Академический Документы
Профессиональный Документы
Культура Документы
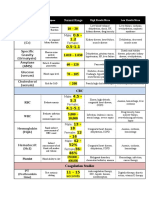
Dysrhythmias Chart
Загружено:
jkrixАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Dysrhythmias Chart
Загружено:
jkrixАвторское право:
Доступные форматы
DYSRHYTHMIAS AND EKG INTERPRETATION 1 | P a g e
RHYTHM
EKG
NORMAL SINUS RHYTHM (NSR)
I N T E R P R E T R H Y T H M , A S S E S S
RATE
RHYTHM
EKG
(BPM)
60 100
Regular
rhythm:
R to R and P
to P interval
constant
T R E A T M E N T
INTERVENTIONS
P wave:
present and
similar
PR interval:
.12 .20 seconds
and consistent
None, normal.
QRS segment:
.04 - .10 seconds
and consistent
SINUS BRADYCARDIA
Causes:
Noncardiac
Athlete
Sleeping
Elderly
Cardiac
SA node disease
Vagal stimulation
Drug Induced
Beta blockers
P wave:
present and
similar
MI
CAD
Less than
60
Antianxiety
Signs and symptoms:
Pale, cool skin
Weakness
Dizziness
Confusion
SOB
Regular
Digitalis
PR interval:
present and
normal
QRS segment:
present and
normal
Hypotension
Angina
Syncope
Disorientation
Assessment
Decreased cardiac output
related to slow heart rate
Blood pressure
Are you dizzy? Light
headed?
Treat only if the patient is
symptomatic
Atropine*
Stimulate patient.
SINUS TACHYCARDIA
Causes
Noncardiac
Anxiety, fright, stress
Pain
Alcohol ingestion
Hypovolemia
Cardiac
MI
Exercise
Fever
P wave:
present and
similar
CHF
Drug Induced
Aminophylline
Caffeine
Dopamine
Nicotine
Amphetamines
Atropine*
Epinephrine
Signs and Symptoms:
Dizziness
Dyspnea
Hypotension
Angina
Increased myocardial oxygenation
Decreased cardiac output
greater than
100
Regular
PR interval:
present and
normal
QRS segment:
present and
normal
Assessment
Decreased cardiac output
related to decreased filling
time
Treatment
Treat the cause*
Pain
Pain management
Hypovolemia
Resolve hypovolemia
Vagal maneuvers*
IV beta blockers*
(Lopressor)
DYSRHYTHMIAS AND EKG INTERPRETATION 2 | P a g e
I N T E R P R E T
R H Y T H M ,
A S S E S S
T R E A T M E N T
ATRIAL DYSRHYTHMIAS
RHYTHM
EKG
Rate
Rhythm
EKG
Treatment
PAC
PREMATURE ATRIAL
CONTRACTIONS (PACS)
Action:
Originates in the atrium
Ectopic foci (irritable cell) in the atria
Not life-threatening
Unifocal versus multifocal
Conducted PAC
P wave:
Different, down
deflection
notched*
Disoriented P wave
AV node stopped (nonconducted PAC)
delayed (lengthened PR
inter.)
Causes
Emotional stress
Fatigue
Caffeine
Tobacco
Alcohol
COPD
Valvular disease
Hypoxia
Electrolyte imbalances
CAD
Variable
Irregular
Nonconducted PAC
Asymptomatic:
No treatment needed
Treat the cause* because
it can cause more lethal
dysrhythmias.
