Академический Документы
Профессиональный Документы
Культура Документы
Preventing Illness and Living With Ill Health
Загружено:
Monique MavronicolasИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Preventing Illness and Living With Ill Health
Загружено:
Monique MavronicolasАвторское право:
Доступные форматы
MONIQUE MAVRONICOLAS PREVENTING ILLNESS AND LIVING WITH ILL HEALTH
1. Introduction
The main objective of this paper is to understand the key characteristics of early
intervention with different methods in preventing ill health. The aim will be to explore a
specific disease Cervical Cancer and the factors that may include possible causes,
prevention, campaigns, treatment, maintenance and statistics surrounding the disease.
Healthcare professionals often use illness and disease interchangeably, however, one
should understand that there is a distinct difference between the two. Tony Ingram defines
them as follows: Disease best refers to an abnormal condition affecting an organism. This
abnormal condition could be due to infection, degeneration of tissue, injury/trauma, toxic
exposure, development of cancer, etc. This is what needs to be cured, especially if its lifethreatening. Illness best refers to the feelings that might come with having a disease.
Feelings like pain, fatigue, weakness, discomfort, distress, confusion, dysfunction, etc. the
reasons people seek healthcare and usually the way people measure their success with
treatment. (http://www.bboyscience.com/disease-vs-illness/).
2. Preventing illness and disease
Healthcare professionals aim to prevent disease than treat the disease and the illnesses
that accompany a disease. Prophylaxis from disease come in many forms, one will often find
that established factors such as the environment, the economy, cultural, social and religious
behaviour will bear influence on these. Preventative measures may include diet, lifestyle,
medication, vaccination, hygiene, religion, meditation and various other forms. History has
taught us that prevention could be broken up into different stages, a mandate to keep the
disease from progressing one could introduce more or new preventative methods. There are
three stages or preventative care, the table below lists the definition of the different stages.
Level
Primary
Definition
Methods to avoid manifestation of disease through excluding possible causes or
MONIQUE MAVRONICOLAS PREVENTING ILLNESS AND LIVING WITH ILL HEALTH
prevention
increasing resistance to disease.
Secondary
prevention
Methods to identify and to attempt to eliminate in an existing disease before the
appearance of symptoms.
Tertiary
prevention
Methods to decrease the negative effect of the suggestive disease, in order to
avoid disability or death, through rehabilitation and management (by means of
medically, chemically, psychologically, sociologically and surgically)
Primordial prevention is the first step in preventative care and consist of the
engagements one has to do to lessen the risks for future illness and disease. It focuses on
comprehensive health factors that could prevent one from the risks of contracting a disease.
Examples of primary prevention methods will include health promotion campaigns against
binge drinking and smoking, eating 5 a day and increasing sport programmes within schools.
These primary prevention methods aim to prevent the onset of certain diseases by shifting
our bad behaviours that could lead to disease or creating a better resistance to the exposure
of illness and disease.
The objectives of primary prevention usually focuses on specific causes and risk factors
which could be prevented through vaccination or immunisation. There has been great
controversy around immunisation and vaccination within the world. UK healthcare providers
(public and private) have done a huge amount of research and have invested a great deal in
informing and educating the public on the pros and cons of getting vaccinated and the
specifics relating to the specific vaccinations. It is an individuals choice whether or not to be
vaccinated or to have their children vaccinated, however, in the USA the government has
made very few exceptions for children to enter public schooling without being vaccinated and
generally have a no vaccination, no school policy.
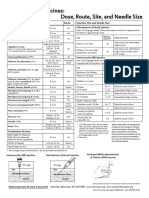
In an attempt to increase preventative primary care the NHS releases a full vaccination /
immunisation schedule every year as illustrated in Figure 1. GP Practices are also
encouraged to invite and remind the people on their practice role of these vaccinations as
and when required, in addition to this, schools and sure start centres also follow up on
vaccinations within children.
MONIQUE MAVRONICOLAS PREVENTING ILLNESS AND LIVING WITH ILL HEALTH
Primary preventative approaches often involve active and passive approaches, example
of an active preventative approach would be regular tooth brushing and flossing to prevent
dental decay and dental related disease, whereas a passive approach would be where a
water company would add fluoride to drinking water or sites using water that is not suitable
for consumption have warning signs.
