Академический Документы
Профессиональный Документы
Культура Документы
Jurnal Kulit Ayu 3
Загружено:
Ayu Nabila Kusuma PradanaАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Jurnal Kulit Ayu 3
Загружено:
Ayu Nabila Kusuma PradanaАвторское право:
Доступные форматы
doi: 10.1111/1346-8138.
12993
Journal of Dermatology 2015; 42: 945953
REVIEW ARTICLE
South-East Asia study alliance guidelines on the management
of acne vulgaris in South-East Asian patients
Chee Leok GOH,1 Flordeliz ABAD-CASINTAHAN,2 Derrick Chen Wee AW,3
Roshidah BABA,4 Lee Chin CHAN,5 Nguyen Thanh HUNG,6 Kanokvalai KULTHANAN,7
Hoe Nam LEONG,8 Marie Socouer MEDINA-OBLEPIAS,9 Nopadon NOPPAKUN,10
Irma Bernadette SITOHANG,11 Titi Lestari SUGITO,12 Su-Ni WONG13
1
National Skin Centre, Singapore, 2Department of Dermatology, Jose R. Reyes Memorial Medical Center, Manila, Philippines,
National University Hospital, Dermatology Clinic, Singapore, 4Department of Dermatology, Hospital Melaka, Melaka, 5Department of
Dermatology, Hospital Pulau Pinang, Pulau Pinang, Malaysia, 6Ho Chi Minh Dermatology and Venereology Hospital, Ho Chi Minh
City, Vietnam, 7Department of Dermatology, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand, 8Rophi
Clinic, Mount Elizabeth Novena Specialist Centre, Singapore, 9Department of Dermatology, Research Institute for Tropical Medicine,
Muntinlupa, Philippines, 10Division of Dermatology, Department of Internal Medicine, Faculty of Medicine, King Chulalongkorn
Memorial Hospital, Bangkok, Thailand, 11Cosmetic Dermatology Division, Department of Dermatovenereology, Faculty of Medicine,
Universitas Indonesia, 12Department of Dermato-Venereology, Faculty of Medicine, University of Indonesia/Dr Cipto Mangunkusumo
Hospital, Jakarta, Indonesia, 13Dr SN Wong Skin, Hair, Nails & Laser Specialist Clinic, Mt Elizabeth Medical Centre, Singapore
3
ABSTRACT
The management of acne in South-East Asia is unique, as Asian skin and local variables require a clinical approach
unlike that utilized in other parts of the world. There are different treatment guidelines per country in the region, and
a group of leading dermatologists from these countries convened to review these guidelines, discuss current practices and recent advances, and formulate consensus guidelines to harmonize the management of acne vulgaris in
the region. Emphasis has been placed on formulating recommendations to impede the development of antibiotic
resistance in Propionibacterium acnes. The group adopted the Acne Consensus Conference system for grading
acne severity. The group recommends that patients may be treated with topical medications including retinoids,
benzoyl peroxide (BPO), salicylic acid, a combination of retinoid and BPO, or a combination of retinoids and BPO
with or without antibiotics for mild acne; topical retinoid with topical BPO and a oral antibiotic for moderate acne;
and oral isotretinoin if the patient fails first-line treatment (a 6- or 8-week trial of combined oral antibiotics and topical retinoids with BPO) for severe acne. Maintenance acne treatment using topical retinoids with or without BPO is
recommended. To prevent the development of antibiotic resistance, topical antibiotics should not be used as monotherapy or used simultaneously with oral antibiotics. Skin care, comprised of cleansing, moisturizing and sun protection, is likewise recommended. Patient education and good communication is recommended to improve
adherence, and advice should be given about the characteristics of the skin care products patients should use.
Key words:
acne, Asian, management, oral antibiotics, topical retinoids.
INTRODUCTION
Acne vulgaris is a chronic inflammatory disease of the pilosebaceous unit with polymorphic manifestations. Clinically, it is
diagnosed by the presence of comedones (its pathognomonic
feature), papules, pustules, nodules and cysts. In recent years,
significant advancements in the understanding of acne have
altered the way it is managed. Food with high glycemic indices
is to be avoided as it is now known that it is associated with
acne. Acne has been recognized as a chronic disease, and
therefore maintenance therapy has been deemed necessary to
prevent acne recurrence.1 Topical retinoids have been shown
to effectively control acne and prevent relapse unlike antibiotics, which have been shown to be ineffective in preventing the
development of the subclinical precursors of both inflammatory
and non-inflammatory acne lesions.1 To address the emerging
problem of antibiotic resistance, the Global Alliance to Improve
Outcomes in Acne group have recommended that topical antibiotics should not be given as monotherapy or maintenance
therapy because it may lead to the development of antibiotic
resistance. Also, combination treatment has been shown to be
superior to monotherapy.1,2
Correspondence: Chee Leok Goh, M.D., MBBS., MMed, MRCP(UK), FRCPE., National Skin Center, 1 Mandalay Road, Singapore 308205.
Email: clgoh@nsc.gov.sg
Received 6 January 2015; accepted 11 May 2015.
2015 Japanese Dermatological Association
945
C.L. Goh et al.
In 2011, a group of experts from 10 countries (Hong Kong,
India, Japan, Korea, Malaysia, the Philippines, Singapore, Taiwan, Thailand and the USA) enumerated several clinically significant differences between Asian and Caucasian skin that
contribute to variations between Asian practice and Global Alliance recommendations.3 Asian skin is more prone to postinflammatory hyperpigmentation (PIH) and irritation when treated
with topical retinoids compared with Caucasian skin.4 These
differences, coupled with the lack of clinical data specifically
about acne in Asian patients, highlight the need for the development of treatment guidelines tailored to the South-East
Asian (SEA) population.
The South-East Asia Study Alliance (SASA) group, comprised of 13 leading dermatologists from six countries in SEA
(Indonesia, Malaysia, the Philippines, Singapore, Thailand and
Vietnam), was formed to address this unmet need. The group
convened to review existing guidelines, discuss current practices and recent advances, formulate consensus guidelines to
harmonize the management of acne vulgaris in the region, and
document this consensus for publication.
The objectives of these guidelines are to provide consensus
recommendations, based on the latest evidence in published
work, current practice and current practice in the region
regarding acne, on: (i) the grading of acne vulgaris in SEA; (ii)
the most appropriate treatment for mild, moderate and severe
acne vulgaris in SEA, as well as maintenance therapy; (iii) antibiotic resistance in the region and appropriate antibiotic use;
and (iv) recommended skin care for patients with acne.
As the consensus recommendations are partly based on the
published work and guidelines, a brief review of published
work and current recommendations of acne management of
various countries from the region are presented prior to a discussion of the groups findings and recommendations.
METHODS
In 2014, the SASA group convened in Singapore to discuss
and provide their insights on current practices and guidelines
regarding acne and its treatment in SEA. Recent developments
and evidence supporting these practices were also shared and
presented. Discussions were then held to assess and determine which practices to adopt and recommend based on evidence and the groups collective experience and expertise.
