Академический Документы
Профессиональный Документы
Культура Документы
International Journal of Surgery Case Reports
Загружено:
Vmiguel LcastilloОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
International Journal of Surgery Case Reports
Загружено:
Vmiguel LcastilloАвторское право:
Доступные форматы
CASE REPORT OPEN ACCESS
International Journal of Surgery Case Reports 4 (2013) 11001103
Contents lists available at ScienceDirect
International Journal of Surgery Case Reports
journal homepage: www.casereports.com
Reconstruction of short bowel syndrome after internal hernia in a
pregnant woman with previous bariatric surgery
Mrta Kristina Borghede a, , Lars Vinter-Jensen a , Jens Christian Andersen b ,
Peter Brndum Mortensen b , Henrik Hjgaard Rasmussen a
a
b
Centre for Nutrition and Bowel Disease, Department of Gastroenterology, Aalborg University Hospital, Hobrovej, DK-9100 Aalborg, Denmark
Department of Surgery, Aalborg University Hospital, Hobrovej, DK-9100 Aalborg, Denmark
a r t i c l e
i n f o
Article history:
Received 8 August 2013
Accepted 13 August 2013
Available online 8 October 2013
Keywords:
Internal hernia
Laparoscopic gastric bypass
Short bowel syndrome
Pregnancy
a b s t r a c t
INTRODUCTION: Bariatric surgery is most often performed with the laparoscopic Roux-en-Y gastric
bypass. A complication to the laparoscopic Roux-en-Y gastric bypass is internal hernia, which occurs
in up to 16% of the patients. Since the laparoscopic Roux-en-Y gastric bypass is performed in women of
fertile age, internal hernia may occur during pregnancy.
PRESENTATION OF CASE: A 22-year old woman with a history of laparoscopic Roux-en-Y gastric bypass suffered from massive internal hernia during pregnancy with widespread bowel necrosis. Extensive surgery
was performed leaving the patient with an intact duodenum, 15 cm of jejunum, 35 cm of ileum and
colon. Parenteral nutrition was initiated and ten months after the internal hernia, intestinal continuity
was re-established. Ten weeks later the patient reached parenteral nutrition independence.
DISCUSSION: Internal hernia after laparoscopic Roux-en-Y gastric bypass can be difcult to diagnose,
especially during pregnancy and might be severe and life threatening for both mother and child.
CONCLUSION: Obstetricians and abdominal surgeons must be aware of this condition. Surgery should
be performed on a wide indication. When bowel necrosis is found it should be resected and in case of
extensive bowel resection the patient should be evaluated in centres specialized in intestinal failure.
2013 The Authors. Published by Elsevier Ltd on behalf of Surgical Associates Ltd.
Open access under CC BY-NC-ND license.
1. Introduction
2. Presentation of case
Bariatric surgery is most often performed with the laparoscopic
Roux-en-Y gastric bypass (LRGB). LRGB has favourable effects such
as weight loss and correction of metabolic disturbances, but is also
associated with serious complications. Internal hernia occurs in up
to 16% of the patients.1 It is a severe complication, which can lead to
massive bowel necrosis that may result in short bowel syndrome
(SBS) and sometimes death.2,3 Pregnant women, who have previously undergone LRBG, represent a diagnostic challenge when
presenting with acute abdomen and internal hernia in this setting
might be particularly risky.
In this case, we present a 22-year-old woman, who had undergone LRGB and who suffered a massive internal hernia during
pregnancy leading to short bowel syndrome.
In January 2012, at 26 weeks of gestation, a 22-year-old woman
was admitted to our surgical department due to sudden onset of
upper abdominal pain. The patient was otherwise healthy and had
at the time she became pregnant lost 50 kg following a LRGB done
two years and 11 months earlier.
Following admission, an acute ultrasound showed gall bladder
stones, and a MRI scan showed no denite signs of internal hernia but could not demonstrate gallstones. Due to severe pain, open
cholecystectomy was performed. A trans-cystic balloon dilation of
the papilla of Vater was done as the cholangiogram demonstrated
poor drainage caused by small gallstones in the common hepatic
bile duct. On the 5th postoperative day she was re-operated due to
cholascos with renewed cystic duct ligation and drainage. On the
following day, endoscopy was performed because of hematamesis,
with the nding of blood in the jejunum, but no specic bleeding site was identied. The clinical condition worsened and she
was transferred to the intensive care unit (ICU) with severe septicaemia and acute respiratory distress syndrome (ARDS). On day 13,
a laparotomy was performed. An internal hernia through Petersens
space with necrosis of 1 m jejunum starting 10 cm below the pouchenteric anastomosis was found. A vital premature girl of 1020 g was
delivered by caesarean and the necrotic intestine was removed.
