Академический Документы
Профессиональный Документы
Культура Документы
Liquido Cefaloraquídeo
Загружено:
xfaborОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Liquido Cefaloraquídeo
Загружено:
xfaborАвторское право:
Доступные форматы
Ovid: Infections of the Central Nervous System
1 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
Authors: Scheld, W. Michael; Whitley, Richard J.; Marra, Christina M.
Title: Infections of the Central Nervous System, 3rd Edition
Copyright 2004 Lippincott Williams & Wilkins
> Table of Contents > Part I: - Approach to the Patient and Diagnostic Evaluation > 2 - Cerebrospinal Fluid in Central Nervous System Infections >
CSF ANALYSIS IN CNS INFECTIONS
2
Cerebrospinal Fluid in Central Nervous System Infections
John E. Greenlee
Karen C. Carroll
Infections within the central nervous system (CNS) frequently, though not invariably, produce changes in ventricular or
lumbar cerebrospinal fluid (CSF). The changes produced may provide invaluable information about the nature of the
infectious process and, in many cases, may permit specific identification of the offending organism. Despite the great
diagnostic value of CSF analysis, however, injudicious attempts to obtain CSF (as in the setting of brain abscess) may cause
severe injury or death, and casual handling of the CSF obtained may render the CSF analysis useless.
This chapter is divided into three parts. The first part reviews the anatomy of the CSF spaces, the physiology of CSF
production and reabsorption, and the effect of infection on CSF physiology and composition. The second part discusses
methods of CSF analysis in CNS infections, and the third part summarizes the CSF analysis in specific CNS infections.
ANATOMY OF THE CSF COMPARTMENT
The CSF is contained within two connecting compartments, the cerebral ventricles and the subarachnoid space (1). Both
compartments may be affected by infectious organisms, and analysis of CSF from both may reflect changes produced by
infectious or parainfectious processes within meninges, brain, or spinal cord. Total CSF volume, as determined by postmortem
studies, in healthy human adults, is roughly 140 mL, of which approximately 22 mL (range, 7 to 56 mL) is contained within the
ventricles and 30 mL within the spinal subarachnoid space (1).
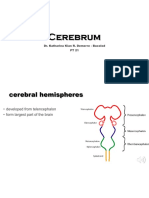
The Ventricular System
The cerebral ventricular system represents, in greatly elaborated form, the remnants of the embryologic neural tube. The
ventricles are lined by a single layer of neuroglial-derived cells, the ventricular ependyma; these are backed by a dense
network of astrocytic foot processes. The ventricular system consists of two lateral ventricles, the third ventricle, and the
fourth ventricle (Fig. 2.1). The lateral ventricles are located within the cerebrum and consist of frontal, temporal, and
occipital horns; these join at the ventricular trigone within the parietal lobe. The third ventricle is an elongated, slitlike
cavity that lies within the midbrain and is bounded inferiorly by the hypothalamus. The fourth ventricle overlies the
brainstem from the level of the midpons to the extreme rostral end of the spinal cord. The roof of the fourth ventricle is the
cerebellum posteriorly and the superior and inferior medullary veli anteriorly. The fourth ventricle is roughly diamond shaped
and is widest at the lateral recesses, which lie between the superior and middle cerebral peduncles.
The cerebral ventricles are connected to each other and with the subarachnoid space through a series of small openings. Each
lateral ventricle drains into the third ventricle through the foramen of Monro, located in the inferomedial wall of the frontal
horn. The third and fourth ventricles are connected by the aqueduct of Sylvius, which extends through the midbrain. The
fourth ventricle drains into the subarachnoid space through three small openings, the foramina of Luschka and the foramen of
Magendie. The foramina of Luschka are located in the lateral recesses of the fourth ventricle and are absent in up to 20% of
the population. The foramen of Magendie is located in the midline and, in most persons, represents the major communication
between the fourth ventricle and the subarachnoid space. As is discussed later, these narrow openings are important in CNS
infections because they represent the sites at which obstruction of CSF flow may most easily occur.
The Meninges and Subarachnoid Space
The brain and spinal cord are surrounded by three layers of meninges (2). The outermost layer of the meninges is a tough
fibrous membrane, the dura mater. Within the skull, the dura forms the inner layer of the cranial periosteum and is tightly
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
2 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
adherent to bone. Below the foramen magnum, the dura and periosteum diverge and are separated by a fat-filled epidural
space. The middle layer of meninges, the arachnoid, is joined to the dura by a specialized layer of fibroblasts, the dural
border cell layer. The cells of this inner dural border are devoid of collagen and have few cellular junctions, providing a
cleavage plane in which infection may develop and rapidly spread. The arachnoid covers the brain and spinal cord loosely and
extends outward along the course of cranial and spinal nerves.
The third layer of meninges, the pia mater, is continuous with the surface of the brain and spinal cord. The pia mater also
follows vessels into brain and spinal cord parenchyma and projects into the ventricles to form the choroid plexuses. The pia
P.6
mater and the ventricular ependyma merge at the foramina of Luschka and Magendie. The CSF is contained in the
subarachnoid space, enclosed between the arachnoid and the pia. The subarachnoid space surrounds the brain and extends
within the spinal canal to the level of the second sacral vertebra. Within the skull, the subarachnoid space widens into
cisterns where pia and arachnoid are more widely separated by irregularities in the contour of the brain. The largest of these,
the cisterna magna, surrounds the brainstem and the cerebellum at the base of the skull and is occasionally used as a source
of CSF for analysis and culture. The subarachnoid space is crossed by trabecular extensions of the arachnoid itself, by cranial
nerves, by a network of small arteries, the rete mirabile, and by numerous bridging veins, which connect the meningeal veins
with the deeper intracranial venous system (2).
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
3 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
FIG. 2.1. The cerebral ventricles. Inset: Shown are the structure of the fourth ventricle and the locations of the
foramina of Luschka and Magendie. (From Greenlee JE. Anatomical considerations in central nervous system infections.
In: Mandell GL, Bennett JE, Dolin R, eds. Principles and practice of infectious diseases, 4th ed. New York: Churchill
Livingstone, 1994:821-831, with permission.)
The subarachnoid space is normally a closed system. Occasionally, however, congenital or posttraumatic communications may
exist between the subarachnoid space and superficial tissues and may provide a route for single or recurrent episodes of
meningitis. Congenital defects arise from incomplete closure of the neural tube. These defects may extend for variable
distances into subcutaneous tissues or to the cutaneous surface and are most common in the upper cervical regions and over
the sacrum. Their presence may be suggested by a cutaneous dimple or a patch of hair. Traumatic communications into the
subarachnoid space are most often associated with basilar skull fractures. The most common sites of involvement are (a) the
thin layers of bone that separate the cranial cavity from the paranasal sinuses and (b) the petrous bone, which separates the
auditory canals and mastoid from the cranial cavity. In rare instances, traumatic defects may occur over the cranial
convexities or along the spinal column.
PHYSIOLOGY OF CSF PRODUCTION AND REABSORPTION
CSF is produced by the choroid plexuses of the lateral, third, and fourth ventricles and, to a lesser extent, by extrachoroidal
sites (1,3). The choroid plexuses are specialized projections of vessels and pia mater into the ventricular cavities. Each
choroid plexus branches into frondlike villi, each of which contains a capillary surrounded by loose connective tissue and a
layer of specialized ependymal cells termed choroidal epithelium. Choroidal epithelial cells, in contrast to ependymal cells
elsewhere in the ventricular system, are columnar in shape and are covered on their ventricular surfaces by a brush border of
microvilli. The villous structure of the choroid plexus and the presence of
P.7
microvilli greatly increase the surface area available for secretion of CSF (1). In the healthy adult, CSF production occurs at a
high rate, approximately 20 mL per hour.
Formation of CSF involves both filtration and active transport (1,3). Filtration of CSF varies inversely with serum osmolality. In
experimental animals, and possibly in humans, CSF production changes 7% for each 1% change in serum osmolality (4). Active
+
secretion of CSF involves Na ,K -adenosine triphosphatase (ATPase)-mediated transport of sodium across choroidal epithelium
into the ventricular lumen, with water, chloride, and bicarbonate ions following through facilitated transport. The carbonic
anhydrase inhibitor acetazolamide reduces CSF secretion by approximately 50%, whereas furosemide and ethacrynic acid, in
experimental animals, reduce CSF production by 25% to 35% (5). Simultaneous use of both agents reduces CSF formation by
75%.
Reabsorption of CSF occurs through arachnoid villi. Most of these are located along the superior sagittal sinus. Smaller
numbers of arachnoid villi are found along other intracranial venous sinuses and around spinal nerve roots (1). During health,
the arachnoid villi along the superior sagittal sinus provide the major site of CSF uptake. The arachnoid villi along other
sinuses and surrounding spinal nerve roots are thought to provide alternative sites of CSF absorption following superior
sagittal sinus thrombosis.
Each arachnoid villus represents an extension of the arachnoid membrane through the dura mater into the lumen of the
venous sinus and functions as a one-way valve, permitting unidirectional flow from CSF into blood. Early work by Welch (6)
demonstrated that the arachnoid villi have a critical in vitro opening pressure of 2 to 5 cm H O; this study also demonstrated
2
that particles up to the size of erythrocytes readily pass from CSF into blood, whereas particles larger than 7.5 m are
excluded. Although these early data suggested that the arachnoid villi might provide a direct communication between CSF
and blood, studies using electron microscopy have demonstrated that arachnoid villi and venous sinuses are separated by a
layer of endothelial cells connected by tight junctions, and that movement of CSF and particulate matter across the
arachnoid villi occurs by transport within giant vesicles (7,8) (Fig. 2.2). These giant vesicles, although they provide efficient
transfer of CSF into blood under normal circumstances, can become obstructed by bacteria and inflammatory cells during
meningitis or by red blood cells (RBCs) during subarachnoid hemorrhage (9,10).
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
4 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
FIG. 2.2. Uptake of CSF by an arachnoid villus. (From Fishman RA. Cerebrospinal fluid in diseases of the nervous
system, 2nd ed. Philadelphia: WB Saunders, 1992, with permission.)
BRAIN AND CSF BARRIER SYSTEMS
The brain and CSF are contained within a series of barrier systems (1). These prevent entry of fluids, electrolytes, and other
substances from blood into CSF or brain by simple diffusion and isolate the CNS from systemic immune responses. The
blood-brain barrier (BBB) is formed by tight junctions between endothelial cells of CNS capillaries and is further reinforced by
a surrounding layer of astrocytes, whose processes terminate in overlapping fashion on the capillary walls. In contrast, the
endothelial cells of the choroid plexuses and arachnoid are separated by gap junctions, which allow diffusion of substances
across the vessel wall, so the blood-CSF barrier, unlike the BBB, is formed by tight junctions between cells of the arachnoid
membrane and similar tight junctions between the epithelial cells of the choroid plexus. The cells of the pia mater, like those
of choroid plexus and arachnoid capillaries, are separated by gap junctions; entry of substances from CSF into brain is
modulated by a basement membrane subjacent to the pia and by a continuous layer of astrocytes beneath the basement
membrane, forming a CSF-brain barrier.
The barrier systems that surround spinal cord and brain exclude from the CNS most of the immunologic mechanisms that
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
5 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
provide host defense elsewhere in the body. Normally, T cells and B cells are present in very small numbers in CSF and only
rarely in brain; immunoglobulins and complement are largely excluded from both CSF and brain; and opsonic activity of CSF,
even in the presence of meningitis, is far less than that of serum (11,12,13,14). CNS infections, thus, beginand progressin
tissue that is poorly equipped to halt their spread.
Work during the last two decades has demonstrated that the barrier systems that isolate CSF, brain, and spinal cord from
blood are not static systems but, instead, are highly dynamic in their ability to interact with and transport a wide variety of
substances (15). In addition, it is increasingly recognized that the endothelial cells and astrocytes of the BBB and the
blood-CSF barrier are important sources of cytokines (including tumor necrosis factor [TNF] and interleukins), and that
astrocytes, in addition to their abilities to regulate solute entry into brain, have the ability to act as antigen-presenting cells
(16). As discussed in Chapter 22, release of cytokines by
P.8
endothelial cells and astrocytes in response to bacterial endotoxins and other bacterial products is fundamental in the
production of inflammation and injury during CNS infections and provides an extremely important area for early therapy
(9,17,18,19).
MAINTENANCE OF CSF HOMEOSTASIS
The BBB and the blood-CSF barrier maintain the cellular and chemical elements of the CSF within narrow ranges (1,3,20).
Lipid-soluble substances within blood readily diffuse across choroidal epithelium or vascular endothelium into CSF or brain.
Passage of fluid and ionically polar substances, however, requires mechanisms for transport and facilitated diffusion. Sodium
+
enters CSF both by Na ,K -ATPase-mediated transport during secretion of CSF and by passive diffusion. Potassium is secreted
into CSF by active transport mechanisms and is actively removed from CSF into brain by transport mechanisms that are
believed to be located in astrocyte foot processes. Movement of calcium, magnesium, and phosphorus into CSF and brain also
occurs predominantly by active transport, and the concentrations of these substances are relatively independent of their
concentrations in serum. Chloride and bicarbonate, like potassium, are actively secreted into and actively removed from CSF.
Glucose, amino acids, amines, and thyroid hormone enter the brain by carrier-mediated transport mechanisms (1,15). Insulin
and transferrin require receptor-mediated transport. Although lipids complexed to proteins were once thought to be excluded
from the CNS, it is now known that complexed lipids undergo dissociation from their carrier proteins at the blood-brain
interface and may enter the CNS without significant exodus of protein from brain capillaries.
Chloride represents the major anion in CSF. Normal CSF chloride concentration is 15 to 20 mEq/L higher than that in serum.
Early workers observed that CSF chloride concentrations were lowered in tuberculous meningitis; for many years, levels of
CSF chloride were used to diagnose and follow the course of this infection (1). It is now recognized, however, that the
lowered CSF chloride concentration observed in tuberculous meningitis is nothing more than a reflection of lowered serum
chloride values and has no diagnostic or prognostic value.
The acid-base balance of the CSF, like its electrolyte concentration, tends to remain fairly constant despite fluctuations in
systemic acid-base balance. In CSF, as opposed to plasma, however, movement of CO occurs readily by diffusion, whereas
2
movement of bicarbonate occurs more slowly by carrier-mediated transport. The discrepancy in the rate of movement of
these two substances may produce delayed (and, at times, paradoxical) responses in CSF pH as compared to systemic pH
during rapid changes in bicarbonate concentration (1). The CSF acid-base balance is also maintained by the choroid plexuses,
which possess transport mechanisms capable of removing weak organic acidsincluding antibiotics such as the penicillins,
cephalosporins, and aminoglycosidesfrom CSF (21,22). Choroid plexus transport of antibiotics and other weak organic acids
can be blocked by probenecid.
ALTERATIONS OF CSF DYNAMICS AND PRESSURE IN CNS INFECTIONS:
HYDROCEPHALUS, INTRACRANIAL HYPERTENSION, AND BRAIN HERNIATION
Acute or chronic CNS infections may produce profound alterations in intracranial pressure (ICP) by obstructing CSF flow or
reabsorption, by behaving as space-occupying lesions, by altering CSF, or by producing hemorrhage or cerebral edema. These
pathologic consequences of infection, acting individually or together, may cause brain herniation and death.
Alteration of CSF Circulation in CNS Infections
Impairment of normal CSF circulation may result in ventricular enlargement and hydrocephalus. Interruption of CSF
reabsorption produces communicating hydrocephalus with normal circulation of CSF through the ventricular system and into
the subarachnoid space. Communicating hydrocephalus is a common complication of bacterial meningitis and, in most cases,
results from obstruction of the arachnoid villi by bacteria and white blood cells (WBCs) (9). Communicating hydrocephalus
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
6 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
may also result from functional occlusion of arachnoid villi during severe meningitis or by RBCs in the course of subarachnoid
hemorrhage during bland or septic subarachnoid hemorrhage (10). Thrombosis of the superior sagittal sinus may also block
CSF reabsorption and thereby produce communicating hydrocephalus. Occlusion of a large portion of the superior sagittal
sinus usually produces catastrophic, often hemorrhagic, cerebral infarction. Involvement of the anterior third of the sinus,
however, may be clinically silent except for the development of hydrocephalus.
Obstructive hydrocephalus results from interruption of CSF flow within the ventricular system or at its point of exit into the
subarachnoid space (2). This may be the consequence of infection of the ventricular ependyma or basilar meninges or may
result from extrinsic compression of the ventricular system by infection within brain parenchyma. Lesions producing
obstructive hydrocephalus most commonly involve the ventricular system at its narrowest points: the foramina of Luschka and
Magendie, the fourth ventricle, the aqueduct of Sylvius, and the foramina of Monro. Obstruction of the foramina of Luschka
and Magendie is characteristic of exudative basilar meningitides such as those caused by Mycobacterium tuberculosis,
Coccidioides immitis, and Cryptococcus neoformans but may also be seen in bacterial meningitis. Hydrocephalus as a result of
obliteration of the fourth ventricle is almost always extrinsic and is the result of ventricular compression by large cerebellar
mass lesions such as cerebellar abscess or hemorrhage. Occlusion of the aqueduct of Sylvius by granulomatous ependymitis
may occur as a complication of tuberculosis, fungal infections, or sarcoidosis. Mumps virus, which replicates in ventricular
ependymal cells, has been shown to produce congenital aqueductal stenosis in experimental animals (23). Rare cases of
acquired aqueductal stenosis have also been reported following mumps meningoencephalitis in humans (24). Extrinsic
compression of the aqueduct of Sylvius may be produced by abscesses or other localized infections
P.9
within the pons or midbrain. Involvement of the foramen of Monro is almost always unilateral and is the consequence of
severe brain shifts caused by abscess, focal encephalitis, or hemorrhage. Hydrocephalus caused by the occlusion of one
foramen of Monro is particularly dangerous because the CSF trapped within the involved lateral ventricle acts as a unilateral
space-occupying lesion, greatly increasing the risk of transtentorial brain herniation.
Computerized tomography (CT) and magnetic resonance imaging (MRI) are invaluable in demonstrating the presence of
hydrocephalus and in determining its cause. Ventricular dilationso-called hydrocephalus ex vacuois common in the elderly
and is characterized by symmetric ventricular dilation accompanied by evidence of cerebral cortical atrophy. In contrast,
hydrocephalus from impaired CSF circulation is accompanied by loss of cortical markings visible on CT or MRI as the brain is
forced outward against the skull and by periventricular areas of increased lucency, representing transependymal leakage of
CSF. Communicating hydrocephalus and hydrocephalus from obstruction of the foramina of Luschka and Magendie are
characterized by symmetric enlargement of all four ventricles. Hydrocephalus from occlusion of the fourth ventricle or
aqueduct of Sylvius results in loss of that structure on CT or MRI, with dilation of the third and lateral ventricles.
Hydrocephalus following compression of the foramen of Monro is almost invariably associated with an identifiable spaceoccupying lesion and a prominent midline shift. Thrombosis of the superior sagittal sinus may be difficult to detect as a cause
of communicating hydrocephalus. CT imaging, even with enhancement, does not reliably detect superior sagittal thrombosis.