RESULTS
based on the number and types of lesions present (Table 1).5
This classification ranges from mild to severe based on the
number of papules, pustules and nodules. The Combined Acne
Severity Classification, developed by the Agency for Healthcare
Research and Quality, is similar but takes into account the
specific numbers of comedones, inflammatory lesions, pseudocysts and the total lesion count (Table 2).6 The Comprehensive Acne Severity Scale (CASS) is a subjective, qualitative,
experiential scale developed as a modification of the Investigator Global Assessment (IGA) for clinical trials in acne and was
validated by a very strong correlation with Leeds grading, a
pictorial acne grading system. Whereas the IGA is composed
of eight grades of facial acne, CASS applied the IGA to other
regions also commonly affected by acne such as the chest
and back.7
The classification system developed by the Acne Severity
Global Alliance differs from these by focusing on the type of
lesions present, as opposed to the number of lesions. In this
system, lesions range in severity from mild comedonal acne,
mild and moderate papulopustular acne, moderate nodular
acne, to severe nodular or conglobata acne.
Current treatment guidelines
Health authorities of SEA countries in collaboration with dermatological societies and acne advisory boards have developed
national treatment guidelines.8,9 These evidence-based guidelines, although similar in their approach to acne management,
vary according to local practice conditions (e.g. types of providers available, ethnic groups comprising the population,
health-care system and insurance coverage) and the availability
of treatment modalities and medications.3
The Malaysian and Singaporean guidelines recommend the
use of the CASS. In Japan, the Acne Study Group developed
an evidence-based grading criteria based on dermatologists
recognition of acne severity and inflammatory eruption counts;
the latter were divided into mild (05), moderate (620), severe
(2150) and very severe (>50).10 These and other current SEA
guidelines classify the disease into categories such as mild,
moderate or severe acne, and patients are treated accordingly.
These recommend that first-line to second-line treatment of
mild to moderate acne involve the use of topical medications
such as benzoyl peroxide (BPO), retinoid, azelaic acid, salicylic
acid or their combinations. Oral antibiotics or hormonal therapy
for female patients may be added for cases of moderate acne.
In addition, these guidelines recognize the emergence of
antibiotic resistance and recommend measures to counter its
Definition, diagnosis and grading of acne vulgaris
Currently, there is no single, uniform, standardized and reproducible grading system for the severity of acne. In practice,
acne is commonly classified by the clinical type of manifestation or by disease severity. Clinical types of manifestation
include comedonal, papular, pustular, nodular, cystic, and
inflammatory or non-inflammatory lesions. Severity classification includes mild, moderate, moderately severe and very
severe disease.
The American Academy of Dermatology Acne Consensus
Conference (ACC) developed a classification of acne severity
946
Table 1. Acne classification, acne consensus
(American Academy of Dermatology)5
conference
Description
Grade
Papules and pustules
Nodules
Mild
Moderate
Severe
Few to several
Several to many
Numerous/extensive
None
Few to many
Many
2015 Japanese Dermatological Association
SASA guidelines on acne vulgaris in SEA
Table 2. Acne
classification6
classification,
combined
acne
severity
Description
Grade
Comedones
Inflammatory
lesions
Mild
Moderate
Severe
<20
20100
>100
<15
1550
>50
Total
lesion
count
Pseudocyst
<30
30125
>125
None
None
>5
development. These include limiting the duration of antibiotic
treatment and avoiding concurrent oral and topical antibiotic
use as well as the use of antibiotics as monotherapy or maintenance therapy.
The guidelines also consider acne to be a chronic disease.
Thus, maintenance therapy, with a topical retinoid or the combination of adapalene and BPO, is universally recommended.8,9
Compared with the SEA guidelines, the guidelines of the
American Academy of Dermatology do not recommend a specific acne grading system, maintaining that there is no consensus regarding a single or best system of classification.
Treatment recommendations and the recognition of antibiotic
resistance are similar, but there is no mention of maintenance
therapy. Finally, these guidelines do not include the topic of
light and laser therapy.5
Compared with the others, the European evidence-based
guidelines not only define the variants of acne but also present
its own clinical classification of acne into comedonal acne,
mildmoderate papulopustular acne, severe papulopustular or
moderate nodular acne, and severe nodular or conglobate
acne. It also more closely matches recommendations for therapeutic interventions with specific types and grades of acne.
Like its SEA counterparts, the European guidelines recognize
the importance of the development of antibiotic resistance and
the need for maintenance therapy. These guidelines make no
mention of some adjuvant therapies such as chemical peels,
glycolic acid or trichloroacetic acid.11
Adherence to treatment
Acne requires prolonged treatment, and patient adherence is
important for treatment success. Evidence has shown that
approximately half (48%) of Asian patients are likely to adhere
poorly to their acne treatment regimen.12 Multivariate analysis
of study data revealed the profile of poorly adherent patients.
These patients are usually accompanied during consultation,
do not use moisturizing creams and cleansers, and are poorly
informed about acne.12
Antibiotic resistance
Propionibacterium acnes colonization and proliferation has an
important role in the pathogenesis of inflammatory acne, and
antibiotics have been routinely utilized as the primary treatment for the condition.1315 However, this approach has con-
2015 Japanese Dermatological Association
tributed to the increase in resistant strains of P. acnes over
time.16,17 Antibiotic resistance represents a significant international public health concern as it may lead to reduced clinical
responses, a potential increase in the pathogenicity of P. acnes and increased resistance in more pathogenic organisms.18
Clinically, P. acnes resistance to antibiotics may result in
a reduced response, absence of response or relapse during
acne treatment. Up to 20% of treatment non-responses can
be attributed to antibiotic resistance.1,19,20 In contrast, inhibition of drug resistance has been associated with reduction
in total P. acnes counts and improvement in clinical outcome.21
Studies have shown that use of antibiotics for the treatment
of acne may lead to the development of resistance in targeted
as well as non-targeted organisms, and acne patients receiving antibiotic treatment may be more likely to develop upper
respiratory tract infections compared with those not treated
with antibiotics.19,22,23 Further evidence showed that the number of antibiotic-resistant strains was significantly higher
among patients who received long-term (2452 weeks) antibiotic therapy compared with those who did not receive prior
antibiotic treatment (P = 0.015) and those who received shortterm (618 weeks) treatment (P = 0.036).24,25
Erythromycin and clindamycin are often involved in cases of
resistance, and there is frequent cross-resistance to the two
antibiotics.2633 In a 2001 study performed in Singapore
(Table 3), these antibiotics showed the greatest percentage of
resistant isolates in patients (69.2% and 50%, respectively) followed by co-trimoxazole (38.5%) and doxycycline (23%).25 In
Malaysia, the rates of resistance to erythromycin and clindamycin are 4.092.0% and 4.095.0%, respectively; the highest
rates among the antibiotics listed in Malaysias guidelines.8 In
Singapore (Fig. 1), the number of resistant P. acnes strains has
doubled in approximately a decade (11.0% in 1999 to 22.3%
in 2010).25,34,35
Antibiotic resistance in P. acnes is a global public health
concern (Table 4), and the prevalence of the problem has
increased from 20% in 1978 to 62% in 1996.2232,34 The highest rates of resistance observed are against clindamycin and
erythromycin.2633
In Europe, data from six countries revealed that antibioticresistant P. acnes was present in 67.8% of patients.16 The
highest rates of resistance were found in Spain (93.6%),
Greece (78.2%) and Italy (65.8%), and combined resistance to
clindamycin and erythromycin was much more common than
resistance to tetracyclines.16
According to the World Economic Forum, the greatest risk
to human health is probably the development of antibiotic
resistance. Thus, preventive measures against the rise of
antibiotic-resistant bacteria are warranted.36,37 Judicious use
of antibiotics is thus recommended. Clinical data have shown
that strict administrative control of mupirocin use against
nasal carriage of methicillin-resistant S. aureus resulted in a
decline of resistance in high- and low-level resistance isolates (from 31% to 4% and from 26% to 10%, respectively).38
947
C.L. Goh et al.
