Академический Документы
Профессиональный Документы
Культура Документы
Chemical Examination
Загружено:
LAb MehАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Chemical Examination
Загружено:
LAb MehАвторское право:
Доступные форматы
Chemical Examination of Urine
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
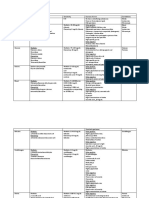
Several colors or intensities of a color for each substance being
tested appear on the chart.
A semi quantitative value of each can be reported.
An estimate of the milligrams per deciliter present is available
for some of the parameters.
A color-producing chemical reaction takes place when the
absorbent pad comes in contact with urine.
The color reactions are interpreted by comparing the color
produced on the pad with a chart supplied by the
manufacturer.
Page
Introduction
Routine chemical examination of urine has changed
dramatically since the early days of urine testing, owing to the
development of the reagent strip method for chemical analysis.
The introduction of the reagent strip currently provide a simple,
rapid screening means for performing medically significant
chemical analysis of urine.
Reagent Strip
An inert plastic strip onto which reagent impregnated test
pads are bonded.
The following are the parameters analyzed using the urinalysis
reagent strip.
pH
Protein
Glucose
Ketones
Blood
Bilirubin
Urobilinogen
Nitrite
Leukocytes
Specific Gravity
Reagent strips consist of chemical impregnated absorbent
pads attached to a plastic strip.
Chemical Examination of Urine
Reagent Strip Technique
Testing Methodology
Dip the reagent strip completely (but briefly) into a wellmixed specimen
Remove excess urine by running the edge of the strip on
the container, test tube or absorbent pad
Wait for the specified time for reactions to take place
Compare color reactions against manufacturers chart
using a good light source
TIPS!
Improper technique can result in error.
RBCs and WBCs sink to the bottom of the specimen
Do not allow the strip to remain too long with the
specimen as this may cause removal of reagents
Excess urine that remains on the strip may cause
chemical run over, hence, distortion of colors
Manufacturers timing should be followed for best results
A good light source is required
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
The strip must be placed very near the color chart but
not making contact with it
Specimens that have been refrigerated must be brought
to room temperature first before actual testing
(enzymatic reactions are temperature dependent)
MTs who are severely color blind should not perform
reagent strip testing
Color masking by drugs and other substances my
interfere with readings (perform chemical testing instead)
Although ascorbic acid has the potential to adversely
affect several reagent strip test results, most
manufacturers use an iodate overlay to prevent this.
Specimens must be tested within 2 hours of collection
Handling and Storage
Strips must be protected from moisture, volatile
chemicals, heat and light
Desiccants should not be removed from the bottle
Strips should be removed prior to testing only and bottle
should be tightly sealed immediately
Bottles should not be opened in the presence of volatile
fumes
Reagent strip bottles should be stored per manufacturer
instructions (usually RT)
All reagent strips used should not be beyond expiration
date
Care should be taken not to touch reagent pads when
removing the strips
Page
Reporting can be done by:
1. In concentration (mg/dL)
2. Descriptive (small, moderate, large)
3. Plus system
Negative
Trace
1+
2+
3+
4+
4. Positive or Negative
Chemical Examination of Urine
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Page
Tablet and Chemical Tests
Each tablet or chemical test must follow manufacturers
directions to ensure reproducible and reliable results
The laboratorian should know the following for each test
and compare it with reagent strip testing
Sensitivity
Specificity
Potential interferences
Chemical and tablet tests are generally performed
1. To confirm results already obtained by reagent strip
2. As an alternative method for highly pigmented urine
3. Because some are more sensitive for the substance
(e.g. Ictotest)
4. Specificity of the test differs from that of the reagent
strip (e.g. SSA, Hoesch)
Quality Control
Each bottle should be checked with a positive and negative
control
minimum once every 24 hours or when a new bottle is
opened
When there are questionable results
Concern about strip integrity
All quality control results should be documented
Distilled water should never be used as a negative control.
All negative controls should read negative.
All positive controls should agree one color block.
All QC results that do not agree should be documented and
resolved before proceeding with urine testing.
Chemical Examination of Urine
pH
Introduction:
The renal system, the pulmonary system, and blood buffers are
major regulators of acid-base content in the body. Through
secretion of Hydrogen in the form of:
1. Ammonium ions
2. Hydrogen phosphate
3. Weak organic acids
4. Reabsorption of bicarbonate
Normal pH of urine of a healthy individual:
First morning/average person: pH 5.0-6.0
after a meal more alkaline (alkaline tide)
Normal range: pH 4.5-8.0
Page
Urinary pH must be considered in conjunction with other patient
information such as:
1. Acid-base content of blood
2. Renal function
3. Infections
4. Dietary intake
5. Age of the specimen
Clinical Significance
An aid in determining the existence of systemic acidbase disorders
o Metabolic
o Respiratory
Management of urinary conditions
Aids in evaluation of kidney reabsorption or secretion
abilities
Calculi formation
Management of infections
Specimen viability
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Chemical Examination of Urine
NOTES:
pH of greater than 8.0 or less than 4.5 are physiologically
impossible, hence, investigation required
if greater than 8.0
highly alkaline medications
urease producing bacteria present
following improper preservation
No known substance is known to interfere with pH pads
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Page
Reagent strip reaction
PRINCIPLE: Double Indicator System
Most reagent strip pH pads measure urine pH in 0.5 or 1
unit increments from pH 5.0 to 9.0
A double indicator system is used to differentiate the pH
range
Methyl Red produces a color change from red
to yellow from pH 4 6
Bromthymol blue turns from yellow to blue in the
range pH 6 9
Color ranges from ORANGE at pH 5.0 through yellow and
green(ph 7.0) to a final deep blue at pH 9
Care must be taken to prevent run over from the protein
area as the latter is acidic and may give a false low pH
(false acidic) when testing alkaline urine
Chemical Examination of Urine
Protein
Introduction:
Of all chemical tests performed on urine, the most indicative of
renal disease is the protein determination. Presence of protein in
urine or proteinuria is almost always associated with early renal
disease.
Normal urine:
Less than 10mg/dL or 100 mg per 24 hours is excreted
Protein excreted is mostly made up of low molecular weight
serum proteins (filtered by the glomerulus and some proteins in
the genitourinary tract)
(Pre renal proteinuria)
Not an actual renal disease
Also called overflow proteinuria
Caused by conditions affecting plasma protein
Increased filtration and exceeds capacity of the renal
tubules to reabsorb resulting in an overflow
Usually transient
Caused by increased levels of:
Low molecular weight plasma proteins
Hemoglobin (after hemolytic episode)
Myoglobin (following muscle injury)
Acute phase reactants (inflammation and
infection)
*Usually not discovered in routine urinalysis since
the protein pad detects primarily albumin
Page
Major protein in urine: ALBUMIN
High concentration in plasma but low in urine because of the
filtration process (Most albumin cannot pass glomerulus and
those that pass are reabsorbed by the tubules)
Other proteins:
1. Serum and tubular microglobulins
2. Tamm-Horsfall protein by tubules
3. Prostatic protein
4. Seminal protein
5. Vaginal secretions
Clinical Significance
Demonstration of urine protein does not always signify
renal disease additional testing is required
Clinical proteinuria (>30mg/dL or 300mg/L)
o Pre renal
o Renal
o Post renal
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Bence Jones Protein
An example of pre renal proteinuria (due to
increased serum protein levels)
Found in patients with Multiple Myeloma (a
proliferative disorder of plasma cells)
Excretion of a unique type of protein called Bence
Jones Protein which are immunoglobulin light
chains
Low molecular weight protein which exceeds the
tubular reabsorption capacity and is excreted in
urine
When BJP is suspected, a screening test is
performed:
Principle:
BJP has a unique solubility characteristic.
BJP coagulates when heated to 40C-60C and
dissolves at 100C.