For this reason, the diagnostic method of choice is MRI (25). The diagnostic value of MRI is based on the finding that protons
carried within flowing blood pass rapidly out of the plane of radiographic section, whereas protons within clotted blood do
not. Thus, blood moving within vessels produces a signal void, whereas clotted blood produces an increased signal on both T1and T2-weighted images. The sensitivity of conventional MRI can be enhanced by use of magnetic resonance venography (25).
Intracranial Hypertension and Brain Herniation
The normal mechanisms of CSF secretion and drainage maintain CSF pressure at a level less than 150 mm of CSF in most
patients (see later discussion). Infection, however, greatly alters these homeostatic mechanisms; moreover, death during the
acute stages of intracranial CNS infections often results from extreme elevation in ICP followed by brain herniation and
respiratory arrest.
For a period of time, the intracranial contents are able to compensate in response to space-occupying lesions before a rise in
ICP occurs. This compensatory ability is termed compliance (dV/dP) and represents the ratio of changes in volume (dV) to
changes in pressure (dP). Compliance in response to space-occupying intracranial lesions consists of several factors. These
include increased rate of reabsorption of CSF (this may be prevented in meningitis by obstruction of the arachnoid villi by
cells and exudate); displacement of CSF; reduction in the total volume of intracranial blood, predominantly by compression of
veins and venous sinuses; and plasticity of the brain itself. Compliance is extremely limited when infection is accompanied by
a rapid increase in ICP, such as during acute bacterial meningitis or subdural empyema. In contrast, the ability of CNS
compliance to compensate for increased ICP may be extensive where space-occupying lesions develop over time (26). Once
compliance is exceeded, however, the increase in pressure in chronic lesions may occur with a rapidity similar to that seen in
more acute processes. Compliance can be measured experimentally and clinically by determining the amount of artificial CSF
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
7 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
that must be instilled into the subarachnoid or ventricular spaces before an increase in pressure occurs (27). In healthy
individuals, instillation of large volumes of artificial CSF has little effect on ICP. Once intracranial compliance is exhausted,
administration of very small amounts of artificial CSF (1 mL or less) may cause a precipitous increase in ICP. Although
measurement of compliance may provide a more accurate assessment of patient status than measurement of ICP, the
technique is not routinely used.
The elevation in CSF pressure seen in infections and other pathologic conditions is not constant but fluctuates considerably.
This fluctuation is usually not observed during the brief period of measurement provided by lumbar puncture but becomes an
important parameter to observe during monitoring of ICP. Minor variation in pressure occurs during Cheyne-Stokes respiration
and during variations in blood pressure produced by Hering-Breuer reflexes. More major variations in ICP occur during plateau
waves. These are abrupt elevations in ICP (usually lasting 5 to 20 minutes) in which ICP may reach 600 to 1,300 mm of CSF (50
to 100 mm Hg) (28). Plateau waves are believed to represent a consequence of disturbed cerebrovascular autoregulation
because of either abnormal sympathetic tone or cyclic changes in perfusion in which mild hypotension is followed by cerebral
vasodilation and increased cerebral blood flow (28). Although plateau waves may be without any detectable clinical effect,
they may also be associated with signs of brainstem compression and impending herniation.
Increased pressure that exceeds intracranial compliance causes downward and backward shifting of the cerebrum and
brainstem (29). Minimal degrees of shift are well tolerated, but a more extensive shift may cause herniation of the cingulate
gyrus beneath the falx cerebri, herniation of the uncus of the temporal lobe over the tentorium cerebelli, and ultimately,
herniation of the lower brainstem and cerebellar tonsils into the foramen magnum. Herniation of the cingulate gyrus is usually
asymptomatic. Uncal herniation, however, initially produces compression of the third cranial nerve as it passes beneath the
tentorium; it subsequently causes compression of the midbrain, with resultant coma. The aqueduct of Sylvius is often
occluded during uncal herniation, and the resultant hydrocephalus increases the mass effect already present. Herniation of
the cerebellar tonsils through the foramen magnum, with compression of medullary respiratory centers and respiratory arrest,
is often the terminal event in CNS infections. Occasionally, space-occupying lesions within the cerebellum cause upward
herniation of posterior fossa contents through the tentorial notch (30). Extreme elevation of CSF pressure may elevate ICP
above systemic
P.10
arterial perfusion pressure, producing global cerebral and brainstem infarction.
Elevation in CSF pressure, as monitored by ICP monitoring devices, may provide an indication of prognosis in bacterial
meningitis and possibly in other CNS infections. Rebaud et al. (31) found that CSF pressures were significantly higher in
patients who succumbed to meningitis or encephalitis than in patients who survived, and they also found that cerebral
perfusion pressure (mean systemic arterial pressure minus ICP) was significantly lower in the former than in the latter.
Goitein and Tamir (32) found that all patients with meningitis or encephalitis who had a cerebral perfusion pressure more
than 30 mm Hg survived, whereas those with lower pressures died.
CSF ANALYSIS IN CNS INFECTIONS
Indications for Lumbar Puncture
Lumbar puncture is essential in the diagnosis of bacterial, viral, or fungal meningitis and may provide valuable information in
encephalitis. Lumbar puncture is also used to detect subarachnoid blood in bacterial endocarditis with mycotic aneurysm or
other potentially hemorrhagic infectious conditions. The procedure is of little specific diagnostic value in the diagnosis of
brain abscess or parameningeal infections. There are no absolute contraindications to lumbar puncture. Nonetheless,
inappropriate lumbar puncture can cause patient death or serious neurologic injury, and the procedure should never be
initiated without consideration of its potential danger to the patient.
Major Complications of Lumbar Puncture
Brain Herniation as a Consequence of Lumbar Puncture in the Setting of Increased
Intracranial Pressure
Though uncommon, brain herniation may result in patient death and is the most feared complication of lumbar puncture.
Lumbar puncture normally results in a mild, transient lowering of lumbar CSF pressure that is rapidly communicated
throughout the entire subarachnoid space. Space-occupying lesions within the skull, however, produce a relative pressure
gradient, with downward displacement of the cerebrum and brainstem (29,33). Lumbar puncture may increase this pressure
gradient and precipitate brain herniation (33,34). Herniation rarely occurs at the time of the lumbar puncture itself; instead,
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
8 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
it usually develops within a few hours of the procedure, as CSF continues to leak through the arachnoid at the site of
puncture.
The likelihood of brain herniation following lumbar puncture in the setting of elevated ICP is greatly influenced by the nature
of the underlying pathologic process and its degree of severity. With rare exceptions, there is little risk of herniation
following lumbar puncture in the setting of viral meningitis, and similarly, lumbar puncture can be performed safely in
patients with subarachnoid hemorrhage unless extensive parenchymal hemorrhage is present as well. Lumbar puncture can
also be performed safely in most patients with bacterial meningitis. However, severe bacterial meningitis may be
accompanied by a number of conditions that render brain herniation likely to occur. These include cortical encephalitis,
microabscesses, cerebral edema, hydrocephalus, and venous sinus or cortical vein thrombosis with hemorrhage (34,35,36).
Rennick, Shann, and de Campo (34) identified brain herniation in 19 of 443 children with bacterial meningitis: herniation was
present in 14 of 31 patients who had a fatal course. Lumbar puncture should, thus, be approached with caution in patients
with bacterial meningitis if one suspects severe elevation of ICP and impending herniation. In such patients, a 22- or 25-gauge
needle should be used, the patient should be watched closely for signs of impending herniation during the hours following the
procedure, and the use of dexamethasone, hyperventilation, and mannitol to lower ICP should be strongly considered, along
with placement of a device to monitor ICP. In extreme cases, it may be most prudent to treat the presumed meningitis with
broad-spectrum antibiotics, achieve medical control of intracranial hypertension, and defer lumbar puncture until the patient
is more stable (37). Careful clinical evaluation is usually able to define patients likely to have abnormal CT scans in the
setting of bacterial meningitis (38). However, the likelihood of brain herniation in the setting of meningitis with elevated ICP
may not be accurately predicted by CT or MRI (34).
The presence of space-occupying lesions significantly increases the risk of brain herniation. Brain abscess represents a rapidly
expanding space-occupying lesion in which focal brain displacement is present from the outset, and the risk of herniation
following lumbar puncture is 10% to 20% (33,39). Subdural empyema, which represents an even more rapidly expanding lesion,
presents a similar or greater risk. Herniation may also follow lumbar puncture in obstructive hydrocephalus (in this setting,
trapped intraventricular CSF behaves as a mass lesion), in patients with large intracranial hemorrhages, and in conditions
associated with extensive cerebral edema such as severe herpes simplex encephalitis, rickettsial encephalitis, or Reye
syndrome.
Patients with suspected meningitis who also have focal findings suggesting brain abscess present a significant clinical
dilemma. Lumbar puncture in such patients is of obvious diagnostic use, but the need to rule out localized infection by CT or
MRI may delay lumbar puncture for as long as several hours. Where concern exists that both meningitis and brain abscess may
be present, presumptive antibiotic therapy should be started immediately. A CT or MRI scan should then be obtained
emergently to exclude abscess, and the patient should undergo lumbar puncture after loculated infection or impending
herniation from the meningitis itself has been excluded. A similar concern may arise in the setting of spinal epidural abscess
or rarely spinal subdural empyema. In this setting, as in suspected brain abscess, presumptive antibiotic therapy should be
initiated, and MRI should be obtained on an emergent basis. CT myelography should be employed if MRI is not available.
Spinal fluid should be obtained at the time of myelography or after a compressive lesion has been ruled out by MRI.
P.11
Spinal Hematoma with Cord Compression
Lumbar puncture in patients with severe disorders of blood coagulation or in patients anticoagulated with heparin or
Coumadin may be complicated by continued bleeding at the site of puncture (40). Epidural or subdural collections of blood
may compress the cauda equina, thereby producing permanent neurologic injury (40). In general, lumbar puncture should be
avoided in such patients until their clotting mechanisms can be transiently or permanently returned to an acceptable range.
Introduction of Infection into the Subarachnoid Space
Inadvertent lumbar puncture through an area of infection overlying the spinal canal may result in seeding of the subarachnoid
space and meningitis. This is a particular risk in spinal epidural abscess or subdural empyema but may occasionally occur in
the setting of superficial or deep paraspinal infections. The problem can be avoided by entering the subarachnoid space at a
level well removed from the site of presumed infection. Thus, in patients with known or suspected focal lumbar infection,
spinal fluid should be obtained under fluoroscopic guidance by high cervical (C2) or cisternal puncture, whereas the lumbar
route should be used in patients with suspected cervical or upper thoracic infections. Introduction of infection into the
subarachnoid space during lumbar puncture in uninfected individuals has been reported as a complication of myelography or
spinal anesthesia but is very rare.
A long-standing concern in the evaluation of febrile patients with suspected CNS infection has been that lumbar puncture in
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
9 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
the setting of bacteremia might result in meningitis. This concern is based partly on experimental work by Petersdorf,
Swarner, and Garcia (41), who demonstrated that 81% of dogs undergoing cisternal puncture in the presence of severe
3
bacteremia (>10 organisms/mL of blood) developed meningitis, whereas meningitis did not develop in similarly bacteremic
3
control animals not undergoing cisternal puncture. Bacteremia at levels higher than 10 organisms/mL of blood, though
unusual in adult infections, may occur in up to 30% of patients with neonatal sepsis, and noteworthy is that investigators have
reported an association between meningitis and lumbar puncture in the setting of bacteremia in children younger than 1 year
but not in older children (42,43). Although these cases are of interest, normal CSF at the time of initial lumbar puncture does
not exclude the possibility that meningitis was already present in its early stages. The diagnostic usefulness of lumbar
puncture in the evaluation of febrile patients with suspected CNS infection far outweighs any small risk that the procedure
itself might lead to meningitis.
Post-Lumbar Puncture Headache
In approximately 30% of patients, lumbar puncture is followed by the development of severe, often disabling headache (44).
The headache is characteristically absent when the patient is recumbent and rapidly appears when the patient stands upright
or strains. Post-lumbar puncture headache is believed to be caused by low CSF pressure as a result of continued lumbar
leakage of CSF (45). The headache usually resolves spontaneously within hours to days, but continued CSF leakage over time
may result in persistent headache with diffuse, symmetric meningeal enhancement on MRI (46) (Fig. 2.3). In rare cases,
lumbar puncture in the setting of intracranial hypotension may result in development of subdural hematoma (47). In
persistent cases, a blood patch, in which the patient's own venous blood is injected outside the meninges at the site of the
lumbar puncture, may be used to seal the site of CSF leakage. Within the past few years, a number of blunt-tipped needles
have been developed for use in lumbar puncture, and these have a significantly lower incidence of post-lumbar puncture
headaches (48). Unfortunately, commercially available lumbar puncture kits almost always contain the older Quincke-point
(cutting-tip) needles.
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
10 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
FIG. 2.3. Gadolinium-enhanced MRI scan of a patient with intracranial hypotension. There is diffuse, symmetric
meningeal enhancement (arrows).
Less Common Complications of Lumbar Puncture
Cortical blindness: Downward displacement of the brainstem in states of increased ICP may compress the posterior cerebral
arteries against the edge of the tentorium cerebelli, causing ischemic infarction of the occipital lobes and cortical blindness
(29). Although this complication of intracranial hypertension is often accompanied by signs of uncal or tonsillar herniation,
compression of the posterior cerebral arteries may also occur before other signs of herniation appear. Prognosis for return of
vision is poor.
Cervical spinal cord infarction: Rarely, lumbar puncture in the setting of bacterial meningitis may be followed within a few
hours by respiratory arrest accompanied by flaccid tetraplegia (49). A variety of mechanisms, including hypotension and
vasculitis, have been postulated as the cause of cervical cord ischemia
P.12
in these patients. In some patients, however, it is likely that displacement of the cerebellar tonsils through the foramen
magnum as the result of greatly elevated ICP compresses the anterior spinal artery or its penetrating branches, with resultant
ischemic infarction of the upper cord (49).
Development of intraspinal epidermoid tumor: This complication of lumbar puncture occurred in patients who underwent
multiple lumbar punctures in which spinal needles were used without stylets. In the absence of the stylet, a small plug of skin
was inserted into the spinal canal and grew to cause a space-occupying mass. Epidermoid tumors do not occur if disposable
spinal needles are inserted with the stylet in place.
Technique of Lumbar Puncture
Numerous reviews have been devoted to techniques of the lumbar puncture, so a detailed description of the procedure is not
given here (1,48). However, one should keep in mind that the purpose of the lumbar puncture is to obtain an accurate
measurement of CSF pressure and collect quantities of CSF adequate for all studies required. These two objectives, though
obvious, may be forgotten or approached haphazardly in the urgency of initiating therapy in a critically ill patient. Thus,
before the procedure is performed, one must decide on the studies that will be required, to ensure that adequate numbers of
tubes are on hand to collect the samples needed and to discuss with the appropriate laboratories any studies that may require
advance preparation. The need for simultaneous evaluation of blood glucose levels should be kept in mind. Because CSF
glucose equilibrates with blood glucose level over time (see later discussion), blood for glucose measurement should be drawn
before rather than after the lumbar puncture. Samples should be delivered promptly to the technicians performing the
individual cultures and other tests. The lumbar puncture should be carefully noted in the patient's record, and the tests
ordered should be listed. When one is dealing with chronic or unusual CNS infections, blood and CSF should be frozen and
saved for future serologic and other tests. Because many clinical laboratories routinely discard samples after 1 to 3 months,
these samples should be placed in a secure location, and their specific locations should be noted, to prevent future loss.
Alternative Routes of Obtaining CSF
Cisternal, high cervical (C2), and ventricular approaches may be used to obtain CSF or to perform myelography if a lumbar
approach is contraindicated by infection or is technically impossible (1). Cisternal puncture has been used in cases of chronic
meningitis, and in a few cases, it has yielded organisms when organisms could not be detected by the lumbar route (50,51).
However, whether cisternal puncture is more useful in the setting of chronic meningitis than lumbar puncture with removal of
large volumes (40 to 50 mL) of CSF is unclear, and cultures of large volumes of fluid obtained by the lumbar route have also
yielded organisms after cultures of cisternal fluid have been negative (52). Spinal puncture at the level of the second cervical
vertebra has been suggested as a less hazardous approach than cisternal puncture, but its actual value remains unproven.
Ventricular CSF may be of great diagnostic value if there is a predominantly intraventricular infection with obstructive
hydrocephalus.
Routine Studies of CSF
Studies routinely obtained at the time of lumbar puncture include measurement of CSF pressure, gross examination of the
fluid for turbidity or changes in color, measurement of CSF protein and glucose concentrations, cell count, Gram and/or
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
11 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
acid-fast stains of CSF sediment, and Gram stain and bacterial culture of the fluid. Differentiation of bacterial meningitis
from viral, mycobacterial, or fungal meningitis on the basis of CSF abnormalities is presumptive unless an organism is seen
and unless the differentiation rests not on only one of these tests but on their sum. Amounts of CSF required by most
laboratories for commonly obtained determinations are listed in Table 2.1. Because clinical laboratories differ in the amounts
of CSF required for individual tests, however, the clinician must determine the amounts of CSF required by the hospital
laboratory for each intended test before performing the lumbar puncture.
CSF Pressure
CSF pressure must be measured in the lateral decubitus positionwith the patient lying horizontally, on his or her side. The
head of the bed should be flat, rather than elevated. Variations in posture and patient size make measurement of ICP
unreliable
P.13
with the patient sitting. Opening CSF pressure in healthy adults, with the patient in the lateral decubitus position, lies
between 50 and 195 mm CSF (3.8 to 15.0 mm Hg) (1). Values less than 150 mm CSF are clearly normal, those between 150 and
200 mm are suspicious, and those higher than 200 mm are abnormal. Normal lumbar CSF pressures in neonates and premature
infants are significantly lower, with mean values of 100 mm H O and 95 mm H O, respectively (53). CSF pressure is not
2
affected during pregnancy (54). However, the CSF pressure can be spuriously elevated by Valsalva maneuver in an anxious or
combative patient and may be falsely lowered by hyperventilation. Delay in obtaining the pressure reading over several
minutes may reduce pressure by allowing fluid to escape around the needle at its point of entry into the subarachnoid space.
Extreme elevation of CSF pressure may herald impending brain herniation. If significantly elevated pressure is found on
lumbar puncture, serious consideration should be given to both (a) use of measures to lower ICP and (b) continuous
monitoring of ICP and arterial pressure. Occasionally, CSF pressure may be normal or even low in the setting of ongoing
tonsillar herniation. The falsely low readings obtained in this setting are believed to reflect occlusion of the CSF space at the
foramen magnum by the herniated tonsils wedged against the lower brainstem. The possibility of complete spinal block should
be kept in mind if CSF pressure falls to zero during the procedure (see earlier discussion).