Table 3. Antibiotic-resistant isolates of Propionibacterium acnes in Singapore23
Antibiotic
No. of
subjects
Percentage of
isolates
Percentage of
resistant isolates
Prior/present
antibiotic history
Doxycycline
Tetracycline
Minocycline
Co-trimoxazole
Clindamycin
Erythromycin
6
3
3
10
13
18
3.4
1.7
1.7
5.7
7.5
10.3
23
11.5
11.5
38.5
50
69.2
4
3
3
3
9
11
Table 4. Percentages of antibiotic resistance in Propionibacterium
acnes from around the world2431
Country
Clindamycin
Erythromycin
Oxytetracycline
Spain
91
91
USA
79
81
63
Greece
75
75
Doxycycline
57
Egypt
65
48
18
Italy
58
58
UK
55.5
55.5
26.4
Hong
53.5
20.9
16.3
16.3
>11.5
Kong
Figure 1. Isolated strains of Propionibacterium acnes, 1999
2010 in Singapore.
DISCUSSION
Diagnosis and treatment of acne
The SASA group adopts the ACC grading system for acne
severity (Table 1), and recommends the treatment of patients
based on disease severity (Table 5).1,3941
There is no consensus on a single or best grading or classification system, but the ACC system is simple to use with only
three grades of acne severity, while being, as a global evaluation system, both quantitative and cognizant of the variable
expression of the disease.5,40 It is simpler than the CASS,
which has six grades of severity (05), and more clearly separates lesion types per grade.5,7 Although equally easy to use,
the system developed by Japans Acne Study Group does not
differentiate between different types of inflammatory eruptions,
which have a bearing on the risk of development of acne
scars.10 Although the ACC system is Western in origin, it is
applicable to the Asian setting as the pathogenesis of acne
and acne scarring (atrophic and hypertrophic scars) appears to
be both the same in Caucasians and Asians. The main difference in the sequelae of the disease between Caucasians and
Asians is the postinflammatory hyperpigmentation, which commonly occurs among those with a darker skin color but generally resolves with time; thus, it is not considered true scarring
in Asia.4,42
Prior to treatment initiation, it is recommended that differential diagnoses be ruled out. These include acne mechanica
(localized acneiform eruption due to friction or occlusion that is
common in athletes), acne cosmetica (a low-grade, persistent
acneiform eruption due to concurrent use of multiple cosmetic
948
Singapore
>50
>50
>11.5
50
52
35
Iran
France
75.1
9.5
9.5
products), drug-induced acneiform eruptions, Gram-negative
folliculitis and Malassezia folliculitis.
In addition, it is necessary to exclude any underlying medical conditions (polycystic ovary syndrome, Cushings syndrome, 21-hydroxylase deficiency and other endocrinopathies)
and aggravating factors (occupational exposure to oils, greases
and aromatic hydrocarbons; cosmetics; drugs such as steroids, anti-epileptics, isoniazid, lithium, danazol, iodides and
bromides; a history of occlusion or friction; stress; and a high
glycemic load diet).
Following diagnosis, classify the severity of the patients
acne using the ACC grading system and initiate treatment
accordingly. For mild acne, the SASA recommends treatment
with one or a combination of the following topical medications:
retinoids (adapalene, isotretinoin, tazarotene, tretinoin) (once
daily), BPO (once to twice daily), fixed-dose combination of retinoid and BPO (once daily) and topical antibiotics (once to
thrice daily depending on the specific antibiotic). Alternative
topical medications include salicylic acid (once to thrice daily),
azelaic acid (twice daily), topical sulfur and azelaic acid combined with topical sulfur (twice daily) (Table 6).
For moderate acne, a combination of an oral antibiotic such
as doxycycline (100200 mg/day), tetracycline (5001000 mg/
day), minocycline (100200 mg/day), lymecycline (300600 mg/
day) or erythromycin (5001000 mg/day) with topical BPO and
topical retinoids (a fixed combination of BPO and topical retinoids may be used) is recommended.43,44 Antibiotics are prescribed for at least 6 weeks, and patients are reassessed after
68 weeks of treatment. Alternative topical therapy include sal-
2015 Japanese Dermatological Association
SASA guidelines on acne vulgaris in SEA
Table 5. Summary of treatment recommendations, South-East Asia acne study alliance
Recommended
Alternatives
Maintenance
Mild
Moderate
Severe
Topical retinoids
(tretinoin, isotretinoin,
adapalene)
Topical BPO
Topical retinoid + BPO
Topical retinoid and
BPO ! topical antibiotics
Topical salicylic acid, azelaic
acid, topical sulfur, and
azelaic acid with topical sulfur
Oral antibiotics
(doxycycline, tetracycline,
minocycline, lymecycline,
erythromycin) + topical
retinoids + topical BPO
Oral isotretinoin after failed
68-week trial of oral antibiotics
in combination with topical
retinoids and BPO
Topical salicylic acid
Azelaic acid
Hormonal therapy where
indicated in females
(oral contraceptive ! anti-androgens)
Topical retinoids ! BPO
Hormonal therapy where
indicated in females
(oral contraceptive ! anti-androgens)
Topical retinoids ! BPO
Topical retinoids ! BPO
Topical antibiotics should not be used as monotherapy. Oral antibiotics should not be used as monotherapy. BPO + topical retinoids fixed combinations may be used. BPO, benzoyl peroxide.
