Академический Документы
Профессиональный Документы
Культура Документы
IMG PDF Current CT Scenario of India
Загружено:
anish_106779530 оценок0% нашли этот документ полезным (0 голосов)
40 просмотров4 страницыpaper
Оригинальное название
Www.voisinconsulting.com IMG PDF Current Ct Scenario of India
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документpaper
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
40 просмотров4 страницыIMG PDF Current CT Scenario of India
Загружено:
anish_10677953paper
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 4
Current Clinical Trial Scenario of India:
Challenges and Solutions
The Indian Clinical Trial
Industry, considered as
the booming sector and
perceived as a potentially
upcoming
segment,
is undergoing turmoil
today with a decline of
9.60 per cent in revenues,
with further decline because
of delay/decreased clinical
trial approvals.
ndia was considered as one of the hubs
for conducting major global multinational
clinical trials. It still has the potential
to establish itself as a hub for global
Clinical Trials (CTs). There are several
reasons to it, including but not limited to
a large treatment nave population with
diversity in the gene pool with a range of
illnesses, many easily accessible tertiary
care hospitals, relatively lower cost of
clinical trials compared to the western
countries, high enrolment rates, good
patient compliance/retention, ICH GCP
trained healthcare professionals (HCPs),
a generation of gifted young medical
students, scientists and researchers
who are eager to contribute valuably to
the advancement of medical science,
availability of trained man power and
infrastructure and fairly accommodative
regulatory environment at least until now.
However, the current scenario tells us a
different story. The recent amendments
to regulation, has contributed to a decline
in the Indian Clinical Trial Industry. There
are several challenges that the sponsor
companies are facing which are diverting
them to conduct their trials in countries like
Dr Rajashree Devarakonda
General Manager and Director
Voisin Consulting Life Sciences
16 July 2013
China and Taiwan as they are disillusioned
with the uncertain regulatory environment
here. As well, many companies are as
well going for locations like US, European
Union, Canada and Malaysia going by
the expertise and speedy clearances,
which will be cheaper in the long run.
Recently few academic NIH trials were
also put on hold by US NIH. This trend
is a big dent to the Indian CT sector.
According to the research firm Frost and
Sullivan, the CTs business in India is
estimated to be worth around USD 500
million, which projects that it will grow to
USD 1 billion by 2016. However, the
industry experts have estimated a loss of
USD 150-200 million in the past six months
due to the changes in the regulations.
We will have to wait to see if this is
still achievable.
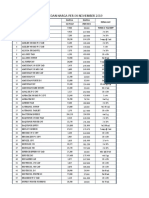
Recent Amendments
Cosmetic Rules
to
Drug
and
In India, Central Drugs Standard Control
Organisation (CDSCO) (headed by Drug
Controller General of India) is the primary
authority and "Drugs and Cosmetics Act,
1940" (along with the rules framed there
122-DAB
The DCR (First
Amendment), 2013
- Compensation in case of injury or death
during CT.
- Free medical management for injury occurring
to CT subject.
- Requirements for financial compensation to
nominee(s) in case of death.
- SAE reporting requirements for Sponsor,
Investigator & ECs etc.
122-DAC
The DCR (Second
Amendment), 2013
-
-
-
-
122-DD
The DCR (Third
Amendment), 2013
- Registration of ECs.
- Requirements & guidelines for EC registration
including application, composition, maintenance
of records etc.
Permission of CTs.
Approval of ECs before trial initiation.
Annual reports of CT status.
Ins pec tion of trial s ite and pers o n n e l b y
CDSCO to check compliance with Schedule Y
and GCPs etc.
Pharma Bio World
Compensation should be limited to the injury or
death of the subject, resulting directly or justifiably
related to the participation of the subjects in the
CTs and not for unrelated events or any injury.
under) is the principal legislation for the
regulation of CTs. Schedule Y of the Drugs
and Cosmetics Rules (DCR), 1945 provides
Rules relating to CTs in India.
bring some stringent regulations and to
create a structure similar or stricter than
few regulated countries, there still are
many lacunas in these amendments.
Since last few years, it was required on
the part of the DCGI to formulate new
regulations or modify the existing ones in
order to streamline the CT process in India.
