Академический Документы
Профессиональный Документы
Культура Документы
Coagulacionn Cambios y ObesidadD
Загружено:
Jack ButcherАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Coagulacionn Cambios y ObesidadD
Загружено:
Jack ButcherАвторское право:
Доступные форматы
Thrombosis Research 129 (2012) 204206
Contents lists available at SciVerse ScienceDirect
Thrombosis Research
journal homepage: www.elsevier.com/locate/thromres
Letter to the Editors-in-Chief
Obesity-related Coagulation Changes in Pregnancy ,
Dear Editors,
Obesity, a health concern of increasing importance in developed
countries, is associated with a four- to ve-fold increased risk of venous
thromboembolism (VTE) in pregnancy [1,2]. In one study, obese pregnant women were three times more likely to suffer a pulmonary embolism (PE) than a deep vein thrombosis (DVT), placing them at greater
risk for mortality than non-obese gravidas [2]. Obesity is also associated
with poor pregnancy outcomes, including a 40 percent increased risk for
stillbirth compared to non-obese gravidas [3].
A respectable body of literature has documented many of the
changes in clotting and brinolysis during normal pregnancy, but little has been reported on the effect of obesity on these processes [48].
We hypothesize that the increased risk of VTE in pregnancy associated with obesity, while likely multifactorial, is partly explained by
changes in coagulation proteins. We compared clotting factor levels
in obese and non-obese pregnant women with the purpose of identifying specic changes in obese gravidas that might place them at
higher risk for VTE than non-obese gravidas.
functional protein S, prothrombin time (PT), activated partial thromboplastin time (aPTT), and activated protein C resistance (APC resistance) were obtained using a Diagnostica Stago STA coagulation
analyzer until 6/2006 or the Diagnostica Stago Evolution from
6/2006 to 12/2006 (Diagnostica Stago, Asnieres, France). Total and
Free Protein S antigen levels were measured by ELISA (Asserachrom
Total Protein S and Asserachrom Free Protein S, Diagnostica Stago,
Asnieres France).
Demographic data and assay data were compiled and analyzed.
Student's t-test was used to compare demographic variables and factor levels between the obese and non-obese subjects. Chi square test
was used to compare distribution of race and co-morbidities between
obese and non-obese groups. Linear regression analysis was then performed for coagulation factors with respect to the other coagulation
factors and demographic variables. Pearson correlation coefcients
(r) were determined to measure the strength of correlations between
coagulation factors and demographic variables.
Finally, all subjects were divided into ve subgroups according to
BMI: BMI b 25 kg/m 2, BMI = 25 to b 30 kg/m 2, BMI = 30 to b 40 kg/m 2,
BMI = 40 to b 50 kg/m 2, and BMI N 50 kg/m 2. This allowed measurement of coagulation factors as a function of degree of obesity. Analysis
of variance (ANOVA) tests were performed to compare the factor
levels across the various BMI subgroups. A p value b0.05 was considered statistically signicant.
Materials and Methods
This was a retrospective cohort study comparing prothrombotic and
brinolytic factors between obese and non-obese pregnant women. The
study population was derived from control subjects who were enrolled
at Duke University Medical Center (DUMC) as part of a multi-center
study of intrauterine growth restriction (IUGR) between August 2003
and December 2006. The study was approved by the Institutional Review
Boards at DUMC (IRB numbers 4698-03-4R0ER through 4698-06-R3ER)
and Center for Disease Control and Prevention (CDC). Women age 18 or
older with normally grown singleton gestations were enrolled between
24 and 40 weeks gestation. Subjects with fetal anomalies, preeclampsia,
prolonged premature rupture of the membranes (N 4 weeks), history of
VTE or receiving therapeutic anticoagulation were excluded.
Approximately 25 cc of blood was collected in sodium citrate from
each subject upon enrollment. Demographic data including maternal
age, race, gestational age, height, weight, medical comorbidities, and
personal habits (i.e. tobacco use) were obtained at enrollment in the
study. Obesity was dened as a body mass index (BMI) N30 kg/m 2 at
the time of enrollment.