Positive result: Turbid urine at 40C-60C and clear at
100C
Not all patients with Multiple Myeloma excrete BJP
Diagnosis of Multiple Myeloma should be
confirmed through serum electrophoresis and
immunoelectrophoresis
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
(Renal Proteinuria)
Proteinuria associated with TRUE RENAL DISEASE
Classified as either:
1. Glomerular Proteinuria
Happens when the glomerular membrane is
damaged
Selective filtration is impaired
A large amount of serum protein, RBCs and WBCs
pass through and are excreted in urine
Conditions that damage the glomerulus
o Amyloid material
o Toxic substances
o Immune complexes found in Lupus
erythematosus and Streptococcal GN
Other conditions but are reversible:
o Increased blood pressure / Hypertension
o Strenous exercise
o Dehydration
o Pregnancy (Pre-eclamptic states)
2. Tubular Proteinuria
Happens when the tubules are no longer capable
of reabsorbing normally filtered albumin
Causes of tubular proteinuria:
o Toxic substances / Heavy metals
o Severe Viral infections
o Fanconi Syndrome
Protein levels found in urine are slightly above
normal to 4g/day
Markedly increased urinary protein is seldom seen
in tubular proteinuria
Page
Chemical Examination of Urine
Chemical Examination of Urine
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
(Post Renal Proteinuria)
Protein that is added to urine ultrafiltrate as it passes
through the lower urinary tract
Ureter
Bladder
Urethra
Prostate
Vagina
Examples of post renal urinary protein causes:
Bacterial infections
Fungal infections
Inflammation (exudates)
Menstruation
Prostatic fluid
Semen
Other Renal Proteinuria:
1. Orthostatic (Postural) Proteinuria
Persistent benign proteinuria
Functional proteinuria
Occurs frequently in young adults
Called ORTHOSTATIC or POSTURAL because urinary
protein increases following periods in vertical position.
Urinary protein returns to normal when horizontal
position is assumed
Caused by pressure on the renal vein
Testing procedure:
Patient is requested to empty bladder before going to
bed and collect a specimen immediately upon arising in
the morning
A second specimen is collected after remaining in
vertical position for several hours
Positive result:
1st specimen is negative for protein and 2nd specimen is positive
2. Microalbumin
A predictive indicator of renal complications
Useful test for diabetic patients
Diabetic nephropathy leads to reduced glomerular
filtration and ends in renal failure (Type I and II
diabetes)
Microalbuminuria is also associated with increased risk
of cardiovascular disease
Detection of microalbumin before needed a 24
hour urine sample
o Results were reported in mg of albumin / 24
hours or AER (Albumin excretion) in ug/min
Newer testing methods use Enzyme immunoassays or
Immunochromographics
o Sensitivity: 0-10 mg/dL for EIA
o Sensitivity: 1.2-8.0 mg/dL for
Immunochromographics
Microalbumin is considered significant if found in urine
at 30 to 300mg albumin secreted in 24 hours or AER is
20-200 ug/min.
Page
NOTE:
Discovery of protein from random samples is not always
pathologic. Several cases are benign.
Chemical Examination of Urine
Page
Reagent strip reactions
Principle: PROTEIN ERROR OF INDICATORS
Colorimetric
Changes color in the presence of a certain protein and
not due to pH (pH held constantly at pH 3.0)
Albumin accepts hydrogen ions from the indicator
The test is sensitive to albumin compared to other
proteins because it has more amino groups to accept
hydrogen ions given by the indicator
Reagents:
o Tetrabromphenol blue or
3,3,5,5 tetrachlorophenol -3,4,5,6tetrabromosulfonphthalein
o Acid buffer (to maintain at an acidic pH)
At pH 3.0, indicators are yellow
As protein concentration increases, the color progresses
through shades of green and finally blue
Reported as
o NEGATIVE
o TRACE (usually less than 30mg/dL)
o 1+, 2+, 3+, and 4+
Semiquantitative reporting:
o 30 mg/dL
o 100 mg/dL
o 300 mg/dL
o 2000mg/dL
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Chemical Examination of Urine
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
10
NOTE: Chemical confirmation of protein results:
o A very high protein result
o Urine is very alkaline
o
2 tests that test for protein other than reagent strip:
1. Sulfosalicylic Acid Precipitation Test
Cold precipitation test
Reacts with all types of protein
Methods vary amongst laboratories
Specimen should be supernatant of urine to remove
any extraneous proteins
Examples of protein that are precipitated but are not
clinically important: (False turbidity)
o Radiographic dyes (high specific gravity)
o Tolbutamide metabolites (Px history)
o Cephalosporins (Px history)
o Penicillins
o Sulfonamides
Highly alkaline urine may overcome acidity of SSA
less turbidity than it should or False negative results
o Use more concentrated SSA
SSA is sensitive to 5mg/dL to 10mg/dL protein
regardless of the type of protein present
When SSA is crystalline, radiographic contrast media
could be present and reagent strip results should be
reported
SSA should never be used to confirm protein results
from reagent strip testing because it lacks protein
specificity
2. Heat and Acetic method
a. Place 5-10mL of urine in a clean test tube
b. Boil upper 1/3 of the tube (1-2 minutes)
c. Add 1-2 drops of glacial acetic acid (5%)
I.
Initial turbidity after flaming is due to
phosphates and carbonates glacial acetic
will clear it up
d. Reboil the specimen
e. Grade the turbidity
Page
Reaction Interference/Limitation
Highly buffered alkaline urine (Major interference)
o Overrides acidic environment of protein pad
o Produces a color change unrelated to protein
concentration
Prolonged contact with urine specimen
o May remove acid buffer
o False positive results when acid buffer is removed
Highly pigmented urine (False positive)
Contamination of quaternary ammonium compounds
(False positive)
Detergents (False positive)
Antiseptics (False positive)
A very high specific gravity (False positive)
Protein other than albumin (False negative)
Page
11
Chemical Examination of Urine
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Chemical Examination of Urine
Introduction:
The glucose test is the most frequent chemical analysis
performed on urine. Its value in the detection and monitoring of
Diabetes mellitus is unchallenged.
More than half of the cases in the world are undiagnosed.
Early diagnosis is the key to improved prognosis.
Gestational diabetes
Hyperglycemia that occurs during pregnancy
Disappears after delivery
Onset is during the 6th month of pregnancy
Due to action of hormones secreted by the
placenta which blocks insulin resulting in
resistance of insulin and hyperglycemia
Detection is important as glucose crosses the
placenta and insulin does not
Glucose will be absorbed by the babys pancreas
will produce a lot of insulin converting all glucose
into fat and stored.
Baby will be at risk for obesity and type 2 diabetes
Women who have gestational diabetes are also
prone to developing type 2 diabetes
Page
Clinical Significance
The kidneys PROXIMAL CONVOLUTED TUBULE (PCT)
reabsorbs glucose almost completely
Reabsorption rate is at 160-180mg/dL (renal threshold)
Should glucose in the blood be too high, renal tubular
reabsorption will be difficult and glucose will appear in
urine
Used for diabetes screening fasting prior to the
collection of samples is recommended
Blood glucose levels fluctuate especially after
meals
2 hours after a meal is recommended
First morning specimens are not recommended
because they do not represent an actual
representation of the bodys ability to clear
glucose (evening meal glucose still in bladder)
Urine glucose should be correlated with FBS
OGTT is used to confirm diabetes
12
Glucose
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Chemical Examination of Urine
Reagent strip reactions
PRINCIPLE: DOUBLE SEQUENTIAL ENZYME REACTION
2 different tests used by laboratories
Glucose oxidase
Specific for glucose
Used in reagent strips/impregnated in
reagent strips
Copper reduction
Detects glucose and other reducing
substances
Reagent strip for glucose employ glucose oxidase by
impregnating the test area with a mixture of (refer below)
to produce a double sequential enzyme reaction
1. Glucose oxidase
2. Peroxidase
3. Chromogen
4. Buffer
st
1 step: Glucose oxidase rapidly catalyzes the reaction of
glucose to produce gluconic acid and hydrogen peroxide.
2nd step: Peroxidase catalyzes the reaction between the
hydrogen peroxide formed and chromogen to form an oxidized
colored compound that represents the presence of glucose.
