Академический Документы
Профессиональный Документы
Культура Документы
OPTH 15696 Treatment of Noninfectious Posterior Uveitis With Dexamethas 120310
Загружено:
Muhammad Habibul IhsanАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
OPTH 15696 Treatment of Noninfectious Posterior Uveitis With Dexamethas 120310
Загружено:
Muhammad Habibul IhsanАвторское право:
Доступные форматы
Clinical Ophthalmology
Dovepress
open access to scientific and medical research
Case Series
Open Access Full Text Article
Treatment of noninfectious posterior uveitis
with dexamethasone intravitreal implant
This article was published in the following Dove Press journal:
Clinical Ophthalmology
3 December 2010
Number of times this article has been viewed
Jane S Myung
Grant D Aaker
Szilrd Kiss
Department of Ophthalmology,
Weill Cornell Medical Center,
New York, NY, USA
Purpose: To report our experience with dexamethasone 0.7mg sustained-release intravitreal
implant (Ozurdex; Allergan, Inc, Irvine, CA) in noninfectious posterior uveitis.
Methods: A retrospective chart review of patients with noninfectious uveitis treated with
sustained-release dexamethasone 0.7 mg intravitreal implant was performed. Complete
ophthalmic examination including signs of inflammatory activity, visual acuity, fundus
photography, fluorescein angiography, optical coherence tomography, and tolerability of the
implant were assessed.
Results: Six eyes of 4 consecutive patients treated with a total of 8 dexamethasone 0.7mg
sustained-release intravitreal implants for posterior noninfectious uveitis were included. Two
patients presented with unilateral idiopathic posterior uveitis; 2 patients had bilateral posterior
uveitis, one secondary to sarcoidosis and the other to Vogt-Koyanagi-Harada syndrome.
All eyes showed clinical and angiographic evidence of decreased inflammation following
implant placement. Mean follow-up time post-injection was 5.25months. Four eyes received
1 and 2 eyes received 2 Ozurdex implants during the follow-up period. The duration of effect
of the implant was 3 to 4months. No serious ocular or systemic adverse events were noted
during the follow-up period.
Conclusions: In patients with noninfectious posterior uveitis, sustained-release dexamethasone
0.7mg intravitreal implant may be an effective treatment option for controlling intraocular
inflammation.
Keywords: corticosteroids, dexamethasone implant, Ozurdex, uveitis
Introduction
Correspondence: Szilrd Kiss
Department of Ophthalmology,
Weill Cornell Medical Center, 1305
York Avenue, 11th Floor, New York,
NY 10021, USA
Tel +1 646-962-2217
Fax +1 646-962-0609
Email szk7001@med.cornell.edu
submit your manuscript | www.dovepress.com
Dovepress
DOI: 10.2147/OPTH.S15696
The mainstay of treatment for noninfectious uveitis remains corticosteroids. Regional
steroids have the advantage of minimizing systemic side effects; however, local side
effects can include increased intraocular pressure, cataract, and sterile and infectious
endophthalmitis.1,2
Dexamethasone has potent anti-inflammatory properties with a favorable side-effect
profile.35 Previous studies demonstrated that dexamethasone in a biodegradable drug
delivery system (Ozurdex; Allergan Inc, Irvine, California, USA) can improve visual
acuity (BCVA) and macular thickness in a variety of settings.35 Here, we describe
our experience with treating noninfectious posterior uveitis with the Ozurdex 0.7mg
dexamethasone intravitreal implant.
Materials and methods
A retrospective chart review of patients treated with Ozurdex for noninfectious posterior
uveitis was undertaken with IRB approval of Weill Cornell Medical College. Included
Clinical Ophthalmology 2010:4 14231426
1423
2010 Myung etal, publisher and licensee Dove Medical Press Ltd. This is an Open Access article
which permits unrestricted noncommercial use, provided the original work is properly cited.
Dovepress
Myung etal
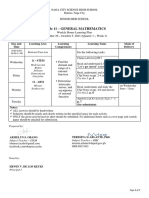
Table 1 Baseline demographics, diagnosis and examination findings of all patients with total follow-up period and final visual acuity
outcomes
Patient
Age
Sex
Diagnosis
Baseline
BVCA
FA
OCT
Prior
treatment
No.
