Академический Документы
Профессиональный Документы
Культура Документы
Hypothyroidism
Загружено:
Lal PathLabsАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Hypothyroidism
Загружено:
Lal PathLabsАвторское право:
Доступные форматы
HYPOTHYROIDISM
INTRODUCTION
Hypothyroidism is defined as a deficiency in thyroid hormone
secretion and action that produces a variety of clinical signs and
symptoms of Hypometabolism.
Overt Hypothyroidism is defined as an elevated serum TSH
concentration (usually above 10 mIU/L) and reduced free
Thyroxine concentration (fT4)
2. Subclinical Hypothyroidism is defined as serum TSH above the
upper reference limit in combination with a normal free Thyroxine
(fT4)
1.
Prevalence
According to a projection from various studies on Thyroid disease,
it has been estimated that about 42 million people in India suffer
from Thyroid diseases. The prevalence of Hypothyroidism was
3.9%. The prevalence of subclinical Hypothyroidism was 9.4%. In
women, the prevalence was higher, at 11.4%, when compared
with men, in whom the prevalence was 6.2%. The prevalence of
subclinical Hypothyroidism increased with age. About 53% of
subjects with subclinical hypothyroidism were positive for antiTPO antibodies.
CLINICAL PRESENTATION
Hypothyroidism
can
affect
all
organ
systems
&
these manifestations are largely independent of the
underlying disorder but are a function of the degree of
hormone deficiency.
CAUSES OF HYPOTHYROIDISM
HASHIMOTOS THYROIDITIS
Hashimotos Thyroiditis is an autoimmune disease in which the thyroid gland is
attacked by a variety of cell and antibody-mediated immune processes, causing
primary Hypothyroidism. The resulting inflammation from Hashimotos disease,
also known as Chronic Lymphocytic Thyroiditis, often leads to an underactive
Thyroid gland (Hypothyroidism).
The diagnosis of Hashimotos Thyroiditis is supported by recognition of
autoantibodies against TPO or Thyroglobulin. 90% of patients with Hashimotos
Thyroiditis have anti-TPO antibodies and anti-Thyroglobulin antibodies, making
these antibodies excellent markers for Hashimotos Thyroiditis. Anti-TPO antibody
positivity is more common at the time of diagnosis than anti-Thyroglobulin
antibody.
Hypothyroidism in Pregnancy
Convincing data suggest that pregnant women who are positive for Thyroid
autoantibodies (especially anti-TPO antibodies) leads to higher frequency of miscarriage
(13.8%) than is seen in pregnant women who lack anti-TPO antibodies (2.4%), and that T4
treatment of the anti-TPO antibody positive group reduces the risk of miscarriage to
approximately 3.5%.
Over Hypothyroidism (OH) in pregnancy is defined as an elevated TSH (>2.5 mIU/L)
in conjunction with a decreased FT4 concentration. Women with TSH levels of 10.0 mIU/L
or above, irrespective of their FT4 levels, are also considered to have OH.
Sub-clinical Hypothyroidism (SCH) in pregnancy is defined as a serum TSH between 2.5
and 10 mIU/L with a normal FT4 concentration.
Isolated Hypothyroxinemia (IH) is defined as a normal maternal TSH concentration
in conjunction with FT4 concentrations in the lower 5th or 10th percentile of the
reference range.
