Академический Документы
Профессиональный Документы
Культура Документы
Hipervitaminosis Vitamin
Загружено:
Hana ZawtumАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Hipervitaminosis Vitamin
Загружено:
Hana ZawtumАвторское право:
Доступные форматы
Bansal et al.
Journal of Medical Case Reports 2014, 8:74
http://www.jmedicalcasereports.com/content/8/1/74
JOURNAL OF MEDICAL
CASE REPORTS
CASE REPORT
Open Access
Iatrogenic hypervitaminosis D as an unusual
cause of persistent vomiting: a case report
Rinkesh Kumar Bansal, Pankaj Tyagi, Praveen Sharma, Vikas Singla, Veronica Arora, Naresh Bansal,
Ashish Kumar and Anil Arora*
Abstract
Introduction: Vitamin D is increasingly recognized to have several beneficial effects. Vitamin D deficiency is widely
prevalent. Physicians often treat patients with high doses of vitamin D for various ailments without any monitoring
for adverse effects and the prescribed doses often far exceed requirements resulting in toxicity. We present here a
classic case of iatrogenic hypervitaminosis D, which presented with persistent vomiting and acute renal failure.
Case presentation: Here we present a case of a 45-year-old Asian Indian woman who presented to us with
persistent vomiting the cause of which was iatrogenic hypervitaminosis D. She was treated with intravenous fluid,
diuretics and calcitonin and had clinical improvement.
Conclusions: We suggest that in any patient presenting with persistent vomiting and hypercalcemia, particularly in
the presence of normal parathyroid hormone, a diagnosis of overdose of vitamin D should be suspected. Its
treatment not only alleviates symptoms but also prevents ongoing acute kidney injury.
Keywords: Hypercalcemia, Hypervitaminosis, Vitamin D
Introduction
Vitamin D is an important prohormone which plays an
important role in calcium homeostasis and bone mineral
metabolism. Vitamin D also subserves in a wide range of
fundamental biological functions like cell differentiation,
inhibition of cell growth as well as immune modulation.
In adults, vitamin D deficiency leads to a mineralization
defect in the skeleton causing osteomalacia. In addition,
the secondary hyperparathyroidism associated with vitamin D deficiency enhances mobilization of calcium from
the skeleton, resulting in porotic bone and increasing
fracture risk. Although no minimum daily dietary intake
of vitamin D has been identified, for adults exposed to
ample sunlight less than 2.0g/day (that is 80 units/day)
of dietary intake is associated with its overt deficiency in
adults. The US National Academy of Science sets a recommended daily allowance for vitamin D as 15g/day
(that is 600 units/day) for people below 70 years, and for
people older than 70 years as 20g/day (that is 800
units/day). Sun exposure and use of fortified or enriched
* Correspondence: dranilarora50@gmail.com
Department of Gastroenterology & Hepatology, Sir Ganga Ram Hospital,
Rajinder Nagar, New Delhi 110 060, India
foods are the methods by which mild vitamin D deficiency can be corrected. Moderate to severe vitamin D
deficiency can be treated by oral administration of
pharmacological dose of vitamin D 50,000IU/week for 6
to 8 weeks [1]. Due to a wide therapeutic index, vitamin
D toxicity is extremely rare; however, it does occur at excessively high doses.
We present here a classic case of iatrogenic hypervitaminosis D, which presented with persistent vomiting
and acute renal failure.
Case presentation
A 45-year-old Asian Indian woman was admitted to our
hospital with a history of recurrent vomiting, pain in her
abdomen, polydipsia, anorexia and constipation for 1.5
months. There was no history of fever, altered sensorium, headache, cough, shortness of breath, or urinary
symptoms. She had been hypertensive for the past year;
2 months ago she underwent arthroscopic repair of her
right knee cruciate ligament.
On physical examination, she was conscious and oriented. Pallor was present; icterus and edema were absent.
Her vitals were: blood pressure 140/100mmHg, pulse 84/
minute, respiratory rate 20/minute, and temperature 37.6C.
2014 Bansal et al.; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative
Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and
reproduction in any medium, provided the original work is properly credited.
Bansal et al. Journal of Medical Case Reports 2014, 8:74
http://www.jmedicalcasereports.com/content/8/1/74
An abdominal examination revealed no abnormalities.
