abdomen.
The management of your care will depend on the
severity of the symptoms.
What is the treatment for OHSS?
There is no treatment that can reverse OHSS.
OHSS will get better with time, so treatment is to
help symptoms and prevent problems. This
includes:
Medication to control nausea and
vomiting. This can be given either as a
tablet to take by mouth or by an injection
into an IV line in your arm/hand.
Analgesia can be given for discomfort or
pain caused by the symptoms of OHSS.
Anti-inflammatory pain relief such as
voltaren should be avoided as it can
cause bleeding. Medication that is given in
the hospital will be safe for your unborn
child should you have an early pregnancy.
You will be given a pair of anti-thromboembolism stockings (called TED
stockings) to help prevent blood clots
developing in your legs or lungs. This is
because the disturbance in liver function
can affect your blood clotting mechanism
putting you at a higher risk of developing
blood clots. You may also be given an
anti-clotting injection into the skin of your
abdomen once a day to reduce the risk of
clotting.
You will be asked to exercise by walking
in the ward as well as moving your legs
and feet in bed. This will help blood
circulation.
An intravenous(IV) line is inserted into a
vein in your arm or hand to give fluid to
help keep you hydrated. The fluid shift
caused by OHSS means that although
you have excess fuid in your abdomen,
this fluid has shifted from your circulation.
As a result, the fluid in your circulation will
decrease causing dehydration and making
you thirsty.
There may be a restriction placed on your
overall fluid intake. This would allow you
GA PIB-37 Issued April 2013 Review April 2016
no more than 2-3 litres of total fluid intake
over a 24 hour period.
If you have difficulty in passing urine, or if
you are passing significantly reduced
amount of urine, a catheter may need to
be placed in your bladder. This will enable
the staff to accurately record the amount of
urine you are passing.
In rare cases where there is a large
amount of fluid in the abdomen causing
significant discomfort, a procedure called
paracentesis may be offered.This involves
a cannula (a thin tube) being inserted into
the abdominal wall to drain off the excess
fluid.
A paracetesis will only be considered in severe
OHSS because it cannot stop the fluid being
collected in the abdominal wall. As with any other
procedure there are risks involved. Should a
paracentesis be recommended the dictor will
discuss the procedure with you first.
Paracenthesis will only provide temporary relief
and fluid may accumalate again causing furter
discomfort.
Is my baby at risk if I have OHSS?
There is no evidence of problems in the baby as a
result of having OHSS.
Leaving Hospital
You will be discharged from hospital once your
condition has improved and you are well enough
to go home.
Contact details
Womens Clinics-Acute Assessment
Level 3 North
Wellington Hospital
Phone 04 8060 740
Ward 4 North (Pod A Gynaecology)
Level 4,
Wellington Hospital
Phone 04 8060 881 (Extension 80881)
Page 2 of 2
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Kondezatori Za Motore Formule ItdДокумент21 страницаKondezatori Za Motore Formule ItdkoskeruОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Kondezatori Za Motore Formule ItdДокумент21 страницаKondezatori Za Motore Formule ItdkoskeruОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Six Sigma Certification GuideДокумент19 страницSix Sigma Certification GuidegoomiОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- App Tiago Final Omsb PDFДокумент153 страницыApp Tiago Final Omsb PDFgoomiОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hardware of ComputerДокумент25 страницHardware of ComputerVIKALP KULSHRESTHAОценок пока нет
- Yale Final Price List Feb17Документ42 страницыYale Final Price List Feb17Rohan KulkarniОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Latest TNPSC News UpdatesДокумент12 страницLatest TNPSC News UpdatesgoomiОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- 55put6233 56 Pss AensaДокумент3 страницы55put6233 56 Pss AensagoomiОценок пока нет
- Sales BrochureДокумент2 страницыSales BrochureMalay Kr SinghОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- Understanding Six SigmaДокумент147 страницUnderstanding Six Sigmamanisankar05100% (2)
- Spincraft BrochureДокумент48 страницSpincraft BrochuregoomiОценок пока нет
- DS Time Domain Reflectometer IRG 2000 BAUR En-GbДокумент2 страницыDS Time Domain Reflectometer IRG 2000 BAUR En-GbgoomiОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Belt Drives & Bearings Reference GuideДокумент124 страницыBelt Drives & Bearings Reference GuideFaizanОценок пока нет
- How To Install Your Ecobee4Документ80 страницHow To Install Your Ecobee4goomiОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
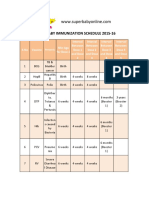
- INDIA - Baby Vacination ScheduleДокумент5 страницINDIA - Baby Vacination ScheduleJayachandar AyyavooОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- MMS e 1401Документ52 страницыMMS e 1401goomiОценок пока нет
- INDIA - Baby Vacination ScheduleДокумент5 страницINDIA - Baby Vacination ScheduleJayachandar AyyavooОценок пока нет
- Pipeline Corrosion and Cathodic ProtectionДокумент177 страницPipeline Corrosion and Cathodic Protectionapi-3698973100% (12)