Recently, in January 2013, DCGI amended
the DCR 1945 to bring the following three
amendments. Few examples of each
amendment are provided as well:
Challenges/Gaps in the Recent
A me ndment(s)
These amendments have brought sudden
change to the CT regulations. Many of
these amendments were long overdue and
were very much required however without
too many lacunas and should have been
done in consultation with the stakeholders
especially while finalising the amendments
(Public, Sponsors, CROs, Academia, Ethics
Committees, Regulators and Ministry) to
avoid the anguish that the CT industry is
undergoing currently.
The amendment has brought in several
good changes (EC/CRO registration, GCP
Compliance and other related quality
changes), as well as challenges. Bringing
these amendments is laudable. However,
the current regulation is leaning primarily
to guard the safety of trial participants
and to improve the much criticised with
a justifiable reason, inefficiencies of
several Clinical research players including
CROs, investigators, ECs, regulators and
sponsors in managing properly ethically
compliant CT process.
Hence, revision of the regulation was very
much needed and is much welcomed after
years of well-documented ethical lapses
in few cases, including informed consent
issues, protocol violations, compensation
issues by the sponsors among others.
Although the DCGI has made an effort to
18 July 2013
The language of regulation itself is
ambiguous at places and has loopholes,
which needs to be clarified.
Compensation for any injury or
death during CTs due to failure of
investigational product to provide the
intended therapeutic effect and use of
placebo in a placebo controlled trial.
Medical coverage and compensation
for any type of injury whether it is
related or not is a major issue, and
there is no clarity for how long and
how much compensation need to be
provided which will be decided by the
regulatory authority and ECs on a case
by case basis. If this compensation
is not provided, this may lead to the
company suspending/losing the license
to conduct CT in India on a case-bycase basis. This is acting as a deterrent
for many pharma MNCs.
The investigators obligation to report
any SAE with 24 hours of the occurrence
of the event is practically impossible as
such information might not be available
in the mentioned time period.
The sponsor needs to report any SAE
of death to EC and expert committee
within 10 days of occurrence, while it is
14 days as per international practice.
21 calendar day timeline for EC to
provide opinion on SAE as well as
financial compensations.
The timelines for EC to examine the SAE
of death and for DCGI to determine the
cause of injury/death are 30 days and 90
days respectively, which looks arbitrary.
The amendments again fail to address
issue of variable timelines for CT
approval leading to significant delays
and lost trust for the sponsor companies.
Challenges of Conducting CTs in India
in General
1) Ethical issues
a. Even though, India has the manpower,
experienced HCPs and infrastructure
to handle more CTs, ethical oversight
is somewhat missing. International
companies are losing trust in the Indian
institutes, as there have been cases of
unethical practices in the past.
b. Until now, the ECs were not required
to register with the DCGI. This led to
independent working of the ECs leading
to in few cases frauds and manipulation
of trial data.
c. Another important challenge lies with
the protection of rights of the subjects
in the CTs.
d. No transparency in informed consent
processing.
e. Involvement of major sub group of
vulnerable
population
(illiterates,
Villagers with lack of awareness,
pregnant women and children) in trials
leading to in few cases exploitation of
the subjects.
2) Quality Issues
a. GCP issues, documentation issues,
data
quality/data
protection/data
compromise and fraud issues.
b. Different quality standards for local/
global trials/BA/BE studies.
c. Laissez faire attitude leading to taking
lightly some of the key ethical steps in
CTs including improper documentation.
3) Regulatory issues
a. Delays/Lack of CT approvals: could be
mainly due to shortage of technical/
trained staff.
b.
Lack
of
standardisation
and
transparency in CT approvals/audits/
inspections and reason for decisions.
4) Cultural issues
a. In India, the personal physician
strongly influences patient decisions,
as do family and friends, which could
raise potential ethical issues with
patient recruitment unless the process
is transparent.
Pharma Bio World
b. Informed consent needs to be in local
language. This means translation needs
to be performed in multiple languages.
5) Media
a. There has been lot of negative publicity
of CTs in India by media sometimes
with biased/inaccurate data on safety
related to CTs, which has led to overall
negativity/uncertainties in subjects,
industry and government leading to
development of laws, which are very
restrictive rather than supportive.
