Академический Документы
Профессиональный Документы
Культура Документы
Autoimmune and Collagen Disorder - Case Studies
Загружено:
viscosity2004Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Autoimmune and Collagen Disorder - Case Studies
Загружено:
viscosity2004Авторское право:
Доступные форматы
AUTOIMMUNE AND COLLAGEN DISORDER CASE STUDIES
1. A 37 year old female presents with slowly progressive hair loss over the last several months.
She notes occasional scaling and redness in her scalp and on her face. She feels that sun
exposure made her face rash worse. She has mild fatigue, but continues to work. She also notes
that her fingertips turn blue-purple and are painful when exposed to cold.
Lab tests include a C3 serum complement test that is slightly depressed. Urinalysis, serum
creatinine, and CBC are normal. Tests for antibodies to nuclear antigens (ANA) and antidsDNA are ordered. What does the ANA test show?
(a) Positive ANA, Speckled pattern
(b) Positive ANA, Homogenous pattern
(c) Positive ANA, Nuclear membrane
pattern
2. What does the Crithidia test show?
(a) Positive kinetoplast, positive for anti-dsDNA
(b) Positive nucleus, not specific for anti-dsDNA
(c) Positive parabasilar body, anti-dsDNA negative
1 OF 8
AUTOIMMUNE AND COLLAGEN DISORDER CASE STUDIES
3. A 53 year old woman notes that her fingers are painful and she has lost grip strength over the
last 2-3 months. She has been taking 1 or 2 tablets of over-the-counter ibuprofen 5 times a day
with minimal improvement.
Physical exam shows mild tenderness and swelling at the proximal interphalangeal joints and
metacarpal phalangeal joints of the second through fifth fingers of both hands.
This figure demonstrates marked swelling of several proximal interphalangeal joints and mild
swelling of the metacarpal-phalangeal ('knuckle') joints.
She wears contact lenses, has had a little more trouble with "mattering" on her eyes, and
occasionally has used eye drops for red eyes over the last 6 months. She also notes that her
mouth has been unusually dry, and she has trouble swallowing dry foods unless water is
available to wash them down. Her mouth and conjunctiva look dry.
Tear production was measured by performing a Schirmer's test, which uses calibrated filter
paper to measure the amount of tear production in 5 minutes. Press the "Play" button for a
demonstration of the Schirmer's test.
For a normal Schirmer's test, 15 mm or more of the filter paper becomes wet over 5 minutes.
Less than 5 mm of wetting is definitely abnormal, and values in between are indeterminate.
Laboratory tests include an elevated ESR and a positive test for rheumatoid factor. An ANA test
was also performed.
What is the ANA pattern?
(a) Mixed speckled and nucleolar
(b) Mixed homogeneous and nucleolar
(c) Homogenous
2 OF 8
AUTOIMMUNE AND COLLAGEN DISORDER CASE STUDIES
4. A 38 year old woman notes that her fingers become painful and turn white on cold exposure.
Her fingers feel somewhat puffy and full. Otherwise, she feels quite well.
Her exam shows normal radial artery pulses. Her fingers are swollen.
This figure demonstrates the white fingers caused by spasm of the digital arteries when they are
exposed to cold, known as 'Raynaud's phenomenon.' This condition may occur in healthy people, but is
more frequent and severe in patients with autoimmune rheumatic diseases.
She has heartburn, which she attributed to eating spicy food. Occasionally she gets up at night
coughing and has noted an acid taste in her mouth.
An upper gastrointestinal tract contrast radiogram demonstrates esophageal reflux, i.e. the swallowed
barium backs up from the stomach into the esophagus.
The figure demonstrates widening of the esophagus and abnormal, upward flow of barium suspension
from the stomach into the esophagus.
General chemistry tests and CBC are normal. ANA is as
shown.
What does the ANA test show? What diagnosis is
associated with this pattern?