PR Interval
Varies but WNL
Withdraw from drug or
caffeine
QRS
Usually normal*
(NORMAL FOR
ALL ATRIAL
ARRHYTHMIAS)
Oxygen
Termed as NSR
with PACs
Electrolyte replacement
Medications*
Digoxin
Quinidine (IA)
Pronestyl (IA)
Signs and Symptoms
Isolated PACs: Not important
Palpitations
Frequent PACs: SVT warming *
Assessment:
Decreased cardiac output
related to decreased filling
time
ineffective myocardial
contraction
ATRIAL FLUTTER
Action
Recurring, regular sawtooth-shaped
flutter waves
Variable Atrial Flutter
Rapid atrial depolarization
Single Ectopic focus
SA node not repolarizing
Causes
Atrial ischemia
Stretched atria such as in fluid overload
or CHF
Signs and Symptoms
Decreased CO: HF with underlying
disease
Increased risk of stroke:
Thrombus formation in atria
Atrial Flutter
Atrial rate:
200-350 per
minute
Ventricular
rate:
< 150
Atrial
Regular*
Ventricular
Irregular*
Flutter waves:
Saw tooth waves
Two or more
before each QRS
PR Interval:
Not measurable
QRS
Usually normal*
(NORMAL FOR
ALL ATRIAL
ARRHYTHMIAS)
Drugs to control rate
Decrease ventricular
response rate for filling time.
Digoxin*
Esmolol (Brevibloc)*
Diltiazem (Cardizem)*
Drugs to control Rhythm
Medications convert back
from atrial flutter to normal
sinus rhythm.
Ibutilide (Corvert) (III)
Pronestyl (IA)
Amiodarone (III) to
cardiovert chemically
Cardioversion
Atrial Pacing
DYSRHYTHMIAS AND EKG INTERPRETATION 3 | P a g e
I N T E R P R E T
R H Y T H M ,
A S S E S S
T R E A T M E N T
ATRIAL DYSRHYTHMIAS
RHYTHM
ATRIAL FIBRILLATION
EKG
RATE
Irregular
Chaotic
Total disorganization of atrial
electroactivity
Loss of effective atrial contraction
Most common*
Clinical Associations
CAD
Rheumatic heart disease
Alcohol intoxication
Stress
Cardiac surgery
Cardiomyopathy
Hypertensive heart disease
Caffeine use
HF
Pericarditis
Electrolyte Imbalances
RHYTHM
Controlled A. Fib:
Atrial rate:
Too fast to
determine
Faster the
rate, the
more regular
it may
appear. But it
is not regular!
>350 BPM
Ventricular
Rate:
Varies
Uncontrolled A. Fib:
Clinical Significance
Decreased CO: ineffective atrial
contractions
Controlled
Less than
100
Uncontrolled
>100
Thombi in atria emboli brain
(stroke)
Complications
Emboli
Cardiac output decreased 20-25%
*they also
have atrial
flutter. When
they see
flutter they
think it is a P
wave. But it
is not a
frigken P
wave! All P
waves must
look the
same.
Random
flutter wave
not P Wave.
EKG
P wave
Not identifiable
Chaotic
PR interval
Not measurable
QRS
Usually normal*
(NORMAL FOR
ALL ATRIAL
ARRHYTHMIAS,
initiated above
the ventricles. )
Cardiac output
likely to be lower
(20-25%):
normally, atria
will squeeze to
increase and rid
of blood and put
it in ventricle
(atrial kick).
SUPRAVENTRICULAR
TACHYCARDIA
(AKA SVT / PAT / PSVT)
COPD
CHF
Hypoxia
P wave:
Often not
identifiable
Absent
PAT / PSVT
150-200 /
minute
Cor Pulmonale
CAD
Post CABG
Anesthesia
Cardiac anomalies
Sypathomimetic drugs
Signs and Symptoms
Prolonged HR
Decreased CO r/t decreased CV
Hypotension
Dyspnea
Angina
Brevibloc
Ibutilide
Digoxin
Dugs to control Rhythm
Pronestyl (IA)
Amiodarone (III)
Anticoagulation***
Warfarin for a fib longer than
48 hours
TEE to rule out presence of
clot in atria, stasis of blood,
emboli
Long term anticoagulation
Cardioversion
Atrial Pacing
Ablation (unresponsive to
cardioversion)
MAZE: stops A fib by
interrupting electrical signals
Treatment
Vagal stimulation through
Valsava maneuver
Slows heart rate down
An irritable foci above the ventricles
Overrides the SA node
Causes
Common in children and young adults
Fever
Sepsis
Caffeine
Tobacco
Alcohol
Stress
TREATMENT
Drugs to control rate
Diltiazem (CCB) (IV)
Decreases ventricular
response
NSR PAC PAT
Regular or
Slightly
Irregular
PR Interval:
Shortened /
normal
QRS:
Usually normal,
initiated above
the ventricles.