TABLE 2.1. MINIMAL VOLUMES OF CSF REQUIRED FOR COMMON DIAGNOSTIC TESTS
Test
Volume of CSF
Required
Cell count and differential
0.5-5.0 mL
Glucose and protein
0.5 mL
Bacterial culture
3-5 mL
Mycobacterial culture; fungal culture (includes acid-fast smear and India ink
preparation)
20 mL
Viral culture and/or PCR
1-2 mL
Cryptococcal antigen
0.5 mL
VDRL
0.5 mL
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
12 de 44
Oligoclonal bands
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
2 mL + serum
VDRL, Venereal Disease Research Laboratories.
>a
Volumes required represent minimal quantities of CSF required by most hospital laboratories. The clinician
should determine the amounts of CSF required by his or her hospital laboratory by each intended test before
performing the lumbar puncture.
Approximately 0.5 mL will be needed for cell count. Amount of CSF required for differential will vary,
depending on whether cytocentrifugation is used or material from centrifuged CSF sediment is studied.
c
Blood drawn before initiating the lumbar puncture should also be submitted with spinal fluid for determination
of simultaneous blood glucose level.
d
As little as 0.5 mL may be submitted for culture if there is great difficulty obtaining fluid. However, the use of
centrifuged sediment from larger volumes of CSF will improve yield on culture in acute bacterial meningitis. The
use of large volumes of CSF is essential in more chronic infections.
e
Yield on culture for acid-fast bacilli and fungi is, in general, extremely poor unless large volumes of CSF (20 mL
or more in adults) are cultured.
f
Serum (2-5 mL) drawn before or after the lumbar puncture should be submitted for electrophoresis along with
CSF.
Gross Appearance of the Spinal Fluid
Normal CSF is colorless and clear. Under pathologic conditions, CSF may become turbid, discolored, or both. The CSF may
3
become turbid as a result of entry of cells, bacteria, or fat; it can be made turbid by as few as 200 WBCs/mm or 400
3
RBCs/mm (1,55). CSF containing RBCs will be grossly bloody if 6,000 or more RBCs are present per cubic millimeter, and it
will be cloudy and xanthochromic or pinkish if 400 to 6,000 cells are present (1). In few patients, turbidity may result from
bacteria or fungi in the absence of cells. Rarely, epidural fat aspirated at the time of lumbar puncture can give a turbid
appearance to the CSF (56).
The CSF may be discolored by the presence of breakdown products of RBCs or by protein, bilirubin, or other pigments.
Discoloration of CSF by intact RBCs usually results in a reddish discoloration and turbidity. Although the average life span of
an RBC is 120 days in the circulation, rapid lysis of RBCs occurs in CSF. This results in a yellowish discoloration termed
xanthochromia or xanthochromasia. In most patients, xanthochromia begins to appear approximately 2 to 4 hours after RBCs
have entered the subarachnoid space. In 10% of patients, however, the appearance of xanthochromia may be delayed for 2 to
4 hours and is occasionally not seen for as long as 12 hours. Because CSF may remain colorless during the first 2 to 4 hours
after the onset of subarachnoid hemorrhage, the absence of xanthochromia during this period cannot be used as evidence of a
traumatic puncture. Xanthochromia may also develop within 1 hour in vitro after CSF has been removed, an important
consideration when the CSF obtained at lumbar puncture has been contaminated by a traumatic tap.
Xanthochromia resulting from lysis of RBCs is initially a result of oxyhemoglobin. After 12 hours, the pigment represents
predominantly bilirubin (1). Leakage of methemoglobin from a chronic parenchymal or subdural hemorrhage may also produce
xanthochromia. Xanthochromia may also represent the presence of increased amounts of protein, as described later, or may
be a consequence of systemic hyperbilirubinemia with a bilirubin level higher than 10 to 15 mg/dl. In rare instances,
xanthochromia may be caused by malignant melanoma metastatic to the meninges.
Viscosity of CSF is usually relatively little affected by the presence of meningeal infection or irritation. A qualitatively
appreciable change in CSF viscosity, however, may be seen in severe cryptococcal infections and is believed to represent
capsular polysaccharides (1). Similar viscosity may be produced by widespread metastasis of adenocarcinoma; in such cases,
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
13 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
mucicarmine stain of dried CSF residue may be positive (1).
Cell Count and Differential
Enumeration and characterization of cells within spinal fluid is of crucial value in the diagnosis of CNS infections and is
valuable in following the course of illness and response to treatment (Table 2.2). Improperly handled or counted CSF,
however, can be a dangerous source of error. The cell count in CSF tends to decrease over time and may be falsely low if
measured after 30 to 60 minutes. This decrease in cell count occurs partly because leukocytes and RBCs settle out over time
if the tube of CSF is
P.14
allowed to stand. In addition, however, lysis of RBCs, polymorphonuclear (PMN) leukocytes, and to a lesser extent,
lymphocytes begins in vitro within 1 to 2 hours of the lumbar puncture and may occasionally occur even more rapidly. WBCs
also adsorb to the glass or plastic walls of the tube and are not easily dislodged by agitation. Because of these factors, the
reduction in cell count that occurs over time is only partially reversible if the tube is vigorously agitated before counting. Any
CSF destined for cell counts should, thus, be handled carefully and expeditiously. Similarly, where serial tubes must be
counted to exclude a traumatic tap, the samples must be handled in the same manner and counted at the same time by the
same person.
TABLE 2.2. NORMAL CSF VALUES OF IMPORTANCE IN INFECTIOUS DISEASES OF THE NERVOUS SYSTEM:
VALUES IN ADULTS, TERM INFANTS, AND PREMATURE INFANTS
Adults
Term
Infants
<5
61
Mean
30
90
115
Range
9-58
20-170
65-150
62
52
50
45-80
34-119
24-63
Mean
0.60
0.81
0.74
Range
0.5-0.8
0.44-2.48
0.55-1.55
Parameter
Cell count (per cubic millimeter)
Percent polymorphonuclear leukocytes
Premature
Infants
57
Protein (mg/dl) (lumbar)
Glucose (mg/dl)
Mean
Range
CSF:blood glucose ratio
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
14 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
Cell counts in term and premature infants represent mean values. The range of cell counts found in normal
3
neonates is 0-32 cells/mm and in premature infants is 0-29, with 2 standard deviations encompassing a range of
3
0-22.4 cells/mm in term and 0-24.4 cells/mm in premature infants. By 1 month of age, normal CSF contains <20
3
cells/mm (2).
b
Rare polymorphonuclear leukocytes may be seen in cytocentrifuged samples of CSF from normal adults. This is
3
not necessarily abnormal if the CSF leukocyte count is 4 cells/mm or less and if protein and glucose levels are
normal.
c
Assumes a blood glucose level of 70-120 mg/dl. At high blood glucose levels (700 mg/dl), normal lower limit of
CSF:blood glucose ratios may approach 0.4 (see text).
Adapted from Fishman RA. Cerebrospinal fluid in diseases of the nervous system, 2nd ed. Philadelphia: WB
Saunders, 1992, with permission.
White Blood Cell Count
Quantification of numbers of cells in CSF should be carried out manually, using a Neubauer counting chamber. Electronic cell
3
counters are inaccurate for counts less than 1,000 cells/mm and should not be used to count CSF (1). The accuracy of the
cell count is open to question unless the specimen is examined immediately after the lumbar puncture has been completed.
Normally, CSF contains fewer than five cells per cubic millimeter (Table 2.2). Most of these cells are small lymphocytes
(nuclear diameter about 6 to 7 m) with scant cytoplasm. The presence of PMN leukocytes should be regarded with concern
(57). Occasionally, however, one to two PMN cells per cubic millimeter will be detected in otherwise normal CSF (1,48,57).
Larger numbers of PMN leukocytes are abnormal in uncentrifuged CSF. C. neoformans is similar in size to a small CSF
lymphocyte and may be mistaken for these cells in the counting chamber, though not in stained cytocentrifuged or otherwise
3
concentrated samples. Neonatal CSF usually contains 8 to 9 WBCs/mm , and up to 32 WBCs/mm has been reported in the
absence of disease (58) (Table 2.2).
Differential White Blood Cell Count
A differential count of CSF leukocytes may be obtained following concentration of CSF through a Millipore filter,
centrifugation of a volume (usually 5 mL) of CSF, concentration by sedimentation, or cytocentrifugation. The differential
normally contains a predominance of lymphocytes and approximately 14.5% neutrophils (1). Differential cell counts of CSF
from healthy neonates may yield up to 60% neutrophils (58). The number of neutrophils is increased in various conditions. In
adults with bacterial meningitis, neutrophils make up an average of 86.4% of cells counted, with neutrophils making up an
average of 34.2% of cells counted in aseptic meningitis (1,59). Large lymphocytes and other mononuclear cells are rarely seen
in normal, unspun CSF but may be present in samples of CSF examined by cytocentrifugation. Plasma cells and eosinophils
should not be present in normal CSF. Increased numbers of plasma cells are seen in infectious and noninfectious disorders and
have little diagnostic significance other than as an indicator of inflammation. CSF eosinophilia is particularly associated with
infections by Taenia solium (cysticercosis), and in patients with a history of residence in Southeast Asia or Pacific Islands, by
Angiostrongylus cantonensis and Gnathostoma spinigerum (1,60,61,62,63,64) (Table 2.3). Other helminthic infections may
also result in significant CSF eosinophilia. In addition, however, CSF eosinophilia has been reported in a wide variety of other
infectious and noninfectious conditions (Table 2.3), so detection of eosinophils within the CSF is not pathognomonic of
parasitic infestation (61,62,63,65).
TABLE 2.3. CONDITIONS ASSOCIATED WITH CSF EOSINOPHILIA
Parasitic infestations
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
15 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
Taenia solium (cysticercosis)
Angiostrongylus cantonensis
Gnathostoma spinigerum
Trichinella spiralis
Ascaris lumbricoides
Toxoplasma gondii
Toxocara cati
Toxocara canis
Other infectious agents or conditions
Mycobacterium tuberculosis
Treponema pallidum
Mycoplasma pneumoniae
Rocky Mountain spotted fever
Subacute sclerosing panencephalitis
Lymphocytic choriomeningitis virus
Fungal meningitides
Central nervous system disorders of noninfectious or unknown origin
Idiopathic eosinophilic meningitis
Granulomatous meningitis
Malignant lymphoma
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
16 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
Hodgkin disease
Leukemia
Multiple sclerosis
Subarachnoid hemorrhage
Obstructive hydrocephalus with shunt
Reaction to intrathecal antibiotics
Data from references 1, 61-65, with permission.
Red Blood Cells
The presence of RBCs in CSF may result from a traumatic lumbar puncture or may indicate subarachnoid or parenchymal
hemorrhage. Grossly bloody fluid that clears visibly as CSF is collected suggests a traumatic tap. Differentiation between a
traumatic lumbar puncture and subarachnoid blood as the result of intracranial or intraspinal pathology becomes more
difficult if only small numbers of RBCs are present. In such cases, one should compare numbers of RBCs present in CSF
obtained at the beginning of the lumbar puncture with numbers present in CSF obtained at the end of the procedure (e.g.,
one should count cells from tubes 1 or 2 and then from tubes 4 or 5). The presence of xanthochromia in samples centrifuged
immediately after obtaining CSF argues against a traumatic tap, although it must be kept in mind that lysis of RBCs in vitro in
CSF obtained during a traumatic tap will produce xanthochromia if the specimen is allowed to sit. Crenation of RBCs may
occur in vitro and has no diagnostic significance (66). Blood entering CSF during spontaneous subarachnoid hemorrhage or as
the result of a traumatic tap contains WBCs and RBCs, and thus, the CSF leukocyte count will increase. Numbers of WBCs
relative
P.15
to those of RBCs in CSF after a traumatic tap should be consistent with the leukocyte count of the peripheral blood, and the
differential count of CSF will be the same. In contrast, actual subarachnoid hemorrhage often produces a lymphocytic
pleocytosis, with elevation in the numbers of cells and alteration in the differential count. A traumatic tap in the setting of
CNS infection will increase the numbers of WBCs already present by an amount that can be calculated by comparing the ratio
of RBCs to WBCs in CSF with that seen in peripheral blood.
CSF Glucose
Most glucose present in CSF (Table 2.2) moves across the choroid plexus and across ventricular and subarachnoid capillaries by
facilitated transport. A smaller amount of glucose enters the CSF by simple diffusion. Glucose is removed from CSF through
utilization by cells lining the ventricles and subarachnoid space and by transport across capillaries and arachnoid villi. Entry of
glucose occurs over time, and more than 2 to 4 hours is required before serum and CSF glucose levels reach equilibrium (1). In
the absence of infection or other pathologic conditions, CSF glucose levels are a predictable reflection of blood glucose, and
the ratio of CSF to blood glucose concentrations is approximately 0.6. The CSF glucose level, equilibrated with a normal blood
glucose level of 70 to 120 mg/dl, thus ranges between 45 and 80 mg/dl (Table 2.2). Levels of glucose in ventricular fluid are 6
to 18 mg/dl higher than those in lumbar fluid (1,67).
CNS infections may alter glucose transport across the blood-CSF barrier, resulting in a low CSF glucose level, termed
hypoglycorrhachia (1). Further reduction in CSF glucose levels may result from glucose consumption by WBCs and organisms
(1). Reduction of CSF glucose relative to blood glucose is characteristic of meningitis because of bacteria, mycobacteria, or
fungi (68,69). The CSF glucose level is usually normal during viral infections. However, low CSF glucose levels are occasionally
observed in meningoencephalitis caused by mumps, enteroviruses, lymphocytic choriomeningitis, herpes simplex, and herpes
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
17 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
zoster viruses (70,71,72,73). Low CSF glucose values have also been described in CNS complications of Mycoplasma
pneumoniae infection, carcinomatous meningitis, CNS sarcoidosis, and subarachnoid hemorrhage (69,74,75,76,77). During
recovery from meningitis, CSF glucose levels tend to return toward normal more rapidly than cell counts and protein levels,
making CSF glucose levels an important parameter to follow in assessing response to therapy (78,79).
Both reduction in CSF glucose values and altered ratios of CSF to blood glucose levels are used as indicators of infection.
However, the literature contains a variety of recommendations about the point at which CSF glucose should be considered
abnormally low (58,71); this is partly because of the prolonged interval over which CSF glucose equilibrates with serum
glucose (1,67,68,80). In general, a CSF/blood glucose ratio less than 0.5 should be considered abnormal. In premature and
full-term infants, however, the normal CSF/blood glucose ratio is 0.74 to 0.96, and a ratio of 0.6 is usually considered
abnormal (58,80). In severe hyperglycemia, transport of glucose into CSF may lag, and at a blood sugar level of 700 mg/dl,
the CSF/blood glucose ratio may approach 0.4. For this reason, a ratio of 0.3 has been suggested as abnormal in diabetics
(81). Silver and Todd (71) addressed the problem of diagnostically significant hypoglycorrhachia in a study of 181 pediatric
patients with CSF glucose levels less than 50 mg/dl or a CSF/blood glucose ratio less than 50%. Patients ranged in age from
younger than 1 week to 14 years, with an average age of 1 years. Their series included patients with bacterial meningitis,
aseptic meningitis, subarachnoid hemorrhage, and CNS carcinomatosis but did not include patients with tuberculous or fungal
meningitis. Blood for glucose analysis was obtained 1 to 114 minutes before the lumbar puncture (average interval, 30
minutes). Of 35 patients with bacterial meningitis in this series, 27 (77%) had CSF glucose levels of 20 mg/dl or less, whereas
CSF glucose levels of 20 mg/dl or less were found in only 10 (7%) of 146 patients with other conditions; and of 37 patients
with glucose levels less than 20 mg/dl, 27 (73%) had bacterial meningitis. A CSF glucose level less than 20 mg/dl or a
CSF/blood glucose ratio less than 0.30 was highly correlated with bacterial meningitis, whereas an absolute CSF glucose value
between 20 and 50 mg/dl was nonspecific; also, a CSF/serum glucose ratio greater than 0.3 was felt to exclude most (but not
all) cases of bacterial meningitis. More recently, Spanos, Harrell, and Durack (82) analyzed the records of 422 patients with
acute bacterial or viral meningitis. These workers found that CSF glucose levels less than 18 mg/dl (1.9 mmol/L) and a
CSF/blood glucose ratio less than 0.23 were individual predictors of bacterial as opposed to viral meningitis, with 99% or
better certainty (82).
CSF Protein
Protein is largely excluded from CSF by the blood-CSF barrier and, under normal conditions, reaches CSF by pinocytotic
transport across capillary endothelia (1). Total CSF protein concentration in lumbar CSF of a healthy adult (Table 2.2) is less
than 40 mg, and the CSF/serum ratio of albumin is 1:200 (1,13). Mean values of lumbar CSF protein in healthy children and
adults have ranged from 23 to 38 mg/dl, and the extreme upper and lower concentrations have been 58 and 9 mg,
respectively (1). The CSF protein level in premature and full-term neonates may range between 20 and 170 mg/dl, with a
mean of 90 mg/dl (58) (Table 2.2). Protein concentrations in cisternal and lumbar CSF are lower, ranging from 13 to 30 mg/dl
(1). Elevation of protein concentration in the setting of CNS infections results from disruption of tight junctions between
endothelial cells of venules and, to a lesser extent, other small meningeal or parenchymal vessels (83). Elevation of CSF
protein level to more than 150 mg/dl may cause the CSF to be xanthochromic. Extreme elevation of protein (to >1.5 g/dl)
may cause formation of a weblike surface pellicle or an actual clot, as may high levels of fibrinogen (1). Levels of CSF protein
may be falsely elevated by deteriorating RBCs following subarachnoid hemorrhage or traumatic lumbar puncture. The amount
of increase is roughly 1 mg/dl per 1,000 RBCs. Accurate assessment of the contribution to total CSF protein made by RBCs
requires that the cell count and protein determination be carried out on the same tube of CSF.
P.16
Changes in the concentration of protein in CSF are the most common and least specific of CSF alterations in disease and are
seen in a wide variety of infectious and noninfectious neurologic conditions. Thus, an elevated CSF protein level, taken alone,
has little specific value in the diagnosis of CNS infections. Elevation of CSF protein to levels more than 100 mg/dl, particularly
if obtained on serial lumbar punctures, argues against viral infection, however, and Spanos, Harrell, and Durack (82) have
recently demonstrated that elevation of protein to a level of 220 mg/dl (2.2 g/L) suggests bacterial as opposed to viral
meningitis, with 99% or greater certainty. The CSF protein levels return to normal more slowly than glucose levels and cell
count during recovery from meningitis and may remain abnormal for months after parenchymal infections. Although elevation
of CSF protein is common in CNS infections, normal protein values are occasionally seen in all types of CNS infections,
including bacterial meningitis.
