Академический Документы
Профессиональный Документы
Культура Документы
ContinuousPositive Airway Pressure and Nasal Trauma in Neonates: A Descriptive Prospective Study
Загружено:
IOSRjournalОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
ContinuousPositive Airway Pressure and Nasal Trauma in Neonates: A Descriptive Prospective Study
Загружено:
IOSRjournalАвторское право:
Доступные форматы
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS)
e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 14, Issue 11 Ver. IV (Nov. 2015), PP 110-116
www.iosrjournals.org
ContinuousPositive Airway Pressure and Nasal Trauma in
Neonates: a descriptive prospective study
Professor Dr.NumanNafie Hameed (FRCPCH, FIBMS, MRCPCH, MAAP, DCH)1,2,
Dr. RaiessYousif Raiees (MBChB)2
1. Department of Pediatrics, College of medicine, Baghdad University, Baghdad
2. Children welfare teaching hospital, medical city, Baghdad, Iraq
Correspondence: Professor Dr. NumanNafie Hameed - College of Medicine, Baghdad University, and
Consultant pediatrician in Children Welfare Teaching Hospital, Medical City Complex, Bab Al-Muadham, PO
box 61023, Code, 12114 Baghdad (Iraq).
Abstract: Objectives:This study aimedto evaluate the frequency and severity of nasal trauma secondary to
nasal continuous positive airway pressure (NCPAP) in neonates.
Methods: This is a prospective observational study carried out in the Neonatal Care Unit (NCU) of Baghdad
teaching hospital,maternity ward, Medical City, Baghdad, Iraq. The study included newborns that underwent
NCPAP with prongs on admission and those receiving NCPAP after weaning from ventilation, from 1st March,
2014 - 1st July, 2014. Patients noses were monitored from the first day of NCPAP treatment until its weaning.
Nasal trauma was reported into three stages: (I) persistent erythema; (II) superficial ulceration; and (III)
necrosis.
Results:Two hundred ten newborns (130 males, 80 females) were enrolled.Mean gestational age was 333.5
weeks (SD), mean birth weight 2044 765g (SD). All patients had some degree of nasal trauma with stage I, II
and III in 93 (44.3%), 52 (24.8%) and 65 (31.0%) patients, respectively. Frequency and severity of trauma were
inversely correlated with gestational age and birth weight. Severe lesion(stageIII)was significantly and directly
positively correlated with the total duration on NCPAP (P<0.00). The risk of nasal trauma was greater in
neonates <32 weeks of gestational age, weighing <1500 g at birth,requiringlarger nasal prong size or smaller
head caps and/or requiringNCPAP>2 days.
Conclusions: Nasal trauma is a frequent complication of NCPAP, especially in smaller preterm babies and in
babies requiring larger nasal prongs or longer NCPAP application.
Keywords:Continuous positive airway pressure, nasal trauma, neonates
I. Introduction
Continuous Positive Airway Pressure (CPAP) has provided an exciting therapy for treating respiratory
distress (RDS) in the newborn. Its primary function is to establish/maintain open airways. The circuit is
structured such that a continuous flow of humidified oxygen in combination with other compressed gases is
delivered to the infants often with nasal prongs or masks(1).
The CPAP goal is accomplished by supplying about 4 8 cmH2O positive airway pressure into infant`s
[2]
airway .To apply this pressure system, three component are essential: continuous flow of a heated and
humidified gas mixture (compressed air and oxygen); a system connecting the device to the patient`s airway
such as facial masks, nasal prongs, nasopharyngeal or endotracheal tubes and a mechanism of positive pressure
generation in thesystem [3-4].
A nasal prong is the most common deviceused because it is a less invasive way of supplying CPAP [3],
typically called nasal CPAP or NCPAP.It is available in different sizes and usually made of light flexible
material [4]. Despite its advantage, this device can harm the nostrils and cause discomfort and disfiguration in the
long term [5].
The local pressure of NCPAP devices may lead to decubitus lesions in the newborn due to its
cutaneous vulnerability and anatomical factors such as end - vascularization of the columella and nostrils [6].In
addition,nasal trauma represents a source of discomfort for patient, possible site of infection and a risk of long
term functional or cosmetic sequelae [7-8].
