Академический Документы
Профессиональный Документы
Культура Документы
Occipital Epilepsy Blume
Загружено:
DrHellenАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Occipital Epilepsy Blume
Загружено:
DrHellenАвторское право:
Доступные форматы
doi:10.
1093/brain/awh458
Brain (2005), 128, 12091225
Occipital epilepsy: lateral versus mesial
Warren T. Blume, Samuel Wiebe and Lisa M. Tapsell
University Hospital, The University of Western Ontario,
London, Ontario, Canada
Correspondence to: Warren T. Blume, University Hospital,
The University of Western Ontario, 339 Windermere
Road, London, Ontario, Canada N6A 5A5
E-mail: warren.blume@lhsc.on.ca
This study compares ictal semiology, neurological examination and scalp EEG between lateral and mesial occipital epilepsy to assess the contribution non-invasive data
make in determining the epileptogenic region within an
occipital lobe. We assessed seizure origin in 41 occipital
patients as lateral (11 patients), mesial (20) and both surfaces (10) as indicated by subdurally recorded seizures
(nine), a lesion whose removal reduced seizure quantity
by >90% (six), or who met both criteria (26). No aspect of
semiology distinguished lateral from mesially originating occipital seizures. A pre-operative visual field deficit
appeared in eight (42%) out of 19 testable patients
with mesial originating seizures, three (30%) out of
10 patients with both surfaces epileptogenic, but none
of the 10 testable patients whose seizures arose only
from the lateral surface (P = 0.0373, lateral versus mesial
and both surfaces). Although occipital seizures appeared
on the majority of the first five scalp EEG recordings in
four (36%) out of 11 patients with laterally originating
occipital seizures compared with none of 20 patients in
whom seizures originated mesially (P = 0.0105), no other
scalp EEG feature distinguished seizures from these surfaces. We conclude that subdural electroencephalography is likely to be necessary to delineate the epileptogenic
region within an occipital lobe. Nonetheless, focally originating scalp-recorded seizures accurately lateralized the
epileptogenic zone in 20 (49%) of our 41 patients compared with only one (2%) which originated contralaterally (P = 0.0001). This relationship held when considering
only the first five scalp EEGs: the seizures of 10 patients
(24%) appeared ipsilaterally and none contralaterally (P =
0.001). Moreover, interictal occipital (01,2) and posterior
temporal (T5, T6) spikes appeared consistently and significantly (P < 0.001) more commonly ipsilateral to epileptogenesis than contralateral using multiple methods of
analysis.
Keywords: epilepsy; occipital; semiology; EEG; location
Abbreviations: BA = Brodmann area
Received September 15, 2004. Revised January 21, 2005. Accepted January 31, 2005. Advance Access publication
March 23, 2005
Introduction
Considering the manifestations of epileptic seizures as providing insight into the workings of the cerebral cortex, John
Hughlings Jackson (quoted by Eadie MJ and Bladin PF,
2001) wrote: Cases of paralysis and convulsions may be
looked on as the results of experiments made by disease on
particular parts of the nervous system of man. Although
clinicalpathological associations formed the bases of his
formulations of cerebral function localization, Jackson nonetheless realized that such correlations were inexact as: (i) the
epileptic region involved relatively normal brain adjacent to a
lesion, not the lesion itself; and (ii) ictal manifestations could
represent propagation of epileptic discharge from its origin.
Thus he indicated: . . . there will be all varieties of epilepsy,
according to the exact position of grey matter altered . . . .
The variability and complexity of epileptic pathophysiology
implied in these prescient statements have been borne out in
subsequent studies. Williamson (1992), reviewing frontal lobe
seizures, indicated that: . . . widely different seizure types can
originate in similar regions of the frontal lobe and . . . similar
seizure types can occur with origin in different frontal
regions . . . . Similarly, attempts to sub-classify temporal
lobe seizures into mesial and neocortical types on the basis
of clinical characteristics have not succeeded (Walczak,
1995). In this context, we are unaware of clinical studies
comparing mesial and lateral occipital seizures, yet this
distinction is requisite in planning surgical resection.
Penfield and Rasmussen (1950) obtained only gross light,
shadows and colours when electrically stimulating the
# The Author (2005). Published by Oxford University Press on behalf of the Guarantors of Brain. All rights reserved. For Permissions, please email: journals.permissions@oupjournals.org
Downloaded from http://brain.oxfordjournals.org/ at Universitatea de Medicina si Farmacie ''Carol Davila on August 19, 2012
Summary
1210
W. T. Blume et al.
be: (i) more often unformed (unstructured); (ii) more
commonly localized focally in the visual field; and (iii)
less often associated with ocular deviation. Decisions surrounding sites of invasive recording for possible surgical
management are determined by the relative localizing values
of ictal semiology, neurological examination, interictal and
ictal EEG, and neuroimaging. Thus, we compare ictal semiology and scalp EEG findings in proven lateral occipital
seizure disorders to those of mesial occipital epilepsy. The
lateralizing value of occipital interictal and ictal epileptiform
potentials is also assessed as previous studies (Williamson
et al., 1992; Salanova et al., 1993) concluded that scalp EEG
fails to distinguish left from right occipital epileptogenesis.
Method
Focal occipital epilepsy was clinically suspected from: (i) ictal semiology (Penfield, 1954; Williamson et al., 1992; Blume and Wiebe,
2000); (ii) scalp interictal and ictal EEG (Blume and Wiebe, 2000),
and (iii) any occipital cortical lesion on MRI. Medical intractability
was determined by the hospitals epilepsy programme and referral
physicians on the bases of seizure incidence and severity, and
response to appropriate focal epilepsy management.
Strip or grid subdural recordings or both were made when noninvasive data did not adequately determine the principal epileptogenic region. Informed consent for telemetred recordings, invasive
recordings and any subsequent operation was obtained. Subdural
grid and strip electrodes consisted of 3 mm stainless steel disks
imbedded in silicon. Subdural strips were placed through burrholes
or by craniotomy for grid placement. All subdurally recorded
patients had bilateral mesial and lateral occipital coverage and
mesial temporal coverage. Most had lateral temporal electrodes
as well. Thus, multiple surface bilateral occipital subdural electroencephalography was performed in 35 out of 41 patients: 26 out of
32 with focal occipital neuroimaging lesions and nine without.