Page
13
Examples of hyperglycemia of non diabetic origin which
also produces glycosuria
Pancreatitis
Pancreatic cancer
Acromegaly
Cushings syndrome
Hyperthyroidism
Pheochromocytoma
Drugs
Liver diseases
CNS damage
Hormonal disorders
Hormones associated with the disorders of
hyperglycemia of non diabetic in origin
Glucagon (increased)
Epinephrine (increased)
Cortisol (increased)
Thyroxine (increased)
GH (increased)
*all of the hormones mentioned oppose insulin function
*Glycogen (fat) is converted into glucose
Glycosuria in the absence of hyperglycemia (Renal
Glycosuria)
Caused by failure of tubules to reabsorb glucose
Seen in:
1. ESRD
2. Cystinosis
3. Fanconi Syndrome
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Chemical Examination of Urine
Reaction Interference
Glucose oxidase is specific for glucose only
o other sugars are not detected
Peroxide and strong oxidizing detergents give False
positive reactions
Strong reducing agents give False negative reactions;
(oxidation will not proceed)
Example:
o Ascorbic acid
Ascorbic acid interference can be minimized by
incorporating iodate into glucose pads; iodate oxidizes
ascorbic acid
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
High specific gravity and low temperature decrease test
sensitivity
Unpreserved specimens give false negative results
o Rapid glycolysis of glucose
Other tests for urine glucose:
1. Copper Reduction Test
One of the earliest chemical test performed on urine
Test relies on the ability of glucose and other
substances to reduce copper sulfate to cuprous
oxide in the presence of alkali and heat
Reducing sugars include:
a. Glucose
b. Fructose
c. Galactose
d. Maltose
e. Pentose
Color change progressing from a negative blue
(CuSO4) through green, yellow, and orange/red
(Cu2O) occurs when the reaction takes place
The best example of Copper reduction is the
Benedicts Test
14
Reagent strip manufacturers use several different
chromogens
Potassium iodide(green to brown)
Tetramethylbenzidine (yellow to green)
Urine glucose is reported in terms of:
NEGATIVE
Trace
1+
2+
3+
4+
Color charts also provide semi-quantitative
measurements
Ranges from 100mg/dL to 2g/dL
The American Diabetes Association recommends
quantitative reporting
Page
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
IMPORTANT NOTE:
Care must be taken to observe the reaction closely
as it is taking place
High glucose OR reducing substances could cause a
PASS THROUGH phenomenon
PASS THROUGH PHENOMENON happens when the color
produced passes through the orange/red stage and returns to
a green-brown color, and if not observed, a high glucose level
may be reported as NEGATIVE
An alternate method uses 2 drops instead of 5 drops
of urine can minimize the occurrence of pass
through
A separate color chart must be used for this
alternate method
The chart provides up to 5g/dL
semiquantitation whereas the regular (5 drops
urine) provides only up to 2g/dL
Sensitivity of Clinitest is 200 mg/dL
Clinitest is still a nonspecific test for reducing
substances and subject to interference from several
other reducing sugars:
1. Galactose
2. Lactose
3. Fructose
4. Maltose
5. Pentoses
6. Ascorbic acid
7. Drug metabolites
8. Antibiotics (Cephalosporins)
Clinitest is not a confirmatory test for urine glucose
Page
The Benedict solution was developed in 1908 and
contains:
o Copper sulfate
o Sodium carbonate
o Sodium citrate buffer
Procedure:
Urine + Benedict Solution + Heat = Precipitate
2. Clinitest
A tablet version of the Benedicts Test
Makes use of the ability of the reducing sugars ability
to convert cupric sulfate to cuprous oxide
The test is based on the ability of reducing substances
to convert cupric sulfate to cuprous oxide
Makes use of a tablet and contains
o Anhydrous copper sulfate
o Sodium carbonate
o Sodium citrate / citric acid
o Sodium hydroxide
Upon addition of the tablet to water and urine, heat is
produced by the hydrolysis of sodium hydroxide and
its reaction with sodium citrate Carbon dioxide is
released from the sodium carbonate to prevent room
air interfering with the reduction reaction
Tubes should be placed on a rack and should not be
held by hand because the heat reaction could
cause a burn
After the effervescence reaction, the tube is gently
shaken and the color ranging from blue to
orange/red can be compared with the
manufacturers color chart
15
Chemical Examination of Urine
Chemical Examination of Urine
Page
16
Clinitest tablets are hygroscopic and should be stored
in tightly packed packages
A strong blue color suggests deterioration of
the tablet due to moisture and should not be
used
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Introduction: The term ketones and ketone bodies represent
three intermediate products of fatty acid metabolism.
1. Acetoacetic acid (1st Ketone formed)
2. Acetone
3. Beta-hydroxybutyric acid
Normally, measurable amounts are not detected in urine
because all the metabolized fat are converted into CO2 and
H2O. However, when the use of available CHO as the major
source becomes compromised, body stores of fat must be
metabolized to supply energy. Ketones are then detected in
urine.
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Clinical Significance
When CHO are available, ketone synthesis is inhibited
and blood ketone levels are below 3mg/dL
Any condition that causes increased fat metabolism
leads to ketonuria and ketonemia. Clinical reasons for
increased fat metabolism:
Inability to metabolize CHO (as in DM)
Increased loss of CHO from vomiting
Inadequate intake of CHO associated with
Starvation
Malabsorption
Testing for urinary ketones is most valuable in the
management and monitoring of insulin dependent
(type 1) DM because of the inability to use CHO
If patient has ketonuria, it shows a deficiency in
insulin and the need to regulate dosage
Ketonuria is an often an early indicator of
insufficient dosage in type 1 Diabetes
Increased amounts of ketone in the blood leads to
Electrolyte imbalance large amount of H20 lost
Dehydration large amount of H20 lost
Acidosis due to ketoacids
Diabetic coma
All kinds of reagent multi-strips have ketone pads
incorporated because it provides valuable information
when correlated with glucose
Ketone renal threshold is 70mg/dL.
When blood ketone is more than 70mg/dL,
ketonuria happens.
Page
Ketones
17
Chemical Examination of Urine
Chemical Examination of Urine
Reagent strip reactions
The 3 ketone compounds present are not in equal amounts in
urine and blood. The average distribution is as follows:
1. Acetoacetic (20%)
a. Acetone (2%)
b. beta-hydroxybutyric acid (78%)
PRINCIPLE: SODIUM NITROPRUSSIDE (NITROFERRICYANIDE)
REACTION
Acetoacetic acid (in an alkaline medium) reacts with
sodium nitroprusside to produce a purple color.
The test does not measure beta-hydroxybutryric and is
only slightly sensitive to acetone (only when glycine is
present)
Not necessary to perform individual testing for
acetone and beta-hydroxybutyric acid
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Results are reported qualitatively or semi quantitatively
as:
NEGATIVE
Trace (5mg/dL)
Small (1+) (15mg/dL)
Moderate (2+) (40mg/dL)
Large (3+) (80-160mg/dL)
Reaction:
Chemical Tests for Ketone bodies:
1. Legals Test or Rotheras Test
Developed by Legal in 1883 and modified by Rothera in
1908
A nitroprusside reaction test
15 20 times more sensitive to acetoacetate than
acetone
Does not react to beta hydroxybutyric acid
No longer performed in clinical laboratories
More sensitive to acetoacetate and acetone than
reagent strip ketone pads
18
Patients with ketonuria have fruity or acetonic breath
odors because acetone is also eliminated by the lungs
Page
Chemical Examination of Urine
Reaction interference
Patients who undergo special diagnostic procedures (i.e.
CT scan guided with contrast) using dyes may produce
an interfering red color in the alkaline medium
Phenolsulfonphthalein
Bromsulphalein
Highly pigmented urine interfere with color reactions
Medications
Levodopa (large amounts)
Sulfhydryl group drugs (atypical color reactions)
Mercaptoethane sulfonate sodium
(MESNA)
Captopril
Improperly timed readings
Improperly preserved specimens
Volatilization of acetone (False decrease or
negative)
Breakdown of acetoactic acid by bacteria (False
decrease or negative)
Deterioration of nitroprusside reagent (both pad and
tablets)
Due to heat, moisture, or light
Page
19
Acetest tablets
A type of chemical test for ketones performed when
there is severe ketosis and serial dilutions are done to
provide a more accurate amount on ketones
Performed using a tablet which consists of:
o Sodium nitroprusside
o Glycine (for acetone and color enhancement)
o Disodium phosphate
o Lactose (provides better color differentiation)
Specimen that can be used with Acetest
o Serum
o Urine
o Other body fluids (ex. CSF, pleural, ascitic fluid,
etc)
Acetest tablets are hygroscopic
If the specimen is not absorbed in 30 seconds, a new
tablet should be used
Sensitivity of the test is 5mg/dL acetoacetate (lower limit)
Any pink, tan, or yellow color is ignored
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Page
20
Chemical Examination of Urine
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Chemical Examination of Urine
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
2. Hemoglobinuria
Hemoglobinuria is the result of either
a. Lysis of red blood cells in the urinary tract
(particularly in dilute alkaline urine)
b. Intravascular hemolysis
c. Subsequent filtering of hemoglobin through the
glomerulus
Lysis of red blood cells usually present hematuria and
hemoglobinuria
Intravascular hemolysis does not show red cells in
urine
21
Introduction:
Blood can enter the urinary tract anywhere from the glomeruli
to the urethra or can be a contaminant.