Blood samples were processed by the Clinical Hemostasis Laboratory of the Division of Blood Disorders at the CDC. Determination of
levels for factors II, VII, and VIII, brinogen, plasminogen, protein C,
Data were originally presented at XXII Congress of the International Society on
Thrombosis and Hemostasis in Boston, Massachusetts on July 16, 2009.
The ndings and conclusions in this report are those of the authors and do not
necessarily represent the ofcial position of the Centers for Disease Control and
Prevention.
0049-3848/$ see front matter 2011 Elsevier Ltd. All rights reserved.
doi:10.1016/j.thromres.2011.08.023
Results
A total of 182 control subjects were identied from the IUGR study.
From this group, 175 met inclusion/exclusion criteria and complete laboratory data were available on 166 subjects. The study population comprised 112 obese subjects, dened as BMI N30 kg/m2 at the time of
enrollment, and 54 non-obese subjects (BMI b 30 kg/m2).
Table 1
Study Population Characteristics.
Age (y)
Parity n (range)
Gestational Age (wk)
Race n (%)
Caucasian
African-American
Hispanic
Other
Comorbidities n (%)
Pre-existing Diabetes
Coronary artery disease
Hypertension
Gestational Diabetes
Tobacco use
BMI b 30 (n = 54)
BMI N 30 (n = 112)
p value
30.3 +/ 6.7
1.06 (04)
32.9 +/ 3.7
29.2 +/ 5.9
1.29 (06)
34.3 +/ 2.7
31 (57)
17 (32)
4 (7)
2 (4)
47 (40)
65 (55)
5 (4.2)
1 (0.8)
0.291
0.238
b0.01
b0.05
-
7
1
7
4
5
20 (17.9)
2 (1.8)
32 (28.6)
20 (17.9)
14 (12.5)
0.505
1
b0.05
0.099
0.613
(13)
(1.9)
(13)
(7.4)
(9.3)
BMI, body mass index.
Data are mean +/ standard deviation or number with range or percentage.
Letter to the Editors-in-Chief
Table 2
Coagulation Factors in Non-obese and Obese Subjects.
PT (sec)
aPTT (sec)
Plasminogen (%)
Fibrinogen (mg/dL)
Factor II (%)
Factor VII (%)
Factor VIII (%)
APC resistance
Protein C (%)
Functional Protein S (%)
Total Protein S Ag (%)
Free Protein S Ag (%)
Reference
Range
BMI b 30
BMI N 30
p value
11.8 - 14.5
22.9 - 35.2
68 - 134
180 - 475
82 - 144
64 - 151
51 - 157
1.96 - 3.18
83 - 162
52 - 130
59 - 158
51 - 122
12.6 +/ 0.6
27.5 +/ 2.6
134.6 +/ 15.3
471.9 +/ 69.9
118.7 +/ 16.7
178.7 +/ 37.8
273.2 +/ 70.2
2.38 +/ 0.30
120.9 +/ 26.3
36.4 +/ 13.3
75.4 +/ 13.7
50.4 +/ 12.0
12.8 +/ 0.8
28.5 +/ 2.8
140.5 +/ 17.8
549.3 +/ 97.0
118.5 +/ 13.3
176.7 +/ 51.4
262.0 +/ 69.1
2.45 +/ 0.26
123.3 +/ 26.9
38.0 +/ 9.9
79.9 +/ 13.7
51.9 +/ 10.4
0.202
0.041
0.04
b 0.001
0.949
0.807
0.331
0.097
0.586
0.437
0.051
0.419
BMI, body mass index; PT, prothrombin time; aPTT, activated partial thromboplastin
time; APC, activated protein C; Ag, antigen.
Data are mean +/ standard deviation.
Subject BMIs ranged from 20.3 59.1 kg/m2. The mean BMI was
39.7 kg/m2 in the obese group and 26.3 kg/m2 in the non-obese group.