6) Training/Mentoring
a. Lack of practical advanced GCP and
CT training of HCPs including regular
up gradation and or maintenance of
certification is a major issue.
b. India has an extraordinary pool of
bright, insightful young medical talent
who are often given minimal guidance
and mentorship, and even less financial
support in their endeavors leading to
waste of talent.
Overcoming the Challenges
It is the hope of the clinical trial industry
stake holders that the recent amendments
to the regulations once lacunas are
addressed should be able to address many
of the following critical steps leading to
solutions to protect the integrity of Indian
19 July 2013
CT industry leading to India back on as a
global hub for global CTs.
The amended regulations are great even
though very stringent in few aspects
and were needed for Mandatory GCP
compliance, mandatory AE reporting, EC/
CRO/CT registration including mandatory
compensation for the subjects. However,
the ambiguity in the regulations has to be
clarified soon, as these regulations look
more patient/subject friendly and lesser
sponsors friendly so that there is a balance
in the regulation enabling researchers
to conduct CTs in India with integrity as
ethically conducted CTs are very much
necessary for drug discovery and treatment
of rare complex diseases in India or globally.
Compensation and safety reporting
amendments specially need to be
revisited. Compensation should be limited
to the injury or death of the subject, which
are resulting directly or justifiably related
to the participation of the subjects in the
CTs and it should not be for unrelated
events or any injury. There should be
clarity on the compensation amount to be
reimbursed. It is important that medical
treatment for trial related injury should be
covered by the sponsors.
However, there should be more clarity on
the amount of compensation to be given,
for how long the medical treatment should
be given, and industry also should be able
to participate in this calculation along
with DCGI and ECs. There is urgency in
this matter, as we have already seen a
decline in the number of CTs in India since
last year and companies moving their
base to other countries. Positive note is
that, the Drug Technical Advisory Board
(DTAB), in their recent meeting on May
16 th, 2013, has proposed few changes to
these amendments which are still under
discussion. For example: including the
words In the case of CT related injury in
the compensation clause to bring clarity
that only trial related death/injury needs
to be compensated for. Although they
have not commented on the amount of
compensation to be provided, they have
recommended that a qualifying clause may
be added in case there is no permanent
injury, the quantum of compensation shall
commensurate with the inconvenience,
loss of wages, transportation. The
DTAB has recommended the removal of
the compensation for the failure of the
investigational drug for intended therapeutic
effect as well; they have added the clause
use of placebo in a placebo controlled trial
if the standard care is denied.
As discussed earlier, the timelines for
SAE reporting are also a major concern
and needs to be revised. For example,
modifying the timelines to meet the
international standards : 14 days instead of
10 days for sponsors and investigators, 30
days (instead of 21) for ECs to report SAE,
60 days (instead of 30) Expert committee
to examine SAE and 60 days (instead of
90) for the DCGI to determine the cause of
injury and decide quantum of compensation.
These are few recommendations that the
DTAB has provided during their meeting
in May. This might help to streamline the
timelines and reduce the ambiguity in the
regulations. However, it needs to be noted
that these are only recommendations at
this stage and are not approved yet.
It is crucial to increase the technical staff
with advanced industry training at the DCGI
office as they are currently understaffed/
undertrained which leads to delays in
approval of CTs. Further training by
international regulator exchange programs
Pharma Bio World
as well as advanced training in clinical
trial design, implementation, monitoring,
data management, and quality assurance
including funding the DCGIs office might
help to improve the consistency of approvals,
reduce the time taken for approvals and
thereby increase the trust factor of the MNCs
in the Indian regulatory system.
Once this is concluded, providing more
power to DCGIs office to make the decisions
might be useful. As well, planned setting up
of technical and regulatory expert committee
to support CT application filing, review and
related activities should take a priority and
be established soon to streamline these
activities. Streamlining of, and improved
cross-communication and cooperation
between the other agencies involved in the
CT process approvals will be useful.
ECs need to be linked to Institutes, should
have appropriate representatives and
ideally should be monitored centrally.