Blood found in urine may be in the form of:
1. Intact (hematuria) red blood cells
2. Free (hemoglobinuria) products of red blood cells
Blood present in large quantities can be detected visually.
Hematuria produces a cloudy red specimen.
Because any amount of blood greater than 5 cells/L urine is
considered clinically significant, visual examination cannot be
relied upon to detect the presence of blood.
Chemical tests for hemoglobin provide the most accurate
means for determining presence of blood in urine because
microscopic analysis may appear negative because some
patients possibly have hemolytic disorders and/or lysis of red
blood cells in which free hemoglobin is produced.
Clinical Significance
The finding of a positive reagent strip test result for blood
indicates
Presence of red blood cells
Hemoglobin
Myoglobin
Each of which has its own clinical significance
1. Hematuria
Closely related to disorders of renal or genitourinary
origin
Bleeding which is the result of TRAUMA or damage to
the organs of these systems
Major causes of hematuria
a. Renal calculi
b. Glomerular diseases
c. Tumors
d. Trauma
e. Pyelonephritis
f. Exposure to toxic chemicals
g. Anticoagulant therapy
Urinalysis is frequently requested when patients
present with certain signs and symptoms like:
a. Severe back pain
b. Severe abdominal pain
Hematuria of nonpathologic significance is observed
following
a. Strenuous exercise
b. menstruation
Page
Blood
Chemical Examination of Urine
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
22
Patients taking cholesterol lowering statin
medications also present with rhabdomyolysis as a
side effect
Heme portions of both Hemoglobin and Myoglobin
are toxic to the renal tubules; therefore, high
concentrations will lead to acute renal failure.
Page
Under normal conditions, haptoglobin captures
hemoglobin and forms complexes but when the
amount of free hemoglobin exceeds haptoglobin
levels, hemoglobin appears in urine. As occurs in:
a. Hemolytic anemias
b. Transfusion reactions
c. Severe burns
d. Brown recluse spider bites
e. Infections
f. Strenuous exercise
When large yellow brown granulated renal tubular
epithelial cells or urine sediments are found in urine,
these are usually due to reabsorption of filtered
hemoglobin and are called FERRITIN and
HEMOSIDERIN
3. Myoglobinuria
Myoglobin is a heme-containing protein found in
muscle tissue
Reacts positively with the reagent strip
Also gives urine a red-brown color
Presence of myoglobin is suspected in patients with
rhabdomyolysis (muscle destruction)
a. Trauma
b. Crush syndromes
c. Prolonged coma
d. Convulsions
e. Muscle wasting diseases
f. Alcoholism
g. Heroin abuse
h. Extensive exertion
Chemical Examination of Urine
Page
23
Hemoglobin vs Myoglobin
The laboratory is uncommonly requested to differentiate
between the presence of hemoglobin and myoglobin in
a urine specimen
Myoglobin is more toxic to the renal tubules than
hemoglobin
Reasons for differentiation:
Diagnosis
Predicting risk for renal failure
Treatment options
Diagnosis of myoglobinuria is usually based on:
Patient history
Elevated CK (Creatinine kinase)
Elevated LDH (Lactic dehydrogenase)
The appearance of patients plasma can also aid in the
differentiation (but of limited value)
Myoglobin clear plasma (myoglobin is rapidly
cleared by kidneys)
Hemoglobin red plasma (haptoglobinhemoglobin complex imparts a red color)
Myoglobin in the urine must be at least 25 mg/dL before
red pigmentation can be visualized
At concentrations 25 mg/dL or more, a precipitation test
called Blondheim Test may be performed to screen for
myoglobin.
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Chemical Examination of Urine
Positive for Myoglobin: Supernatant tests positive on reagent
strip and retains a red color
Positive for Hemoglobin: Red precipitate and supernatant tests
negative on blood reagent strip
Principle of Blondheim Test:
Based on the fact that the larger hemoglobin molecules are
precipitated by the ammonium sulfate and myoglobin remains
in the supernatant.
*Clinically no longer useful because of latest testing procedures
NOTE:
Myoglobin is not stable in very acidic urine and, if denatured,
may precipitate with ammonium sulfate.
In cases where specimen processing is delayed, neutralization
and freezing it would be proper.
Immunoassay procedures are available to measure serum
myoglobin levels.
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Blood testing areas are incorporated with
Peroxide
Tetramethylbenzidine
Buffer
Color charts for differentiation are provided
Hematuria
Hemoglobinuria/ Myoglobinuria
Free myoglobin/hemoglobin give a uniform color ranging
from a negative yellow to green to a strongly positive
green blue appear on the pad
Intact RBCs are lysed when they come in contact with
the pad and liberating hemoglobin showing an isolated
reaction which is a speckled/dotted/mottled pattern
Reagent strips can detect concentrations as low as 5
cells/L
Must be correlated with microscopic analysis
Reporting of results:
NEGATIVE
Trace
Small / 1+
Moderate / 2+
Large / 3+
24
Reagent strip reactions
PRINCIPLE: PSEUDOPEROXIDASE ACTIVITY OF HEMOGLOBIN
Hemoglobin peroxidase catalyzing a reaction between H2O2
and the chromogen TETRAMETHYLBENZIDINE to produce an
oxidized chromogen, which is blue-green (from yellow)
Page
Blondheim Test procedure:
- Add 2.8g of 80% ammonium sulfate to 5mL urine (freshly
voided)
o Hemoglobin is precipitated out of the solution
o Myoglobin stays dissolved in supernatant
- Mix
- Allow the specimen to sit for 5mins.
- Centrifuge specimen mixture
- Test the supernatant using the blood reagent pad
Chemical Examination of Urine
Page
25
Reaction Interference
False positive reactions may be seen in:
Menstruating women
Strong oxidizing reagents in specimen containers
Vegetable peroxidase
Bacterial enzymes (E. coli peroxidase)
False negative reactions
High ascorbic acid (25 mg/dL)
Directly reacts with H2O2 and removes it
Can be minimized when an iodate mesh or an
iodate scavenger pad is used
High specific gravity
Red cells crenate and do not lyse when
they come in contact with the pad
Decreased reactivity of pad
Formalin used as preservative
Patient taking Captopril
High concentrations of nitrite (greater than
10mg/dL)
Failure to mix specimen properly
Red cells settle to the bottom of the
specimen ensure proper mixing
If hemoglobin is present, supernatant urine
and uncentrifuged specimens will still react
with the test pad
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Chemical Examination of Urine
Production of Bilirubin
- Under normal conditions, RBC life span is 120 days
- After 120 days, RBCs are sequestered in the spleen and
liver by phagocytic cells of the RES(reticuloendothelial)
- Liberated hemoglobin is broken down into its component
parts;
1. Iron (body reuses)
2. Protein (body reuses)
3. Protoporphyrin (converted to bilirubin by RES)
- Bilirubin (water - insoluble) is released into blood
circulation
- Bilirubin binds with ALBUMIN and transported to the LIVER
- Bilirubin then undergoes conjugation with GLUCURONIC
ACID by the action of GLUCURONYL TRANSFERASE to
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Hemoglobin degradation
NOTE: Kidneys cannot clear bilirubin bound to albumin (large
and water insoluble)
26
Introduction:
Bilirubin is an intensely orange yellow pigment that when
present in significant amount causes a characteristic coloration
of plasma and urine.
The principal source of bilirubin (85%) is hemoglobin released
from the breakdown of senescent red blood cells in the RES.
Other sources come from RBC precursors from bone marrow
and other heme containing proteins such as myoglobin and
cytochromes.