- SP4009 MS7-500 SeriesДокумент3 страницыSP4009 MS7-500 Seriesgoomi100% (1)
- Rotork PDFДокумент4 страницыRotork PDFgoomiОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- E175e PDFДокумент88 страницE175e PDFgoomiОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- Microchip Vector Motor ControlДокумент68 страницMicrochip Vector Motor ControlShelby PerezОценок пока нет
- DTEd1 EnglishДокумент251 страницаDTEd1 EnglishNagarajan MalmuruganОценок пока нет
- Cap501 2.4.0-2rnenДокумент5 страницCap501 2.4.0-2rnensbat721Оценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Training on Operation and Maintenance of Horizontal & Vertical PumpsДокумент68 страницTraining on Operation and Maintenance of Horizontal & Vertical Pumpsgoomi100% (1)
- Grammar WorksheetsДокумент28 страницGrammar WorksheetsTanja Jovcevska100% (1)
- Power Factor ControllerДокумент20 страницPower Factor ControllergoomiОценок пока нет
- Individual Spelling Words Record SheetДокумент1 страницаIndividual Spelling Words Record SheetgoomiОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Dolch Common NounsДокумент1 страницаDolch Common NounsgoomiОценок пока нет
- Cellulitis (A Serious, Bacterial Skin Infection), Its Causes and Its Symptoms.Документ2 страницыCellulitis (A Serious, Bacterial Skin Infection), Its Causes and Its Symptoms.Encompass HealthCare and Wound MedicineОценок пока нет
- Progestin-Only Injectables: Characteristics and Health BenefitsДокумент11 страницProgestin-Only Injectables: Characteristics and Health BenefitsRazaria DailyneОценок пока нет
- 15 Immunogenetics-89402Документ34 страницы15 Immunogenetics-89402SunuОценок пока нет
- MCQ (Endocrine)Документ7 страницMCQ (Endocrine)aminata680% (5)
- Hypertensive Emergencies in The Emergency DepartmentДокумент13 страницHypertensive Emergencies in The Emergency DepartmentLuis Lopez RevelesОценок пока нет
- Aapi Ebook June 19 2017Документ621 страницаAapi Ebook June 19 2017AAPIUSAОценок пока нет
- How Do We Use Philosophy To Figure Out What Is True?Документ5 страницHow Do We Use Philosophy To Figure Out What Is True?Pik NikОценок пока нет
- Safety Data Sheet for Fiber Glass Fabric FG-100Документ5 страницSafety Data Sheet for Fiber Glass Fabric FG-100Chukwuma Emmanuel OnwufujuОценок пока нет
- Congenital SyphilisДокумент28 страницCongenital SyphilisMeena Koushal100% (4)
- Kelas 3Документ5 страницKelas 3RojОценок пока нет
- Imaging of Nasopharyngeal CarcinomaДокумент9 страницImaging of Nasopharyngeal CarcinomayohanasmjtОценок пока нет
- Baterial & Fungal Corneal UlcersДокумент28 страницBaterial & Fungal Corneal UlcersVasishta NadellaОценок пока нет
- Dementia Presentation Feb 19Документ28 страницDementia Presentation Feb 19Rhu Pugo, La UnionОценок пока нет
- Borderline Personality Disorder, Bipolar Disorder, Depression, Attention ... Narcissistic Personality Disorder, Diferential Diagnostic, KernbergДокумент23 страницыBorderline Personality Disorder, Bipolar Disorder, Depression, Attention ... Narcissistic Personality Disorder, Diferential Diagnostic, KernbergjuaromerОценок пока нет
- Quantitative EstimationДокумент4 страницыQuantitative EstimationSarah BODOFIAОценок пока нет
- Diabetes Mellitus: DefinitionДокумент95 страницDiabetes Mellitus: DefinitionMalik Rizwan ElahiОценок пока нет
- Inspiration Powerpoint NoteДокумент13 страницInspiration Powerpoint Noteapi-201676767Оценок пока нет
- Mood Disorders - Bipolar Disorder: Professor Macdonald, MSN, RNДокумент47 страницMood Disorders - Bipolar Disorder: Professor Macdonald, MSN, RNmaha abdallahОценок пока нет
- Basic Life Support Field GuideДокумент56 страницBasic Life Support Field GuidelmaoheartsОценок пока нет
- Kim (2015) - Lemon Detox Diet Reduced Body FatДокумент12 страницKim (2015) - Lemon Detox Diet Reduced Body FatRodrigo MelloОценок пока нет
- ABG AnalysisДокумент15 страницABG AnalysisPabhat Kumar100% (2)
- Information Bulletin A FMC Mbbs 2021Документ27 страницInformation Bulletin A FMC Mbbs 2021Bidyut Bikash BaruahОценок пока нет
- Emropub 2016 en 19266Документ45 страницEmropub 2016 en 19266jamshaidjiОценок пока нет
- Physical Education Mcqs For All Govt ExamДокумент108 страницPhysical Education Mcqs For All Govt Examrabiaghafar855Оценок пока нет
- Dhatupaushtik ChurnaДокумент6 страницDhatupaushtik ChurnaShoeb MirzaОценок пока нет
- EGurukul GlaucomaДокумент15 страницEGurukul GlaucomaOscar Daniel Mendez100% (1)
- DR.ZHU'S SCALP ACUPUNCTURE GUIDEДокумент25 страницDR.ZHU'S SCALP ACUPUNCTURE GUIDEMajid Mushtaq100% (2)
- Plant Based Diet A Way To Healthier Life: September 2020Документ9 страницPlant Based Diet A Way To Healthier Life: September 2020MihryazdОценок пока нет
- Peritoneal DialysisДокумент9 страницPeritoneal Dialysispinkygurlz1990Оценок пока нет
- GugulipidДокумент7 страницGugulipidManish WadhwaniОценок пока нет
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionОт EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionРейтинг: 4 из 5 звезд4/5 (402)
- Why We Die: The New Science of Aging and the Quest for ImmortalityОт EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityРейтинг: 3.5 из 5 звезд3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisОт EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisРейтинг: 4 из 5 звезд4/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedРейтинг: 5 из 5 звезд5/5 (78)
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (13)