Coughing
Carotid massage:
dont do it!
Can have person stroke. Do
not massage both sides at
the same time.
Cardioversion
AV ablation
Surgical cardiac cath EPS
study
Medications
Digoxin
Pronestyl (IA)
Inderal (II)
IV Adenosine*
DYSRHYTHMIAS AND EKG INTERPRETATION 4 | P a g e
I N T E R P R E T
R H Y T H M ,
A S S E S S
T R E A T M E N T
HEART BLOCKS
RHYTHM
EKG
RATE
RHYTHM
TREATMENT
Usually asymptomatic
No treatment needed.
Monitor and drugs.
FIRST DEGREE HEART BLOCK
Impulse is slowed through the AV node
Clinical Conditions Associated
MI
CAD
Rheumatic Fever
Vagal stimulation
Hyperthyroidism
Drug use of: digoxin, b-blockers, CCB,
flecainimide
EKG
Varies but
normal
Regular
PR Interval:
Greater than .20
seconds,
prolonged*
QRS:
Normal
Prolonged PR interval. Looks like NSR but PR interval is LONGER.
Adjust drug therapy
Atropine: if symptomatic
and bradycardic
Monitored for progression
into more advanced degree of
block
SECOND DEGREE HEART BLOCK
TYPE I MOBITZ I * / WENKEBACH
Gradual lengthening of PR interval
Occurs in the AV node
Clinical Associations
Digoxin Use
Beta blocker use
CAD
Clinical Significance
MI or infarction
Warning signs of *more serious AV
conduction
Disturbance
Normal
Dropped QRS. PR interval progressively becoming prolonging. The
PR interval, longer, longer, longer, then it DROPS a QRS complex.
Atrial
Rhythm:
Normal
Pattern of
grouped beats
Ventricular
Rhythm:
Slow
blocked QRS
PR progressively
lengthens until a
QRS complex is
dropped*
Symptomatic:
Atropine* to increase HR
Temporary pacemaker
Asymptomatic:
Closely observe rhythm
Poor conduction through the AV node.
Discontinue causative
medications
SECOND DEGREE HEART BLOCK
TYPE II AKA MOBITZ II*
Clinical Associations
Rheumatic Heart Disease
CAD
Anterior MI
Drug toxicity
Atrial
Rate:
Normal
Ventricular
Rate
Slow
Clinical Significance
Progressive to type III heart block
Poor prognosis
Conduction through AV node variable.
Same constant PR interval.
Atrial
Rhythm:
Normal
Ventricular
Rhythm:
Irregular
Sudden
dropped
complex*
P wave:
Normal
PR Interval:
Constant
CONSISTENT*
QRS:
Suddenly dropped
complex
Often WIDE
Drugs Used
Atropine*
Epinephrine*
Temporary pacemaker
Permanent pacemaker
needed*
Increases sinus rate
Monitor for progression into
third degree heart block
DYSRHYTHMIAS AND EKG INTERPRETATION 5 | P a g e
I N T E R P R E T
R H Y T H M ,
A S S E S S
T R E A T M E N T
HEART BLOCKS
RHYTHM
THIRD DEGREE HEART BLOCK
AKA COMPLETE HEART BLOCK
EKG
RATE
RHYTHM
AV dissociation
Independent atrial and ventricular
activity
No impulses from atria and ventricles
Clinical Associations
Severe heart disease
Myocarditis
Amyloidosis
CAD
MI
Cardiomyopathy
Sclerosis
Medications: digoxin
B-blockers
P wave:
Normal
Atrial faster
than
ventricular
Atria and
ventricular
independently
regular
CCB
Clinical Significance
Asymptomatic or Life threatening
Decreased CO with subsequent
ischemia, HF, and stroke
EKG
More than 1 P wave for every QRS. Totally miscommunication. P
to P. No dropped beat.