Presence of bilirubin in urine can provide an early indication of
liver disease. It is often detected long before the development
of jaundice.
form water soluble bilirubin diglucuronide (conjugated
bilirubin)
Conjugated bilirubin directly passes through the bile
ducts and into the intestine
In the intestine, intestinal bacteria reduce bilirubin to
urobilinogens
Urobilinogens are oxidized and excreted in the feces in
the form of UROBILIN
Page
Bilirubin
Chemical Examination of Urine
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
27
No urobilinogen enters the intestine
negative urine urobilinogen
Stool is acholic (pale white or tan)
bilirubinuria and bilirubinemia is detected long before
Jaundice (blood bilirubin levels 2-3mg/dL) is seen
Differentation of jaundice cases
Results be correlated with urobilinogen
Page
Clinical Significance
Disturbances in any aspect of bilirubin formation, hepatic
uptake, metabolism, storage or excretion can cause
bilirubin to appear in urine (bilirubinuria)
Healthy individual bilirubin in urine (0.02 mg/dL)
Increased bilirubin in urine indicates distruption or
an increase in hemoglobin catabolism
Three principal mechanisms of altered bilirubin
metabolism occur
Prehepatic
Due to an increase breakdown of RBCs or
overproduction of heme to bilirubin
Unconjugated bilirubin cannot pass
through kidney glomerulus
Liver function is normal
Urine bilirubin is negative; Urine Urobilinogen
high due to reabsorption from intestine
Hepatic
Due to hepatocellular disorders or disease
Conjugated bilirubin leaks and readily
passes glomerulus positive urine bilirubin
Urine urobilinogen depends on extent of
liver damage normal or increased
Post hepatic obstruction
Blockage of bile duct or biliary system
Liver function is normal
Overflow of conjugated bilirubin and
reverts backs into blood circulation and
cleared by kidneys positive bilirubin
Chemical Examination of Urine
Chemical tests for bilirubin
Ictotest tablets are used for questionable results
Ictotest consist testing mats and tablets containing
1. P-nitrobenzene-diazonium-p-toluenesulfonate
2. SSA
3. Sodium carbonate
4. Boric acid
Less subject to interference
Sensitive to 0.05 mg/dL or 0.10 mg/dL of bilirubinuria
sometimes requested to detect early stages of
liver disease
Reagent strip has a lower sensitivity of 0.40 mg/dL
The mat has special absorbent properties which allow
bilirubin to stick to the surface as urine is absorbed
Page
28
Reagent Strip Reactions
Routine testing for bilirubin using reagent strip uses the
diazo reaction or azo coupling reactions
Bilirubin combines with a diazonium salt
2,4-dichloroaniline diazonium salt
OR
2,6-dichlorobenzene-diazonium-tetrafluoroborate
Uses an acid medium to produce an azo dye
Color ranges from light tan to beige or pink to violet
Qualitative test results are reported as
NEGATIVE
1+ / Small
2+ / Moderate
3+ / Large
Most difficult to read amongst others
Pigments of other substances
Color overlapping
Lower limit of detection is 0.5 mg/dL of conjugated
bilirubin
A 25 fold increase of urine bilirubin must be
present in order for the test to be positive
Reaction:
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Chemical Examination of Urine
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
29
Free unconjugated bilirubin is less reactive
on reagent strips
High concentrations of ascorbic acid (greater
than 25 mg/dL) and nitrite medications
Combines with diazonium salt and prevents
reaction with bilirubin
Page
If interfering substances are suspected, adding water
directly to the mat after urine has been added fixes the
problem.
POSITIVE REACTION: A blue to purple color appears on the mat
when bilirubin is present
NEGATIVE REACTION: Any other color
*Interferences of Ictotest are same with reagent pad for bilirubin
since they share the same principle
Other Bilirubin Methods
1. Shake test
a. Performed when urine is beer brown or dark
yellow brown in color
b. Characteristic YELLOW foam appears when urine
is agitated or shaken
Reaction Interference
False positive
Other urine pigments such as from
phenazopyridine compounds thick pigment
chlorpromazine metabolites can react to
diazonium salts
Indican
Metabolites of Lodine (medication)
False negative
Improperly preserved specimens (most frequent)
Photo-oxidized specimens
When specimens are exposed to light and
bilirubin is converted to biliverdin (does not
react with diazo tests)
Hydrolysis of bilirubin diglucuronide (conjugated
bilirubin)
Chemical Examination of Urine
Urobilinogen
Introduction:
Urobilinogen is one of the products of bacterial reduction of
conjugated bilirubin. The other is Stercobilinogen, which cannot
be reabsorbed and further reduced to UROBILIN, which is
responsible for the characteristic color of stool.
Some of the urobilinogen is reabsorbed from the intestine into
the blood, recirculates to the liver, and is excreted back into the
intestine through the bile duct.
Urobilinogen appears in the urine because as it circulates in
blood en route to the liver, it passes through the kidneys and is
filtered by the glomerulus. Therefore, a small amount of
urobilinogen less than 1mg/dL or Ehrlich unit is normally
found in the urine.
Page
30
Clinical Significance
Measurement of urine urobilinogen can be valuable in
the detection of early liver disease
1% of nonhospitalized patients and 9% of
hospitalized patients exhibit high results owing to
constipation
Increased urine urobilinogen (greater than 1 mg/dL) is
seen in:
Liver disease
Liver impairment decreases the ability of
the liver to process urobilinogen
recirculated from the intestines
Excess urobilinogen shows up in urine
Hemolytic disorders
Jaundice due to excess unconjugated
bilirubin and leads to high conjugated
bilirubin entering the intestines
Cycle goes on in which urobilinogen is
reabsorbed
Liver is overworked and by time is unable to
process urobilinogen at a normal rate
More urobilinogen will circulate and be
presented to the kidneys for excretion
Absence of urobilinogen in urine and feces is clinically
significant
Cannot be detected using reagent strip
Represents bile duct obstruction
Absence of urobilin also indicates bile duct
obstruction
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Chemical Examination of Urine
REAGENT STRIPS CANNOT DETERMINE THE ABSENCE OF
UROBILINOGEN
Important indicator of biliary obstruction
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
31
Azo coupling (diazo) reaction
Urobilinogen reacts with 4methoxybenzene-diazoniumtetrafluoroborate
Colors produced range from white to pink
More specific for urobilinogen compared to
Ehrlich
Results are in mg/dL
Reaction Interference
Ehrlich reaction is subject to a variety of interferences
called Ehrlich reactive compounds
False positive reactions due to:
1. Porphobilinogen (clinically significant)
2. Indicant
3. P-aminosalicylic acid
4. Sulfonamides
5. Methyldopa
6. Procaine
7. Chlorpromazine compounds
*Reagent strip cannot differentiate or screen for
presence of PBG
Sensitivity increases with temperature (RT)
Highly pigmented urine cause atypical readings for both
methods
Urobilinogen is high after meals because of bile
salt excretion
False negative readings for both methods
Occur in improperly preserved specimens
Urobilinogen is photo-oxidized to Urobilin
Formalin used as preservative
High concentrations of nitrite interfere with azo
coupling reactions
Page
Reagent Strip Reactions and Interference
2 different urobilinogen reactions exist and are used by
different manufacturers
Ehrlichs aldehyde reaction
Urobilinogen reacts with pdimethylaminobenzaldehyde (Ehrlichs
reagent)
Colors produced are from light to dark pink
Results are reported as Ehrlich units (EU)
which are equal to mg/dL
Normal value: 0.2-1.0 EU
Chemical Examination of Urine
Page
2. Hoesch Screening Test for PBG
Rapid screening for urinary PBG
2 drops of urine added to 2mL Hoesch reagent (Ehrlichs
reagent dissolved in 6M HCl)
6M HCl inhibits urobilinogen
POSITIVE TEST: Top solution shows red color
The test detects approximately 2mg/dL of PBG
False positive tests
Methyldopa (high concentrations)
Indican (high concentrations)
Highly pigmented urine
3. Watson Schwartz Differentiation Test
The classic test for differentiating PBG, urobilinogen and
Ehrlich reactive compounds
Procedure:
Tube 1
Tube 2
2mL urine
2mL urine
2mL chloroform
2mL butanol
4mL sodium acetate
4mL sodium acetate
Tube 1
Chloroform will extract UROBILINOGEN producing a
colorless URINE TOP layer and a red CHLOROFORM
BOTTOM
PBG nor other ERC are soluble in chloroform
Tube 2
Butanol will extract both UROBILINOGEN and ERCs
producing a red BUTANOL TOP layer and a colorless
bottom urine layer if PBG is present
PBG is not soluble in butanol
Before reporting the test as positive for both substances, an
additional chloroform extraction should be performed on
the red urine (upper) layer in Tube 1
To make sure its not due to an excess of urobilinogen
32
Chemical Tests for Urobilinogen and other Ehrlich reactive
substances
Introduction:
Urobilinogen or other Ehrlich reactive tests were not done
before because they were time consuming and nonspecific.
When necessary, the following 3 were performed.
1. Ehrlich Tube Test
Normally, addition of Ehrlich reagent to urine produces a
cherry red color and adding sodium acetate enhances
color reaction (when urobilinogen is present)
Using the Ehrlich Tube method, one part Ehrlich reagent is
added to 10 parts urine. Tube is mixed and examined for red
color.
