Академический Документы
Профессиональный Документы
Культура Документы
Management Ectopic Pregnancy SLCOG
Загружено:
Melissa Aina Mohd YusofАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Management Ectopic Pregnancy SLCOG
Загружено:
Melissa Aina Mohd YusofАвторское право:
Доступные форматы
SLCOG National Guidelines
Management of Ectopic Pregnancy
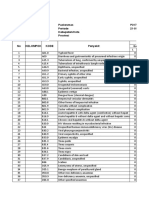
Contents
2.Management of Ectopic
Pregnancy
Page
2.1 Scope of the guideline
2.1.1 Definition
2.1.2 Importance of ectopic pregnancy
29
29
29
2.2 Aetiology
30
2.3 Epidemiology
31
2.4 Diagnosis
2.4.1 History
2.4.2 Examination
2.4.3 Investigations
32
32
33
33
2.5 Management
2.5.1 Levels of management
2.5.2 Management strategies
34
34
35
2. Special circumstances
40
2. .1 Ruptured ectopic pregnancy-management 40
2. .2 Anti-D immunoglobulin
41
2.7 Summary
41
2.8 References
43
Contributed by
Dr. A.G.S.K. Ranaraja
Dr. Saradah Hemapriya
Dr. Harsha Attapattu
Dr. R.M.A.K. Rathnayaka
28
Management of Ectopic Pregnancy
Introduction
The aim of this guideline is to provide recommendations to
aid General Practitioners and Gynaecologists in the
management of Ectopic Pregnancy. This treatment could
be initiated in a primary care setting or in centres with
advanced facilities. The objective of management in
ectopic pregnancy is to make an early diagnosis, treat,
prevent complications, and consequently to improve
quality of life
2.1
fertilized egg to the uterus). On the other hand increase
availability of Gynaecologists and ultrasonography (USS)
facility, most of the ectopic pregnancies are diagnosed
earlier and appropriate management carried out with
reducing maternal mortality and morbidity. This guideline
is intended to improve the morbidity and mortality
associated with ectopic pregnancy.
2.2 Aetiology
Scope of the guideline
2.1.1 Definition
an
SLCOG National Guidelines
An ectopic pregnancy is a pregnancy implanted in
abnormal location (outside of the uterus).
2.1.2 Importance of ectopic pregnancy.
Ectopic pregnancy account for maternal deaths.
The incidence of ectopic pregnancy is 1.8/1000(According
to the UK data). Most of the ectopic pregnancies are sub
clinical/biochemical; therefore true incidence may be
higher. The most common site of ectopic implantation is
the fallopian tube. Other sites such as the abdomen, ovary,
cervix or cornu of the uterus are far less common but are
associated with higher mortality. This higher mortality is
due to greater detection difficulty and to massive bleeding
that can result if rupture occurs at these sites. As a result of
septic abortions and pelvic inflammatory disease (PID), the
incidence of ectopic pregnancies show an increased trend
over the past decades. (During the past 40 years its
incidence has been steadily increasing concomitant with
increased STD rates and associated salpingitis. Such
abnormalities of the tubes prevent normal transport of the
29
The commonest cause of ectopic pregnancy is
salphingitis (causes 50% of first time ectopic
pregnancies).
40% have no known cause. One hypothesis is that
there is slowing of transport through the fallopian
tube of the fertilized egg. This slow transport could
possibly be due to hormonal imbalance (such as
due to progesterone releasing IUD, progestin-only
oral contraceptives). This could also happen in
Artificial Reproductive Technique procedures
(ART) or possibly an abnormality of the embryo.
(e.g. chromosomal)
Cigarette smoking significantly increases a woman's
risk.
Previous history of ectopic pregnancy increases the
risk for another ectopic pregnancy. (Incidence is
7%)
About 25% of women with an ectopic pregnancy
have a history of previous surgery in the abdomen.
30
Management of Ectopic Pregnancy
SLCOG National Guidelines
2.3 Epidemiology
2.4 Diagnosis
How many women suffer from an ectopic pregnancy?
The occurrence of ectopic pregnancy is reported to
be at a rate of about 1-2% of pregnancies and can occur in
any sexually active fertile woman. The increase in incidence
in the past few decades is thought to be due to two factors:
2.4.1 History
I. Increased incidence of salpingitis (infection of the
fallopian tube, usually due to a sexually transmitted
disease (STD), such as Chlamydia or Gonorrhea),
and,
II. Improved ability to detect ectopic pregnancies.
There is a marked increase in ectopic pregnancy
rate with increasing age from . per 1000 pregnancies in
women aged 15 to 24, to 21.5 per 1000 pregnancies in
women aged 35 to 44.
Most ectopic pregnancies occur in women who
have had more than one pregnancy. Only 10% to 15% of
ectopic pregnancies occur in women who have never been
pregnant before.
31
What symptoms can a woman experience with ectopic
pregnancy?