CSF Immunoglobulins
Immunoglobulins are almost totally excluded from normal CSF. The blood/CSF ratio of immunoglobulin G (IgG) in normal CSF
is usually in the range of 500:1. Immunoglobulin M (IgM) is essentially absent from CSF. Studies with radioiodinated IgG have
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
18 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
demonstrated that CSF IgG in healthy individuals is derived entirely from serum, requiring 3 to 6 days to reach equilibrium
(84). Immunoglobulins enter CSF less readily than albumin; and in health, immunoglobulin/albumin ratios in CSF are reduced
relative to those in serum. Elevation in CSF immunoglobulins may follow disruption of the BBB, allowing passage of
immunoglobulins across capillary endothelium, or may result from local antibody synthesis within the brain. Increased levels
of CSF IgG per se have little diagnostic value in CNS infections. Detection of oligoclonal IgG bands unique to CSF and not seen
in serum on gel electrophoresis provides strong evidence for an ongoing immune response within the brain. Oligoclonal bands
have been described in a variety of acute and chronic CNS infections of bacterial, mycobacterial, fungal, and viral origins, as
well as in a number of noninfectious neurologic disorders, so detection of oligoclonal bands in CSF is not reliable evidence of
infection.
Microscopic Methods for Detecting Infectious Organisms
Gram Stain
Gram stain is of crucial value in providing rapid identification of the offending organism in bacterial meningitis (Fig. 2.4). It is
usually the single most important piece of information the clinician uses to guide initial antibiotic therapy and should be an
invariable part of the CSF evaluation. Diagnostic accuracy of a properly prepared Gram stain is a function of the number of
3
organisms present. Work by LaScolea and Dryja (85) has shown that 25% of smears will be positive with 10 or fewer colony3
forming units (CFU) of bacteria per milliliter, 60% with 10 to 10 CFU/mL, and 97% with more than 10 CFU/mL. In general,
Gram stain is positive in 60% to 80% of untreated patients (85,86,87). The yield is approximately 20% lower in patients who
have received prior antibiotic therapy (86,87,88). Several pitfalls exist in obtaining an accurate study, all of which are largely
correctable with patience and experience. Haste in carrying out an examination of the material may allow the examiner to
miss organisms present in small numbers. This is less true for gram-positive organisms than for gram-negative bacteria and is
particularly true in the case of Neisseria meningitidis, which tends to be intracellular. Staphylococcus aureus may be
mistaken for streptococci if present as individual organisms. Listeria monocytogenes may be mistaken for diphtheroid
contaminants or for Streptococcus pneumoniae. False-positive Gram stains may result from bacteria present in the collecting
tubes, slides, or reagents, or rarely from bacterial contamination from a skin fragment excised by a spinal needle used
without its stylet (89,90).
Microscopic examination and culture require that the specimen be concentrated. Recommendations are that for volumes
more than 0.5 mL, the specimen be centrifuged for a minimum of 15 minutes at 3,000 g (30 minutes at 1,500 g).
Observation of bacteria on Gram stain preparations can be enhanced using cytocentrifugation. Two studies indicate that slides
prepared in a cytospin centrifuge (Shandon Southern Products Ltd., Cheshire, England) improve microscopic detection of
organisms in Gram-stained CSF when compared to conventional centrifugation (91). Leukocyte morphology is also preserved.
A disadvantage of this technique is the requirement for 0.4 to 0.5 mL of specimen, which is then not available for other
studies. If the volume of CSF available for culture and microscopic studies is less than 0.5 mL, then the entire unspun
specimen should be used for microscopic examination and culture (91).
The sensitivity of the Gram stain procedure varies to some extent with the offending organism. Organisms will be detected by
Gram stain in almost 90% of cases of pneumococcal or staphylococcal meningitis, 86% of cases caused by Haemophilus
influenzae, and 75% of patients with N. meningitidis meningitis (92). In contrast, organisms are present on Gram stain in only
50% of cases of gram-negative meningitis and in fewer than 50% of cases of meningitis caused by L. monocytogenes or
anaerobic organisms.
The utility of additional stains such as acridine orange, which may be used in conjunction with or in place of Gram stain, is
reviewed elsewhere (93). The acridine orange stain is a fluorochrome stain that has been shown to improve detection of
bacteria in CSF specimens, especially in patients who have partially treated bacterial meningitis (93). The Quellung test,
which uses a polyvalent antiserum against capsular antigens of bacteria such as S. pneumoniae, has been supplanted by other
tests for detection of bacterial antigens.
Acid-fast Stain
The sensitivity of the acid-fast stain depends greatly on the skill and persistence of the examiner and the amount of fluid
concentrated. In general, as large a volume of CSF as possibleat least 20 mLshould be taken for smear and culture unless
contraindicated by the presence of elevated ICP or a
P.17
focal mass lesion (69). In most series, acid-fast bacilli (AFB) have been detected in the first sample in fewer than 37% of
patients, although organisms may be detected in up to 87% of patients if material from four different lumbar punctures is
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
19 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
evaluated by experienced personnel (94). The likelihood of detecting organisms on acid-fast stain will be far less, however, if
only 1 to 2 mL of CSF is used to prepare the smear, if the examiner is unskilled, or if insufficient time is spent examining the
specimen. In a retrospective review of patients with tuberculous meningitis, Barrett-Connor (95) found that the AFB stain was
positive in only 2 of 21 patients. In a similar study of 43 children with tuberculous meningitis, Idriss, Sinno, and Kronfol (96)
found a positive AFB stain in only 5 (12%). In the series by Roberts (97), all 13 samples sent for AFB stain from patients who
were eventually found to have tuberculous meningitis were negative. Sensitivity of the acid-fast stain can be considerably
increased by immunofluorescence methods using auramine-rhodamine (98).
FIG. 2.4. Gram stains of CSF from patients with bacterial meningitis. A: Streptococcus pneumoniae. B: Neisseria
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
20 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
meningitides. C: Gram-negative meningitis.
P.18
Microscopic Detection of Ehrlichia, Fungi, and Protozoa in CSF
In a few cases, intracellular morulae have been detected in CSF of patients with meningitis due to Ehrlichia infection (99).
Fungi, including C. neoformans, Blastomyces dermatitidis, C. immitis, and Candida albicans, may occasionally be detected on
Gram or silver stains of concentrated CSF (100). In many cases of fungal meningitis, however, organisms are too few to be
readily detectable, and negative Gram or silver stains of CSF sediment in no way exclude the possibility of fungal infection.
India ink preparations, in which CSF sediment from 3 to 5 mL of CSF is mixed with a drop of India ink, provide a useful means
of outlining the capsule of C. neoformans in cases of cryptococcal meningitis (Fig. 2.5). Sensitivity of the India ink preparation
is about 50% in patients who are not infected with acquired immunodeficiency syndrome (AIDS) and more than 75% in patients
with AIDS. In patients without AIDS in particular, samples from several lumbar punctures may need to be examined before
organisms are found (69,101,102). Cryptococcal antigen detection has replaced India ink preparations in most laboratories.
FIG. 2.5. India ink preparation of CSF, from a patient with cryptococcal meningitis. The capsule of a cryptococcal
organism is clearly outlined by ink particles.
Wet mount preparations may be used to identify motile trophozoites in the CSF of patients with primary amebic
meningoencephalitis (103). Search for motile organisms in wet mounts may be made more reliable by the use of phasecontrast microscopy.
CSF Culture for Bacteria and Fungi
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
21 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
Choice of culture media, methods of handling, and lengths of time over which cultures are to be maintained are thoroughly
discussed in standard reviews and texts (100,104,105). The CSF should be submitted to the laboratory immediately after the
lumbar puncture and should be placed in culture promptly to avoid loss of fastidious organisms such as H. influenzae, N.
meningitidis, or anaerobes. CSF cultured for bacteria should, at a minimum, be plated on a 5% sheep blood agar, chocolate
agar, and inoculated into an enrichment broth (e.g., thioglycolate, Columbia, Brucella, supplemented peptone, or eugonic)
(104). A minimum of 2 mL (ideally 5 mL or more) should be submitted for Gram stain and bacterial culture. It is important for
the clinician to communicate with the laboratory if the patient has a condition that predisposes to anaerobic meningitis so
appropriate additional media can be added to the routine cultures.
Mycobacterial culture methods for the diagnosis of tuberculous meningitis overall have been disappointing: cultures may take
6 weeks or longer to become positive, and yield on culture in most Western countries is between 52% and 78% (94,106,107).
For this reason, there is great interest in newer molecular techniques employing the polymerase chain reaction (PCR) (see
Polymerase Chain Reaction Methods, later in this chapter). If infection by M. tuberculosis or fungi is suspected, at least 20
mL of CSF should be submitted for culture if not contraindicated by intracranial mass lesions or hydrocephalus, and 40 to 50
mL should be cultured if at all possible. Frequently, a second lumbar puncture is performed to obtain these larger volumes.
Sensitivity of cultures varies widely. The laboratory workers should be informed if cocci or Histoplasma infection is suspected
because of the risks.
C. neoformans is cultured from the CSF in approximately 72% of patients on the first lumbar puncture and in more than 90%
on multiple attempts (69,108). Frequency of recovery of C. albicans from CSF is also high (69,109,110). Isolation of other
organisms such as Histoplasma capsulatum or Brucella species often proves difficult (69,111). In both mycobacterial and
fungal infections, cultures of large volumes from multiple lumbar punctures may be required before an organism is identified
(69,111).
In most bacterial and fungal infections, extraneural sites of possible infection should also be cultured. Depending on the
organism being sought, these sites may include blood, urine, paranasal sinuses, ears, oropharynx, sputum, bone marrow,
prostate, or abscess material.
P.19
Viral Culture
Isolation of viral agents by tissue culture methods has been the traditional means of diagnosis in cases of suspected viral
meningitis or encephalitis. Newer methods of virus isolation have improved diagnostic yield; these include the incorporation
of multiple tissue culture cell lines and a combination of culture and staining procedures (shell vial assay for early antigen
detection, enzyme immunoassays, and immunofluorescence staining). Enteroviruses can be isolated in 43% to 77% of patients,
depending on the predominant viral serotype in a particular community. In approximately half of these cases, virus will be
isolated by day 3 and in more than 80% by day 7 (112). Mumps virus and lymphocytic choriomeningitis virus, the agents of
western and eastern equine encephalitides, may also be recovered from CSF. Herpes simplex virus (HSV) types 1 and 2 can be
isolated from cases of meningitis but are rarely recovered from CSF in cases of encephalitis. Varicella-zoster virus,
cytomegalovirus, and California, St. Louis, and Japanese encephalitis viruses are rarely recovered (113). At present, as is
discussed later, PCR methods have largely replaced tissue culture methods for enteroviruses, Herpetoviridae (herpes simplex,
herpes zoster, cytomegalovirus, Epstein-Barr virus), JC virus, and West Nile virus. West Nile virus meningoencephalitis is
diagnosed largely by serology because the virus is only rarely isolated by tissue culture methods at the time patients present
with neurologic symptoms (114).
ADJUNCTIVE AND MOLECULAR STUDIES OF CSF IN THE DIAGNOSIS OF CNS
INFECTION
The need for rapidly available accurate diagnostic information in CNS infections, the poor sensitivity of microscopic
examination of CSF sediment, and the delays inherent in obtaining results of CSF culture have led to the development of a
wide variety of rapid diagnostic tests for CNS infections. Availability and accuracy of these tests vary from institution to
institution, and the physician should learn which tests are readily available at his or her institution. The most promising of
these methods has been the use of PCR methods: PCR has largely supplanted tissue culture methods for the diagnosis of
enteroviral CNS infections and has provided a diagnostic tool far superior to traditional methods in the diagnosis of CNS
infections caused by herpesviruses, JC virus, and Tropheryma whippelii.
Bacterial Infections
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
22 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
Lactic Acid and C-Reactive Protein
Elevation of lactic acid levels in CSF occurs more frequently in bacterial than in viral meningitis. A CSF lactate cutoff value of
more than 3.5 to 4.2 mmol/L provides supportive evidence for a bacterial infection in untreated patients. Although earlier
literature reported poor specificity due to viral infections (115), subarachnoid hemorrhage, and other noninfectious causes at
lower cutoff values, two more recent studies report sensitivities of 0.88 to 0.96 and specificities of 0.98 to 1.0 using the
higher cutoff values (116,117). Determination of CSF lactate level may be particularly useful in differentiating bacterial
meningitis from nonbacterial meningitis in patients following neurosurgery, because the usual parameters of glucose, protein,
and cell count/differential are abnormal and overlap in both conditions. Differentiating D-lactate, made exclusively by
bacteria, from L-lactate, made by both bacterial and human cells, has not been shown to be of diagnostic value because only
10% of the CSF lactate is generated by organisms. The major component of CSF lactate is of human brain cell origin (118).
Both serum and CSF C-reactive protein (CRP) have been studied as potentially useful tools for discriminating bacterial
meningitis from other causes of CSF leukocytosis. This acutephase reactant is synthesized by the liver in response to various
infectious and noninfectious inflammatory conditions (119). Serum CRP concentrations are several-fold higher than those of
CSF; hence, many investigators have found serum a more useful measurement, particularly for monitoring serial
measurements as a response to therapy (120).
The greatest criticisms of CSF CRP as a useful measurement relate to poorly defined normal ranges, reported overlap in values
in patients with bacterial versus viral meningitis, and the impractical nature of testing multiple CSF samples over time (119).
Nevertheless, a metaanalysis of 35 studies of both children and adults with meningitis found a very high negative predictive
value for CRP (121). Improvements in assay performance have increased the sensitivity of available tests (119,120). Current
literature supports the assertion that CRP may be a useful supplement in the diagnosis and management of a subset of
patients with ambiguous CSF analysis. However, this test should be used with caution as the sole criterion in the
differentiation of bacterial versus viral meningitis (119,121).
Detection of Bacterial Antigens
Antigen-detection tests were developed to assist clinicians with rapid diagnosis of meningitis caused by H. influenzae type b,
N. meningitidis serogroups A, B, C, Y, and W135, S. pneumoniae, E. coli K1, and Streptococcus group B, and over the years,
the countercurrent immunoelectrophoresis (CIE) methods initially employed have been replaced with less technically
demanding latex agglutination assays. In general, these tests find little application; antigen-detection tests are less sensitive
than bacterial culture, and their diagnostic reliability and usefulness may vary from institution to institution. Routine use of
these assays offers few advantages over Gram stain and culture in the diagnosis of bacterial meningitis and cannot be justified
from a cost-effectiveness standpoint (122,123,124). In addition, the changing epidemiology of bacterial meningitis, as a result
of dramatic decreases in H. influenzae type b and a shift toward pathogens not detected by these assays, renders these tests
less diagnostically useful except in rare circumstances. Recent literature reports sensitivities as low as 7% to 28% (122,125)
and high false-positive rates (54% in one published series) (123). Bacterial antigen testing has been suggested to be of value in
cases of partially treated meningitis in which Gram stain and culture results are negative, but other CSF parameters are
suggestive of a bacterial process. However, even this scenario has been challenged by a study that assessed the utility of
antigen-detection
P.20
tests for pathogen detection in patients who met well-validated criteria for a clinical definition of acute bacterial meningitis.
In that study, bacterial antigen detection by latex agglutination had a sensitivity of 7% (125). Situations in which antigendetection tests are not likely to be helpful include cases in which the Gram stain is positive, in which the CSF WBC count and
chemistries are within normal limits, and in which the CNS infection is hospital acquired (123,124).
Polymerase Chain Reaction Methods
Early studies of PCR for diagnosis of bacterial pathogens were largely single-pathogen assays using nesting and other
procedures that were both cumbersome and susceptible to contamination (126). More recent studies have employed universal
primers from conserved regions of the 16S ribosomal RNA (rRNA) genes common to all eubacteria (127,128,129,130), with
subsequent identification of the PCR products as to species by immunoassays (131), restriction fragment digest (129), or
sequence analysis (128,130). Multiplex PCR using 5-exonuclease chemistry and real-time fluorescence technology has been
shown to allow specific diagnosis of common bacterial pathogens (e.g., S. pneumoniae, H. influenzae, and N. meningitidis)
within 2 to 3 hours (132,133). Sensitivity of these methods on culture-positive patients has exceeded 90% in most cases, and
the studies have a potential advantage over culture methods in that they are less rapidly affected by antibiotic therapy.
However, routine use of PCR in the diagnosis of bacterial infections is greatly limited by the skills and expertise required to
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
23 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
perform these assays in routine laboratories, their high costs compared with bacterial culture methods, and the lack of
available Food and Drug Administration (FDA)-cleared assays.
Mycobacterial Infections
Measurement of Adenosine Deaminase Levels in CSF
Adenosine deaminase is an enzyme that is widely distributed in human tissues and is present in high concentrations in
lymphocytes. Elevation of CSF adenosine deaminase levels may occur in a variety of neurologic disorders, including bacterial
meningitis, brain abscess, neurobrucellosis, cryptococcal meningitis, and CNS lymphoma. Elevated levels of lymphocyte
adenosine deaminase are frequently present in the CSF of patients with tuberculous meningitis, and measurement of this
enzyme has been used to provide presumptive evidence of M. tuberculosis infection and to evaluate response to treatment
(134,135,136). The test, though both sensitive and useful, is not specific, because it detects a component of host response
and does not detect a structural component of the organism itself.
Detection of Mycobacterial Antigens and Antibodies
Various immunologic tests have been developed to detect mycobacterial antigens and/or antibodies to mycobacterial
products in the CSF of patients with tuberculous meningitis. The most promising of these have employed enzyme-linked
immunosorbent assay (ELISA) methods using as a substrate either (a) monoclonal antibodies to mycobacterial products or (b)
antigens derived from bacille Calmette-Gurin (BCG) or M. tuberculosis. The sensitivity of these has ranged between 52.0%
and 81.25%, with a diagnostic specificity of more than 90% (137,138,139,140). In a study performed in a high prevalence
population in India (140), IgG antibody levels to a panel of six M. tuberculosis antigens were found to be high in 65% to 87% of
patients with tuberculous meningitis, depending on the stage of illness and the presence of human immunodeficiency virus
(HIV) disease. All noninfected control patients had IgG levels well below an established threshold level for positive results
(140). These tests are of considerable potential value because they are easy to perform and could readily be sold in kit form.
At present, however, each of the aforementioned techniques remains experimental, and a standardized ELISA for
mycobacterial infections of the nervous system is not yet in general use.
Polymerase Chain Reaction
There is no gold standard laboratory test for tuberculous meningitis. Culture and acid-fast stain have high specificity, but low
sensitivity. Diagnostic algorithms based on clinical and CSF parameters may be useful in high prevalence populations (141);
however, these are not adequate in areas where the prevalence of tuberculosis is low. For these reasons, molecular assays
have received great interest. Two commercial assays have been approved by the FDA: the Amplicor M. tuberculosis test
(Roche Diagnostics Systems, Inc., Branchburg, NJ) and the Enhanced Mycobacterium tuberculosis Direct Test (Gen-Probe, San
Diego, CA). FDA approval, however, has been for testing respiratory specimens, not CSF, and application of these tests to CSF
has given varying results (142). In part, this variation is due to the prevalence of disease in the population being studied.
