Академический Документы
Профессиональный Документы
Культура Документы
Nej M 199907293410514
Загружено:
Adina OlteanuОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Nej M 199907293410514
Загружено:
Adina OlteanuАвторское право:
Доступные форматы
CORR ES POND ENCE
Correspondence
Delirium in Hospitalized Older Patients
To the Editor: In their study of the prevention of delirium in hospitalized older patients (March 4 issue),1 Inouye
et al. provide data on the cumulative incidence of delirium
as a function of the length of hospitalization that suggest
that prolonged exposure to the hospital environment itself
is a significant risk factor for delirium. These data support
the need for effective plans for early discharge of older patients and suggest the need to assess whether providing
hospital-level care to older persons in more hospitable environments than acute care hospitals, such as home hospitals,2,3 could reduce the incidence of hospital-related complications such as delirium.
BRUCE LEFF, M.D.
Johns Hopkins University School of Medicine
Baltimore, MD 21224
1. Inouye SK, Bogardus ST Jr, Charpentier PA, et al. A multicomponent
intervention to prevent delirium in hospitalized older patients. N Engl J
Med 1999;340:669-76.
2. Leff B, Burton LC, Guido S, Greenough WB, Steinwachs D, Burton
JR. Home hospital program: a pilot study. J Am Geriatr Soc (in press).
3. Gravil JH, Al-Rawas OA, Cotton MM, Flanigan U, Irwin A, Stevenson
RD. Home treatment of exacerbations of chronic obstructive pulmonary
disease by an acute respiratory assessment service. Lancet 1998;351:18535.
To the Editor: . . . We have two criticisms of the study
by Inouye et al. The first is related to the authors decision
to exclude almost 100 patients because of a language bar-
rier. The reason for this decision is difficult to understand,
since hospitals are required to provide translators for patients who do not speak English. Miscommunication resulting from a language barrier may in itself contribute to
the development of delirium, particularly when it occurs
in the setting of an acute and catastrophic illness. In our
multicultural society, this possibility should be taken into
account by physicians who are considering interventions
to prevent delirium in the elderly.
Our second comment relates to the authors failure to
include a component concerning patients families and
their integration into the medical care system. The omission of this component is also difficult to understand,
since the authors themselves cite a previous study in which
such a component was reported to be beneficial.1 Perhaps
having a gerontologic social worker involved would further reduce the risks of delirium in hospitalized elderly
patients.
V.A. PORTNOI, M.D.
T. REDLING, D.O.
S.C. AMESTY, M.D.
Beth Israel Medical Center
New York, NY 10003
1. Chatham MA. The effect of family involvement on patients manifestations of postcardiotomy psychosis. Heart Lung 1978;7:995-9.
To the Editor: Both the study by Inouye et al. and the
accompanying editorial by Rowe1 discuss delirium as if it
were a condition like coronary artery disease, which can
be prevented by targeting base-line risk factors. These risk
factors are the so-called benign causes of delirium (e.g.,
acute confusion in response to the novel and frightening
hospital environment) in persons with cognitive, visual,
or hearing impairment or all three conditions. The study
by Inouye et al. demonstrates that we can potentially reduce the overall incidence of delirium by targeting these
risk factors.
Delirium is, however, often the first sign of an impend-
INSTRUCTIONS FOR LETTERS TO THE EDITOR
Letters to the Editor are considered for publication (subject to editing and abridgment) provided they do not contain material that has been
submitted or published elsewhere. Please note the following: Your letter must be typewritten and triple-spaced. Its text, not including
references, must not exceed 400 words (please include a word count). It must have no more than five references and one figure or table.
It should not be signed by more than three authors. Letters referring to a recent Journal article must be received within four weeks of its
publication. Please include your full address, telephone number, and fax number (if you have one). You may send us your letter by post, fax,
or electronic mail.
Our address: Letters to the Editor New England Journal of Medicine 10 Shattuck St. Boston, MA 02115
Our fax numbers: 617-739-9864 and 617-734-4457
Our e-mail address: letters@nejm.org
We cannot acknowledge receipt of your letter, but we will notify you when we have made a decision about publication. We are unable to
provide prepublication proofs. Please enclose a stamped, self-addressed envelope if you want unpublished material returned to you.
Financial associations or other possible conflicts of interest must be disclosed. Submission of a letter constitutes permission for the Massachusetts Medical Society, its licensees, and its assignees to use it in the Journal s various editions (print, data base, and optical disk) and in
anthologies, revisions, and any other form or medium.
Vol ume 341
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2015. For personal use only. No other uses without permission.
Copyright 1999 Massachusetts Medical Society. All rights reserved.
Numb e r 5
369
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
ing medical disaster in elderly and other vulnerable patients. Its onset should trigger a rapid and thorough search
for life-threatening medical illnesses that may have caused
it. In his classic studies of delirium, Lipowski found that
as many as one third of elderly patients who are hospitalized for medical reasons and in whom delirium develops
die within 30 days.2,3 The leading cause is infection, with
metabolic derangements and failures of other organ systems following close behind.4 As Eidelman et al. demonstrated in patients with sepsis, delirium is strongly associated with more severe disease and increased mortality
rates.5 Clearly, all patients should have the type of prophylactic interventions that Inouye et al. propose as part of
high-quality medical care. Nevertheless, when delirium
occurs, it should be treated as a potentially life-threatening
emergency.
CHARLES E. SCHWARTZ, M.D.
Montefiore Medical Center
Bronx, NY 10467
1. Rowe JW. Geriatrics, prevention, and the remodeling of Medicare.
N Engl J Med 1999;340:720-1.
2. Lipowski ZJ. Delirium in the elderly patient. N Engl J Med 1989;320:
578-82.
3. Idem. Transient cognitive disorders (delirium, acute confusional states)
in the elderly. Am J Psychiatry 1983;140:1426-36.
4. Wise MG, Lieberman JA III. Delirium, dementia, and amnestic disorders. In: Goldman LS, Wise TN, Brody DS, eds. Psychiatry for primary
care physicians. Chicago: American Medical Association, 1998:140.
5. Eidelman LA, Putterman D, Putterman C, Sprung CL. The spectrum
of septic encephalopathy: definitions, etiologies, and mortalities. JAMA
1996;275:470-3.
To the Editor: Behavioral interventions and environmental control are important in the management of delirium, as the study by Inouye et al. underscores. It is also
useful to prepare the family and the medical and surgical
staff for the likely emergence of delirium in high-risk patients. Delirium is very likely to occur in elderly patients
with dementia who are in pain and who are subjected to
surgery, sedation, and new surroundings, such as those
undergoing elective joint replacement. Families benefit
from knowing that delirium is a possibility and from understanding what delirium entails. There is an associated
risk of injury with delirium, of course, and this point
should really be brought out in the informed-consent
process. Metabolic encephalopathies in elderly patients
with some degree of cognitive impairment may take 6 to
12 weeks to resolve.
BRUCE D. SNYDER, M.D.
Minneapolis Clinic of Neurology
Golden Valley, MN 55422
SHARON K. INOUYE, M.D., M.P.H.
Yale University School of Medicine
New Haven, CT 06504
1. Inouye SK. The dilemma of delirium: clinical and research controversies
regarding diagnosis and evaluation of delirium in hospitalized elderly medical patients. Am J Med 1994;97:278-88.
2. Idem. Delirium in hospitalized older patients. Clin Geriatr Med 1998;
14:745-64.
3. Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons: predictive model and interrelationship with baseline
vulnerability. JAMA 1996;275:852-7.
Risk Factors for Schizophrenia
Dr. Inouye replies:
To the Editor: Dr. Schwartz stresses that delirium is often
a warning sign of life-threatening disease and frequently
serves as a barometer of the underlying health of elderly
patients.1,2 The development of delirium should be handled as a potential medical emergency, prompting a careful medical evaluation and a search for the underlying
370
causes. The high morbidity and mortality rates associated
with delirium, however, highlight the need for broader approaches to prevent delirium by addressing known risk factors.3 The iatrogenic influences contributing to delirium
during hospitalization (including the use of psychoactive
medications, immobilization, sleep deprivation, dehydration, and disorienting influences) are far from benign; and
as our findings suggested, reducing them will substantially
reduce the rates of delirium.