Second and third look operations were performed the next days
with further small bowel resections leaving her with a saliva stula
Corresponding author at: Department of Gastroenterology, Aalborg University
Hospital, Mlleparkvej 4, 9000 Aalborg, Denmark. Tel.: +45 99326241;
fax: +45 99326507.
E-mail address: marta.borghede@gmail.com (M.K. Borghede).
2210-2612 2013 The Authors. Published by Elsevier Ltd on behalf of Surgical Associates Ltd. Open access under CC BY-NC-ND license.
http://dx.doi.org/10.1016/j.ijscr.2013.08.025
CASE REPORT OPEN ACCESS
M.K. Borghede et al. / International Journal of Surgery Case Reports 4 (2013) 11001103
1101
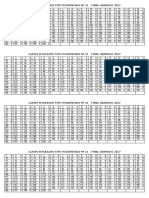
Fig. 1. The intestinal system of a 22-year old woman with previous gastric bypass operation after internal herniation with massive bowel necrosis. The patient ended up
with a saliva stula from the pouch-enteric anastomosis, a jejunostomy 15 cm from the ligament of Treitz, and a blind closed ileum 35 cm from the ileo-coecal valve (left).
Ten months later the intestinal continuity was reestablished (right).
10 cm below the pouch-enteric anastomosis, a jejunostomy 15 cm
from the ligament of Treitz and a blind closed ileum 35 cm from the
ileo-coecal valve (Fig. 1).
After 3 months in the ICU and surgical ward with several other
complications, such as infectious complications, pneumothorax,
thrombosis of the superior mesenteric vein as well as the iliac
veins and a exposed bowel parquet covered with split skin, the
patient was transferred to our intestinal failure unit. The patient
had a good appetite and enjoyed the meals, but obviously she
had no absorption of food due to the very short stula below the
pouch-enteric anastomosis. Through a central venous line (Hickmann catheter) she initially received 2200 kcal and later when
she increased her daily activities this was increased according to
2700 kcal given as SMOF Kabiven (Fresenius) added with vitamins and trace elements, and in addition 3 l of isotonic saline
to maintain the uid balance. Also in this phase complications
occurred, and the Hickmann catheter eventually had to be removed
due to a yeast infection with candida albicans. The nutrition was
thereafter delivered through a peripherally inserted central venous
catheter (PICCline). After four months of hospitalization the patient
was discharged with home parenteral nutrition. In November
2012, ten month after the internal herniation, intestinal continuity was reconstructed, and a defect having a width of up to
12 cm in the anterior abdominal wall was closed with bilateral
partial component separation technique ad modum Ramirez.4 Six
weeks after the operation, the PICCline occluded and was removed.
The patient insisted on trying without parenteral nutrition, and
10 weeks later, she was doing well. Her weight had increased
2 kg since the operation, she had 12 bowel movements a day
and blood values for haemoglobin and albumin had increased as
well.
3. Discussion
This patient suffered from massive small bowel internal hernia
with extensive bowel resection leading to SBS dependent on parenteral nutrition during her pregnancy. The patient was left with an
intact duodenum, 15 cm of jejunum, 35 cm of ileum and her colon.
Initially she was treated with 100% parenteral nutrition, but after
reconstructive surgery with re-established intestinal continuity the
amount of parenteral nutrition was rapidly reduced, and after six
weeks she was weaned off parenteral nutrition.
Several cases of internal hernias during pregnancies have been
reported and three maternal deaths have been described.5 Renault
et al.3 and Loar et al.6 describe severe internal hernias in pregnant
women, involving the entire small intestine, parts of the colon and
in Renault et al. even parts of the ventricle. In these cases surgical
and medical interventions were considered futile and the patients
died. Our patient also suffered a severe internal hernia with necrotic
intestine. She underwent extensive bowel resection leading to an
acute intestinal failure associated with severe complications (type 2
intestinal failure). After treatment in a specialized intestinal failure
unit, she underwent a long and complicated rehabilitation period
and was discharged with a short bowel syndrome treated with
home parenteral nutrition and uids (type 3 intestinal failure), and
she survived.
