Академический Документы
Профессиональный Документы
Культура Документы
Neoreviews 2015 Mukhopadhyay E221 30
Загружено:
Sleepy WinterОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Neoreviews 2015 Mukhopadhyay E221 30
Загружено:
Sleepy WinterАвторское право:
Доступные форматы
Article
infectious diseases
Neonatal Early-Onset Sepsis: Epidemiology and Risk
Assessment
Sagori Mukhopadhyay,
MD, MMSc, Karen
M. Puopolo, MD, PhD
Author Disclosure
Drs Mukhopadhyay
and Puopolo have
disclosed no financial
relationships relevant
to this article. This
commentary does not
contain a discussion of
an unapproved/
investigative use of
a commercial product/
Educational Gap
There is a need for increased understanding of methods of risk assessment for neonatal
early-onset sepsis.
Abstract
Neonatal early-onset sepsis (EOS) continues to be a signicant source of morbidity
and mortality among newborns, especially among very low-birth-weight infants. Epidemiologic risk factors for EOS have been dened, and considerable resources are devoted to the identication and evaluation of infants at risk for EOS. The widespread
implementation of intrapartum antibiotic prophylaxis for the prevention of early-onset
neonatal group B streptococcal disease has reduced the overall incidence of neonatal
EOS and inuenced the microbiology of persistent early-onset infection. Recommendations for perinatal risk factorbased evaluation and empiric antibiotics treatment of
neonates result in a large proportion of uninfected infants undergoing medical intervention, including antibiotic therapy. Objective risk assessment tools have been developed that may allow safe restriction of medical intervention in uninfected newborns,
promote antibiotic stewardship, and optimize resource use.
device.
Objectives
After completing this article, readers should be able to:
1. Describe the incidence and pathogenesis of neonatal early-onset sepsis.
2. Understand the host, pathogen, and environmental mediators of neonatal early-onset
sepsis epidemiology.
3. Review the effect of group B Streptococcus prophylaxis policies on the epidemiology
of neonatal early-onset sepsis.
4. Understand the need for and methods of risk assessment in approaching neonatal
early-onset sepsis.
Introduction
Bacterial sepsis and meningitis continue to be major causes of morbidity and mortality in
newborns, particularly in very low-birth-weight (VLBW) infants (birth weight <1,500 g).
(1)(2) Neonatal early-onset sepsis (EOS) is dened by the Centers for Disease Control and
Prevention (CDC) as blood and/or cerebrospinal uid cultureproven infection occurring
in the newborn at less than 7 days of age. (3) For the continuously hospitalized VLBW
infant, EOS is dened as culture-proven infection occurring at less than 72 hours of
age. (2) The alternative denition in VLBW infants is justied by 2 ndings: (1) the risks
of infection in VLBW infants after age 72 hours primarily derive from the specics of ongoing neonatal intensive care rather than from perinatal risk factors, and (2) the organisms
that cause infection after age 72 hours among VLBW infants reect the nosocomial ora of
the neonatal intensive care unit (NICU) more than perinatally acquired maternal ora.
Epidemiology of Neonatal EOS
The overall incidence of EOS in the United States is estimated to be 0.77 case per 1,000
live births (95% condence interval, 0.720.84) by Weston et al (2) in a population-based
study using data from 2005 to 2008. A slightly higher rate of 0.98 per 1,000 live births
Childrens Hospital of Philadelphia Newborn Care at Pennsylvania Hospital, Philadelphia, PA.
NeoReviews Vol.16 No.4 April 2015 e221
Downloaded from http://neoreviews.aappublications.org/ at Indonesia:AAP Sponsored on September 22, 2015
infectious diseases / early-onset sepsis
(range, 0.332.44 across centers) was reported by Stoll
et al (1) in a study of more than 390,000 live birth deliveries between 2006 and 2009 at 16 university-based
neonatal centers in the United States that constituted
the Neonatal Research Network (NRN). Incidence is
strongly inuenced by gestational age at birth. Among infants born at 37 weeks gestation or more in 16 centers in
California and Massachusetts, the incidence was only
0.53 per 1,000 live births. (4) In contrast, among the preterm population (<37 weeks gestation at birth), the incidence of EOS is approximately 7 times higher at 3.71
per 1,000 live births and 20 times higher among the
VLBW infants at 10.96 per 1,000 live births. (1)(2) Case
fatality rates range from 11% to 16%, with more than 90%
of the deaths occurring among the preterm population.
These ndings translate to approximately 3,300 newborns affected and more than 340 deaths annually in
the United States. (1)(2)
Group B Streptococcus (GBS) emerged as the leading
cause of EOS in the 1970s and continues to remain so
among the term population, accounting for approximately
40% of EOS cases. Its absolute national incidence, however, has decreased substantially by 87% (1.8 cases per
1,000 live births in 1990 to 0.24 case per 1,000 live births
in 2013) with the widespread implementation of intrapartum antibiotic prophylaxis (IAP) for the prevention of
early-onset GBS disease. (5)(6) Coincident with the increased use of IAP for GBS, gram-negative enteric bacteria
(primarily Escherichia coli) have become the leading cause
of EOS in preterm infants. (2)(7)(8) E coli accounts for
more than 38% of EOS cases affecting preterm infants
(Table 1). The remaining organisms causing EOS are
listed in Table 1; similar results are observed both within
NRN centers and at a single large maternity center. Most
of the organisms in Table 1 normally colonize the maternal
gastrointestinal and genitourinary tract. The pathogenesis
of EOS is that of ascending colonization of the fetal
compartment through ruptured and less frequently intact
amniotic membranes. This can result in intra-amniotic infection or colonization of the infant during the process of
delivery, leading to invasive infection soon thereafter. EOS
caused by Listeria monocytogenes is a notable exception;
Listeria EOS occurs via hematogenous spread of the organism across the placenta (see below).
capsular polysaccharide serotypes (types Ia, Ib, and II
IX). Most GBS EOS in the United States is currently
caused by types Ia, Ib, II, III, and V GBS. (3) Type III
GBS is more commonly associated with late-onset sepsis
and meningitis. Early-onset GBS infection is acquired
via colonization of the infant in utero or during passage
through the birth canal. Approximately 20% to 30% of
US women are colonized with GBS at any given time, although a longitudinal study of GBS colonization in a cohort of primarily young, sexually active women found that
nearly 60% of women are colonized with GBS at some
point during a 12-month period. (9)(10) In the absence
of IAP, approximately 50% of infants born to mothers colonized with GBS are colonized at birth, and 1% to 2% of
colonized infants develop invasive GBS disease. (5) Lack of
maternally derived, protective capsular, polysaccharidespecic antibody is associated with the development of
invasive GBS disease. Other factors that predispose the newborn to GBS disease are less well understood, but relative
deciencies in complement, neutrophil function, and innate
immunity may be important.