Dr. Portnoi and colleagues raise the important clinical
issue of the need to provide translators to minimize the
risk of miscommunication and to keep patients oriented
and informed during hospitalization. Although the lack of
translators has not been demonstrated to increase the risk
of delirium, we concur that it is likely to be a risk factor.
Despite great efforts to maximize the use of existing translation services and to recruit translators from the hospital
and the community, logistic constraints precluded us from
enrolling many patients with a language barrier, because
not enough translators were available to cover the multiple
interactions with patients that were required by the protocol for 12 hours each day.
We considered many other interventions to prevent delirium, including those involving patients families, physicians, social workers, and chaplains. The chief criticism of
multicomponent intervention trials has concerned the
number, complexity, and unfocused or difficult-to-replicate nature of the interventions. Thus, we limited the
number of interventions in the trial. The final choices were
based on the effectiveness, feasibility, and reproducibility
of the interventions. We agree that many other important
interventions were not examined and remain important areas for future research.
Dr. Leff s proposal that the home hospital is an environment that will reduce the risk of delirium is compelling, and it should be examined in future studies. On the
basis of our work, we would recommend interventions to
eliminate risk factors for delirium (e.g., avoid immobilization and provide reorientation) in the home setting
as well.
To the Editor: Mortensen et al. (Feb. 25 issue)1 acknowledge that a family history of schizophrenia is the bestestablished risk factor for the disorder but suggest that environmental factors, including the place and season of birth,
are major determinants. This argument is based on estimates of the population attributable risk regarding factors
Jul y 2 9 , 19 9 9
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2015. For personal use only. No other uses without permission.
Copyright 1999 Massachusetts Medical Society. All rights reserved.
CORR ES POND ENCE
point to genetic or early neurodevelopmental factors (or
both) as major determinants.
70
Population Attributable Risk (%)
RR=3.0
60
PETER MCGUFFIN, M.B., PH.D.
50
Institute of Psychiatry
London SE5 8AF, United Kingdom
RR=2.0
IRVING I. GOTTESMAN, PH.D.
40
University of Virginia
Charlottesville, VA 22903
RR=1.5
30
20
10
0
0
10
20
30
40
50
60
70
80
90
1. Mortensen PB, Pedersen CB, Westergaard T, et al. Effects of family history and place and season of birth on the risk of schizophrenia. N Engl
J Med 1999;340:603-8.
2. Kramer MS. Clinical epidemiology and biostatistics: a primer for clinical
investigators and decision-makers. Berlin, Germany: Springer-Verlag, 1988.
3. Cardno AG, Marshall EJ, Coid B, et al. Heritability estimates for psychotic disorders: the Maudsley twin psychosis series. Arch Gen Psychiatry
1999;56:162-8.
4. McGuffin P, Owen MJ, ODonovan MC, Thapar A, Gottesman II.
Seminars in psychiatric genetics. London: Gaskell, 1994.
Prevalence of Risk Factor (%)
Figure 1. Relation between the Population Attributable Risk and
the Prevalence of a Risk Factor When the Relative Risk (RR) Is
Fixed.
found to be associated with schizophrenia in their population-based cohort. Unfortunately, their assertions about
the relative importance of various risk factors overlook the
fact that the calculation of population attributable risk is
dependent on the frequency of the risk factor in a population. The calculation of relative risk, however, is not dependent on the population base rate. Thus, for a given relative risk (RR), the population attributable risk can be
calculated with use of the following equation: population
attributable risk=P(RR1)P[(RR1)+1], where P is
the prevalence of the risk factor in the population.2
Figure 1 shows the curvilinear relation between the
population attributable risk and the prevalence of a risk
factor for three fixed relative risks and demonstrates that a
modest relative risk can correspond to a very high attributable risk if the risk factor is common.
Thus, although Mortensen and colleagues have provided us with an elegant set of epidemiologic data on schizophrenia, their interpretation of these data is questionable.
Their ability to replicate the associations between the season of birth, the place of birth, and schizophrenia is intriguing, but far from demonstrating that these are proxy
variables for major environmental factors, the findings
probably reveal that in Denmark, more people live in urban areas or are born in February or March than have a
first-degree relative with schizophrenia. The relative risk of
schizophrenia among the identical twins of patients with
schizophrenia is about 503,4 and is little changed in the
small sample of identical twins reared apart. The relative
risk among adopted children in Denmark with a biologic
parent with schizophrenia is about 10,4 which is well within the range reported1 for children reared in the same
household as an affected parent. Such findings seem to
To the Editor: In the study by Mortensen et al. of risk
factors for schizophrenia, the ratio of males to females was
2.3:1.0 in the 2669 patients with schizophrenia. Clinical
information on both parents was available for 91 percent
of the patients, and 120 affected parents were identified
(37 fathers and 83 mothers). Unless there is a sex-specific
genetic risk factor, the male:female ratio in the group of
affected parents should resemble that in the probands; instead, the ratio was reversed (1.0:2.2). With this correction for male predominance, chi-square analysis comparing the observed and expected ratios in the 120 affected
parents reveals a statistically significant difference (P<
0.001). Even if one conservatively predicts that an equal
number of fathers and mothers will be affected, the observed and expected ratios are significantly different
(P<0.001).
In this data set, there is either an overrepresentation of
affected mothers or an underrepresentation of affected
fathers. The latter case is possible, since the clinical histories of 251 fathers were unknown; if we assume that the
male:female ratio in the group of affected parents reflects
the ratio in the probands, 154 of these unknown fathers
should have schizophrenia, a rather high proportion. Alternatively, a maternally inherited genetic factor, either
X-linked or mitochondrial, could account for an overrepresentation of affected mothers.
This finding of a reversal of the male:female ratio from
one generation of patients with schizophrenia to the next
is not unique.1 Although the explanation for this change
is unclear, it is important to note that in mitochondrial
genetics there can be sporadic expression of maternally
inherited phenotypes and that the expression of mitochondrial genes appears to be altered in patients with
schizophrenia.2
RUSSELL H. SWERDLOW, M.D.
DANIEL BINDER, B.S.
W. DAVIS PARKER, M.D.
University of Virginia Health Sciences Center
Charlottesville, VA 22908
Vol ume 341
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2015. For personal use only. No other uses without permission.
Copyright 1999 Massachusetts Medical Society. All rights reserved.
Numb e r 5
371
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
1. Shimizu A, Kurachi M, Yamaguchi N, Torii H, Isaki K. Morbidity risk
of schizophrenia to parents and siblings of schizophrenic patients. Jpn J
Psychiatry Neurol 1987;41:65-70.
2. Whatley SA, Curti D, Marchbanks RM. Mitochondrial involvement in
schizophrenia and other functional psychoses. Neurochem Res 1996;21:
995-1004.
To the Editor: Mortensen et al. correlated the incidence
of schizophrenia according to the month of birth and
found the highest incidence among those born in February and March and the lowest incidence among those born
in August and September. In the entire population studied, were more children born in February and March than
in August and September? Among those in whom schizophrenia did not develop, how many were born in February
and March and how many in August and September?
RALPH WEILERSTEIN, M.D.
Phenylketonuria is an example of a disease that could
be eliminated either by removing the susceptible genotype or by removing phenylalanine from the diet (i.e.,
the attributable risk for each factor is 100 percent). At
present, primary prevention of schizophrenia is not possible. However, just as for phenylketonuria, in the future
there may be more than one way of preventing schizophrenia. Whether preventive measures targeting genetic
or environmental factors are feasible, however, remains in
question.
PREBEN BO MORTENSEN, D.M.SC.
Psychiatric Hospital of Aarhus
DK-8240 Risskov, Denmark
CARSTEN BCKER PEDERSEN, M.SC.
Statens Serum Institut
DK-2300 Copenhagen, Denmark
1080 Miller Ave.
Berkeley, CA 94708
HENRIK EWALD, D.M.SC.