Women in whom it is suspected that they are in
danger of ectopic pregnancy, with the use of testing and
imaging it is now often possible to detect an ectopic
pregnancy
before
symptoms
develop.
It is important to be aware of the symptoms of ectopic
pregnancy because it can occur in any sexually active
woman whether or not she is using contraceptives or has
undergone tubal sterilization.
Symptoms occur as the embryo grows and as
bleeding occurs due to leaking of blood through the
fimbrial opening of the fallopian tube or from rupture of
the tube. Mild bleeding can also occur without causing
symptoms.
The most common symptoms that with which a
woman presents to a doctor are abdominal pain (90-100%
of women), delayed menses (75-90%) and unexpected
bleeding through the vagina (50-80%).
Before rupture occurs, a vague soreness or spastic
(colic) pain in the abdomen may be the only symptom
present.
Abdominal pain can be generalized, or it can be
localized on one side or both sides. About one quarter of
women also have pain in the shoulder because of
diaphragmatic irritation from blood in the abdomen.
During rupture, the pain usually becomes intense.
Other symptoms also occur though less commonly.
Dizziness and fainting occur in about one third of women
with symptoms. Pregnancy symptoms also occur in about
32
Management of Ectopic Pregnancy
20% of women with symptoms. 10% of the time, there can
be an urge to have bowel movement.
2.4.2 Examination
2.4.2.1 Signs
The most common finding is tenderness in the
abdomen and pelvis. Often, a mass is felt on the side of the
uterus (adnexial mass). In about one third of women, an
enlarged uterus is found which is smaller than would be
found in a normal pregnancy, except when an interstitial
pregnancy is present. Tachycardia and hypotension can be
found if there has been profuse blood loss. However, in
most early ectopic pregnancies no abnormal findings
can be found.
SLCOG National Guidelines
2.5 Management
2.5.1 Levels of management.
Level 1.
General Practitioner (GP), Public Health Midwife (PHM),
Medical Officer of Maternal Care (MOMC)
Identification of risk mothers of ectopic pregnancy:
Past history of;
ectopic pregnancy,
septic abortion,
pelvic inflammatory disease (PID).
Recommendation:
Early referral to level 2
2.4.3 Investigations
-HCG Blood levels,
Transvaginal ultrasonography.
(Grade X)
Level 2.
Base Hospital with Obstetrician and Gynaecologist.
Ultrasonography (USS) facility,
Laparotomy facility with or with out Laparoscopy facility.
Level 3.
General Hospital/Teaching Hospital with Obstetrician and
Gynaecologist with all level 2 facilities.
Human
Chorionic
Gonadotrophin
(hCG)
level
measurements available (24 hours)
33
34
Management of Ectopic Pregnancy
2.5.2 Management strategies
2.5.2.1 Expectant management.
Ideal at Level 3.
(Grade Y)
Not all ectopic pregnancy ends up with maternal
morbidity and mortality1. There is 89.3 percent selfresolution of the ectopic pregnancies, but there is poor
efficacy of this method.
Expectant management is an option for;
When ectopic sac less than 2cm. with no identifiable
fetal pole and less than 50ml. of haemoperitoneum on
ultrasonography (USS).
Clinically stable woman with minimal symptoms and a
pregnancy of unknown location.
Clinically stable asymptomatic woman with an
ultrasound diagnosis of ectopic pregnancy and a
decreasing serum human chorionic gonadotrophin
levels (hCG), initially less than serum 1000 iu/l.
SLCOG National Guidelines
should be counselled about the importance of compliance
with follow-up and should be within easy access to the
hospital.
2.5.2.2 Medical Management.
However, one need to realize that selection of
patients for expectant management should be done
selectively with full compliance of the patient following
detailed counselling.
Women managed expectantly should be followed
twice weekly with serial hCG measurements and weekly by
transvaginal examinations to ensure a rapidly decreasing
hCG level (ideally less than 50% of its initial level within
seven days) and a reduction in the size of adnexial mass by
seven days.
Thereafter weekly hCG and transvaginal ultrasound
examinations are advised until serum hCG levels are less
than 20 iu/l as there are case reports of tubal rupture at
low levels of -hCG. In addition, women selected for
expectant management of pregnancy of unknown origin
(Grade Y)
Ideal at level 3
Medical therapy should be offered to suitable
women, and units should have treatment and follow-up
protocols for the use of methotrexate in the treatment of
ectopic pregnancy. In stable patients a variety of medical
treatment options are as effective as surgery.17
If medical therapy is offered, women should be
given clear information (preferably written) about the
possible need for further treatment and adverse effects
following treatment. Women should be able to return easily
for assessment at any time during follow-up.