This test is subject to false positive results when
porphobilinogen and Ehrlich reactive compounds were
present.
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Page
33
Chemical Examination of Urine
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Chemical Examination of Urine
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
The nitrite test is a valuable test for detecting initial
bladder infection (cystitis) because most patients are
asymptomatic and that would not lead the physician to
order a urine culture.
PYELONEPHRITIS, a complication of cystitis, is the inflammatory
process of the kidney and adjacent renal pelvis.
Pyelonephritis can lead to:
1. Renal tissue damage
2. Impairment of renal function
3. Hypertension
4. Septicemia
The nitrite test can also be used to evaluate:
1. Success of antibiotic therapy
2. Screen people who have recurring infections
3. Diabetic patients
4. Pregnant women (high risk for UTI)
Many laboratories use the nitrite test in conjunction with the
leukocyte esterase test to determine necessity of performing a
urine culture.
34
Introduction and Clinical Significance:
The reagent pad for nitrite provides a rapid screening
test for the presence of urinary tract infections (UTI)
UTI can involve the bladder (cystitis), the renal pelvis and
tubules (pyelonephritis), or both
2 possible routes for UTI:
1. Movement of bacteria up the urethra into the bladder
(ascending infection)
2. Movement of bacteria from the bloodstream into the
kidneys and urinary tract
Most common infecting microorganisms
1. Escherichia coli
2. Proteus species
3. Enterobacter species
4. Klebsiella species
UTI is 8 times more common in females than in males
UTI can begin as the result of urinary obstruction
1. Tumor
2. Bladder dysfunction
3. Urine stasis
The test is designed to detect cases in which the need for
a culture may not be apparent but not to replace it as
the primary test for diagnosing and monitoring bacterial
infections.
Most UTI cases start in the bladder as a result of external
contamination and move upward to the tubules, renal
pelvis and kidney. (ascending infection)
Page
NITRITE
Chemical Examination of Urine
To prevent false positive reactions by externally
contaminated specimens
Test sensitivity is standardized to 100,000
organisms/mL
The test does not measure degree of bacteriuria
Any shade of pink is considered to represent a clinically
significant amount of bacteria
Positive Test: Pink reagent pad
Negative Test: White reagent pad
Page
Reaction Interference
Several major factors influence reliability of nitrite test
Tests with negative results in the presence of vaguely
suspicious clinical symptoms should always be thoroughly
investigated
The following are major considerations when interpreting
the nitrite test.
1. Bacteria that lack the enzyme reductase
a. Cannot reduce nitrate to nitrite
b. Enzyme found in some gram negative bacteria
(Enterobacteriaceae)
c. Most bacteria that cause UTI are gram negative
d. Gram positive and yeast also cause infection but
do not reduce nitrate to nitrite
2. Bacteria must remain long enough in urine
a. Nitrite test should be performed on first morning
urine
b. Urine that remained in the bladder for at least 4
hours is another alternative for first morning urine
3. Enough nitrate diet
a. Green vegetables are a good source of nitrate
b. This is seldom a problem
c. False negative if nitrate is not enough
4. Further reduction
a. Nitrate to nitrite to nitrogen
b. Occurs when large amounts of bacteria present
35
Reagent Strip Reactions
PRINCIPLE: GREISS REACTION
Chemical basis of the nitrite test is the ability of certain
bacteria to reduce nitrate (from diet) into nitrite (not
normally found in urine)
Bacteria must produce nitrate reductase to convert
nitrate
Nitrite is detected using Greiss reaction
Nitrite, at an acidic pH, reacts with an aromatic
amine (para-arsanilic acid or sulfanilamide) to
form a diazonium compound that then reacts with
tetrahydrobenzoquinolin compounds (azo
coupling reaction )to produce a pink colored
azo dye
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Chemical Examination of Urine
Page
36
5. Miscellaneous
a. When patient is already under antibiotic therapy
i. Antibiotics inhibit bacteria action of
reduction
b. Large quantities of ascorbic acid
i. Interferes with diazo reaction
c. High specific gravity decreases test sensitivity
d. All give false negative results
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Chemical Examination of Urine
Introduction:
Prior to the development of LE, urinary leukocytes were
detected only by microscopy using urine sediments.
Microscopy can be subject to variation depending on the
method used to prepare the sediment and the technical
personnel examining the sediment.
Chemical testing for leukocytes in urine standardized the means
for detection.
The test is not designed to measure the concentration of
leukocytes quantitation should be done by microscopy
An advantage in using LE is that it detects the presence of
leukocytes that have been lysed, particularly in dilute,
hypotonic, alkaline urine, in which would not appear in
microscopy.
Clinical Significance
Normal value: 0 2 /hpf up to 0 5 / hpf or 0-8/hpf
Women tend to have higher numbers than men as a
result of vaginal contamination
Increased urinary leukocyte is an indicator of UTI
The test detects the presence of ESTERASE in azurophilic
granules of granulocytic white blood cells (in cytoplasm)
Neutrophils
Eosinophils
Basophils
Monocytes and macrophages have granules as well,
although they are not entirely granulocytic
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Lymphocytes are not detected using LE because they
are agranular
Esterases are also present in Trichomonas
RBCs, bacteria, and renal tissue cells do not contain
esterases
A positive LE test result is most frequently accompanied
by the presence of bacteria
Bacteria may or may not produce a positive nitrite
reaction
Infections caused by the following cause leukocyturia
without bacteriuria
Trichomonas
Chlamydia
Yeast infection (Moniliasis)
Inflammation of renal tissue (interstitial nephritis)
Screening urine specimens using LE and nitrite determine
the necessity of performing urine cultures
This can be a cost effective measure
LE test has more reliability in the practice of medical
diagnosis than nitrite
37
Page
Leukocyte Esterase (LE)
Chemical Examination of Urine
Page
LE reaction requires the longest time of all the reagent
strip reactions
2 minutes or 120 seconds
Reactions are reported as
NEGATIVE
TRACE
SMALL / 1+
MODERATE / 2+
LARGE / 3+
Trace results may not be significant
Repeat test with a fresh specimen
Advantages of the LE screening test
Detect the presence of intact and lysed WBCs
Serve as a screening for WBC that is independent
of procedural variations for sediment preparation
The LE Test detects 10 to 25 WBCs/L
Reaction Interference
False positive reactions
Formalin in the collection container
Strong oxidizing reagents
Phenazophyridine
Beets
Atypical color reactions
Highly pigmented urine
Nitrofurantoin
False negative reactions
High concentration of protein (greater than 500
mg/dL)
High glucose (greater than 3g/dL)
Oxalic acid
Ascorbic acid (combines with diazonium salt)
High specific gravity
Leukocytes crenate and prevent esterase
release
Strong oxidizing agents
Interfere with reaction pH
Antibiotics (decreased sensitivity)
Gentamicin
Cephalosporins
Cephalexin
Cephalothin
Tetracycline
38
Reagent strip reaction
PRINCIPLE: LEUKOCYTE ESTERASE
The action of LE to catalyze the hydrolysis of an acid
ester embedded on the reagent pad to produce an
aromatic compound and acid
The aromatic compound then combines with a
diazonium salt present on the pad to produce a purple
dye
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Page
39
Chemical Examination of Urine
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Chemical Examination of Urine
Specific Gravity
The polyelectrolyte ionizes, releasing hydrogen ions in
proportion to the number of ions in the solution
The higher the concentration of urine, the more
hydrogen ions are released, thereby lowering the pH
Incorporation of the indicator bromthymol blue on the
reagent pad measures the change in pH.
As the specific gravity increases, the indicator changes
from blue (1.000 [alkaline]), through shades of green to
yellow (1.030 [acid])
Readings can be made in 0.005 intervals by careful
comparison with the color chart.
Page
40
Introduction:
Specific gravity is a physical property of urine and an expression
of solute concentration.
The ultrafiltrate that enters the Bowmans space of the glomeruli
has the same SG as protein free plasma (1.010) isosthenuria
As the ultrafiltrate passes through the nephrons, solutes and
water are selectively absorbed and secreted thus increasing or
decreasing SG.
Normal SG is from 1.002 to 1.035. Values greater or lesser than
these require further investigation.
SG that is 1.000 or 1.040 is physiologically impossible.
The addition of SG to the test strip has eliminated a time
consuming step in routine urinalysis and has provided a
convenient method for routine screening.
Osmometry and Refractometry should never be replaced for
fluid monitoring as these are more accurate compared to
reagent strip testing for SG.