Psychiatric Hospital of Aarhus
DK-8240 Risskov, Denmark
The authors reply:
To the Editor: Swerdlow et al. suggest that X-linked or
mitochondrial inheritance could account for the difference
in the male:female ratio between the affected parents of
patients with schizophrenia and their offspring. However,
we believe that the explanation is more simple: a relatively
smaller proportion of men with schizophrenia than of
women with schizophrenia have any children. The possibility is confirmed by comparing the relative number of
person-years at risk for men and women in Table 1 of our
paper.
Regarding Weilersteins comment: the relative numbers
of births in February and March and in August and September were taken into account in the analyses that included the exact number of person-years of exposure to
risk for subjects born in each of these months.
McGuffin and Gottesman disagree with our suggestion
that environmental factors can be major determinants of
schizophrenia. Instead, they suggest that the high relative
risk of schizophrenia among the identical twins of affected
patients and adopted children who had a parent with
schizophrenia means that genetic or early neurodevelopmental factors are the major determinants. They ascribe
the high population attributable risk we reported to the
high frequency of the factors we studied in other
words, many people are born in cities or during February
and March. Although we agree with many of their comments, we do not agree that on this basis, our conclusion
is erroneous.
As McGuffin and Gottesman point out, the population
attributable risk has two determinants, the relative risk and
the frequency of the exposure in a population. The unknown risk factors underlying the association between
schizophrenia and the season or place of birth may be
common and therefore of substantial importance on a
population level, even if the risk associated with them is
small, or even trivial, for any individual subject. We do not
challenge the role of genes in causing schizophrenia, nor
do we find it fruitful to view genetic and environmental
risk factors as competing or mutually exclusive.
372
Calcium-Channel Blockade and Hypertension
To the Editor: Tuomilehto and colleagues present a post
hoc analysis (March 4 issue)1 of a trial of nitrendipinebased treatment for older patients with isolated systolic
hypertension.2 The authors evaluated the outcome in patients with diabetes, a group that accounted for 10 percent
of the population originally studied. It is difficult and often misleading to make meaningful conclusions on the basis of an analysis of small subgroups chosen after the study
design has been established and the results recorded.
However, the authors conclude that antihypertensive treatment with dihydropyridine calcium-channel blockers may
be particularly helpful for patients with diabetes, not
harmful as mounting evidence suggests.3
The active-treatment group in the study received various
combinations of nitrendipine, enalapril, and hydrochlorothiazide, and the control group received placebo alone.
Only half the patients in the active-treatment group, including diabetic and nondiabetic patients, received nitrendipine alone, and the number of cardiovascular events in
this subgroup did not differ significantly from the number
in the placebo group (75 vs. 77 events), despite a substantial reduction in systolic and diastolic blood pressure. It is
unfortunate that the authors chose not to provide more
details on the effect of nitrendipine alone, including statistically significant differences, in the original article or in
a subsequent subgroup analysis.2,4 The other half of the
patients in the active-treatment group, who received other study medications (enalapril, hydrochlorothiazide, or
both), with or without nitrendipine, had substantially fewer cardiovascular events than the placebo group (62 vs.
109 events).
The authors contend that the rate of cardiovascular
events among the patients with diabetes was reduced to a
similar extent with nitrendipine alone and with the other
study medications. However, the numbers of events recorded in these subgroups were very small, and no statis-
Jul y 2 9 , 19 9 9
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2015. For personal use only. No other uses without permission.
Copyright 1999 Massachusetts Medical Society. All rights reserved.
CORR ES POND ENCE
tical information was provided, making this conclusion
questionable. It is quite possible that treatment with nitrendipine reduced the risk of stroke by lowering systolic
blood pressure but actually increased the risk of cardiac
events such as myocardial infarction, heart failure, and
sudden death. The main benefit in the diabetic patients in
this study may be related to the significant reductions in
risk associated with the use of angiotensin-converting
enzyme inhibitors and diuretics.5,6
been randomly assigned to a treatment group, one third
have diabetes mellitus.
JAAKKO TUOMILEHTO, M.D.
National Public Health Institute
FIN-00300 Helsinki, Finland
JAN A. STAESSEN, M.D., PH.D.
University of Leuven
B-3000 Leuven, Belgium
SHELLEY SALPETER, M.D.
Santa Clara Valley Medical Center
San Jose, CA 95128
1. Tuomilehto J, Rastenyte D, Birkenhger WH, et al. Effects of calciumchannel blockade in older patients with diabetes and systolic hypertension.
N Engl J Med 1999;340:677-84.
2. Staessen JA, Fagard R, Thijs L, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. Lancet 1997;350:757-64.
3. Pahor M, Kritchevsky SB, Zuccala G, Guralnik JM. Diabetes and risk
of adverse events with calcium antagonists. Diabetes Care 1998;21:1934.
4. Staessen JA, Fagard R, Thijs L, et al. Subgoups and per-protocol analysis of the randomized European Trial on Isolated Systolic Hypertension in
the Elderly. Arch Intern Med 1998;158:1681-91.
5. Curb JD, Pressel SL, Cutler JA, et al. Effect of diuretic-based antihypertensive treatment on cardiovascular disease risk in older diabetic patients
with isolated systolic hypertension. JAMA 1996;276:1886-92. [Erratum,
JAMA 1997;277:1356.]
6. UK Prospective Diabetes Study Group. Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in
type 2 diabetes: UKPDS 39. BMJ 1998;317:713-20.
The authors reply:
To the Editor: Subgroup analyses must be interpreted
cautiously, because they deviate from the lines of randomization. Dr. Salpeters comments in this regard are equally
applicable to our trial and to the Systolic Hypertension in
the Elderly Program study.1 However, the comparison of
these two independent trials mutually reinforces their conclusions. In the two studies, the nondiabetic patients had
the same risks and similar benefits from treatment. Diabetes at base line increased the cardiovascular risk to the
same extent in the control groups in the two trials, and
active treatment resulted in similar reductions in systolic
pressure in the nondiabetic and diabetic patients. The
main differences between the two trials were the first-line
antihypertensive drug used and the outcome in the diabetic patients.
As we have previously reported,2 the patients in our trial who continued to receive monotherapy with nitrendipine had the full benefit of active treatment. Moreover,
our findings in diabetic patients were recently confirmed
in the placebo-controlled Systolic Hypertension in Elderly Chinese (Syst-China) trial,3 in which active treatment
was also initiated with nitrendipine. Confirmation of the
observation that hypertensive patients with diabetes fare
better with a dihydropyridine than with a thiazide is required, but data bearing on the question will be available
in 2002, when the Antihypertensive and Lipid Lowering
Treatment to Prevent Heart Attack Trial is completed.
This trial compares amlopidine, lisinopril, and doxazosin
with chlorthalidone. Of the 40,000 patients who have
WILLEM H. BIRKENHGER, M.D., PH.D.
Erasmus University
3015 GE Rotterdam, the Netherlands
1. Curb JD, Pressel SL, Cutler JA, et al. Effect of diuretic-based antihypertensive treatment on cardiovascular disease risk in older diabetic patients
with isolated systolic hypertension. JAMA 1996;276:1886-92. [Erratum,
JAMA 1997;277:1356.]
2. Staessen JA, Thijs L, Fagard RH, et al. Calcium channel blockade and
cardiovascular prognosis in the European trial on isolated systolic hypertension. Hypertension 1998;32:410-6.
3. Syst-China trial. Arch Intern Med (in press).
Diagnosis of Constrictive Pericarditis by Tagged
Cine Magnetic Resonance Imaging
To the Editor: Constrictive pericarditis is characterized
by a thickened and adherent pericardium that restricts diastolic filling of the heart.1 Although many diagnostic criteria for constrictive pericarditis have been proposed, not
all cases necessarily fulfill them.2 Thus, the diagnosis of
constrictive pericarditis is sometimes difficult.
