Академический Документы
Профессиональный Документы
Культура Документы
Facial Burns
Загружено:
sevattapillaiАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Facial Burns
Загружено:
sevattapillaiАвторское право:
Доступные форматы
Facial Burns - Our Experience
Received: 11 January 2013; Accepted: 15 February 2013
Conflict of interest: none declared.
AVICENA 2013
DOI: 10.5455/msm.2013.25.26-27
original paper
Mat Soc Med. 2013 Mar 25(1): 26-27
Facial Burns - Our Experience
Violeta Zatriqi 1, Hysni Arifi1, Skender Zatriqi2, Shkelzen Duci1, Sh. Rrecaj1, M. Martinaj1
University Clinical Center of Kosovo, Surgery Clinic, Department of Plastic and Reconstructive Surgery, Pristine Kosovo1
University Clinical Center of Kosovo, Surgery Clinic, Department of abdominal surgery, Pristine, Kosovo2
Corresponding author: Dr. Violeta Zatriqi, candidate PhD. University Clinical Center of Kosovo, Surgery Clinic, Department of Plastic
and Reconstructive Surgery, Pristine, Kosovo. e-mail: vzatriqi@yahoo.com; mob tel. +377 44 136-976
ABSTRACT
Facial burns are generally considered severe. This is due to the possibility of respiratory complications. First responders check the nostrils for singed
hairs. In severe cases there may be soot around the nose and mouth and coughing may produce phlegm that includes ash. Facial and inhalational
burns compromise airways. They pose difficulties in pre-hospital resuscitation and are challenge to clinicians managing surviving burn victims in
the intensive care setting. Management problems resuscitation, airway maintenance and clinical treatment of facial injuries are compounded if the
victim is child. Inhalational burns reduce survivability, certainly in adult victim. In our retrospective study we found that facial burns dominated in
male gender, liquids and scalds are the most common causes of facial burns in children whereas the flame and electricity were the most common
causes of facial burns in adults. We came to the conclusion in our study that surgical treatment minimizes complications and duration of recovery
Key words: facial burns, texture, deeply burned.
1. Introduction
The head and neck region is the most frequent site where a
burn injury occurs. These percentages vary between 27 to 60%,
depending on country, the setting and the definition of what
constitutes a facial burn. Children represent 25 to 50 % of the
total burn population and the prevalence of facial burns in
children is between 24 and 52 % (1). The face is a psychologically significant area of the body and its disfigurement has been
found to have numerous potential psychosocial consequences
for patients. Facial burns are extremely common, making up at
least 30 to 50% of minor to moderate burns. Facial burns are
also present in over 50% of large burns, the vast majority being
partial thickness. Because of the difficulty and complexity of
wound care including pain and the frequent cleansing to avoid
infection, partial thickness burns of the face, often require hospital care (2-6). Superficial second-degree facial burns usually
heal spontaneously without scarring or pigmentary changes.
Medium-thickness second-degree burns, which epithelialize in
10 to 14 days, often heal without scarring, although long-term
alterations in skin pigmentation and texture are frequent. Medium to deep second-degree burns, which epithelialize in 14 to
28 days or longer, must be carefully monitored because they are
prone to the development of late hypertrophic scarring (7)? In
the face, full-thickness burns are rare since the high vascularity
of the face rapidly dissipates the heat. (8, 9).
Also facial burns are often caused by flash burns, which
usually cause partial-thickness burns. However, full-thickness
burns can be seen, especially in contact burns and in the event
of prolonged exposure to the heating source, for example if the
patient was sub- or unconscious or paralyzed at the time of accident. In addition, in some places (e.g. the nose and ears) facial
26
skin is very thin and more vulnerable to deep burns. If nose and
ears are deeply burned, the anatomical structures can change
or disappear (8).
2. Objective
The objective of this study is to understand the causes of
facial burns, depth of facial burns, localization, distribution of
facial burns by gender and over years, the methods of treatments.
3. Materials and methods
This is a retrospective study that included 350 patients with
facial burns treated in 2006-2011 period in Department of Plastic and Reconstructive Surgery Kosova. The data was collected
and analyzed from the archives and protocols of the University
Clinical Center of Kosova.