(a) The ANA is positive, speckled pattern, which is
seen in a variety of autoimmune rheumatic
diseases
(b) The ANA is positive, multiple nuclear dot
(MND) pattern, which is associated with
autoimmune liver disease
(c) The ANA is positive, centromere pattern, which
is associated with a form of scleroderma
3 OF 8
AUTOIMMUNE AND COLLAGEN DISORDER CASE STUDIES
5. A 52 year old man presents with progressive breathlessness and fever for two days. He has been
coughing up bloody sputum. His nasal mucosa has been slightly bloody and crusted over the
last month. He denies chest pain.
Exam shows crusted blood in both nostrils. Lung exam demonstrates mild wheezing in the left
upper posterior lung field. Heart exam is normal.
Chest x-ray revealed a large mass in the left upper lung, with some evidence of cavity
formation. There is also an abnormality in the right mid-lung field.
Routine labs:
Hematocrit 25%
WBC 25,000/mm3
Platelets 490,000 /mm3
Serum creatinine 2.9 mg/dL
BUN 45 mg/dL
Na 139 meq/L
K 5.0 meq/L
CO2 19 mg/dL
Urinalysis shows 2+ proteinuria, 2+ hematuria, trace WBC. Urine, and sputum gram stains are
negative, and cultures are set up.
Tests for antibodies to basement membrane (antiGBM)
were negative. The ANA test was negative.
A nasal biopsy was performed, but it revealed only nonspecific inflammatory changes.
ANCA testing is ordered.
What does the (ethanol-fixed) ANCA test show? What is
the likely diagnosis?
(a) The ANCA is positive, P-ANCA pattern
Likely diagnosis is microscopic polyangilitis
(MPA)
(b) The ANCA is positive, C-ANCA pattern
Likely diagnosis is Wegener's granulomatosis
(c) The ANCA has an atypical pattern
The clinical correlation is uncertain
4 OF 8
AUTOIMMUNE AND COLLAGEN DISORDER CASE STUDIES
6. A 50 year old woman presented to clinic with shortness of breath and fatigue for the past month.
She has been experiencing tingling and numbness of the fingers and toes. Her tongue has been
sore.
Physical examination. The patient is very pale. The sclera of her eyes are slightly yellow and
conjunctivae are pale. The tongue is smooth and beefy red. The heart exam is normal except for
a resting tachycardia of 110 beats per min. On neurological exam, there was decreased
sensation to pinprick and vibration in her feet.
Laboratory tests: CBC - hematocrit 20, WBC - normal. Red cell indices - MCV 109, Blood
smear - Several polymorphonuclear white cells have five lobes. Total bilirubin 2.5 mg/dl. What
pattern is present on the IFA MSK study?
(a) Antibodies to parietal cells
(b) Antibodies to mitochondria
(c) Antibodies to liver kidney microsomes
(LKM)
5 OF 8
AUTOIMMUNE AND COLLAGEN DISORDER CASE STUDIES
7. A 45 year old woman was seen in clinic with symptoms of progressive fatigue and itching of
her skin over the past five years. The itching initially started on her palms and soles but now has
become widespread. She has noted that her arms and face have become darker. She also
mentioned that her mouth was dry making it difficult to swallow solid food without water. Her
eyes on awaking in the morning felt scratchy. On further questioning, the patient was aware that
her stools were greasy, foul smelling and floated.
Physical examination. She had numerous excoriations (scratch marks) over her extremities and trunk.
The skin of sun exposed areas on her arms and face were more pigmented. Her eyes were slightly
yellow. The mouth and conjunctivae were dry. The exam was otherwise unremarkable.
Laboratory tests: CBC and urinalysis were normal. The alkaline phosphatase was quite elevated.
Bilirubin was 4 mg/dl and mostly direct. The ALT and AST were moderately elevated.
What does the IFA MSK testing show?
(a) Antibodies to parietal cells
(b) Antibodies to mitochondria
(c) Antibodies to liver kidney microsomes
(LKM)
6 OF 8
AUTOIMMUNE AND COLLAGEN DISORDER CASE STUDIES
ANSWERS:
1. The specimen is ANA positive, homogeneous pattern.
The homogeneous pattern has uniform staining of the resting cell nuclei. The dividing cell
chromatin is strongly positive.