We cared for a patient with constrictive pericarditis for
whom we used tagged cine magnetic resonance imaging
(cine MRI)3 and successfully identified adhesion of the
thickened pericardium to the myocardium, which is the
essential feature of constrictive pericarditis. Tagged cine
MRI is a new, noninvasive imaging technique for labeling
and monitoring specific regions of the heart; the patterns
of regional displacement accurately reflect the intervening
motion within a cardiac cycle.
The patient, a 28-year-old woman, was seen for refractory ascites, which had been present for four years. Her
principal symptoms were dyspnea on exertion, abdominal
swelling, and edema. On auscultation, a pericardial knock
was prominent. A chest film showed mild enlargement of
the cardiac silhouette. A computed tomographic scan of
the chest showed a thickened pericardium with calcification around the atrioventricular sulcus, a finding consistent
with the diagnosis of constrictive pericarditis. The patient
had no history of tuberculosis, collagen disease, malignant
disease, myocardial infarction, cardiac surgery, or radiation
therapy, and therefore the specific cause of the constrictive
pericarditis could not be determined. Cardiac catheterization revealed a normal left ventricular ejection fraction and
normal coronary arteries; however, the right ventricular
and left ventricular end-diastolic pressures were elevated
and almost equal (20 and 23 mm Hg, respectively). Recordings of the right and left ventricular pressures had a
characteristic dip and plateau contour, and a recording
of the right atrial pressure had a prominent y descent.
Vol ume 341
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2015. For personal use only. No other uses without permission.
Copyright 1999 Massachusetts Medical Society. All rights reserved.
Numb e r 5
373
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
MRI of the chest by the T2-weighted spinecho technique
revealed a thickened pericardium around the right and left
ventricles (Fig. 1). More important, tagged cine MRI revealed tight adhesion of the thickened pericardium to the
myocardium of the right and left ventricles, indicated by
the persistent concordance of tagged signals between the
pericardium and the myocardium throughout the diastolic
and systolic phases (Fig. 2). The diagnosis of idiopathic
constrictive pericarditis was confirmed at surgery and by
subsequent histologic examination. After pericardiectomy,
the ascites disappeared and the patient had no dyspnea on
effort.
We conclude that examination for adhesion of the thickened pericardium to the myocardium by tagged cine MRI
is a useful and reliable noninvasive method to diagnose
constrictive pericarditis.
SUNAO KOJIMA, M.D.
NAOAKI YAMADA, M.D.
YOICHI GOTO, M.D.
National Cardiovascular Center
Osaka 565-8565, Japan
1. Lorell BH. Constrictive pericarditis. In: Braunwald E, ed. Heart disease:
a textbook of cardiovascular medicine. 5th ed. Philadelphia: W.B. Saunders,
1997:1496-505.
2. Vaitkus PT, Kussmaul WG. Constrictive pericarditis versus restrictive
cardiomyopathy: a reappraisal and update of diagnostic criteria. Am Heart
J 1991;122:1431-41.
3. Zerhouni EA, Parish DM, Rogers WJ, Yang A, Shapiro EP. Human
heart: tagging with MR imaging a method for noninvasive assessment
of myocardial motion. Radiology 1988;169:59-63.
B
Figure 2. Tagged Cine MRI Images at End Diastole (Panel A) and
End Systole (Panel B).
Tagged grids with 8-mm-wide spacing that were generated at
end diastole (arrows in Panel A) remained unchanged at end
systole (arrows in Panel B), indicating tight adhesion between
the pericardium and the underlying myocardium.
RV
LV
Figure 1. T2-Weighted SpinEcho MRI Scan of the Chest.
Thickened pericardium (arrows) is visible around the right ventricle (RV) and left ventricle (LV).
374
Carcinoma of the Corneoscleral Limbus
in a Patient Treated with Cyclosporine
after Heart Transplantation
To the Editor: It is well established that immunosuppression after organ transplantation carries an increased risk of
certain malignant tumors. Of these tumors, those of the
skin and lip and lymphomas are the most common.1 We
report a carcinoma of the corneoscleral limbus in a patient
who was treated with cyclosporine after undergoing heart
transplantation.
A 60-year-old man was referred because of a tumor of
the corneoscleral limbus in his left eye. He had undergone
a heart transplantation five years earlier. The patient had
not previously had cancer or ocular disease, and he had
not worn contact lenses. After undergoing transplantation,
Jul y 2 9 , 19 9 9
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2015. For personal use only. No other uses without permission.
Copyright 1999 Massachusetts Medical Society. All rights reserved.
C ORR ES POND ENCE
Figure 1. Slit-Lamp Photograph Showing a Tumor of the Corneoscleral Limbus in a 60-Year-Old Man Treated with Cyclosporine after Undergoing Heart Transplantation.
he had been treated with prednisone and cyclosporine. The
dose of prednisone was tapered over a period of two years
and then stopped. The blood cyclosporine level was usually in the therapeutic range. Gum hypertrophy required
surgical resection 24 and 32 months after transplantation.
Unilateral ocular symptoms (irritation and tearing) developed 50 months after transplantation. A tumor of the
corneoscleral limbus subsequently appeared in the patients left eye (Fig. 1). It was excised, and pathological examination showed a 5-mm pedunculated tumor. Normal
squamous epithelium lined the peduncle, and epithelial
proliferation with elongated ridges and high-grade dysplasia
(carcinoma in situ) was prominent in the head of the tumor.
The role of treatment with cyclosporine in the development of this carcinoma is unknown. In addition to its effects on the immune system, cyclosporine may affect the
eye directly. After oral administration, cyclosporine has been
found in tears.2 In addition, pharmacokinetic studies have
shown that cyclosporine has a strong affinity for the cornea.3
It is likely that cyclosporine had a major role in the development of this exceptional tumor.
OLIVIER TOUZEAU, M.D.
VINCENT M. BORDERIE, M.D., PH.D.
LAURENT LAROCHE, M.D.
Hpital Saint-Antoine
75571 Paris CEDEX 12, France
1. Penn I. Why do immunosuppressed patients develop cancer? Crit Rev
Oncog 1989;1:27-52.
2. BenEzra D, Maftzir G, de Courten C, Timonen P. Ocular penetration
of cyclosporin A. III. The human eye. Br J Ophthalmol 1990;74:350-2.
[Erratum, Br J Ophthalmol 1992;76:320.]
3. Oh C, Saville BA, Cheng YL, Rootman DS. A compartmental model
for the ocular pharmacokinetics of cyclosporine in rabbits. Pharm Res
1995;12:433-7.
Hyper-IgE Syndrome
1
To the Editor: Grimbacher et al. (March 4 issue) described in detail 30 patients with hyper-IgE syndrome.
Recently, a 29-year-old Italian woman was admitted to our
hospital because of acute back pain due to spontaneous
fracture of the L3 vertebral body. She had a history of
chronic generalized eczematoid lesions, diffuse microlymphadenopathy, bronchial asthma, rhinosinusal polyps, migraine-like headache, and recurrent vaginal candidiasis.
During childhood, she had had frequent skin infections and
recurrent pneumonitis. Additional findings included hypoplasia of the right mandibular condylus, cleft of the posterior arch of the S1 vertebra, bilateral keratoconus, ovarian and renal cysts, and fibroadenoma of the breast.
Physical examination showed facial traits strongly resembling those described by Grimbacher et al. Laboratory
analyses revealed high levels of total IgE (peak, 38,600 IU
per milliliter) and mild eosinophilia (peak eosinophil
count, 1100 per cubic millimeter), with a normal whitecell count. The patient had a younger brother with eczematous dermatitis and high levels of IgE (3100 IU per milliliter).
Immunophenotypic analysis of peripheral-blood lymphocytes demonstrated a 64 percent increase in CD4+
T cells. Since lymphokine-producing CD4+ T cells may
influence IgE synthesis by releasing lymphokines, we evaluated cytokine expression by peripheral-blood T cells.