Medical therapy option may be considered for
women with an hCG level below 3000 iu/l.20, 21
The presence of cardiac activity in an ectopic
pregnancy is associated with a reduced chance of success
following medical therapy and should be considered a
contraindication to medical therapy.11, 12
The drug of choice is methotrexate. It can be given
intravenous / intramuscular /oral or local injection at the
site of the ectopic either laparoscopically, ultra sound
guided hysteroscopically. Intramuscular methotrexate given
as a single dose calculated from patients body surface area
(50 mg/m2). For most women this will be between 75 mg.
and 90 mg. Serum hCG levels are checked on days four
and seven and a further dose is given if hCG levels have
failed to fall by more than 15% between day four and day
seven.12, 18,19
However, the success rate is 75%. According to a
small randomised controlled trial (RCT) there is no
35
36
Management of Ectopic Pregnancy
difference in the outcome except in whom given by local
injection. This also gives rise to relatively low drug related
side effects. Therefore local injection of methotrexate is
preferable to its use systemically.
There are no studies to comment on the
subsequent fertility rate, as most of the trials are small.
Method of administration needs to be addressed carefully
after proper selection of patients.
For example there is high failure rate if the ectopic
is more than 2cm. of fetal pole.
2.5.2.3 Surgical management
i. Laparatomy.
Ideal at level 2
(Grade Y)
Most of the ectopic pregnancies in Sri-lanka
present after rupture and haemo-dynamically unstable.
According to randomised controlled trials (RCT) there is
controversies of stabilizing the patient and then proceeding
with the laparatomy. However, results need to be
considered cautiously. Laparotomy is preferred in haemodynamically unstable patients over laparoscopy. According
to two randomised controlled trials (RCT), laparotomy
patients give subsequent 55% intra-uterine pregnancy
(IUP) rate, 1 . % of recurrent ectopic rate and 1.8%
persistent tropoblastic activity.
SLCOG National Guidelines
randomised controlled trials (RCT) laporoscopic method
give rise to less blood loss, less hospital stay, low cost and
less post-operative analgesic requirements. This study
shows higher intra-uterine pregnancy (IUP) (70%) rate, less
recurrent ectopic (50%) and higher trophoblastic tissue
activity (12. %).
Type of surgery
i. Salphingectomy.
According to meta analysis, this method gives rise
less recurrent ectopic pregnancy rate (10%) and with no
failure of removal of all ectopic tissue. However, there is
no diferrence between laparatomy and laparoscopy except
the advandages of laparoscopy.
In the presence of a healthy contralateral tube there
is no clear evidence that salpingotomy should be used in
preference to salphingectomy.0 -12
ii. Salphingotomy.
Ideal at level 3. This depend on the consultants
preference, and is possible in level 2 as well.
A laparoscopic approach in the surgical
management of tubal pregnancy, in the haemo-dynamically
stable patient, and is preferable to a laparotomy.
This method may be preferable for the ectopic
when diagnosed early and unruptured.1 According to three
According to good quality randomised controlled
trials (RCT) there is higher rate of recurrent ectopic
associated with this method (15%) and higher rate of
trophoblastic activity (11%). However trophoblastic
activity can be managed medically. There is no significant
deference in intrauterine pregnancy (IUP) in both methods.
According to a randomised controlled trial (RCT),
that there is no additional benefit of suturing the
salphingostomy site, because the intrauterine pregnancy
(IUP) rate is similar at 12 month after the surgery with or
without suturing.
Randomised controlled trials (RCT) results suggest
that there may be a higher subsequent intrauterine
pregnancy rate associated with salphingotomy but the
magnitude of this benefit may be small. Data from future
randomised controlled trial (RCT) examining this question
37
38
ii. Laparoscopy.
Management of Ectopic Pregnancy
is needed. The use of conservative surgical techniques
exposes women to a small risk of tubal bleeding in the
immediate postoperative period and the potential need for
further treatment for persistent trophoblastic tissue. Both
these risks and the possibility of further ectopic
pregnancies in the conserved tube should be discussed if
salphingotomy is being considered by the surgeon or
requested by the patient13-1
Laparoscopic salphingotomy should be considered
as the primary treatment when managing tubal pregnancy
in the presence of contralateral tubal disease and the desire
for future fertility.
In women with a damaged or absent contralateral
tube, in vitro fertilization is likely to be required if
salphingectomy is performed13-1 . Because of the
requirement for postoperative follow-up and the treatment
of persistent trophoblasts, the short-term costs of
salphingotomy are greater than salphingectomy.21 However,
if the subsequent need for assisted conception is taken into
account, an increase in intrauterine pregnancy rate of only
3% would make salphingotomy more cost effective than
salphingectomy.19 In the presence of contralateral tubal
disease the use of more conservative surgery is appropriate.
These women must be made aware of the risk of a further
ectopic pregnancy.13
39
SLCOG National Guidelines
Recommendations.
(Grade X)
1.Laparascopic method is superior to laparatomy method with
regard to less cost, shorter hospital stay, less analgesic
requirements, higher subsequent intrauterine pregnancy
(IUP) and less recurrent ectopic rates. Therefore,
laparascopic method needs to be considered as a first
option in unruptured ectopic.
2.Laparatomy is best in the case of life saving as well as with
inadequate facilities.