Clinical Factors Associated With GBS EOS
A number of studies helped dene maternal and neonatal
factors that are associated with an increased risk of GBS
and bacterial all-cause EOS (Table 2). Benitz et al (11)
performed a literature review and data reanalysis of studies performed in the 1970s to the 1990s, demonstrating
that maternal GBS colonization alone was by far the greatest predictor of GBS-specic EOS. Because only a few
pregnant women are colonized with GBS, the recognition
of the importance of colonization alone provides the basis
for the current recommendation for use of IAP based on
maternal GBS colonization status. GBS bacteriuria during
pregnancy is associated with heavy colonization of the rectovaginal tract and is considered a signicant risk factor for
EOS. Black infants in the United States have a higher burden of GBS EOS that is not fully explained by colonization
rates among black women, suggesting there may be socioeconomic mediators of EOS. The most recent CDC surveillance data indicate twice the incidence of neonatal GBS
EOS among black infants compared with white infants. (6)
Additional maternal clinical factors predictive of early-onset GBS disease are listed in Table 2.
EOS Caused by GBS
GBS frequently colonizes the human genital and gastrointestinal tracts and the upper respiratory tract in young infants. GBS organisms are facultative diplococci that are
primarily identied by the Lanceeld group B carbohydrate antigen. They are further subtyped into 10 distinct
Evolution of Guidelines for IAP for the
Prevention of Early-Onset GBS Infection
With the recognition that maternal colonization with GBS
was the greatest risk factor for neonatal GBS disease, multiple trials found that the use of intrapartum penicillin or
e222 NeoReviews Vol.16 No.4 April 2015
Downloaded from http://neoreviews.aappublications.org/ at Indonesia:AAP Sponsored on September 22, 2015
infectious diseases / early-onset sepsis
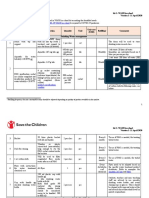
Table 1.
Organisms That Cause Neonatal Early-Onset Sepsis
No. (%) of Organisms
Organism
NICHD (n [ 370)
BWH (n[335)
GBS
Escherichia coli
Other streptococcia
Enterococcus
Staphylococcus aureus
Coagulase-negative Staphylococcus
Listeria
Bacteroides species
Klebsiella
Hemophili
Other gram-negative organismsb
Otherc
Fungi
Total gram positive
Total gram negative
159
107
39
10
9
3
2
3
1
11
15
9
2
231
137
139
71
39
13
13
14
2
15
4
6
8
8
3
228
104
(43.0)
(28.9)
(10.5)
(2.7)
(2.4)
(0.8)
(0.5)
(0.8)
(0.3)
(3.0)
(4.1)
(2.4)
(0.5)
(62.4)
(37.0)
(41.5)
(20.2)
(11.6)
(3.9)
(3.8)
(4.2)
(0.6)
(4.5)
(1.2)
(1.9)
(2.6)
(2.4)
(0.9)
(68.1)
(31.0)
The BWH data are from all early-onset sepsis cases among infants born in a single center for the period 1990 to 2007. The NICHD data are from all earlyonset sepsis cases among multiple centers from 2006 to 2009.
BWHBrigham and Womens Hospital; GBSgroup B Streptococcus; NICHDEunice Kennedy Shriver National Institute of Child Health and Human
Development.
a
Other streptococci include Streptococcus pneumoniae, Streptococcus bovis, Streptococcus mitis, Peptostreptococcus, group D Streptococcus, a-hemolytic
streptococcus, Streptococcus morbillorum, Streptococcus mutans, Streptococcus oralis, Streptococcus pneumoniae, Streptococcus salivarius, Streptococcus sanguinis,
and viridans streptococci.
b
Other gram-negative organisms include Enterobacter, Citrobacter, Acinetobacter, Pseudomonas, Proteus, Brevundimonas vesicularis, Moraxella species,
Capnocytophaga species, Morganella species, and Yersinia.
c
Other organisms include Bacillus, Actinomyces odontolyticus, gram positive not specied, and Clostridium.
Adapted from Stoll et al (1) and Puopolo and Eichenwald (8).
ampicillin signicantly reduces the rate of neonatal colonization with GBS and the incidence of early-onset GBS disease. The efcacy of IAP was most substantially revealed in
a trial of only 160 women in 1986. (12) IAP for the prevention of GBS EOS can be administered to pregnant
women during labor based on (1) specic clinical risk factors for early-onset GBS infection or (2) the results of
antepartum screening of pregnant women for GBS colonization. The CDC has published consensus guidelines that
endorsed the use of IAP for prevention of neonatal GBS
disease, rst in 1996 and subsequently in revised form
in 2002 and 2010 recommending universal GBS screening
among pregnant women. (5)(13)(14) Risk factors to consider include maternal GBS colonization status determined
at 35 to 37 weeks gestation, documented GBS bacteriuria
during pregnancy, prior delivery of an infant with GBS disease, preterm labor, unknown GBS status combined with
an intrapartum temperature of 100.4F (38C), or duration of rupture of membranes of 18 hours or longer. Adequate IAP was dened as the administration of one of the
endorsed antibiotics 4 or more hours before delivery. The
most current version also endorses intrapartum use of nucleic acid amplication tests (NAATs) as an acceptable
alternative if culture-based screening results are not available.
The 2010 CDC statement also contains recommendations for the evaluation of infants at risk for both GBSspecic and all-cause EOS. Evaluation of infants with
clinical signs of sepsis and those born to mothers with
chorioamnionitis is recommended. In a change from prior
statements, the latest version recommends evaluation of
infants born in the setting of inadequately indicated
GBS IAP only with the additional risk factors of birth at
less than 37 weeks gestation or duration of rupture of
membranes of 18 hours or longer. The revised guidelines
can be accessed at http://www.cdc.gov/mmwr/pdf/rr/
rr5910.pdf. With widespread implementation of the CDC
recommendations, the provisional national GBS-specic
EOS incidence for 2013 is estimated at 0.24 per 1,000 live
births (approximately 950 cases per year) with a persistent
gap in the incidence among white population (0.21 per
1,000 US live births) compared with the black population
(0.44 per 1,000 US live births). (6)(14) Most GBS EOS
among term infants now occurs in mothers who have
screened negative for GBS colonization. (15)(16)(17)
There is a low incidence (approximately 4%) of nonconcordance between results of maternal GBS screening
NeoReviews Vol.16 No.4 April 2015 e223
Downloaded from http://neoreviews.aappublications.org/ at Indonesia:AAP Sponsored on September 22, 2015
infectious diseases / early-onset sepsis
Table 2.