Lymphokine-producing CD4+ T cells can be subdivided
into two broad categories, called TH1 and TH2, according
to their pattern of lymphokine production. TH1 cells secrete
interleukin-2, interferon-g, and tumor necrosis factor b;
they inhibit cytokine secretion by TH2 lymphocytes and
IgE synthesis through the release of interferon-g. In contrast, TH2 lymphocytes produce interleukin-4, interleukin-5, interleukin-6, interleukin-9, and interleukin-10; inhibit proliferation of TH1 cells; and favor IgE synthesis and
eosinophil activation.2 In our patient, intracellular study of
TH1- and TH2-related cytokines revealed a TH0 profile
with expression of both interleukin-4 and interferon-g
(Fig. 1, next page) but not interleukin-2. The expression of
interleukin-4 was limited to CD4+ T lymphocytes. Because
of the restricted pattern of cytokine expression, T-cell
receptor genes were analyzed. As shown in Figure 1, rearrangement bands were seen, indicating the presence of
at least one T-cell clonal population.
On the basis of these findings, we speculate that the hyper-IgE syndrome might be related to a disruption of the
T-cell compartment that has evolved into a clonal expansion and accumulation of T cells with a TH0 profile. Finally, our data suggest that immunophenotyping and molecular study of peripheral-blood lymphocytes should be
performed in patients with this syndrome to understand
the immunopathogenic mechanisms involved and possibly
to design future treatment strategies.
FABIO PRESOTTO, M.D.
LIVIO TRENTIN, M.D.
CARLO AGOSTINI, M.D.
Padua University
School of Medicine
35128 Padua, Italy
1. Grimbacher B, Holland SM, Gallin JI, et al. Hyper-IgE syndrome with
recurrent infections an autosomal dominant multisystem disorder.
N Engl J Med 1999;340:692-702.
2. Romagnani S. The Th1/Th2 paradigm. Immunol Today 1997;18:263-6.
Vol ume 341
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2015. For personal use only. No other uses without permission.
Copyright 1999 Massachusetts Medical Society. All rights reserved.
Numb e r 5
375
nt
l
Pa
43%
56%
1%
0%
CD4
Co
tie
ro
nt
tie
Pa
Co
nt
ro
nt
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
11 kb
8.5 kb
6.5 kb
Interleukin-4
6%
52%
3.6 kb
CD4
4 kb
6%
36%
EcoRI
HindIII
Interferon-g
Figure 1. Southern Blot Analysis of T-CellReceptor b Genes (Panel A) and Flow-Cytometric Analysis of Intracellular
Cytokine Expression by CD4+ T Cells (Panel B).
In Southern blot analysis, DNA from control cells (K-562) and the patients peripheral-blood mononuclear cells were
digested with the EcoRI and HindIII restriction enzymes and studied with a T-cellreceptor bJ/bC probe.
To the Editor: Grimbacher et al. describe what they consider the characteristic facial appearance of patients with
the hyper-IgE syndrome. For years, dysmorphologists and
geneticists have debated and pondered what constitutes a
characteristic facial appearance. Twenty-five years ago a
colleague and I reported normal values for selected facial
features,1 and more reports were subsequently published.2-4 These data are available but are frequently not
used. Grimbacher et al. substantiated their clinical impression of increased interalar distances by comparing their
measurements with published standard values, but the majority of the other facial characteristics mentioned were
not documented.
An increasing array of newer techniques that can provide anthropometric measurements are now available, such
as magnetic resonance imaging, stereoscopic imaging,
computed tomography, and ultrasonography. It is not always practical to use these methods in clinical practice;
however, if findings are to be published, these techniques
can help substantiate an authors impression of a characteristic facial appearance. Granted, not all facial features
can be adequately measured.
I also want to stress the importance of the clinicians
ability to diagnose what we used to term a facial gestalt
that is, a pattern of clinically observed, physical facial
findings that is derived from the sum of its parts and that
376
culminates in a distinctive and characteristic appearance or
image. In Grimbachers photographs of the patients with
the hyper-IgE syndrome, despite the lack of many specific
measurements, the facial gestalt of the patients appears to
be characteristic. However, my clinical impressions have
been wrong before, which is why we need anthropometric
measurements.
MURRAY FEINGOLD, M.D.
National Birth Defects Center
Waltham, MA 02451
1. Feingold M, Bossert WH. Normal values for selected physical parameters: an aid to syndrome delineation. Birth Defects Orig Artic Ser 1974;
10(13):1-16.
2. Saksena SS, Bader P, Bixler D. Facial dysmorphology, roentgenographic
measurements, and clinical genetics. J Craniofac Genet Dev Biol 1989;9:
29-43.
3. Allanson JE. Objective techniques for craniofacial assessment: what are
the choices? Am J Med Genet 1997;70:1-5.
4. Ward RE, Jamison PL, Farkas LG. Craniofacial variability index: a simple measure of normal and abnormal variation in the head and face. Am J
Med Genet 1998;80:232-40.
The authors reply:
To the Editor: As stated in our article, the hyper-IgE syndrome in nonfamilial cases is diagnosed on the basis of
Jul y 2 9 , 19 9 9
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2015. For personal use only. No other uses without permission.
Copyright 1999 Massachusetts Medical Society. All rights reserved.
C ORR ES POND ENCE
skin abscesses, pneumonia with formation of pneumatoceles, and recurrent eczematoid rashes, as well as extreme
elevations in serum IgE levels. The woman described by
Presotto et al. may have hyper-IgE syndrome, although
from the limited information given and in the absence of
boils or pneumatoceles, she would not meet our criteria
for an affected proband, nor would a brother with isolated
IgE elevation be considered to have a hyper-IgE genotype.
Moreover, it is not clear whether this womans clonal
T cells or CD4+ cells producing interleukin-4 and interferon-g, described at a single point in time, would be continuously present. The specific primary immunologic defect in the hyper-IgE syndrome has remained elusive,
despite more than 30 years of immunologic investigations.
A wide array of lymphocyte abnormalities and cytokines
has been noted, but these findings have not been present
in all patients or at all times. For this reason, we have elected to pursue a genetic-linkage strategy; identification of a
gene that, when mutated, results in hyper-IgE syndrome
may be the most efficient way to understand the syndromes primary cause.
Feingold stresses the importance of anthropometric
measurements in the definition of syndromic phenotypes.
We performed a series of external measurements of the
body, head, and face, including height, weight, arm span,
head circumference, inner and outer canthal distances, interpupillary distance, interalar distance, and lengths of
the nose, philtrum, ears, hands, palms, and feet. These
were compared with population standards and are available on request. For brevity, we reported only the measurements for which the values for our patients with hyperIgE syndrome differed from population means: interalar
distance and head circumference. We did not confirm the
increased outer canthal distance reported for such patients
by Borges et al.1 Further measurements, such as quantitation of asymmetry by methods requiring exposure to radiation, sedation of young children, or substantial expense,
were not undertaken in this study in part because the facial gestalt assessment was so highly reproducible by independent observers who viewed our subjects.
BODO GRIMBACHER, M.D.
National Human Genome Research Institute
STEVEN M. HOLLAND, M.D.
National Institute of Allergy and Infectious Diseases
JENNIFER M. PUCK, M.D.
National Human Genome Research Institute
Bethesda, MD 20892
1. Borges WG, Hensley T, Carey JC, Petrak BA, Hill HR. The face of Job.
J Pediatr 1998;133:303-5.
Treatment of Intestinal Parasites in Immigrants
To the Editor: The conclusion by Muennig et al. (March
11 issue)1 that empirical treatment of all U.S. immigrants
at risk for parasitosis would result in a net health benefit is
driven by the assumption in their decision-analysis model
that albendazole has no serious side effects. The authors
base this assumption on the seven field trials of albendazole
that found no serious side effects requiring medical attention. However, these trials studied the use of albendazole
in a total of fewer than 3000 patients. Most of the trials
monitored patients for three weeks or less and relied principally on the patients reports of adverse events. Only two
of the trials evaluated post-treatment laboratory data.