Constant monitoring and accountability
of the ECs as well is the key to ensure
quality ethical operation. ECs should do
proper monitoring of trials including the
consenting aspects, ensuring the diversity
of trial populations so as to avoid misuse of
vulnerable population including recruitment
of poor homogeneous rural communities.
CROs when not meeting ICH GCP
quality and ethical standards should be
removed. A barrier needs to be created
between industry and CT investigators to
ensure ethical conduct of research. CROs
should conduct trials to the internationally
recognised standards by conformance to
CT protocol and independent monitoring.
Independent research in private clinics
without supervision should not be allowed.
There should be transparency at all levelssponsors, CROs, Investigators, Regulators
and ECs. Sponsors should ensure
registration of all CTs in the CTs registry.
Sponsors should also communicate risks/
benefits of the trials including safety issues
related to the drug/device including trial
related risks to all the subjects including
vulnerable
population.
Investigators
should be transparent about the treatment
given, adverse events, relatedness to
the trial activities etc. with the public and
regulators. Informed consent process need
20 July 2013
to be highly transparent and it should be
voluntary and documented properly.
Transparency by the regulators in the
entire process of CT application review
with the appropriate reasons for approval
or rejection of the application, approval
criteria will be very useful. Transparency
on CT audit, its process will be useful
to build confidence in integrity of the
data coming out of India. Increase in the
number of Government regulated and
funded CT centres, new initiatives for
funding translational science/medicine with
high-quality training in clinical research
management, basic science research and
Quality assurance is very much needed.
Industry exchange programs should be
encouraged at all levels so that Biotech/
pharma/clinical trial experts from developed
regulated regions should be allowed to
come to India to train our CT community
including for regulators vice versa to foster
cross-country collaboration initiatives.
Clinical research professionals including
medical doctors in India need to be
appropriately trained on ethics from the
beginning during medical school. They need
to be educated on the impact of unethical
research on the subject, their family, CT
industry and the country eventually. There
should, not only be ethics courses included
in the curriculum from the beginning, but
also, annual ethics certification for CRAs
and investigators to keep them up to date
with the current regulations, GCPs and
ethical conduct of CTs. CME credit could
be provided to attend these training at
least once or twice a year.
People should own up responsibilities and
the attitude of Laissez faire or casual
attitude towards consenting, ethical/quality
trials process including documentation need
to go. The standard of clinical trial should be
high irrespective of to which market this drug
will go and whether the trial is local or global.
Same high ethical and quality ICH GCP
standards should be maintained at all levels
(Sponsors, Investigator, CROs, Regulators,
Ethics committees)
Media holds a key responsibility in the
process too and it is hence critical for the
media to present the right accurate data and
not biased data especially on the CT related
activities, adverse events, deaths and
injuries related to CTs as presented before
in several instances. It is very important
for the regulators, the industry and the
Government to come together and plan the
regulations that protect the interest of the
public at all times but, still have regulations
that are supportive to the industry leading to
the economic growth of the country.
Conclusion
There is an urgent requirement for
readdressing some of the amendments to
continue protecting the interests of subjects
as a priority however, simultaneously
upholding
scientific
research
and
development that will be beneficial to
society. It is critical that clinical research
community at all levels diligently follow the
laws that are in place, understand and apply
the guidelines and create a transparent
trusted environment so that integrity of
the Indian CT industry is maintained. It
is the hope of Indian CT fraternity that
new and reformed regulations once
amended further will be able to bring back
Indian CT industry to the highest global
ethical standards.
Insufficient training or mentoring of young
scientific community on advanced practical
CT activities including practical GCPs is
a real loss to Indian scientific community,
as India could easily become a centre of
basic medical and clinical excellence with a
true Evidence-based Integrative Medicine.
At every level the sponsor, investigator,
monitor, regulator, inspector, CRA, clinical
coordinator, there should be a clear focus
on integrity and quality for Indias CTs
industry to grow. Years may still be required
before further clarity if brought in to address
the current lacuna in the regulation,
quality and ethical standards to effect all
transformations, but it is the hope that this
year forwards will see a tremendous move
forward towards that goal.
(Author would like to thank Rushin P Jhala,
Dinesh Babu Sukumar and Ravi Rajhans
of Voisin Consulting Life Sciences for
their valuable support in preparation of
this article.)