3.Medical management should be conducted only by wellexperienced consultants with emergency facilities at hand.
4.Expectant management should be carried out only with
reliable and compliable patients.
2.6 Special circumstances
2.6.1 Ruptured Ectopic Pregnancy Management
Management of tubal pregnancy in the presence of
haemodynamic instability should be by the most
expedient method. In most cases this will be laparotomy.
There is no role for medical management in the
treatment of tubal pregnancy or suspected tubal pregnancy
when a patient shows signs of hypovolaemic shock.
Transvaginal ultrasonography can rapidly confirm the
presence of haemoperitoneum, if there is any diagnostic
uncertainty. But expedient resuscitation and surgery should be
undertaken. Experienced operators may be able to manage
laparoscopically, women with even a large haemoperitoneum
safely, but the surgical procedure which prevents further
blood loss most quickly should be used. In most centers this
will be laparotomy.
(Grade X)
40
Management of Ectopic Pregnancy
2.6.2 Anti-D immunoglobulin
Non-sensitized women who are Rhesus negative
with a confirmed or suspected ectopic pregnancy should
receive anti-D immunoglobulin.
(Grade X)
SLCOG National Guidelines
ultrasonography and weekly -hCG measurements
until the level is < 10 mIU/ml.
All pregnant women who are Rh-negative should
receive Rh immunoglobulin.
2.7 Summary
Single dose methotrexate is best used for those who
are asymptomatic, whose -hCG is < 3000
mIU/ml, have tubal size < 3 cm, have no fetal
cardiac activity on ultrasonography, and will come
in to be followed closely. It cannot be used if there
is a heterotopic pregnancy.
Despite low and declining -hCG levels, tubal
rupture can still occur with methotrexate treatment.
With severe pelvic pain, monitoring of vital signs
and hematocrit can help differentiate between tubal
abortion and tubal rupture.
Most common side effects of methotrexate are;
a) stomatitis,
b) conjunctivitis,
c) mild abdominal pain of short duration. Rare
side effects include dermatitis and pruritis.
Surgery is done only if transvaginal ultrasonography
shows an ectopic pregnancy.
Laparoscopic surgery has been found to be superior
to laparotomy and can treat most patients.
Persistent ectopic pregnancy refers to the continued
growth of trophoblastic tissue after surgery. Special
attention should be given to the proximal portion
during surgery and the ectopic pregnancy should be
flushed out with suction irrigation.
Expectant management is done when ectopic
pregnancy is suspected, and transvaginal
ultrasonography does not show an ectopic
pregnancy. The patient is followed with weekly
41
42
Management of Ectopic Pregnancy
2.6 References
01. Medline search 200 first quarter.
02. North American O&G journal 200 /july.
03. Progress of O&G 12th edition.
04.Green top Guideline Royal College of Obstetricians &
Gynaecologists guideline No 21 June 2004
05. Hospital medicine 200 /August
0 . Thornton K, Diamond M, DeCerney A. Linear salpingostomy for
ectopic pregnancy. Obstet Gynecol Clin North Am 1991; 18:95
109.
07. Clausen I. Conservative versus radical surgery for tubal pregnancy.
Acta Obstet Gynecol Scand. 199 ;75:812.
08. Mol BW,Hajenius PJ, Engelsbel S,Ankum WM,Hemrika DJ, van
der Veen F, et al. Is conservative surgery for tubal pregnancy
preferable to salpingectomy? An economic analysis. Br J Obstet
Gynaecol 1997; 104:8349.
09. Parker J, Bisits A. Laparoscopic surgical treatment of ectopic
pregnancy: salpingectomy or salpingostomy? Aust. N Z J Obstet
Gynaecol 1997; 37:1157. Gynecol 1999;42:318.
10. Tulandi T, Saleh A. Surgical management of ectopic pregnancy.
Clin Obstet Gynecol 1999;42:318.
11. Yao M,Tulandi T.Current status of surgical and nonsurgical
management of ectopic pregnancy. Fertil Steril 1997; 7: 2133.
12. Sowter M, Frappell J. The role of laparoscopy in the management
of ectopic pregnancy. Rev Gynaecol Practice 2002;2:7382.
13. Silva P, Schaper A, Rooney B. Reproductive outcome after 143
laparoscopic procedures for ectopic pregnancy. Fertil Steril 1993;
81:7105.
14. Job-Spira N, Bouyer J, Pouly J, Germain E, Coste J,AubletCuvelier B, et al. Fertility after ectopic pregnancy: first results of a
population-based cohort study in France.Hum Reprod 199 ;11:99
104.
15. Mol B,Matthijsse H,Tinga D,Huynh T,Hajenius P,Ankum W, et al.
Fertility after conservative and radical surgery for tubal
pregnancy.Hum Reprod 1998;13:18049.
1 . Bangsgaard N,Lund C,Ottesen B,Nilas L.Improved fertility
following conservative surgical treatment of ectopic pregnancy. Br
J Obstet Gynaecol 2003; 110:7 570.