Ozurdex
Total
follow-up
(months)
Final
BCVA
30
Sarcoidosis
20/20 OU
No CME
6 OU
20/20 OU
49
Vogt-KoyanagiHarada
Count fingers
OU
Prednisone
60mg and
STT
STT
1 OU
1 OD
2 OS
2 OD
4 OS
20/20 OD
20/30 OS
29
Idiopathic retinal
vasculitis
Hand motion
OS
81
Idiopathic
anterior NG
uveitis with CME
20/50 OD
Disc and
perivascular
leakage
Hyperfluorescent
dots at level of
RPE with leakage
into serous RDs
Extensive disc,
perivascular, and
parafoveal leakage
Late parafoveal
leakage
Serous
RDs
CME
None
20/40 OS
CME
Topical
prednisolone
acetate
20/50 OD
Abbreviations: BCVA, best-corrected visual acuity Snellen equivalent in the study eye; CME, cystoid macular edema; STT, sub-Tenons triamcinolone; RD, retinal
detachment; NG, nongranulomatous; OD, right eye; OS, left eye; OU, both eyes; OCT, optical coherence tomography; FA, fluorescein angiography.
were demographics, etiology of inflammation, BCVA, prior
therapies, examination, and adverse events.
Patients underwent a comprehensive examination including
optical coherence tomography (OCT), fluorescein angiography
(FA), and fundal photography. A systemic work-up included
laboratory and radiographic imaging for infectious and noninfectious etiologies. Ozurdex was administered in accordance
with the manufacturers instructions using the 22-gauge
applicator device (Ozurdex package http://www.allergan.
com/assets/pdf/ozurdex_pi.pdf).
Results
Six eyes of 4 patients were included. Patient demographics,
diagnosis, and examination findings are summarized
in Table 1. Mean follow-up time post-injection was
5.25months (range 28months). No serious systemic or
ocular treatment-related adverse events occurred. Subconjunctival hemorrhage occurred at the injection site.
Intraocular pressures remained unchanged in all eyes during
follow-up.
Patient 1
A 30-year-old female presented with papillitis and retinal
vasculitis of the left eye (OS). A work-up revealed a
diagnosis of sarcoidosis. Despite 60 mg of oral prednisone and 1 sub-Tenons triamcinolone injection OS, there
was persistent inflammation. Similar findings developed
in the right eye (OD). Ozurdex was administered in both
eyes (OU). Six months post-Ozurdex and off oral steroids,
the patient shows no signs of inflammation (Figure1).
1424
submit your manuscript | www.dovepress.com
Dovepress
Figure 1 A) Fluorescein angiography (FA) left eye (OS) of patient 1 showing
persistent leakage of the disc and perivascular leakage (yellow arrows) after
treatment with oral prednisone and sub-Tenons triamcinolone OS. B) FA right eye
(OD) showing progression to the fellow eye with leakage of the disc and perivascular
leakage (yellow arrow) while on oral prednisone. CD) FA 4 weeks following the
0.7 mg dexamethasone implantation in both eyes showing resolution of papillitis
vasculitis. E) Fundal photography shows the location of the implant in the inferior
vitreous base in OS. FG) FA 4 months following the 0.7 mg dexamethasone
intravitreal implant and 6 weeks after finishing oral steroids, showing no recurrence
of papillitis or vasculitis in both eyes.
Clinical Ophthalmology 2010:4
Dovepress
Patient 2
A 49-year-old male presented with bullous serous retinal detachments (RD) OU. OCT showed multiple large
serous RDs. A work-up was positive for HLA-DR4.
A diagnosis of probable Vogt-Koyanagi-Harada (VKH)
disease was made.6 The patient received 1 sub-Tenons
triamcinolone injection OS with no improvement. Ozurdex
was administered OS and oral prednisone 60mg started.
BCVA improved to 20/50 OD and 20/25 OS. For persistent
subretinal fluid (SRF) OD, Ozurdex was given. Both eyes
developed recurrent SRF after oral prednisone taper.