The staining is slightly more intense at the outer rim of the nucleus. Antibodies to dsDNA or
histones sometimes have this type of pattern.
2. There is intense staining of the kinetoplast. This is a positive result for anti-dsDNA. Some cells
also have weak staining of the parabasilar body, which is a non-specific finding.
The patient has a high-titer, homogeneous ANA. Anti-dsDNA antibodies were detected by the
Crithidia test. These test results help to diagnose systemic lupus erythematosus (SLE).
3. The resting cells have a very fine speckled staining. The pattern is not considered homogeneous
because the dividing cell chromatin is negative. Many of the cells also have some staining on
the nucleolus.
A speckled pattern ANA can be associated with many disorders, and with antibodies to
'extractable nuclear antigens'.
ELISA tests demonstrate a positive test for antibodies to SS-A/Ro and SS-B/La.
4. The centromere pattern has distinct speckled staining in the resting cells. The chromatin of the
dividing cells also has discrete speckled staining.
The presence of anticentromere antibodies allowed the clinician to confirm the clinical
impression that the patient had limited cutaneous scleroderma, also known as CREST
syndrome.
5. The ANCA test demonstrates a C-ANCA pattern, which is highly associated with Wegener's
granulomatosis.
The C-ANCA pattern stains the cytoplasm of ethanol fixed neutrophils with a granular speckled pattern
that is most intense in the center of the cell.
EIA testing was run to confirm the ANCA pattern. The specimen is strongly positive for anti-PR3,
negative for anti-MPO.
6. The immunofluorescence test shows anti-parietal cell antibodies.
Antibodies that are specific for parietal cells only stain the stomach parietal cells. The kidney layer is
negative.
The patient has a macrocytic anemia and more than the usual number of nuclear lobes in the PMNs,
both of which can be due to vitamin B12 deficiency.
Because of increased red cell turnover, the indirect bilirubin is slightly elevated. The findings suggest
pernicious anemia.
Pernicious anemia is caused by low levels of vitamin B12, which is necessary for normal maturation of
red cells and other cells. Vitamin B12 is not absorbed because of lack of functional intrinsic factor, a
protein produced by the stomach parietal cells.
7 OF 8
AUTOIMMUNE AND COLLAGEN DISORDER CASE STUDIES
ANSWERS (continued):
7. The MSK immunofluorescence pattern shows antibodies to mitochondria.
Mitochondrial antibodies stain the cytoplasm of the parietal cells in the stomach mucosal layer and the
renal tubules in the kidney layer.
This patient has the clinical and laboratory features of primary biliary cirrhosis (PBC). This is an
autoimmune disorder characterized by destruction of the biliary ducts in the liver leading eventually to
cirrhosis. The lack of bilirubin excreted into the small intestine prevents the emulsification of ingested
fat leading to steatorrhea (greasy stools). Patients first note fatigue and itching. The alkaline
phosphatase is elevated early in the course of disease.
Anti-mitochondrial antibodies are detected in 90% of patients with PBC and are present early in the
disease.
The figures show the histologic pattern of a liver biopsy demonstrating primary biliary cirrhosis with
many inflammatory cells destroying bile ducts. A normal biopsy is shown for comparison.