Additionally, however, studies comparing PCR to culture-positive samples, without considering the pretest probability based
on clinical features, may overstate the sensitivity of these assays (143,144,145,146). Sensitivities in some studies have been in
the range of about 60% to 85%, but these studies involved patients already on empirical therapy and used CSF volumes
identical to those recommended by the manufacturers for respiratory samples (142,143). Several investigators have reported
enhanced sensitivity with these commercial products by increasing the volume of sample extracted, obtaining CSF before
empirical therapy is initiated, or pretreating the sample with detergents or other substances to remove inhibitors (142,145). A
variety of in-house assays using both single-copy and multicopy gene targets have also been developed and have been
reviewed elsewhere (147,148). Sensitivity of these assays has been similar to that observed with off-label use of the
commercial products (149,150). Despite the future promise of PCR in the diagnosis of tuberculous meningitis, molecular
assays should not be used as standalone tests for the diagnosis of tuberculous meningitis. A negative result by PCR should not
be assumed to indicate absence of M. tuberculosis, especially in the partially treated patient or in the patient with
appropriate epidemiology and clinical manifestations.
P.21
Lyme Disease
The overall sensitivity and specificity of tests for diagnosis of Lyme disease are still being determined, as is the accuracy of
tests used to diagnose CNS involvement. In the United States, the Centers for Disease Control and Prevention (CDC)
recommends using a two-step process for testing serum from patients suspected of having Lyme disease (151). Step one
involves screening with a sensitive assay such as ELISA or immunofluorescence assay. Those samples that are negative by such
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
24 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
an assay are not tested further. All equivocal or positive results are subsequently confirmed by immunoblotting (Western blot)
(151). Standardized criteria for interpretation of both IgM and IgG are outlined elsewhere (151). Antibody to Borrelia
burgdorferi may be absent early in the course of infection, and seronegative Lyme disease, diagnosed by T-cell proliferation
to Lyme disease, has been reported (152). False-positive test results for Lyme disease may be seen in patients with infectious
mononucleosis, positive serology for syphilis, and autoimmune conditions.
In the acute form of neuroborreliosis, there is usually pronounced synthesis of IgM antibody production (153). IgG and IgA
synthesis is seen in the chronic forms of disease (153). Detection of intrathecal antibody production is considered the most
specific test for neuroborreliosis (154). However, not all patients develop CSF antibodies. The CSF antibody production in
subtle CNS disease is inconsistent and may be lacking in patients with only peripheral nerve involvement (154). Detection of
CSF antibody is not essential for diagnosis (155,156). Accuracy and reliability of tests vary considerably between laboratories;
therefore, positive values reported by laboratories unfamiliar to the physician must be approached with caution and, if
necessary, confirmed.
PCR methods have been extensively studied for their utility in diagnosing Lyme neuroborreliosis, but results have varied
widely, depending on the selection of patients (acute vs. chronic disease), gene targets, PCR methods and controls, and
comparative test results (153,157,158). A recent metaanalysis derived from published PCR results irrespective of methods or
targets from patients with all stages of Lyme neuroborreliosis demonstrated an overall sensitivity of 19% and a specificity of
100% (157). Other reports have indicated that PCR is no more sensitive as a diagnostic tool than the measurement of
intrathecal antibody production and overall is less useful (159,160,161). PCR should not be considered a stand alone test
and a negative result does not rule out neuroborreliosis. At present, molecular assays may, at most, have a limited role as
adjunctive tests in patients who are seronegative and who have a high likelihood of infection (e.g., as in the case of the
immunodeficient patient). As research tools, molecular assays may provide insight into pathogenesis and clinical course when
used prospectively during the course of illness.
Fungal and Other Infections
Fungal Infections
Detection of cryptococcal antigen in spinal fluid is the most practical diagnostic test for cryptococcal meningitis. The test has
a high degree of specificity and is positive in 83% to 98% of patients (162,163). Early experience with false-positive titers in
some clinical situations have been eliminated by using pronase to digest rheumatoid-like factors present in CSF specimens
(164). Detection of cryptococcal antigen has replaced India ink stains, which are positive in 50% of non-AIDS patients and
more than 75% of patients with AIDS (165). Despite its sensitivity and specificity, however, assays for cryptococcal antigen
may occasionally give false-negative results in both immunocompetent and immunocompromised patients (162,166).
Complement-fixing antibodies have been reported in CSF in up to 95% of cases of meningitis caused by C. immitis infection
(167), although yield of detection has not been that high in all series (168). Diagnosis of Histoplasma meningitis can be
extremely difficult, especially the chronic form of the disease, which may occur in the absence of other manifestations of
disseminated infection (169,170). Detection of CSF antibodies may be useful, but false-positive results have been reported in
patients with fungal meningitis caused by other organisms and by diffusion of serum antibodies to H. capsulatum into the CSF
during other inflammatory conditions of the meninges (169). Histoplasma polysaccharide antigen detection by
radioimmunoassay has been reported in 40% of patients with meningitis. Diagnostic yield can be increased to more than 60% if
antigen is also detected in urine or serum (169,170).
Development of molecular techniques for diagnosis of fungal infections has lagged behind those assays for detection of other
pathogens. There are many reasons for this, but the most compelling is the ubiquitous nature of fungi in the environment and
the difficulties with contamination control. Initial assays used species-specific, single-copy genes (171). More recently,
investigators have evaluated the use of highly conserved, multicopy genes that are universal to all or most fungal species
(171). Such targets have included 18S rRNA subunit genes, 28S rRNA genes, mitochondrial genes, and the ITS region of the
rRNA gene (171,172). Specific organism identification can be established after amplification by using biotinylated universal
probes or other means (172). Such studies are promising but will require extensive clinical evaluation.
Toxoplasmosis
Encephalitis is the most common presentation of toxoplasmosis in the immunocompromised patient and most commonly
results from reactivation of latent infection (173). CSF antibody titers have been used to diagnose and follow CNS infections
caused by Toxoplasma gondii in both patients with AIDS and patients without AIDS (173,174,175). Intrathecal synthesis of
antibodies to T. gondii may be detected in a subset of patients with AIDS with toxoplasmic encephalitis, not all of whom will
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
25 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
have a demonstrable elevation in serum antibody titers (175). PCR may be useful in the absence of typical serologic or
radiologic studies (173). Current literature reports high specificity and positive predictive value but variable sensitivity
(176,177,178). The latter may reflect variations in primer selections and treatment status of the patients tested
(176,177,178). However, PCR detection could reduce the need for biopsy confirmation of T. gondii infection in patients with
AIDS and other immunocompromised
P.22
patients with negative serum antibody titers and atypical clinical presentations.
Whipple Disease
Whipple disease is a systemic illness caused by T. whippelii. Illness is characterized by a predominance of intestinal
manifestations, but extraintestinal manifestations including endocarditis, myocarditis, pericarditis, and CNS disease occur
with relative frequency (179). Although cultivation of the organism has been reported (180), diagnosis is generally made by a
combination of cytologic analysis of tissue and fluids using periodic acid-Schiff (PAS) staining to demonstrate the presence of
macrophages laden with intracellular organisms and electron microscopy (179). PCR has been helpful in the diagnosis of CNS
and other extraintestinal manifestations, particularly when these are the predominating clinical presentations (179). PCR has
also been used to determine the stage of disease and monitor response to therapy (181). False-positive PCR results have been
reported in asymptomatic individuals, and for this reason, PCR cannot be recommended in place of standard diagnostic
techniques (182).
Viral Infections
Before the advent of PCR, CSF antibody titers and determination of CSF/serum antibody ratios were used as methods of acute
viral diagnosis. Determination of CSF antibody titers per se has been found valuable in the diagnosis of chronic CNS infections
such as tropical spastic paraparesis or subacute sclerosing panencephalitis (183), but CSF antibody titers alone are of limited
value in most cases of acute viral encephalitis. Comparison of serum and CSF titers of IgG and IgM antiviral antibodies has
been proposed as a diagnostic test in encephalitis caused by HSV and other agents, but the test, which is dependent on
intrathecal antibody synthesis, is of limited value at the time of presentation, and intrathecal antibody may become
detectable only as virus is cleared from the CSF compartment (184,185,186,187,188). Most patients presenting with West Nile
virus infection already have CSF IgM antibodies to the virus, making this the diagnostic method of choice (114).
PCR methods have had their greatest impact in the diagnosis of viral meningitis and encephalitis. Despite the lack of
commercially available, FDA-cleared assays, PCR has replaced tissue culture methods in the diagnosis of enteroviral infections
of the CNS and/or as an adjunct to antibody testing for enteroviruses (189,190,191), HSV-1 and HSV-2 (192,193,194,195),
varicella-zoster virus (195,196), cytomegalovirus (197), Epstein-Barr virus (198), JC virus (199), and arboviruses, including
West Nile virus (200,201). Many university, reference, and public health laboratories offer highly sensitive and specific assays.
Physicians ordering these tests should request information regarding the validation of these assays and should be given upon
request data relating to analytic and clinical sensitivity and specificity, as well as inhibition rates. Indiscriminate ordering of
these assays on CSF samples should be discouraged. Triaging of CSF samples to particular assays should be based on
abnormalities of the CSF, seasonality, geographic location, immune status, and other clinical and epidemiologic data, as
suggested by Thomson and Bertram (100).
Compared to viral culture (overall sensitivity, 14% to 24%), the sensitivity of PCR ranges from 75% to 100% depending on the
virus (100,202). Molecular detection of viral nucleic acid sequences in CSF has not only improved diagnosis but also has largely
replaced invasive methods such as brain biopsy, has shortened time to specific diagnosis, and particularly in enteroviral CNS
infections, has proven cost-effective through decreased use of empirical antibacterial therapy and reduction in hospital stay
(189,190,193,194). Finally, molecular assays have added greatly to our understanding of the epidemiology and pathogenesis of
these infections (193,194).
Other Adjunctive Tests in the Diagnosis of CNS Infections
Gas-Liquid Chromatography
Gas-liquid chromatography (GLC) has been used to provide rapid diagnosis of bacterial meningitis and to differentiate
mycobacterial from fungal and viral meningitis (100,203). GLC has also been used with mass spectrometry to identify both the
mycobacterial metabolite 3-(2-ketohexyl)indoline and the mycobacterial component tuberculostearic acid (204). The study by
French et al. (204) is of particular interest because tuberculostearic acid was detected in the CSF of 21 of 22 patients and was
found in 1 patient after 237 days of therapy. The rather extensive technical requirements for accurate and reliable use of
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
26 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
GLC, with or without mass spectrometry, limit these methods to a few specialized laboratories.
Detection of Cytokines in CSF
TNF, interleukin-1 (IL-1), and other cytokines have received increasing attention as mediators of the inflammatory response
during bacterial meningitis (205,206,207). Leist et al. (206) have reported detection of TNF- in the CSF of three of three
patients with bacterial meningitis, but in none of seven patients with viral meningitis. Lopez-Cortez et al. (205) have recently
demonstrated that a TNF- level of more than 150 pg/mL and IL-1 level more than 90 pg/mL showed sensitivities of 74% and
90%, respectively, in discriminating viral from aseptic meningitis (205). Mustafa et al. (207) have demonstrated that IL-1 can
be detected in the CSF of 95% of infants and children with bacterial meningitis and that levels higher than 500 pg/mL were
correlated with increased risk of neurologic sequelae. These findings, though requiring both confirmation and amplification,
suggest that analysis of TNF and other cytokines, in particular IL-1, may prove valuable in differentiating acute bacterial
meningitis from viral meningitis and possibly in detecting patients at particular risk of adverse outcome. Their role in guiding
adjunctive therapy, such as corticosteroids and nonsteroidal treatment of BBB injury, is also under investigation.
CHARACTERISTIC CSF FINDINGS IN MAJOR CNS SYSTEM INFECTIONS
CSF changes in CNS infections often provide provisional or suggestive diagnostic significance. It must be kept in mind,
however,
P.23
that CSF changes in the absence of detectable organisms are not pathognomonic of any group of conditions and that CSF
findings must be interpreted in light of clinical, neurologic, and neuroradiologic findings. The need for caution is particularly
important when there is a question of viral versus bacterial infections. Here, an erroneous decision to withhold antimicrobial
therapy based on CSF interpretation alone may result in death (82).
Bacterial Meningitis
Bacterial meningitis characteristically produces a PMN pleocytosis, a depressed level of glucose, and an elevated protein
level. Numbers of PMN leukocytes may vary from a few to many thousand and usually range between 1,000 and 10,000 cells. A
predominantly (>50% of cells) lymphocytic pleocytosis has been reported in up to 14% of patients (208) and may be more
common in meningitis caused by L. monocytogenes infection (209). A predominance of lymphocytes may also be seen in
neonatal gram-negative meningitis (210). Leukocytes may be absent from CSF very early in the course of infection, in
neonatal meningitis, or in severely immunocompromised patients (68,211,212). Glucose levels less than 40 mg/dl or a
CSF/blood glucose ratio less than 0.4 should raise strong suspicion of bacterial meningitis, and a CSF/blood glucose ratio less
than 0.5 should be of concern. Glucose levels less than 18 mg/dl or a CSF/serum glucose ratio of 0.23 makes bacterial
meningitis extremely likely (71,82). Normal glucose values will be obtained in approximately 9% of patients. Protein levels
correspond with the intensity of meningeal inflammation but are between 100 and 500 mg/dl in most patients. Yield on Gram
stain varies from organism to organism (see previous discussion) but is positive in 60% to 80% of untreated patients.
Partially Treated Bacterial Meningitis
In general, antibiotics have little effect on CSF cell count, differential, protein, or glucose concentrations during the first 2 to
3 days of therapy (87,213,214,215). In a minority of patients, however, antibiotic therapy may result in a shift from a PMN to
a lymphocytic pleocytosis (214). Prior antibiotic therapy can be expected to reduce the diagnostic yield of Gram stain by
about 20% and that of culture by about 30% (213,215). Immunologic studies for bacterial antigens or, under experimental
conditions, PCR may permit identification of the causative organism.
Brain Abscess and Parameningeal Infection
Lumbar puncture in loculated parenchymal or parameningeal infections is usually not helpful and is contraindicated by the
risk of brain herniation. The CSF findings are nonspecific and may include (a) a mixed, predominantly lymphocytic pleocytosis,
(b) normal glucose level, and (c) elevated protein level. Organisms are not present unless there is accompanying meningitis,
in which case CSF findings will be those of bacterial meningitis (216).
Tuberculous Meningitis
Typical findings in tuberculous meningitis are (a) a pleocytosis with lymphocytic predominance, (b) lowered glucose level, and
(c) elevated protein level (94,95). In approximately 70% of patients, the cell count is between 100 and 400 cells (94).
However, as many as 1,000 to 1,200 cells may be present, and in few patients, the CSF is acellular despite the presence of
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
27 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
organisms, elevation in protein, and hypoglycorrhachia. Although most cells in the CSF are lymphocytes, relative numbers of
lymphocytes and PMN leukocytes may vary from lumbar puncture to lumbar puncture. Neutrophils predominate in
approximately 27% of patients and are most likely to be present early in the course of infection or in severe infection (97).
Small numbers of cells or acellular CSF may be found in patients with AIDS or those in other states of severe immune
deficiency. Protein levels are 100 to 500 mg/dl in 65% of patients and may reach levels of 1,000 mg or more if treatment is
delayed (94,95). In 25% of patients, protein levels are normal (94). Glucose levels are 30 to 45 mg/dl in 50% of patients and
may occasionally be less than 10 mg/dl. In 17% of patients, CSF glucose levels are normal (94).
M. tuberculosis may be extremely difficult to detect on smear or to recover by culture. When tuberculous meningitis is
strongly suspected, at least 20 mL of CSF should be submitted for acid-fast smear and culture unless contraindicated by
increased ICP; larger volumes (40 to 50 mL) should be submitted if possible. Frequently, the need for a second lumbar
puncture to obtain this large amount of CSF is first suggested by the abnormalities detected in the initial CSF sample. PCR, if
locally available, may provide a rapid means of diagnosis superior to acid-fast stain (142,143,144,145,146). During appropriate
therapy, the CSF glucose level returns toward normal before cell count or protein levels. The CSF cell counts and protein
levels may remain abnormal for protracted periods (94,95,106).
Fungal and Other Chronic Meningitides
Initial requirements for CSF analysis in suspected fungal infections are similar to those described for tuberculous meningitis,
and the same material may be sent for both mycobacterial and fungal culture. CSF should be submitted for cryptococcal
antigen and, if the patient has a history of residence in an endemic area, for complement-fixing antibodies to C. immitis or B.
burgdorferi. Additional samples of CSF should be submitted for serologic studies for H. capsulatum, Brucella, or other
organisms as indicated by history and occupational exposure. Serum and CSF should be frozen and held for future serologic
studies. CSF findings in fungal infections are similar to those described for tuberculous meningitis, except that PMN leukocytes
may be found less often. The number of cells present may vary widely, and as in tuberculous meningitis, CSF may be acellular
in severely immunocompromised patients, including those with AIDS (217,218). An exception to this rule is seen in infections
with Mucorales, in which the extremely destructive nature of the infection may result in large numbers of neutrophils (219).
As in tuberculous meningitis, CSF glucose level may return toward normal before changes are seen in cell count and protein.
Neurosyphilis
Suspicion of neurosyphilis is predicated on the presence of positive serum rapid plasma reagin (RPR) and fluorescent
treponemal
P.24
antibody-absorption (FTA-ABS) test results. CSF should be sent for Venereal Disease Research Laboratories (VDRL)
determination (see Chapter 37). The CSF may contain variable numbers of lymphocytes and an elevated protein level during
late primary and early secondary stages of the disease and during asymptomatic or symptomatic neurosyphilis (1). The
findings are extremely variable, however, and normal CSF cell count, protein, and glucose values do not exclude active
disease (220,221). Rarely, syphilis may present as an acute meningitis, with CSF findings similar to those of bacterial
meningitis (1). False-negative CSF VDRL determinations that became positive with penicillin therapy have been described in
neurosyphilis associated with AIDS (222). The diagnostic utility of detection of locally produced antibody against the antigens
of T. pallidum by Western blotting and PCR detection of DNA in the CSF is under investigation (223,224).
Lyme Borreliosis
The CSF changes in Lyme neuroborreliosis are typically a mild lymphocytic pleocytosis, modest elevation of protein level, and
normal glucose level. The CSF may be normal, however, or conversely may occasionally exhibit changes identical to those
seen in bacterial meningitis (155,225,226).
Infections Caused by Mycoplasma, Rickettsia, or Ehrlichia
CSF in meningoencephalitis associated with M. pneumoniae infections may be normal but has also been characterized by a
usually lymphocytic pleocytosis, elevated protein level, and mildly depressed glucose level (227). CSF in Rocky Mountain
spotted fever is usually acellular but may contain increased protein level (228); typhus may be accompanied by lymphocytic
pleocytosis and elevation of protein level (229). CSF in infections with Ehrlichia may resemble that of viral meningitis or may
be normal. One study has detected Ehrlichia morulae in CSF (99). In each of these illnesses, diagnosis may be made by
culture, serology, or PCR (230,231,232).