Figure 1 Complete routine immunisation schedule 2013/2014
(https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/227651/8515
_DoH_Complete_Imm_schedule_A4_2013_09.pdf)
When to
immunise
Two months old
Three months old
Four months old
Between 12 and 13
months old within a
month of the first
birthday
Two and three
years old3
Diseases
protected against
Vaccine
given
Immunisation
site1
Diphtheria, tetanus, pertussis (whooping
cough), polio and Haemophilus influenzae
type b (Hib)
DTaP/IPV/Hib (Pediacel)
Thigh
Pneumococcal disease
Rotavirus
PCV (Prevenar 13)
Rotavirus (Rotarix)
Thigh
By mouth
Diphtheria, tetanus, pertussis, polio and
Hib
DTaP/IPV/Hib (Pediacel)
Thigh
Meningococcal group C disease (MenC)
Rotavirus
Men C (NeisVac-C or Menjugate)2
Rotavirus (Rotarix)
Thigh
By mouth
Diphtheria, tetanus, pertussis, polio and
Hib
DTaP/IPV/Hib (Pediacel)
Thigh
Pneumococcal disease
PCV (Prevenar 13)
Thigh
Hib/MenC
Hib/MenC (Menitorix)
Upper arm/thigh
Pneumococcal disease
Measles, mumps
and rubella (German measles)
PCV (Prevenar 13)
Upper arm/thigh
MMR (Priorix or MMR VaxPRO)2
Upper arm/thigh
Influenza4 (from September)
Flu nasal spray (Fluenz) (annual)
(if Fluenz unsuitable, use inactivated flu
vaccine)
Nostrils
Upper arm
Diphtheria, tetanus, pertussis and polio
dTaP/IPV (Repevax) or
DTaP/IPV (Infanrix-IPV)2
Upper arm
Measles, mumps and rubella
MMR (Priorix or MMR VaxPRO) (check
first dose has been given)2
Upper arm
Cervical cancer caused by human
papillomavirus types 16 and 18 (and
genital warts caused by types 6 and 11)
HPV (Gardasil)
Upper arm
Crown copyright 2013 Available as a pdf only. Published
by Public Health England 2013.
Three years four
months old or soon
after
Girls aged 12 to 13
years old
Tetanus, diphtheria and polio
Td/IPV (Revaxis), and check MMR status
Upper arm
Around 14 years old
MenC
MenC (Meningitec, Menjugate or NeisVacC)2 6
Upper arm
65 years old
Pneumococcal disease
PPV
Pneumococcal
vaccine (Pneumovax II)
polysaccharide
Upper arm
3
The safest way to protect children and adults
Immunisation Informatio
MONIQUE MAVRONICOLAS PREVENTING ILLNESS AND LIVING WITH ILL HEALTH
65 years of age and
older
Influenza4
Flu injection (annual)
Upper arm
70 years old
Shingles (from September)
Shingles (Zostavax)
Upper arm
(subcutaneous)
Immunisations for those at risk7
At birth, 1 month old,
2 months old and 12
months old
Hepatitis B
Hep B
Thigh
At birth
Tuberculosis
BCG
Upper arm (intradermal)
Six months up to two
years
Influenza4
Inactivated flu vaccine (annual)
Upper arm/thigh
Two years up to under
65 years
Pneumococcal disease
PPV Pneumococcal polysaccharide vaccine
(Pneumovax II)
Upper arm
Over two up to less
than 18 years
Influenza4 (from September)
Flu nasal spray (Fluenz) (annual)
(if Fluenz unsuitable, use inactivated flu
vaccine)
Nostrils
Upper arm
18 up to under 65
years
Influenza4
Inactivated flu vaccine (annual)
Upper arm
Pertussis
dTaP/IPV (Repevax)
Upper arm
From 28 weeks of
pregnancy8
1
Where two or more injections are required at once,
these should ideally be given in different limbs.
Where this is not possible, injections in the same
limb should be given 2.5cm apart. For more details
see Chapters 4 and 11 in the Green Book. All
vaccines are given intramuscularly unless stated
otherwise.
NB Where a vaccine is manufactured by more than
one supplier, it may, on occasion be necessary to
substitute an alternative brand.
3
This is defined as children aged two or three years
(but not four years) on 1 September 2013.
4
The vaccine is given prior to the flu season usually
in September and October.
2
This vaccination will be introduced during the
2013/14 academic year.
The vaccine supplied will depend on the brands
available at the time of ordering.
7
See individual chapters of the Green Book for
clinical risk groups.
8
See CMO letter of October 2012.
5
Secondary Preventative methods are the systematically designed to detect the start or
beginning or even early stages of a specific disease and allowing intervention and an
attempt to control the disease before comprehensive symptoms develop. Early interventions
are not only cost effective but also a way of identifying causes and impacts that could be
illuminated in order for one to prolong ones life. Routine checks, whether cholesterol, blood
sugar, cervical screening and mammograms are regularly the first step that leads to early
intervention before other symptoms appear.
The last and final step of preventative care could possible also be seen as manageable
care, these methods are known as tertiary preventative methods. When a patient reaches
tertiary care the disease has in all probability been established and we could assume that
the preventative methods used in primary prevention has been unsuccessful, however, due
to the second preventative stage, the disease were identified in the early stages and have
possibly minimised the full impact of the disease, The focus of tertiary prevention include,
preventing pain and more damage to the human body, attempting to stop any further
4
MONIQUE MAVRONICOLAS PREVENTING ILLNESS AND LIVING WITH ILL HEALTH
progression or any more complications that the disease has already caused and attempting
to reinstate better health and increase the standard of living to the patient.