A second Ozurdex implant was given OS and oral prednisone re-started. At final visit 4months after initial Ozurdex
implant, on oral prednisone, BCVA was 20/20 OD and 20/30
OS with no SRF OU.
Patient 3
A 29-year-old female presented with hand motion
vision OS. Examination showed vitritis, papillitis, and
vasculitis OS. OCT showed cystoid macular edema (CME).
Uveitis work-up was negative; the patient was diagnosed with
idiopathic ocular inflammtion. Ozurdex was administered.
At 2.5 months post-Ozurdex, BCVA was 20/40 without
CME. At 4-month follow-up, OCT showed recurrent CME.
A second Ozurdex was given. Four months after the second
implant, BCVA was 20/40 with no CME (Figure2).
Patient 4
An 81-year-old female presented with recurrent nongranulomatous uveitis OD treated with topical prednisolone.
Treatment of noninfectious uveitis with dexamethasone intravitreal implant
Uveitis work-up was unrevealing. BCVA was 20/50.
Examination showed anterior chamber inflammation. OCT
showed CME OD. The patient received Ozurdex. At 1-month
follow-up, off of topical steroids, inflammation and CME
resolved. BCVA remained 20/50 due to pre-existing cataract.
Four months post-implant, inflammation and CME returned;
patient deferred further intervention.
Discussion
In the present series, Ozurdex was able to successfully control inflammation and improve CME in 4 eyes of 3 patients.
Two cases failed prior local therapy. The duration of effect
of the implant was approximately 3 to 4months. No patients
developed major systemic or ocular side effects, particularly
ocular hypertension. However, follow-up time was insufficient to assess cataract formation.
There was recurrence of SRF after oral prednisone taper
despite recent Ozurdex implants with probable VKH. There
have been a few reports of VKH treatment with intravitreal
corticosteroids with mixed results.79 Thus, systemic treatment remains the mainstay of therapy. However, intravitreal
corticosteroids may play a role as adjuvant therapy.
Although the results of phase 3 trial of Ozurdex in
noninfectious uveitis have been completed and Ozurdex
recently received approval in the United States, this series
is, to the best of our knowledge, one of first to report clinical
experience with Ozurdex.10 Our series confirms that Ozurdex
can be effective for treating noninfectious uveitis; however,
the durability of that effect was considerably shorter than the
6-month reinjection interval typically utilized in retinal vein
Figure 2 A) Baseline fundal photography left eye (OS) of patient 3 showing vitritis, papillitis and widespread vasculitis with extensive sheathing of the vessels in OS.
B) Baseline fluorescein angiography (FA) right eye (OD) showing no evidence of inflammation. C) Baseline FA OS revealed papillitis and considerable vasculitis OS. D)
Baseline optical coherence tomography (OCT) OS with cystoids macular edema (CME). E) FA OS 11days following the 0.7mg dexamethasone intravitreal implant showed
significantly decreased perivascular, optic disc, and parafoveal leakage, and F) OCT revealed a drastic reduction in CME. G) 2.5months following implant placement OCT OS
showed no recurrence of CME. H) Almost 4months following implant placement OCT OS showed return of CME. I) Two months after receiving a second dexamethasone
implant OCT OS showed resolution of CME.
Clinical Ophthalmology 2010:4
submit your manuscript | www.dovepress.com
Dovepress
1425
Myung etal
occlusion.11 Further prospective, controlled studies need to
be performed to better determine efficacy, duration of effect,
and side effects.
Disclosure
Dr Szilrd Kiss serves on the Physician Speakers Bureau for
Allergan, Inc, Irvine, California. No financial support was
received for this study. Drs Jane S. Myung and Grant D. Aaker
declare no potential conflicts of interest.
References
1. van Kooji B, Rothova A, de Vries P. The pros and cons of intravitreal
triamcinolone injections for uveitis and inflammatory cystoid macular
edema. Ocul Immunol Inflamm. 2006;14:7385.
2. Goldstein DA, Godfrey DG, Hall A, et al. Intraocular pressure in
patients with uveitis treated with fluocinolone acetonide implants.
Arch Ophthalmol. 2007;125:14781485.