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
28 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
Viral and Other Acute Meningoencephalitides
Basic requirements for CSF analysis are identical to those for bacterial meningitis. The meningitis should be assumed to be
bacterial until proven otherwise. Lumbar puncture should be performed immediately, and CSF should always be submitted for
bacterial culture. Volumes and handling of CSF for viral culture should be reviewed with the laboratory, but the initial lumbar
puncture should not be delayed if arrangements cannot be made immediately. Viral meningitis produces a lymphocytic
3
pleocytosis, usually in the range of 10 to 1,000 cells/mm . PMN leukocytes may at times constitute more than 50% of the cells
during the first 24 to 36 hours of the infection (233,234) and in one series were shown to be present for several days (235). In
some patients, with coxsackievirus infections of the CNS, PMN leukocytes may constitute 90% of cells at the onset of
infection, and the predominance of PMN leukocytes may persist for longer than 24 hours. There are also reports of CSF
samples with few or no cells yielding enteroviruses on culture or by PCR (112,236). Protein is elevated in the range of 50 to
100 mg/dl but may sometimes be higher. Glucose is usually normal, but depression of glucose to levels approaching those of
bacterial meningitis has been reported in infections with HSV-2, herpes zoster virus, mumps, and lymphocytic
choriomeningitis virus (70,71,72,73,237,238). Spanos, Harrell, and Durack (82) have developed a helpful nomogram for
distinguishing between bacterial and viral meningitis. However, presumptive antibiotic therapy for bacterial meningitis should
be initiated if the diagnosis of viral meningitis is in doubt. CSF should be sent for PCR analysis for enteroviruses and, if there
is clinical suspicion, for herpes simplex, herpes zoster, and Mycoplasma infection (100,190). Both CSF and serum should be
frozen for future serologic testing.
Requirements for CSF analysis in cases of suspected viral encephalitis are similar to those for viral meningitis, and CSF
findings are often similar. PMN leukocytes may be present in large numbers in severe encephalitides accompanied by
extensive destruction of brain tissue. HSV classically produces a hemorrhagic encephalitis, and small amounts of blood may be
seen in the spinal fluid. However, HSV is not unique in its ability to produce hemorrhagic necrosis of brain, and RBCs are often
not detected; thus, the presence or absence of RBCs cannot be used to differentiate HSV encephalitis from other conditions.
As in viral meningitis, CSF should be sent for PCR and/or viral culture as appropriate, and both serum and CSF should held for
future serologic studies. CSF should be sent for IgM antibody determination in cases of suspected West Nile encephalitis.
AIDS
Abnormalities of CSF in HIV infection are protean and may reflect either (a) a response to CNS invasion by the agent itself, as
in HIV-related meningitis, meningoencephalitis, and encephalopathy, (b) meningitis or parenchymal infection by other agents,
or (c) meningeal reaction to neoplastic or ischemic events within brain or spinal cord. The response to any of these conditions
is often modified by the immunosuppressive effect of the virus (239,240). In HIV-infected individuals, normal findings on
routine CSF studies do not exclude infectious disease of the nervous system. The neurologic complications of HIV infection and
the approach to the patient with suspected neurologic involvement are discussed in detail elsewhere (Chapter 18).
Slow Infections Caused by Conventional Viruses
Three viruses are associated with protracted, often fatal human infection: JC virus, which causes progressive multifocal
leukoencephalopathy (PML); measles virus, which causes subacute sclerosing panencephalitis (SSPE); and human T
lymphotrophic virus type 1, which causes tropical spastic paraparesis (TSP). CSF in each of these conditions is almost always
acellular, with normal glucose and normal or minimally elevated protein levels. Rarely, PML may be accompanied by a modest
lymphocytic pleocytosis (241). CSF in SSPE and many cases of TSP contains oligoclonal bands and high titers of antiviral
antibody,
P.25
which can be used for specific diagnosis (242,243). Detection of JC virus in suspected cases of PML can be accomplished by
PCR of CSF (241). PCR has also been used for viral diagnosis SSPE and TSP (244).
Prion Diseases
Prion diseases do not elicit a cellular reaction in CSF, so the presence of a CSF pleocytosis essentially excludes this group of
diseases. Mild elevation of protein may occasionally be seen (245). In recent years, 14-3-3 protein, S100 protein, tau protein,
and neuron-specific enolase in CSF have been studied as markers for Creutzfeldt-Jakob disease; of these, 14-3-3 protein has
proven most valuable when used in appropriate clinical context. CSF may contain 14-3-3 protein in other neurologic
conditions, however, and its detection is thus not specific for prion diseases (246). CSF from cases of known or suspected
Creutzfeldt-Jakob disease should be regarded as infectious and handled according to current guidelines (247) (see Chapter
17).
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
29 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
REFERENCES
1. Fishman RA. Cerebrospinal fluid in diseases of the nervous system, 2nd ed. Philadelphia: WB Saunders, 1992.
2. Bleck TP, Greenlee JE. Approach to the patient with central nervous system infection. In: Mandell GL, Bennett JE,
Dolin R, eds. Principles and practice of infectious diseases. Philadelphia: Churchill Livingstone, 2000:950-959.
3. Strazielle N, Ghersi-Egea JF. Choroid plexus in the central nervous system: biology and physiopathology. J
Neuropathol Exp Neurol 2000;59(7):561-574.
4. Dimattio J, Hochwald GM, Malhan C, et al. Effects of changes in serum osmolality on bulk flow of CSF into cerebral
ventricles and on brain water content. Pflugers Arch 1975;359:253-264.
5. Johanson CE, Palm DE, Dyas ML, et al. Microdialysis analysis of effects of loop diuretics and acetazolamide on chloride
transport from blood to CSF. Brain Res 1994;641:121-126.
6. Welch K. The principles of physiology of the cerebrospinal fluid in relation to hydrocephalus including normal pressure
hydrocephalus. In: Friedlander WJ, ed. Advances in neurology. Current reviews. New York: Raven Press, 1975:345-375.
7. Yamashima T. Functional ultrastructure of cerebrospinal fluid drainage channels in human arachnoid villi.
Neurosurgery 1988;22:633-641.
8. Krisch B. Ultrastructure of the meninges at the site of penetration of veins through the dura mater, with particular
reference to Pacchionian granulations: investigations in the rat and two species of New World monkeys (Cebus apella,
Callitrix jacchus). Cell Tissue Res 1988; 251:621-631.
9. Tunkel AR, Scheld WM. Pathogenesis and pathophysiology of bacterial meningitis. Clin Microbiol Rev 1993;6:118-136.
10. Ellington E, Margolis G. Block of arachnoid villus by subarachnoid hemorrhage. J Neurosurg 2003;30:651-657.
11. Scheld WM. Bacterial meningitis in the patient at risk. Am J Med 1984;76(5A):193-207.
12. Simmerkoff MS, Moldover NH, Rahal JJ Jr. Absence of detectable bactericidal and opsonic activities in normal and
infected human cerebrospinal fluids: a regional host defense deficiency. J Lab Clin Med 1980;95:362-372.
13. Leibowitz S, Hughes RAC. Immunology of the nervous system. London: Arnold, 1983.
14. Zwahlen A, Nydegger UE, Vaudaux P, et al. Complement-mediated opsonic activity in normal and infected human
cerebrospinal fluid: early response during bacterial meningitis. J Infect Dis 1982;145(5):635-646.
15. Partridge WM. Recent advances in blood-brain barrier transport. Annu Rev Pharmacol Toxicol 1988;28:25-39.
16. Aschner M. Astrocytes as mediators of immune and inflammatory responses in the CNS. Neurotoxicology
1998;19(2):269-281.
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
30 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
17. Mustafa MM, Mertsola J, Ramilo O, et al. Increased endotoxin and interleukin-1 beta concentrations in cerebrospinal
fluid of infants with coliform meningitis and ventriculitis associated with intraventricular gentamicin therapy. J Infect
Dis 1989;160(5):891-895.
18. Pfister HW, Scheld WM. Brain injury in bacterial meningitis: therapeutic implications. Curr Opin Neurol
1997;10(3):254-259.
19. McCracken GH Jr, Mustafa MM, Ramilo O, et al. Cerebrospinal fluid interleukin 1-beta and tumor necrosis factor
concentrations and outcome from neonatal gram-negative enteric bacillary meningitis. Pediatr Infect Dis J
1989;8(3):155-159.
20. Gloor SM, Wachtel M, Bolliger MF, et al. Molecular and cellular permeability control at the blood-brain barrier. Brain
Res Brain Res Rev 2001;36(2-3):258-264.
21. Fishman RA. Blood-brain and CSF barriers to penicillin and related organic acids. Arch Neurol Psychiatry
1966;15:113-124.
22. Spector R. The transport of gentamicin in the choroid plexus and cerebrospinal fluid. J Pharmacol Exp Ther
1975;194(1):82-88.
23. Johnson RT, Johnson KP. Hydrocephalus following viral infection: the pathogenesis of aqueductal stenosis developing
after experimental mumps virus infection. J Neuropathol Exp Neurol 1968;27:591-606.
24. Timmons GD, Johnson KP. Aqueductal stenosis and hydrocephalus after mumps encephalitis. N Engl J Med
1970;283:1505-1507.
25. Mattle HP, Wentz KU, Edelman RR, et al. Cerebral venography with MR. Radiology 1991;178:453-458.
26. Bergsneider M. Evolving concepts of cerebrospinal fluid physiology. Neurosurg Clin N Am 2001;12(4):631-638, vii.
27. Mann JD, Butler AB, Rosenthal JE. Regulation of intracranial pressure in rat, dog, and man. Ann Neurol
1978;3:156-165.
28. Lundberg N, Cronquist S, Kjallquist A. Clinical investigations on the inter-relationships between intracranial pressure
and intracranial hemodynamics. Prog Brain Res 1968;30:69-81.
29. Plum F, Posner JB. The diagnosis of stupor and coma, 3rd ed. Philadelphia: FA Davis, 1980.
30. Cuneo RA, Caronna JJ, Pitts L, et al. Upward transtentorial herniation: seven cases and a literature review. Arch
Neurol 1979;36(10):618-623.
31. Rebaud P, Berthier JC, Hartemann E, et al. Intracranial pressure in childhood central nervous system infections.
Intensive Care Med 1988;14:522-525.
32. Goitein KJ, Tamir I. Cerebral perfusion pressure in central nervous system infections of infancy and childhood. J
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
31 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
Pediatr 1983;103:40-43.
33. Duffy GP. Lumbar puncture in the presence of raised intracranial pressure. Br Med J 1969;1:407-409.
34. Rennick G, Shann F, de Campo J. Cerebral herniation during bacterial meningitis in children. Br Med J
1993;306:953-955.
35. Pfister HW, Feiden W, Einhaupl KM. Spectrum of complications during bacterial meningitis in adults. Arch Neurol
1993;50:575-581.
36. Dodge PR, Swartz MN. Bacterial meningitisa review of selected aspects II. Special neurologic problems,
postmeningitic complications, and clinicopathological complications (concluded). N Engl J Med 1965;272:1003-1010.
37. Harper JR, Lorber J, Hillas SG, et al. Timing of lumbar puncture in severe childhood meningitis. BMJ
1985;291(6496):651-652.
38. Hasbun R, Abrahams J, Jekel J, et al. Computed tomography of the head before lumbar puncture in adults with
suspected meningitis. N Engl J Med 2001;345:1727-1733.
39. Wispelwey B, Scheld WM. Brain abscess. J Neuropharmacol 1987;10:483-510.
40. Domenicucci M, Ramieri A, Ciappetta P, et al. Nontraumatic acute spinal subdural hematoma: report of five cases
and review of the literature. J Neurosurg 1999;91[1 Suppl]:65-73.
41. Petersdorf RG, Swarner DR, Garcia M. Studies on the pathogenesis of meningitis. II. Development of meningitis
following pneumococcal bacteremia. J Clin Invest 1962;41:320-327.
P.26
42. Dietzman DE, Fischer GW, Schoenknecht FD. Neonatal Escherichia coli septicemiabacterial counts in blood. J
Pediatr 1974;85(1):128-130.
43. Teele DW, Dashefsky B, Rakusan T, et al. Meningitis after lumbar puncture in children with bacteremia. N Engl J Med
1981;305(18):1079-1081.
44. Evans RW, Armon C, Frohman EM, et al. Assessment: prevention of post-lumbar puncture headaches: report of the
therapeutics and technology assessment subcommittee of the American Academy of Neurology. Neurology
2000;55:55-909.
45. Lay CM. Low cerebrospinal fluid pressure headache. Curr Treat Options Neurol 2002;4(5):357-363.
46. Krause I, Kornreich L, Waldman D, et al. MRI meningeal enhancement with intracranial hypotension caused by
lumbar puncture. Pediatr Neurol 1997;16(2):163-165.
47. Francia A, Parisi P, Vitale AM, et al. Life-threatening intracranial hypotension after diagnostic lumbar puncture.
Neurol Sci 2001;22(5):385-389.
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
32 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
48. Evans RW. Lumbar puncture and cerebrospinal fluid evaluation. In: Evans RW, ed. Saunders manual of neurologic
practice. Philadelphia: Saunders (Elsevier), 2003:77-85.
49. Norman MG. Respiratory arrest and cervical spinal cord infarction following lumbar puncture in meningitis. Can J
Neurol Sci 1982;9:443-447.
50. Berger MP, Paz J. Diagnosis of cryptococcal meningitis. JAMA 1976;236:2517-2518.
51. Gonyea EF. Cisternal puncture and cryptococcal meningitis. Arch Neurol 1973;28:200-201.
52. Berlin L, Pincus JH. Cryptococcal meningitis: false-negative antigen test results and cultures in
nonimmunosuppressed patients. Arch Neurol 1989;46:1312-1316.
53. Vidyasagar D, Raju TNK. A simple noninvasive technique of measuring intracranial pressure in the newborn.
Pediatrics 1977;59:957-961.
54. Davis LE. Normal laboratory values of CSF during pregnancy. Arch Neurol 1979;36:443.
55. Patten BM. How much blood makes the cerebrospinal fluid bloody? JAMA 1968;206:378.
56. Mealy J. Fat emulsion as a cause of cloudy cerebrospinal fluid. JAMA 1962;180:246-248.
57. Bonadio WA. Bacterial meningitis in children whose cerebrospinal fluid contains polymorphonuclear leukocytes
without pleocytosis. Clin Pediatr (Phila) 1988;27(4):198-200.
58. Sarff LD, Platt LH, McCracken GH Jr. Cerebrospinal fluid evaluation in neonates: comparison of high-risk infants with
and without meningitis. J Pediatr 1976;88(3):473-477.
59. Mengel M. The use of the cytocentrifuge in the diagnosis of meningitis. Am J Clin Pathol 1985;84:212-216.
60. Bosch I, Oehmichen M. Eosinophilic granulocytes in the spinal fluid: analysis of 94 cerebrospinal fluid specimens and
review of the literature. J Neurol 1978;219:93-105.
61. Kuberski T. Eosinophils in the cerebrospinal fluid. Ann Intern Med 1979;91:70-75.
62. Ragland AS, Arsura E, Ismail Y, et al. Eosinophilic pleocytosis in coccidioidal meningitis: frequency and significance.
Am J Med 1993;95(3):254-257.
63. Weller PF. Eosinophilic meningitis. Am J Med 1993;95(3):250-253.
64. Tsai HC, Liu YC, Kunin CM, et al. Eosinophilic meningitis caused by Angiostrongylus cantonensis: report of 17 cases.
Am J Med 2001;111(2):109-114.
65. Grabb PA, Albright AL. Intraventricular vancomycin-induced cerebrospinal fluid eosinophilia: report of two patients.
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
33 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
Neurosurgery 1992;30(4):630-634.
66. Matthews WF, Frohmeyer WB Jr. The in vitro behavior of erythrocytes in human cerebrospinal fluid. J Lab Clin Med
1955;45:508-515.
67. Meyer GC, Netsky MG. Relation of blood and cerebrospinal fluid glucose. Arch Neurol Psychiatry 1962;6:18-20.
68. Swartz MN, Dodge PR. Bacterial meningitisa review of selected aspects 1. General clinical features, special
problems, and unusual meningeal reactions mimicking bacterial meningitis. N Engl J Med 1965;272:779-787.
69. Ellner JJ, Bennett JE. Chronic meningitis. Medicine 1976;55:341-369.
70. Adair CV, Gauld RL, Smadel JE. Aseptic meningitis, a disease of diverse etiology: clinical and etiologic studies on 854
cases. Ann Intern Med 1953;39:675-704.
71. Silver TS, Todd JK. Hypoglycorrhachia in pediatric patients. Pediatrics 1976;58:67-71.
72. Wolf SM. Decreased cerebrospinal fluid glucose in herpes zoster meningitis. Arch Neurol 1974;30:109.
73. Wilfert CM. Mumps meningoencephalitis with low cerebrospinalfluid glucose, prolonged pleocytosis with elevation of
protein. N Engl J Med 1969;280:855-858.
74. Klimek JJ, Russman BS, Quintiliani R. Mycoplasma pneumoniae meningoencephalitis and transverse myelitis in
association with low cerebrospinal fluid glucose. Pediatrics 1976;58(1):133-135.
75. Sharma OP. Neurosarcoidosis: a personal perspective based on the study of 37 patients. Chest 1997;112(1):220-228.
76. Zeller JA, Zunker P, Witt K, et al. Unusual presentation of carcinomatous meningitis: case report and review of
typical CSF findings. Neurol Res 2002;24(7):652-654.
77. Pasquier F, Leys D, Vermersch P, et al. Severe hypoglycorrhachia after subarachnoid hemorrhage: two cases with
spontaneous recovery in adults. Acta Neurol Belg 1987;87(2):76-79.
78. Valmari P, Peltola H, Kataja M. Cerebrospinal fluid white cell, glucose and protein changes during the treatment of
Haemophilus influenzae meningitis. Scand J Infect Dis 1986;18(1):39-43.
79. Roine I, Foncea LM, Ledermann W, et al. Slow recovery of cerebrospinal fluid glucose and protein concentrations
distinguish pneumococcal from Haemophilus influenzae and meningococcal meningitis in children. Pediatr Infect Dis J
1995;14(10):905-907.
80. Omene JA, Okolo AA, Longe AC, et al. The specificity and sensitivity of CSF and blood glucose concentration in the
diagnosis of neonatal meningitis. Ann Trop Paediatr 1985;5(1):37-39.
81. Powers WJ. Cerebrospinal fluid to serum glucose ratios in diabetes mellitus and bacterial meningitis. Am J Med
1981;71(2):217-220.
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
34 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
82. Spanos A, Harrell FE, Durack DT. Differential diagnosis of acute meningitis, an analysis of the predictive value of
initial observations. JAMA 1989;262:2700-2707.
83. Quagliarello VJ, Ma A, Stukenbrok H, et al. Ultrastructural localization of albumin transport across the cerebral
microvasculature during experimental meningitis in the rat. J Exp Med 1991;174(3):657-672.
84. Cutler RWP, Watters GV, Hammerstad JP. The origin and turnover rates of cerebrospinal fluid albumin and gamma
globulin in man. J Neurol Sci 1970;10:259-268.
85. LaScolea LJ Jr, Dryja D. Quantitation of bacteria in cerebrospinal fluid and blood of children with meningitis and its
diagnostic significance. J Clin Microbiol 1984;19(2):187-190.