Figure 2 - Examples of primary, secondary, and tertiary prevention interventions
targeting individuals and populations
Disease
Intervention Primary
level
Secondary
Tertiary
Colorectal
cancer
Individual
Counselling on healthy
lifestyles: dietary
counselling for people at
risk of colorectal cancer,
etc.
Hemoccult stool
testing to detect
colorectal cancer
early
Follow-up exams to
identify recurrence or
metastatic disease:
physical examination,
liver enzyme tests,
chest x-rays, etc.
Population
Publicity campaigns
alerting the public to the
benefits of lifestyle
changes in preventing
colorectal cancers;
promotion of high fibre
diets; subsidies to help
people access exercise
programmes; anti-smoking
campaigns
Organized
colonoscopy
screening
programs
Implementation of
health services
organizational models
that improve access to
high-quality care
Individual
Counselling on safe drug
use to prevent hepatitis C
virus (HCV) transmission;
counselling on safer sex
Screening for
HCV infection of
patients with a
history of
injection drug
use
HCV therapy to cure
infection and prevent
transmission
Population
HCV prevention includes
safer sex practices,
programmes to discourage
needle sharing among
intravenous drug users,
etc.
Establish a
universal testing
system for HCV
in high risk
groups
(Similar to primary
prevention): ensuring
close control of high risk
sites such as tattoo
parlours that have been
associated with
outbreaks
Individual
Nutrition and exercise
counselling
Screening for
diabetes
Referral to cardiac
rehabilitation clinics
Population
Built environment
favourable for active
transport (walking,
bicycling rather than using
a car)
Community level Implementation of
weight loss and
multidisciplinary clinics
exercise
programs to
control metabolic
syndrome
Infectious
diseases:
hepatitis C
Metabolic
syndrome
MONIQUE MAVRONICOLAS PREVENTING ILLNESS AND LIVING WITH ILL HEALTH
3. Cervical Cancer
According to Cancer Research UK in 2011 there were 3064 woman diagnosed with
cervical cancer and in 2012, 919 woman
died as a result of cervical cancer even
though it is considered as the most
preventable cancer. Cervical cancer
deaths have decreased with more than
71% since 1970, yet Cancer Research UK
believes that the main cause of cervical
cancer could have a 100% prevention rate
through early detection: Cervical
screening can prevent around 45% of
cervical cancer cases in women in their
30s, rising with age to 75% in women in
their 50s and 60s, who attend regularly (www.cruk.org/cancerstats).
In 2009 the UK had an extra 400 000 women who went for cervical screenings after the
death of Jade Goodie. Unfortunately the Jade Goodie effect has worn off and new figures
from Cancer Research UK shows that one in three women refuse or make excuses to go for
their cervical screenings and One in five women do not attend screening when invited and
many delay it for more than a year. Awareness campaigns has been launched to encourage
women to attend cervical screenings in the UK include:
GSK in support of Joes Cancer trust launched and new campaign TIME TO
TEST where employers commit to give employees flexible time off to have their
cervical screening tests done
Dr Dawn Harper did a smear test on LIVE television as part of the
NoFearGoSmear Campaign, to show people how 5 minutes of your time might
save your life.
Cervical Screening Awareness Week (CSAW - 15 - 21 June 2015) is a UK-wide
initiative led by Jo's Cervical Cancer Trust. The week aims to highlight the
importance of cervical screening (smear) and how attending a screening
invitation can help to prevent cervical cancer.
NO EXCUSES is a cervical screening campaign launched and produced by NHS
Milton Keynes and Northamptonshire and NHS Leicester, Leicestershire and
MONIQUE MAVRONICOLAS PREVENTING ILLNESS AND LIVING WITH ILL HEALTH
Rutland PCT Cluster
There are a number of causes that increases the risk of cervical cancer development,
these factors include, age, genetics, smoking, HIV, oral contraceptives and most of all, Highrisk human papillomavirus (HPV) infection. There are more than 100 viruses within the HVP
group, of those around 40 types of HPV infections have an effect on ones genital area.
These viruses affect ones skin and moist membranes in our mouths, cervix, throat and anus
and is transmitted through any sexual activity, including oral and anal sex. The virus has the
ability to cause abnormal tissue growth for example in the cervix that has the possibility to
lead to cervical cancer.
As part of the NHS childhood vaccine programme as seen in Figure 2, all girls in year 8
(age 12-13) are offered the vaccine. The NHS believes that just by vaccination, over 400 live
could be saved yearly from cervical cancer. They also believe that in conjunction with the
vaccinations and regular cervical screening (every 3 years) 70% of cervical cancer cases
could be avoided.