Risk Factors for Early-Onset Sepsis
Study
Study Specifics
Benitz et al, 1999
Pre-IAP era
GBS early-onset sepsis only
All newborns
Escobar et al, 2000
Schrag et al, 2003
Puopolo et al,b 2010
Post-IAP era
BW of 2,000 g
N[2,785 infants, including
62 cases
Post-IAP
Escherichia coli early-onset
sepsis only
All newborns
N[ 132 cases, 1,212 controls
Post-IAP
34 weeks gestation
N[350 cases, 1,063 controls
Risk Factors
Odds Ratio (95% CI)a
204 (100419)
Maternal GBS colonization
BW <1,000 g
BW <2,500 g
ROM >18 hours
Chorioamnionitis
Intrapartum fever >99.5F
(>37.5C)
Model 1: No IAP (N[ 1,568)
Temperature 101.5F (38.6C)
ROM 12 hours
Low ANC for age
Infant asymptomatic
Meconium in amniotic fluid
Model 2: Received IAP (N [ 1,217)
Fever 101.5C (38.6C)
Low ANC for age
Infant asymptomatic
Intrapartum fever
PROM
GA 33 weeks
GA 3436 weeks
GA (per day)
GBS status
Positive
Unknown
Duration of ROM (per hour)
Highest intrapartum temperature
(per degrees Celsius)
GBS IAP given on time or any
antibiotic given <4 hours
Broad-spectrum antibiotic
given >4 hours
24.8
7.37
7.28
6.42
4.05
(12.250.2)
(4.4812.1)
(4.4212.0)
(2.3217.8)
(2.177.56)
5.78
2.05
2.82
0.27
2.24
(1.5721.29)
(1.063.96)
(1.505.34)
(0.110.65)
(1.194.22)
3.50
3.60
0.42
6.6
(1.309.42)
(1.458.96)
(0.161.11)
(3.313.2)
3.5
26.5
5.3
0.001
1.78
1.04
3.41
2.38
(2.15.8)
(15.046.8)
(3.09.7)
(0.00010.014)
(1.112.85)
(0.761.44)
(2.235.20)
(2.052.77)
0.35 (0.230.53)
0.31 (0.130.71)
ANCabsolute neutrophil count; BWbody weight; CIcondence interval; GAgestational age; GBSgroup B Streptococcus; IAPintrapartum antibiotic
prophylaxis; PROMpremature rupture of membranes; ROMrupture of membranes.
a
Benitz et al reported unadjusted odds ratios, whereas the other 3 studies reported adjusted odds ratios.
b
Model also included a gestational age squared (adjusted odds ratio, 1.09; 95% CI, 1.051.13).
performed at 35 to 37 weeks gestation and repeat screening on presentation for delivery at term, which may account for many cases of persistent GBS EOS. (18) Use
of NAATs for intrapartum GBS detection where available
may facilitate identication among mothers with onset of
labor before 35 to 37 weeks gestation or with missed
screening results. The clinical efcacy and cost-effectiveness
of an approach that uses NAATs at the time of presentation for delivery to rescreen GBS-negative mothers remain
to be determined. Ultimately, the development of effective
GBS vaccines may be needed to eliminate GBS-specic
EOS entirely.
e224 NeoReviews Vol.16 No.4 April 2015
Downloaded from http://neoreviews.aappublications.org/ at Indonesia:AAP Sponsored on September 22, 2015
infectious diseases / early-onset sepsis
Epidemiology of E coli EOS
E coli is the second most common organism that causes
EOS in all neonates and the single most common EOS
organism in VLBW infants. (1)(2) E coli are facultative,
anaerobic, gram-negative rods found universally in the
human intestinal tract and commonly in the human vagina and urinary tract. There are hundreds of different
antigenic types of E coli, but EOS E coli infections, particularly those complicated by meningitis, are primarily
due to strains with the K1-type polysaccharide capsule.
With the implementation of IAP against GBS, concern
has been raised regarding increasing incidence of E coli
specic EOS and particularly ampicillin-resistant EOS.
Multiple single-center and multicenter studies have produced conicting results. One analysis of 23 reports of
EOS in the era of GBS prophylaxis concluded that there
is no evidence of an increase in the absolute incidence of
non-GBS EOS among term infants. (19) Data from the
Eunice Kennedy Shriver National Institute of Child
Health and Human Development NRN indicate an overall decrease in the incidence of EOS among VLBW infants (from 19.3 per 1,000 VLBW births in 19911993
to 11.0 per 1,000 VLBW births in 20062009). (1)(7)(20)
However, an absolute increase in the incidence of
E colispecic EOS has been documented since 1991
to 1993. An increase in non-GBS EOS in VLBW infants
has also been reported by single centers. (21) In addition,
with a decrease in GBS-specic EOS among VLBW infants, an increasing proportion of VLBW EOS is due to
E coli, much of which is ampicillin-resistant E coli. In contrast, absolute increases in E coli and/or ampicillin-resistant
EOS among term infants have not been found in casecontrol studies conducted by the CDC or in a singlecenter study analyzing EOS during an 18-year period
in a large birth center in Boston. (8)(22) Clinicians caring
for both premature and term infants must be aware, however, that with decreases in GBS-specic EOS, a signicant proportion of any EOS that occurs will be due to an
ampicillin-resistant gram-negative organism. In clinical situations where a critically ill infant has a high likelihood of
EOS, empiric antibiotic coverage for ampicillin-resistant
gram-negative organisms is warranted until blood culture
results are known.
Other Organisms Responsible for EOS
In addition to GBS and E coli, there are a number of
pathogens that cause EOS in the United States that deserve special note. L monocytogenes are gram-positive,
b-hemolytic, motile bacteria that most commonly infect
humans via the ingestion of contaminated food. An association with prepared foods held at moderate temperature
(particularly cheeses and deli meats) has been documented, occasionally in epidemic outbreaks. These bacteria do not cause signicant disease in immunocompetent
adults but can cause severe illness in pregnant women
and their fetuses and in newborns. The true incidence of
listeriosis in pregnancy is difcult to determine because
many cases are undiagnosed when they result in spontaneous abortion of the previable fetus. Obligate anaerobic
bacteria (primarily the encapsulated enteric organism Bacteroides fragilis) can cause neonatal EOS and justify the use
of both aerobic and anaerobic blood culture bottles in the
evaluation of EOS. Although methicillin-sensitive Staphylococcus aureus and methicillin-resistant S aureus cause
a large proportion of hospital-acquired infection in VLBW
infants and are increasing issues in community-acquired
pediatric infections, these remain rare causes of neonatal
EOS. A recent study of 5,732 pregnant women documented a 3.5% incidence of MRSA in GBS rectovaginal
screening cultures but found no cases of MRSA neonatal
EOS in delivered infants. (23) Finally, fungal organisms
(primarily Candida species) rarely cause neonatal EOS.
Fungal EOS is largely found in preterm and VLBW infants,
often associated with very prolonged antibiotic (>24 hours)
exposure of pregnant mothers before delivery.