86. Mandal BK. The dilemma of partially treated bacterial meningitis. Scand J Infect Dis 1976;8(3):185-188.
87. Jarvis CW, Saxena KM. Does prior antibiotic treatment hamper the diagnosis of acute bacterial meningitis? An
analysis of a series of 135 childhood cases. Clin Pediatr (Phila) 1972;11(4):201-204.
88. Davis SD, Hill HR, Feigl P, et al. Partial antibiotic therapy in Haemophilus influenzae meningitis: its effect on
cerebrospinal fluid abnormalities. Am J Dis Child 1975;129(7):802-807.
89. Joyer RW, Idriss ZH, Wilfert CM. Misinterpretation of cerebrospinal fluid Gram stain. Pediatrics 1974;54(3):360-362.
90. Southern PM Jr, Colvin DD. Pseudomeningitis again: association with cytocentrifuge funnel and Gram-stain reagent
contamination. Arch Pathol Lab Med 1996;120(5):456-458.
91. Chapin-Robertson K, Dahlberg SE, Edberg SC. Clinical and laboratory analyses of cytospin-prepared Gram stains for
recovery and diagnosis of bacteria from sterile body fluids. J Clin Microbiol 1992;30(2):377-380.
92. Graves M. Cerebrospinal fluid infections. In: Herndon RM, Brumback RA, eds. The cerebrospinal fluid. Boston:
Kluwer Academic, 1989:143-165.
P.27
93. Kleiman MB, Reynolds JK, Watts NH, et al. Superiority of acridine orange stain versus Gram stain in partially treated
bacterial meningitis. J Pediatr 1984;104(3):401-404.
94. Kennedy DH, Fallon RJ. Tuberculous meningitis. JAMA 1979;241(3):264-268.
95. Barrett-Connor E. Tuberculous meningitis in adults. South Med J 1967;60:1061-1067.
96. Idriss ZH, Sinno AA, Kronfol NM. Tuberculous meningitis in childhood: forty-three cases. Am J Dis Child
1976;130(4):364-367.
97. Roberts FJ. Problems in the diagnosis of tuberculous meningitis. Arch Neurol 1981;38(5):319-320.
98. Edberg SC, Samuels S. Conventional and molecular techniques for the laboratory diagnosis of infections of the
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
35 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
central nervous system. Neurol Clin 1986;4:13-39.
99. Berry DS, Miller RS, Hooke JA, et al. Ehrlichial meningitis with cerebrospinal fluid morulae. Pediatr Infect Dis J
1999;18(6):552-555.
100. Thomson RB Jr, Bertram H. Laboratory diagnosis of central nervous system infections. Infect Dis Clin North Am
2001;15(4):1047-1071.
101. Sabetta JR, Andriole VT. Cryptococcal infection of the central nervous system. Med Clin North Am
1985;69:333-344.
102. Treseler CB, Sugar AM. Fungal meningitis. Infect Dis Clin North Am 1990;4(4):789-808.
103. Singh U, Petri WA Jr. Free-living amebas. In: Mandell GL, Bennett JE, Dolin R, eds. Principles and practice of
infectious diseases. Philadelphia: Churchill Livingstone, 2000:2811-2817.
104. Gray LD, Fedorko DP. Laboratory diagnosis of bacterial meningitis. Clin Microbiol Rev 1992;5(2):130-145.
105. Krieg AF. Cerebrospinal fluid and other body fluids. In: Henry JB, ed. Clinical diagnosis and management by
laboratory methods. Philadelphia: WB Saunders, 1979:635-637.
106. Lincoln EM, Sordillo SVR, Davies PA. Tuberculous meningitis in children: a review of 167 untreated and 74 treated
patients with special reference to early diagnosis. J Pediatr 1960;57:807-823.
107. Sumaya CV, Simek M, Smith MH, et al. Tuberculous meningitis in children during the isoniazid era. J Pediatr
1975;87(1):43-49.
108. White MH. Cryptococcosis. Inf Dis Clin North Am 1994;8:383-398.
109. Fernandez M, Moylett EH, Noyola DE, et al. Candidal meningitis in neonates: a 10-year review. Clin Infect Dis
2000;31(2):458-463.
110. Sanchez-Portocarrero J, Perez-Cecilia E, Corral O, et al. The central nervous system and infection by Candida
species. Diagn Microbiol Infect Dis 2000;37(3):169-179.
111. Gripshover BM, Ellner JJ. Chronic meningitis. In: Mandell GL, Bennett JE, Dolin R, eds. Principles and practice of
infectious diseases. Philadelphia: Churchill Livingstone, 2000:997-1009.
112. Chonmaitree T, Baldwin CD, Lucia HL. Role of the virology laboratory in diagnosis and management of patients with
central nervous system disease. Clin Microbial Rev 1989;2:1-14.
113. Storch GA. The diagnosis of viral infections. Infect Dis Clin Pract 1993;2:1-20.
114. Campbell GL, Marfin AA, Lanciotti RS, et al. West Nile virus. Lancet Infect Dis 2002;2:1-16.
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
36 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
115. Jordan GW, Statland B, Halsted C. CSF lactate in diseases of the CNS. Arch Intern Med 1983;143:85-87.
116. Leib SL, Boscacci R, Gratzl O, et al. Predictive value of cerebrospinal fluid (CSF) lactate level versus CSF/blood
glucose ratio for the diagnosis of bacterial meningitis following neurosurgery. Clin Infect Dis 1999;29(1):69-74.
117. Genton B, Berger JP. Cerebrospinal fluid lactate in 78 cases of adult meningitis. Intensive Care Med
1990;16(3):196-200.
118. Wellmer A, Prange J, Gerber J, et al. D- and L-lactate in rabbit and human bacterial meningitis. Scand J Infect Dis
2001;33(12):909-913.
119. Jaye DL, Waites KB. Clinical applications of C-reactive protein in pediatrics. Pediatr Infect Dis J
1997;16(8):735-746.
120. Tatara R, Imai H. Serum C-reactive protein in the differential diagnosis of childhood meningitis. Pediatr Int
2000;42(5):541-546.
121. Gerdes LU, Jorgensen PE, Nexo E, et al. C-reactive protein and bacterial meningitis: a meta-analysis. Scand J Clin
Lab Invest 1998;58(5):383-393.
122. Mein J, Lum G. CSF bacterial antigen detection tests offer no advantage over Gram's stain in the diagnosis of
bacterial meningitis. Pathology 1999;31(1):67-69.
123. Perkins MD, Mirrett S, Reller LB. Rapid bacterial antigen detection is not clinically useful. J Clin Microbiol
1995;33(6):1486-1491.
124. Kiska DL, Jones MC, Mangum ME, et al. Quality assurance study of bacterial antigen testing of cerebrospinal fluid. J
Clin Microbiol 1995;33(5):1141-1144.
125. Tarafdar K, Rao S, Recco RA, et al. Lack of sensitivity of the latex agglutination test to detect bacterial antigen in
the cerebrospinal fluid of patients with culture-negative meningitis. Clin Infect Dis 2001;33(3):406-408.
126. du Plessis M, Smith AM, Klugman KP. Rapid detection of penicillinresistant Streptococcus pneumoniae in
cerebrospinal fluid by a seminested-PCR strategy. J Clin Microbiol 1998;36(2):453-457.
127. Saravolatz LD, Manzor O, VanderVelde N, et al. Broad-range bacterial polymerase chain reaction for early detection
of bacterial meningitis. Clin Infect Dis 2003;36(1):40-45.
128. Kotilainen P, Jalava J, Meurman O, et al. Diagnosis of meningococcal meningitis by broad-range bacterial PCR with
cerebrospinal fluid. J Clin Microbiol 1998;36(8):2205-2209.
129. Lu JJ, Perng CL, Lee SY, et al. Use of PCR with universal primers and restriction endonuclease digestions for
detection and identification of common bacterial pathogens in cerebrospinal fluid. J Clin Microbiol
2000;38(6):2076-2080.
130. Seward RJ, Towner KJ. Use of an automated DNA analysis system (DARAS) for sequence-specific recognition of
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
37 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
Neisseria meningitidis DNA. Clin Microbiol Infect 2000;6(1):29-33.
131. Seward RJ, Towner KJ. Evaluation of a PCR-immunoassay technique for detection of Neisseria meningitidis in
cerebrospinal fluid and peripheral blood. J Med Microbiol 2000;49(5):451-456.
132. Corless CE, Guiver M, Borrow R, et al. Simultaneous detection of Neisseria meningitidis, Haemophilus influenzae,
and Streptococcus pneumoniae in suspected cases of meningitis and septicemia using real-time PCR. J Clin Microbiol
2001;39(4):1553-1558.
133. Guiver M, Borrow R, Marsh J, et al. Evaluation of the Applied Biosystems automated Taqman polymerase chain
reaction system for the detection of meningococcal DNA. FEMS Immunol Med Microbiol 2000;28(2):173-179.
134. Choi SH, Kim YS, Bae IG, et al. The possible role of cerebrospinal fluid adenosine deaminase activity in the
diagnosis of tuberculous meningitis in adults. Clin Neurol Neurosurg 2002;104(1):10-15.
135. Lopez-Cortes LF, Cruz-Ruiz M, Gomez-Mateos J, et al. Adenosine deaminase activity in the CSF of patients with
aseptic meningitis: utility in the diagnosis of tuberculous meningitis or neurobrucellosis. Clin Infect Dis
1995;20(3):525-530.
136. Pettersson T, Klockars M, Weber TH, et al. Diagnostic value of cerebrospinal fluid adenosine deaminase
determination. Scand J Infect Dis 1991;23(1):97-100.
137. Sada E, Ruiz-Palacios GM, Lopez-Vidal Y, et al. Detection of mycobacterial antigens in cerebrospinal fluid of
patients with tuberculous meningitis by enzyme-linked immunosorbent assay. Lancet 1983;2(8351):651-652.
138. Prabhakar S, Oommen A. ELISA using mycobacterial antigens as a diagnostic aid for tuberculous meningitis. J Neurol
Sci 1987;78(2):203-211.
139. Watt G, Zaraspe G, Bautista S, et al. Rapid diagnosis of tuberculous meningitis by using an enzyme-linked
immunosorbent assay to detect mycobacterial antigen and antibody in cerebrospinal fluid. J Infect Dis
1988;158(4):681-686.
140. Chandramuki A, Lyashchenko K, Kumari HB, et al. Detection of antibody to Mycobacterium tuberculosis protein
antigens in the cerebrospinal fluid of patients with tuberculous meningitis. J Infect Dis 2002;186(5):678-683.
141. Thwaites GE, Chau TT, Stepniewska K, et al. Diagnosis of adult tuberculous meningitis by use of clinical and
laboratory features. Lancet 2002;360(9342):1287-1292.
142. Gamboa F, Manterola JM, Vinado B, et al. Direct detection of Mycobacterium tuberculosis complex in
nonrespiratory specimens by Gen-Probe amplified Mycobacterium tuberculosis direct test. J Clin Microbiol
1997;35(1):307-310.
143. Bonington A, Strang JI, Klapper PE, et al. Use of Roche Amplicor Mycobacterium tuberculosis PCR in early diagnosis
of tuberculous meningitis. J Clin Microbiol 1998;36(5):1251-1254.
P.28
144. Chedore P, Jamieson FB. Rapid molecular diagnosis of tuberculous meningitis using the Gen-Probe amplified
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
38 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
Mycobacterium tuberculosis direct test in a large Canadian public health laboratory. Int J Tuberc Lung Dis
2002;6(10):913-919.
145. Baker CA, Cartwright CP, Williams DN, et al. Early detection of central nervous system tuberculosis with the
Gen-Probe nucleic acid amplification assay: utility in an inner city hospital. Clin Infect Dis 2002;35(3):339-342.
146. Bonington A, Strang JI, Klapper PE, et al. TB PCR in the early diagnosis of tuberculous meningitis: evaluation of the
Roche semi-automated COBAS Amplicor MTB test with reference to the manual Amplicor MTB PCR test. Tuber Lung Dis
2000;80(4-5):191-196.
147. Kaul KL. Molecular detection of Mycobacterium tuberculosis: impact on patient care. Clin Chem
2001;47(8):1553-1558.
148. Soini H, Musser JM. Molecular diagnosis of mycobacteria. Clin Chem 2001;47(5):809-814.
149. Narayanan S, Parandaman V, Narayanan PR, et al. Evaluation of PCR using TRC(4) and IS6110 primers in detection
of tuberculous meningitis. J Clin Microbiol 2001;39(5):2006-2008.
150. Caws M, Wilson SM, Clough C, et al. Role of IS6110-targeted PCR, culture, biochemical, clinical, and immunological
criteria for diagnosis of tuberculous meningitis. J Clin Microbiol 2000;38(9):3150-3155.
151. Centers for Disease Control and Prevention. Recommendations for test performance and interpretation from the
second national conference on serological diagnosis of Lyme disease. MMWR Morb Mortal Wkly Rep 1995;44:590.
152. Dattwyler RJ, Volkman DJ, Luft BJ, et al. Seronegative Lyme disease: dissociation of specific T- and B-lymphocyte
responses to Borrelia burgdorferi. N Engl J Med 1988;319(22):1441-1446.
153. Kaiser R. Neuroborreliosis. J Neurol 1998;245(5):247-255.
154. Steere AC, Berardi VP, Weeks KE, et al. Evaluation of the intrathecal antibody response to Borrelia burgdorferi as a
diagnostic test for Lyme neuroborreliosis. J Infect Dis 1990;161:1203-1209.
155. Halperin JJ, Luft BJ, Anand AK, et al. Lyme neuroborreliosis: central nervous system manifestations. Neurology
1989;39(6):753-759.
156. Tylewska-Wierzbanowska S, Chmielewski T. Limitation of serological testing for Lyme borreliosis: evaluation of
ELISA and western blot in comparison with PCR and culture methods. Wien Klin Wochenschr 2002;114(13-14):601-605.
157. Dumler JS. Molecular diagnosis of Lyme disease: review and metaanalysis. Mol Diagn 2001;6(1):1-11.
158. Reed KD. Laboratory testing for Lyme disease: possibilities and practicalities. J Clin Microbiol 2002;40(2):319-324.
159. Zbinden R, Goldenberger D, Lucchini GM, et al. Comparison of two methods for detecting intrathecal synthesis of
Borrelia burgdorferi-specific antibodies and PCR for diagnosis of Lyme neuroborreliosis. J Clin Microbiol
1994;32(7):1795-1798.
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
39 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
160. Christen HJ, Eiffert H, Ohlenbusch A, et al. Evaluation of the polymerase chain reaction for the detection of
Borrelia burgdorferi in cerebrospinal fluid of children with acute peripheral facial palsy. Eur J Pediatr
1995;154(5):374-377.
160. Christen HJ, Eiffert H, Ohlenbusch A, et al. Evaluation of the polymerase chain reaction for the detection of
Borrelia burgdorferi in cerebrospinal fluid of children with acute peripheral facial palsy. Eur J Pediatr
1995;154(5):374-377.
161. Lebech AM, Hansen K, Brandrup F, et al. Diagnostic value of PCR for detection of Borrelia burgdorferi DNA in
clinical specimens from patients with erythema migrans and Lyme neuroborreliosis. Mol Diagn 2000;5(2):139-150.
162. Currie BP, Freundlich LF, Soto MA, et al. False-negative cerebrospinal fluid cryptococcal latex agglutination tests
for patients with culture-positive cryptococcal meningitis. J Clin Microbiol 1993;31(9):2519-2522.
163. Treseler CB, Sugar AM. Fungal meningitis. Infect Dis Clin North Am 1990;4:789-809.
164. Hamilton JR, Noble A, Denning DW, et al. Performance of cryptococcus antigen latex agglutination kits on serum
and cerebrospinal fluid specimens of AIDS patients before and after pronase treatment. J Clin Microbiol
1991;29(2):333-339.
165. Sato Y, Osabe S, Kuno H, et al. Rapid diagnosis of cryptococcal meningitis by microscopic examination of
centrifuged cerebrospinal fluid sediment. J Neurol Sci 1999;164(1):72-75.
166. Berlin L, Pincus JH. Cryptococcal meningitis: false-negative antigen test results and cultures in
nonimmunosuppressed patients. Arch Neurol 1989;46(12):1312-1316.
167. Bouza E, Dreyer JS, Hewitt WL, et al. Coccidioidal meningitis: an analysis of thirty-one cases and review of the
literature. Medicine (Baltimore) 1981;60(3):139-172.
168. Williams PL, Johnson R, Pappagianis D, et al. Vasculitic and encephalitic complications associated with Coccidioides
immitis infection of the central nervous system in humans: report of 10 cases and review. Clin Infect Dis
1992;14(3):673-682.
169. Wheat LJ, Kohler RB, Tewari RP, et al. Significance of Histoplasma antigen in the cerebrospinal fluid of patients
with meningitis. Arch Intern Med 1989;149(2):302-304.
170. Wheat LJ, Batteiger BE, Sathapatayavongs B. Histoplasma capsulatum infections of the central nervous system: a
clinical review. Medicine (Baltimore) 1990;69(4):244-260.
171. Stevens DA. Diagnosis of fungal infections: current status. J Antimicrob Chemother 2002;49[Suppl 1]:11-19.
172. Lindsley MD, Hurst SF, Iqbal NJ, et al. Rapid identification of dimorphic and yeast-like fungal pathogens using
specific DNA probes. J Clin Microbiol 2001;39(10):3505-3511.
173. Montoya JG. Laboratory diagnosis of Toxoplasma gondii infection and toxoplasmosis. J Infect Dis 2002;185 Suppl
1:S73-S82.
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
40 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
174. Luft BJ, Hafner R, Korzun AH, et al. Toxoplasmic encephalitis in patients with the acquired immunodeficiency
syndrome. N Engl J Med 1993;329:995-1000.
175. Potasman I, Resnick L, Luft BJ, et al. Intrathecal production of antibodies against Toxoplasma gondii in patients
with toxoplasmic encephalitis and the acquired immunodeficiency syndrome (AIDS). Ann Intern Med 1988;108(1):49-51.
176. Julander I, Martin C, Lappalainen M, et al. Polymerase chain reaction for diagnosis of cerebral toxoplasmosis in
cerebrospinal fluid in HIV-positive patients. Scand J Infect Dis 2001;33(7):538-541.
177. Contini C, Cultrera R, Seraceni S, et al. The role of stage-specific oligonucleotide primers in providing effective
laboratory support for the molecular diagnosis of reactivated Toxoplasma gondii encephalitis in patients with AIDS. J
Med Microbiol 2002;51(10):879-890.
178. Lin MH, Chen TC, Kuo TT, et al. Real-time PCR for quantitative detection of Toxoplasma gondii. J Clin Microbiol
2000;38(11):4121-4125.
179. Gerard A, Sarrot-Reynauld F, Liozon E, et al. Neurologic presentation of Whipple disease: report of 12 cases and
review of the literature. Medicine (Baltimore) 2002;81(6):443-457.
180. Raoult D, Birg ML, La Scola B, et al. Cultivation of the bacillus of Whipple's disease. N Engl J Med
2000;342(9):620-625.