PR Interval:
varies
QRS interval:
Normal or wide
Normal: above
bundle
Widened: Below
of His
TREATMENT
Atropine*
Increases HR and BP
For bradycardia
More effective with Mobitz I,
does not work well with
Mobitz II
Calcium Chloride
For CCB toxicity
Pacemaker:
Temporary, and if no
improvement permanent
Transthoracic pacemaker
Syncope: severe bradycardia / asystole
VENTRICULAR DYSRHYTHMIAS
RHYTHM
PREMATURE VENTRICULAR
CONTRACTIONS (PVCS)
EKG
RATE
RHYTHM
EKG
Unifocal PVC
Ectopic focus or foci in the ventricle,
emitting impulses which are early in the
cycle and override the SA node impulse
Each focus creates an impulse which
looks the same each time
Depends on
underlying
rhythm and
the # of
PVCs
Potentially lethal* and lead to V. tach
1.
2.
3.
4.
5.
Unifocal: same shaped PVCs
Multifocal: PVCs appearing
different
V. trigeminy: every 3rd beat as
PVC
V. Bigeminy: every 2nd beat as
PVC
Couplet: two consecutive PVCs
Causes
cardiac disease
electrolyte imbalance
K and Mg
Multifocal PVCs
Similar to
atrial.
Because
they are
occurring
early, QRS
complex
gets wide.
Runs of PVCs
hypoxemia
stimulants (caffeine)
Signs and Symptoms
Reduced CO: angina and acute MI
Pulse deficit
"
Irregular
TREATMENT
CRITERIA FOR
TREATMENT:
More than 6 per minute
Multiform
Runs of PVCs: indicates
ventricular tachycardia*
R on T
P wave:
No P wave
preceding PVC
CORRECT CAUSE:
Correct hypoxia with oxygen
therapy
PR Interval:
Immeasurable
Check pulse ox
QRS of PVC:
>0.12 seconds
Premature
occurrence of the
QRS wide and
distorted
T wave:
Large and
opposite direction
Correct electrolyte
imbalance with electrolyte
replacement
Especially Mg and K
Before administering
medications, consider the
underlying rhythm/rate
MEDICATIONS:
Lidocaine* if underlying rate
normal or tachycardic (IB) to
erase PVC and what is
causing it. If land on T wave,
can put them into code.
Atropine* if underlying rate
is bradycardic
DYSRHYTHMIAS AND EKG INTERPRETATION 6 | P a g e
RHYTHM
VENTRICULAR TACHYCARDIA
EKG
I N T E R P R E T R H Y T H M , A S S E S S
RATE
RHYTHM
EKG
Three or more PVCs
Foci fire repetitively: ventricle takes
control as pacemaker
1.
2.
Monomorphic: QRS complexes
same
Polymorphic: QRS complexes
change back and forth
Hypokalemia
Hypoxia
T R E A T M E N T
TREATMENT
If conscious and stable:
Lidocaine
bolus and drip (IB)
Torsades De Pointes* TREATMENT MUST BE MAGNESIUM, OR YOU
WILL NOT GET THEM BACK.
Cough CPR
Cardioversion
Torsades de Pointes:
Polymorphic VT associated with
prolonged QT
Life-threatening dysrhythmia*
Causes
MI
Hypomagnesimia
P wave:
Usually not
identifiable
Ventricular Tachycardia
150 200
per minute
Regular
PR Interval:
Not applicable
QRS Complex:
>0.12 seconds
Signs and Symptoms
Stable (with a pulse)
Unstable (Pulseless)
If unconscious and
pulseless
CPR - full code
Defibrillation
Vasopressors Epinephrine
Antidysrhythmics
Aminodarone
Treat cause
electrolytes
drug toxicities
AICD
Sustained:
Less than 30 seconds
Decreased CO leading to:
Hypotension
Pulmonary Edema
Decreased cerebral blood flow
Cardiopulmonary arrest
Torsades de Pointe:
Magnesium first!