Cervical Screenings is so important due to the limited presentable symptoms of cervical
cancer. Some early symptoms of abnormal cell growth and cervical cancer can include,
vaginal bleeding, painful and uncomfortable intercourse and foul smelling vaginal discharge.
However, if these abnormal cells are left untreated and one disregards cervical screening,
this could lead to growths that could lead to cervical cancer. Advance cervical cancer has the
ability to spread out of the cervix into any of the surrounding tissues and organs. If the
cancer starts spreading, more noticeable symptoms might include; bone pain, haematuria
(blood in the urine), constipation, weight loss and even hydronephrosis (severe pain caused
by swollen kidneys).
Should one be diagnosed with cervical cancer the treatments options will be based on
the stage of the cancer. The NHS has a 4 stage cancer scale for cervical cancer:
stage 0 pre-cancer (not cancer as yet) cells have been detected this is called
cervical intraepithelial neoplasia (CIN) or carcinoma in situ (CIS), these are also
listed in stages and can be easily treated and monitored or managed
stage 1 contained within the cervix
stage 2 cancer spread to outside the cervix and the surrounding tissue,
although the cancer has not extended to the tissue lining the pelvic wall or the
lower part of the vagina
tage 3 spread into the pelvic wall and/or lower section of the vagina
stage 4 spread into the bowel, bladder or other organs, such as the lungs
7
MONIQUE MAVRONICOLAS PREVENTING ILLNESS AND LIVING WITH ILL HEALTH
A multidisciplinary team (MDTs) will recommend in the majority of cases that in the event
of early cervical cancer that one have one of three possible options of surgery depending the
spread of the cancer (radical trachelectomy, hysterectomy or pelvic exentertion) or have
radiotherapy, however in some cases a combination of the 2 might be suggested. In
advanced cervical cancer either radiotherapy or chemotherapy or an amalgamation of the
two, often surgery might also be added if possible to remove some growths.
Cervical cancer is survivable in early detection, hence the importance of cervical
screenings, Figure 2 reflects a one year survival chart within the different stages of the
cancer.
Figure 2 Cervical Cancer (C53): 2006-2010 - One-Year Relative Survival (%) by
Stage, Adults Aged 15-99, Former Anglia Cancer Network
(http://info.cancerresearchuk.org/cancerstats/faqs/#How)
Relative survival can be greater than 100% because it accounts for background
mortality. A relative survival figure greater than 100 indicates that people diagnosed have a
better chance of surviving one (five) year(s) after diagnosis than the general population.
Lifestyle changes could have positive effects on living with cervical cancer depends on
the diagnosis and the treatment plan. Treatment may remove and destroy all the cancer for
8
MONIQUE MAVRONICOLAS PREVENTING ILLNESS AND LIVING WITH ILL HEALTH
some woman, and life will continue as normal, but for others the cancer might never go
away. In either of these cases one should look at healthy life changes by means of quitting
smoking, eating well (plenty of fresh fruit and vegetables with a higher intake of fibre foods,
minimising animal fats, red meats, salt and smoked or pickled foods), have a regular low
impact exercise programme, try and stick to sensible alcohol drinking guidelines and try and
have as many alcohol free days as possible and last but not least, emotional support.
Depending on the treatment one has had or having on a continuous basis, it could affect
how one feels. Apart from coping emotionally, one could have ongoing side effects that could
have an additional impact on ones emotional state of well-being. Talk to friends and family,
speak to health professionals if you have questions, join a support group, read every
possible survival story you can find, as hope is as much as part of recovery as all the other
things.
4. Conclusion
Over the years there have been accumulative acknowledgement in the way disease is
treated and managed and often that responses were too late. The aim of the NHS is to
engage people more in their personal health and well-being and prolong their lives be
preventing illness rather than curing. The British journal of cancer reported in December
2013 that nearly half of all cancers diagnosed in the UK every year is attributed by avoidable
life choices such as smoking, not eating enough fresh fruit and vegetables, being overweight
and other environmental factors. Professor Max Parkin, the lead author of the report stated:
Looking at all the evidence, its clear that around 40% of all cancers are caused by things we
mostly have the power to change. (http://www.healthiq.co.uk/component/k2/item/159prevention-is-better-than-cure.html). The concept of preventing illness is just like the old
proverb used by Henry de Bracton An ounce of prevention is worth a pound of cure and
with more prevention comes less need for cure.