17. Lipscomb G, Bran D, McCord M, Portera J, Ling F.Analysis of
three hundred fifteen ectopic pregnancies treated with single-dose
methotrexate. Am J Obstet Gynecol 1998; 178:13548.
43
SLCOG National Guidelines
18. Saraj A,Wilcox J, Najmabadi S, Stein S, Johnson M, Paulson R.
Resolution of hormonal markers of ectopic gestation: a
randomized
trial
comparing
single-dose
Intramuscular
methotrexate with salpingostomy. Obstet Gynecol 1998;92:98994.
19. Sowter M, Farquhar C, Petrie K, Gudex G. A randomized trial
comparing single dose systemic methotrexate and laparoscopic
surgery for the treatment of unruptured tubal pregnancy. Br J
Obstet Gynaecol 2001; 108:192203.
20. Sowter M, Farquhar C, Gudex G.An economic evaluation of single
dose systemic methotrexate and laparoscopic surgery for the
treatment of unruptured ectopic pregnancy. Br J Obstet Gynaecol
2001; 108:20412.
21. Mol B,Hajenius P,Engelsbel S,Ankum W,Hemrika D,Van der Veen
F, et al. Treatment of tubal pregnancy in the Netherlands:an
economic comparison of systemic methotrexate administration
and laparoscopic salpingostomy. Am J Obstet Gynecol 1999;
181:94551.
44
Вам также может понравиться
- Brief DescriptionДокумент7 страницBrief DescriptionPrincess Pilove GawongnaОценок пока нет
- Ectopic PregnancyДокумент5 страницEctopic PregnancyFaith FuentevillaОценок пока нет
- No. 34. Management of Infertility Caused by Ovulatory DysfunctionДокумент19 страницNo. 34. Management of Infertility Caused by Ovulatory DysfunctionAnnisa JuwitaОценок пока нет
- Jurnal KEДокумент16 страницJurnal KEMuhammad Harris ZainalОценок пока нет
- Ectopic Pregnancy-American Family PhysicianДокумент8 страницEctopic Pregnancy-American Family PhysicianSi vis pacem...Оценок пока нет
- Ultrasonographic Diagnosis and Management of Ectopic PregnancyДокумент25 страницUltrasonographic Diagnosis and Management of Ectopic PregnancyMuhammad AbeeshОценок пока нет
- Ectopic Pregnancy Diagnosis and TreatmentДокумент39 страницEctopic Pregnancy Diagnosis and TreatmentFecky Fihayatul IchsanОценок пока нет
- Pregnant Woman TemplateДокумент11 страницPregnant Woman TemplateRegine Mae Morales EncinadaОценок пока нет
- Tubal Ectopic PregnancyДокумент38 страницTubal Ectopic Pregnancy6ixSideCreate MОценок пока нет
- Nama: Zaimah Shalsabilla Kelas: Alpha NIM: 04011181520071Документ11 страницNama: Zaimah Shalsabilla Kelas: Alpha NIM: 04011181520071shalsaОценок пока нет
- Early Pregnancy Loss - Practice Essentials, Background, PathophysiologyДокумент10 страницEarly Pregnancy Loss - Practice Essentials, Background, PathophysiologyAldair SanchezОценок пока нет
- Tubal Ectopic Pregnancy PB193Документ13 страницTubal Ectopic Pregnancy PB193Sheyla Orellana PurillaОценок пока нет
- Bleeding During PregnancyДокумент69 страницBleeding During PregnancyMohnnad Hmood AlgaraybhОценок пока нет
- Ectopic PregnancyДокумент24 страницыEctopic PregnancybertouwОценок пока нет
- Practice Bulletin: Medical Management of Ectopic PregnancyДокумент7 страницPractice Bulletin: Medical Management of Ectopic PregnancyChangОценок пока нет
- Ectopic Pregnancy: MoreДокумент18 страницEctopic Pregnancy: Moreaaaaa_01Оценок пока нет
- Ectopic Pregnancy22Документ43 страницыEctopic Pregnancy22Sunil YadavОценок пока нет
- Ectopic Pregnancy: Causes, Symptoms & TreatmentДокумент10 страницEctopic Pregnancy: Causes, Symptoms & TreatmentXo Yem0% (1)
- Ectopic Pregnancy ThesisДокумент8 страницEctopic Pregnancy ThesisWriteMyPaperCollegeSingapore100% (2)
- Practice Bulletin: Management of Preterm LaborДокумент10 страницPractice Bulletin: Management of Preterm LaborXimena OrtegaОценок пока нет
- Incomplete AbortionДокумент4 страницыIncomplete AbortionAira Jane MuñozОценок пока нет
- Early Pregnancy Problems: Presented byДокумент28 страницEarly Pregnancy Problems: Presented byMalk OmryОценок пока нет