To our knowledge, no pregnant woman with LRGB has previously survived an internal herniation with such massive bowel
necrosis as in this case, see Table 1. This illustrates the importance of extensive surgery, second and third looks operations. The
University of Nebraska Medical Center describes in a series of
papers that 5 out of 210 patient with postoperative SBS had previous gastric bypass operation,7 and thereafter they scrutinized
CASE REPORT OPEN ACCESS
1102
M.K. Borghede et al. / International Journal of Surgery Case Reports 4 (2013) 11001103
Table 1
Review of reported cases of internal hernias in pregnant women with previous gastric bypass. Reports on bowel resection, foetal death and maternal outcome are
shown.3,6,8,1015
Authors
Bowel resection
Foetal death
Maternal outcome
Moore et al.14
61 cm
Yes
Charles et al.10
Non viable portions of
the Roux-limb
No, surgery considered
futile
20 cm
100 cm
150 cm
Resection of jejunal
anastomosis
Yes, 70 cm small
intestine remaining
No, surgery considered
futile
Yes, 50 cm small
intestine remaining
Yes
Death, ventricular
brillation
Survived
Loar et al.6
15
Wang et al.
Efthimiou et al.11
Gazzalle et al.12
Hooks et al.13
Boland et al.8
3
Renault et al.
Current study
No
No
Yes
No
No
Death, three days
postpartum
Survived
Survived
Survived
Survived
No
SBS
No
Death, three days
postpartum
SBS
No
SBS = short bowel syndrome; IH = internal hernia.
9 patients with SBS that had bariatric surgery performed.2 In a
more recent paper, they reviewed 9 cases with massive bowel
resection during pregnancy leading to small bowel syndrome.8
One of these had previous LRGB. Internal hernia during pregnancy
mostly occur in the third trimester and postpartum. It is believed
to be caused by the growing uterus, which increases the intraabdominal pressure, or postpartum as the uterus rapidly decreases
in size.3
The surveys of series of patients with previous bariatric surgery
demonstrate that up to 16% of the patients develop internal
herniation.1 Most bariatric surgeries have been performed in
women of reproductive age, and as LRGB increases fertility,
complications during pregnancy are to be expected. It is suggested that the changed anatomy during pregnancy disposes for
herniation to occur. During pregnancy, the cause of abdominal
pain can be difcult to diagnose, with potentially fatal consequences for both mother and foetus. This should be of particular
concern for obstetricians and abdominal surgeons. It is most
important that relevant tools such as MRI or CT scans are not
postponed. Interpretation of MRI and CT scan can be difcult
especially in pregnant women, thus laparoscopy should be performed on a wide indication, when there is clinical suspicion of
internal hernia and laparotomy performed if the anatomy is not
clear.
In the present paper, we describe a successful reconstruction.
The literature provides other successful reconstructions after LRGB
complicated with internal obstruction. A case report of a 44-yearold woman, who suffered from volvulus after LRGB, leaving her
with an intact duodenum, 25 cm of jejunum and ileum and colon,
has been described. Interestingly she eventually managed after
reconstruction without parenteral nutrition.9 The younger age of
our patient leaves her with an even better chance to stay off parenteral nutrition.
4. Conclusion
Since internal hernia is potentially life threatening for mother
and foetus, both obstetricians and abdominal surgeons must be
aware of this condition and surgery should be performed on a wide
indication. When bowel necrosis is found it should be resected
and in case of extensive bowel resection the patient should start
parenteral nutrition, and an evaluation should be made in centres
specialized in intestinal failure.
Authors contributions
All authors have contributed to acquisition of data, analysis and
interpretation of data, writing, drafting the article and revising it
critically for important intellectual content and approved of the
nal version.
Conict of interest statement
None.
Role of funding sources
None.
Ethical approval
Written informed consent was obtained from the patient for
publication of this case report and case series and accompanying
images. A copy of the written consent is available for review by the
Editor-in-Chief of this journal on request.