3. Kupperman BD, Blumenkranz MS, Haller JA, etal. Dexamethasone
DDS Phase II Study Group. Randomized controlled study of an
intraveitreous dexamethasone drug delivery system in patients with
persistent macular edema. Arch Ophthalmol. 2007;125:309317.
4. Williams GA, Haller JA, Kupperman BD, et al. Dexamethasone
DDS Phase II Study Group. Dexamethasone Posterior-Segment Drug
Delivery System in the treatment of macular edema resulting from uveitis
or Irvine-Gass syndrome. Am J Ophthalmol. 2009;147:10481054.
Clinical Ophthalmology
Publish your work in this journal
Clinical Ophthalmology is an international, peer-reviewed journal
covering all subspecialties within ophthalmology. Key topics include:
Optometry; Visual science; Pharmacology and drug therapy in eye
diseases; Basic Sciences; Primary and Secondary eye care; Patient
Safety and Quality of Care Improvements. This journal is indexed on
Dovepress
5. Haller JA, Kupperman BD, Blumenkranz MS, etal. Dexamethasone
DDS Phase II Study Group. Randomized controlled trial of intravitreous
dexamethasone drug delivery system in patients with diabetic macular
edema. Arch Ophthalmol. 2010;128:289296.
6. Read RW, Holland GN, Rao NA, etal. Revised diagnostic criteria for
Vogt-Koyanagi-Harada disease: report of an international committee
on nomenclature. Am J Ophthalmol. 2001;131:647652.
7. Karacorlu M, Arf Karacorlu S, Ozdemir H. Intravitreal triamcinolone acetonide in Vogt-Koyanagi-Harada syndrome. Eur J Ophthal.
2006;16:481483.
8. Andrade RE, Muccioli C, Farah ME, Nussenblatt RB, Belfort R.
Intravitreal triamcinolone in the treatment of serous retinal detachments
in Vogt-Koyanagi-Harada syndrome. Am J Ophthalmol. 2004;137:
572574.
9. Khalifa Y, Loh AR, Acharya NR. Fluocinolone acetonide intravitreal
implants in Vogt-Koyanagi-Harada disease. Ocul Immunol Inflamm.
2009;17:431433.
10. United States Food and Drug Administration Website. http://www.
accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm?fuseaction=Search.
DrugDetails. Accessed 2010 Sep 30.
11. Haller JA, Bandello F, Belfort R Jr, etal. OZURDEX GENEVA Study
Group. Randomized, sham-controlled trial of dexamethasone intravitreal
implant in patients with macular edema due to retinal vein occlusion.
Ophthalmology. 2010;117:11341146.
Dovepress
PubMed Central and CAS, and is the official journal of The Society of
Clinical Ophthalmology (SCO). The manuscript management system
is completely online and includes a very quick and fair peer-review
system, which is all easy to use. Visit http://www.dovepress.com/
testimonials.php to read real quotes from published authors.