Ictal semiology was obtained by descriptions from the patient and
witness, and those of hospital personnel during seizures recorded by
the Epilepsy Unit. Specific aspects included: (i) location of formed
and unformed visual phenomena (Blume et al., 2001b); (ii) dyscognitive (complex partial) components; and (iii) motor phenomena
including ocular and cephalic versive, tonic, clonic and tonic
clonic features. Neurological examination features principally
sought included visual fields, motor deficits and congenital dermatological abnormalities.
Ictal and interictal epileptiform and non-epileptiform occipital,
temporal and diffuse scalp EEG patterns were visually assessed from
1618 channel out-patient and telemetered recordings comparing
mesially versus laterally originating occipital seizures as indicated
below. Each EEG feature was analysed in four ways, i.e. whether a
phenomenon appeared on: (i) any of the first five scalp recordings;
(ii) a majority of the first five scalp recordings; (iii) any of the scalp
recordings; and (iv) a majority of all the recordings.
We studied the following scalp EEG phenomena: (i) alpha symmetry; (ii) delta presence and location; (iii) occipital, temporal and
parietal spikes; (iv) bisynchronous epileptiform activity including
spike-waves; and (v) location of clinical and sub-clinical electrographic seizures, including the proportion with ambiguous origin.
We selected consecutive candidates for epilepsy surgery in whom
at least the majority of clinical seizures arose from an occipital lobe.
Thus, we included patients whose subdurally recorded seizures arose
Downloaded from http://brain.oxfordjournals.org/ at Universitatea de Medicina si Farmacie ''Carol Davila on August 19, 2012
occipital lobe and only occipital lobe stimulation produced
such unformed (unstructured) visual phenomena. Similarly,
Penfield (1954) described occipital seizures as consisting
of unstructured visual phenomena, although some of his
case reports describe generalized motor seizures as well.
He further indicated considerable overlap of visual phenomena between mesial and lateral occipital attacks; but only that
lateral occipital ictal visual phenomena were more apt to be
twinkling and bilateral than were mesial ones.
As the stages of sequential visual processing are unequally
represented on the mesial and lateral occipital surfaces, we
postulated that surface-specific ictal semiology would emerge.
In humans, the primary visual cortex [V1 or Brodmann area
17 (BA17)] lies mainly on the mesial aspect of the occipital
lobe (Truex and Carpenter, 1969). As the initial cortical area
of visual perception, stimuli recorded by the retina are
processed at V1 to provide information of features such as
precise retinal locus, spatial contrast, and orientation (Inouye,
1909; Hubel and Wiesel, 1979). Stimulation of the primary
visual cortex elicits simple phenomena such as flashes of light
[Forster (1929), cited by Brodal, 1981].
The first order visual association areas, particularly V4 and
V5, lie in the prestriate cortex (BA 18, 19) that surrounds the
primary visual cortex on the mesial surface and occupies all
the lateral occipital surface anterior to a rudiment of V1
(Gloor, 1997; Truex and Carpenter, 1969). V4, inhabiting
the caudal fusiform and adjacent lingual gyrus, constitutes
the principal origin of the ventral stream of visual processing providing inputs into the inferotemporal-occipital cortex
whose neurons are sensitive to form, pattern and colour
(Desimone and Ungerleider, 1989); this was subsequently
confirmed by human PET studies (Haxby et al., 1991).
The prestriate area also contains V5, probably at the region
of confluence of the occipital-parietal-temporal lobes. V5 is
a corresponding relay of the dorsal stream of visual processing concerned mainly with object localization and eyehand coordination (Goodale and Milner, 1992). The prestriate
cortex also contains multiple retinotopic maps of the contralateral visual field, each with a distinct functional role
(Zeki, 1976), but such maps lack the discrete and orderly
properties of the striate cortex (Kandel and Wurtz, 2000).
Thus, both V4 and V5 of the prestriate cortex convey stimuli
into higher-order visual processing areas in the occipitaltemporal lobe (ventral stream) and the parietal lobe (dorsal
stream). As V4 and V5 function as relays to the two streams
of higher-order visual processing, it is not surprising that
stimulation of the prestriate region by Forster (1929) elicited
more complex visual sensations such as animals, people and
various objects. Additionally, ocular deviation can be
obtained by stimulating the prestriate area (BA 18, 19),
but not the striate area (BA 17) (Truex and Carpenter,
1969). As a higher proportion of the mesial occipital region
is occupied by the striate cortex than is the lateral surface and
because of the considerable striate epileptogenicity (Ebersole
and Chatt, 1986), we postulated that, compared with
lateral originating seizures, mesial ictal phenomena would
Occipital epilepsy: lateral versus mesial
1211
Ictal semiology, age of onset, pathology
Results
EEG: ipsilateral versus contralateral
Seizures originated on the mesial surface in 20 patients, the
lateral surface in 11, and on both surfaces in 10 patients.
Occipital seizures appeared ipsilateral to the side of ultimately established epileptogenesis in the first five records
(A)
No aspect of ictal semiology (Tables 1 and 2) distinguished
laterally from mesially originating occipital seizures. A preoperative visual field defect appeared in eight (42%) of the
19 testable patients with mesially originating seizures, three
(30%) of the 10 patients with both surfaces epileptogenic, but
none of the 10 testable patients whose seizures arose only
from the lateral surface (P = 0.0265, lateral versus mesial;
P = 0.0373, lateral versus mesial and both; Table 3).
Age of current seizure onset did not significantly differ
among the groups (Table 4) nor did type of pathology
(Table 5).
Ictal semiology and epileptogenic areas of individual
patients appear in the Appendix.
EEG analyses: mesial versus lateral
With a single exception, none of the studied scalp EEG features (Table 6) distinguished lateral versus mesial occipital
epileptogenesis when analysed according to the presence of
a phenomenon on any, or a majority, of the first five or all preinvasive scalp recordings. The single exception was that
occipital seizures appeared in a majority of the first five
scalp EEG recordings in four (36%) out of 11 patients
with laterally originating occipital seizures compared with
none of 20 patients in whom the seizures originated mesially
(P = 0.0105).
1
2
3
4
5
6
7
8
9
10
Fig. 1 Continued on next page.