The mean gestational age in the non-obese group was 32.9 +/
3.7 weeks (range 26 to 40 weeks) and in the obese group was 34.3 +/
2.7 weeks (range 27 to 40 weeks). With the exception of hypertension,
which was present in 29 percent of subjects in obese group versus 13 percent in the non-obese group (pb 0.05), there were no signicant differences between the two groups in terms of patient's age, parity, and
medical comorbidities (see Table 1). Obese subjects were more likely to
be African-American and non-obese subjects were more likely to be Caucasian (p b0.05, Table 1).
Both brinogen and plasminogen were signicantly elevated in
the obese group (see Table 2). Plasminogen and brinogen levels
also increased with increasing BMI (see Table 3). A moderate association existed between brinogen and BMI (r = 0.457), whereas the
association between BMI and plasminogen was weaker (r = 0.262).
In linear regression analyses, increases in brinogen levels were
associated with increasing plasminogen levels and vice versa
(p b 0.001). There were no associations between medical comorbidities and brinogen or plasminogen levels. Race and parity had no effect on brinogen or plasminogen levels. Increased brinogen levels
were associated with increasing gestational age (p b 0.001) and plasminogen levels appeared to decrease with increasing gestational age
(p b 0.001) in regression analysis. There was no association between
brinogen levels and maternal age (p = 0.107), whereas plasminogen
levels appeared to decrease with increasing maternal age (p = 0.008).
Activated partial thromboplastin times (aPTT) were slightly elevated
in the obese subjects compared to non-obese (p = 0.041, see Table 2)
205
and the highest mean aPTT was observed in subjects with BMI N50
(see Table 3). There was decreased activated protein C resistance levels
with increasing obesity (p = 0.001 and r = 0.184, see Tables 2 and 3).
With most other coagulation factor levels, there were no signicant differences between obese and non-obese subjects and across BMI categories (see Tables 2 and 3).
Discussion
We report the impact of maternal obesity on coagulation factor
levels in pregnancy. Increased brinogen levels have been observed
in pregnancy and have been noted to increase progressively throughout the pregnancy [5]. To our knowledge, the signicant increase in
brinogen levels related to obesity, above and beyond the normal increase in pregnancy, has not previously been described.
In our obese subjects, the brinogen levels were 16% higher than
in non-obese and overweight subjects. Most interestingly, brinogen
levels increased with increasing severity of obesity, with our morbidly obese subjects (BMI N 40) having brinogen levels 30% higher than
subjects with a normal BMI (BMI b25). This suggests an obesityrelated dose-dependent effect on brinogen levels in addition to
the typically observed increased brinogen levels in pregnancy (see
Table 3).
We also report a 4.3% increase in plasminogen levels in our obese
subjects relative to the non-obese subjects. Like brinogen, plasminogen also appears to increase with increasing severity of obesity
(see Table 3). The signicance of increased plasminogen levels with
obesity is unknown, but may indicate a compensatory response to
the increase in brinogen levels or reaction to other changes in coagulation factor levels.
Activated partial thromboplastin times (aPTT) were increased in
obese subjects as well as among the obese subgroups, but the clinical
signicance is unclear since the mean values are all within the normal
reference range. Likewise, we observed a trend toward a signicant
difference in APC resistance between obese and non-obese subjects,
but the mean level for both groups was within the normal range
(N2.20). The APC resistance is a ratio based on the aPTT, which
could explain the higher ratio in obese subjects, but the signicance,
if any, of these ndings or their relationship is unknown. Most subjects in both groups (85.6%) had normal values and less than 5% of
all subjects would be classied as having APC resistance, which is interesting since APC resistance has been reported in up to 40-50% of
normal pregnancies [7,8]. We found no signicant differences between the two groups with respect to other factor levels.
Although the nature of this study limits the ability to control for confounding variables, such as gestational age, race and comorbidities, there
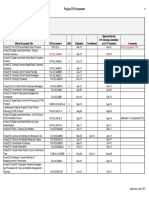
Table 3
Coagulation Factors Grouped by BMI Categories.