Submit your manuscript here: http://www.dovepress.com/clinical-ophthalmology-journal
1426
submit your manuscript | www.dovepress.com
Dovepress
Clinical Ophthalmology 2010:4
Вам также может понравиться
- Sala Lauak: 500 Grams of Rice Powder 50 Grams of Small Shrimp 2 Centimeters of GinggerДокумент1 страницаSala Lauak: 500 Grams of Rice Powder 50 Grams of Small Shrimp 2 Centimeters of GinggerMuhammad Habibul IhsanОценок пока нет
- COVERДокумент1 страницаCOVERMuhammad Habibul IhsanОценок пока нет
- Disorders Transition To Schizophrenia in Acute and Transient PsychoticДокумент8 страницDisorders Transition To Schizophrenia in Acute and Transient PsychoticMuhammad Habibul IhsanОценок пока нет
- Governance, Risk and Compliance Final Exam PaperДокумент1 страницаGovernance, Risk and Compliance Final Exam PaperMuhammad Habibul IhsanОценок пока нет
- You Give Me Something ChordДокумент2 страницыYou Give Me Something ChordMuhammad Habibul IhsanОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- SMF Update Barang 05 Desember 2022Документ58 страницSMF Update Barang 05 Desember 2022Apotek Ibnu RusydОценок пока нет
- Why We're Still Learning New Things About The JFK AssassinationДокумент8 страницWhy We're Still Learning New Things About The JFK AssassinationNolan SОценок пока нет
- Introduction To Financial Management: Topic 1Документ85 страницIntroduction To Financial Management: Topic 1靳雪娇Оценок пока нет
- Noli Me Tangere CharactersДокумент4 страницыNoli Me Tangere CharactersDiemОценок пока нет
- Untitled PresentationДокумент6 страницUntitled PresentationWayne ChenОценок пока нет
- POWEV2434234Документ461 страницаPOWEV2434234John M. HemsworthОценок пока нет
- Longman Communication 3000Документ37 страницLongman Communication 3000irfanece100% (5)
- Unit 9:: What Did You See at The Zoo?Документ11 страницUnit 9:: What Did You See at The Zoo?ARiFin MoHaMedОценок пока нет
- LEC 2017 - Post-Test in Organized Crime InvesДокумент8 страницLEC 2017 - Post-Test in Organized Crime InvesBokhary Dimasangkay Manok EliasОценок пока нет
- Back To Basics MROДокумент5 страницBack To Basics MROrstein666Оценок пока нет
- Bago Project CharterДокумент6 страницBago Project CharterLarize BautistaОценок пока нет
- Lab Exercise: 8Документ5 страницLab Exercise: 8Test UserОценок пока нет
- Στέργος Νεκτάριος-Μικκιος-CVДокумент4 страницыΣτέργος Νεκτάριος-Μικκιος-CVNektarios MikkiosОценок пока нет
- EikonTouch 710 ReaderДокумент2 страницыEikonTouch 710 ReaderShayan ButtОценок пока нет
- p2 Process Model 2017Документ1 страницаp2 Process Model 2017Miguel Fernandes0% (1)
- MacbethДокумент2 страницыMacbethjtwyfordОценок пока нет
- Maria Da Piedade Ferreira - Embodied Emotions - Observations and Experiments in Architecture and Corporeality - Chapter 11Документ21 страницаMaria Da Piedade Ferreira - Embodied Emotions - Observations and Experiments in Architecture and Corporeality - Chapter 11Maria Da Piedade FerreiraОценок пока нет
- Sir Rizwan Ghani AssignmentДокумент5 страницSir Rizwan Ghani AssignmentSara SyedОценок пока нет
- General Mathematics - Module #3Документ7 страницGeneral Mathematics - Module #3Archie Artemis NoblezaОценок пока нет
- Astro ExamДокумент7 страницAstro ExamRitu DuaОценок пока нет
- Business Finance Chapter 4Документ15 страницBusiness Finance Chapter 4chloe frostОценок пока нет
- 3 Murex HIV Ag Ab CombinationДокумент7 страниц3 Murex HIV Ag Ab CombinationElias Dii Rivas GarvanОценок пока нет
- Lecture - 4 - 28june2023Документ18 страницLecture - 4 - 28june2023vanshikaОценок пока нет
- March 2009 Caro-Kann B12 by Sasa Velickovic Informant83Документ6 страницMarch 2009 Caro-Kann B12 by Sasa Velickovic Informant83kiprijanovОценок пока нет
- Compilation 2Документ28 страницCompilation 2Smit KhambholjaОценок пока нет
- RBG - CRM BRD - Marketing - v4.1Документ68 страницRBG - CRM BRD - Marketing - v4.1Manvi Pareek100% (2)
- Chairperson 2012 Bar Examinations Committee: Bar Exam Question 2012 Martin S. Villarama, JRДокумент73 страницыChairperson 2012 Bar Examinations Committee: Bar Exam Question 2012 Martin S. Villarama, JRsejinma0% (1)
- Vip90 2021 Deso10Документ6 страницVip90 2021 Deso10Đỗ KhangОценок пока нет
- Filters SlideДокумент17 страницFilters SlideEmmanuel OkoroОценок пока нет
- RFP Nms 070708Документ183 страницыRFP Nms 070708Md RajaulОценок пока нет