Research classifies nasal injuries caused by the use of prongs in three stages: mild, moderate and
severe: The mild stage (I) is described as redness or nasal hyperemia; the moderate (II) presents bleeding
injuries and the severe stage (III) refers to injuries with necrosis [9].
Local irritation and trauma to the nasal septum may occur due to misalignment or improper fixation of
nasal prongs [10]. Breakdown and erosion low on the septum at the base of the philtrum can occur when using
nasal masks or prongs, and columella necrosis can occur after only short periods of receiving NCPAP. Nasal
DOI: 10.9790/0853-14114110116
www.iosrjournals.org
110 | Page
Continuouspositive Airway Pressure And Nasal Trauma In Neonates: A Descriptive Prospective
snubbing and circumferential distortion (widening) of the nares can be caused by nasal prongs, especially if
NCPAP is being used for more than just a few days. Inadequate humidification can lead to nasal mucosal
damage [11].
In Baghdad, Iraq, a few studiesof the use of CPAP in neonates but to the best of our knowledge, no
study about nasal trauma after CPAP in neonates in Baghdad has been published.[12] Thisobservational
prospective study aimed to fill this research gap by determiningthe frequency and severity of nasal trauma
secondary to NCPAPwith prongs in neonatal care unit in maternity ward of Baghdad teaching hospital.
II. Methods
This descriptive prospective study was carried out in the Neonatal Care Unit (NCU) of Baghdad
teaching hospital maternity ward.The Ethical committee of the hospital approved this study.One of the research
team(RYR) observed the neonates withtheresponsible nurses help to observe nasal injuries without touching
them.
The study included newborns that underwent NCPAP with prongs on admission and those receiving
NCPAP after weaning from ventilation, from 1st March, 2014 - 1st July, 2014. The sample size was 210
newborns. They were prospectively observed to detect nasal trauma from the first day of NCPAP treatment until
its weaning.
Standard policy in our NCU is to promote the routine use of NCPAP within minutes after birth for all
newborns with respiratory distress regardless of etiology. Pressure of 4 - 6 cmH2O is maintained and oxygen is
adjusted to keep PaO2 >50mm Hg. Endotracheal intubation and mechanical ventilation are considered when
NCPAP is not sufficient to achieve a satisfactory PaO2 while breathing 80100% O2 and/or lower the PaCO2
<65 mm Hg, or to relieve marked retractions or frequent apneas. Weaning NCPAP is considered when the
tachypnea and retractions become minimal or have disappeared and when there is no longer need for
supplemental oxygen. NCPAP is reintroduced when the infant has tachypnea >70/min, deep retractions or
frequent episodes of apnea and bradycardia.
Throughout the study period, the same NCPAP system was used (Fisher and PayKel Bubble-CPAP
system BC 161, New Zealand, UK ). This system involves a source of gas flow (6-8 L /min), air oxygen
blender, humidifier (MR85,Fisher& Paykel Health Care, New Zealand) and respiratory circuit. Nasal tubing
(Flexi trunk) and nasal prongs and masks were alternativelyusedto deliver CPAP. A transparent template is
available from Fisher-Paykel to suggest appropriate nasal prong-size according to the circumference of the nasal
cavity and the width of the septumwas used to determine the size of prongs needed for each infant. Generally
using these guidelines: neonates <1000 g required 35/20; neonates 1000 2000 g required 40/30, and neonates
1500 2499 g required 50/40. The prongs were positioned at least 2 mm from the septum to avoid pressure
necrosisand were secured using a head cap and Velcro felt. [13]
Infant were positioned supine, prone or on their sides generallyflexed.Nursing care included gentle
massages of pressure points of nasal devices every 24 hrwithout any ointment. When a nasal trauma was noted,
an ointment (sodium fusidate 20 mg) was applied with massages. In case of persistent trauma or increased in
severity, a piece of cotton was placed between pressure points and NCPAP devices.
To collect and establish lesions caused by the NCPAP prongs, the stage of lesions, use of protection,
number and type of prongs used, the nurse and researcher took the prongs out of newborns nostrils briefly,
checked their nostrils and immediately replace the prongs. Because inspection was external and not
instrumented, it waspossible to miss isolated internal trauma of the nostrils. Other complimentary data were
extracted from the neonatology charts, medical evolution records and nursing files.