Downloaded from http://brain.oxfordjournals.org/ at Universitatea de Medicina si Farmacie ''Carol Davila on August 19, 2012
from a single occipital lobe (nine patients), those with an occipital
lesion whose removal reduced seizure quantity by >90% (six
patients), or who met both criteria (26 patients). Anterior limits
of the occipital lobe were determined on the lateral surface by
the upper end of the parietal occipital fissure and the preoccipital
notch (Leavens, 1991). The mesial occipital surface was defined as
the cuneus and the lingual gyrus, each extending to the anterior
limits as above defined. Therefore, the inferior limit of the mesial
surface was considered the collateral sulcus and its anterior limit the
parietal-occipital fissure and a line extending from it inferiorly to
the pre-occipital notch. Its superior limit was the border between the
mesial surface and the lateral convexity (Truex and Carpenter,
1969). The remainder of the occipital lobe was considered lateral
for the purpose of this study. Anatomical borders were applied to
both electrographic and imaging data. The epileptogenic surface was
identified as lateral, mesial or both based on subdural seizure origin,
location of an epileptogenic lesion or both. Lateral or mesial was
identified if all seizures arose from a single surface and any epileptogenic lesion resided there (Fig. 1). Both surfaces were considered
epileptogenic within an occipital lobe if: (i) seizure origins varied
between mesial and lateral surfaces or onset appeared on both surfaces; (ii) a relevant lesion involved both surfaces; or (iii) a lesion
occupied mostly one aspect while seizures arose from the other.
Excluded were occipital seizure patients with a more active extraoccipital epileptogenic zone defined by scalp, invasive EEG, or both.
Forty-one patients satisfied these criteria.
Prior to invasive recordings (subdurals in 35 patients: electrocorticography in six patients), five patients had 15 outpatient and
telemetered EEGs, 16 patients had 610 recordings, 15 patients
had 1120 recordings, and five patients had >20 recordings.
1212
W. T. Blume et al.
(B)
1
2
3
4
6
7
8
9
10
(C)
1
2
3
4
5
6
7
8
9
10
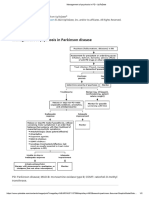
Fig. 1 Representation of subdurally recorded EEGs of patient whose occipital seizures arose simultaneously from both mesial and lateral
surfaces. Depicts a limited sample of multiple left mesial and lateral electrode positions. First four channels represent a vertically orientated
mesial line extending from just above the calcarine cortex downwards; the bottom six lines depict an obliquely-placed electrode extending
from the junction of the mesial and lateral surfaces (channel 5) around to the convexity in a posterior to anterior direction on the occipital
lobe convexity (channels 610). (A) Widely synchronous interictal spikes involving principally the lateral surface but clearly present on
mesial derivations as well. (B) Clinical seizure begins as high frequency waves in principally the lateral surface (channels 69) and
evolving instantly to a more restricted portion of the mesial surface (channels 3,4). (C) Seizure now involves principally the mesial surface
(channels 3,4) but involves both surfaces in a widespread fashion. Settings: 50 mV/mm; 30 mm/sec.
Downloaded from http://brain.oxfordjournals.org/ at Universitatea de Medicina si Farmacie ''Carol Davila on August 19, 2012
Occipital epilepsy: lateral versus mesial
Table 1 Seizure semiology and surface of
occipital seizure origin
Table 5 Pathology* and epileptogenic surface
Lateral
Mesial
Both
Total
11
10
9
5
1
3
1
2
3
9
0
8
10
10
2
0
20
15
13
8
5
4
6
2
3
17
2
10
16
17
8
1
10
10
9
6
0
3
4
0
0
6
0
5
8
10
3
0
41
35
31
19
6
10
11
4
6
32
2
23
34
37
13
1
All relationships in this table are statistically non-significant.
Table 2 Unformed visual ictal phenomena
Number of patients
Contralateral
Bilateral
Ipsilateral
Lateral
Mesial
Both
11
4
6
0
20
9
5
0
10
8
6
0
P = 0.4908 (not significant).
Table 3 Visual fields
Number of patients
Normal
Quadrantopia/hemianopia
Untestable (optic atrophy)
Lateral
Mesial
Both
11
10
0
1
20
11
8
1
10
7
3
0
P = 0.0265 (10 lateral versus 19 mesial testable patients).
P = 0.0373 [lateral versus mesial and both (39 testable patients)].
Table 4 Age of current seizure onset (years)
Number of patients
Mean
Median
Lateral
Mesial
Both
11
10.7
12
20
11.5
8
10
13
10.5
ANOVA P value = 0.8580 (not significant).
of 10 (24%) of these 41 patients and none appeared contralaterally (P = 0.001) (Table 7). Considering all pre-invasive
EEGs among these 41 patients, ipsilaterally originating occipital seizures appeared in 20 (49%) compared with one (2%)
contralaterally (P = 0.0001).
All four methods of scalp EEG analysis disclosed that
occipital (01, 02) and posterior temporal (T5, T6) spikes
each appeared more commonly ipsilateral to epileptogenesis
Number of patients
Dysplasia
Ischaemia/ulegyria
Ganglioglioma
Arteriovenous malformation
Lateral
Mesial
Both
11
2
0
1
1
20
2
3
3
1
10
1
2
0
2
*Four most common pathological findings. Others are: astrocytoma (three patients); dysembryoblastic neuroepithelial tumour
(two); traumatic scar (two); non-specific gliosis (two); chronic
encephalitis (one); meningeal angiomatosis (one); normal (eight);
unavailable (four).
Table 6 EEG items present on any of first five scalp
EEGs (31 patients)*
Number of patients
Ipsilateral alpha reduction
Ipsilateral posterior delta
Bilateral posterior delta
Ipsilateral occipital spikes
Contralateral occipital spikes
Ipsilateral posterior temporal spikes
Contralateral posterior temporal spikes
Ipsilateral anterior temporal spikes
Contralateral anterior temporal spikes
Ipsilateral parietal spikes
Contralateral parietal spikes
Bisynchronous spikes
Ambiguous seizure origin
Seizure ipsilateral occipital
Seizure contralateral occipital
Any ipsilateral anterior temporal abnormality
Any contralateral temporal abnormality
Lateral
Mesial
11
6
6
1
6
1
6
0
2
1
7
0
3
2
5
0
3
1
20
9
7
4
8
3
11
2
8
4
6
1
8
10
3
0
9
4
(55)
(55)
(9)
(55)
(9)
(55)
(0)
(18)
(9)
(64)
(0)
(27)
(18)
(45)
(0)
(27)
(9)
(45)
(35)
(20)
(40)
(15)
(55)
(10)
(40)
(20)
(30)
(5)
(40)
(50)
(15)
(0)
(45)
(20)
*Percentages given in parentheses. The incidence of none of these
features differs significantly between mesial and lateral occipital
epileptogenesis.
than contralateral (Table 7). Anterior temporal spikes
appeared contralateral to occipital epileptogenesis in 11 out of
41 patients (27%) but in fewer patients than ipsilateral ones.