Approaching the Risk of EOS
The goal of clinical risk assessment in EOS is to use ndings from validated research studies to identify high-risk
newborns and subsequently prevent the onset and/or
progression of the disease. Current approaches use algorithms to identify the highest-risk infants, followed by
medical examination and diagnostic evaluations, with
or without administration of empiric antibiotics pending
laboratory tests (or clinical status). Recommendations are
published by the CDC and the American Academy of Pediatrics for term and preterm infants to evaluate risk of
EOS. (14)(24)(25) Although some minor details differ,
the principles include consideration of the following:
1. Perinatal risk factors. These risk factors participate in
disease pathogenesis or susceptibility (eg, maternal
GBS colonization, prolonged duration of membrane
rupture, maternal fever, and gestational age) (Table 2).
2. Clinical status of the newborn. A total of 60% to 90%
of EOS cases, depending on the population studied,
will become symptomatic in the rst 24 to 48 hours.
(26)(27) Asymptomatic status is associated with decreased risk. (26)(28)
3. Laboratory results. The most commonly used laboratory diagnostics are complete blood cell count (with
components of the white blood cell differential),
NeoReviews Vol.16 No.4 April 2015 e225
Downloaded from http://neoreviews.aappublications.org/ at Indonesia:AAP Sponsored on September 22, 2015
infectious diseases / early-onset sepsis
C-reactive protein, and blood cultures. A variety of biomarkers are subject to investigation (eg, CD64 or procalcitonin) but are either not clinically available or not
validated in EOS. The components of the complete
blood cell count and C-reactive protein perform relatively poorly when used as single values to assess EOS
risk; the low incidence of EOS among term infants
means there is little value in their positive and negative
predictive values. A full discussion of the use of laboratory results to predict EOS is beyond the scope of
this review.
Both the CDC and the American Academy of Pediatrics advocate evaluation of infants who are born with
signs of illness, well-appearing infants born in the setting
of maternal chorioamnionitis (with maternal intrapartum
fever often used as a surrogate for that condition), and
infants born to women who received inadequately indicated GBS IAP, with consideration given to gestational
age at birth and duration of rupture of membranes.
(14)(24)(25) Individual care centers often implement
these recommendations with local variation in practice.
We recently surveyed EOS risk assessment practices
among 23 NICUs in Massachusetts. Three-quarters of
the surveyed units had local written protocols for EOS
evaluation of term and late preterm infants. Most were
aligned with the CDC 2010 recommendations, (14) approximately 10% were aligned with the American Academy of Pediatrics recommendations, (24)(25) and one
center still adhered to the CDC 2002 recommendations.
(13) Signicant variation was reported with respect to
chorioamnionitis as a risk factor and in the use of laboratory tests for EOS evaluation.
Unintended Consequences of Current
Evaluation Approach
The low incidence of EOS in United States, particularly
among term and late preterm infants, leads to a relatively
high incidence of evaluation and empiric antibiotic treatment of uninfected newborns. We have studied the effect
of implementing the CDC 2010 recommendations at
a large perinatal center in Massachusetts. (29) We found
that approximately 7% of the lowest-risk group (asymptomatic term and near-term newborns) was evaluated
for EOS, and 75% of those evaluated received broadspectrum empiric antibiotics. During a 12-month period,
these evaluations had signicant economic costs and used
hundreds of hours of specialized care. In a separate study
that examined breastfeeding practices among term, wellappearing infants undergoing EOS evaluation, we found
that infants separated from their mothers for the
evaluation within 2 hours of birth were more likely to
have delayed breastfeeding initiation and increased formula supplementation. (30) Studies have also found associations between antibiotic exposure in the newborn
period and subsequent risk of necrotizing enterocolitis
in VLBW infants and wheezing in the general population.
(31)(32)
Risk Stratification Using Bayesian Modeling
The low absolute risk of EOS and the effect of current
evaluation algorithms suggest a need to improve the efciency of EOS risk assessment. Standard approaches to
EOS risk assessment use individual risk factors in isolation
and usually in dichotomized form. Such algorithms do
not account for interactions between risk factors and impose cut-off points that can result in loss of information.
For example, determining EOS risk due to rupture of
membranes by dichotomizing the infant as being or
not being at risk suggests a sudden change of risk at precisely 18 hours, when in reality risk due to rupture of
membranes is more likely to change in a graded fashion.
Puopolo et al (4) developed a multivariate model that
uses established EOS risk factors in a multivariate manner
to quantitatively determine risk among infants born at 34
weeks gestation or greater. These investigators took a
Bayesian approach, starting with the prior probability
of EOS in the population. This probability is modied using objective data from intrapartum risk factors for EOS
and then subsequently modied by the newborns clinical
condition to establish a nal posterior probability of infection. The model was developed using a nested casecontrol design, with 350 EOS cases and 1,063 controls
obtained from a birth cohort of more than 600,000 live
births in 14 different centers. The intrapartum risk model
(the maternal prior probability) uses gestational age, duration of rupture of membranes, and highest maternal intrapartum temperature as continuous variables and GBS
status and type and timing of intrapartum antibiotics as
categorical variables. Using split validation, the investigators found that use of this maternal prior probability
alone would reduce unnecessary evaluations by 60%.
Newborn examination results and vital signs at 6, 12,
and 24 hours after birth were used to classify infants into
categories of clinical illness, equivocal appearance, and
well-appearing. (24) The likelihood ratios from the newborn examination were combined with the multivariate
risk predictions to generate a nal predicted posterior
probability of infection. A proposed management pathway for EOS risk using this objective approach is shown
in the Figure. The number needed to treat refers to the
number of infants needed to be evaluated to identify each
e226 NeoReviews Vol.16 No.4 April 2015
Downloaded from http://neoreviews.aappublications.org/ at Indonesia:AAP Sponsored on September 22, 2015
infectious diseases / early-onset sepsis
Figure. Quantitative risk stratification for early-onset sepsis. A quantitative risk stratification scheme is shown for infants born
at 34 weeks gestation or more. Stratification is based on newborn clinical condition during the first 12 hours after birth and the
sepsis risk at birth estimated from maternal/intrapartum risk factors. Infants who have a sepsis risk at birth of 1.54 per 1,000 live
births or more or who have a sepsis risk at birth of 0.65 or more per 1,000 live births and an equivocal presentation fall into the
treat empirically group, which has a number needed to treat (NNT) of 118 and accounts for 4% of all live births. Infants with an
equivocal presentation or who are well-appearing but whose sepsis risk at birth is 0.65 to 1.54 per 1,000 fall into the observe
and evaluate group; these groups together have an NNT of 823 and account for 11% of all live births. The largest group, wellappearing infants with a sepsis risk at birth of less than 0.65 per 1,000, has an NNT of 9,370 and accounts for 85% of all live
births. Adapted from Escobar et al. (24)
EOS case. User-friendly versions of this combined model
can be found at http://www.dor.kaiser.org/external/
DORExternal/research/InfectionProbabilityCalculator.
aspx and www.newbornsepsiscalculator.org. The use of
this type of objective, multivariate approach is estimated
to safely reduce the number of infants evaluated and empirically treated for EOS by 80,000 to 240,000 infants
per year. (24)
American Board of Pediatrics NeonatalPerinatal
Content Specifications
Know the clinical manifestations,
laboratory features, and differential
diagnosis of neonatal sepsis.