It may not be valid to extrapolate the finding that there
were no adverse events in the relatively small number of
patients treated in these field trials to a population of approximately 700,000 immigrants at risk. Albendazole is
known to be teratogenic in animals and is thus contraindicated in pregnant women. SmithKline Beecham reports
in this years Physicians Desk Reference that albendazole
has been associated with rare deaths due to pancytopenia
or granulocytopenia.2
With their model, Muennig et al. predict that the empirical use of albendazole in approximately 700,000 immigrants would save 33 lives. However, if albendazole caused
a serious adverse event in even 1 of every 50,000 patients,
much of its net health benefit would be lost. As Muennig
et al. note, almost all deaths due to parasites in the United
States are due to Strongyloides stercoralis hyperinfection.
This phenomenon occurs almost exclusively in patients
who are immunosuppressed.3 Instead of treating all immigrants at risk for parasitosis with albendazole, a more prudent course of action would be to target immigrants at
risk for S. stercoralis hyperinfection that is, those who
are currently immunocompromised and those who are
likely to receive immunosuppressive therapy.
EDWARD MITRE, M.D.
New York University
New York, NY 10016
1. Muennig P, Pallin D, Sell RL, Chan M-S. The cost effectiveness of strategies for the treatment of intestinal parasites in immigrants. N Engl J Med
1999;340:773-9.
2. Physicians desk reference. 53rd ed. Montvale, N.J.: Medical Economics,
1999:3018-9.
3. Mahmoud AA. Strongyloidiasis. Clin Infect Dis 1996;23:949-53.
To the Editor: As clinicians who care for many lowincome immigrants, we doubt that our patients would follow the recommendation of Muennig et al. to take a medication as prophylaxis against conditions (disseminated
strongyloidiasis and ascariasis) for which the lifetime chance
of death is less than 1/5 of 1 percent. This is especially
true because many immigrants who have recently arrived
in the United States do not have health insurance, and most
are not eligible for Medicaid. Financial factors adversely
affect health status and access to care among low-income
immigrants. Would a low-income family of five asymptomatic immigrants opt to pay $58.95 for albendazole (the
retail cost for five persons treated with 400 mg of albendazole per day, given orally for five days, at the Boston Medical Centers outpatient pharmacy) because we say empirical treatment will save society a few million dollars and
prevent 33 deaths nationally each year? We think not.
A better focus for the study would have been the provision of empirical antiparasitic treatment to immigrants
with high-risk medical conditions (such as asthma or
autoimmune disease) just before their departure from
Vol ume 341
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2015. For personal use only. No other uses without permission.
Copyright 1999 Massachusetts Medical Society. All rights reserved.
Numb e r 5
377
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
countries where the parasites are endemic (perhaps as part
of the medical evaluation of applicants for U.S. visas) or
shortly after their arrival in the United States. The costs of
strongyloidiasis and ascariasis in immunosuppressed patients could have been estimated in advance, in order to
focus the study on a more practical approach that probably
would have increased the documented savings. Yet, except
in the case of refugee visa holders, overseas evaluation
(and hence empirical antiparasitic treatment) is also at the
immigrants expense. . . .
PAUL GELTMAN, M.D., M.P.H.
ALAN MEYERS, M.D., M.P.H.
Boston University
School of Medicine
Boston, MA 02118
The authors reply:
To the Editor: We agree with Drs. Geltman and Meyers
that an immigrant may be reluctant to spend current dollars to avert future ills of dubious likelihood. This reluctance results from the natural tendency to discount future
costs and the difficulty of making rational decisions about
events of low probability. The physician is also likely to
base his or her decision on feelings, in accordance with the
notion that medicine is an art, not a science. Formal analysis of cost effectiveness contributes to rational decision
making by quantifying discounting and using stochastic
models with sensitivity analysis to calculate expected
values.
Decision making emphasizes that which is certain and
in the present or near future over that which is unlikely
and in the more distant future. Our patients must often be
convinced of the necessity of an annual Papanicolaou
smear, which has concrete costs in the present and averts
a future event of low probability. Whether the recommended preventive regimen of albendazole should be administered after immigrants arrive in the United States or
during the overseas examination is a decision for policy
makers.
On the other hand, if the regimen of low-dose albendazole that we studied proved to have clinically significant
side effects, the analysis would need to be repeated. The
adverse effects cited by Dr. Mitre occurred with prolonged
regimens, such as those required for the treatment of neurocysticercosis or echinococcosis.1 These regimens generally involve a dose of 800 mg of albendazole per day for a
minimum of 30 days, whereas we studied a regimen of
400 mg per day for 5 days. In areas where the parasites are
endemic, similar low-dose regimens of the medication
have been used for almost 10 years for the presumptive
treatment of parasitosis.
Our model was based on the assumption that the only
side effects would be mild somatic symptoms requiring a
single medical visit for reassurance. The net health benefits
and cost savings would be maintained as long as less than
20 percent of persons receiving treatment encountered
this problem.
We did not claim that most or all deaths from parasitic
infections in the United States were due to S. stercoralis.
378
Instead, this organism was responsible for most of the
deaths due to parasitic disease in our model, which included the costs and outcomes for only four parasites. The preventive regimen we studied would also cure many parasitic
infections not included in the analysis.
DANIEL J. PALLIN, M.D.
PETER A. MUENNIG, M.D., M.P.H.
New York City Department of Health
New York, NY 10013
1. Albenza. Philadelphia: SmithKline Beecham Pharmaceuticals, 1997
(package insert).
A Surprise during Pediatric Endoscopy
To the Editor: A 10-year-old boy was admitted to the
hospital with crampy epigastric pain after eating. He mentioned swallowing a small object. Gastroscopy revealed a
Figure 1. Gastroscopy Showing a Toy Flashlight.
toy flashlight (2.5 cm in diameter) emblazoned with a cartoon character (Fig. 1). The boys symptoms were relieved
after the flashlight was removed, and his flashlight still
worked.
TOBIAS G. WENZL, M.D.
HEINO SKOPNIK, M.D.
Childrens Hospital Worms
D-67550 Worms, Germany
1999, Massachusetts Medical Society.
Jul y 2 9 , 19 9 9
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2015. For personal use only. No other uses without permission.
Copyright 1999 Massachusetts Medical Society. All rights reserved.