- NCM 109-Module 1 Lesson 1Документ30 страницNCM 109-Module 1 Lesson 1MARY ROSE DOLOGUINОценок пока нет
- Assessment and Management of Miscarriage: Continuing Medical EducationДокумент5 страницAssessment and Management of Miscarriage: Continuing Medical EducationCallithya BentleaОценок пока нет
- Ectopic PregnancyДокумент17 страницEctopic PregnancyMelissa Aina Mohd YusofОценок пока нет
- Threatened Abortion ReportДокумент8 страницThreatened Abortion ReportMohamad RaisОценок пока нет
- Ectopic Pregnancy: by Amielia Mazwa Rafidah Obstetric and Gynecology DepartmentДокумент43 страницыEctopic Pregnancy: by Amielia Mazwa Rafidah Obstetric and Gynecology DepartmentAlrick AsentistaОценок пока нет
- Best modality for diagnosing ectopic pregnancyДокумент31 страницаBest modality for diagnosing ectopic pregnancyantonio91uОценок пока нет
- Infertility PDFДокумент12 страницInfertility PDFdian_c87100% (1)
- Tubal Ectopic Pregnancy: (Replaces Practice Bulletin Number 191, February 2018)Документ18 страницTubal Ectopic Pregnancy: (Replaces Practice Bulletin Number 191, February 2018)Rubio Sanchez JuanОценок пока нет
- Early Pregnancy LossДокумент20 страницEarly Pregnancy LossRima HajjarОценок пока нет
- Articles of Abnormal Obstetrics CasesДокумент11 страницArticles of Abnormal Obstetrics CasesMarjun MejiaОценок пока нет
- Ectopic PregnancyДокумент3 страницыEctopic PregnancySiska FriedmanОценок пока нет
- Ectopic Pregnancy: Medlineplus TopicsДокумент9 страницEctopic Pregnancy: Medlineplus TopicsJonathan BendecioОценок пока нет
- INTRODUCTIO1Документ10 страницINTRODUCTIO1Diane ChuОценок пока нет
- Detecting and Managing Ectopic PregnancyДокумент21 страницаDetecting and Managing Ectopic Pregnancyﻣﻠﻚ عيسىОценок пока нет
- Clinical Manifestations, Diagnosis, and Management of Ectopic PregnancyДокумент18 страницClinical Manifestations, Diagnosis, and Management of Ectopic PregnancyJorge MincholaОценок пока нет
- Medical and Surgical Complications of Pregnancy 08 AДокумент139 страницMedical and Surgical Complications of Pregnancy 08 A2012Оценок пока нет
- Ectopic PregnancyДокумент18 страницEctopic PregnancyWondimu EliasОценок пока нет
- Ectopic PregnancyДокумент26 страницEctopic PregnancyMalek.Fakher1900Оценок пока нет
- Abortion and Ectopic PregnancyДокумент3 страницыAbortion and Ectopic PregnancyJefelson Eu Palaña NahidОценок пока нет
- PRESENTING PATIENTДокумент70 страницPRESENTING PATIENTCharmaineTadereraОценок пока нет
- Breast CancerДокумент6 страницBreast CancercchiechieОценок пока нет
- Elizabeth G. Querubin BSN 3E1-9 - Group 195 A Ectopic PregnancyДокумент16 страницElizabeth G. Querubin BSN 3E1-9 - Group 195 A Ectopic PregnancyLizeth Querubin97% (38)
- Ectopic Pregnancy1Документ34 страницыEctopic Pregnancy1Kreshimaricon FurigayОценок пока нет
- 2022.TP (Ectopic Pregnancy) NOUNSДокумент6 страниц2022.TP (Ectopic Pregnancy) NOUNSWilson BenitezОценок пока нет
- PREGNANC1Документ20 страницPREGNANC1SriramОценок пока нет
- Belle Preterm BirthДокумент9 страницBelle Preterm BirthRashed ShatnawiОценок пока нет
- Diagnosis of Preterm Labor and Overview of Preterm BirthДокумент15 страницDiagnosis of Preterm Labor and Overview of Preterm BirthKenny IncsОценок пока нет
- Prolonged PregnancyДокумент41 страницаProlonged PregnancyArif Febrianto100% (1)
- Embarazo Ectopico Tubarico ACOG 2018Документ13 страницEmbarazo Ectopico Tubarico ACOG 2018Jesus SuarezОценок пока нет
- Postterm Pregnancy and IUFDДокумент24 страницыPostterm Pregnancy and IUFDNejib M/AminОценок пока нет
- CS - PP FinalДокумент30 страницCS - PP FinalNicole ArandingОценок пока нет
- Case Study On Ectopic PregnancyДокумент4 страницыCase Study On Ectopic PregnancyDalene Erika GarbinОценок пока нет
- Ectopic Pregnancy TestДокумент20 страницEctopic Pregnancy Testali alrashediОценок пока нет
- EctopicДокумент13 страницEctopicAnonymous P5efHbeОценок пока нет
