Академический Документы
Профессиональный Документы
Культура Документы
Guidelines Insulin PDF
Загружено:
YulizalOkИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Guidelines Insulin PDF
Загружено:
YulizalOkАвторское право:
Доступные форматы
DOCUMENT REFERENCE NO: WE/08/GUI0005/NM
Type: Guideline
Diabetes Insulin initiation and adjustment
Relevant to: Clinicians involved with diabetes
Produced by:
Responsible Executive Director:
Date of Approval:
Date of Implementation:
Due Review Date:
Responsible Reviewing Officer:
This document replaces:
Signed:
Community DSN, Primary Care Support
Director of Commissioning
04.01.2010
Immediate after Approval
04.01.2012
Community DSN, Primary Care Support
Diabetes Insulin initiation and
adjustment Version 1 (May 2008)
Chief Executive:
For Office Use Only
Scheme of Publication
Drive:
Name:
X
Scheme of
Publication
Section no:
5
Sub Folder:
commissioning
NHS West Essex Diabetes Insulin Initiation and adjustment
Version 2 January 2010
Issued February 2010
File: as above
WE/08/GUI0005/NM
Page 1 of 6
POLICY VALIDITY STATEMENT
THIS POLICY IS DUE FOR REVIEW ON
04.01.2012
After this date, this document will become invalid.
Policy users should ensure that they are consulting the
currently valid version of the documentation.
Initial insulin prescription
NHS West Essex Diabetes Insulin Initiation and adjustment
Version 2 January 2010
Issued February 2010
WE/08/GUI0005/NM
Page 2 of 6
Indications:
Type 2 diabetes, where oral therapies are failing to achieve
desired target levels
Usual target levels:
HbA1c 7.0%/53mmol/mol or less
Blood glucose before meals 4 7 mmol/l
Blood glucose after meals 6 8 mmol/l
Individual targets according to circumstances may apply
Select from the following options: Once daily insulin choose one:
Good choice for older patients or
introduction to insulin. May achieve
target where HbA1c <8.5%
Gives constant background level.
Continue OHAs (except glitazones)
Use Lantus/Levemir 1st choice where
hypos are a risk
Insulatard or Humulin I first choice
Rx = novopen 4 + Insulatard penfill cartridge
or Innolet (egg timer) disposable
or Humapen Luxura + penfill cartridges
or Humulin I Kwikpen (disposable)
or
Lantus
Rx = Lantus Solostar prefilled disposable
pen
or
Levemir
Rx = Levemir Flexpen (disposable) or
3 ml penfill Levemir cartridges with
Novopen 4 (or Innolet egg timer)
Good for reasonably active, but fairly
habitual lifestyle
Probably better where HbA1c >8.5%/
68 mmol/mol
Stop OHAs (except Metformin)
b.d. mixture
Novomix 30
Rx = Novomix 30 Flexpen (disposable)
OR
Novomix 30 penfill cartridges with Novopen 4
Humalog Mix 25 Rx = Humapen Luxura + Humalog Mix 25
Cartridges or Mix 25 Kwikpen (disposable)
q.d.s (basal bolus)
Good for active lifestyle where
flexibility is important.
Stop OHAs (except Metformin)
Basal = Insulatard or Humulin I or
Lantus or Levemir
Bolus = Novorapid
Rx = as above Once daily
PLUS: Rx = Novorapid Flexpen
or
Novofill penfill cartridges plus
Novopen 4
Also prescribe for all patients:
Sharps safe/guard
Pen needles 6 mm (8 mm if obese)
Supply of blood glucose monitoring strips
BD Safeclip needle clipper
or
Bolus = Humalog (Lispro)
or
Bolus = Apidra
Rx = Humapen Luxura plus
Humalog cartridges or
Humalog Kwikpen
Rx = Apidra Solostar prefilled
disposable pen
Insulin titration
NHS West Essex Diabetes Insulin Initiation and adjustment
Version 2 January 2010
Issued February 2010
WE/08/GUI0005/NM
Page 3 of 6
B.D. (twice daily) insulin mixtures
Novomix 30/Humalog Mix 25
Start dose:
10 - 12 units with breakfast
8 - 10 units with evening meal
Insulin to be injected with meal or
within 15 minutes of eating
Monitor blood glucose twice daily:
Before breakfast and one other, e.g.: Before lunch/evening meal/bedtime/after
a meal
Pre-breakfast blood glucose > target
Increase evening insulin by 2 units (or
10%) every 3 days
Pre-evening meal blood glucose >
target
Increase morning insulin by 2 units (or
10%)
Adjust one dose at a time
Increase insulin by 2 units (or 10%) every 3 days to
achieve target levels usually: 4 - 7 mmol/l before meals
6 - 8 mmol/l after meals
If all blood glucose readings > 12 mmol/l increase
insulin by 4 units.