References
1. Higa K, Ho T, Tercero F, Yunus T, Boone KB. Laparoscopic Roux-en-Y gastric
bypass: 10-year follow-up. Surg Obes Relat Dis 2011;7(July (4)):51625.
2. McBride CL, Petersen A, Sudan D, Thompson J. Short bowel syndrome following
bariatric surgical procedures. Am J Surg 2006;192(December (6)):82832.
3. Renault K, Gyrtrup HJ, Damgaard K, Hedegaard M, Sorensen JL. Pregnant woman
with fatal complication after laparoscopic Roux-en-Y gastric bypass. Acta Obstet
Gynecol Scand 2012;91(July (7)):8735.
4. Ramirez MM, Turrentine MA. Gastrointestinal hemorrhage during pregnancy
in a patient with a history of vertical-banded gastroplasty. Am J Obstet Gynecol
1995;173(November (5)):16301.
5. Leal-Gonzalez R, Garza-Ramos R, Guajardo-Perez H, Ayala-Aguilera F, Rumbaut
R. Internal hernias in pregnant women with history of gastric bypass surgery:
case series and review of literature. Int J Surg Case Rep 2013;4(1):447.
6. Loar III PV, Sanchez-Ramos L, Kaunitz AM, Kerwin AJ, Diaz J. Maternal
death caused by midgut volvulus after bariatric surgery. Am J Obstet Gynecol
2005;193(November (5)):17489.
7. Thompson JS, DiBaise JK, Iyer KR, Yeats M, Sudan DL. Postoperative short bowel
syndrome. J Am Coll Surg 2005;201(July (1)):859.
8. Boland E, Thompson JS, Grant WJ, Botha J, Langnas AN, Mercer DF. Massive
small bowel resection during pregnancy causing short bowel syndrome. Am
Surg 2011;77(December (12)):158992.
9. Genton L, Nardo P, Huber O, Pichard C. Parenteral nutrition independence
in a patient left with 25 cm of ileum and jejunum: a case report. Obes Surg
2010;20(May (5)):66671.
CASE REPORT OPEN ACCESS
M.K. Borghede et al. / International Journal of Surgery Case Reports 4 (2013) 11001103
10. Charles A, Domingo S, Goldfadden A, Fader J, Lampmann R, Mazzeo R. Small
bowel ischemia after Roux-en-Y gastric bypass complicated by pregnancy: a
case report. Am Surg 2005;71(March (3)):2314.
11. Efthimiou E, Stein L, Court O, Christou N. Internal hernia after gastric bypass
surgery during middle trimester pregnancy resulting in fetal loss: risk of internal
hernia never ends. Surg Obes Relat Dis 2009;5(May (3)):37880.
12. Gazzalle A, Braun D, Cavazzola LT, Wendt LR, Navarini D, Fauri MA, et al. Late
intestinal obstruction due to an intestinal volvulus in a pregnant patient with a
previous Roux-en-Y gastric bypass. Obes Surg 2010;20(December (12)):17402.
1103
13. Hooks III WB, Westbrook AD, Clancy TV, Hope WW. Small bowel obstruction
in a postpartum woman after laparoscopic Roux-en-Y gastric bypass. Surg Obes
Relat Dis 2010;6(March (2)):20910.
14. Moore KA, Ouyang DW, Whang EE. Maternal and fetal deaths after gastric bypass surgery for morbid obesity. N Engl J Med 2004;351(August (7)):
7212.
15. Wang CB, Hsieh CC, Chen CH, Lin YH, Lee CY, Tseng CJ. Strangulation of upper
jejunum in subsequent pregnancy following gastric bypass surgery. Taiwan J
Obstet Gynecol 2007;46(September (3)):26771.