Surgical follow-up
As the focus of this study was not surgical effectiveness, its
follow-up was only assessed retrospectively from material
available on hospital charts. Of the 32 patients for whom
adequate (>2 years) follow-up was obtained, seven (22%)
were seizure-free on one or more antiepileptic medications,
14 (44%) were improved and 11 (34%) were not helped.
Effectiveness did not significantly vary among the epileptogenic areas.
Discussion
Although the array of visual, dyscognitive and motor attacks
matched those of other substantial series, the incidences of
these ictal phenomena differed somewhat, possibly reflecting
referral patterns or seizure definitions. Unformed visual
Downloaded from http://brain.oxfordjournals.org/ at Universitatea de Medicina si Farmacie ''Carol Davila on August 19, 2012
Number of patients
Visual aura
Visual unformed
Visual formed
Never visual
Autonomic
Abdominal cephalic
Unilateral somatosensory
Bilateral somatosensory
Dyscognitive
Never aura
Unilateral motor
Bilateral motor
Any motor
Versive contralateral
Versive ipsilateral
1213
1214
W. T. Blume et al.
Table 7 Lateralizing value of scalp EEG features (41 patients)
EEG feature
Occipital seizure
First five scalp EEG recordings
All pre-invasive recordings
Any
Any
Majority
IPSI
CONTRA
10
IPSI
4
(0.0010)
Occipital (01,02) spikes
19
15
14
1
(N.S.)
22
24
CONTRA
0
(N.S.)
7
(0.001)
0
IPSI
(0.0001)
(0.0001)
5
(N.S.)
20
(0.0001)
(0.0001)
12
CONTRA
3
(0.0001)
25
11
(0.0035)
17
1
(0.0001)
16
1
(0.0001)
3
2
(N.S.)
N.S. = not significant. Any/majority = feature appeared on any/majority of such recordings. IPSI/CONTRA = feature ipsilateral/
contralateral to epileptogenesis. Parentheses = two-sided P values IPSI versus CONTRA.
phenomena appeared in 31 out of 41 (76%) of our patients,
15 out of 25 (60%) of the Williamson et al. (1992) series and
26 out of 55 (47%) of the patients studied by Ludwig and
Ajmone Marsan (1975). Formed visual phenomena were
recorded in 19 (46%) of our patients compared with three
(12%) and eight (14%) of these other series, respectively.
Dyscognitive or temporal lobe-like attacks occurred in 32
(78%) of this seriesmore than the 44% of the Williamson
series and 29% of the study by Ludwig and Ajmone Marsan.
Various types of motor seizures occurred in 91% of the Ludwig and Ajmone Marsan series and 37 (90%) of our series,
but only 12% of the Williamson series.
Physiological and anatomical factors may be invoked to
explain the inability of ictal semiological and scalp EEG
features to distinguish lateral from mesial occipital epilepsy.
We first describe properties facilitating mesial occipital to
lateral occipitaltemporal propagation, then components
mediating lateral to mesial occipital spread.
Studying penicillin-induced seizures with [14C]deoxyglucose autoradiography in the rat occipital cortex, Collins and
Caston (1979) found that relatively mild (1525 units) mesial
foci spread readily to the lateral occipital region and vice
versa. Stronger foci (80 units) involved most of the occipital
lobe ipsilateral to injection and contralaterally; seizure activity spread extensively to adjacent neocortex and limbic structures. Cain (1982) readily produced kindling of deep layers of
rat occipital cortex, but rarely when stimulating superficial
layers. Using microinjections of penicillin into each of the
several layers of visual cortex, Ebersole and Chatt (1986) also
found layer 4 to be the most epileptogenic. Layer 4 apparently
serves as a pacemaker for epileptogenesis in other visual
cortical areas particularly to layers 3, then 2. The pyramidal
neurons of layers 2 and 3 have abundant axonal connections
to other cortical areas both ipsilaterally and contralaterally.
Abundant multisynaptic projections from the occipital cortex to lateral and mesial temporal structures exist (Jones and
Powell, 1970; Turner et al., 1980). Thus, occipital-originating
seizures may readily spread to the ipsilateral and even the
contralateral temporal lobe as disclosed by both intracranial
(Olivier et al., 1982; Salanova et al., 1992; Williamson et al.,
1992; Palmini et al., 1993; Fava and Blume, 2002) and scalp
EEG (Ludwig and Ajmone Marsan, 1975). Penfield and Perot
(1963) elicited experiential (structured) visual phenomena by
electrical stimulation of various temporal neocortical sites as
did Gloor et al. (1982) by amygdala electrical stimulation.
These anatomical and physiological relationships indicate
that experiential visual and dyscognitive ictal phenomena
could represent seizures arising at any point along this
striate cortexamygdala axis and thus fail, as in this series,
to distinguish a lateral occipital from a mesial occipital
seizure origin. Visual experiential phenomenaseizurerelated or spontaneously occurringmay require participation of both neocortical and limbic structures (Blume et al.,
1993b).
Although processing of unformed (unstructured) visual
phenomena occurs in primary visual cortex (V1 or BA 17)
(Hubel and Wiesel, 1959, 1962), such simple visual phenomena have been evoked by stimulation of both primary visual
(striate) and extra-striate and prestriate (BA 18 and 19)
cortices by Penfield (1954). Although the occipital to temporal neocortex pathway was recognized earlier (see above),
reciprocal connections have more recently been demonstrated
between temporal neocortex and the primary visual cortex
(Felleman and Van Essen, 1991; Kastner and Ungerleider,
2000; Albright and Stoner, 2002).
Epileptogenic properties of primary visual cortex (see
above) apparently invite propagation of epileptic discharge
from other parts of the occipital cortex. Jasper (1969)
indicated that an area of propagation would sustain an epileptic discharge if inhibition were relatively weak, as in layer
4 of visual cortex (Ebersole and Chatt, 1986), or if it received
sufficient excitatory drive. Enhanced synaptic efficiency
with high frequency action potentials of epileptic discharges
(Lisman, 1997) would promote the latter. Similarly, Chervin
et al. (1988), studying epileptic propagation in bicucullinetreated neocortical slices, indicated that relative efficacy of
horizontal excitatory projections influenced the direction of
propagation. Such effects would augment the tendency of a
lateral occipital originating seizure to propagate backward
to the primary visual cortex and contribute further to the
Downloaded from http://brain.oxfordjournals.org/ at Universitatea de Medicina si Farmacie ''Carol Davila on August 19, 2012
22
IPSI
(N.S.)