Prevalence
10%-20% of all pregnant women in the first trimester of pregnancy are Thyroid
Peroxidase (TPO) or Thyroglobulin (Tg) antibody positive and Euthyroid
16% of the women who are Euthyroid and positive for TPO or Tg antibody in the
first trimester will develop a TSH that exceeds 4.0 mIU/L by the third trimester,
and 33%-50% of women who are positive for TPO or Tg antibody in the first
trimester will develop postpartum Thyroiditis
2%3% of apparently healthy, non-pregnant women of childbearing age have an
elevated serum TSH. Among these healthy non-pregnant women of childbearing
age it is estimated that 0.3%-0.5% of them would, after having Thyroid function
tests, be classified as having OH, while 2%2.5% of them would be classified as
having SCH
Specific adverse outcomes associated
with maternal Hypothyroidism include:
An increased risk of premature birth, low birth weight, and miscarriage. Such
patients carry an estimated 60% risk of fetal loss when OH was not adequately
detected and treated
Negro and colleagues published data suggesting SCH also increases the risk
of pregnancy complications in anti-thyroid peroxidase antibody positive
(TPOAb+) women
Negro et al. reported a significantly higher miscarriage rate in TPOAb+_ women
with TSH levels between 2.5 and 5.0 mIU/ L compared with those with TSH levels
below 2.5 mIU/L
Recommendations:
Women who are positive for TPOAb and have SCH should be treated with LT4
Women with SCH in pregnancy, who are not initially treated, should be
monitored for progression to OH with a serum TSH and FT4 approximately every 4
weeks until 16-20 weeks gestation and at least once between 26 and 32 weeks
gestation
Isolated Hypothyroxinemia should not be treated in pregnancy
Recommendations:
Anti-Thyroid Peroxidase Antibody (TPOAb) measurements should be considered
when evaluating patients with subclinical Hypothyroidism.
If anti-thyroid antibodies are positive, Hypothyroidism occurs at a rate of 4.3%
per year versus 2.6% per year when anti-thyroid antibodies are negative.
Assessment of serum free T4, in addition to TSH, should be considered when
monitoring L-thyroxine therapy.
Treatment based on individual factors for patients with TSH levels between the
upper limit of a given laboratorys reference range and 10 mIU/L should be
considered particularly if patients have symptoms suggestive of Hypothyroidism,
positive TPOAb or evidence of atherosclerotic cardiovascular disease, heart
failure, or associated risk factors for these diseases.
Recommendations:
Patients whose serum TSH levels exceed 10 mIU/L are at increased risk for heart
failure and cardiovascular mortality, and should be considered for treatment with
L-thyroxine.
Euthyroid women (not receiving LT4) who are TPOAb + require monitoring
for Hypothyroidism during pregnancy. In addition to the risk of Hypothyroidism, it
has been described that being TAb + constitutes a risk factor for miscarriage,
premature delivery, Perinatal death , post-partum dysfunction, and low motor and
intellectual development (IQ) in the offspring.
TEST RANGE AVAILABLE
References:
1.
Indian Journal of Endocrinology & Metabolism. 2011 Jul; 15(Suppl2): S78S81.
2.
Williams text book of Endocrinology, Eleventh edition
3.
Tietz Textbook of Clinical Biochemistry, Fifth Edition
4.
Clinical Practice Guidelines for Hypothyroidism in Adults: Cosponsored by the
American Association of Clinical Endocrinologists and the American Thyroid
Association
References:
1.
Negro R, Schwartz A, Gismondi R, Tinelli A, Mangieri T, Stagnaro-Green A
2010 Universal screening versus case finding for detection and treatment of
thyroid hormonal dysfunction during pregnancy. J Clin Endocrinol Metab
95:16991707.
2.