8 OF 8
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Hemorrhagic Unilateral RetinopathyДокумент7 страницHemorrhagic Unilateral RetinopathyHanna_RОценок пока нет
- Antinuclear Antibody TestДокумент3 страницыAntinuclear Antibody TestElise Señadoza Aulmo-BarcenasОценок пока нет
- Laboratory Diagnosis of Autoimmune DiseasesДокумент6 страницLaboratory Diagnosis of Autoimmune DiseasesYustina BubnovaОценок пока нет
- LimfadenopatiДокумент8 страницLimfadenopatiZulkarnain PrakosoОценок пока нет
- Systemic Lupus Erythematosus in Dogs and CatsДокумент7 страницSystemic Lupus Erythematosus in Dogs and CatsJireh SlatОценок пока нет
- Fmge Important TopicsДокумент33 страницыFmge Important Topicsdocprash100% (1)
- Cracking D' Boards Study & Review Center, Inc. Patho SecretsДокумент10 страницCracking D' Boards Study & Review Center, Inc. Patho SecretsKathryn KleinОценок пока нет
- Discoid Lupus Erythematosus: A Profile: Original ArticleДокумент4 страницыDiscoid Lupus Erythematosus: A Profile: Original ArticleAngelin LigiantoОценок пока нет
- Diagnostic MedlabДокумент585 страницDiagnostic MedlabKiko KiwiblokeОценок пока нет
- Ra PDFДокумент28 страницRa PDFVijay SharmaОценок пока нет
- ABMLI Sample Questions 000Документ7 страницABMLI Sample Questions 000samy100% (1)
- Yousaf Ali (Auth.) - Self Assessment Questions in Rheumatology-Humana Press (2009)Документ147 страницYousaf Ali (Auth.) - Self Assessment Questions in Rheumatology-Humana Press (2009)Amr AmalОценок пока нет
- Anti-Nuclear Antibody Test ReportДокумент2 страницыAnti-Nuclear Antibody Test ReportShweta PatilОценок пока нет
- Clinical Presentations of Sjogren's Syndrome in Benghazi, PDFДокумент6 страницClinical Presentations of Sjogren's Syndrome in Benghazi, PDFKhaled AlsaeitiОценок пока нет
- Genetic and Pediatric Diseases Chapter SummaryДокумент16 страницGenetic and Pediatric Diseases Chapter SummaryJustine HungОценок пока нет
- EASL Clinical Practice Guidelines: Autoimmune HepatitisДокумент34 страницыEASL Clinical Practice Guidelines: Autoimmune HepatitisBety Puma PauccaraОценок пока нет
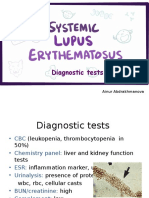
- PBL 3 - SLE (Diagnostic Tests)Документ9 страницPBL 3 - SLE (Diagnostic Tests)Ainur AbdrakhmanovaОценок пока нет
- Group 3 Sjogrens SyndromeДокумент9 страницGroup 3 Sjogrens SyndromeFrancine LerioОценок пока нет
- Ulcerative Dermatosis of The Shetland Sheepdog and Rough Collie Dog May Represent A Novel Vesicular Variant of Cutaneous Lupus ErytheДокумент9 страницUlcerative Dermatosis of The Shetland Sheepdog and Rough Collie Dog May Represent A Novel Vesicular Variant of Cutaneous Lupus ErythejenОценок пока нет
- Test Description Revid TesДокумент4 страницыTest Description Revid Tesjoe andarestaОценок пока нет
- Sle Report NotesДокумент3 страницыSle Report NotesVane UcatОценок пока нет
- Food& The Nutrition Care Process 15Th Edition Student Resources On Evolve Evolve' Access Code Inside ELSEVIERДокумент8 страницFood& The Nutrition Care Process 15Th Edition Student Resources On Evolve Evolve' Access Code Inside ELSEVIEROmar Zenteno-FuentesОценок пока нет
- Systemic Lupus ErythematosusДокумент10 страницSystemic Lupus ErythematosuszkxxyyОценок пока нет
- Liver Function Test InterpretationДокумент48 страницLiver Function Test InterpretationKiattipoom SukkulcharoenОценок пока нет
- Lab Tests Help Diagnose LupusДокумент4 страницыLab Tests Help Diagnose LupusLukes GutierrezОценок пока нет
- Autoimmune Disease PDFДокумент9 страницAutoimmune Disease PDFNikky NamdeoОценок пока нет
- Systemic Lupus ErythematosusДокумент80 страницSystemic Lupus ErythematosusLarissa Miguel Severa100% (2)
- Systemic Lupus Erythematosus: Mariano Marcos State University College of Health Sciences Department of Nursing Batac CityДокумент10 страницSystemic Lupus Erythematosus: Mariano Marcos State University College of Health Sciences Department of Nursing Batac CityEyySiEffVeeОценок пока нет
- PathologyДокумент48 страницPathologyAjay DivvelaОценок пока нет