(0.0004)
Posterior temporal
(T5,T6) spikes
Anterior temporal spikes
(M1,2; F7,8;T3,4)
CONTRA
Majority
Occipital epilepsy: lateral versus mesial
Acknowledgements
Cortical resective surgery was performed by Dr. John Girvin
and Dr. Andrew Parrent. Mrs Maria Raffa carefully typed the
manuscript and helped to create the Appendix.
References
Albright TD, Stoner GR. Contextual influences on visual processing.
Annu Rev Neurosci 2002; 25: 33979.
Bien CG, Benninger FO, Urbach H, Schramm J, Kurthen M, Elger CE.
Localizing value of epileptic visual auras. Brain 2000; 123: 24453.
Blume WT, Wiebe S. Occipital lobe epilepsies. Adv Neurol 2000; 84: 17387.
Blume WT, Borghesi JL, Lemieux JF. Interictal indices of temporal seizure
origin. Ann Neurol 1993a; 34: 7039.
Blume WT, Girvin JP, Stenerson P. Temporal neocortical role in ictal experiential phenomena. Ann Neurol 1993b; 33: 1057.
Blume WT, Holloway G, Wiebe S. Temporal epileptogenesis: localising
value of scalp and subdural interictal and ictal data. Epilepsia 2001a;
42: 50814.
Blume WT, Luders HO, Mizrahi E, Tassinari C, van Emde BW, Engel J Jr.
Glossary of descriptive terminology for ictal semiology: report of the
ILAE task force on classification and terminology. Epilepsia 2001b; 42:
12128.
Brodal A. The optic system. In: Neurological Anatomy in Relation to Clinical
Medicine, Third Edition, Oxford,Oxford UniversityPress;1981. p. 578601.
Cain DP. Kindling in sensory systems: neocortex. Exp Neurol 1982; 76:
27683.
Chervin RD, Pierce PA, Connors BW. Periodicity and directionality in the
propagation of epileptiform discharges across neocortex. J Neurophysiol
1988; 60: 169513.
Collins RC, Caston TV. Functional anatomy of occipital lobe seizures: an
experimental study in rats. Neurology 1979; 29: 70516.
Desimone R, Ungerleider LG. Neural mechanisms of visual processing in
monkeys. In: Boller F, Grafman J, editors. Handbook of neuropsychology.
Vol. 2. Amsterdam: Elsevier; 1989. p. 26799.
Eadie MJ, Bladin PF. Jackson and afterwards. In: Eadie MJ, Bladin PF,
editors. A disease once sacred. A history of the medical understanding
of epilepsy. Eastleigh (Hampshire), UK: John Libbey; 2001. p. 139, 142.
Ebersole JS, Chatt AB. Spread and arrest of seizures: the importance of layer
4 in laminar interactions during neocortical epileptogenesis. In: DelgadoEscueta AV, Ward AA Jr, Woodbury DM, Porter RJ, editors. Advances in
neurology. New York: Raven Press; 1986. p. 51558.
Fava MA, Blume WT. Propagation patterns of occipital seizures recorded
subdurally [abstract]. Epilepsia 2002; 43 (Suppl 7); 53.
Felleman DJ, Van Essen DC. Distributed hierarchical processing in the primate cerebral cortex. Cereb Cortex 1991; 1: 147.
Forster O. Beitrage zur pathophysiologie der Sehbahn end der Sehsphare.
Psychol Neurol (Lpz) 1929; 39: 46385.
Gloor P. Visual association cortex. In: Gloor P, editor. The temporal lobe
and limbic system. New York: Oxford University Press; 1997. p. 163201.
Gloor P, Olivier A, Quesney LF, Andermann F, Horowitz S. The role of the
limbic system in experiential phenomena of temporal lobe epilepsy. Ann
Neurol 1982; 12: 12944.
Goodale MA, Milner AD. Separate visual pathways for perception and action.
Trends Neurosci 1992; 15: 205.
Haxby JV, Grady CL, Horwitz B, Ungerleider LG, Mishkin M, Carson RE,
et al. Dissociation of object and spatial visual processing pathways in
human extrastriate cortex. Proc Natl Acad Sci USA 1991; 88: 16215.
Hubel DH, Wiesel TN. Receptive fields of single neurones in the cats straite
cortex. J Physiol (Lond) 1959; 148: 57491.
Hubel DH, Wiesel TN. Receptive fields, binocular interaction and functional
architecture in the cats visual cortex. J Physiol (Lond) 1962; 160: 10654.
Hubel DH, Wiesel TN. Brain mechanisms of vision. Sci Am 1979; 241: 15062.
Inouye T. Die Sehstorungen bei Schussverletzungen der kortikalen Sehsphare
nach Beobachtungen an Versundeten der letzten Japanische Kriege.
W. Engelmann, 1909.
Jasper HH. Mechanisms of propagation: extracellular studies. In: Jasper HH,
Ward AA, Pope A, editors. Basic mechanisms of the epilepsies. Boston
(MA): Little Brown; 1969. p. 42140.
Jones EG, Powell TP. An anatomical study of converging sensory pathways
within the cerebral cortex of the monkey. Brain 1970; 93: 793820.
Kandel ER, Wurtz RH. Constructing the visual image. In: Kandel ER,
Schwartz JH, Jessell TM, editors. Principles of neural sciences. 4th ed.
New York: McGraw-Hill; 2000. p. 492506.
Kastner S, Ungerleider LG. Mechanisms of visual attention in the human
cortex. Annu Rev Neurosci 2000; 23: 31541.
Leavens ME. Occipital lobectomy. In: Rengachary SS, Wilkins RH, editors.
Neurosurgical operative atlas. Vol. 1. Chicago: American Association of
Neurological Surgeons; 1991. p. 11521.
Lisman JE. Bursts as a unit of neural information: making unreliable synapses
reliable. Trends Neurosci 1997; 20: 3843.
Ludwig B, Ajmone Marsan C. Clinical ictal patterns in epileptic patients with
occipital electroencephalographic foci. Neurology 1975; 25: 46371.
Olivier A, Gloor P, Andermann F, Ives J. Occipitotemporal epilepsy studied
with stereotaxically implanted depth electrodes and successfully treated by
temporal resection. Ann Neurol 1982; 11: 42832.
Palmini A, Andermann F, Dubeau F, Gloor P, Olivier A, Quesney LF, et al.