VENTRICULAR FIBRILLATION
Asynchronous, chaotic, impulses
emitted from multiple foci in the
ventricle.
Quivering of the heart
No cardiac output
Cardiac arrest
Clinical Associations
Acute MI
Myocardial ischemia
Cardiac pacing Catheterization
Chronic HF
Cardiomyopathy
Coronary Perfusion
Accidental electrical shock
Hyperkalemia
Hypoxemia
Acidosis
Drug toxicity
Clinical significance
Unresponsive
Pulseness
Apneic
Death
Defibrillation
CPR
P wave
Not visible
Defibrillation
Not
measurable
Irregular and
chaotic
PR Interval and
QRS:
Not measurable
Medications
Amiodorone (III)
Lidocaine (IB)
This is the most common
terminal event in sudden
cardiac death syndrome*
AED
Вам также может понравиться
- Cardiac Dysrhythmia Chart Med-Surg NUR4Документ3 страницыCardiac Dysrhythmia Chart Med-Surg NUR4ktfosterfd2096% (97)
- Cardiac DysrhythmiasДокумент3 страницыCardiac DysrhythmiasKatherine Santiago92% (62)
- EKG ExamplesДокумент9 страницEKG ExamplesMayer Rosenberg99% (235)
- Cardiac DrugsДокумент10 страницCardiac DrugsNursePoor98% (48)
- Ecg Cheat Sheet 35Документ2 страницыEcg Cheat Sheet 35jessjaylee80% (5)
- Cardiac Meds ChartДокумент1 страницаCardiac Meds ChartCharlotte Louise75% (4)
- Cardiac Dysrhythmia Chart Med Surg NUR4 PDFДокумент3 страницыCardiac Dysrhythmia Chart Med Surg NUR4 PDFlml100% (1)
- Lab ValuesДокумент3 страницыLab Valuessurviving nursing school100% (1)
- ArrhythmiaДокумент2 страницыArrhythmiaChris Pritchard93% (30)
- EKG Cheat SheetДокумент9 страницEKG Cheat SheetAlert Twitter100% (5)
- Lab CheatsheetДокумент1 страницаLab CheatsheetRick Frea86% (7)
- Basic Arrhythmia RulesДокумент3 страницыBasic Arrhythmia Rulesgreenflames0997% (30)
- EKG Practice TestДокумент16 страницEKG Practice TestAbdul Rohim100% (1)
- Acid-Base WorksheetДокумент2 страницыAcid-Base WorksheetMayer Rosenberg100% (18)
- EKG Pocket GuideДокумент2 страницыEKG Pocket GuideFabian Ramirez HincapiéОценок пока нет
- EKG | ECG Interpretation. Everything You Need to Know about 12-Lead ECG/EKG InterpretationОт EverandEKG | ECG Interpretation. Everything You Need to Know about 12-Lead ECG/EKG InterpretationРейтинг: 3 из 5 звезд3/5 (1)
- EKG | ECG: An Ultimate Step-By-Step Guide to 12-Lead EKG | ECG Interpretation, Rhythms & Arrhythmias Including Basic Cardiac DysrhythmiasОт EverandEKG | ECG: An Ultimate Step-By-Step Guide to 12-Lead EKG | ECG Interpretation, Rhythms & Arrhythmias Including Basic Cardiac DysrhythmiasРейтинг: 3 из 5 звезд3/5 (5)
- EKG Flash CardsДокумент5 страницEKG Flash CardsRyann Sampino FreitasОценок пока нет
- Cardiac Med ChartsДокумент6 страницCardiac Med ChartsNursingSchoolNotes100% (15)
- Cardiac DrugsДокумент5 страницCardiac Drugseric100% (17)
- Inherent Rates: Cardiovascular System Alterations Module BДокумент7 страницInherent Rates: Cardiovascular System Alterations Module Bmp_329Оценок пока нет
- Cardiac Study GuideДокумент11 страницCardiac Study Guidejenwiley318096% (73)
- ACLS EKG Rhythms and InterpretationДокумент10 страницACLS EKG Rhythms and Interpretationdonheyzz_02Оценок пока нет
- Cardiac MedicationsДокумент9 страницCardiac Medicationsnovikane100% (1)
- Ekg PracticeДокумент7 страницEkg PracticeMichelle Cobb Matthews100% (1)