Table 6. Level of evidence and strength of recommendation for acne medications
Level of evidence and
strength of recommendation
Medication
Therapy
Adapalene
Adapalene 0.1% + BPO 2.5%
Mild to moderate acne vulgaris68
Acne vulgaris when comedones,
papules and pustules are present69
Severe acne vulgaris70
1A1
1A1
Severe acne (nodular or conglobate
acne or acne at risk of permanent scarring)71
Acne vulgaris72
Acne vulgaris20,73
Acne vulgaris when antibiotic
therapy is considered necessary20,74
Papulopustular lesions75
Infections sensitive to tetracycline including acne20,76
Moderate to severe acne related to androgen sensitivity77
Acne vulgaris78
Mild to moderate papulopustular acne7981
Acne82
1A40
Adapalene 0.1% + BPO
2.5% + doxycycline
Isotretinoin
Tretinoin
BPO (2.55.0%)
Tetracycline
Doxycycline
Minocycline
Combined oral contraceptive pill
Salicylic acid
Azelaic acid
Topical sulfur + its combination
1A1,39
1A40
1A40
1A40,41
1A40,41
1A40,41
1A45,46
1A40
1A11,40,7981
2C40
Few well-designed trials of salicylic acids safety and efficacy exist; however, it has been used for many years for the treatment of acne.40 BPO,
benzoyl peroxide.
icylic acid or azelaic acid. For females, hormonal therapy may
be used if indicated; oral contraceptives with or without antiandrogens (e.g. chlormadinone acetate, cyproterone acetate,
drospirenone) may be prescribed.45,46 The efficacy of contraceptive pills has been well demonstrated; they are effective in
reducing inflammatory and non-inflammatory facial acne
lesions, and in meta-analyses, they have been shown to be
probably better first-line alternatives to systemic antibiotics for
long-term acne management in women.45,46 In Asia, however,
the SASA group notes that the acceptability of contraceptive
pills is low, even as an effective form of contraception, due to
perceived adverse effects and cultural or religious factors,
which should be addressed in consultation with the patient.
For severe acne, patients should be initially treated for 6
8 weeks with the recommended regimen for moderate acne. In
2015 Japanese Dermatological Association
the absence of clinical response or improvement after this period, patients with severe acne may be treated with oral isotretinoin, which may be administrated at a dose of 0.51 mg/kg
per day. No substantial additional benefit is expected beyond
a cumulative dose of 120150 mg/kg, and remission is typically
achieved with a 1624-week course of treatment.47 Hormonal
therapy is an alternative approach for female patients with
severe acne, and oral contraceptives with or without antiandrogens may be prescribed.
Maintenance treatment for acne
Acne is a chronic disease and patients may relapse following
treatment discontinuation. The number of microcomedones,
which are reduced during treatment, may increase after topical
treatment is withheld. Hence, maintenance therapy is important
949
C.L. Goh et al.
to prevent relapse.48 Although no consensus definition exists
for maintenance therapy, Wolf et al. provides a useful definition: The regular use of appropriate therapeutic agents to
ensure that visible acne lesions remain in remission.42,48,49
Maintenance treatment is recommended as all acne patients
should benefit from it, especially patients with severe acne, frequent relapses, acne scars and a family history (parental) of
acne scars, a diminished quality of life and long-standing acne.
Medications used as maintenance therapy should target comedones and microcomedones, have a favorable safety profile,
be efficacious and prevent the development of antibiotic resistance in P. acnes.
The most effective therapeutic agents for maintenance therapy are topical retinoids due to their anti-comedogenic and
comedolytic properties.50 Adapalene (level of evidence, 1;
strength of recommendation, A), a topical retinoid, has been
shown to significantly decrease microcomedone formation in
acne patients.48,51 Thiboutot et al. showed that adapalene
0.1% gel significantly reduces lesion counts after 16 weeks of
maintenance therapy compared with placebo.52
Adapalene may also be used in a fixed-dose combination
with BPO. Studies have shown that prolonged treatment
(9 months) with a combination of adapalene 0.1% gel and
BPO 2.5% gel (level of evidence, 1; strength of recommendation, A) maintained low levels of P. acnes and was efficacious
and satisfactory as a maintenance regimen for those with
severe acne.5355
Other medications that may be used for maintenance therapy include BPO and topical azelaic acid. BPO may be used
alone or in combination with a topical retinoid.13,42,56
Adjuvant acne treatment
Patients with acne may be treated with chemical peels. Glycolic acid may be used for comedo-inflammatory lesions and
superficial scars, salicylic acid in polyethylene glycol or salicylic
acid in ethanol may be used for comedo-inflammatory lesions,
and trichloroacetic acid may be used to treat superficial
scars.57
A lipophilic hydroxyl-acid derivative of salicylic acid has
been shown in a randomized trial to be as effective as 5%
BPO for mild to moderate acne, reducing inflammatory and
non-inflammatory acne by 44% and 19%, respectively, in
12 weeks.58 In another study, an antioxidant-optimized topical
1.5% salicylic acid cream containing natural skin penetration
enhancers was shown to be effective and safe when applied
twice daily for the reduction of mild to moderate facial acne.59
Laser, energy-based devices and photodynamic therapies
(PDT) may be used as alternative treatment modalities for
patients who are unable to tolerate or are non-responsive to
standard acne therapies. These include intense pulsed light,
pulsed dye laser, potassium titanyl phosphate laser, neodymium:yttriumaluminumgarnet laser, Q-switched lasers, ultraviolet (UV) light, red and blue lights, and PDT.
Preventing the development of antibiotic resistance
In agreement with guideline recommendations, the SASA highlights the need for effective measures to prevent the develop-
950
ment of antibiotic resistance. These include the avoidance of
antibiotic monotherapy or concurrent oral and topical antibiotic
use, limiting the duration of antibiotic treatment and avoidance
of the use of antibiotics as maintenance therapy. Topical antibiotics should be used in combination with BPO and a topical
retinoid.60 The SASA group recommends that the duration of
oral and topical antibiotic treatment of acne vulgaris should be
less than 12 weeks, with good compliance to treatment. This is
a reasonable duration between the minimum of more than
3 weeks (the amount of time by which antibiotic treatment typically produces an observable improvement) and 68 weeks
(when a reasonable assessment of the efficacy of oral antibiotics can be performed) and the maximum of 816 weeks after
initiation of antibiotic therapy when a patient should be suspected of antibiotic resistance.9,44,61 The SASA recommends
that the response to treatment may be assessed every 8
12 weeks.
Recommended skin care for acne
Skin care is important in the management of acne and involves
cleansing, moisturizing and sun protection (protection against
UV radiation). Studies have shown that washing the face twice
daily with a mild cleanser produced significant improvements
in the skin of patients with acne, and cleansers reduced both
the inflammatory and non-inflammatory lesion counts.62,63 The
ideal cleanser should be non-comedogenic, non-acnegenic,
non-irritating and non-allergenic. Cleansers should also be suitable for the patients skin type; gentle, alcohol-free, and nonabrasive; and may contain active anti-acne ingredients such as
BPO or salicylic acid.