If blood glucose < 4.0 mmol/l at
any time, decrease nearest
preceding insulin dose by 2 units
(or 10%)
NB: referral to dietician is advisable
For further support and advice contact
Jackie Watts, Diabetes Specialist Nurse (Primary Care Support)
01279 827238
email: jacqueline.watts@westessexpct.nhs.uk
Insulin titration
NHS West Essex Diabetes Insulin Initiation and adjustment
Version 2 January 2010
Issued February 2010
WE/08/GUI0005/NM
Page 4 of 6
M.D.I/Basal bolus insulin
Basal dose: Start Insulatard or Humulin I or Levemir or Lantus 8 - 12 units at
bedtime/evening meal
*Bolus:
Start Novorapid/Humalog/Apidra 2 - 6 units with meals
(* dose according to carbohydrate of food)
Monitor blood glucose 4 times a day
Before breakfast plus others: before meals, after meals, before bed
Titrate basal (bedtime) insulin first in order to establish pre-breakfast levels
4 - 7 mmol/l by increases of 2 - 4 units (or 10%) every 3 days
NOTE: Increasing the basal dose may necessitate reduction of mealtime
(bolus) doses as it will raise general background insulin level
Once the correct basal dose is established, titrate mealtime (bolus)
doses by 2 units up or down to achieve post meal blood glucose levels of
6 - 8 mmol/l. Advise patient regarding adjusting according to prospective
carbohydrate content of the meal
NB: referral to dietician is advised
For further support and advice contact
Jackie Watts, Diabetes Specialist Nurse (Primary Care Support)
01279 827238
email: jacqueline.watts@westessexpct.nhs.uk
Insulin titration
NHS West Essex Diabetes Insulin Initiation and adjustment
Version 2 January 2010
Issued February 2010
WE/08/GUI0005/NM
Page 5 of 6
Once daily Insulatard, Humulin I, Levemir or Lantus
in combination with Oral Hypoglycaemic Agents (OHA)
Start dose 8 10 units
Usually given in the evening/bedtime
Monitor blood glucose twice daily
Before breakfast plus one other, e.g.: before lunch/evening meal/bedtime/after meal
Increase by 2 units (or 10%) every 3 days to achieve pre-breakfast
target usually 4 7 mmol/l
(if all blood glucose readings > 10 mmol/l increase by 4 units)
N.B: Usual post-meal and pre-bed target 6 8 mmo/l
N.B: If blood glucose < 4 mmol/l reduce dose by 2 units or 10%
NB: referral to dietician is advised
For further support and advice contact
Jackie Watts, Diabetes Specialist Nurse (Primary Care Support)
01279 827238
email: jacqueline.watts@westessexpct.nhs.uk
NHS West Essex Diabetes Insulin Initiation and adjustment
Version 2 January 2010
Issued February 2010
WE/08/GUI0005/NM
Page 6 of 6
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (120)
- HypoglycemiaДокумент17 страницHypoglycemiaJohnjohn Mateo100% (1)
- Treatment Based On: Pathophysiology of HyperglycemiaДокумент38 страницTreatment Based On: Pathophysiology of HyperglycemiaRoby KieranОценок пока нет
- 2.1 The Importance of Reducing Hypoglycaemia - Dr. Rudy Mokodompit.,Sp - PDДокумент16 страниц2.1 The Importance of Reducing Hypoglycaemia - Dr. Rudy Mokodompit.,Sp - PDakhmadidrisbayuОценок пока нет
- Diabetic Ketoacidosis LOДокумент19 страницDiabetic Ketoacidosis LOlzbthshayОценок пока нет
- Dka and HHSДокумент25 страницDka and HHSMouhammad Dawoud100% (2)
- Nut Stat BMI-for-Age GIRLSДокумент4 страницыNut Stat BMI-for-Age GIRLSSheryl HorcaОценок пока нет
- Clinical Chemistry Case AnalysisДокумент6 страницClinical Chemistry Case Analysisaliana100% (5)