Reagent strip reaction
PRINCIPLE:
CHANGE IN pKa (dissociation constant) OF A POLYELECTROLYTE
IN AN ALKALINE MEDIUM
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Chemical Examination of Urine
Reasons for a 1.000 SG:
1. Specimen might not be urine
a. Check urea and creatinine. Urine always has urea
and creatinine while ordinary water does not.
2. Check QC of reagent strip
a. Strip might be outdated or deteriorated
Reasons for a 1.040 SG
1. Mannitol IV
The use of refractometry or osmometry usually resolves problems
with very high or low SG (counterchecking)
Page
41
Reaction Interference
Measures only ionic solutes
Thereby, eliminating interference by large organic
molecules such as:
Urea
Glucose
Radiographic contrast media
Plasma expanders
Analysts should consider what type of method is used
when testing for SG
Elevated concentrations of protein slightly increase the
readings as a result of protein anions
Specimens with a pH of 6.5 or higher have decreased
readings
Interference with the bromthymol blue indicator
Bromthymol blue reacts best with alkaline pH and
low specific gravity
Manufacturers recommend adding 0.005 to SG
when pH is 6.5 or higher
Correction is performed when using
automated strip readers
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
Chemical Examination of Urine
Overview
System Description
Semi-automated urine chemistry analyzer
Tests Measured
Automatic Measurement
Leukocyte, Nitrite, Protein, Blood, Glucose, Ketone, Bilirubin,
Urobilinogen, pH, Specific Gravity, Creatinine,* and Protein-to-Creatinine
Ratio*
Urine color
Test Format
Dry chemistry reagent strips
Test Measurement
Color change measured by reflectance photometry
Dual readings at reactive and reference wavelengths
Automatically adjusts for urine color
Sample Clarity
Results entered via keyboard or bar code reader
- Identification and reporting for validated Siemens strip
types
- Humidity exposure tested on every strip with leukocyte
pad
- Sample interferences, availability dependent upon strip
type**
Automatic Checks
(Auto-Checks)
You can fail at something you dont want, so might as
well take a chance doing what you love.
~James Eugene Carrey
By: Ken Kawakami, RMT, MLS(ASCPi)CM
@japanesejuan
42
Respond to demands for higher productivity and high quality
with the CLINITEK Advantus Analyzer. Streamline your workflow
with flexible operation.
Immediate start-up.
Automatic calibration.
Network ready.
A wide range of options.
Added QC features.
Flexible operation to meet your needs.
Page
(CLINITEK Advantus Analyzer)
Sources:
1. Urinalysis and Body Fluids by Susan King Strasinger and
Marjorie Schaub Di Lorenzo 5th edition
2. Urine and Body Fluid Analysis by Nancy A. Brunzel 3rd
edition
Вам также может понравиться
- Chemical ExaminationДокумент42 страницыChemical ExaminationpixiedustОценок пока нет
- Review in Clinical MicrosДокумент103 страницыReview in Clinical MicrosSyvelmarie Tinte100% (1)
- Urinalysis and Body Fluids for Cls & MltОт EverandUrinalysis and Body Fluids for Cls & MltОценок пока нет
- Recall Questions-February 14, 2018 Wyne Brent M. Corpuz, RMTДокумент4 страницыRecall Questions-February 14, 2018 Wyne Brent M. Corpuz, RMTRafael CayananОценок пока нет
- Clinical Chemistry KeyNotes For Board ExaminationДокумент12 страницClinical Chemistry KeyNotes For Board ExaminationPrincess Alen Aguilar100% (2)
- Hematology Review NotesДокумент29 страницHematology Review NotesCattrainuh100% (2)
- Hematology ReviewДокумент4 страницыHematology ReviewAlfred ChowОценок пока нет
- COMPLETE BLOOD COUNT Lecture GuideДокумент9 страницCOMPLETE BLOOD COUNT Lecture GuideKaycee Gretz LorescaОценок пока нет
- Chapter 13 Rodaks HematologyДокумент10 страницChapter 13 Rodaks HematologyRALPH JAN T. RIOОценок пока нет
- Compiled Quizes AubfДокумент39 страницCompiled Quizes AubfCharmaine BoloОценок пока нет
- Immunohematology-Unit 1 Exam: Please Provide The Correct AnswerДокумент11 страницImmunohematology-Unit 1 Exam: Please Provide The Correct AnswerchavelОценок пока нет
- Hema 311 Lecture Guide Notes No. 8 - Anemia (Part 3)Документ6 страницHema 311 Lecture Guide Notes No. 8 - Anemia (Part 3)Nel TinduganiОценок пока нет
- University of The Immaculate Conception: ProteinДокумент13 страницUniversity of The Immaculate Conception: ProteinDams ZainalОценок пока нет
- Staphylococci: Streptococcus PyogenesДокумент20 страницStaphylococci: Streptococcus PyogenesPharmacy2015100% (2)
- Ascpi Recalls 2016Документ9 страницAscpi Recalls 2016Zylene Gabriel100% (1)
- Clinical Microscopy ExamДокумент3 страницыClinical Microscopy ExamKarla GiorlaОценок пока нет
- Clinical Chemistry 2 Lecture Notes in Trace ElementsДокумент6 страницClinical Chemistry 2 Lecture Notes in Trace ElementsMoira Pauline LibroraniaОценок пока нет
- Must To Know in Immunology and Serology ImmunologyДокумент19 страницMust To Know in Immunology and Serology ImmunologyCath PortezОценок пока нет
- Immunology Serology ReviewДокумент211 страницImmunology Serology ReviewRachel Marie M. Gania100% (1)
- MUST To KNOW in Blood Banking 1Документ19 страницMUST To KNOW in Blood Banking 1Aya Virtucio100% (1)
- Medical TechnologyДокумент13 страницMedical Technologyangelina buenaОценок пока нет
- Clin Chem CompiledДокумент9 страницClin Chem CompiledReg LagartejaОценок пока нет
- Clinical Chemistry Notes With BlanksДокумент34 страницыClinical Chemistry Notes With Blanksepson printerОценок пока нет
- Hematology ReviewerДокумент10 страницHematology ReviewerAldren BeliberОценок пока нет
- Notes CM 1Документ15 страницNotes CM 1Mae HernandezОценок пока нет
- Clinical Chemistry Notes (Blanked) - ABI PDFДокумент34 страницыClinical Chemistry Notes (Blanked) - ABI PDFAnya IgnacioОценок пока нет
- Blood Banking Course BookДокумент2 страницыBlood Banking Course BookShukr Wesman BlbasОценок пока нет
- Beginings of MTДокумент65 страницBeginings of MTMel JamitoОценок пока нет
- Hematology2 - Laboratory TestsДокумент3 страницыHematology2 - Laboratory Testskthmnts100% (1)
- Clinical Microscopy: Definition and Volume Disease and Cause PolyuriaДокумент5 страницClinical Microscopy: Definition and Volume Disease and Cause PolyuriaJovanni andesОценок пока нет
- Role of Blood Vessels in Hemostasis: Villa, M.D. MLS 4CДокумент10 страницRole of Blood Vessels in Hemostasis: Villa, M.D. MLS 4CMarianne Dennesse100% (1)
- 8.nature of Clinical Laboratory - EditedДокумент56 страниц8.nature of Clinical Laboratory - EditedJr BalagtasОценок пока нет
- Chapter 1: An Overview of Clinical LaboratoryДокумент13 страницChapter 1: An Overview of Clinical LaboratoryAshley Tañamor100% (2)
- Immunology and Serology TestsДокумент2 страницыImmunology and Serology TestsPearlregine Cianne MirandaОценок пока нет
- Must To Know HemaДокумент44 страницыMust To Know HemaKaycee Gretz LorescaОценок пока нет
- Summary of Reagent Strip TestsДокумент8 страницSummary of Reagent Strip TestsDarla YsavelОценок пока нет
- Chapter 4 Physical Examination PDFДокумент4 страницыChapter 4 Physical Examination PDFJulie Anne Soro ValdezОценок пока нет
- ISBBhandoutДокумент55 страницISBBhandoutRed GillianОценок пока нет