Moisturizers may be used for dry and irritated skin due to
acne treatment and should be water-based, non-greasy, noncomedogenic, non-acnegenic and hypoallergenic. Moisturizers
prevent treatment-induced dryness and improve local tolerance
to topical treatment (level of evidence, 1; strength of recommendation, A).64,65 Moreover, moisturizers do not affect the
efficacy of topical acne treatment, while improving stratum corneum water content and reducing the sensation of dryness.62
These benefits were demonstrated in a study involving adapalene in which patients were randomized to receive either
adapalene alone or adapalene in combination with a moisturizer. At the end of 4 weeks, more patients on adapalene with a
moisturizer remained adherent to treatment and significantly
prolonged the treatment period. The concomitant use of a
moisturizer improved patient adherence without producing
adverse effects or diminishing the therapeutic effects of adapalene. The study further found that adapalene and moisturizers
should be used in combination from the beginning of treatment
to avoid discontinuation due to adverse reactions.66
Protection from UV radiation is an important form of adjuvant therapy in acne treatment, preventing PIH and reducing
photodermatitis due to oral and topical retinoid use. Patients
should be educated and encouraged to protect themselves
using umbrellas or hats as well as sunscreen formulations
which have been shown to be clinically and aesthetically
appropriate for use in the management of acne-prone
patients.67 A broad spectrum, non-comedogenic sunscreen
2015 Japanese Dermatological Association
SASA guidelines on acne vulgaris in SEA
with a sun protection factor of 30 or higher is recommended.
To avoid irritation, a water-based or light liquid-based sunscreen is the best option.
Addressing patient adherence
Based on the profile of non-adherent patients, actions are recommended to address patient non-adherence. Inadequate
knowledge about acne can be addressed by educating or
informing the patient and establishing open communication.
Treatment expectations, the duration of therapy and the time
required to achieve observable improvement must be discussed with the patient. Finally, the importance of skin care
(cleansing and moisturizing) in improving adherence, must be
emphasized.
CONCLUSION
The management of acne vulgaris in SEA is different from that
practiced elsewhere in the world, owing to local variation and
the differences between Asian and Caucasian skin. SASAs
review of the current guidelines used in the region has enabled
the group to devise evidence-based recommendations for the
management of acne.
Compared with the US, European and other SEA guidelines,
the SASA guidelines on the management of acne vulgaris in
SEA patients adopts the use of the ACC grading system for
classification and selection of treatment for patients; specifies
durations of treatment and time frames for expected results
and patient reassessment; and discusses a fuller range of adjuvant acne treatments including chemical peels, laser and PDT.
Among all the guidelines, the SASA guidelines uniquely
address the need for skin care, including cleansing, moisturizing and protection from UV radiation, in the management of
acne and the importance and relationship of skin care to
patient adherence.
Following proper diagnosis of acne, disease severity may be
classified according to the ACC grading system. Patients may
be treated according to disease severity, noting that treatment
must still be individualized. Mild acne may be treated with topical medications including retinoids, BPO, a combination of retinoid and BPO, or a combination of retinoids and BPO with or
without antibiotics. Moderate acne may be treated with a combination of topical retinoid, BPO and an oral antibiotic. Hormonal therapy may be used if indicated in female patients.
Severe acne may be treated with oral isotretinoin if the patient
fails a 68-week trial of combined oral antibiotics and topical
retinoids with BPO. Maintenance treatment is recommended,
and patients may be prescribed topical retinoids with or without BPO. To prevent the development of antibiotic resistance,
topical antibiotics should not be used as monotherapy or used
concurrently with oral antibiotics. These should be used with
good compliance for a maximum of 12 weeks, and the
response to the regimen should be assessed every 8
12 weeks. Skin care during treatment is recommended and
patients should be educated and informed about cleansing,
moisturizing and sun protection. Patient education and communication between the treating physician and the patient is
2015 Japanese Dermatological Association
essential to improve adherence and ensure successful treatment of acne.
ACKNOWLEDGMENTS: The authors would like to thank
MIMS, Singapore for editorial assistance. These recommendations were
developed at an advisory board meeting supported financially by Galderma International.
CONFLICT OF INTEREST:
The authors received research
and traveling grants and honoraria from Galderma International. The authors
have no financial interest in any of the products related to this work.
REFERENCES
1 Thiboutot D, Gollnick H, Bettoli V et al. New insights into the management of acne: an update from the Global Alliance to Improve
Outcomes in Acne group. J Am Acad Dermatol 2009; 60 (5 Suppl):
S1S50.
2 Bowe WP, Joshi SS, Shalita AR. Diet and acne. J Am Acad Dermatol 2010; 63: 124141.
3 Abad-Casintahan F, Chow SK, Goh CL et al. Toward evidencebased practice in acne: consensus of an Asian Working Group.
J Dermatol 2011; 38: 10411048.
4 Chan HH, Alam M, Kono T, Dover JS. Clinical application of lasers
in Asians. Dermatol Surg 2002; 28: 556563.
5 Pochi PE, Shalita AR, Strauss JS et al. Report of the Consensus
Conference on Acne Classification. Washington, D.C., March 24
and 25, 1990. J Am Acad Dermatol 1991; 24: 495500.
6 Issued by funding/sponsoring agency: Management of Acne Volume 1: Evidence Report and Appendixes. Rockville, Md: Dept. of
Health and Human Services (US),Public Health Service; 2001 Sep.
Report No.: 01-E019.Issued by performing agency: Lehmann HP,
Andrews JS, Robinson KA, Holloway VL, Goodman SN. Johns
Hopkins Evidence-based Practice Center. Contract No. 29097
006. Sponsored by the Agency for Healthcare Research and
Quality.
7 Tan JK, Tang J, Fung K et al. Development and validation of a comprehensive acne severity scale. J Cutan Med Surg 2007; 11(6): 211
216.
8 MOH Malaysia. Malaysian Clinical Practice Guidelines on Management of Acne Vulgaris. Malaysia, 2012. Available at: http://
www.moh.gov.my/attachments/7190.pdf. Accessed on 25 June,
2014.
9 Acne Board of the Philippines. Multidisciplinary Treatment Guidelines for Acne. Manila, Philippines: MIMS Pte, 2013.
10 Hayashi N, Akamatsu H, Kawashima M, Acne Study Group. Establishment of grading criteria for acne severity. J Dermatol 2008; 35:
255260.
!no B, Bettoli V et al. European evidence-based (S3)
11 Nast A, Dre
guidelines for the treatment of acne. J Eur Acad Dermatol Venereol
2012; 26 (Suppl 1): 129.
!no B, Thiboutot D, Gollnick H et al. Large-scale worldwide
12 Dre
observational study of adherence with acne therapy. Int J Dermatol
2010; 49: 448456.
13 Gollnick H, Cunliffe W, Berson D et al. Management of acne: a
report from a Global Alliance to Improve Outcomes in Acne. J Am
Acad Dermatol 2003; 49 (1 Suppl): S1S37.