Occipitotemporal epilepsies: evaluation of selected patients requiring depth
electrodes studies and rationale for surgical approaches. Epilepsia 1993;
34: 8496.
Penfield W. Visual sensation. In: Penfield W, Jasper H, editors. Epilepsy and
the functional anatomy of the human brain. Boston (MA) Little, Brown and
Company; 1954. p. 11626.
Penfield W, Rasmussen T. The cerebral cortex of man: a clinical study of
localization of function. New York: McMillan, 1950.
Penfield W, Perot P. The brains record of auditory and visual experience. A
final summary and discussion. Brain 1963; 86: 595696.
Salanova V, Andermann F, Olivier A, Rasmussen T, Quesney LF. Occipital
lobe epilepsy: electroclinical manifestations, electrocorticography, cortical
stimulation and outcome in 42 patients treated between 1930 and 1991.
Surgery of occipital lobe epilepsy. Brain 1992; 115: 165580.
Salanova V, Andermann F, Rasmussen TB. Occipital lobe epilepsy. In:
Wyllie E, editor. The treatment of epilepsy, principles and practice. Philadelphia: Lea & Febiger; 1993. p. 53340.
Truex RC, Carpenter MB. In: Truex RC, Carpenter MB. Gross consideration
of the central nervous system. In: Human neuroanatomy. 6th ed. Baltimore
(MD): Williams & Wilkins; 1969. p. 2658.
Turner BH, Mishkin M, Knapp M. Organization of the amygdalopetal projections from modality-specific cortical association areas in the monkey.
J. Comp Neurol 1980; 191: 51543.
Walczak TS. Neocortical temporal lobe epilepsy: characterizing the
syndrome. Epilepsia 1995; 36: 6335.
Williamson PD. Frontal lobe seizures. Problems of diagnosis and classification. In: Chauvel P, Delgado-Escueta AV, Halgren E, Bancaud J, editors.
Advances in neurology. Vol. 57. New York: Raven Press; 1992. p. 289309.
Downloaded from http://brain.oxfordjournals.org/ at Universitatea de Medicina si Farmacie ''Carol Davila on August 19, 2012
similarity of occipital epileptic semiology between lateral and
mesial occipital origins. That Bien et al. (2000) reported
visual aura from extra-occipital as well as occipital sources
may also reflect these propagation mechanisms.
This facilitated intra-occipital ictal propagation may underlie the similar motor semiology of lateral and mesial occipital
epileptogenesis: equal access to supra-Sylvian or to brainstem
motor regions may be available for lateral or mesial originating attacks.
Although no aspect of scalp EEG distinguished mesial from
lateral occipital epileptogenesis (Table 6), interictal and ictal
epileptiform abnormalities correlated highly with ictal lateralization (Table 7). EEG provided similar lateralizing help in
temporal lobe epilepsy (Blume et al., 1993a, 2001a).
1215
1216
W. T. Blume et al.
Williamson PD, Thadani VM, Darcey TM, Spencer DD, Spencer SS,
Mattson RH. Occipital lobe epilepsy: clinical characteristics, seizure
spread patterns, and results of surgery. Ann Neurol 1992; 31: 313.
Zeki SM. The functional organization of projections from striate to prestriate
visual cortex in the rhesus monkey. Cold Spring Harb Symp Quant Biol
1976; 40: 591600.
Appendix
Patient
Ictal Semeiology
LATERAL
01
A A-G
Multicoloured flashing lights right upper quadrant. Right arm
numbness and jerking. Impaired awareness and dysphasia.
GTC.
02
AK
Visual blurring or dimming diffusely. Bright lights in all fields
or objects very bright. Horizontal black and white stripes in
centre of visual field. Diffuse numbness, loss of awareness.
GTC.
03
DC
Objects frozen in position like looking through a window,
diffuse; head leftward and GTC. Diffuse numbness. Staring.
04
DS
No visual aura. Cephalic sensation; stares, right or both eyelids
twitch, hyperventilates, clonic rightward conjugate eye
deviation, talks nonsense with normal words; face flushed.
05
JC
Bilateral blurred vision beginning at periphery of fields and
moving towards centre; flickering lights at centre of field;
stares, looks around, confused or may fall atonically.
Left limb or bilateral numbness and jerking.
Epileptogenic Area(s)
Downloaded from http://brain.oxfordjournals.org/ at Universitatea de Medicina si Farmacie ''Carol Davila on August 19, 2012
Patient No.
Occipital epilepsy: lateral versus mesial
1217
Appendix Continued
Patient
Ictal Semeiology
06
NL
Diffuse black vision and staring with diffuse tremor; epigastric
sensations; automatisms of right hand; head rightward or right
limbs tonic; GTC.
07
PMc
Difficulty focusing and concentrating; right manual
automatisms; walks about. Tonic seizure, right limbs; GTC.
08
RH
Right upper quadrant flashing lights; bilateral retroorbital
headache with face flushed. Right homonymous hemianopia
and GTC.
09
TC
Sudden complete bilateral visual loss (90% of seizures), or
complete bilateral blurring, or objects enlarge and contract;
(10%) stares, looks around, fear; (rare) tonic left face, arm in
flexion, rarely both legs or GTC.
10
WA
Pulsating light in right upper quadrant with scotoma;
difficulty understanding what he is seeing; dysphasia;
(rarely) GTC.
Epileptogenic Area(s)
Downloaded from http://brain.oxfordjournals.org/ at Universitatea de Medicina si Farmacie ''Carol Davila on August 19, 2012
Patient No.
1218
W. T. Blume et al.
Appendix Continued
Patient
Ictal Semeiology
11
WV
Vision diffusely black; restless, flexes left leg; left hand
automatisms. Dots, left visual field, vision spinning;
right hand automatisms, left arm tonically flexed; right
tonic-clonic, face flushed. Sees circles, limbs stiff.
MESIAL
12
CB
White circles, coloured circles, lights, all right upper visual
field; rightward head deviation. Epigastric sensation, fear, right
hemifield images slanted, head leftward. Loss of awareness,
oroalimentary automatisms, bimanual automatisms; arms
flexed. GTC (rare). Diffuse sensation (rare).
13
DC
Flashing white lights, right upper visual field; lights spread to
centre; split in two phenomena which revolve about each other.
Darkening of vision; mumbling, left hand automatisms. Head
leftward, diffuse rigidity in flexion. Undescribable diffuse
sensation; GTC. GTC without warning.
14
DL
Whirling, shimmering visual phenomenon left upper quadrant;
spatial disorientation. Sees school scene or self brushing teeth or
smurfs in different episodes.