There is currently no widely recognized classification available to describe the severity of nasal trauma
secondary to NCPAP in neonates. We therefore classified trauma based on the standardized classification of
decubitus lesions from the US National Pressure Ulcer Advisory Panel (NPUAP) [14,15].Stage I: erythema not
blanching, on an otherwise intact skin. Stage II: superficial ulcer or erosion, with partial thickness skin loss.
Stage III: necrosis, with full thickness skin loss. When a patient presented with a nasal trauma of different
stages, only the most severe stage was used.
Statistical analysis:Data were analyzed by using the statistical package for social sciences (SPSS) version 21.
Descriptive statistics were presented as mean, standard deviation (SD), frequencies (NO.) and percentages (%).
Chi square testing was used to assess the significance of the association between categorical variables
(frequencies). Students t test was used to compare two means while ANOVA test (analysis of variances) was
used to compare three means. Level of significance (p. value) <0.05 was considered significant. Finally results
and findings were presented in tables and figures with explanatory paragraphs.
DOI: 10.9790/0853-14114110116
www.iosrjournals.org
111 | Page
Continuouspositive Airway Pressure And Nasal Trauma In Neonates: A Descriptive Prospective
III. Results
A total of 210 neonates were enrolled in this study.The mean gestational age was 33.2 3.5 weeks
(range: 25 40). Sixteen neonates (7.6%) had gestational age of < 28 weeks, 69 (32.9%) were 28 32 weeks,
81 (38.6%) were 33 36 weeks and 44 (21%) were 37 weeks.One-Thirty neonates (61.9%) were males versus
80 (38.1%) females. Birth weight ranged from 650 to 3900 grams with a mean of 2044 765 grams. From
these,14 neonates (6.7%) weighed < 1000 gm, 121 (57.6%) weighed 1000 2499 gm, and 75 (35.7%) weighed
2500 gm.
Respiratory distress syndrome (RDS) was the most frequent indication for NCPAP occurring in 144
(68.6%) while 62 (29.5%) had transient tachypnea of the newborn (TTN), and only 2 had apnea of prematurity
and 2 needed respiratory support post extubation.All patients had some degree of nasal trauma with stage I, II
and III in 93 (44.3%), 52 (24.8%) and 65 (31.0%) patients, respectively.
The cross-tabulation (Table 1) between gestational age categories and the lesion stage, and also the
comparison of mean gestational age and stage of the lesion revealed an inverse (negative) but significant
correlation. Additonally, neonates who had a lower gestational age had significantly more severe lesions.
Furthermore the mean gestational age of those neonates with stage 1(mild) lesions was significantly higher than
those with moderate (stage II) and/or severe lesions (stage III) (Fig.1).
There was a significant inverse correlation between the birth weight and stage of the lesion,both
compared as categories or mean along the stages, P<0.001, (Table 2& Fig .2).
There was a direct (positive) significant correlation between the lesion stage and size of nasal piece
(P=0.023). A significant inverse correlation had been found between severity of lesion and the size of head cap
(P<0.001).(Table3)
There was no statistically significant association between the age CPAP was applied and the lesion
stages (P=0.32). Neonates with moderate lesion had the higher mean age when put on CPAP than those with
stage I and stage III, respectively, (P<0.001).
A significant association was found between the age when injury developed and the lesion stages.
The lesion stage was significantly and directly (positive correlation) correlated with the total duration
on CPAP, with severe lesion (stage III)requiring longer duration of NCPAP, (P<0.00), (Table 4 and Fig.3).
IV. Discussion
Nasal CPAP is the preferred means of ventilatory support for most neonates with respiratory distress.
Complications can thus be expected and should be looked for and quantified whenever possible. To date, there
are limited reports in the literature regarding intranasal complications [14].
Comparisons between published studies are difficult because of highly variable descriptions and
definitions of nasal trauma, which can differ in severity from limited local redness to full necrosis. We proposed
a simple and reproducible classification system including three stages adapted from the general classification of
the US NPUAP [14, 15].
The most frequent indication of NCPAP in our study was RDS (68.6%) followed by TTN (29.5%).
These result differ from those of Fischer et al [16], which reveal TTN in the majority of cases (43%), followed
by,aspiration syndrome (30%) and RDS (9%). This may be due to high rate of premature deliveries, elective
cesarean section delivery. The difference in etiologies might effect the rates of different stages of nasal trauma
between locations but this would need require further studies.