14 Tzellos T, Zampeli V, Makrantonaki E, Zouboulis CC. Treating acne
with antibiotic-resistant bacterial colonization. Expert Opin Pharmacother 2011; 12: 12331247.
15 World Health Organization. The Evolving Threat of Antimicrobial
Resistance - Options for Action. Geneva, Switzerland: World Health
Organization, 2012.
16 Ross JI, Snelling AM, Carnegie E et al. Antibiotic-resistant acne: lessons from Europe. Br J Dermatol 2003; 148: 467478.
951
C.L. Goh et al.
17 Eady EA. Bacterial resistance in acne. Dermatology 1998; 196: 59
66.
18 Humphrey S. Antibiotic resistance in acne treatment. Skin Therapy
Lett 2012; 17: 13.
19 Mills O Jr, Thornsberry C, Cardin CW, Smiles KA, Leyden JJ. Bacterial resistance and therapeutic outcome following three months of
topical acne therapy with 2% erythromycin gel versus its vehicle.
Acta Derm Venereol 2002; 82: 260265.
20 Ozolins M, Eady EA, Avery AJ et al. Comparison of five antimicrobial regimens for treatment of mild to moderate inflammatory facial
acne vulgaris in the community: randomised controlled trial. Lancet
2004; 364: 21882195.
21 Cunliffe WJ, Holland KT, Bojar R, Levy SF. A randomized, doubleblind comparison of a clindamycin phosphate/benzoyl peroxide gel
formulation and a matching clindamycin gel with respect to microbiologic activity and clinical efficacy in the topical treatment of acne
vulgaris. Clin Ther 2002; 24: 11171133.
22 Levy RM, Huang EY, Roling D, Leyden JJ, Margolis DJ. Effect of
antibiotics on the oropharyngeal flora in patients with acne. Arch
Dermatol 2003; 139: 467471.
23 Margolis DJ, Bowe WP, Hoffstad O, Berlin JA. Antibiotic treatment
of acne may be associated with upper respiratory tract infections.
Arch Dermatol 2005; 141: 11321136.
24 Tan HH, Goh CL, Yeo M. Antibiotic sensitivity of Propionibacterium
acnes isolates studied in a skin clinic in Singapore. Arch Dermatol
1999; 135: 723.
25 Tan HH, Goh CL, Yeo MG, Tan ML. Antibiotic sensitivity of Propionibacterium acnes isolates from patients with acne vulgaris in a tertiary dermatological referral centre in Singapore. Ann Acad Med
Singapore 2001; 30: 2225.
26 Rosen T. Antibiotic resistance: an editorial review with recommendations. J Drugs Dermatol 2011; 10: 724733.
27 Luk NM, Hui M, Lee HC et al. Antibiotic-resistant Propionibacterium
acnes among acne patients in a regional skin centre in Hong Kong.
J Eur Acad Dermatol Venereol 2013; 27: 3136.
28 Abdel Fattah NS, Darwish YW. In vitro antibiotic susceptibility patterns of Propionibacterium acnes isolated from acne patients: an
Egyptian university hospital-based study. J Eur Acad Dermatol
Venereol 2013; 27: 15461551.
29 Leyden JJ, Del Rosso JQ. Oral antibiotic therapy for acne vulgaris:
pharmacokinetic and pharmacodynamic perspectives. J Clin Aesthet Dermatol 2011; 4: 4047.
!rate C, Wozniak A, Garcia P. Antimi30 Schafer F, Fich F, Lam M, Ga
crobial susceptibility and genetic characteristics of Propionibacterium acnes isolated from patients with acne. Int J Dermatol 2013; 52:
418425.
31 Mendoza N, Hernandez PO, Tyring SK, Haitz KA, Motta A.
Antimicrobial susceptibility of Propionibacterium acnes isolates
from acne patients in Colombia. Int J Dermatol 2013; 52: 688
692.
32 Moon SH, Roh HS, Kim YH, Kim JE, Ko JY, Ro YS. Antibiotic resistance of microbial strains isolated from Korean acne patients. J Dermatol 2012; 39: 833837.
33 Nakase K, Nakaminami H, Noguchi N, Nishijima S, Sasatsu M. First
report of high levels of clindamycin-resistant Propionibacterium acnes carrying erm(X) in Japanese patients with acne vulgaris. J Dermatol 2012; 39: 794796.
34 Tan HH, Tan AW, Barkham T, Yan XY, Zhu M. Community-based
study of acne vulgaris in adolescents in Singapore. Br J Dermatol
2007; 157: 547551.
35 Coates P, Vyakrnam S, Eady EA, Jones CE, Cove JH, Cunliffe WJ.
Prevalence of antibiotic-resistant propionibacteria on the skin of
acne patients: 10-year surveillance data and snapshot distribution
study. Br J Dermatol 2002; 146: 840848.
36 Spellberg B, Bartlett JG, Gilbert DN. The future of antibiotics and
resistance. N Engl J Med 2013; 368: 299302.
37 Howell L, ed. Global Risks 2013, An Initiative of the Risk Response
Network, 8th edn. Geneva, Switzerland: World Economic Forum,
2013.
952
38 Walker ES, Levy F, Shorman M, David G, Abdalla J, Sarubbi FA. A
decline in mupirocin resistance in methicillin-resistant Staphylococcus aureus accompanied administrative control of prescriptions.
J Clin Microbiol 2004; 42: 27922795.
39 Jarratt M, Bucko AD, Zugaj D, Antipolis S, Dhuin JC. Treatment with
adapalene 0.1%, BPO 2.5% and doxycycline 100 mg/day resulted
in rapid and sustained decrease in Propionibacterium acne. J Am
Acad Dermatol 2010; 62: AB1.
40 Strauss JS, Krowchuk DP, Leyden JJ et al. Guidelines of care for
acne vulgaris management. J Am Acad Dermatol 2007; 56: 651
663.
!no B, Bettoli V, Ochsendorf F, Layton A, Mobacken H, Degreef
41 Dre
H. European recommendations on the use of oral antibiotics for
acne. Eur J Dermatol 2004; 14: 391399.
42 Wolf JE Jr. Maintenance therapy for acne vulgaris: the fine balance
between efficacy, cutaneous tolerability, and adherence. Skinmed
2004; 3: 2326.
43 Davis EC, Callender VD. A review of acne in ethnic skin: pathogenesis, clinical manifestations, and management strategies. J Clin Aesthet Dermatol 2010; 3: 2438.
44 Savage LJ, Layton AM. Treating acne vulgaris: systemic, local and
combination therapy. Expert Rev Clin Pharmacol 2010; 13: S63
S80.
45 Arowojolu AO, Gallo MF, Lopez LM, Grimes DA. Combined oral
contraceptive pills for treatment of acne. Cochrane Database Syst
Rev 2012; 7: CD004425.