- AUB - Chemical Analysis of UrineДокумент5 страницAUB - Chemical Analysis of UrineJeanne RodiñoОценок пока нет
- Hema Notes (Lec)Документ50 страницHema Notes (Lec)Anonymous 0zrCNQОценок пока нет
- LN Hematology MLT FinalДокумент549 страницLN Hematology MLT FinalMahfuzur Rahman100% (3)
- Clinical Microscopy ReviewerДокумент31 страницаClinical Microscopy ReviewerbokbokbokОценок пока нет
- MUST To KNOW in Clinical ChemistryДокумент53 страницыMUST To KNOW in Clinical ChemistryMonkey LuffyОценок пока нет
- CHEM 2 CH 29 Review QuestionsДокумент2 страницыCHEM 2 CH 29 Review QuestionsthrowawyОценок пока нет
- Week 2 Chemical Examination of UrineДокумент44 страницыWeek 2 Chemical Examination of UrineDayledaniel SorvetoОценок пока нет
- Disorders of Iron Kinetics and Heme MetabolismДокумент12 страницDisorders of Iron Kinetics and Heme MetabolismJoanne JardinОценок пока нет
- Pre and Post Analytical Procedures: Subtopic: Receiving, Accessioning, & Releasing of ResultsДокумент29 страницPre and Post Analytical Procedures: Subtopic: Receiving, Accessioning, & Releasing of ResultsShara AboОценок пока нет
- Lecture & Review Guide in HEMATOLOGY 1 & 2 (COMPLETE)Документ58 страницLecture & Review Guide in HEMATOLOGY 1 & 2 (COMPLETE)Kirt Anonuevo100% (3)
- Week3-Physical Examination of UrineДокумент24 страницыWeek3-Physical Examination of UrineDayledaniel SorvetoОценок пока нет
- AUB - Intro To UrinalysisДокумент3 страницыAUB - Intro To UrinalysisJeanne RodiñoОценок пока нет
- AUBF QuetionsДокумент34 страницыAUBF QuetionsAprille Patol100% (1)
- Mls 419: Aubf Lab Semen Analysis 5% Spermatozoa 60-70% Seminal Fluid 20-30% Prostate FluidДокумент24 страницыMls 419: Aubf Lab Semen Analysis 5% Spermatozoa 60-70% Seminal Fluid 20-30% Prostate FluidLyra Dennise LlidoОценок пока нет
- CC Musttoknow RodriguezДокумент44 страницыCC Musttoknow RodriguezAngelo Mercede100% (1)
- Microscopic Examination of UrineДокумент4 страницыMicroscopic Examination of UrineGlaiza Erika Baes GudaОценок пока нет
- Chapter 2 Introduction To Urinalysis PDFДокумент4 страницыChapter 2 Introduction To Urinalysis PDFJulie Anne Soro ValdezОценок пока нет
- Clinical Chemistry Notes Without Blanks LegitДокумент43 страницыClinical Chemistry Notes Without Blanks LegitPearl Isabelle SudarioОценок пока нет
- Agglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4От EverandAgglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4Оценок пока нет
- Concreteness For 40000 Words BrysbaertДокумент27 страницConcreteness For 40000 Words BrysbaertLAb MehОценок пока нет
- 8 Mind-Blowing Myths About Rizal: Kjane L. Felicilda History 12Документ2 страницы8 Mind-Blowing Myths About Rizal: Kjane L. Felicilda History 12LAb MehОценок пока нет
- College AlgebraДокумент297 страницCollege AlgebraLAb Meh100% (1)
- MICROSCOPIC EXAMINATION OF URINE 2015 Notes PDFДокумент11 страницMICROSCOPIC EXAMINATION OF URINE 2015 Notes PDFLAb Meh100% (1)
- Ediza M. Martinez: ShielaДокумент14 страницEdiza M. Martinez: ShielaLAb MehОценок пока нет
- Car ProjectДокумент37 страницCar ProjectLAb MehОценок пока нет
- My Teaching Philosophy: By: Eden Key L. Felicilda BSED-MATHДокумент8 страницMy Teaching Philosophy: By: Eden Key L. Felicilda BSED-MATHLAb MehОценок пока нет
- CHAPTER 5 - STATES OF MATTER (S) Edit20152016Документ12 страницCHAPTER 5 - STATES OF MATTER (S) Edit20152016PAKK20622P Syarifah Nor Izzah binti Syed Abd HamidОценок пока нет
- WEEK 3 LAB EXERCISE - Cell Structures and Functions - UY-OCOДокумент4 страницыWEEK 3 LAB EXERCISE - Cell Structures and Functions - UY-OCOBianca LouiseОценок пока нет
- Development of Elevator Ropes: Tech Tip 15Документ2 страницыDevelopment of Elevator Ropes: Tech Tip 15أحمد دعبسОценок пока нет
- Morita Therapy For Depression and AnxietyДокумент13 страницMorita Therapy For Depression and AnxietyPedro GuimarãesОценок пока нет
- Industrial SpecialtiesДокумент103 страницыIndustrial SpecialtiesRahul ThekkiniakathОценок пока нет
- 6th Grade Spelling ListsДокумент10 страниц6th Grade Spelling Listsapi-326416336Оценок пока нет
- Barangay Clearance SampleДокумент1 страницаBarangay Clearance SampleBarangay Onse Malaybalay100% (3)
- CSF LeaksДокумент3 страницыCSF LeaksDrTarek Mahmoud Abo KammerОценок пока нет
- Powermatic 58480438-Millrite-Mvn-Manual PDFДокумент54 страницыPowermatic 58480438-Millrite-Mvn-Manual PDFJason Willis75% (4)
- Chuyên Anh S Hà N I 2021Документ5 страницChuyên Anh S Hà N I 2021Jennifer WatsonОценок пока нет
- 15-Statutory Report Statutory Define Law (Legal Protection) Statutory MeetingДокумент2 страницы15-Statutory Report Statutory Define Law (Legal Protection) Statutory MeetingRaima DollОценок пока нет
- Gastroschisis and Omphalocele PDFДокумент8 страницGastroschisis and Omphalocele PDFUtama puteraОценок пока нет
- Marantz - dv-4200 DVD Player PDFДокумент60 страницMarantz - dv-4200 DVD Player PDFH.V KayaОценок пока нет
- Operator's Manual: SE Series Slab ScissorsДокумент52 страницыOperator's Manual: SE Series Slab ScissorsthuanОценок пока нет
- All Vaccinees Are Requested To Bring Certificate of Dose-II From COWIN Portal Alongwith Registered Mobile Number Before Proceeding For VaccinationДокумент7 страницAll Vaccinees Are Requested To Bring Certificate of Dose-II From COWIN Portal Alongwith Registered Mobile Number Before Proceeding For VaccinationRakesh KumarОценок пока нет
- Stats Review CH 1-6Документ15 страницStats Review CH 1-6Megha BanerjeeОценок пока нет
- Chapter 23Документ9 страницChapter 23Trixie Myr AndoyОценок пока нет
- Phyilosophy of Midwifery Care 2Документ13 страницPhyilosophy of Midwifery Care 2Noella BezzinaОценок пока нет
- Screenshot 2019-10-30 at 12.44.00Документ25 страницScreenshot 2019-10-30 at 12.44.00Miền VũОценок пока нет
- The Nursing ShortageДокумент6 страницThe Nursing Shortageapi-455495817Оценок пока нет
- Anesthesia 3Документ24 страницыAnesthesia 3PM Basiloy - AloОценок пока нет
- GASESДокумент55 страницGASESja_QuinineОценок пока нет
- Materials Management in Hospital Industry Nandi ProjectДокумент27 страницMaterials Management in Hospital Industry Nandi Projectkumaraswamy226Оценок пока нет
- MODEL 1332 MODEL 1432: Slide LengthДокумент8 страницMODEL 1332 MODEL 1432: Slide LengthFabian FragosoОценок пока нет
- PED16 Foundation of Inclusive Special EducationДокумент56 страницPED16 Foundation of Inclusive Special EducationCHARESS MARSAMOLO TIZONОценок пока нет
- Sadcas TR 14 - Sadcas Policy - Iso Iec 17025-2017 TransitionДокумент16 страницSadcas TR 14 - Sadcas Policy - Iso Iec 17025-2017 TransitionSuresh KumarОценок пока нет
- ZX 470Документ13 страницZX 470Mohammed Shaheeruddin100% (1)
- Recognizing Fractures and Dislocations: Corpuz, Rachella Nicole PДокумент46 страницRecognizing Fractures and Dislocations: Corpuz, Rachella Nicole PRachella Nicole CorpuzОценок пока нет
- Application of Knowledge QuestionsДокумент16 страницApplication of Knowledge QuestionsElllie TattersОценок пока нет
- Unit Plan Adult Health Nursing Unit IIДокумент7 страницUnit Plan Adult Health Nursing Unit IIDelphy VargheseОценок пока нет