The results of her chest and cardiovascular examinations
were also normal. An examination of her central nervous
system showed generalized muscle weakness without any
focal neurological deficit. Her deep tendon reflexes were
normal.
On laboratory investigation the following results were
obtained: hemoglobin 9.2g/dL, white blood cell count
12.2103/mm3, platelet count 242103/mL, blood urea
nitrogen (BUN) 57mg/dL, creatinine 4.1mg/dL, sodium
139mEq/L, potassium 3.7mEq/L, serum calcium 11.54mEq/L,
phosphorous 2.8mEq/L, serum bilirubin 0.60mg/dL,
protein 6.3g/dL, albumin 3.6g/dL, globulin 2.7g/dL, alanine transaminase 22IU/L, aspartate transaminase 20IU/L,
alkaline phosphatase 22IU/L, and erythrocyte sedimentation rate 76mm. The result of her Mantoux test was negative, her angiotensin-converting enzyme was 18.20mg/dL
and her parathyroid hormone was 11.60pg/mL. The reference ranges of our lab for analytes are given in Table 1.
Her urine analysis and microscopy were normal. Her urine
for Bence Jones protein was negative. Protein electrophoresis did not reveal any monoclonal bands. Her chest X-ray
was normal and her electrocardiogram showed lowvoltage complexes. An ultrasound of her abdomen was
normal. An ultrasound of her neck did not reveal any
parathyroid mass. High-resolution computed tomography
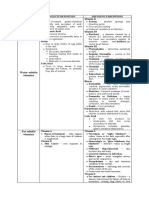
Table 1 Reference ranges for analytes
Hb
1315g/dL
WBC
400010,000 per mm3
Platelet count
150400103/mL
BUN
523mg/dL
Creatinine
0.61.3mg/dL
Sodium
132148mEq/L
Potassium
3.55.5mEq/L
Calcium
8.210.4mg/dL
Phosphorous
2.8mg/dL
Serum bilirubin
0.21mg/dL
Protein
6.68.7g/dL
Albumin
3.55g/dL
Globulin
1.53.5g/dL
ALT
060IU/L
AST
040IU/L
ALP
39117IU/L
ESR
010mm after end of first hour
ACE
<40mg/dL
PTH
1264pg/mL
Abbreviations: ACE, angiotensin-converting enzyme; ALP, alkaline phosphatase;
ALT, alanine transaminase; AST, aspartate transaminase; BUN, blood urea
nitrogen; ESR, erythrocyte sedimentation rate; Hb, hemoglobin; PTH, parathyroid
hormone; WBC, white blood cell count.
Page 2 of 4
of her chest and magnetic resonance imaging of her brain
were also essentially normal.
Hence the biochemical evaluation revealed only raised
BUN and serum creatinine suggesting acute renal failure
with hypercalcemia, in the absence of evidence of
chronic kidney disease, multiple myeloma or hyperparathyroidism. A detailed history of previous treatment revealed that she had received an injection of Arachitol
(vitamin D3) 600,000IU intramuscularly, every alternate
day for 10 doses just after her knee surgery 2 months
back. We found her serum 25-hydroxyvitamin D (25
(OH)D) level to be 150ng/mL which was in the toxic
range (normal 20 to 30ng/mL). So a diagnosis of vitamin
D toxicity-induced acute kidney injury and hypercalcemia was established. To rule out chronic kidney disease
a nephrology consultation was sought and ultrasound
for her kidneys and routine urine microscopy were ordered, which were normal.
For hypercalcemia, she was treated with intravenous
fluid, diuretics and calcitonin and had clinical improvement. Her serum calcium and creatinine levels were
monitored regularly; they gradually declined to normal
levels in the next 15 days. She was discharged with a prescription of an antihypertensive and calcium-restricted
diet along with good hydration; she is doing well.
Discussion
In this case report a classic case of iatrogenic hypervitaminosis D, which presented with persistent vomiting
and acute renal failure, has been described. Hypervitaminosis D can occur when pharmaceutical vitamin D is
taken in excess, as in our case. The manifestation could
be related to hypercalcemia, or acute kidney injury, or
both as in our case [2].