Вам также может понравиться
- A Pain-Free' Death: Fiona Hicks and Elizabeth ReesДокумент19 страницA Pain-Free' Death: Fiona Hicks and Elizabeth Reesbdalcin5512Оценок пока нет
- What Should We Know About Dementia in The 21st Century? A Delphi Consensus StudyДокумент13 страницWhat Should We Know About Dementia in The 21st Century? A Delphi Consensus Studyyeremias setyawanОценок пока нет
- Review Series - Palliative Medicine: Palliative Care For Dementia-Time To Think Again?Документ4 страницыReview Series - Palliative Medicine: Palliative Care For Dementia-Time To Think Again?agniajolandaОценок пока нет
- Anesthesia Analgesia September 2009Документ291 страницаAnesthesia Analgesia September 2009Alexandra PavloviciОценок пока нет
- Livingston Dementia Prevention Intervention CareДокумент129 страницLivingston Dementia Prevention Intervention Careandrea palmaОценок пока нет
- Palliative Care in AdvancedДокумент24 страницыPalliative Care in AdvancedClaudio Silva FilhoОценок пока нет
- Obesity and Lung Disease: A Guide to ManagementОт EverandObesity and Lung Disease: A Guide to ManagementAnne E. DixonОценок пока нет
- Acute Rheumatic FeverДокумент5 страницAcute Rheumatic FeverSyahmi AhmadОценок пока нет
- Tugas Merangkum Epidemiologi Safira M.20.02.050Документ5 страницTugas Merangkum Epidemiologi Safira M.20.02.050safira saalОценок пока нет
- Referat: Pneumonia in ElderlyДокумент41 страницаReferat: Pneumonia in Elderlyathieqah say-syahidahОценок пока нет
- Bortolato2016 Depresi Pada KankerДокумент50 страницBortolato2016 Depresi Pada KankerYudha HudayaОценок пока нет
- Predicting Dementia From Primary Care Records: A Systematic Review and Meta-AnalysisДокумент23 страницыPredicting Dementia From Primary Care Records: A Systematic Review and Meta-AnalysisDeedee RenovaldiОценок пока нет
- Comprehensive Case Study On Pulmonary Embolism: Prepared byДокумент17 страницComprehensive Case Study On Pulmonary Embolism: Prepared byKristopher John JimenezОценок пока нет
- Hard BoundДокумент369 страницHard BoundClang SantiagoОценок пока нет
- Nursing Diagnoses and Interventions For Cardiological Patients in Palliative Care Original ArticleДокумент9 страницNursing Diagnoses and Interventions For Cardiological Patients in Palliative Care Original ArticleMaginta Resy DianaОценок пока нет
- Managing Depression Among Ethnic Communities: A Qualitative StudyДокумент6 страницManaging Depression Among Ethnic Communities: A Qualitative StudyCSilva16Оценок пока нет
- BronchiolitisДокумент7 страницBronchiolitisRiski DohartuaОценок пока нет
- Communicating Difficult News in MedicineДокумент8 страницCommunicating Difficult News in MedicineIrina Cez100% (1)
- Pott Disease PDFДокумент5 страницPott Disease PDFAndri wijayaОценок пока нет
- Discrimination of drunken patients in EDsДокумент3 страницыDiscrimination of drunken patients in EDsiis intanОценок пока нет
- Ameet EtalДокумент5 страницAmeet EtaleditorijmrhsОценок пока нет
- 02 NewhorizonsДокумент8 страниц02 NewhorizonsgloriaОценок пока нет
- Original Research: Patient and Physician Explanatory Models For Acute BronchitisДокумент6 страницOriginal Research: Patient and Physician Explanatory Models For Acute BronchitisJumria Tandi PanggaloОценок пока нет
- Example Research Paper On LupusДокумент8 страницExample Research Paper On Lupuswhrkeculg100% (1)
- Multiple Sclerosis Research Paper ConclusionДокумент9 страницMultiple Sclerosis Research Paper Conclusiongz91rnat100% (1)
- Schizophrenia: Clinical ReviewДокумент5 страницSchizophrenia: Clinical ReviewPuji Arifianti RamadhanyОценок пока нет
- Lupus Term PaperДокумент10 страницLupus Term Paperc5qdk8jn100% (1)
- Sickle Cell Anemia Students Name Professor's Name Institutional Affiliation Course Unit DateДокумент6 страницSickle Cell Anemia Students Name Professor's Name Institutional Affiliation Course Unit Datejob ominoОценок пока нет
- Thesis EpidemiologyДокумент6 страницThesis Epidemiologykatieparkersaintpaul100% (3)
- Lupus Research Paper ThesisДокумент7 страницLupus Research Paper Thesisgz8reqdc100% (1)
- A Key Problem For Medicine in TheДокумент2 страницыA Key Problem For Medicine in TheSenaОценок пока нет
- Management of COPD in Primary and Secondary Care, TheОт EverandManagement of COPD in Primary and Secondary Care, TheРейтинг: 5 из 5 звезд5/5 (1)
- Personality disorders and criminal behavior focus of psychiatric studyДокумент1 страницаPersonality disorders and criminal behavior focus of psychiatric studyAyu Ersya WindiraОценок пока нет
- Jurnal Perawatan PaliatifДокумент16 страницJurnal Perawatan Paliatifnurwanda hamidaОценок пока нет
- Journal Reading on Alzheimer's Disease and Psychiatric ComorbiditiesДокумент24 страницыJournal Reading on Alzheimer's Disease and Psychiatric ComorbiditiesRevienaОценок пока нет
- Sick Individuals and Sick Population by Rose. GДокумент7 страницSick Individuals and Sick Population by Rose. GTate SimbaОценок пока нет
- Ebola and QuarantineДокумент2 страницыEbola and Quarantinem_rinaldi_sufri3298Оценок пока нет
- Delirium in The Intensive Care Unit: ReviewДокумент9 страницDelirium in The Intensive Care Unit: ReviewCristopher Castro RdОценок пока нет
- CAP in Elderly PatientsДокумент18 страницCAP in Elderly PatientsAlex Toman Fernando SaragihОценок пока нет
- Dissertation ProposalДокумент15 страницDissertation ProposalJitesh SoniОценок пока нет
- Killer Diseases, Modern-Day Epidemics: Keys to Stopping Heart Disease, Diabetes, Cancer, and Obesity in Their TracksОт EverandKiller Diseases, Modern-Day Epidemics: Keys to Stopping Heart Disease, Diabetes, Cancer, and Obesity in Their TracksОценок пока нет
- Research Proposal: Role of Nurse in Delay Wound HealingДокумент25 страницResearch Proposal: Role of Nurse in Delay Wound HealingNaveeda IqbalОценок пока нет
- Libro Enfermedades Pulmonares HuérfanasДокумент789 страницLibro Enfermedades Pulmonares HuérfanasLeiniker NavarroОценок пока нет
- JournalsДокумент11 страницJournalsrachmaniabudiatiОценок пока нет
- OET R Bed Bugs PaperДокумент8 страницOET R Bed Bugs PaperVic KwanОценок пока нет
- Assessment 9Документ5 страницAssessment 9api-525782290Оценок пока нет
- End of Life IssuesДокумент8 страницEnd of Life IssuesJo RanamoОценок пока нет
- Communication Skills For MedicДокумент455 страницCommunication Skills For MedicLangit SkalaОценок пока нет
- Diffi Cult To Treat Asthma: Sandhya Khurana Fernando Holguin EditorsДокумент339 страницDiffi Cult To Treat Asthma: Sandhya Khurana Fernando Holguin Editorsneumologia.intervencionОценок пока нет
- Demencia FrontotemporalДокумент10 страницDemencia FrontotemporalIsaac EliasОценок пока нет
- Untitled DocumentДокумент2 страницыUntitled DocumentOmer KhanОценок пока нет
- Infectious EndocarditisДокумент49 страницInfectious EndocarditisDennisFrankKondoОценок пока нет
- Arthritis and Society: The Impact of Musculoskeletal DiseasesОт EverandArthritis and Society: The Impact of Musculoskeletal DiseasesОценок пока нет
- Descriptive EpidemiologyДокумент7 страницDescriptive EpidemiologyVineeta JoseОценок пока нет
- Epidemiiology SeminarДокумент15 страницEpidemiiology SeminarMugu 123Оценок пока нет
- Phenomenology of Squalor, Hoarding and Self-NeglectДокумент5 страницPhenomenology of Squalor, Hoarding and Self-NeglectastrogliaОценок пока нет
- Epidem. Lecture 1 & 2Документ18 страницEpidem. Lecture 1 & 2sajad abasew100% (1)
- Neuro-Oncology and Palliative Care: A Challenging InterfaceДокумент5 страницNeuro-Oncology and Palliative Care: A Challenging InterfaceJiaОценок пока нет