5. References
Disease vs Illness available at - http://www.bboyscience.com/disease-vs-illness/
accessed on 10 December 2014
Preventing Illness available at http://www.sciencemuseum.org.uk/broughttolife/themes/treatments/preventing.aspx
accessed on 10 December 2014
9
MONIQUE MAVRONICOLAS PREVENTING ILLNESS AND LIVING WITH ILL HEALTH
Stages of prevention available at - http://phprimer.afmc.ca/Part1TheoryThinkingAboutHealth/Chapter4BasicConceptsInPreventionSurveillanceAndHealthPro
motion/Thestagesofprevention accessed on 10 December 2014
Primary prevention available at http://www.kingsfund.org.uk/projects/gpcommissioning/ten-priorities-for-commissioners/primary-prevention - accessed on 10
December 2014
Prevention and Reduction: A review of strategies for intervening early to prevent or
reduce youth crime and anti-social behaviour available at
http://www.natcen.ac.uk/media/25254/prevention-reduction-review-strategies.pdf - accessed
11 December 2014
Call to Action: Commissioning for Prevention available at http://www.england.nhs.uk/wpcontent/uploads/2013/11/call-to-action-com-prev.pdf accessed 11 December 2014
Preventative medicine, integrative medicine & the health of the public available at
http://www.iom.edu/~/media/Files/Activity%20Files/Quality/IntegrativeMed/Preventive
%20Medicine%20Integrative%20Medicine%20and%20the%20Health%20of%20the
%20Public.pdf accessed on 11 December 2014
Preventative Healthcare available at http://en.wikipedia.org/wiki/Preventive_healthcare
accessed on 11 December 2014
Levels of Medical Care: Primary, Secondary, Tertiary and Quaternary Care available at http://patients.about.com/od/moreprovidersbeyonddocs/a/Stages-Of-Care-PrimarySecondary-Tertiary-And-Quaternary-Care.htm - accessed on 12 December 2014
Primary, Secondary, and Tertiary Prevention: Important in Certification and Practice
available at - www.fhea.com/CertificationCols/level_prevention.htm accessed on 12
December 2014
Cervical Cancer Statistics available at http://www.cancerresearchuk.org/cancerinfo/cancerstats/types/cervix/ accessed on 12 December 2014
Cervical cancer vaccine available at http://www.nhs.uk/Conditions/vaccinations/Pages/hpvhuman-papillomavirus-vaccine.aspx accessed on 12 December 2014
10
MONIQUE MAVRONICOLAS PREVENTING ILLNESS AND LIVING WITH ILL HEALTH
No Excuses available at http://www.noexcuses-nhs.co.uk/ accessed on 12 December
2014
Cervical Screening Awareness Week available at http://www.jostrust.org.uk/getinvolved/campaign/cervical-screening-awareness-week accessed on 12 December 2014
Time-to-test Campaign available at http://time-to-test.com/ accessed on 12 Dcember
2014
NoFearGoSmear campaign available at http://www.itv.com/thismorning/health/no-feargo-smear-cervical-cancer-screening-campaign accessed on 12 December 2014
11
Вам также может понравиться
- Language of PreventionДокумент9 страницLanguage of Prevention1234chocoОценок пока нет
- Reflection Paper EcheДокумент2 страницыReflection Paper Echeceline dela cruz100% (1)
- Thesis Prevention of Nosocomial Infections As Percieved by Staff NursesДокумент7 страницThesis Prevention of Nosocomial Infections As Percieved by Staff NursesDhonnalyn Amene Caballero100% (1)
- Carl Ransom RogersДокумент8 страницCarl Ransom RogersMonique MavronicolasОценок пока нет
- Mental Health Campaign ToolkitДокумент11 страницMental Health Campaign ToolkitMonique MavronicolasОценок пока нет
- Lesson Plan - HPVДокумент6 страницLesson Plan - HPVMonique MavronicolasОценок пока нет
- Roosendaal Study of Vaccinated vs. Unvaccinated Children in The Netherlands: Results SurveyДокумент4 страницыRoosendaal Study of Vaccinated vs. Unvaccinated Children in The Netherlands: Results Surveythomas_austin_189% (9)
- FOH-25 Tuberculosis Screening (M.25)Документ1 страницаFOH-25 Tuberculosis Screening (M.25)Maria CabañasОценок пока нет
- The Problem: (Insert Citation)Документ52 страницыThe Problem: (Insert Citation)Trisha100% (1)
- Describe Five Examples of How Each Level of Disease Prevention Is Practiced in Your CountryДокумент1 страницаDescribe Five Examples of How Each Level of Disease Prevention Is Practiced in Your Countryhasfa konsoОценок пока нет