The biologically active metabolite of vitamin D, 1,25dihydroxyvitamin D(3), affects mineral homeostasis and
has numerous other diverse physiologic functions including effects on growth of cancer cells and protection
against some immune disorders [3]. Adequate vitamin D
status has been linked to decreased risks of developing
specific cancers, including cancers of the esophagus,
stomach, colon, rectum, gallbladder, pancreas, lung,
breast, uterus, ovary, prostate, urinary bladder, kidney,
skin, thyroid, and hematopoietic system (for example,
Hodgkins lymphoma, non-Hodgkins lymphoma, multiple myeloma); bacterial infections; rheumatoid arthritis;
Crohns disease; periodontal disease; multiple sclerosis;
asthma; type 2 diabetes; cardiovascular disease; stroke;
peripheral artery disease; hypertension; chronic kidney disease; muscle weakness; cognitive impairment; Alzheimers
disease; clinical depression; and premature death [4].
Whereas inadequate vitamin D status during human pregnancy may be associated with increased risk for the development of type 1 diabetes in the offspring [4].
Bansal et al. Journal of Medical Case Reports 2014, 8:74
http://www.jmedicalcasereports.com/content/8/1/74
Vitamin D deficiency can be treated by oral administration of a pharmacological dose of vitamin D
50,000IU/week for 6 to 8 weeks [1]. Even though vitamin
D toxicity is extremely rare, due to the wide therapeutic
index, it does occur at excessively high doses. The guidelines of the Food and Nutrition Board of the USA specify 2000IU as the highest vitamin D intake that healthy
adults can consume daily without risk of hypercalcemia
[5]. However, these patients should be monitored by
periodic estimation of 24-hour urinary calcium excretion, which should not exceed 250mg. Very little is
known about the mechanism of vitamin D toxicity [6].
The lipophilic nature of vitamin D explains its adipose
tissue distribution and its slow turnover in the body
(half-life approximately 2 months), whereas its main
transported metabolite, 25-hydroxyvitamin D(3) (25
(OH)D(3)), has a half-life of approximately 15 days. Animal experiments involving vitamin D3 intoxication have
established that 25(OH)D(3) can reach concentrations
up to 2.5micromol/L, at which it is accompanied by hypercalcemia and other pathological sequelae resulting
from a high calcium/phosphate product [6]. Although
current data support the viewpoint that the biomarker
plasma 25(OH)D concentration must rise above
750nmol/L to produce vitamin D toxicity, the more prudent upper limit of 250nmol/L might be retained to ensure a wide safety margin. There also is evidence that
despite the current heavy reliance on serum 25(OH)D(3)
concentration for the diagnosis of an individuals vitamin
D status, local tissue vitamin D intoxication may be
present in individuals with much lower serum 25(OH)D
(3) concentrations than are currently appreciated [6].
Only rarely are the symptoms of local tissue vitamin D
intoxication associated with vitamin D status or intake.
An individuals serum 25(OH)D(3) concentration may
appear to be low for reasons totally independent of
sunlight exposure or vitamin D intake. Serum 25(OH)D
(3) concentration is only poorly responsive to increases
in vitamin D intake, and the prolonged routine consumption of thousands of international units of vitamin
D may interfere with the regulation of phosphate
homeostasis by fibroblast growth factor-23 and the
Klotho gene product, with consequences that are detrimental to human health [6].
Clinical manifestations of vitamin D toxicity include:
hypercalcemia, hypercalciuria, kidney stones, hyperphosphatemia, polyuria, polydipsia, ectopic calcification of
soft tissues (kidney and lung), nausea, vomiting, anorexia, constipation, headache, and hypertension [7,8].
In a recent paper Pandita et al. [9] reported a case series
of 15 patients (most of them elderly) with iatrogenic
symptomatic hypercalcemia in whom toxicity occurred
due to empirical excessive administration of vitamin D
by oral and parenteral route. To prevent iatrogenic
Page 3 of 4
vitamin D toxicity the authors suggested that awareness
should be increased among healthcare providers regarding the toxic potential of mega doses of vitamin D, despite its wide margin of safety [9]. In another case series
by Koul et al. [10] 10 cases of hypercalcemia due to vitamin D intoxication were reported with features of
vomiting, polyuria, polydipsia, encephalopathy and renal
dysfunction. All the patients had demonstrable hypercalcemia and vitamin D levels were high in nine of the 10
cases. The patients had received high doses of vitamin D
and no other cause of hypercalcemia was identified.