BMI
PT (sec)
aPTT (sec)
Plasminogen (%)
Fibrinogen (mg/dL)
Factor II (%)
Factor VII (%)
Factor VIII (%)
APC resistance
Protein C (%)
Functional Protein S (%)
Total Protein S Ag (%)
Free Protein S Ag (%)
Reference
b 25
25 - 30
30 - 40
40 - 50
N50
Range
(n = 16)
(n = 38)
(n = 69)
(n = 29)
(n = 14)
11.8 - 14.5
22.9 - 35.2
68 - 134
180 - 475
82 - 144
64 - 151
51 - 157
1.96 - 3.18
83 - 162
52 - 130
59 - 158
51 - 122
12.8 +/ 0.7
28.8 +/ 3.1
138.9 +/ 18.8
460.2 +/ 66.7
126.6 +/ 13.4
175.7 +/ 35.9
265.4 +/ 70.7
2.16 +/ 0.32
121.1 +/ 19.6
38.6 +/ 11.2
76.7 +/ 11.7
50.6 +/ 13.9
12.6 +/ 0.6
27.0 +/ 2.2
132.8 +/ 13.4
476.8 +/ 71.6
115.4 +/ 17.0
179.9 +/ 39.0
276.5 +/ 70.6
2.46 +/ 0.25
120.0 +/ 28.8
35.6 +/ 14.1
74.8 +/ 14.6
50.3 +/ 11.4
12.8 +/ 0.8
27.9 +/ 2.3
137.2 +/ 18.3
523.0 +/ 91.6
117.8 +/ 13.7
177.4 +/ 56.2
261.6 +/ 72.2
2.42 +/ 0.26
120.4 +/ 25.7
37.7 +/ 8.2
78.7 +/ 14.0
51.3 +/ 9.6
12.7 +/ 0.6
29.2 +/ 2.9
143.7 +/ 16.3
600.0 +/95.3
118.4 +/ 11.3
177.4 +/ 43.6
269.2 +/ 69.4
2.49 +/ 0.26
124.9 +/ 26.5
35.6 +/ 12.2
81.1 +/ 14.0
51.3 +/ 11.0
12.9 +/ 0.7
29.9 +/ 4.1
149.9 +/ 14.3
574.1 +/ 82.9
122.3 +/ 14.9
171.9 +/43.6
248.9 +/ 53.3
2.52 +/ 0.24
134.2 +/ 32.0
44.7 +/ 9.8
83.0 +/ 11.3
56.7 +/ 12.8
BMI, body mass index; PT, prothrombin time; aPTT, activated partial thromboplastin time; APC, activated protein C; Ag, antigen.
Data are mean +/ standard deviation.
p value
NS
0.001
0.009
b0.001
NS
NS
NS
0.001
NS
NS
NS
NS
206
Letter to the Editors-in-Chief
is still a strong relationship between brinogen and obesity. Though brinogen is expected to increase over the course of pregnancy and the
difference in mean gestational age between obese and non-obese subjects reached statistical signicance (see Table 1), this difference is not
clinically signicant and we do not think that this accounts for the difference in brinogen levels between the obese and non-obese subjects.
Although we have identied an association between obesity and
brinogen in the context of pregnancy, this association has also
been identied in non-pregnant populations, specically patients undergoing bariatric surgery [9]. Additional work is needed to evaluate
the consequences of the relationship between obesity and increased
brinogen levels. Further study of obesity's effect on coagulation factors in pregnancy may provide new insight into the causes underlying
the increased risk of poor pregnancy outcomes and complications in
obese women.
Conict of Interest Statement
The contributing authors have no relevant conicts of interest to
disclose.
References
[1] James AH, Jamison MG, Brancazio LR, Myers ER. Venous thromboembolism during
pregnancy and the postpartum period: incidence, risk factors, and mortality. Am J
Obstet Gynecol 2006;194:13115.
[2] Larsen TB, Sorensen HT, Gislum M, Johnsen SP. Maternal smoking, obesity, and risk
of venous thromboembolism during pregnancy and the puerperium: a populationbased nested case-control study. Thromb Res 2007;120:5059.