Know the infectious agents that cause
neonatal sepsis.
Know the maternal, perinatal, and
neonatal risk factors for neonatal sepsis.
Know the epidemiology, prevention, and pathogenesis of
perinatal/neonatal group B streptococcal infections.
References
1. Stoll BJ, Hansen NI, Snchez PJ, et al; Eunice Kennedy Shriver
National Institute of Child Health and Human Development Neonatal
Research Network. Early onset neonatal sepsis: the burden of group B streptococcal and E. coli disease continues. Pediatrics. 2011;127(5):817826
2. Weston EJ, Pondo T, Lewis MM, et al. The burden of invasive
early-onset neonatal sepsis in the United States, 2005-2008.
Pediatr Infect Dis J. 2011;30(11):937941
3. Phares CR, Lyneld R, Farley MM, et al; Active Bacterial Core
surveillance/Emerging Infections Program Network. Epidemiology of invasive group B streptococcal disease in the United States,
1999-2005. JAMA. 2008;299(17):20562065
4. Puopolo KM, Draper D, Wi S, et al. Estimating the probability
of neonatal early-onset infection on the basis of maternal risk
factors. Pediatrics. 2011;128(5):e1155e1163
5. Centers for Disease Control and Prevention. Prevention of
perinatal group B streptococcal disease: a public health perspective.
MMWR Recomm Rep. 1996;45(RR-7):124
6. Centers for Disease Control and Prevention. Active bacterial core
surveillance report, emerging infections program network, group B streptococcus, 2013 [Internet]. Updated 2013. http://www.cdc.gov/abcs/
reports-ndings/survreports/gbs13.pdf. Accessed September 18, 2014
7. Stoll BJ, Hansen N, Fanaroff AA, et al. Changes in pathogens
causing early-onset sepsis in very-low-birth-weight infants. N Engl J
Med. 2002;347(4):240247
NeoReviews Vol.16 No.4 April 2015 e227
Downloaded from http://neoreviews.aappublications.org/ at Indonesia:AAP Sponsored on September 22, 2015
infectious diseases / early-onset sepsis
8. Puopolo KM, Eichenwald EC. No change in the incidence of
ampicillin-resistant, neonatal, early-onset sepsis over 18 years.
Pediatrics. 2010;125(5):e1031e1038
9. Campbell JR, Hillier SL, Krohn MA, Ferrieri P, Zaleznik DF,
Baker CJ. Group B streptococcal colonization and serotype-specic
immunity in pregnant women at delivery. Obstet Gynecol. 2000;96
(4):498503
10. Meyn LA, Moore DM, Hillier SL, Krohn MA. Association of
sexual activity with colonization and vaginal acquisition of group B
Streptococcus in nonpregnant women. Am J Epidemiol. 2002;155
(10):949957
11. Benitz WE, Gould JB, Druzin ML. Risk factors for early-onset
group B streptococcal sepsis: estimation of odds ratios by critical
literature review. Pediatrics. 1999;103(6):e77
12. Boyer KM, Gotoff SP. Prevention of early-onset neonatal
group B streptococcal disease with selective intrapartum chemoprophylaxis. N Engl J Med. 1986;314(26):16651669
13. Schrag S, Gorwitz R, Fultz-Butts K, Schuchat A. Prevention of
perinatal group B streptococcal disease: revised guidelines from
CDC. MMWR Recomm Rep. 2002;51(RR-11):122
14. Verani JR, McGee L, Schrag SJ; Division of Bacterial Diseases,
National Center for Immunization and Respiratory Diseases,
Centers for Disease Control and Prevention (CDC). Prevention
of perinatal group B streptococcal diseaserevised guidelines from
CDC, 2010. MMWR Recomm Rep. 2010;59(RR-10):136
15. Van Dyke MK, Phares CR, Lyneld R, et al. Evaluation of
universal antenatal screening for group B streptococcus. N Engl J
Med. 2009;360(25):26262636
16. Puopolo KM, Madoff LC, Eichenwald EC. Early-onset group
B streptococcal disease in the era of maternal screening. Pediatrics.
2005;115(5):12401246
17. Puopolo KM, Madoff LC. Type IV neonatal early-onset group
B streptococcal disease in a United States hospital. J Clin Microbiol.
2007;45(4):13601362
18. Yancey MK, Schuchat A, Brown LK, Ventura VL, Markenson
GR. The accuracy of late antenatal screening cultures in predicting
genital group B streptococcal colonization at delivery. Obstet
Gynecol. 1996;88(5):811815
19. Moore MR, Schrag SJ, Schuchat A. Effects of intrapartum
antimicrobial prophylaxis for prevention of group-B-streptococcal
disease on the incidence and ecology of early-onset neonatal sepsis.
Lancet Infect Dis. 2003;3(4):201213
20. Stoll BJ, Hansen NI, Higgins RD, et al; National Institute of
Child Health and Human Development. Very low birth weight
preterm infants with early onset neonatal sepsis: the predominance
of gram-negative infections continues in the National Institute of
Child Health and Human Development Neonatal Research Network, 20022003. Pediatr Infect Dis J. 2005;24(7):635639
21. Bizzarro MJ, Dembry LM, Baltimore RS, Gallagher PG.
Changing patterns in neonatal Escherichia coli sepsis and ampicillin
resistance in the era of intrapartum antibiotic prophylaxis. Pediatrics. 2008;121(4):689696
22. Schrag SJ, Hadler JL, Arnold KE, Martell-Cleary P, Reingold
A, Schuchat A. Risk factors for invasive, early-onset Escherichia coli
infections in the era of widespread intrapartum antibiotic use.
Pediatrics. 2006;118(2):570576
23. Andrews WW, Schelonka R, Waites K, Stamm A, Cliver SP,
Moser S. Genital tract methicillin-resistant Staphylococcus aureus: risk
of vertical transmission in pregnant women. Obstet Gynecol. 2008;111
(1):113118
24. Polin RA; Committee on Fetus and Newborn. Management of
neonates with suspected or proven early-onset bacterial sepsis.
Pediatrics. 2012;129(5):10061015
25. Brady MT, Polin RA. Prevention and management of infants with
suspected or proven neonatal sepsis. Pediatrics. 2013;132(1):166168
26. Escobar GJ, Puopolo KM, Wi S, et al. Stratication of risk of
early-onset sepsis in newborns 34 weeks gestation. Pediatrics.