- Course Work Communicable Diseases RomДокумент5 страницCourse Work Communicable Diseases RomAtim RomeoОценок пока нет
- Chapter 9 - Prevention in General Practice: DefinitionsДокумент20 страницChapter 9 - Prevention in General Practice: Definitionsprofarmah6150Оценок пока нет
- Clinical Epidemiology Assignment I: Submitted By: Ibalawanpynhun WriangДокумент6 страницClinical Epidemiology Assignment I: Submitted By: Ibalawanpynhun WriangElegant WriangОценок пока нет
- Grade 8 Health Quarter 3Документ3 страницыGrade 8 Health Quarter 3montenegrokrishamae36Оценок пока нет
- Neral Practice, Prevention2Документ17 страницNeral Practice, Prevention2Mahmoud hilmyОценок пока нет
- Module 6.1 Prevention and Health ServicesДокумент35 страницModule 6.1 Prevention and Health ServicesSamuel MbiriОценок пока нет
- Hed 313 - Epidemiology-1Документ7 страницHed 313 - Epidemiology-1Tobi OladipupoОценок пока нет
- Health Promotion and Ilness PreventionДокумент7 страницHealth Promotion and Ilness Preventionzach felix100% (1)
- Adult Immunization ScheduleДокумент3 страницыAdult Immunization Schedulemo0nseerratОценок пока нет
- Principles of EpidemiologyДокумент5 страницPrinciples of EpidemiologyJaffar ZabertОценок пока нет
- SGD Lbm1 Modul PrioritasДокумент33 страницыSGD Lbm1 Modul PrioritasNor KhasanahОценок пока нет
- Application of Epidemiology in Health Care DeliveryДокумент15 страницApplication of Epidemiology in Health Care DeliveryDebipriya Mistry100% (5)
- Level of PreventionДокумент54 страницыLevel of PreventionArun kumar100% (1)
- Quinary PreventionДокумент15 страницQuinary Preventionjilaba4171Оценок пока нет
- Levels of Disease PreventionДокумент4 страницыLevels of Disease Preventionkagehaprecious31Оценок пока нет
- 2021-MPHFT-A01 ExamsДокумент13 страниц2021-MPHFT-A01 ExamsƏfąþą RobertОценок пока нет
- SHD Lecture Slides 2023 Themes 5 6Документ44 страницыSHD Lecture Slides 2023 Themes 5 6pinehas nguluОценок пока нет
- Health Study GuideДокумент6 страницHealth Study GuideZaira Beatrice CruzОценок пока нет
- TUIL 4 - Ivan Wima Aditama - 20548 - 05 PDFДокумент6 страницTUIL 4 - Ivan Wima Aditama - 20548 - 05 PDFIvan Wima AditamaОценок пока нет
- Prevention of Disease & Health PromotionДокумент2 страницыPrevention of Disease & Health PromotionGhith WhiuОценок пока нет
- CHN - ManaloДокумент3 страницыCHN - ManaloclydeqtmanaloОценок пока нет
- Antonio SlidesCarnivalДокумент25 страницAntonio SlidesCarnivalSophia Marie DaparОценок пока нет
- A Public Health Intervention Is An Organized Effort To Promote Those Specific Behaviors and Habits That Can Improve PhysicalДокумент5 страницA Public Health Intervention Is An Organized Effort To Promote Those Specific Behaviors and Habits That Can Improve PhysicalYonas MamoОценок пока нет
- Preventive Medicine FunctionsДокумент4 страницыPreventive Medicine Functionsnahomy reyesОценок пока нет
- PBH101 Assignment 01Документ5 страницPBH101 Assignment 01Siam AhmedОценок пока нет
- Questions For Assignment - MoPДокумент11 страницQuestions For Assignment - MoPAbdirahman MohamedОценок пока нет
- Concept of PreventionДокумент48 страницConcept of Preventionmahmoud100% (1)
- IFMSA Program Communicable-DiseasesДокумент6 страницIFMSA Program Communicable-Diseasesshivanjali srivastavaОценок пока нет
- The Stages of Prevention - Primer On Public Health PopulationДокумент2 страницыThe Stages of Prevention - Primer On Public Health PopulationBSN 201450% (2)
- Community NutritionДокумент16 страницCommunity NutritionSathvik BangiramaneОценок пока нет
- Activity Sheet In: MAPEH (Health)Документ12 страницActivity Sheet In: MAPEH (Health)Meycauayan NHS (Region III - Meycauayan City)Оценок пока нет
- Black and WhiteДокумент24 страницыBlack and WhiteGerry PingenОценок пока нет
- Western Mindanao State University College of Nursing Zamboanga CityДокумент16 страницWestern Mindanao State University College of Nursing Zamboanga CityRoshin TejeroОценок пока нет
- Levels of PreventionДокумент5 страницLevels of PreventionSofia JuliaОценок пока нет
- Public Health Group AssignmentДокумент7 страницPublic Health Group AssignmentNANNYONGA OLGAОценок пока нет