The nasal trauma secondary to NCPAP was a frequent complication in our neonates. Stage I lesions
were seen in (44.3%), (stage II) in (24.8%) and (stage III) in (31.0%). These result differ from Nascimento et al
[17]
, who found stage I in 79.6%, stage II in 19.7% and stage III in 0.7% of their neonates.
We postulate that the formation of nasal lesions may be related to health professionals inappropriately
fixing the prongs into the newborns nostrils. More severe damage would be expected if the entire prongs are
inserted such that the device is in direct contact with the columella. In this study, no nasal protection was used,
while it was used in (96.6%) of patients in the study by Nascimento et al [17].
More severe lesions would be expected without the use of protection. Addtionally, inappropriately
small prongs may move more inside the nostrils causing more damage to the septum.
Because of our limited supply of prongs, we could not use new prongs each time therefore, we had to
disinfect our prongs between use Addtionally, we did not exchange and sterilization the system every two
days as recommended in the literature . Routine disinfection of prongs likely leds to detoriation of the material
making it less flexible, a potential risk factor for the development of nasal lesions [18].
There was an inverse (negative) significant correlation between mean gestational age and the lesion
stage. As expected, neonates with younger gestational age had the more severe lesion, as also seen by Fischer et
al [16] and Alsop et al [19], who found that the frequency and severity of nasal trauma increased with lower
gestational age (> 90% in neonate <32 week of gestational age).
DOI: 10.9790/0853-14114110116
www.iosrjournals.org
112 | Page
Continuouspositive Airway Pressure And Nasal Trauma In Neonates: A Descriptive Prospective
As also expected their was a significant inverse correlation between the birth weight and lesion stage,
in agreement with Fischer et al[16]and Robertson et al [20], who estimated relative risk was significantly higher in
patient weighing < 1500 (25%), (20%) respectively.
There was a direct (positive) significant correlation between the lesion stage and size of nasal piece
(P=0.023), as also found by Nascimento et al [17]. Our limited choice of prong sizes may led to more nasal
lesions. The ideal prong size reported in the literature is one not so large that it distends the nostrils and not so
small that it allows extra space between the prong and nostrils [18]. Even though lesions are still observed with
the correct size of prongs, they are present in a smaller proportion. [21]
In contrast toNascimento et al [17], we found a significant but inverse correlation between severity of
lesion and the size of head cap (P<0.001). One explanation maybe that caps too large for the neonates head may
led to increase tube movement and thus trauma to the nose.Thus, it is advisable to ensure adequate cap sizes
limiting pressure on the nostrils to the minimum[20]. Importantly, when the neonate is premature, low birth
weight and/or has a small head circumference he need small head cup and will likely need more time on CPAP,
resulting in increase risk factors for development of nasal injury. In the absence of caps, bandages were fixed
around the head with patches with the same function immobilizing the prongs also possibly affecting the
severity of the nasal lesions. As much as possible, NCPAP tubing should be positioned on the hat following the
manufacturers recommendations without pressure on the skin, pull on the nasal septum, ensuring the absence of
a brow furrow, (indicative of excessive pressure on the nasal septum)[10].
The lesion stage was significantly and directly (positive correlation) correlated with the total duration
on CPAP with severe lesion (stage III) associated withthe longer duration. This was also found by several other
researhers including Fischer et al [16], Yong et al[21], Nascimento et al [17] and Squires and Hyndman [22],who
concluded the frequency of lesions with the use of CPAP with prongs after a minimum period of two days was
100% and time was a risk factor for the development of lesions[17].
V. Conclusions
Nasal trauma is a frequent complication of NCPAP, especially in preterm neonates with RDS. Risk
factors for advanced stages of nasal lesions includes lower gestational age and birth weight, larger size of nasal
prongs, smaller size of head caps and longer duration on CPAP.
We recommend paying special attention when using NCPAP in preterm and low birth weight neonates
especially those with RDS. Addtionally we recommend ensuring application of appropriate size of prongs and
caps; particularly avoiding the use of prongs and caps which are too small. Finally, when possible shorten the
total duration of NCPAP use.
Declaration of interest:The authors report no declarations of interest
Author's contributions: NNH participated in the study design, sequence alignment and drafting and
finalization of the manuscript and submission to the journal. RYR participated in the study design, data
collection, sequence alignment and drafting and finalization of the manuscript. All authors read and approved
the final manuscript.