- ECG ReadingДокумент11 страницECG ReadingSuresh Shrestha100% (1)
- Dysrhythmia Recognition Pocket Reference Card PDFДокумент14 страницDysrhythmia Recognition Pocket Reference Card PDFjenn1722100% (2)
- The 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsОт EverandThe 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsОценок пока нет
- Presentation of Audrey M Battu From Clinton Health Access Initiative (CHAI)Документ17 страницPresentation of Audrey M Battu From Clinton Health Access Initiative (CHAI)bobbyramakant0% (1)
- ECG StripsДокумент5 страницECG Stripssurviving nursing school100% (1)
- EKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!От EverandEKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!Оценок пока нет
- Cardiac Tamponade, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandCardiac Tamponade, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- May/No P: Inverted/B/ A Qrs P (Befor e QRS) - 0.12Документ3 страницыMay/No P: Inverted/B/ A Qrs P (Befor e QRS) - 0.12is_aradanas0% (1)
- Spotlight On Cardiac DrugsДокумент2 страницыSpotlight On Cardiac Drugspauerish100% (2)
- Critical Care - Hemodynamic Monitoring TableДокумент7 страницCritical Care - Hemodynamic Monitoring TableVictoria Romero100% (2)
- Reading A EKGДокумент10 страницReading A EKGMayer Rosenberg100% (15)
- Ekg Guidelines PDFДокумент7 страницEkg Guidelines PDFd.ramadhan100% (1)
- EKG Rhythms2 PDFДокумент7 страницEKG Rhythms2 PDFAya KamajayaОценок пока нет
- A Simplified ECG GuideДокумент4 страницыA Simplified ECG Guidejalan_z96% (27)
- Mini Test QUIZДокумент9 страницMini Test QUIZAbdul RohimОценок пока нет
- ECG Interpretation - Axis and Conduction AbnormalitiesДокумент9 страницECG Interpretation - Axis and Conduction Abnormalitiesradha1000100% (1)
- Ecg Reading NotesДокумент17 страницEcg Reading NotesMarian FloresОценок пока нет
- ECG StripsДокумент5 страницECG StripsNursingSchoolNotes100% (1)
- ECG and ArrhythmiasДокумент25 страницECG and ArrhythmiasRashed ShatnawiОценок пока нет
- ECGДокумент6 страницECGMatthew MackeyОценок пока нет
- ECG & EKG Interpretation: How to interpret ECG & EKG, including rhythms, arrhythmias, and more!От EverandECG & EKG Interpretation: How to interpret ECG & EKG, including rhythms, arrhythmias, and more!Оценок пока нет
- Congenital Heart Diseases, A Simple Guide to these Medical ConditionsОт EverandCongenital Heart Diseases, A Simple Guide to these Medical ConditionsОценок пока нет
- Advance Cardiac Life Support: Short, Sweet and to the PointОт EverandAdvance Cardiac Life Support: Short, Sweet and to the PointРейтинг: 3 из 5 звезд3/5 (2)
- PulseДокумент43 страницыPulseAngelo LacisteОценок пока нет
- Pulse 160311110553Документ43 страницыPulse 160311110553forever studentОценок пока нет
- Arrhythmias Sherry Vickers, RN, MSN, CCRNДокумент9 страницArrhythmias Sherry Vickers, RN, MSN, CCRNSydney DeringОценок пока нет
- Ngaji Arrythmia Cordis 3Документ122 страницыNgaji Arrythmia Cordis 3Dhita Dwi NandaОценок пока нет
- Approach To Delay PubertyДокумент33 страницыApproach To Delay PubertyRaja Iqbal Mulya HarahapОценок пока нет
- Nurses Notes TBДокумент4 страницыNurses Notes TBSanvar Mal Soni0% (2)