Treatment of hypercalcemia resulted in clinical recovery
in nine cases [10].
Conclusions
Thus we conclude that if a patient presents with persistent vomiting and hypercalcemia particularly in the presence of normal parathyroid hormone, then a diagnosis
of overdose of vitamin D should be suspected because
its correction not only alleviates symptoms but can also
prevent acute kidney injury.
Consent
Written informed consent was obtained from the patient
for publication of this manuscript and accompanying
images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Abbreviations
25(OH)D: 25-hydroxyvitamin D; 25(OH)D(3): 25-hydroxyvitamin D(3);
BUN: Blood urea nitrogen.
Competing interests
The authors declare that they have no competing interests.
Authors contributions
RKB was the resident in charge of the case and was a major contributor in
writing the initial draft of the manuscript. PT, PS, VS, NB, VA and AK
contributed in writing and editing the manuscript. NB was the attending
physician in charge of the case and was responsible for sections on the
diagnosis and management of the patient. AA was the unit head and was
responsible for management of the patient and supervised and edited the
case report. All authors read and approved the final manuscript.
Received: 22 April 2013 Accepted: 16 December 2013
Published: 26 February 2014
References
1. Robert MR, Paolo MS: Vitamin and trace mineral deficiency and excess. In
Harrisons Principles of Internal Medicine, Volume 1. 18th edition. Edited by
Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J. New
York: Mc Graw Hill; 2012:594605.
2. Hathcoch JN, Glao A, Vieth R, Haeny R: Risk assessment for vitamin D.
Am J Clin Nutr 2007, 85:618.
3. Christakos S, Ajibade DV, Dhawan P, Fechner AJ, Mady LJ: Vitamin D:
metabolism. Endocrinol Metab Clin North Am 2010, 39(2):243253.
4. Glade MJ: Vitamin D: health panacea or false prophet? Nutrition 2013,
29(1):3741.
5. John TP Jr, Harald J: Disorders of the parathyroid gland and calcium
homeostasis. In Harrisons Principles of Internal Medicine, Volume 2. 18th
edition. Edited by Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL,
Loscalzo J. New York: Mc Graw Hill; 2012:30963120.
Bansal et al. Journal of Medical Case Reports 2014, 8:74
http://www.jmedicalcasereports.com/content/8/1/74
Page 4 of 4
6.
Jones G: Pharmacokinetics of vitamin D toxicity. Am J Clin Nutr 2008,
88(2):582S586S.
7. Bouillon R: Vitamin D: from photosynthesis, metabolism, and action to
clinical application. In Endocrinology. 6th edition. Edited by DeGroot LJ,
Jameson JL. Philadelphia: WB Saunders; 2010:10891110.
8. Maji D: Vitamin D toxicity. Indian J Endocrinol Metab 2012, 16(2):295296.
9. Pandita KK, Razdan S, Kudyar RP, Beigh A, Kuchay S, Banday T: Excess good
can be dangerous. A case series of iatrogenic symptomatic
hypercalcemia due to hypervitaminosis D. Clin Cases Miner Bone Metab
2012, 9(2):118120.
10. Koul PA, Ahmad SH, Ahmad F, Jan RA, Shah SU, Khan UH: Vitamin d
toxicity in adults: a case series from an area with endemic
hypovitaminosis d. Oman Med J 2011, 26(3):201204.
doi:10.1186/1752-1947-8-74
Cite this article as: Bansal et al.: Iatrogenic hypervitaminosis D as an
unusual cause of persistent vomiting: a case report. Journal of Medical
Case Reports 2014 8:74.