[3] Salihu HM, Dunlop AL, Hedayatzadeh M, Alio AP, Kirby RS, Alexander GR. Extreme
obesity and risk of stillbirth among black and white gravidas. Obstet Gynecol
2007;110:5527.
[4] Cerneca F, Ricci G, Simeone R, Malisano M, Alberico S, Guaschino S. Coagulation and
brinolysis changes in normal pregnancy. Increased levels of procoagulants and reduced levels of inhibitors during pregnancy induce a hypercoagulable state, combined with a reactive brinolysis. Eur J Obstet Gynecol Reprod Biol 1997;73:316.
[5] Stirling Y, Woolf L, North WR, Seghatchian MJ, Meade TW. Haemostasis in normal
pregnancy. Thromb Haemost 1984;52:17682.
[6] Jorgensen M, Philips M, Thorsen S, Selmer J, Zeuthen J. Plasminogen activator
inhibitor-1 is the primary inhibitor of tissue-type plasminogen activator in pregnancy plasma. Thromb Haemost 1987;58:8728.
[7] Clark P, Brennand J, Conkie JA, McCall F, Greer IA, Walker ID. Activated protein C
sensitivity, protein C, protein S and coagulation in normal pregnancy. Thromb
Haemost 1998;79:116670.
[8] Holmes VA, Wallace JM. Haemostasis in normal pregnancy: a balancing act?
Biochem Soc Trans 2005;33(Pt 2):42832.
[9] Overby DW, Kohn GP, Cahan MA, Galanko JA, Colton K, Moll S, Farrell TM. Prevalence
of thrombophilias in patients presenting for bariatric surgery. Obes Surg 2009;19:
127885.
Michael P. Smrtka
Betty Thames
Duke University Medical Center, Department of Obstetrics and
Gynecology, Durham, North Carolina
Corresponding author at: Duke University Medical Center,
Department of Obstetrics and Gynecology , DUMC Box 3967, Durham,
NC 27710. Tel.: + 1 919 681 5220; fax: +1 919 681 7861.
E-mail address: michael.smrtka@duke.edu (M.P. Smrtka).
Michele Beckman
Centers for Disease Control and Prevention,
National Center for Birth Defects and Developmental Disabilities,
Division of Blood Disorders, Atlanta, Georgia
Dimple Rajgor
Duke University Medical Center,
Center for Excellence in Surgical Outcomes, Durham, North Carolina
Mihir Gandhi
Biostatistics, Singapore Clinical Research Institute, Singapore
Centre for Quantitative Medicine, Ofce of Clinical Sciences, Duke-NUS
Graduate Medical School, Singapore
Andra H. James
Duke University Medical Center, Department of Obstetrics and
Gynecology, Durham, North Carolina
10 June 2011
Вам также может понравиться
- Allen2009 PDFДокумент8 страницAllen2009 PDFJack ButcherОценок пока нет
- Neumonia AspirativaДокумент11 страницNeumonia AspirativaJack ButcherОценок пока нет
- Alcohol Alcohol Algodon Algodon Algodon L AlgodonДокумент1 страницаAlcohol Alcohol Algodon Algodon Algodon L AlgodonJack ButcherОценок пока нет
- Neumonia AspirativaДокумент11 страницNeumonia AspirativaJack ButcherОценок пока нет
- Clinical CasesДокумент183 страницыClinical Casesdaisyputih80% (5)
- Clinical CasesДокумент183 страницыClinical Casesdaisyputih80% (5)
- Bouch Lario To U 2014 GGGДокумент7 страницBouch Lario To U 2014 GGGJack ButcherОценок пока нет
- AbruptionДокумент12 страницAbruptionAdhy PallyОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Mullā Ṣadrā and Causation - Rethinking A Problem in Later Islamic Philosophy AuthorДокумент15 страницMullā Ṣadrā and Causation - Rethinking A Problem in Later Islamic Philosophy AuthorKadag LhundrupОценок пока нет
- Fret Position Calculator - StewmacДокумент1 страницаFret Position Calculator - StewmacJuan Pablo Sepulveda SierraОценок пока нет