Acknowledgement
We would like to thank Tina M. Slusher, MD, Associate Professor of Pediatrics, University of
Minnesota-Divsion of Global Pediatrics, Staff Intensivist, Pediatric Intensive Care Unit, Hennepin County
Medical Center, for her generous reviewing the manuscript.
References
[1].
[2].
[3].
[4].
[5].
[6].
[7].
[8].
[9].
PolinRA,Sahni R. Newer experience with CPAP. Seminar on Neonatology, 2002 Oct.; 7(5):379-89.
Liptsen E, Aghai ZH, Pyon KH, Saslow JG, Nakhla T, Long J, et al. Work of breathing during nasal continuous positive airway
pressure in preterm infants: a comparison of bubble vs. variable-flow devices.J Perinatology 2005; 25(7):453-458.
Kahn DJ, Habib RH, Courtney SE.Effects of flow amplitudes on intraprong pressures during bubble versus ventilator-generated
nasal continuous positive airway pressure in premature infants. Pediatrics 2008; 122(5):1009-1013.
Kaur C, Sema A, Beri RS, Puliyel JM. A simple circuit to deliver bubbling CPAP.IndianPediatr 2008; 45 (4):312-314.
Campbell DM, Shah OS, Shah V, Kelly EN. Administration of the continuous positive airway pressure (CPAP) nasal mask versus
nasal prong in premature baby.J. Perinatology 2006 sep.; 26:546-9.
Cartlidge P. The epidermal barrier.SeminNeonatol2000; 5:27380.
Kopelman AE, Holbert D. Use of oxygen cannulas in extremely low birth weight infants is associated with mucosal trauma and
bleeding, and possibly with coagulase-negative staphylococcal sepsis. J Perinatol2003; 23:94.
Smith LP, Roy S. Treatment strategy for iatrogenic nasal vestibular stenosis in young children.Int J PediatrOtorhinolaryngol2006;
70:136973.
Buettiker V, Hug MI, Baenziger O, Meyer C, Frey B. Advantages and disadvantages of different nasal CPAP systems in
newborns.NeonatePed. Intensive Care 2004 Mar.; 30:926-30.
DOI: 10.9790/0853-14114110116
www.iosrjournals.org
113 | Page
Continuouspositive Airway Pressure And Nasal Trauma In Neonates: A Descriptive Prospective
[10].
[11].
[12].
[13].
[14].
[15].
[16].
[17].
[18].
[19].
[20].
[21].
[22].
Loftus BC, Ahn J, Haddad J Jr. Neonatal nasal deformities secondary to nasal continuous positive airway pressure.Laryngoscope
1994; 104(8 Pt 1):1019-1022.
Lee SY, Lopez V. Physiological effects of two temperature settings in preterm infants on nasal continuous airway pressure
ventilation. J ClinNurs 2002;11 (6):845-847.
Hameed NN, Abdul Jaleel RK, Saugstad OD. The use of continuous positive airway pressure in preterm babies with respiratory
distress syndrome: a report from Baghdad, Iraq. J. maternal fetal neonatal medPublished online 19 August 2013, early online: 14.2013 Informa UK Ltd.doi: 10.3109/14767058.2013.825595
De Paoli AG, Morley CJ, Davis P.G. Nasal CPAP for neonates: What do we know in 2003?Arch Dis Child Fetal and Neonatal Ed
2003 May; 88(1):f168-72.
The National Pressure Ulcer Advisory Panel. Pressure ulcer prevalence, cost and risk assessment: consensus development
conference statement.Decubitus 1989; 2: 248.
Black J, Baharestani MM, Cuddigan J, et al. National Pressure Ulcer Advisory Panels updated pressure ulcer staging system. Adv
Skin Wound Care 2007; 20:26974.
Fischer C, Bertelle V, Hohlfeld J, Forcada-Guex M, Stadelmann-Diaw C, Tolsa JF. Nasal trauma due to continuous positive airway
pressure in neonates. Arch Dis Child Fetal Neonate 2010; 95: F447-451.
Nascimento RM, Ferreira ALC, Coutinho ACFP, Verssimo RCSS. The frequency of nasal injury in newborns due to the use of
continuous positive airway pressure with prongs.Rev Latino-am Enfermagem 2009 julho-agosto; 17(4):489-94.