- Evidence Based Health Maintenance Protocols (Screening) in Adult/elderlyДокумент58 страницEvidence Based Health Maintenance Protocols (Screening) in Adult/elderlyB 70 Mohit KumarОценок пока нет
- Health Promotion Andprimaryprevention Include Interventionsthatpromote Health Andstriveto Prevent Theinitiation Ofsubstance UseДокумент2 страницыHealth Promotion Andprimaryprevention Include Interventionsthatpromote Health Andstriveto Prevent Theinitiation Ofsubstance UseM MОценок пока нет
- And Through State And: Primary PreferableДокумент3 страницыAnd Through State And: Primary PreferableIBETH NAVARRETEОценок пока нет
- Malaria Measles Mental Fam PlanningДокумент5 страницMalaria Measles Mental Fam PlanningABBEYGALE JOYHN GALANОценок пока нет
- Prevention Models - FINALДокумент4 страницыPrevention Models - FINALAmy LalringhluaniОценок пока нет
- MPH 5103 Lecture 1 - 02092022 - ZTMДокумент38 страницMPH 5103 Lecture 1 - 02092022 - ZTMRezwana SultanaОценок пока нет
- Integrated Management of Childhood IllnessДокумент8 страницIntegrated Management of Childhood IllnessSehar162Оценок пока нет
- Introduction To Epidemiology Dr. Abdikani Ali MbbsДокумент38 страницIntroduction To Epidemiology Dr. Abdikani Ali Mbbsabdikani hassanОценок пока нет
- Strengthen Community ActionsДокумент5 страницStrengthen Community ActionstermskipopОценок пока нет
- Chapter 10 - Health Promotion and Patient EducationДокумент19 страницChapter 10 - Health Promotion and Patient Educationprofarmah6150Оценок пока нет
- One Health IntroductionДокумент20 страницOne Health Introductiondecastro.thomasОценок пока нет
- Models of Health Promotion and Illness Prevention 1Документ7 страницModels of Health Promotion and Illness Prevention 1Krishnaveni MurugeshОценок пока нет
- 8190224-Order 4541206 - EG - Health Promotion PlanДокумент6 страниц8190224-Order 4541206 - EG - Health Promotion PlanKelvin Troubadour MchelseaОценок пока нет
- Integrated Management of Childhood IllnessДокумент5 страницIntegrated Management of Childhood Illnessjulieyauder624Оценок пока нет
- Four Types of Chronic Disease and Prevention MeasuresДокумент4 страницыFour Types of Chronic Disease and Prevention MeasuresjosephineОценок пока нет
- Objectives of EpidemiologyДокумент23 страницыObjectives of EpidemiologyAnitha sujith75% (4)
- Infectious Disease Management:: WWW - Immunise.health - Gov.auДокумент2 страницыInfectious Disease Management:: WWW - Immunise.health - Gov.auCassieJenkinsОценок пока нет
- Guide to Health Maintenance and Disease Prevention: What You Need to Know. Why You Should Ask Your DoctorОт EverandGuide to Health Maintenance and Disease Prevention: What You Need to Know. Why You Should Ask Your DoctorОценок пока нет
- Mold Illness Diet: A Beginner's 3-Week Step-by-Step Guide to Healing and Detoxifying the Body through Diet, with Curated Recipes and a Sample Meal PlanОт EverandMold Illness Diet: A Beginner's 3-Week Step-by-Step Guide to Healing and Detoxifying the Body through Diet, with Curated Recipes and a Sample Meal PlanОценок пока нет
- Long Life Strategy: A guidebook for living a longer, healthier, and more fulfilling lifeОт EverandLong Life Strategy: A guidebook for living a longer, healthier, and more fulfilling lifeОценок пока нет
- Monique Mavronicolas - Research ProjectДокумент44 страницыMonique Mavronicolas - Research ProjectMonique MavronicolasОценок пока нет
- Research Project ReflectionДокумент2 страницыResearch Project ReflectionMonique MavronicolasОценок пока нет
- Advanced Practice Nurses: Promoting Evidence Based Practice and Capturing Impact: Lessons From Two UK StudiesДокумент34 страницыAdvanced Practice Nurses: Promoting Evidence Based Practice and Capturing Impact: Lessons From Two UK StudiesMonique MavronicolasОценок пока нет
- Dissemination Project WritingДокумент9 страницDissemination Project WritingMonique MavronicolasОценок пока нет
- Monique Mavronicolas - Research Project ProposalДокумент3 страницыMonique Mavronicolas - Research Project ProposalMonique MavronicolasОценок пока нет
- Building Resilience, Promoting WellbeingДокумент35 страницBuilding Resilience, Promoting WellbeingMonique MavronicolasОценок пока нет