Submit your next manuscript to BioMed Central
and take full advantage of:
Convenient online submission
Thorough peer review
No space constraints or color gure charges
Immediate publication on acceptance
Inclusion in PubMed, CAS, Scopus and Google Scholar
Research which is freely available for redistribution
Submit your manuscript at
www.biomedcentral.com/submit
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Tacfit Survival - Bonus1 28 Days PrimalДокумент17 страницTacfit Survival - Bonus1 28 Days Primalimre100% (1)
- Micronutrients in Hair LossДокумент9 страницMicronutrients in Hair LossIkbal Adi SaputraОценок пока нет
- HowtogrowtallerДокумент30 страницHowtogrowtallerPhu TRANОценок пока нет
- Medical Nutrition Therapy For Hemodialysis PatientsДокумент24 страницыMedical Nutrition Therapy For Hemodialysis Patientsraquelt_65Оценок пока нет
- Latihan Penilaian Harian 3Документ2 страницыLatihan Penilaian Harian 3FEBRIAN RISQI FIRMANSYAHОценок пока нет
- Vitamins All AboutДокумент31 страницаVitamins All Aboutvu aneelaОценок пока нет
- Passmedicine MRCP Notes-NephrologyДокумент73 страницыPassmedicine MRCP Notes-Nephrologysalwabeshir542Оценок пока нет
- Vitamins & Minerals: Name: - DateДокумент1 страницаVitamins & Minerals: Name: - DateWiktoria StahlОценок пока нет
- Biochemical Assessment of Vitamin DДокумент24 страницыBiochemical Assessment of Vitamin DKarunya VkОценок пока нет
- Dietary Recommendations For Toddlers, Preschool, and School-Age Children - UpToDateДокумент39 страницDietary Recommendations For Toddlers, Preschool, and School-Age Children - UpToDateĐỗ Trần Giang SơnОценок пока нет
- Abstracts On NDDSДокумент55 страницAbstracts On NDDSprasanthiОценок пока нет
- Instruction: Read The Instructions Carefully and Answer Directly To The Test QuestionnaireДокумент6 страницInstruction: Read The Instructions Carefully and Answer Directly To The Test QuestionnaireMenoj SantuyoОценок пока нет
- Water Soluble Vitamins: Vitamins Toxicity/Definition Deficiency/Definition Niacin Vitamin AДокумент3 страницыWater Soluble Vitamins: Vitamins Toxicity/Definition Deficiency/Definition Niacin Vitamin ARoshin TejeroОценок пока нет
- CHEM216 Research 8Документ5 страницCHEM216 Research 8Theo Vito PradipaОценок пока нет
- Practice 1 m12 Đã G PДокумент22 страницыPractice 1 m12 Đã G PAnh ThưОценок пока нет
- Chapter 11 - Nutrition Through The Life Span: Pregnancy and LactationДокумент12 страницChapter 11 - Nutrition Through The Life Span: Pregnancy and LactationMario MagtakaОценок пока нет
- Southern Derbyshire Share Vitamin D March 2012Документ7 страницSouthern Derbyshire Share Vitamin D March 2012dr rashid khanОценок пока нет
- Presentation DДокумент18 страницPresentation DGauravPathaniaОценок пока нет
- 11 2016 Prevention and Treatment of Vitamin D and Calcium Deficiency inДокумент7 страниц11 2016 Prevention and Treatment of Vitamin D and Calcium Deficiency insheyla alegreОценок пока нет
- Easy To ReadДокумент73 страницыEasy To Readdaljit chahalОценок пока нет
- Nutritional Considerations For Healthy Aging and Reduction in Age-Related Chronic DiseaseДокумент10 страницNutritional Considerations For Healthy Aging and Reduction in Age-Related Chronic DiseaseSilvana RamosОценок пока нет
- Society Achievers April 2023Документ108 страницSociety Achievers April 2023magnatepublishingpvtltdОценок пока нет
- The Skincarefalsepdf PDFДокумент8 страницThe Skincarefalsepdf PDFTeraОценок пока нет
- Everyday ScienceДокумент117 страницEveryday ScienceFawad Hayat MohmandОценок пока нет
- Skripsi Jonathan Darell Widjaja 1206230025Документ41 страницаSkripsi Jonathan Darell Widjaja 1206230025Jonathan Darell WijayaОценок пока нет
- Suplements in RehabДокумент20 страницSuplements in RehabpetrОценок пока нет
- 100 Passage Based Biology QuestionsДокумент17 страниц100 Passage Based Biology QuestionsMahmoud EbaidОценок пока нет
- Community Medicine Solved BCQs 8th Semester MBBS LUMHS-1Документ27 страницCommunity Medicine Solved BCQs 8th Semester MBBS LUMHS-1rameez ahmedОценок пока нет
- Vasvi and Vardah CC Report (1) .DocxkkkkkkkДокумент35 страницVasvi and Vardah CC Report (1) .Docxkkkkkkk9810102550aОценок пока нет