Mazzella M, Bellini C, Calevo MG, Campone F, MassoccoD,Mezzano P, et al. A randomised control study comparing the
InfantFlow Driver with nasal continuous positive airway pressure in preterminfants. Arch Dis Child Fetal Neonatal Ed 2001;
85(2):86-90.
Alsop EA, Cooke J, Gupta S, Sinha SK. Nasal trauma in preterm infants receiving continuous positive airway pressure.Arch Dis
Child 2008; 93: 23.
Robertson NJ, McCarthy LS, Hamilton PA, et al. Nasal deformities resulting from flow driver continuous positive airway pressure.
Arch Dis Child Fetal Neonatal Ed 1996; 75: F20912.
Yong SC, Chen SJ, Boo NY. Incidence of nasal trauma associated with nasal prong versus nasal mask during continuous positive
airway pressure treatment in very low birthweight infants: a randomised control study. Arch Dis Child FetalNeonatal Ed 2005;
90:F480483.
Squires A J, HyndmanM.Prevention of nasal injuries secondary to NCPAP application in the ELBW infant. Neonatal Network
2009; 28(1) 13-26.
Table 1: Correlation between gestational age and lesion stage (severity)
Gestational
Age (weeks)
Total
No.
< 28
28 32
33 36
37
Total
Mean SD
16
69
81
28
210
Lesion stage
Stage I
(mild)
no.
%
3
18.8
11
15.9
51
63.0
28
63.6
93
44.3
34.9 3.3
P
Stage II
(moderate)
no.
0
23
21
8
52
33.3 2.8
%
0.0
33.3
25.9
18.2
24.8
Stage III
(severe)
no.
13
35
9
8
65
30.6 3.5
%
81.3
50.7
11.1
18.2
31.0
0.001sig
0.001sig
Table 2: Correlation between lesion stage and birth weight (N=210)
Birth weight (gm)
< 1000
1000 - 2499
2500
Total
Mean SD
Total
No.
14
121
75
210
Lesion stage
Stage I
(mild)
no.
%
3
21.4
38
31.4
52
69.3
93
44.3
2422 688
P
Stage II
(moderate)
no.
1
36
15
52
2010 680
%
7.1
29.8
20.0
24.8
Stage III
(severe)
no.
10
47
8
65
1530 622
%
71.4
38.8
10.7
31.0
<0.001sig
<0.001sig
Table 3: Correlation between lesion stages and size of nasal piece and head cap
Variable
Size of nasal piece
35 - 20
40 - 30
45 - 40
50 - 40
Size of head cap
17- 22
22- 25
25- 29
29- 36
Total
No.
Lesion stage
Stage I
(mild)
no.
%
Stage II
(moderate)
no.
150
24
2
34
57
14
0
22
38.0
58.3
0.0
64.7
24
95
7
84
5
26
2
60
20.8
27.4
28.6
71.4
DOI: 10.9790/0853-14114110116
Stage III
(severe)
no.
41
5
0
6
27.3
20.8
0.0
17.6
52
5
2
6
34.7
20.8
100.0
17.6
0.023
sig
2
33
2
15
8.3
34.7
28.6
17.9
17
36
3
9
70.8
37.9
42.9
10.7
<0.001
sig
www.iosrjournals.org
114 | Page
Continuouspositive Airway Pressure And Nasal Trauma In Neonates: A Descriptive Prospective
Table 4: Distribution of mean age of put on CPAP, age at injury developed and duration on CPAP
according to the lesion stages
Variable
Lesion stage
Stage I
(mild)
Stage II
(moderate)
Stage III
(severe)
Age when put on CPAP (hrs.)
24 1.1
28.6 12.8
26.4 12.6
0.32NS
Age when injury developed (hrs.)
35.7 13.2
48.2 14.6
43.5 11.7
<0.001
Total duration on CPAP (hrs.)
50.0 14.7
96.4 32.5
137.3 36.3
<0.001
Figure1: Comparison of mean gestational age according to lesion stage
Figure 2: Comparison of mean birth weight according to lesion stage
DOI: 10.9790/0853-14114110116
www.iosrjournals.org
115 | Page
Continuouspositive Airway Pressure And Nasal Trauma In Neonates: A Descriptive Prospective
Figure 3: Comparison of mean duration on CPAP according to lesion stages.