- Latihan To: Nilai: 7.4 Benar: 37 Salah: 13Документ17 страницLatihan To: Nilai: 7.4 Benar: 37 Salah: 13glensОценок пока нет
- Approved Project 25 StandardsДокумент5 страницApproved Project 25 StandardsepidavriosОценок пока нет
- Understanding Bernoulli's Principle Through Simulations PDFДокумент4 страницыUnderstanding Bernoulli's Principle Through Simulations PDFIoannis GaroufalidisОценок пока нет
- Iron Ore ProcessДокумент52 страницыIron Ore Processjafary448067% (3)
- Exercise 9 Two Factor Factorial Experiments and Derivation of Expected Mean SquaresДокумент14 страницExercise 9 Two Factor Factorial Experiments and Derivation of Expected Mean SquaresHasmaye PintoОценок пока нет
- Relationsh Between EM and Young S ModuliДокумент7 страницRelationsh Between EM and Young S ModuliDwight AndersonОценок пока нет
- DCS YokogawaДокумент17 страницDCS Yokogawasswahyudi100% (1)
- Cell Wall Synthesis InhibitorsДокумент6 страницCell Wall Synthesis InhibitorsRPh Krishna Chandra JagritОценок пока нет
- Generalized Anxiety DisorderДокумент24 страницыGeneralized Anxiety DisorderEula Angelica OcoОценок пока нет
- A Presentation On-: Dr. Nikhil Oza Intern BvdumcДокумент43 страницыA Presentation On-: Dr. Nikhil Oza Intern BvdumcMaheboob GanjalОценок пока нет
- BS746 2014Документ22 страницыBS746 2014marco SimonelliОценок пока нет
- Communication Models in Internet of Things: A SurveyДокумент5 страницCommunication Models in Internet of Things: A SurveyIJSTEОценок пока нет
- VTA28-G5: Fuel OptimizedДокумент3 страницыVTA28-G5: Fuel OptimizedIslam HemdanОценок пока нет
- Overall Method StatementДокумент33 страницыOverall Method Statementsaranga100% (1)
- Sheet Metal Manufacturing Companies NoidaДокумент9 страницSheet Metal Manufacturing Companies NoidaAmanda HoldenОценок пока нет
- Five Star Hotel and ResortДокумент9 страницFive Star Hotel and ResortAISHОценок пока нет
- Abdominal Examination OSCE GuideДокумент30 страницAbdominal Examination OSCE Guideزياد سعيدОценок пока нет
- Tesla Magazine Vol4Документ48 страницTesla Magazine Vol4jonathan100% (1)
- Paranoia XP - Gamemaster Screen Booklet - Mandatory Fun Enforcement PackДокумент24 страницыParanoia XP - Gamemaster Screen Booklet - Mandatory Fun Enforcement PackStBash100% (3)
- Tsel Manual ThermoselДокумент25 страницTsel Manual ThermoselPedro AlvelaisОценок пока нет
- PEДокумент12 страницPEMae Ann Base RicafortОценок пока нет
- Motor CAT C13 AcertДокумент3 страницыMotor CAT C13 AcertJosé Gonzalez100% (4)
- Marvell 88F37xx Product Brief 20160830Документ2 страницыMarvell 88F37xx Product Brief 20160830Sassy FiverОценок пока нет
- Navy Supplement To The DOD Dictionary of Military and Associated Terms, 2011Документ405 страницNavy Supplement To The DOD Dictionary of Military and Associated Terms, 2011bateljupko100% (1)
- Aluminium Alloy - Wikipedia, The Free EncyclopediaДокумент12 страницAluminium Alloy - Wikipedia, The Free EncyclopediaAshishJoshi100% (1)
- 09.tracheostomy Management by Speech Language Pathologists in SwedenДокумент12 страниц09.tracheostomy Management by Speech Language Pathologists in SwedenCarlonchaCáceresОценок пока нет
- Zest O CorporationДокумент21 страницаZest O CorporationJhamane Chan53% (15)
- LPPДокумент4 страницыLPPMargarida ReisОценок пока нет