4. Results
In this retrospective study we included 350 patients in 6 year
period with facial burns. Facial burns were predominant in male
patients with 291 cases or 83.1% while only 59 were female or
16.9% (Table 1). Scald and liquid was responsible for burns in
156 cases or 44.6%, followed by burns due to flame and fire
burns in 109 cases or 31.1% and in 85 cases or 24.3% the cause
of facial burns were flame due electricity (Table 1). Nineteen or
5.4% of patients had only a facial burn and 331 of patients or
94.6% were patients who except face have burned other parts of
the body (Table 1). Superficial burns were present in 298 cases
or 85.1 %, and deep burns were present with 52 cases or 14.9%.
Conservative treatments were applied in 335 cases or 95.7% with
cleaning of burned surface and therefore surgical treatment were
applied in 15 cases or 4.3% (Table 2).
original paper Mat Soc Med. 2013 Mar 25(1): 26-27
Facial Burns - Our Experience
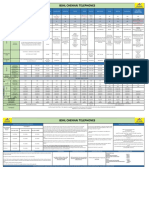
Gender
No.
Male
291
83.1
Female
59
16.9
Cause
350
100.0
scald
156
44.6
flame
109
31.1
electricity
85
24.3
Localization
350
100.0
face
19
5.4
other parts of the body
331
94.6
Total
350
100.0
Table 1. Case distribution by gender, cause and localization.
Depth of the burns
No.
Superficial burns
298
85.1
Deep burns
52
14.9
Treatment
350
100.0
Conservative treatment
335
95.7
Surgical treatment
15
4.3
Total
350
100.0
around the nose and mouth and coughing may produce phlegm
that includes ash. Facial and inhalational burns compromise airways. They pose difficulties in pre-hospital resuscitation and are
challenge to clinicians managing surviving burn victims in the
intensive care setting. Management problems resuscitation,
airway maintenance and clinical treatment of facial injuries are
compounded if the victim is child. Inhalational burns reduce
survivability, certainly in adult victim. In our retrospective study
we found that facial burns dominated in male gender, liquids
and scalds are the most common causes of facial burns in children whereas the flame and electricity were the most common
causes of facial burns in adults. We came to the conclusion in
our study that surgical treatment minimizes complications and
duration of recovery.
REFERENCES
1.
2.
3.
Table 2. Depth of the burns and treatment.
4.
5. Discussion
Facial and inhalational burns compromise airways. They
pose difficulties in pre-hospital resuscitation and are challenge
to clinicians managing surviving burn victims in the intensive
care setting (10-11). In this retrospective study we included 350
patients in 6 year period with facial burns. Facial burns were
predominant in male patients with 291 cases or 83.1% while only
59 were female or 16.9%. A similar study of 1061 patients with
facial burns by Castana et al. reported that females predominated, with an incidence of 61%, compared to a male incidence
of 39% (12). Scald and liquid was responsible for burns in 156
cases or 44.6%, followed by burns due to flame and fire burns in
109 cases or 31.1% and in 85 cases or 24.3% the cause of facial
burns were flame due electricity. Another similar study of 277
patients conducted by Mustafa H.Ali reported that scalds were
the main causes of burn injuries with 49.1%, followed by flame
burns with 37.5% (13). Nineteen or 5.4% of patients had only a
facial burn and 331 of patients or 94.6% were patients who except face have burned other parts of the body. Superficial burns
were present in 298 cases or 85.1%, and deep burns were present
with 52 cases or 14.9%. Conservative treatments were applied in
335 cases or 95.7% with cleaning of burned surface and therefore
surgical treatment were applied in 15 cases or 4.3%.
5.
6. Conclusion
Facial burns are generally considered severe. This is due to the
possibility of respiratory complications. First responders check
the nostrils for singed hairs. In severe cases there may be soot
Mat Soc Med. 2013 Mar 25(1): 26-27 original paper
6.
7.
8.
9.
10.
11.
12.
13.
Hop MJ. Epidemiology of facial burns in Burn Centre Groningen. Master thesis, University of Groningen, Dept. of Medicine
2008.
Robert H. Demling, Leslie Desanti Management of partial
thickness facial burns (comparison of topical antibiotics and bioengineered skin substitutes), Burns 25 (1999), 256-261.
Roper-Hall M. Immediate treatment of thermal and chemical
burns. In: Troutman R, editor. Plastics and reconstructive surgery, Washington: Butterworth, 1962, p. 1991.
Dowling J, Foley, Moncrieff J. Chondritis in the burned ear.
Plastic Reconstr. Surg. 1968:42:115-20.
Baker R. Jones C. Sanders C et al. Degree of burn, location and
length of hospital stay as predictors of psychosocial status and
physical functioning. J. Burn Care Rehab. 1998:17:327-32.