DOI: 10.9790/0853-14114110116
www.iosrjournals.org
116 | Page
Вам также может понравиться
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1091)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- SFMA Score Sheet PDFДокумент7 страницSFMA Score Sheet PDFdgclarkeОценок пока нет
- 9 Major Benefits of Inner Sexual Alchemy AudioДокумент21 страница9 Major Benefits of Inner Sexual Alchemy AudioVasco GuerreiroОценок пока нет
- EvilHat DontReadThisBookДокумент200 страницEvilHat DontReadThisBookfabtinusОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Ophtha SIM 2nd EdДокумент250 страницOphtha SIM 2nd EdRalphОценок пока нет
- Cardiac OutputДокумент37 страницCardiac OutputIndrashish Chakravorty100% (1)
- Arnica The Miracle Remedy - Case RecordsДокумент4 страницыArnica The Miracle Remedy - Case Recordskaravi schiniasОценок пока нет
- VoacangaДокумент12 страницVoacangaLarry Selorm Amekuse100% (1)
- The Impact of Technologies On Society: A ReviewДокумент5 страницThe Impact of Technologies On Society: A ReviewInternational Organization of Scientific Research (IOSR)100% (1)
- Xerostomia Clinical Aspects and TreatmentДокумент14 страницXerostomia Clinical Aspects and TreatmentThanh Điền LưuОценок пока нет
- Peripheral Nerve InjuriesДокумент29 страницPeripheral Nerve InjuriesbrillniksОценок пока нет
- Orbital Trauma NCP and Drug StudyДокумент5 страницOrbital Trauma NCP and Drug StudyDersly LaneОценок пока нет
- Prisma Med - Schneider Electric - or SwitchboardДокумент20 страницPrisma Med - Schneider Electric - or SwitchboardAna RuxandraОценок пока нет
- Prof Ad 100Документ18 страницProf Ad 100Jennine Reyes100% (2)
- Attitude and Perceptions of University Students in Zimbabwe Towards HomosexualityДокумент5 страницAttitude and Perceptions of University Students in Zimbabwe Towards HomosexualityInternational Organization of Scientific Research (IOSR)Оценок пока нет
- "I Am Not Gay Says A Gay Christian." A Qualitative Study On Beliefs and Prejudices of Christians Towards Homosexuality in ZimbabweДокумент5 страниц"I Am Not Gay Says A Gay Christian." A Qualitative Study On Beliefs and Prejudices of Christians Towards Homosexuality in ZimbabweInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Socio-Ethical Impact of Turkish Dramas On Educated Females of Gujranwala-PakistanДокумент7 страницSocio-Ethical Impact of Turkish Dramas On Educated Females of Gujranwala-PakistanInternational Organization of Scientific Research (IOSR)Оценок пока нет
- The Role of Extrovert and Introvert Personality in Second Language AcquisitionДокумент6 страницThe Role of Extrovert and Introvert Personality in Second Language AcquisitionInternational Organization of Scientific Research (IOSR)Оценок пока нет
- A Review of Rural Local Government System in Zimbabwe From 1980 To 2014Документ15 страницA Review of Rural Local Government System in Zimbabwe From 1980 To 2014International Organization of Scientific Research (IOSR)Оценок пока нет
- A Proposed Framework On Working With Parents of Children With Special Needs in SingaporeДокумент7 страницA Proposed Framework On Working With Parents of Children With Special Needs in SingaporeInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Comparative Visual Analysis of Symbolic and Illegible Indus Valley Script With Other LanguagesДокумент7 страницComparative Visual Analysis of Symbolic and Illegible Indus Valley Script With Other LanguagesInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Assessment of The Implementation of Federal Character in Nigeria.Документ5 страницAssessment of The Implementation of Federal Character in Nigeria.International Organization of Scientific Research (IOSR)Оценок пока нет
- Investigation of Unbelief and Faith in The Islam According To The Statement, Mr. Ahmed MoftizadehДокумент4 страницыInvestigation of Unbelief and Faith in The Islam According To The Statement, Mr. Ahmed MoftizadehInternational Organization of Scientific Research (IOSR)Оценок пока нет