Contact: devarakonda@voisinconsulting.com
Pharma Bio World
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Online Magazine On PharmaДокумент19 страницOnline Magazine On Pharmaanish_10677953Оценок пока нет
- Report of MalariaДокумент3 страницыReport of Malariaanish_10677953Оценок пока нет
- Indian Council of Medical ResearchДокумент9 страницIndian Council of Medical Researchkuldeepgju17Оценок пока нет
- Updated List 2014 of DrugsДокумент4 страницыUpdated List 2014 of Drugsanish_10677953Оценок пока нет
- Sanskrit University Sampurnanand Sanskrit University Is An Asian Institution of Higher Learning Located inДокумент2 страницыSanskrit University Sampurnanand Sanskrit University Is An Asian Institution of Higher Learning Located inanish_10677953Оценок пока нет
- Pdfs CritspinManualДокумент17 страницPdfs CritspinManualanish_10677953Оценок пока нет
- 11431451965Документ1 страница11431451965PrashantVedwanОценок пока нет
- Untitled DocumentДокумент2 страницыUntitled Documentanish_10677953Оценок пока нет
- Supply List of Mesa LabДокумент2 страницыSupply List of Mesa Labanish_10677953Оценок пока нет
- 2014 04 22 02 39 47 How-to-apply-OfflineДокумент1 страница2014 04 22 02 39 47 How-to-apply-Offlineanish_10677953Оценок пока нет
- University Grants CommisionДокумент1 страницаUniversity Grants Commisionanish_10677953Оценок пока нет
- Diagnostics Report Form 20130115Документ5 страницDiagnostics Report Form 20130115anish_10677953Оценок пока нет
- Darjeeling Travel GuideДокумент16 страницDarjeeling Travel Guideanish_10677953Оценок пока нет
- Roll Number 653298: Ukssv %& VH FKHZ Izr SD Iz'U I GSRQ Vyx&Vyx Izos'K I E Miflfkfr I Mkmuyksm DjsaaДокумент1 страницаRoll Number 653298: Ukssv %& VH FKHZ Izr SD Iz'U I GSRQ Vyx&Vyx Izos'K I E Miflfkfr I Mkmuyksm Djsaaanish_10677953Оценок пока нет
- Project On Body LanguageДокумент51 страницаProject On Body Languagevikash88% (8)
- Guru Ghasidas Vishwavidyalaya Bilaspur (C.G.)Документ4 страницыGuru Ghasidas Vishwavidyalaya Bilaspur (C.G.)anish_10677953Оценок пока нет
- Application Form For Non-Teaching Contractual Engagement1Документ2 страницыApplication Form For Non-Teaching Contractual Engagement1AnamikaShuklaОценок пока нет
- BSNL Bill 1Документ1 страницаBSNL Bill 1anish_10677953Оценок пока нет
- Marketing Brand Role in Buying Behaviour of YouthДокумент61 страницаMarketing Brand Role in Buying Behaviour of Youthanish_10677953Оценок пока нет
- 20.5.14-Bachelor of Education (Special Education - Hearing Impaired)Документ14 страниц20.5.14-Bachelor of Education (Special Education - Hearing Impaired)anish_10677953Оценок пока нет
- Schedule yДокумент58 страницSchedule yanish_10677953Оценок пока нет
- Net JRFДокумент10 страницNet JRFB. Rajeev Kungur100% (2)
- Aryans Institute of Management & TechnologyДокумент53 страницыAryans Institute of Management & TechnologyvikashОценок пока нет
- NABARDДокумент110 страницNABARDKini Shi100% (1)
- BD Product ListДокумент48 страницBD Product Listanish_10677953100% (1)
- Employee WelfareДокумент76 страницEmployee Welfareanish_10677953Оценок пока нет
- The Concept of ValueДокумент17 страницThe Concept of Valueanish_10677953Оценок пока нет
- STRESS MnagmentДокумент107 страницSTRESS Mnagmentanish_10677953Оценок пока нет