- Romanian (Delta Dunərij) Ukrainian (De T Dun Ju) ʎ Ɐ Ɑ River Delta Europe Volga Delta Danube Romania Tulcea County Ukraine Odessa Oblast Razim - SinoeДокумент1 страницаRomanian (Delta Dunərij) Ukrainian (De T Dun Ju) ʎ Ɐ Ɑ River Delta Europe Volga Delta Danube Romania Tulcea County Ukraine Odessa Oblast Razim - SinoeAdina OlteanuОценок пока нет
- What Happens After The First EpisodeДокумент13 страницWhat Happens After The First EpisodeAdina OlteanuОценок пока нет
- English Today Vol.5 Varianta 2Документ95 страницEnglish Today Vol.5 Varianta 2Adina OlteanuОценок пока нет
- Assessment and Treatment of Post-Stroke DepressionДокумент40 страницAssessment and Treatment of Post-Stroke DepressionalinaОценок пока нет
- Computer Simulation of Cardiac Mechanics for TeachingДокумент1 страницаComputer Simulation of Cardiac Mechanics for TeachingAdina OlteanuОценок пока нет
- English Today Vol.6 Varianta 2Документ96 страницEnglish Today Vol.6 Varianta 2Adina OlteanuОценок пока нет
- English Today Vol.7 Varianta 2Документ95 страницEnglish Today Vol.7 Varianta 2Adina OlteanuОценок пока нет
- Model Abstracts FinalДокумент5 страницModel Abstracts FinalAdina OlteanuОценок пока нет
- English Today Vol.8 Varianta 2Документ93 страницыEnglish Today Vol.8 Varianta 2Ionut Fiorosu100% (1)
- OEGCA OnlineMistakesAnsДокумент1 страницаOEGCA OnlineMistakesAnsMohit Chowdary NОценок пока нет
- Poster Template Lightblue 31x44 - VertДокумент1 страницаPoster Template Lightblue 31x44 - VertAdina OlteanuОценок пока нет
- AlexithymiaДокумент2 страницыAlexithymiaAdina OlteanuОценок пока нет
- Nej M 199509213331207Документ7 страницNej M 199509213331207Adina OlteanuОценок пока нет
- HGVFCXDZДокумент7 страницHGVFCXDZAdina OlteanuОценок пока нет
- Appendix G Medication Audit ToolДокумент12 страницAppendix G Medication Audit ToolAdina OlteanuОценок пока нет
- Nej M CPC 0900643Документ10 страницNej M CPC 0900643Adina OlteanuОценок пока нет
- Model Abstracts FinalДокумент5 страницModel Abstracts FinalAdina OlteanuОценок пока нет
- Screening and Assessment Tools for Post Stroke DepressionДокумент21 страницаScreening and Assessment Tools for Post Stroke DepressionAdina OlteanuОценок пока нет
- Hospitalization For Mental Illness Among Parents After The Death of A ChildДокумент7 страницHospitalization For Mental Illness Among Parents After The Death of A ChildAdina OlteanuОценок пока нет
- Nej M 199509213331207Документ7 страницNej M 199509213331207Adina OlteanuОценок пока нет
- Nej M 199603073341014Документ6 страницNej M 199603073341014Adina OlteanuОценок пока нет
- Drug Ther Apy D U T S: EditorДокумент8 страницDrug Ther Apy D U T S: EditorAdina OlteanuОценок пока нет
- Nej M 199907293410514Документ10 страницNej M 199907293410514Adina OlteanuОценок пока нет
- Nej Mic M 030851Документ1 страницаNej Mic M 030851Adina OlteanuОценок пока нет
- Psychotomimetic Effects of Drugs - A Common Pathway To Schizophrenia?Документ2 страницыPsychotomimetic Effects of Drugs - A Common Pathway To Schizophrenia?Adina OlteanuОценок пока нет
- Behavioural Weight Loss Intervention With Serious Mentall IllnessДокумент9 страницBehavioural Weight Loss Intervention With Serious Mentall Illnesstugba1234Оценок пока нет
- Nej M 200202073460618Документ8 страницNej M 200202073460618Adina OlteanuОценок пока нет
- What Happens After The First EpisodeДокумент13 страницWhat Happens After The First EpisodeAdina OlteanuОценок пока нет
- First-Episode Psychosis: An Update: ArticlesДокумент6 страницFirst-Episode Psychosis: An Update: ArticlesAdina OlteanuОценок пока нет
- NCM 114 Midterm ReviewerДокумент9 страницNCM 114 Midterm ReviewerAngelicaОценок пока нет
- Old Age Homes Perspective Social Support and Life Satisfaction Insights From The Retirement CommunityДокумент7 страницOld Age Homes Perspective Social Support and Life Satisfaction Insights From The Retirement CommunityAjmal Khan MandokhailОценок пока нет
- Iloilo City Regulation Ordinance 2012-027Документ4 страницыIloilo City Regulation Ordinance 2012-027Iloilo City CouncilОценок пока нет
- Etiology and Pattern of Impacted Mandibular Third Molars - A StudyДокумент4 страницыEtiology and Pattern of Impacted Mandibular Third Molars - A Studynasya naurahОценок пока нет
- Poster TemplateДокумент1 страницаPoster Templateapi-607378712Оценок пока нет
- Audit of BloodДокумент15 страницAudit of Bloodjuszmyyusuf0% (1)
- Daftar PustakaДокумент3 страницыDaftar PustakaDeska Nurmasari100% (1)
- Surgical Safety ChecklistДокумент1 страницаSurgical Safety ChecklistDarren Cariño100% (1)
- AEHRC Annual Report 2018Документ88 страницAEHRC Annual Report 2018Anonymous 1jLT1GAPОценок пока нет
- Food Poisoning Final Print!Документ3 страницыFood Poisoning Final Print!Joeven HilarioОценок пока нет
- Promotion Safe Med ChildrensДокумент64 страницыPromotion Safe Med ChildrensAbdul khodir jaelani100% (1)
- Low Cardiac Output SyndromeДокумент21 страницаLow Cardiac Output SyndromeMuaath Algoribi100% (1)
- Global Stem Cell Therapy Market IHealthcareAnalyst, IncДокумент2 страницыGlobal Stem Cell Therapy Market IHealthcareAnalyst, InciHealthcareAnalyst, Inc.Оценок пока нет
- Dengue FeverДокумент5 страницDengue FeverMae AzoresОценок пока нет
- ASA PS Classification System: Physical Status Definitions and ExamplesДокумент2 страницыASA PS Classification System: Physical Status Definitions and ExamplesAnonymous 6iLtIrОценок пока нет
- Effectiveness of nebulized N-acetylcysteine in treating children with acute bronchiolitisДокумент4 страницыEffectiveness of nebulized N-acetylcysteine in treating children with acute bronchiolitisIvan VeriswanОценок пока нет
- Crodua Prioritization TableДокумент10 страницCrodua Prioritization TableThea DuoОценок пока нет
- AmoebiasisДокумент64 страницыAmoebiasisLarry MathisОценок пока нет
- Work Immersion Experience at Bugo Health CenterДокумент18 страницWork Immersion Experience at Bugo Health Centerqueen rholyn100% (2)
- Postoperative Nursing ResponsibilitiesДокумент1 страницаPostoperative Nursing ResponsibilitiesDarlyn AmplayoОценок пока нет
- Definition, Scope, of Community PharmacyДокумент19 страницDefinition, Scope, of Community PharmacyBhavya JindalОценок пока нет
- Diabetes Foot Care Education Resource Pack: June 2016Документ16 страницDiabetes Foot Care Education Resource Pack: June 2016AthenaОценок пока нет
- Activity Intolerance Related To Decreased Cardiac Output, Due To EndocarditisДокумент4 страницыActivity Intolerance Related To Decreased Cardiac Output, Due To EndocarditisJohn AlcantaraОценок пока нет
- PEDIATRICS Timetable 5yr, Rot2, Sem1!20!22-NewДокумент7 страницPEDIATRICS Timetable 5yr, Rot2, Sem1!20!22-NewMawanda NasserОценок пока нет
- Autism Spectrum Disorder-MANUSCRIPT2CДокумент20 страницAutism Spectrum Disorder-MANUSCRIPT2CPaul AnteОценок пока нет
- SellersPaulineM 2018 SectionOneMaternalAnd SellersMidwiferyДокумент1 страницаSellersPaulineM 2018 SectionOneMaternalAnd SellersMidwiferyQedeniОценок пока нет
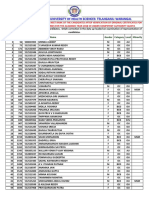
- 1430 Mbbsbdsfinalmeritlist201819 PDFДокумент205 страниц1430 Mbbsbdsfinalmeritlist201819 PDFVINEETH VinnuОценок пока нет
- Practical ScheduleДокумент5 страницPractical ScheduleJutt GeОценок пока нет
- Research Paper On Bells PalsyДокумент5 страницResearch Paper On Bells Palsyklbndecnd100% (1)
- Kamagra Tablets Are A Outstanding Treatment For EDwmqrm PDFДокумент3 страницыKamagra Tablets Are A Outstanding Treatment For EDwmqrm PDFcherryburn67Оценок пока нет