- Personality and HealthДокумент6 страницPersonality and HealthMonique MavronicolasОценок пока нет
- Mental Health PPPДокумент6 страницMental Health PPPMonique MavronicolasОценок пока нет
- Pass or Fail: Mark - Please Circle The ResultДокумент1 страницаPass or Fail: Mark - Please Circle The ResultMonique MavronicolasОценок пока нет
- Self Harm PDFДокумент2 страницыSelf Harm PDFMonique MavronicolasОценок пока нет
- HPV Lesson Plan PDFДокумент25 страницHPV Lesson Plan PDFMonique MavronicolasОценок пока нет
- Depression PDFДокумент2 страницыDepression PDFMonique MavronicolasОценок пока нет
- Human Papilloma Virus: by Monique MavronicolasДокумент13 страницHuman Papilloma Virus: by Monique MavronicolasMonique MavronicolasОценок пока нет
- Psychosomatic DisordersДокумент11 страницPsychosomatic DisordersJasmin Jacob100% (3)
- Esthetic in Pediatric DentistryДокумент13 страницEsthetic in Pediatric DentistryAtikahОценок пока нет
- Paper 3 Argumentative Essay Alexis-2Документ9 страницPaper 3 Argumentative Essay Alexis-2api-314832012Оценок пока нет
- p3085 PDFДокумент1 страницаp3085 PDFEivon Eyaf Love TormonОценок пока нет
- Child - ImmunizationsДокумент1 страницаChild - ImmunizationsJOHN100% (1)
- Vis DtapДокумент2 страницыVis DtapBeeco SiboroОценок пока нет
- Instructions Design Laboratory Production Animal Vaccine Cell CultureДокумент56 страницInstructions Design Laboratory Production Animal Vaccine Cell CultureRasu KuttyОценок пока нет
- Vaccine Epidemic - Press ReleaseДокумент2 страницыVaccine Epidemic - Press Releasekingofswords100% (1)
- Improving Cold Chain SystemДокумент7 страницImproving Cold Chain SystemEduardОценок пока нет
- A Study On The Implementation of Mother and Child Tracking SystemДокумент28 страницA Study On The Implementation of Mother and Child Tracking Systemsivanayak100% (1)
- A For and Against EssayДокумент4 страницыA For and Against Essayluciana20straОценок пока нет
- Updated Operational Guidelines For Mission IndradhanushДокумент76 страницUpdated Operational Guidelines For Mission IndradhanushZLOOffice BankuraОценок пока нет
- Infection in PediatricДокумент36 страницInfection in PediatricSitaОценок пока нет
- Title Author's Name: Why You Should Vaccinate Your KidsДокумент1 страницаTitle Author's Name: Why You Should Vaccinate Your KidsVir UmlandtОценок пока нет
- Azithromycin in PediatricsДокумент40 страницAzithromycin in PediatricsKishore ChandkiОценок пока нет
- Ms. Sanna MESMAN - EU Legislation On Bluetongue Regarding Control MeasuresДокумент23 страницыMs. Sanna MESMAN - EU Legislation On Bluetongue Regarding Control Measuresvidzr6330Оценок пока нет
- Drugs Re QuestionsДокумент6 страницDrugs Re Questionslipe167Оценок пока нет
- EARSS 2005 - tcm61-34899Документ147 страницEARSS 2005 - tcm61-34899api-3760696Оценок пока нет
- Case Study On: Importance of Mission IndradhanushДокумент9 страницCase Study On: Importance of Mission IndradhanushRohit RaneОценок пока нет
- PD996 Compulsory ImzДокумент2 страницыPD996 Compulsory Imzapi-19824701Оценок пока нет
- Day Scholar Application2007-08Документ13 страницDay Scholar Application2007-08Bild Andhra PradeshОценок пока нет
- Im SQ Admin PDFДокумент2 страницыIm SQ Admin PDFAlvin JjОценок пока нет
- Pulse PolioДокумент6 страницPulse Poliopriyankakgp100% (1)
- Sumbad, Mark Bhen E.-Activity-6-IMCIДокумент3 страницыSumbad, Mark Bhen E.-Activity-6-IMCIMb SumbadОценок пока нет
- In Reply Please Quote:: WWW - Homeaffairs.gov - AuДокумент4 страницыIn Reply Please Quote:: WWW - Homeaffairs.gov - AuLinh TranОценок пока нет
- Rabies BrochureДокумент2 страницыRabies Brochureselvie87Оценок пока нет
- Cost Break Down For Kaluthra Kalu, Mahrgama Nine Puppies and DeltaДокумент10 страницCost Break Down For Kaluthra Kalu, Mahrgama Nine Puppies and DeltaAdopt a Dog in Sri LankaОценок пока нет
- 9851 BCG Vaccine Professional HCWДокумент4 страницы9851 BCG Vaccine Professional HCWIuliana PanaitОценок пока нет
- EPI Vaccines: Department of Vaccines and BiologicalsДокумент25 страницEPI Vaccines: Department of Vaccines and Biologicalssanjaysinghania07Оценок пока нет