Вам также может понравиться
- Asma - NelsonДокумент22 страницыAsma - NelsonVmiguel LcastilloОценок пока нет
- 19 Claves STR Nº19 Final Usamedic 2017 Print PDFДокумент1 страница19 Claves STR Nº19 Final Usamedic 2017 Print PDFVmiguel LcastilloОценок пока нет
- 21 Claves STR #21 Final Usamedic 2017 PDFДокумент1 страница21 Claves STR #21 Final Usamedic 2017 PDFVmiguel LcastilloОценок пока нет
- Respuesta in MuneДокумент23 страницыRespuesta in MuneVmiguel LcastilloОценок пока нет
- Ranking General 2do Sim NacionalДокумент13 страницRanking General 2do Sim NacionalVmiguel LcastilloОценок пока нет
- Predictores de CorioДокумент12 страницPredictores de CorioVmiguel LcastilloОценок пока нет
- Diabetology & Metabolic Syndrome: Post-Transplant Diabetes MellitusДокумент4 страницыDiabetology & Metabolic Syndrome: Post-Transplant Diabetes MellitusVmiguel LcastilloОценок пока нет
- Journal of Pediatric Surgery: Wendy K. Fujioka, Robert A. CowlesДокумент3 страницыJournal of Pediatric Surgery: Wendy K. Fujioka, Robert A. CowlesVmiguel LcastilloОценок пока нет
- P 44Документ10 страницP 44hannediantaОценок пока нет
- Itu en DiabetesДокумент6 страницItu en DiabetesVmiguel LcastilloОценок пока нет
- Nri 3341Документ14 страницNri 3341Vmiguel LcastilloОценок пока нет
- 1 s2.0 S2212267213005182 MainДокумент9 страниц1 s2.0 S2212267213005182 MainVmiguel LcastilloОценок пока нет
- Antitumor Effects of Octreotide LAR, A Somatostatin AnalogДокумент2 страницыAntitumor Effects of Octreotide LAR, A Somatostatin AnalogVmiguel LcastilloОценок пока нет
- Self-Medication in Older Urban Mexicans: An Observational, Descriptive, Cross-Sectional StudyДокумент2 страницыSelf-Medication in Older Urban Mexicans: An Observational, Descriptive, Cross-Sectional StudyVmiguel LcastilloОценок пока нет
- Team 13BДокумент13 страницTeam 13BVmiguel LcastilloОценок пока нет
- PNTD 0001819Документ12 страницPNTD 0001819Vmiguel LcastilloОценок пока нет
- 1 285 1 PBДокумент5 страниц1 285 1 PBVmiguel LcastilloОценок пока нет
- Automedicación en Brasil)Документ7 страницAutomedicación en Brasil)Vmiguel LcastilloОценок пока нет
- Suicidality and Depression Disparities Between Sexual Minority and Heterosexual YouthДокумент9 страницSuicidality and Depression Disparities Between Sexual Minority and Heterosexual YouthVmiguel LcastilloОценок пока нет
- Prediction Clinical Profile To Distinguish Between Systolic and Diastolic Heart Failure in Hospitalized PatientsДокумент6 страницPrediction Clinical Profile To Distinguish Between Systolic and Diastolic Heart Failure in Hospitalized PatientsVmiguel LcastilloОценок пока нет
- Upper GI BleedingДокумент24 страницыUpper GI BleedingRosalía Arroyo FloresОценок пока нет
- Embriologia Del Sistema Urogenital y Anomalias CongenitasДокумент42 страницыEmbriologia Del Sistema Urogenital y Anomalias CongenitasVmiguel LcastilloОценок пока нет
- Quiste Pancreatico - Revisión - Colegio Americano de CirugiaДокумент9 страницQuiste Pancreatico - Revisión - Colegio Americano de CirugiaVmiguel LcastilloОценок пока нет
- JNC 8 PDFДокумент14 страницJNC 8 PDFAlan NophalОценок пока нет
- Prevención de Eventos Tromboembólicos en Cirugía GinecológicaДокумент13 страницPrevención de Eventos Tromboembólicos en Cirugía GinecológicaVmiguel LcastilloОценок пока нет
- Antibioticos para Vias Respiratorias AltasДокумент12 страницAntibioticos para Vias Respiratorias AltasVmiguel LcastilloОценок пока нет
- Vacunación Contra Malaria - RevisiónДокумент3 страницыVacunación Contra Malaria - RevisiónVmiguel LcastilloОценок пока нет