181. von Herbay A, Ditton HJ, Schuhmacher F, et al. Whipple's disease: staging and monitoring by cytology and
polymerase chain reaction analysis of cerebrospinal fluid. Gastroenterology 1997;113(2):434-441.
182. Fenollar F, Fournier PE, Raoult D, et al. Quantitative detection of Tropheryma whipplei DNA by real-time PCR. J
Clin Microbiol 2002; 40(3):1119-1120.
183. Puccioni-Sohler M, Rios M, Carvalho SM, et al. Diagnosis of HAM/TSP based on CSF proviral HTLV-I DNA and HTLV-I
antibody index. Neurology 2001;57(4):725-727.
184. Sauerbrei A, Eichhorn U, Hottenrott G, et al. Virological diagnosis of herpes simplex encephalitis. J Clin Virol
2000;17(1):31-36.
185. Sauerbrei A, Wutzler P. Laboratory diagnosis of central nervous system infections caused by herpesviruses. J Clin
Virol 2002;25[Suppl 1]:S45-S51.
186. Koskiniemi M, Piiparinen H, Rantalaiho T, et al. Acute central nervous system complications in varicella zoster virus
infections. J Clin Virol 2002;25(3):293-301.
187. Vartdal F, Vandvik B, Norrby E. Intrathecal synthesis of virus-specific oligoclonal IgG, IgA, and IgM antibodies in a
case of varicella-zoster meningoencephalitis. J Neurol Sci 1982;57(1):121-132.
P.29
188. Vandvik B, Vartdal F, Norrby E. Herpes simplex virus encephalitis: intrathecal synthesis of oligoclonal virus-specific
IgG, IgA, and IgM antibodies. J Neurol 1982;228(1):25-38.
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
41 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
189. Ramers C, Billman G, Hartin M, et al. Impact of a diagnostic cerebrospinal fluid enterovirus polymerase chain
reaction test on patient management. JAMA 2000;283(20):2680-2685.
190. Robinson CC, Willis M, Meagher A, et al. Impact of rapid polymerase chain reaction results on management of
pediatric patients with enteroviral meningitis. Pediatr Infect Dis J 2002;21(4):283-286.
191. Rotbart HA, Sawyer MH, Fast S, et al. Diagnosis of enteroviral meningitis by using PCR with a colorimetric microwell
detection assay. J Clin Microbiol 1994;32(10):2590-2592.
192. Guffond T, Dewilde A, Lobert PE, et al. Significance and clinical relevance of the detection of herpes simplex virus
DNA by the polymerase chain reaction in cerebrospinal fluid from patients with presumed encephalitis. Clin Infect Dis
1994;18(5):744-749.
193. Cinque P, Cleator GM, Weber T, et al. The role of laboratory investigation in the diagnosis and management of
patients with suspected herpes simplex encephalitis: a consensus report. The EU Concerted Action on Virus Meningitis
and Encephalitis. J Neurol Neurosurg Psychiatry 1996;61(4):339-345.
194. Fodor PA, Levin MJ, Weinberg A, et al. Atypical herpes simplex virus encephalitis diagnosed by PCR amplification of
viral DNA from CSF. Neurology 1998;51(2):554-559.
195. Read SJ, Kurtz JB. Laboratory diagnosis of common viral infections of the central nervous system by using a single
multiplex PCR screening assay. J Clin Microbiol 1999;37(5):1352-1355.
196. Kleinschmidt-DeMasters BK, Gilden DH. Varicella-Zoster virus infections of the nervous system: clinical and
pathologic correlates. Arch Pathol Lab Med 2001;125(6):770-780.
197. Bestetti A, Pierotti C, Terreni M, et al. Comparison of three nucleic acid amplification assays of cerebrospinal fluid
for diagnosis of cytomegalovirus encephalitis. J Clin Microbiol 2001;39(3):1148-1151.
198. Weinberg A, Li S, Palmer M, et al. Quantitative CSF PCR in Epstein-Barr virus infections of the central nervous
system. Ann Neurol 2002; 53:543-548.
199. Garcia de Viedma D, Alonso R, Miralles P, et al. Dual qualitativequantitative nested PCR for detection of JC virus in
cerebrospinal fluid: high potential for evaluation and monitoring of progressive multifocal leukoencephalopathy in AIDS
patients receiving highly active antiretroviral therapy. J Clin Microbiol 1999;37(3):724-728.
200. Briese T, Glass WG, Lipkin WI. Detection of West Nile virus sequences in cerebrospinal fluid. Lancet
2000;355(9215):1614-1615.
201. Lanciotti RS, Kerst AJ. Nucleic acid sequence-based amplification assays for rapid detection of West Nile and St.
Louis encephalitis viruses. J Clin Microbiol 2001;39(12):4506-4513.
202. Reiber H, Peter JB. Cerebrospinal fluid analysis: disease-related data patterns and evaluation programs. J Neurol
Sci 2001;184(2):101-122.
203. French GL, Chan CY, Poon D, et al. Rapid diagnosis of bacterial meningitis by the detection of a fatty acid marker
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
42 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
in CSF with gas chromatography-mass spectrometry and selected ion monitoring. J Med Microbiol 1990;31(1):21-26.
204. French GL, Teoh R, Chan CY, et al. Diagnosis of tuberculous meningitis by detection of tuberculostearic acid in
cerebrospinal fluid. Lancet 1987;2(8551):117-119.
205. Lopez-Cortes LF, Marquez-Arbizu R, Jimenez-Jimenez LM, et al. Cerebrospinal fluid tumor necrosis factor-alpha,
interleukin-1beta, interleukin-6, and interleukin-8 as diagnostic markers of cerebrospinal fluid infection in neurosurgical
patients. Crit Care Med 2000;28(1):215-219.
206. Leist TP, Frei K, Kam-Hansen S, et al. Tumor necrosis factor alpha in cerebrospinal fluid during bacterial, but not
viral, meningitis: evaluation in murine model infections and in patients. J Exp Med 1988;167(5):1743-1748.
207. Mustafa MM, Lebel MH, Ramilo O, et al. Correlation of interleukin-1 beta and cachectin concentrations in
cerebrospinal fluid and outcome from bacterial meningitis. J Pediatr 1989;115(2):208-213.
208. Powers WJ. Cerebrospinal fluid lymphocytosis in acute bacterial meningitis. Am J Med 1985;79:216-220.
209. Lavetter A, Leedom JM, Mathias AW, et al. Meningitis due to Listeria monocytogenes: a review of 25 cases. N Engl J
Med 1971;285:589-603.
210. Bonadio WA. Acute bacterial meningitis: cerebrospinal fluid differential count. Clin Pediatr (Phila)
1988;27(9):445-447.
211. Fishbein DB, Palmer DL, Porter KM, et al. Bacterial meningitis in the absence of CSF pleocytosis. Arch Intern Med
1981;141(10):1369-1372.
212. Mangi RJ, Quintiliani R, Andriole VT. Gram-negative bacillary meningitis. Am J Med 1975;59(6):829-836.
213. Dalton HP, Allison MJ. Modification of laboratory results by partial treatment of bacterial meningitis. Am J Clin
Pathol 1968;49(3):410-413.
214. Converse GM, Gwaltney JM Jr, Strassburg DA, et al. Alteration of cerebrospinal fluid findings by partial treatment
of bacterial meningitis. J Pediatr 1973;83(2):220-225.
215. Blazer S, Berant M, Alon U. Bacterial meningitis: effect of antibiotic treatment on cerebrospinal fluid. Am J Clin
Pathol 1983;80(3):386-387.
216. Tunkel AR, Wispelwey B, Scheld WM. Brain abscess. In: Mandell GL, Bennett JE, Dolin R, eds. Principles and
practice of infectious diseases. New York: Churchill Livingstone, 2000:1016-1028.
217. Shaunak S, Schell WA, Perfect JR. Cryptococcal meningitis with normal cerebrospinal fluid. J Infect Dis
1989;160:912.
218. Panther LA, Sande MA. Cryptococcal meningitis in the acquired immunodeficiency syndrome. Semin Respir Infect
1990;5(2):138-145.
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
43 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
219. Lehrer RI, Hoard DH, Sypherd PS, et al. Mucormycosis. Ann Intern Med 1980;93:93-108.
220. Hutchinson CM, Hook EW III. Syphilis in adults. Med Clin North Am 1990;74(6):1389-1416.
221. Johns DR, Tierney M, Felsenstein D. Alteration in the natural history of neurosyphilis by concurrent infection with
the human immunodeficiency virus. N Engl J Med 1987;316(25):1569-1572.
222. Feraru ER, Aronow HA, Lipton RB. Neurosyphilis in AIDS patients: initial CSF VDRL may be negative. Neurology
1990;40:541-543.
223. Centurion-Lara A, Castro C, Shaffer JM, et al. Detection of Treponema pallidum by a sensitive reverse transcriptase
PCR. J Clin Microbiol 1997;35(6):1348-1352.
224. Marra CM, Gary DW, Kuypers J, et al. Diagnosis of neurosyphilis in patients infected with human immunodeficiency
virus type 1. J Infect Dis 1996;174(1):219-221.
225. Steere A. Lyme disease. N Engl J Med 1989;321:586-595.
226. Bourke SJ, Baird A, Bone FJ, et al. Lyme disease with acute purulent meningitis. Br Med J 1988;297:460-461.
227. Greenlee JE, Rose JW. Controversies in neurological infectious diseases. Semin Neurol 2000;20(3):375-386.
228. Miller JQ, Price TR. The nervous system in Rocky Mountain spotted fever. Neurology 1972;22:561-566.
229. Massung RF, Davis LE, Slater K, et al. Epidemic typhus meningitis in the southwestern United States. Clin Infect Dis
2001;32:979-982.
230. Socan M, Ravnik I, Bencina D, et al. Neurological symptoms in patients whose cerebrospinal fluid is culture- and/or
polymerase chain reaction-positive for Mycoplasma pneumoniae. Clin Infect Dis 2001;32(2):E31-E35.
231. Lotric-Furlan S, Petrovec M, Avsic-Zupanc T, et al. Epidemiological, clinical, and laboratory distinction between
human granulocytic ehrlichiosis and the initial phase of tick-borne encephalitis. Wien Klin Wochenschr
2002;114(13-14):636-640.
232. Paddock CD, Greer PW, Ferebee TL, et al. Hidden mortality attributable to Rocky Mountain spotted fever:
immunohistochemical detection of fatal, serologically unconfirmed disease. J Infect Dis 1999;179(6):1469-1476.
233. Feigin RD, Shackleford PG. Value of repeat lumbar puncture in the differential diagnosis of meningitis. N Engl J
Med 1973;289:571-574.
234. Varki AP, Puthuran P. Value of second lumbar puncture in confirming a diagnosis of aseptic meningitis. Arch Neurol
1979;36:581-582.
235. Negrini B, Kelleher KJ, Wald ER. Cerebrospinal fluid findings in aseptic versus bacterial meningitis. Pediatrics
11/07/2012 09:59 p.m.
Ovid: Infections of the Central Nervous System
44 de 44
http://eresources.library.mssm.edu:2216/sp-3.5.1a/ovidweb.cgi
2000;105(2):316-319.
P.30
236. Henquell C, Chambon M, Bailly JL, et al. Prospective analysis of 61 cases of enteroviral meningitis: interest of
systematic genome detection in cerebrospinal fluid irrespective of cytologic examination results. J Clin Virol
2001;21(1):29-35.
237. Brenton DW. Hypoglycorrhachia in herpes simplex type 2 meningitis. Arch Neurol 1980;37:317.
238. Reimer LG, Beller LB. CSF in herpes zoster meningoencephalitis. Arch Neurol 1981;38(10):668.
239. Saez-Llorens X, Ramilo O, Mustafa MM, et al. Molecular pathophysiology of bacterial meningitis: current concepts
and therapeutic implications. J Pediatr 1990;116:671-684.
240. Woods WJ, Berger JR, Kaderman R, et al. Human immunodeficiency virus infection of the brain. Clin Microbiol Rev
1993;6:339-366.
241. Greenlee JE, O'Neill FP. Polyomaviruses. In: Richman DD, Whitley RJ, Hayden FG, eds. Clinical virology.
Washington, DC: ASM Press, 2002:537-555.
242. Kitze B, Usuku K, Izumo S, et al. Diversity of intrathecal antibody synthesis against HTLV-I and its relation to HTLV-I
associated myelopathy. J Neurol 1996;243(5):393-400.
243. Salmi AA, Norrby E, Panelius M. Identification of different measles virus-specific antibodies in the serum and
cerebrospinal fluid from patients with subacute sclerosing panencephalitis and multiple sclerosis. Infect Immun
1972;6(3):248-254.
244. Baram TZ, Gonzalez-Gomez I, Xie ZD, et al. Subacute sclerosing panencephalitis in an infant: diagnostic role of
viral genome analysis. Ann Neurol 1994;36(1):103-108.
245. Roos R, Gajdusek DC, Gibbs CJ Jr. The clinical characteristics of transmissible Creutzfeldt-Jakob disease. Brain
1973;96(1):1-20.
246. Satoh J, Kurohara K, Yukitake M, et al. The 14-3-3 protein detectable in the cerebrospinal fluid of patients with
prion-unrelated neurological diseases is expressed constitutively in neurons and glial cells in culture. Eur Neurol
1999;41(4):216-225.
247. Weber DJ, Rutala WA. Managing the risk of nosocomial transmission of prion diseases. Curr Opin Infect Dis
2002;15(4):421-425.
11/07/2012 09:59 p.m.
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Neuroanatomy MCQДокумент7 страницNeuroanatomy MCQi can always make u smile :D78% (9)
- Neuroanatomy Laboratory Guide 2011Документ8 страницNeuroanatomy Laboratory Guide 2011Steve BlubaughОценок пока нет
- Laurie Lundy-Ekman-Neuroscience - Fundamentals For Rehabilitation-Saunders (2007) (Trashed 2016-03-14 10-21-35) (Trashed 2019-05-29 09-55-40)Документ645 страницLaurie Lundy-Ekman-Neuroscience - Fundamentals For Rehabilitation-Saunders (2007) (Trashed 2016-03-14 10-21-35) (Trashed 2019-05-29 09-55-40)Razvan Cde100% (1)
- Cerebrospinal FluidДокумент154 страницыCerebrospinal Fluidabhirox69100% (1)
- Ventricles of The Brain and CSFДокумент22 страницыVentricles of The Brain and CSFVytheeshwaran Vedagiri100% (9)
- Atlas Of: Human Body Ultrasound ScanningДокумент575 страницAtlas Of: Human Body Ultrasound ScanningGARY WILLIAMS CORTEZ PEREZОценок пока нет
- Neonatal-Cranial-Ultrasonography 2nd EditionДокумент162 страницыNeonatal-Cranial-Ultrasonography 2nd Editionpalina86Оценок пока нет
- Cross-Sectional Anatomy For Computed TomographyДокумент87 страницCross-Sectional Anatomy For Computed TomographyMurat hüseyin AtinОценок пока нет
- Gillenwater - Adult and Pediatric Urology 4th EdДокумент1 564 страницыGillenwater - Adult and Pediatric Urology 4th EdRoxana Boloaga100% (1)
- Congenital Malformations of The BrainДокумент57 страницCongenital Malformations of The Brainmanisha paikarayОценок пока нет
- Case Study HydrocephalusДокумент19 страницCase Study HydrocephalusJane Mae JesoroОценок пока нет
- 01 - B. S. Rama Murthy - Imaging of Fetal Brain and Spine - An Atlas and Guide (2019, Springer Singapore)Документ342 страницы01 - B. S. Rama Murthy - Imaging of Fetal Brain and Spine - An Atlas and Guide (2019, Springer Singapore)Nicolas50% (2)
- Impact of Spaced Repetition Learning Model On Long Term Memory Retrieval of Neuroanatomy Among 1styear Medical StudentsДокумент1 страницаImpact of Spaced Repetition Learning Model On Long Term Memory Retrieval of Neuroanatomy Among 1styear Medical StudentsduffuchimpsОценок пока нет
- Rain Natomy: Adapted From Human Anatomy & Physiology by Marieb and Hoehn (9 Ed.)Документ16 страницRain Natomy: Adapted From Human Anatomy & Physiology by Marieb and Hoehn (9 Ed.)vibs1994Оценок пока нет
- Color Atlas of BrainДокумент8 страницColor Atlas of BrainMWОценок пока нет
- Brain Volumes and Their Ratios in Alzheimer S Disease On Magnetic Resonance Imaging Segmented Using Freesurfer 6.0Документ5 страницBrain Volumes and Their Ratios in Alzheimer S Disease On Magnetic Resonance Imaging Segmented Using Freesurfer 6.0Edgar RamirezОценок пока нет
- UERM GROSS Cerebrum Cerebellum and CT ScanДокумент82 страницыUERM GROSS Cerebrum Cerebellum and CT Scanroxanne.viriОценок пока нет
- ProcedureДокумент1 страницаProcedureJoanna EdenОценок пока нет
- Esclerosis Mesial Temporal (Emt)Документ21 страницаEsclerosis Mesial Temporal (Emt)kennethlgОценок пока нет
- Featured Applied Radiology Article: Pediatric Neuroradiology Part 1 - Embryo Logic Basis For Brain MalformationДокумент12 страницFeatured Applied Radiology Article: Pediatric Neuroradiology Part 1 - Embryo Logic Basis For Brain MalformationradRounds Radiology NetworkОценок пока нет
- (White Paper) WP202208-ViewAssistTM and BiometryAssistTMДокумент8 страниц(White Paper) WP202208-ViewAssistTM and BiometryAssistTMultrasound tomОценок пока нет
- Sistem Ventrikel Dan LCSДокумент22 страницыSistem Ventrikel Dan LCSsamiratumananОценок пока нет
- Anatomi 1Документ82 страницыAnatomi 1Gek NissaОценок пока нет
- Vascular Supply To The BrainДокумент38 страницVascular Supply To The BrainGhea Putri HendrianiОценок пока нет
- White Matter of The Cerebral HemispheresДокумент50 страницWhite Matter of The Cerebral HemispheresSandy MonirОценок пока нет
- Case Report: Intracranial Multiple Germ Cell Tumors: A Case Report and Review of LiteratureДокумент6 страницCase Report: Intracranial Multiple Germ Cell Tumors: A Case Report and Review of Literaturearcobaleno589Оценок пока нет
- Blood Supply of The Neck and HeadДокумент56 страницBlood Supply of The Neck and HeadAdrianaОценок пока нет
- Cerebrum: Dr. Katharina Kian R. Demerre - Bacolod PT 21Документ111 страницCerebrum: Dr. Katharina Kian R. Demerre - Bacolod PT 21Hephzibah JaporОценок пока нет
- Structures of The Brai N: WorksheetДокумент1 страницаStructures of The Brai N: WorksheetPrince Arguelles EdañoОценок пока нет
- Predictor Scale of Delayed Cerebral Ischemic in Aneurysmal Subarachnoid Hemorrhage Case Series: What A Radiologist Should KnowДокумент5 страницPredictor Scale of Delayed Cerebral Ischemic in Aneurysmal Subarachnoid Hemorrhage Case Series: What A Radiologist Should KnowPopy TheresiaОценок пока нет