2014;133(1):3036
27. Cantoni L, Ronfani L, Da Riol R, Demarini S; Perinatal Study
Group of the Region Friuli-Venezia Giulia. Physical examination
instead of laboratory tests for most infants born to mothers
colonized with group B Streptococcus: support for the Centers for
Disease Control and Preventions 2010 recommendations. J
Pediatr. 2013;163(2):568573
28. Escobar GJ, Li DK, Armstrong MA, et al. Neonatal sepsis
workups in infants >/2000 grams at birth: A population-based
study. Pediatrics. 2000;106(2, pt 1):256263
29. Mukhopadhyay S, Dukhovny D, Mao W, Eichenwald EC,
Puopolo KM. 2010 perinatal GBS prevention guideline and
resource utilization. Pediatrics. 2014;133(2):196203
30. Mukhopadhyay S, Lieberman ES, Puopolo KM, et al. Effect of
early-onset sepsis evaluations on breastfeeding among asymptomatic term neonates. Hosp Pediatr. In press
31. Alexander VN, Northrup V, Bizzarro MJ. Antibiotic exposure
in the newborn intensive care unit and the risk of necrotizing
enterocolitis. J Pediatr. 2011;159(3):392397
32. Goksr E, Alm B, Thengilsdottir H, Pettersson R, berg N,
Wennergren G. Preschool wheeze - impact of early sh introduction and neonatal antibiotics. Acta Paediatr. 2011;100(12):
15611566
e228 NeoReviews Vol.16 No.4 April 2015
Downloaded from http://neoreviews.aappublications.org/ at Indonesia:AAP Sponsored on September 22, 2015
infectious diseases / early-onset sepsis
NeoReviews Quiz Requirements
To successfully complete 2015 NeoReviews articles for AMA PRA Category 1 CreditTM, learners must demonstrate a minimum performance level of
60% or higher on this assessment, which measures achievement of the educational purpose and/or objectives of this activity. If you score less than
60% on the assessment, you will be given additional opportunities to answer questions until an overall 60% or greater score is achieved.
NOTE: Learners can take NeoReviews quizzes and claim credit online only at: http://neoreviews.org.
1. A 4-day-old infant who was born at 24 weeks gestational age with a birth weight of 600 g is noted to have
a positive blood culture result. The culture was obtained at age 48 hours. Which of the following regarding the
timing of infection and definitions of sepsis in newborns is correct?
A. If this patient is diagnosed as having sepsis, it would be correctly categorized as early-onset sepsis.
B. For infants with birth weight greater than 1,500 g, culture-proven infection occurring before 48 hours is
considered as early-onset sepsis and after 48 hours as late-onset sepsis.
C. The risk of infection in very low-birth-weight infants after 72 hours up to age 1 week derives primarily
from prenatal and maternal risk factors.
D. The organisms found in blood cultures of very low-birth-weight infants at this age (48 hours) are more
likely to reflect the nosocomial flora of the neonatal intensive care unit (NICU) than positive culture
obtained later in hospitalization.
E. The incidence of early-onset sepsis for very low-birth-weight infants in the United States is 10 per 1,000
live births in recent years.
2. A term newborn infant has respiratory distress soon after birth and is admitted to the NICU. Blood culture is
obtained, and antibiotics are administered in case the patient has sepsis. Which of the following is true
regarding the microorganisms that cause neonatal sepsis?
A. With increasing colonization in the general population, the incidence of early-onset sepsis caused by group
B Streptococcus (GBS) has increased steadily during the past 4 decades.
B. Intrapartum antibiotic prophylaxis has reduced the severity of GBS early-onset sepsis in newborns but has
not had any effect on its incidence.
C. Early-onset sepsis caused by gram-negative enteric bacteria is found in term infants but not in preterm
infants.
D. The pathogenesis of early-onset sepsis involves ascending colonization of the fetal compartment through
ruptured and less frequently intact amniotic membranes.
E. Clostridium difficile is the most common cause of early-onset sepsis in both term and preterm infants.
3. The patients blood culture yields GBS. Which of the following statements concerning GBS is correct?
A. GBS is always a pathogenic organism and is found only in humans during pregnancy complicated by
chorioamnionitis or in newborns after intrapartum infection.
B. Most early-onset sepsis caused by GBS in the United States is currently caused by capsular polysaccharide
serotypes Ia, Ib, II, III, and V.
C. Early-onset sepsis associated with GBS is most often caused by transmission through breastfeeding during
the first 24 hours after birth.
D. Maternal GBS colonization has no effect on the development of GBS sepsis in newborns.
E. Current recommendations from the Centers for Disease Control and Prevention (CDC) do not suggest any
benefit of routine testing for GBS or a benefit of prophylactic intrapartum antibiotics for prevention of
GBS sepsis.
4. A male infant is born at 26 weeks gestational age after spontaneous preterm labor. A blood culture is obtained
in the NICU soon after admission and later yields Escherichia coli. Which of the following is correct regarding
early-onset sepsis in very low-birth-weight infants?
A. E coli is currently the most common organism causing early-onset sepsis in very low-birth-weight infants.
B. All large epidemiologic studies have found that increased use of intrapartum prophylactic antibiotics leads
to an absolute decrease in E colispecific early-onset sepsis and a decreased proportion of sepsis caused by
E coli for very low-birth-weight infants.
NeoReviews Vol.16 No.4 April 2015 e229
Downloaded from http://neoreviews.aappublications.org/ at Indonesia:AAP Sponsored on September 22, 2015
infectious diseases / early-onset sepsis
C. Methicillin-resistant Staphylococcus aureus is strongly associated with early-onset sepsis in very lowbirth-weight infants when mothers have recently ingested contaminated foods, such as soft cheeses and
deli meats.
D. Because the likelihood of anaerobic bacteria causing neonatal early-onset sepsis is exceedingly low, only
aerobic blood cultures are warranted.
E. Since the introduction of intrapartum antibiotic prophylaxis, more than 50% of neonatal early-onset
sepsis by S aureus is methicillin resistant.
5. Your maternal child unit is developing guidelines for risk assessment and practice surrounding neonatal earlyonset sepsis. Which of the following statements concerning risk assessment for early-onset sepsis is correct?
A. Because of conflicting studies, the CDC and the American Academy of Pediatrics have both declined to
make overarching recommendations surrounding this issue.
B. Because clinical status can often be misleading, infant symptoms should not be included in risk assessment
strategies.
C. Single components of the complete blood cell count or C-reactive protein level can perform very well as
predictors of early-onset sepsis, and it is up to each unit to determine which component to use as its main
test for risk assessment.
D. Use of a multivariable model that takes into account prior probability of sepsis based on multiple variables,
including maternal factors, can help to reduce the number of infants evaluated and empirically treated for
early-onset sepsis.