- Hba1 Conversion Table: DefinitionsДокумент1 страницаHba1 Conversion Table: DefinitionsWidya Astri LinteraОценок пока нет
- DIABETES InfographicДокумент1 страницаDIABETES InfographicDail Xymere YamioОценок пока нет
- Arterial Blood Gas InterpretationДокумент9 страницArterial Blood Gas InterpretationSunny AghniОценок пока нет
- Neonatal Diabetes Mellitus: DR Nahim DM Neo Resident, ICH & HCДокумент62 страницыNeonatal Diabetes Mellitus: DR Nahim DM Neo Resident, ICH & HCBhupendra GuptaОценок пока нет
- Mod 9 DMДокумент3 страницыMod 9 DMRoxanne Nasingao100% (1)
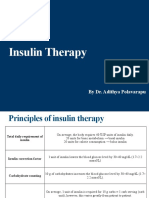
- Insulin Therapy: by Dr. Adithya PolavarapuДокумент18 страницInsulin Therapy: by Dr. Adithya Polavarapuadithya polavarapuОценок пока нет
- Parathyroid Glands, High Calcium, and HyperparathyroidismДокумент2 страницыParathyroid Glands, High Calcium, and HyperparathyroidismsyafeiОценок пока нет
- Type 1 DiabetesДокумент8 страницType 1 DiabetesSam SyawallОценок пока нет
- Quality of Life in Diabetes - Tutorial 4Документ10 страницQuality of Life in Diabetes - Tutorial 4Axiu Xabi'alonsoNyОценок пока нет
- Sample Doctor Letter From Practical Diabetology PDFДокумент1 страницаSample Doctor Letter From Practical Diabetology PDFPainОценок пока нет
- Department of Education School Form 8 Learner's Basic Health and Nutrition Report (SF8)Документ9 страницDepartment of Education School Form 8 Learner's Basic Health and Nutrition Report (SF8)Ireneo Aposacas Jr.Оценок пока нет
- Tata Laksana DM Dan Hipertensi Sesuai StandarДокумент32 страницыTata Laksana DM Dan Hipertensi Sesuai Standardesi eka restiОценок пока нет
- Risk Factors For Progression To Referable Diabetic.11Документ11 страницRisk Factors For Progression To Referable Diabetic.11library SDHBОценок пока нет
- Acanthosis Nigricans in Obese Versus Non-Obese in A Tertiary Care Hospital Association With Bmi and Central ObesityДокумент10 страницAcanthosis Nigricans in Obese Versus Non-Obese in A Tertiary Care Hospital Association With Bmi and Central ObesityIJAR JOURNALОценок пока нет
- ADA GuidlinesДокумент154 страницыADA GuidlinesJazmin AguillonОценок пока нет
- What Is DiabetesДокумент2 страницыWhat Is DiabetesJewel BrondaОценок пока нет
- ID Geriatric With Diabetes Melitus UncontroДокумент8 страницID Geriatric With Diabetes Melitus UncontroArfa RahmahОценок пока нет
- History of Pump TechnologyДокумент9 страницHistory of Pump TechnologyMridula Ayush BhargavaОценок пока нет
- QuizДокумент8 страницQuizTareq EmadОценок пока нет
- Diabetes Mellitus Complications: Ssenabulya F Ronny MBCHB V Moderator Dr. Mutebi 4B Endocrinology UnitДокумент55 страницDiabetes Mellitus Complications: Ssenabulya F Ronny MBCHB V Moderator Dr. Mutebi 4B Endocrinology UnitNinaОценок пока нет
- Hyper - and HypoglycemiaДокумент3 страницыHyper - and HypoglycemiaaerugiОценок пока нет
- (MM2016-3-73) Artur Chwalba, Ewa Otto-Buczkowska: Nowe, Pediatryczne Wskazania Do Stosowania Metforminy - Systematyczny PrzeglądДокумент6 страниц(MM2016-3-73) Artur Chwalba, Ewa Otto-Buczkowska: Nowe, Pediatryczne Wskazania Do Stosowania Metforminy - Systematyczny PrzeglądTowarzystwo Edukacji TerapeutycznejОценок пока нет
- Pre-Diabetes:: Don't Let It Lead To Type-2Документ1 страницаPre-Diabetes:: Don't Let It Lead To Type-2ARIA MINDОценок пока нет