46 Koo EB, Petersen TD, Kimball AB. Meta-analysis comparing efficacy
of antibiotics versus oral contraceptives in acne vulgaris. J Am Acad
Dermatol 2014; 71: 450459.
47 Isotretinoin [summary of product characteristics]. Wiltshire, UK: Alliance Pharmaceuticals Ltd, 2013.
48 Gollnick HP, Finlay AY, Shear N, Global Alliance to Improve Outcomes in Acne. Can we define acne as a chronic disease? If so,
how and when? Am J Clin Dermatol 2008; 9: 279284.
pke EM, Gollnick H. Lipid analysis of fol49 Thielitz A, Helmdach M, Ro
licular casts from cyanoacrylate strips as a new method for studying
therapeutic effects of antiacne agents. Br J Dermatol 2001; 145: 19
27.
50 Villasenor J, Berson D, Kroshinsky D. Combination therapy. In: Shalita A, Del Rosso JQ, Webster G, eds. Acne Vulgaris. New York:
Informa Healthcare, 2011.
51 Thielitz A, Sidou F, Gollnick H. Control of microcomedone formation
throughout a maintenance treatment with adapalene gel, 0.1%.
J Eur Acad Dermatol Venereol 2007; 21: 747753.
52 Thiboutot DM, Shalita AR, Yamauchi PS et al. Adapalene gel, 0.1%,
as maintenance therapy for acne vulgaris: a randomized, controlled,
investigator-blind follow-up of a recent combination study. Arch
Dermatol 2006; 142: 597602.
53 Tan J, Stein Gold L, Schlessinger J et al. Short-term combination
therapy and long-term relapse prevention in the treatment of severe
acne vulgaris. J Drugs Dermatol 2012; 11: 174180.
54 Brodell RT, Schlosser BJ, Rafal E et al. A fixed-dose combination of
adapalene 0.1%-BPO 2.5% allows an early and sustained improvement in quality of life and patient treatment satisfaction in severe
acne. J Dermatolog Treat 2012; 23: 2634.
55 Poulin Y, Sanchez NP, Bucko A et al. A 6-month maintenance therapy with adapalene-benzoyl peroxide gel prevents relapse and continuously improves efficacy among patients with severe acne
vulgaris: results of a randomized controlled trial. Br J Dermatol
2011; 164: 13761382.
56 Leyden JJ. A review of the use of combination therapies for the
treatment of acne vulgaris. J Am Acad Dermatol 2003; 49 (3 Suppl):
S200S210.
57 Japanese Dermatological Association. Guidelines for chemical peels
in Japan. J Dermatol 2012; 39: 321325.
! S et al. Randomized study compar58 Bissonnette R, Bolduc C, Seite
ing the efficacy and tolerance of a lipophillic hydroxy acid derivative
of salicylic acid and 5% benzoyl peroxide in the treatment of facial
acne vulgaris. J Cosmet Dermatol 2009; 8: 1923.
2015 Japanese Dermatological Association
SASA guidelines on acne vulgaris in SEA
59 Zheng Y, Wan M, Chen H et al. Clinical evidence on the efficacy
and safety of an antioxidant optimized 1.5% salicylic acid (SA)
cream in the treatment of facial acne: an open, baseline-controlled
clinical study. Skin Res Technol 2013; 19: 125130.
60 Ng HP, Lim C, Pascual RD, et al, eds. Disease management charts,
acne vulgaris. In: MIMS Antimicrobial Thailand 2013/2014, 7th edn.
Bangkok: TIMS (Thailand) Ltd, 2013; A113.
61 Collier AP, Freeman SR, Dellavalle RP. Acne vulgaris. In: Williams
H, Bigby M, Diepgen T, Herxheimer A, Naldi L, Rzany B, eds. Evidence-Based Dermatology, 2nd edn. BMJ BooksUK: 2008; 83
104.
62 Choi JM, Lew VK, Kimball AB. A single-blinded, randomized, controlled clinical trial evaluating the effect of face washing on acne vulgaris. Pediatr Dermatol 2006; 23: 421427.
63 Choi YS, Suh HS, Yoon MY et al. A study of the efficacy of cleansers for acne vulgaris. J Dermatol Treat 2010; 21: 201205.
64 Matsunaga K, Leow YH, Chan R, Kerrouche N, Paliargues F.
Adjunctive usage of a non-comedogenic moisturizer with adapalene
gel 0.1% improves local tolerance: a randomized, investigatorblinded, split-face study in healthy Asian subjects. J Dermatol Treat
2013; 24: 278282.
65 Munehiro A, Murakami Y, Shirahige Y et al. Combination effects of
cosmetic moisturisers in the topical treatment of acne vulgaris.
J Dermatol Treat 2012; 23: 172176.
66 Hayashi N, Kawashima M. Study of the usefulness of moisturizers
on adherence of acne patients treated with adapalene. J Dermatol
2014; 41: 592597.
67 Rougier AM, Zelenkova H, Stracenska J, Richard A. Protective
effect of a broadspectrum UVA-UVB sunscreen in the retinoid
therapy during summer season. J Am Acad Dermatol 2004; 50:
P16.
68 Adapalene (Differin) 0.1% Cream Summary of Product Characteristics. Watford: Galderma (UK) Ltd, March 2014.
69 Adapalene/Benzoyl peroxide (Epiduo) 0.1%/2.5% Gel Summary of
Product Characteristics. Watford: Galderma (UK) Ltd, June 2014.
2015 Japanese Dermatological Association
70 Gold LS, Cruz A, Eichenfield L et al. Effective and safe combination
therapy for severe acne vulgaris: a randomized, vehicle-controlled,
double-blind study of adapalene 0.1%-benzoyl peroxide 2.5%
fixed-dose combination gel with doxycycline hyclate 100 mg. Cutis
2010; 85: 94104.
71 Isotretinoin (Rizuderm) 20 mg Capsule Summary of Product Characteristics. Wiltshire: Alliance Pharmaceuticals Ltd, 08 April 2013.
72 Tretinoin Gel US Pharmacopeia. New Jersey: Triax Pharmaceuticals
LLC, July 2005.
73 Benzoyl peroxide (Acnecide) 5% Gel Cream Summary of Product
Characteristics. Watford: Galderma (UK) Ltd, December 2013.
74 Tetracycline 250 mg Tablet Summary of Product Characteristics.
Berkshire: Intrapharm Laboratories Ltd, 3 January 2014.
75 Doxycycline (Efracea) 40 mg Modified-release Hard Capsules Summary of Product Characteristics. Watford: Galderma (UK) Ltd, 27
February 2014.
76 Minocycline (Aknemin) 100 mg Capsule Summary of Product Characteristics. Reinbek: Almirall Hermal GmbH, 04 September 2013.