Negro R, Schwartz A, Gismondi R, Tinelli A, Mangieri T, Stagnaro-Green A
2010 Increased pregnancy loss rate in thyroid antibody negative women with
TSH levels between 2.5 and 5.0 in the first trimester of pregnancy. J Clin
Endocrinol Metab 95:E448
For more information about Health Disease visit https://www.lalpathlabs.com
Hyperthyroidism
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Adrenal Gland - Physiology, Pathology, and Pharmacology - Lecturio PDFДокумент8 страницAdrenal Gland - Physiology, Pathology, and Pharmacology - Lecturio PDFfaiz alamОценок пока нет
- Oet Online - Reading Test 4 A4: 9-If A Hashimoto's Patient Has High Blood Pressure, What Does It Usually Indicate?Документ2 страницыOet Online - Reading Test 4 A4: 9-If A Hashimoto's Patient Has High Blood Pressure, What Does It Usually Indicate?Vistaa SunnyОценок пока нет
- Endocrinology Lab ReportДокумент10 страницEndocrinology Lab Reportapi-285297202Оценок пока нет
- Thyroid GlandДокумент30 страницThyroid GlandahmedkomranОценок пока нет
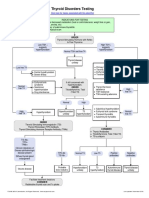
- Thyroid Testing AlgorithmДокумент1 страницаThyroid Testing AlgorithmRezi HelperОценок пока нет
- KKPMT EndokrinДокумент6 страницKKPMT EndokrinDyah CitraОценок пока нет
- Manifestasi Kulit DAN HipotiroidДокумент26 страницManifestasi Kulit DAN HipotiroidAa SsОценок пока нет
- Sciences2lp ModakiratДокумент29 страницSciences2lp Modakiratapi-24974205850% (4)
- HipertiroidДокумент42 страницыHipertiroidCoass XII BonamОценок пока нет
- Diasino Thyroid Test Solutions: Help Raise Thyroid Health AwarenessДокумент2 страницыDiasino Thyroid Test Solutions: Help Raise Thyroid Health AwarenessAbdalazeez AlsayedОценок пока нет
- Performance Task 1Документ3 страницыPerformance Task 1Jellie May RomeroОценок пока нет
- Reproductive Processes: Chapter-34-Lesson-2 Page-961-966Документ26 страницReproductive Processes: Chapter-34-Lesson-2 Page-961-966JanaОценок пока нет
- Anatomy & Physiology of Endocrine SystemДокумент34 страницыAnatomy & Physiology of Endocrine SystemUzma Khan100% (1)
- 015 Physiology MCQ ACEM Primary EndocrineДокумент11 страниц015 Physiology MCQ ACEM Primary Endocrinesandesh100% (1)
- Stages of Lactation ExplainedДокумент35 страницStages of Lactation ExplainedIgnacio FelicityОценок пока нет
- What Is Hormonal ImbalanceДокумент2 страницыWhat Is Hormonal ImbalancestimunoОценок пока нет
- Endocrine System ExplainedДокумент18 страницEndocrine System ExplainedMerlintaОценок пока нет
- Vitamin D and Thyroid Test ResultsДокумент4 страницыVitamin D and Thyroid Test ResultsEkta SinhaОценок пока нет
- MenstrualcyclelecturedrirabonДокумент32 страницыMenstrualcyclelecturedrirabonHananya ManroeОценок пока нет
- Integumentary System TortoraДокумент24 страницыIntegumentary System TortorasyafiqahОценок пока нет
- Pathology of Thyroid DiseasesДокумент5 страницPathology of Thyroid DiseasesGerardLum100% (2)
- TLE Grade-10-3rd-Quarter-Dll-PrДокумент51 страницаTLE Grade-10-3rd-Quarter-Dll-PrMartie AvancenaОценок пока нет
- The skin: the body's largest organДокумент27 страницThe skin: the body's largest organNico Gil GonzalesОценок пока нет
- Endocrine System: Theoretical HandoutДокумент153 страницыEndocrine System: Theoretical HandoutAmy AmyОценок пока нет
- Vphy 143 Lab Experiment 4Документ12 страницVphy 143 Lab Experiment 4Regulus Fidelis SevillaОценок пока нет
- Science 10 - Quiz 1 - Q3W1Документ1 страницаScience 10 - Quiz 1 - Q3W1ChelleОценок пока нет
- Natural World Series Science and Technology Biology.: Heart-The Heart Is A Part of The Circulatory SystemДокумент8 страницNatural World Series Science and Technology Biology.: Heart-The Heart Is A Part of The Circulatory SystemjowieОценок пока нет
- Investigation Observed Value Unit Biological Reference Interval AMH Mullerian Inhibiting Substance 0.185Документ1 страницаInvestigation Observed Value Unit Biological Reference Interval AMH Mullerian Inhibiting Substance 0.185Gangotri GayatriОценок пока нет
- Third Quarter Exam in Science 10Документ3 страницыThird Quarter Exam in Science 10Marife GuadalupeОценок пока нет
- Thyroid Case StudyДокумент68 страницThyroid Case Studyshadydogv5Оценок пока нет