E. The most pragmatic approach that leads to highest sensitivity and specificity for diagnosis of early-onset
sepsis is to evaluate and treat all infants whose mother had more than 18 hours of ruptured membranes.
e230 NeoReviews Vol.16 No.4 April 2015
Downloaded from http://neoreviews.aappublications.org/ at Indonesia:AAP Sponsored on September 22, 2015
Neonatal Early-Onset Sepsis: Epidemiology and Risk Assessment
Sagori Mukhopadhyay and Karen M. Puopolo
NeoReviews 2015;16;e221
DOI: 10.1542/neo.16-4-e221
Updated Information &
Services
including high resolution figures, can be found at:
http://neoreviews.aappublications.org/content/16/4/e221
References
This article cites 30 articles, 14 of which you can access for free at:
http://neoreviews.aappublications.org/content/16/4/e221#BIBL
Subspecialty Collections
This article, along with others on similar topics, appears in the
following collection(s):
Epidemiology
http://neoreviews.aappublications.org/cgi/collection/epidemiology_s
ub
Fetus/Newborn Infant
http://neoreviews.aappublications.org/cgi/collection/fetus:newborn_i
nfant_sub
Infectious Diseases
http://neoreviews.aappublications.org/cgi/collection/infectious_disea
ses_sub
Journal CME
http://neoreviews.aappublications.org/cgi/collection/journal_cme
Neonatology
http://neoreviews.aappublications.org/cgi/collection/neonatology_su
b
Pediatric Drug Labeling Update
http://neoreviews.aappublications.org/cgi/collection/pediatric_drug_l
abeling_update
Permissions & Licensing
Information about reproducing this article in parts (figures, tables) or
in its entirety can be found online at:
http://neoreviews.aappublications.org/site/misc/Permissions.xhtml
Reprints
Information about ordering reprints can be found online:
http://neoreviews.aappublications.org/site/misc/reprints.xhtml
Downloaded from http://neoreviews.aappublications.org/ at Indonesia:AAP Sponsored on September 22, 2015
Neonatal Early-Onset Sepsis: Epidemiology and Risk Assessment
Sagori Mukhopadhyay and Karen M. Puopolo
NeoReviews 2015;16;e221
DOI: 10.1542/neo.16-4-e221
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
http://neoreviews.aappublications.org/content/16/4/e221
Neoreviews is the official journal of the American Academy of Pediatrics. A monthly publication,
it has been published continuously since . Neoreviews is owned, published, and trademarked by
the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk Grove Village, Illinois,
60007. Copyright 2015 by the American Academy of Pediatrics. All rights reserved. Online
ISSN: 1526-9906.
Downloaded from http://neoreviews.aappublications.org/ at Indonesia:AAP Sponsored on September 22, 2015
Вам также может понравиться
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Diagnosis of Multiple Personality DisorderДокумент15 страницThe Diagnosis of Multiple Personality DisorderSleepy WinterОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Gambar CA CervixДокумент6 страницGambar CA CervixSleepy WinterОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Erikson Child DevelopmentДокумент12 страницErikson Child Developmentgmahanti100% (2)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Vaginal HysterectomyДокумент7 страницVaginal HysterectomySleepy Winter0% (1)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Cleft Lip and Cleft PalateДокумент57 страницCleft Lip and Cleft PalateSleepy WinterОценок пока нет
- AnemiaДокумент21 страницаAnemiaSleepy WinterОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- C32 337nxnkXNckxNkДокумент9 страницC32 337nxnkXNckxNkSleepy WinterОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Serenity Programme™ - Dissociative Experiences Scales (DES)Документ4 страницыSerenity Programme™ - Dissociative Experiences Scales (DES)Diana DumitrescuОценок пока нет
- 1 SafdaskjfjasidjasofjasjfosjfopДокумент90 страниц1 SafdaskjfjasidjasofjasjfosjfopSleepy WinterОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- International Pediatric Sepsis Consensus Conference-PediatrCritCar2005-eДокумент7 страницInternational Pediatric Sepsis Consensus Conference-PediatrCritCar2005-eAna Belén VizcarraОценок пока нет
- The Diagnosis of Multiple Personality DisorderДокумент15 страницThe Diagnosis of Multiple Personality DisorderSleepy WinterОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Urolithiasis GuidelineДокумент71 страницаUrolithiasis GuidelineSleepy WinterОценок пока нет
- Fsanfjlksafnklnasklfnkalfjklasjfjasfjasjf Asjfjsl FJL Asjf AsjfДокумент9 страницFsanfjlksafnklnasklfnkalfjklasjfjasfjasjf Asjfjsl FJL Asjf AsjfSleepy WinterОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- ACR Recommendations For The Use of Nonpharmacologic and Pharmacologic Therpies in OA of The Hand, Hip and KneeДокумент10 страницACR Recommendations For The Use of Nonpharmacologic and Pharmacologic Therpies in OA of The Hand, Hip and KneeA. Isma NursyamsuОценок пока нет
- Uhkhdahfhiahfioehf Jahfwjfhlhfb Dhfjshflhalfhlk BDFKJFKJSBFKJSB SBFJSBFJDSBF DbfjbsjkfbjadkbfjДокумент3 страницыUhkhdahfhiahfioehf Jahfwjfhlhfb Dhfjshflhalfhlk BDFKJFKJSBFKJSB SBFJSBFJDSBF DbfjbsjkfbjadkbfjSleepy WinterОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- 3 Kelainan Yg Ditemukan PD Hipospadia Chordee Ventral HoodДокумент2 страницы3 Kelainan Yg Ditemukan PD Hipospadia Chordee Ventral HoodSleepy WinterОценок пока нет
- ACR Recommendations For The Use of Nonpharmacologic and Pharmacologic Therpies in OA of The Hand, Hip and KneeДокумент10 страницACR Recommendations For The Use of Nonpharmacologic and Pharmacologic Therpies in OA of The Hand, Hip and KneeA. Isma NursyamsuОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- ACR Recommendations For The Use of Nonpharmacologic and Pharmacologic Therpies in OA of The Hand, Hip and KneeДокумент10 страницACR Recommendations For The Use of Nonpharmacologic and Pharmacologic Therpies in OA of The Hand, Hip and KneeA. Isma NursyamsuОценок пока нет
- 3 Kelainan Yg Ditemukan PD Hipospadia Chordee Ventral HoodДокумент2 страницы3 Kelainan Yg Ditemukan PD Hipospadia Chordee Ventral HoodSleepy WinterОценок пока нет