- Guide to Pediatric Urology and Surgery in Clinical PracticeОт EverandGuide to Pediatric Urology and Surgery in Clinical PracticeОценок пока нет
- Creamy Chicken EnchiladasДокумент2 страницыCreamy Chicken EnchiladasMelissa Aina Mohd YusofОценок пока нет
- Enchiladas With Smoked Salmon English 1Документ2 страницыEnchiladas With Smoked Salmon English 1Melissa Aina Mohd YusofОценок пока нет
- Capone A Final ProposalДокумент8 страницCapone A Final ProposalMelissa Aina Mohd YusofОценок пока нет
- Recipe - Spiced Pecan ChickenДокумент1 страницаRecipe - Spiced Pecan ChickenMelissa Aina Mohd YusofОценок пока нет
- Chicken Enchiladas With Chopped CabbageДокумент1 страницаChicken Enchiladas With Chopped CabbageMelissa Aina Mohd YusofОценок пока нет
- Chicken MitochondriaДокумент9 страницChicken MitochondriaMelissa Aina Mohd YusofОценок пока нет
- Mel's Case Write Up 2Документ18 страницMel's Case Write Up 2Melissa Aina Mohd YusofОценок пока нет
- TV Recipe - Chicken Enchiladas - April 2011Документ1 страницаTV Recipe - Chicken Enchiladas - April 2011Melissa Aina Mohd YusofОценок пока нет
- David Stroka Recipes - Whole EnchiladaДокумент1 страницаDavid Stroka Recipes - Whole EnchiladaMelissa Aina Mohd YusofОценок пока нет
- Medieval Norwegian Baked Cinnamon-Saffron ChickenДокумент2 страницыMedieval Norwegian Baked Cinnamon-Saffron ChickenMelissa Aina Mohd YusofОценок пока нет
- Chicken Chicken Chicken: Chicken Chicken: Doug Zongker University of WashingtonДокумент3 страницыChicken Chicken Chicken: Chicken Chicken: Doug Zongker University of WashingtonMelissa Aina Mohd YusofОценок пока нет
- Speciesnotes DomesticfowlДокумент4 страницыSpeciesnotes DomesticfowlMelissa Aina Mohd YusofОценок пока нет
- KCBS Meat Inspections GuideДокумент2 страницыKCBS Meat Inspections GuideMelissa Aina Mohd YusofОценок пока нет
- Anglo-Saxon Chicken Stew with Herbs & BarleyДокумент1 страницаAnglo-Saxon Chicken Stew with Herbs & BarleyMelissa Aina Mohd YusofОценок пока нет
- Boston Medical Center Nutrition Resource Center: Recipe by Tracey BurgДокумент1 страницаBoston Medical Center Nutrition Resource Center: Recipe by Tracey BurgMelissa Aina Mohd YusofОценок пока нет
- Pan Seared Orange ChickenДокумент2 страницыPan Seared Orange ChickenMelissa Aina Mohd YusofОценок пока нет
- Easy Roasted Chicken Recipe for OneДокумент1 страницаEasy Roasted Chicken Recipe for OneMelissa Aina Mohd YusofОценок пока нет
- 3759 Frozen To Finish RecipesДокумент4 страницы3759 Frozen To Finish RecipesMelissa Aina Mohd YusofОценок пока нет
- ChickenpoxДокумент2 страницыChickenpoxMelissa Aina Mohd YusofОценок пока нет
- ChickenДокумент2 страницыChickenMelissa Aina Mohd YusofОценок пока нет
- Chicken Chicken Chicken: Chicken Chicken: Doug Zongker University of WashingtonДокумент3 страницыChicken Chicken Chicken: Chicken Chicken: Doug Zongker University of WashingtonMelissa Aina Mohd YusofОценок пока нет
- Chicken Prices (: Boneless/Skinless Chicken Breast................ $2.29/lbДокумент1 страницаChicken Prices (: Boneless/Skinless Chicken Breast................ $2.29/lbMelissa Aina Mohd YusofОценок пока нет
- Chicken Goujons - DipДокумент1 страницаChicken Goujons - DipMelissa Aina Mohd YusofОценок пока нет
- Chicken Primavera Grocery ListДокумент1 страницаChicken Primavera Grocery ListMelissa Aina Mohd YusofОценок пока нет
- Production of Transgenic Chickens Using Lentiviral VectorsДокумент3 страницыProduction of Transgenic Chickens Using Lentiviral VectorsMelissa Aina Mohd YusofОценок пока нет
- Chicken GoujonsДокумент1 страницаChicken GoujonsMelissa Aina Mohd YusofОценок пока нет
- Vals ChickenДокумент1 страницаVals ChickenMelissa Aina Mohd YusofОценок пока нет
- Easy Roasted Chicken Recipe for OneДокумент1 страницаEasy Roasted Chicken Recipe for OneMelissa Aina Mohd YusofОценок пока нет
- LH Poultry Home Production Broiler ChickensДокумент4 страницыLH Poultry Home Production Broiler ChickensMelissa Aina Mohd YusofОценок пока нет