- No Content Page No 1 1 1.1: Employee Performanc Objectives of Performance AppraisalДокумент2 страницыNo Content Page No 1 1 1.1: Employee Performanc Objectives of Performance Appraisalanish_10677953Оценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (120)
- Conatct ListДокумент58 страницConatct ListBadal Bhattacharya50% (2)
- RanbaxyДокумент18 страницRanbaxyDipankar PandeyОценок пока нет
- Case 6.3 "Off-Label" Marketing: GROUP 8 - Lecture: Alang ThoДокумент12 страницCase 6.3 "Off-Label" Marketing: GROUP 8 - Lecture: Alang ThoNganОценок пока нет
- Guideline For Drug Master FilesДокумент33 страницыGuideline For Drug Master FilesRambabu komati - QA100% (3)
- Homework1 SirrolaДокумент4 страницыHomework1 Sirrolarniyatee90Оценок пока нет
- Conference Delegate Wish ListДокумент55 страницConference Delegate Wish ListThinkLink, Foreign Affairs www.thinklk.comОценок пока нет
- PHARMA COMPANIES Details With Websites 09Документ1 страницаPHARMA COMPANIES Details With Websites 09Irfan SheikОценок пока нет
- ShimadzuДокумент17 страницShimadzuMuhammed FarrukhОценок пока нет
- Franklin Fink CVДокумент27 страницFranklin Fink CVThe Florida Times-UnionОценок пока нет
- Economics of The Pharmaceutical IndustryДокумент12 страницEconomics of The Pharmaceutical IndustrySambasiva RaoОценок пока нет
- Pharmaceutical EngineeringДокумент5 страницPharmaceutical EngineeringmikebluberryОценок пока нет
- The Regulatory Trends: Cross-Contamination in Drug ManufacturingДокумент9 страницThe Regulatory Trends: Cross-Contamination in Drug Manufacturinglina kharratОценок пока нет
- General Profile of Pharmaceutical CompaniesДокумент3 страницыGeneral Profile of Pharmaceutical CompaniesHaile Kassa100% (1)
- Regen PDFДокумент6 страницRegen PDFaditisinghaniaОценок пока нет
- Trends in Oncology Business DevelopmentДокумент25 страницTrends in Oncology Business DevelopmentSheltie ForeverОценок пока нет
- ATH Stocks, Technical Analysis ScannerДокумент4 страницыATH Stocks, Technical Analysis Scanneromkarambale1Оценок пока нет
- The Road To Digital Success in Pharma - McKinsey & CompanyДокумент10 страницThe Road To Digital Success in Pharma - McKinsey & CompanyharshalОценок пока нет
- PDFДокумент156 страницPDFvidhi hiteshОценок пока нет
- PM Journal1Документ10 страницPM Journal1gireesh_babuОценок пока нет
- Data Transaksi Obat Sanbe SD 06032019Документ2 031 страницаData Transaksi Obat Sanbe SD 06032019desiduwiОценок пока нет
- Trump Legal CBD OilДокумент9 страницTrump Legal CBD OilChiefJustice Middleton100% (1)
- Mukund SДокумент19 страницMukund SHajime HikariОценок пока нет
- Bonus Product Sales April-2023Документ3 страницыBonus Product Sales April-2023Mahbub Alam SarkerОценок пока нет
- Vol 19.2 Dementia.2013Документ208 страницVol 19.2 Dementia.2013Martoiu MariaОценок пока нет
- The Searle Company (SEARL) - Reinstating With A BuyДокумент17 страницThe Searle Company (SEARL) - Reinstating With A BuySHAHZAIB -Оценок пока нет
- Senario Case StudyДокумент19 страницSenario Case Studymaya100% (1)
- Drug Policy 2017 (Medex - Com.bd)Документ64 страницыDrug Policy 2017 (Medex - Com.bd)মোঃ এমদাদুল হকОценок пока нет
- Daftar Peoduk SanbeДокумент7 страницDaftar Peoduk SanbeDuduSaepudinОценок пока нет
- Revision 1 2021Документ23 страницыRevision 1 2021Rin AkaneОценок пока нет
- Imcops Price List From 01 - 11 - 2015 PDFДокумент26 страницImcops Price List From 01 - 11 - 2015 PDFGoutham PillaiОценок пока нет