- An Evaluation of Lowell's Poem "The Quaker Graveyard in Nantucket" As A Pastoral ElegyДокумент14 страницAn Evaluation of Lowell's Poem "The Quaker Graveyard in Nantucket" As A Pastoral ElegyInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Edward Albee and His Mother Characters: An Analysis of Selected PlaysДокумент5 страницEdward Albee and His Mother Characters: An Analysis of Selected PlaysInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Relationship Between Social Support and Self-Esteem of Adolescent GirlsДокумент5 страницRelationship Between Social Support and Self-Esteem of Adolescent GirlsInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Role of Madarsa Education in Empowerment of Muslims in IndiaДокумент6 страницRole of Madarsa Education in Empowerment of Muslims in IndiaInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Designing of Indo-Western Garments Influenced From Different Indian Classical Dance CostumesДокумент5 страницDesigning of Indo-Western Garments Influenced From Different Indian Classical Dance CostumesIOSRjournalОценок пока нет
- Importance of Mass Media in Communicating Health Messages: An AnalysisДокумент6 страницImportance of Mass Media in Communicating Health Messages: An AnalysisInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Topic: Using Wiki To Improve Students' Academic Writing in English Collaboratively: A Case Study On Undergraduate Students in BangladeshДокумент7 страницTopic: Using Wiki To Improve Students' Academic Writing in English Collaboratively: A Case Study On Undergraduate Students in BangladeshInternational Organization of Scientific Research (IOSR)Оценок пока нет
- BTK AGUSTUS MutasiObatДокумент48 страницBTK AGUSTUS MutasiObatwulanwidya06Оценок пока нет
- Journal On Threpetical Study On MutraДокумент6 страницJournal On Threpetical Study On MutraVijay DawarОценок пока нет
- Patty NCP HyperthermiaДокумент4 страницыPatty NCP HyperthermiaPatricia Jean FaeldoneaОценок пока нет
- Rockaway TimesДокумент48 страницRockaway TimesPeter J. MahonОценок пока нет
- Shock Cheat Sheet PDFДокумент2 страницыShock Cheat Sheet PDFsarahjaimee100% (1)
- Consumos Medicamentos 2020Документ568 страницConsumos Medicamentos 2020LUCERO LOPEZОценок пока нет
- An Insight Into The Quality Assurance of Ayurvedic, Siddha and Unani DrugsДокумент10 страницAn Insight Into The Quality Assurance of Ayurvedic, Siddha and Unani DrugsHomoeopathic PulseОценок пока нет
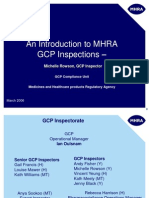
- An Introduction To MHRA GCP Inspections - : Michelle Rowson, GCP InspectorДокумент26 страницAn Introduction To MHRA GCP Inspections - : Michelle Rowson, GCP InspectorSwapnil PanpatilОценок пока нет
- Project Title: Lemon-Garlic Insect RepellentДокумент4 страницыProject Title: Lemon-Garlic Insect RepellentJayvie JavierОценок пока нет
- Pain After Laparoscopic CholecystectomyДокумент6 страницPain After Laparoscopic CholecystectomyMauro Hernandez CoutiñoОценок пока нет
- Housekeeping Check Lists-UpdatedДокумент26 страницHousekeeping Check Lists-UpdatedtanishaОценок пока нет
- RPOC and Homoeopathy - A Practical StudyДокумент4 страницыRPOC and Homoeopathy - A Practical StudyHomoeopathic Pulse100% (2)
- Red Blood Cell CountДокумент4 страницыRed Blood Cell CountMohamed MokhtarОценок пока нет
- Bmi Data May Joie J. AlcarazДокумент13 страницBmi Data May Joie J. AlcarazMay Joie JaymeОценок пока нет
- Current Views On Treatment of Vertigo and Dizziness (JURDING)Документ22 страницыCurrent Views On Treatment of Vertigo and Dizziness (JURDING)arifОценок пока нет
- Andrew Davies - Human Physiology - Ch08 Renal SystemДокумент85 страницAndrew Davies - Human Physiology - Ch08 Renal Systemapi-3814824Оценок пока нет
- HandoutДокумент3 страницыHandoutapi-336657051Оценок пока нет
- L & R PronunciationДокумент265 страницL & R PronunciationdooblahОценок пока нет