- Ti41 04Документ0 страницTi41 04Vmiguel LcastilloОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Marieb - Chapter 10 Muscular System Lecture 17Документ20 страницMarieb - Chapter 10 Muscular System Lecture 17kuyha kuyhaОценок пока нет
- CGHS Rates - Chandigarh1Документ111 страницCGHS Rates - Chandigarh1renuОценок пока нет
- Congenital Diaphragmatic Hernias (CDH)Документ24 страницыCongenital Diaphragmatic Hernias (CDH)tsega tilahunОценок пока нет
- Opd NewДокумент42 страницыOpd NewNaima YaseenОценок пока нет
- Hernia OSCE ExaminationДокумент3 страницыHernia OSCE ExaminationkylieverОценок пока нет
- Hernia: Information For PatientsДокумент2 страницыHernia: Information For Patientsrianrifaldi123_98497Оценок пока нет
- Assessing The Male GenitaliaДокумент23 страницыAssessing The Male GenitaliaArjay Christian Del RosarioОценок пока нет
- PEDIA PresentationДокумент195 страницPEDIA PresentationKatrina Lim-HatagueОценок пока нет
- Tap Block ThesisДокумент8 страницTap Block Thesisafaybjktm100% (1)
- Surgery PDF 4TH Yr 7TH Sem Solved On The Basis of Previous Yr Paper and Books Ankit AkelaДокумент25 страницSurgery PDF 4TH Yr 7TH Sem Solved On The Basis of Previous Yr Paper and Books Ankit Akelachai rinОценок пока нет
- GIT SurgeryДокумент24 страницыGIT SurgerySaja Hussein95Оценок пока нет
- Kr2med 2005engДокумент60 страницKr2med 2005engHind YousifОценок пока нет
- Laparoscopic Hernia Repair: Eva Deerenberg, Irene Mulder and Johan LangeДокумент25 страницLaparoscopic Hernia Repair: Eva Deerenberg, Irene Mulder and Johan LangeKamran AfzalОценок пока нет
- Basics of Laparoscopy: Anirudha DoshiДокумент54 страницыBasics of Laparoscopy: Anirudha DoshiAnirudha DoshiОценок пока нет
- Detailed Lesson Plan (DLP) Format: Instructional PlanningДокумент9 страницDetailed Lesson Plan (DLP) Format: Instructional PlanningMerce Tojino ManigosОценок пока нет
- CGHS Rates 2014 - BhopalДокумент40 страницCGHS Rates 2014 - BhopalUpendra SahuОценок пока нет
- Examination of HerniaДокумент2 страницыExamination of HerniaNabighah ZukriОценок пока нет
- HERNIAДокумент34 страницыHERNIAAtiqah ShahОценок пока нет
- Acute AbdomenДокумент30 страницAcute Abdomenraisa cesarda100% (1)
- 06 Inguinal Hernia SrsДокумент10 страниц06 Inguinal Hernia SrslowhillОценок пока нет
- Hernia - Surgery PrecisДокумент1 страницаHernia - Surgery PrecisSherif WagdyОценок пока нет
- Surgery Cycle MCQSДокумент27 страницSurgery Cycle MCQSHeeb Warda100% (1)
- Ventral Hernia Causes and ManagementДокумент13 страницVentral Hernia Causes and ManagementOttofianus Hewick KalangiОценок пока нет
- Is Baar Sabka Achha HogaДокумент29 страницIs Baar Sabka Achha HogasurajmotwaniОценок пока нет
- Name: Emanuel Charles Coates Registration #: 2018010033 Topic: Case Inguinal HerniaДокумент11 страницName: Emanuel Charles Coates Registration #: 2018010033 Topic: Case Inguinal Herniaemanuel coatesОценок пока нет
- SURGERY 2018-2008 Regular-Supplementary Chapter Wise Question Papers WBUHSДокумент16 страницSURGERY 2018-2008 Regular-Supplementary Chapter Wise Question Papers WBUHSAnirban ChakrabortyОценок пока нет
- Professional Guide To Signs and Symptoms 6th Edition PDFДокумент822 страницыProfessional Guide To Signs and Symptoms 6th Edition PDF1102sn83% (6)
- MainДокумент3 страницыMaindivyanshu kumarОценок пока нет
- Final Past Papers With Common MCQS: MedicineДокумент17 страницFinal Past Papers With Common MCQS: MedicineKasun PereraОценок пока нет
- Hernia PDFДокумент5 страницHernia PDFAngelica SanabriaОценок пока нет