- Healing Following Implant Surgery: Osseous Healing-Early PhaseДокумент2 страницыHealing Following Implant Surgery: Osseous Healing-Early PhaseUrjita PatilОценок пока нет
- The British Journal of Cardiology May-June 2010, Volume 17 Supplement 2Документ16 страницThe British Journal of Cardiology May-June 2010, Volume 17 Supplement 2mbarrales_4Оценок пока нет
- Group 7 (GIT & Hepatobiliary Case Simulation)Документ41 страницаGroup 7 (GIT & Hepatobiliary Case Simulation)Zil Kamleshkumar PanchalОценок пока нет
- Renal MedsurgДокумент14 страницRenal MedsurgCliff Lois ╭∩╮⎷⎛⎝⎲⏝⏝⎲⎠⎷⎛╭∩╮ Ouano100% (1)
- Dry Fasting The AMAZING Health Benefits Everyone Should Know AboutДокумент4 страницыDry Fasting The AMAZING Health Benefits Everyone Should Know AboutMariaОценок пока нет
- E Stimation of HemoglobinДокумент13 страницE Stimation of HemoglobinSANAОценок пока нет
- Algorithm GERD Primary Care Pathway Ahs SCN DH 2020 15262Документ7 страницAlgorithm GERD Primary Care Pathway Ahs SCN DH 2020 15262Mihaela ShimanОценок пока нет
- Primer On Nephrology 2022Документ1 713 страницPrimer On Nephrology 2022Maievp53100% (1)
- First Aid Kits & Their ImportanceДокумент25 страницFirst Aid Kits & Their ImportanceJennette BelliotОценок пока нет
- Deyo 1992Документ6 страницDeyo 1992Wwwanand111Оценок пока нет
- Guideline Perkeni 2019 - 4Документ36 страницGuideline Perkeni 2019 - 4jktrlsОценок пока нет
- Vein Artery Capillary: Thin Wall Wide Lumen Valve Thick Wall Narrow Lumen One Cell Thick WallДокумент1 страницаVein Artery Capillary: Thin Wall Wide Lumen Valve Thick Wall Narrow Lumen One Cell Thick WallHuiso RohОценок пока нет
- Understanding Depression and SuicideДокумент27 страницUnderstanding Depression and Suicideproject creatorОценок пока нет
- Presc Audit ReportДокумент85 страницPresc Audit ReportAnuj KaushalОценок пока нет
- American College of Women's Health PhysiciansДокумент16 страницAmerican College of Women's Health PhysiciansSex & Gender Women's Health CollaborativeОценок пока нет
- Abdominal Swelling and Ascites: Global ConsiderationsДокумент5 страницAbdominal Swelling and Ascites: Global ConsiderationsJacob BorongОценок пока нет
- Common Breast DiseasesДокумент64 страницыCommon Breast Diseasesamirahmei100% (1)
- Informative Speech Outline Group 3Документ4 страницыInformative Speech Outline Group 3Princee RaaidОценок пока нет
- FM Theme2-5Документ61 страницаFM Theme2-5Jolena Fajardo SajulgaОценок пока нет
- NyeriДокумент33 страницыNyeriAndriHernadiОценок пока нет
- Jurnal BTKV Herman 1Документ11 страницJurnal BTKV Herman 1Elyas MuhammadОценок пока нет
- Bhopal (M.P.) : Assignment OnДокумент9 страницBhopal (M.P.) : Assignment OnamitОценок пока нет
- Basic First Aid (Bfa)Документ118 страницBasic First Aid (Bfa)Hamza Moussa100% (1)
- Veneracion NCP 1Документ2 страницыVeneracion NCP 1Romm JacobОценок пока нет
- Science Form 3 PPTnewДокумент9 страницScience Form 3 PPTnewRedzuan SulaimanОценок пока нет
- Lambdoid Sutures: at The Coronal SutureДокумент14 страницLambdoid Sutures: at The Coronal SutureSyed Irfan ArifОценок пока нет
- First Aid For Snake BiteДокумент11 страницFirst Aid For Snake BiteHenryVanDerSchyffОценок пока нет