77 Cyproterone acetate 2 mg and ethinylestradiol 35 mcg (Dianette)
Tablet Summary of Product Characteristics. Berkshire: Bayer PLC,
01 May 2014.
78 Salicylic acid (Acnisal) 2.0% Cutaneous Solution Summary of Product Characteristics. Wiltshire: Alliance Pharmaceuticals Ltd, 8
December 2014.
79 Azelaic acid (Finacea) 15% Gel Summary of Product Characteristics.
Berkshire: Bayer PLC, 30 June 2014.
80 Iraji F, Sadeghinia A, Shahmoradi Z, Siadat AH, Jooya A. Efficacy of
topical azelaic acid gel in the treatment of mild-moderate acne vulgaris. Indian J Dermatol Venereol Leprol 2007; 73: 9496.
81 Katsambas A, Graupe K, Stratigos J. Clinical studies of 20% azelaic
acid cream in the treatment of acne vulgaris. Comparison with vehicle and topical tretinoin. Acta Derm Venereol Suppl (Stockh) 1989;
143: 3539.
82 Keri J, Shiman M. An update on the management of acne vulgaris.
Clin Cosmet Investig Dermatol 2009; 2: 105110.
953
Вам также может понравиться
- Research Article Plasma Fibrin Clot Properties As Determinants of Bleeding Time in Human Subjects: Association With Histidine-Rich GlycoproteinДокумент11 страницResearch Article Plasma Fibrin Clot Properties As Determinants of Bleeding Time in Human Subjects: Association With Histidine-Rich GlycoproteinAyu Nabila Kusuma PradanaОценок пока нет
- Maternity Hospital Bag Checklist PDFДокумент1 страницаMaternity Hospital Bag Checklist PDFAyu Nabila Kusuma PradanaОценок пока нет
- Jurnal Kulit Ayu 5Документ2 страницыJurnal Kulit Ayu 5Ayu Nabila Kusuma PradanaОценок пока нет
- Journal Pone 0104375Документ7 страницJournal Pone 0104375Ayu Nabila Kusuma PradanaОценок пока нет
- Rabu, 1 Juli 2015 06:00 WIB S/D Kamis, 2 Juli 2015 Pk. 06:00 WIBДокумент23 страницыRabu, 1 Juli 2015 06:00 WIB S/D Kamis, 2 Juli 2015 Pk. 06:00 WIBAyu Nabila Kusuma PradanaОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Acid Base Electolytes QuestionsДокумент4 страницыAcid Base Electolytes QuestionsDonna R. Joyce0% (1)
- Therapeutics in Endodontics: DR Mohamed RabieДокумент75 страницTherapeutics in Endodontics: DR Mohamed RabieAbdelrahman GalalОценок пока нет
- NDC LA - AmerigroupДокумент5 страницNDC LA - Amerigroupkarts23Оценок пока нет
- A 20 Year Old Man Suffered From A Spinal Cord Injury at The C2 To C3 Level As The Result of A Motorcycle AccidentДокумент4 страницыA 20 Year Old Man Suffered From A Spinal Cord Injury at The C2 To C3 Level As The Result of A Motorcycle AccidentqingwenОценок пока нет
- Zentel Tablets: What Is in This LeafletДокумент3 страницыZentel Tablets: What Is in This LeafletLadyKahluaОценок пока нет
- health care system of swedenبДокумент34 страницыhealth care system of swedenبAhmedAljebouli0% (1)
- The Tylenol Crisis: How Effective Public Relations Saved Johnson & JohnsonДокумент7 страницThe Tylenol Crisis: How Effective Public Relations Saved Johnson & Johnsonchocobearsweets100% (1)
- Phenytoin Drug StudyДокумент3 страницыPhenytoin Drug StudyCheezy Bread100% (1)
- Drugs That Require Frequent MonitoringДокумент22 страницыDrugs That Require Frequent MonitoringNader Smadi100% (7)
- Kuantitas Obat Tahun NewДокумент18 страницKuantitas Obat Tahun NewFathia Afriza KurniawatiОценок пока нет
- Classification of DrugsДокумент15 страницClassification of DrugsAwani OОценок пока нет
- Algorithm Hypertension Sci PDFДокумент1 страницаAlgorithm Hypertension Sci PDFGustavo CabanasОценок пока нет
- Incepta Pharmaceuticals LTD Bangladesh Products ListДокумент35 страницIncepta Pharmaceuticals LTD Bangladesh Products Listelectryfing asif82% (11)
- Cream & SalepДокумент6 страницCream & SalepDesti WulandariОценок пока нет
- Medication Conversion ChartДокумент2 страницыMedication Conversion ChartIlinca mirnoviciОценок пока нет
- TGP Luzon SRP - PDF Nov 27Документ14 страницTGP Luzon SRP - PDF Nov 27Hatingmewont Keepyoupretty100% (1)
- 1 Laporan Pengeluaran Obat Dan Alkes Depyan 28 SEPTEMBER 2019Документ18 страниц1 Laporan Pengeluaran Obat Dan Alkes Depyan 28 SEPTEMBER 2019Indah SetyowatiОценок пока нет
- MorphineДокумент13 страницMorphineNajihah Izzah100% (2)
- BAD Specials BookletДокумент12 страницBAD Specials BookletzfjasimОценок пока нет
- Community Pharmacy Practice in PakistanДокумент18 страницCommunity Pharmacy Practice in Pakistanthundercat123Оценок пока нет
- Bek Kelompok 1Документ19 страницBek Kelompok 1kiranaОценок пока нет
- Aparato 3 USP DisoluciónДокумент5 страницAparato 3 USP Disoluciónalejandro elizaldeОценок пока нет
- SH0512Документ12 страницSH0512Anonymous 9eadjPSJNgОценок пока нет
- Psychiatric MedicationДокумент22 страницыPsychiatric MedicationSofia Centro TaerОценок пока нет
- Data Pasien Potensi PRB Jan-Juni 2019Документ212 страницData Pasien Potensi PRB Jan-Juni 2019Adra AdeОценок пока нет
- Co-Pay Rise To Hurt Indigenous: Guardian Picks Up Satisfaction Award 9,062 Meds EnquiriesДокумент2 страницыCo-Pay Rise To Hurt Indigenous: Guardian Picks Up Satisfaction Award 9,062 Meds EnquiriespharmacydailyОценок пока нет
- Drugs MnemonicsДокумент6 страницDrugs MnemonicsDarrylJavier100% (1)
- Drug Deaths in Jefferson County 2015Документ16 страницDrug Deaths in Jefferson County 2015Jeremy W. Gray100% (1)
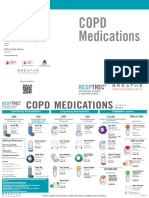
- Courses Offered:: Copd MedicationsДокумент2 страницыCourses Offered:: Copd MedicationsDave BoyОценок пока нет
- Stock Opname Bulan September 2018Документ138 страницStock Opname Bulan September 2018Miftah RamadhanОценок пока нет