- Chicken Forage ListДокумент2 страницыChicken Forage ListMelissa Aina Mohd YusofОценок пока нет
- Hubungan Pengetahuan Dan Sikap Tentang Antenatal Care Dengan Kunjungan K4 Di Puskesmas Seririt IДокумент12 страницHubungan Pengetahuan Dan Sikap Tentang Antenatal Care Dengan Kunjungan K4 Di Puskesmas Seririt IKETUT TRISIKA PIBRYANAОценок пока нет
- Course Syllabus-Maternity TheoryДокумент6 страницCourse Syllabus-Maternity TheoryannairishybОценок пока нет
- FGDHGNДокумент26 страницFGDHGNAchmad YunusОценок пока нет
- PSmarkup - ARTIKEL PRENATAL MASSAGE-LILIS SURYA WATIДокумент9 страницPSmarkup - ARTIKEL PRENATAL MASSAGE-LILIS SURYA WATIRiya WahyuniОценок пока нет
- Forceps Delivery and Vaccum ExtractionДокумент84 страницыForceps Delivery and Vaccum ExtractionushaОценок пока нет
- 2nd Trimester BleedingДокумент50 страниц2nd Trimester BleedingRaiden VizcondeОценок пока нет
- Course Syllabus Course Name: Obstetrics and Gynecology-2 Sixth YearДокумент18 страницCourse Syllabus Course Name: Obstetrics and Gynecology-2 Sixth Yearali tahseenОценок пока нет
- Obesteric Gynacology Short Notes For Usmle Step 2Документ32 страницыObesteric Gynacology Short Notes For Usmle Step 2Rodaba Ahmadi Meherzad100% (1)
- OB ObjectivesДокумент2 страницыOB ObjectivesDavid LadinОценок пока нет
- Is Sex During Pregnancy Safe?Документ3 страницыIs Sex During Pregnancy Safe?mirrawahabОценок пока нет
- FPДокумент4 страницыFPHearty ArriolaОценок пока нет
- Antenatal Care Counseling: Roll No 11 To 23Документ11 страницAntenatal Care Counseling: Roll No 11 To 23adityarathod612Оценок пока нет
- 2011 - Unsafe Abortion and Postabortion Care - An OverviewДокумент9 страниц2011 - Unsafe Abortion and Postabortion Care - An OverviewJeremiah WestОценок пока нет
- Diagnosis of PregnancyДокумент4 страницыDiagnosis of PregnancyIsrael WoseneОценок пока нет
- Lapkas Ruptur UteriДокумент10 страницLapkas Ruptur UterirandyardinalОценок пока нет
- Puerperal Sepsis Diagnosis and TreatmentДокумент36 страницPuerperal Sepsis Diagnosis and TreatmentRufai Abdul WahabОценок пока нет
- Sample First Trimester Twin Ultrasound ReportДокумент2 страницыSample First Trimester Twin Ultrasound ReportPriyankaОценок пока нет
- A Century of Labor Induction MethodsДокумент4 страницыA Century of Labor Induction MethodsSimon ReichОценок пока нет
- Laporan Bulanan Lb1: 0-7 HR Baru LДокумент20 страницLaporan Bulanan Lb1: 0-7 HR Baru LOla SarlinaОценок пока нет
- No. 31. Assessment of Risk Factors For Preterm BirthДокумент9 страницNo. 31. Assessment of Risk Factors For Preterm BirthenriqueОценок пока нет
- Breech PresentationДокумент46 страницBreech PresentationushaОценок пока нет
- Post Partum HemorrhageДокумент18 страницPost Partum Hemorrhageeric100% (1)
- Multiple PregnancyДокумент7 страницMultiple Pregnancymohammed alkananiОценок пока нет
- Trias RevisiДокумент20 страницTrias RevisiDion PratamaОценок пока нет
- Cesarean Section Audit FormatДокумент6 страницCesarean Section Audit FormatRahul JalauniaОценок пока нет
- Ojsadmin, 993Документ6 страницOjsadmin, 993pondyОценок пока нет
- Duran, Fatima Medriza B. - DR Written OutputsДокумент9 страницDuran, Fatima Medriza B. - DR Written OutputsFatima Medriza DuranОценок пока нет
- Obstetrics V10 Common Obstetric Conditions Chapter Pathology of The Placenta 1663285373Документ11 страницObstetrics V10 Common Obstetric Conditions Chapter Pathology of The Placenta 1663285373Nurliana NingsihОценок пока нет
- Mark Fredderick R. Abejo RN, MAN: Maternal and Child Nursing BulletsДокумент10 страницMark Fredderick R. Abejo RN, MAN: Maternal and Child Nursing BulletsMark DaenosОценок пока нет
- Acog Practice Bulletin Summary: Gestational Hypertension and PreeclampsiaДокумент4 страницыAcog Practice Bulletin Summary: Gestational Hypertension and PreeclampsiaAji PatriajatiОценок пока нет