Epileptogenic Area(s)
Downloaded from http://brain.oxfordjournals.org/ at Universitatea de Medicina si Farmacie ''Carol Davila on August 19, 2012
Patient No.
Occipital epilepsy: lateral versus mesial
1219
Appendix Continued
Patient
Ictal Semeiology
15
DMac
Nausea; confused, talks nonsense; oroalimentary automatisms.
GTC.
16
DR
Unpleasant fearful diffuse sensation; moans, oroalimentary
automatisms, left or right hand automatisms. Flashing lights
then darkness left visual field. Right hemiclonic; GTC.
17
GS-J
Flashing white lights in peripheral portion of right field;
rightward ocular and cephalic deviation; GTC.
18
HW
Coloured monsters. Cephalic sensation; merging of coloured
objects; a desk appears; micropsia, macropsia; complete
loss of vision.
19
JB
No visual aura; sick sensation; left arm automatisms; eyes
closed, neck flexed; bilateral tonic, left leg jerking.
Epileptogenic Area(s)
Downloaded from http://brain.oxfordjournals.org/ at Universitatea de Medicina si Farmacie ''Carol Davila on August 19, 2012
Patient No.
1220
W. T. Blume et al.
Appendix Continued
Patient
Ictal Semeiology
20
JF
Visual blurring diffusely; head leftward, arms tonic, eyes
upwards. Designs or word-like figures in a French-like
script. Diffuse blackening of vision; sounds distant; all limbs
stiffen, leftward ocular and cephalic deviation; bimanual
automatisms.
21
JL
White or coloured flashing lights, right upper visual field
proximally; eyes left. GTC.
22
JS
Bilateral black and white spots peripherally moving to centre;
loss of awareness, blinking, eyes left; myoclonic movements
of arms, left leg. Fear, sensation of someone sneaking up
behind her.
23
JW
Walls converging; stares, gaze leftward, confused;
oroalimentary automatisms. GTC.
24
KH
Confused, automatisms. Diffuse loss of vision; fearful
abdominal sensation; oroalimentary and bimanual automatisms;
left arm numb and tonic, eyes left.
Epileptogenic Area(s)
Downloaded from http://brain.oxfordjournals.org/ at Universitatea de Medicina si Farmacie ''Carol Davila on August 19, 2012
Patient No.
Occipital epilepsy: lateral versus mesial
1221
Appendix Continued
Patient
Ictal Semeiology
25
LS
Intermixed colours especially blue and purple like a blob of oil
on water in right lower quadrant; sour taste, abdominal
sensation; impaired awareness, dysphasia; right sided motor;
GTC. Cephalic sensation, vision darkened. Pencil outline of a
face and threatening voices. Father standing in right lower
quadrant.
26
MD
Flashing lights right visual field. Old cars and old fashion
objects. Stares, fear without visual aura; abdominal sensation,
oroalimentary automatisms; eyes right; blinks. GTC.
27
MH
No visual aura. Stares, bimanual automatisms. Atonic drop
attacks.
28
ML
Ictus emeticus. Stares; bimanual and oroalimentary
automatisms.
29
NK
Sees colours in all fields or left field. Abdominal sensation;
bimanual automatisms; atonic fall. GTC.
Epileptogenic Area(s)
Downloaded from http://brain.oxfordjournals.org/ at Universitatea de Medicina si Farmacie ''Carol Davila on August 19, 2012
Patient No.
1222
W. T. Blume et al.
Appendix Continued
Patient
Ictal Semeiology
30
SS
Rightward head and eye deviation. Peripheral blurred and
distorted vision bilaterally and changing colours in centre.
Colour alteration and darkening diffusely. Diffuse tingling, left
arm numbness and left shoulder clonus. CPS. GTC.
31
TE
Macropsia, jamais vu. Anxiety, disoriented, bimanual
automatisms, oroalimentary automatisms, mute.
BOTH
32
CC
Blurred vision diffusely; epigastric sensation; eyes fluttering.
GTC.
33
EMc
Flickering colours right field and diffusely. Stares, automatisms.
Head and eyes right; GTC.
Epileptogenic Area(s)
Downloaded from http://brain.oxfordjournals.org/ at Universitatea de Medicina si Farmacie ''Carol Davila on August 19, 2012
Patient No.
Occipital epilepsy: lateral versus mesial
1223
Appendix Continued
Patient
Ictal Semeiology
34
JMc
Light flashes right upper quadrant. Familiar scene right
centrally. Anxiety, fear, staring, oroalimentary automatisms.
GTC.
35
KMac
Blurring and flickering in right field proximally; right clonic
ocular deviation. Loss of awareness, automatisms.
36
LG
GTC. Loss of vision diffusely, atonic falls. Vertiginous visual
sensation, feels hot or cold.
Epileptogenic Area(s)
Downloaded from http://brain.oxfordjournals.org/ at Universitatea de Medicina si Farmacie ''Carol Davila on August 19, 2012
Patient No.
1224
W. T. Blume et al.
Appendix Continued
Patient
Ictal Semeiology
37
MA
Multicoloured stripes, left field or bilateral; blinks; diplopia,
floor slanted; loss of vision; nausea; unresponsive,
impaired awareness. GTC.
38
SE
Flashing yellow and red balls of lights, right lower field,
enlarging gradually, face flushed; GTC.
39
SF
Flashing lights, left field; white flashing circles in centre of field;
head, eyes, body leftward; abdominal sensation, loss of
awareness, oroalimentary automatisms.
Epileptogenic Area(s)
Downloaded from http://brain.oxfordjournals.org/ at Universitatea de Medicina si Farmacie ''Carol Davila on August 19, 2012
Patient No.
Occipital epilepsy: lateral versus mesial
1225
Appendix Continued
Patient
Ictal Semeiology
40
ST
Blurred vision bilaterally or left field; head, eyes left;
oroalimentary automatisms, unresponsive; GTC.
41
YD
Flashing lights left upper field; GTC. Yellow and white dots
diffusely. Vision tunnel-like. Visual scenes of past life.
Distortion or blurring in left field and diffusely. Abdominal
sensation, vacant sensation. Left sided numbness.
Epileptogenic Area(s)
Semiology: Commas (,) separate simultaneous components. Semicolons (;) distinguish sequential features. Full stop (.) separate
complete seizures. GTC = generalized tonic-clonic; Epileptogenic areas: Based on subdurally recorded clinically typical seizures; except for
Patient No. 3 where area combines recorded seizures and a lesion; and Patients 8, 10, 14, 20, 35, and 38 which describe epileptogenic
lesions only.