- Mitral Valve Repair Experience in Harapan Kita Hospital: Maizul Anwar, MDДокумент24 страницыMitral Valve Repair Experience in Harapan Kita Hospital: Maizul Anwar, MDSleepy WinterОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- P 114Документ7 страницP 114Sleepy WinterОценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Chart Title: Uhkhdahfhiahfioehf Jahfwjfhlhfb Dhfjshflhalfhlk BDFKJFKJSBFKJSB SBFJSBFJDSBF DbfjbsjkfbjadkbfjДокумент3 страницыChart Title: Uhkhdahfhiahfioehf Jahfwjfhlhfb Dhfjshflhalfhlk BDFKJFKJSBFKJSB SBFJSBFJDSBF DbfjbsjkfbjadkbfjSleepy WinterОценок пока нет
- Uhkhdahfhiahfioehf Jahfwjfhlhfb Dhfjshflhalfhlk BDFKJFKJSBFKJSB SBFJSBFJDSBF DbfjbsjkfbjadkbfjДокумент3 страницыUhkhdahfhiahfioehf Jahfwjfhlhfb Dhfjshflhalfhlk BDFKJFKJSBFKJSB SBFJSBFJDSBF DbfjbsjkfbjadkbfjSleepy WinterОценок пока нет
- Draft 222 Hfhlwfhlihf DnsflshfklhfklehflkhwДокумент3 страницыDraft 222 Hfhlwfhlihf DnsflshfklhfklehflkhwSleepy WinterОценок пока нет
- 1 SafdaskjfjasidjasofjasjfosjfopДокумент90 страниц1 SafdaskjfjasidjasofjasjfosjfopSleepy WinterОценок пока нет
- Urolithiasis GuidelineДокумент71 страницаUrolithiasis GuidelineSleepy WinterОценок пока нет
- Fsanfjlksafnklnasklfnkalfjklasjfjasfjasjf Asjfjsl FJL Asjf AsjfДокумент9 страницFsanfjlksafnklnasklfnkalfjklasjfjasfjasjf Asjfjsl FJL Asjf AsjfSleepy WinterОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- 3 Kelainan Yg Ditemukan PD Hipospadia Chordee Ventral HoodДокумент2 страницы3 Kelainan Yg Ditemukan PD Hipospadia Chordee Ventral HoodSleepy WinterОценок пока нет
- C32 337nxnkXNckxNkДокумент9 страницC32 337nxnkXNckxNkSleepy WinterОценок пока нет
- Brand Guidelines Oracle PDFДокумент39 страницBrand Guidelines Oracle PDFMarco CanoОценок пока нет
- MPPWD 2014 SOR CH 1 To 5 in ExcelДокумент66 страницMPPWD 2014 SOR CH 1 To 5 in ExcelElvis GrayОценок пока нет
- Ewellery Ndustry: Presentation OnДокумент26 страницEwellery Ndustry: Presentation Onharishgnr0% (1)
- Business Plan GROUP 10Документ35 страницBusiness Plan GROUP 10Sofia GarciaОценок пока нет
- Ril Competitive AdvantageДокумент7 страницRil Competitive AdvantageMohitОценок пока нет
- DevelopmentPermission Handbook T&CPДокумент43 страницыDevelopmentPermission Handbook T&CPShanmukha KattaОценок пока нет
- ILRF Soccer Ball ReportДокумент40 страницILRF Soccer Ball ReportgabalauiОценок пока нет
- Black BookДокумент28 страницBlack Bookshubham50% (2)
- Toshiba Satellite L200 M200 M203 M206 KBTIДокумент59 страницToshiba Satellite L200 M200 M203 M206 KBTIYakub LismaОценок пока нет
- Best Practices in Developing High PotentialsДокумент9 страницBest Practices in Developing High PotentialsSuresh ShetyeОценок пока нет
- Study of Means End Value Chain ModelДокумент19 страницStudy of Means End Value Chain ModelPiyush Padgil100% (1)
- Fast Binary Counters and Compressors Generated by Sorting NetworkДокумент11 страницFast Binary Counters and Compressors Generated by Sorting Networkpsathishkumar1232544Оценок пока нет
- Module 5 - Multimedia Storage DevicesДокумент10 страницModule 5 - Multimedia Storage Devicesjussan roaringОценок пока нет
- Mathematics 2 First Quarter - Module 5 "Recognizing Money and Counting The Value of Money"Документ6 страницMathematics 2 First Quarter - Module 5 "Recognizing Money and Counting The Value of Money"Kenneth NuñezОценок пока нет
- Project 1. RockCrawlingДокумент2 страницыProject 1. RockCrawlingHằng MinhОценок пока нет
- Certification DSWD Educational AssistanceДокумент3 страницыCertification DSWD Educational AssistancePatoc Stand Alone Senior High School (Region VIII - Leyte)Оценок пока нет
- Dbms UPDATED MANUAL EWITДокумент75 страницDbms UPDATED MANUAL EWITMadhukesh .kОценок пока нет
- Carelink Connect: User GuideДокумент41 страницаCarelink Connect: User GuideMiha SoicaОценок пока нет
- Software Testing Notes Prepared by Mrs. R. Swetha M.E Unit I - Introduction at The End of This Unit, The Student Will Be Able ToДокумент30 страницSoftware Testing Notes Prepared by Mrs. R. Swetha M.E Unit I - Introduction at The End of This Unit, The Student Will Be Able ToKabilan NarashimhanОценок пока нет
- Nguyen Dang Bao Tran - s3801633 - Assignment 1 Business Report - BAFI3184 Business FinanceДокумент14 страницNguyen Dang Bao Tran - s3801633 - Assignment 1 Business Report - BAFI3184 Business FinanceNgọc MaiОценок пока нет
- Press Release - INTRODUCING THE NEW LAND ROVER DEFENDER PDFДокумент6 страницPress Release - INTRODUCING THE NEW LAND ROVER DEFENDER PDFJay ShahОценок пока нет
- It14 Belotti PDFДокумент37 страницIt14 Belotti PDFHolis AdeОценок пока нет
- Rideable Segway Clone - Low Cost and Easy Build: Digital MPU6050 Accelerometer/gyro IMU BoardДокумент45 страницRideable Segway Clone - Low Cost and Easy Build: Digital MPU6050 Accelerometer/gyro IMU BoardpaolaОценок пока нет
- Safety Inspection Checklist Project: Location: Inspector: DateДокумент2 страницыSafety Inspection Checklist Project: Location: Inspector: Dateyono DaryonoОценок пока нет
- Kit 2: Essential COVID-19 WASH in SchoolДокумент8 страницKit 2: Essential COVID-19 WASH in SchooltamanimoОценок пока нет
- Fortigate Fortiwifi 40F Series: Data SheetДокумент6 страницFortigate Fortiwifi 40F Series: Data SheetDiego Carrasco DíazОценок пока нет
- Sec2 8 PDFДокумент3 страницыSec2 8 PDFpolistaОценок пока нет
- Verma Toys Leona Bebe PDFДокумент28 страницVerma Toys Leona Bebe PDFSILVIA ROMERO100% (3)
- 7933-Article Text-35363-1-10-20230724Документ8 страниц7933-Article Text-35363-1-10-20230724Ridho HidayatОценок пока нет
- 0901b8038042b661 PDFДокумент8 страниц0901b8038042b661 PDFWaqasAhmedОценок пока нет
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОт EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОценок пока нет
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisОт EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisРейтинг: 4.5 из 5 звезд4.5/5 (42)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeРейтинг: 2 из 5 звезд2/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsОт EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsРейтинг: 5 из 5 звезд5/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (24)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedРейтинг: 5 из 5 звезд5/5 (80)