Downloaded from http://brain.oxfordjournals.org/ at Universitatea de Medicina si Farmacie ''Carol Davila on August 19, 2012
Patient No.
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Abnormal VermisДокумент1 страницаAbnormal VermiscalmlandОценок пока нет
- Major Categories of Mimics of VasculitisДокумент1 страницаMajor Categories of Mimics of VasculitisDrHellenОценок пока нет
- Combining Antiplatelet and Anticoagulant Therapy in Cardiovascular Disease - 2020 - AHAДокумент7 страницCombining Antiplatelet and Anticoagulant Therapy in Cardiovascular Disease - 2020 - AHADrHellenОценок пока нет
- Non-Vitamin K Antagonist Oral Anticoagulants in Patients with β-Thalassemia 2023Документ8 страницNon-Vitamin K Antagonist Oral Anticoagulants in Patients with β-Thalassemia 2023DrHellenОценок пока нет
- Brain Tumours (Primary) - NICE Guide 2021Документ69 страницBrain Tumours (Primary) - NICE Guide 2021DrHellenОценок пока нет
- Management of Psychosis in PDДокумент2 страницыManagement of Psychosis in PDDrHellenОценок пока нет
- An Update On Best Practice of Deep Brain Stimulation in Parkinson's DiseaseДокумент20 страницAn Update On Best Practice of Deep Brain Stimulation in Parkinson's DiseaseDrHellenОценок пока нет
- Handwritten Pattern Recognition For Early Parkinson's Disease Diagnosis - Bernardo2019Документ7 страницHandwritten Pattern Recognition For Early Parkinson's Disease Diagnosis - Bernardo2019DrHellenОценок пока нет
- Boala Binswanger PDFДокумент12 страницBoala Binswanger PDFDrHellenОценок пока нет
- Preventive Strategies For Cognitive Decline and DementiaДокумент13 страницPreventive Strategies For Cognitive Decline and DementiaDrHellenОценок пока нет
- Dementia Prevention, Intervention, and Care - 2020 Report of The Lancet CommissionДокумент35 страницDementia Prevention, Intervention, and Care - 2020 Report of The Lancet CommissionDrHellenОценок пока нет
- 24-06-2020 HMB EnglishДокумент20 страниц24-06-2020 HMB EnglishRakshith GowdaОценок пока нет
- Agricultural Performance Survey of 2021 Wet Season in NigeriaДокумент361 страницаAgricultural Performance Survey of 2021 Wet Season in NigeriaEnemona ShellengОценок пока нет
- Mod 6 Soft Tissue InjuriesДокумент5 страницMod 6 Soft Tissue Injuriesrez1987100% (1)
- Vitamins and Minerals: Nutrient (Vitamins) Needed For Key SourcesДокумент4 страницыVitamins and Minerals: Nutrient (Vitamins) Needed For Key SourcesKevin Carl A. CorpuzОценок пока нет
- Moving The TeethДокумент117 страницMoving The TeethThirunavukkarasu Srinivasan100% (2)
- Week9&10 LEC Clinical Parasitology NEMATODESДокумент18 страницWeek9&10 LEC Clinical Parasitology NEMATODESSamuel ReyesОценок пока нет
- Assessment of The Ear, Nose and ThroatДокумент40 страницAssessment of The Ear, Nose and Throatsnickers_j100% (3)
- Arachnoid Cyst: From Wikipedia, The Free EncyclopediaДокумент11 страницArachnoid Cyst: From Wikipedia, The Free EncyclopediaOsama Bin RizwanОценок пока нет
- KumeДокумент28 страницKumeGrace Clemenia-GrefaldiaОценок пока нет
- Neck Lump HistoryДокумент4 страницыNeck Lump HistoryAlmomnbllah Ahmed100% (1)
- Rabies - WikipediaДокумент22 страницыRabies - WikipediaBruno BusnelloОценок пока нет
- CABERGOLINE Safety2Документ6 страницCABERGOLINE Safety2Kane SmithОценок пока нет
- The Cool Night Breeze Whistled SoftlyДокумент1 страницаThe Cool Night Breeze Whistled SoftlysiddiqpatelОценок пока нет
- Natural Remedies For FibroidsДокумент2 страницыNatural Remedies For Fibroidsafm2026Оценок пока нет
- Wednesday - Session A01 - Arello - Basic Suturing Skills and TechniquesДокумент30 страницWednesday - Session A01 - Arello - Basic Suturing Skills and TechniquesSuresh Thapa ChhetriОценок пока нет
- Risk Management Prelim ReviewerДокумент3 страницыRisk Management Prelim ReviewerCharmaigne BañaresОценок пока нет
- Research Life ScienceДокумент21 страницаResearch Life ScienceKeyth Abegail RendonОценок пока нет
- Chapter 6. The Circulatory System: Short QuestionsДокумент31 страницаChapter 6. The Circulatory System: Short QuestionsParardha DharОценок пока нет
- Function Human HeartДокумент13 страницFunction Human Heartshyam_inkОценок пока нет
- History of NeuroscienceДокумент17 страницHistory of NeurosciencerazorviperОценок пока нет
- 3 Minute German Die KörperteileДокумент11 страниц3 Minute German Die KörperteileBahar TukanovaОценок пока нет
- Top Homeopathic Remedies For ColdsДокумент2 страницыTop Homeopathic Remedies For ColdsAkash kumarОценок пока нет
- Ielts 5.0 l1 R DoneДокумент14 страницIelts 5.0 l1 R DoneMai TrangОценок пока нет
- Anatomy and Physiology of Oral CavityДокумент15 страницAnatomy and Physiology of Oral Cavity28 manan patelОценок пока нет
- Beginner's Guide To Getting Started With DiscusДокумент18 страницBeginner's Guide To Getting Started With DiscusGary HoustonОценок пока нет
- The HelpДокумент7 страницThe HelpRajipah OsmanОценок пока нет
- Allergy Diagnostic TestingДокумент149 страницAllergy Diagnostic TestingArrow Ou100% (1)
- What Is The Effect of Swallowing Without Chewing Properly? What Happen With The Chewing Gum?Документ15 страницWhat Is The Effect of Swallowing Without Chewing Properly? What Happen With The Chewing Gum?Jorge Enrique Olaya LiévanoОценок пока нет
- CALDOBДокумент2 страницыCALDOBSatyendra Pandey50% (2)