Comitte on trauma. American College of Surgeons. Resources
for optimum care of patients with burn injury. In Resources for
optimum care of the injured patient. Chicago. H. The American
College of Surgeons, 1990. p. 58.
Joseph G. McCarthy, Robert D. Galiano, Sean G. Boutros. Current therapy in Plastic Surgery, Saunders Elsevier, 2006 p.184-93.
Van Baar ME, Oen IMMH, Middelkoop E, Nieuwenhuis MK,
Topical treatment for facial burns (Protocol). Cochrane Database
of Systematic Reviews 2009(4).
Choi M. Panthaki ZJ. Tangential Excision of Burn Wounds.
Journal of Craniofacial Surgery 2008:19(4):1056-60.
Caroline Acton et all. Facial burns in children: A series analysis
with implications for resuscitation and forensic odontology,
Australian Dental Journal 1999:44 :(1):20-24.
Muguti GI, Doolabh DP, Chakanyuka C, Fleming AN. A review
of burns treated over a one year period at Mpilo Central Hospital,
Zimbabwe. J R Coll Surg Edinb 1994; 39:214-217.
Castana et al. Epidemiological survey of burn victims treated as
emergency cases in our hospital in the last five years, Ann Burns
Fire Disasters. 2008 December 31:21(4):171-174.
Mustafa H. Ali. Pattern of burn injuries at King Fahad Hospital,
Al-Baha: A study of 277 cases. Annals of Saudi Medicine. Vol
17(1):1997:104-107.
27
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (120)
- The Health Effects of Cannabis and CannabinoidsДокумент487 страницThe Health Effects of Cannabis and CannabinoidsMiguel Salas-GomezОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Transfusion Reactions and Their ManagementДокумент59 страницTransfusion Reactions and Their ManagementAida AlaudinОценок пока нет
- Myocardial InfarctionДокумент2 страницыMyocardial InfarctionnkosisiphileОценок пока нет
- home-delhimed-downloadfile-IMA NATCON SCIENTIFIC PROGRAME PDFДокумент15 страницhome-delhimed-downloadfile-IMA NATCON SCIENTIFIC PROGRAME PDFRaveenaОценок пока нет
- Pedia ReviewerДокумент27 страницPedia ReviewerEvangeline GoОценок пока нет
- Life and Work of Shri Hans Ji MaharajДокумент75 страницLife and Work of Shri Hans Ji Maharajsevattapillai100% (1)
- Alzheimer's Disease Fact SheetДокумент6 страницAlzheimer's Disease Fact SheetInternational Business Times100% (2)
- LipidsДокумент25 страницLipidsJeaniee Zosa Ebias50% (10)
- Writing Nursing Sample Test 2 2014Документ4 страницыWriting Nursing Sample Test 2 2014Praveen B S PrasadОценок пока нет
- CANINE Impaction Oral SurgeryДокумент46 страницCANINE Impaction Oral SurgeryFourthMolar.com100% (5)
- Penjelasan Consort Utk Artikel KlinisДокумент28 страницPenjelasan Consort Utk Artikel KlinisWitri Septia NingrumОценок пока нет
- Tesis Artcl 13Документ6 страницTesis Artcl 13Setu KatyalОценок пока нет
- Praveena Clinic Visiting CardДокумент1 страницаPraveena Clinic Visiting CardsevattapillaiОценок пока нет
- Profession Tax Procedure OnlineДокумент1 страницаProfession Tax Procedure Onlinehemanvshah892Оценок пока нет
- Closed Reduction Nasal Fracture Post Op InstructionsДокумент2 страницыClosed Reduction Nasal Fracture Post Op InstructionssevattapillaiОценок пока нет
- Plan Vouchers 12092019Документ2 страницыPlan Vouchers 12092019sevattapillaiОценок пока нет
- Basic Preprosthetic SurgeryДокумент27 страницBasic Preprosthetic SurgerysevattapillaiОценок пока нет
- Best Practices OMFS DEPTДокумент2 страницыBest Practices OMFS DEPTsevattapillaiОценок пока нет
- Sterilization of ArmamentariumДокумент41 страницаSterilization of ArmamentariumsevattapillaiОценок пока нет
- Nerve InjuriesДокумент39 страницNerve InjuriessevattapillaiОценок пока нет
- Antibiotics in Oral & Maxillofacial SurgeryДокумент50 страницAntibiotics in Oral & Maxillofacial SurgerysevattapillaiОценок пока нет
- The Effects of Using Hyaluronic Acid On The Extraction SocketsДокумент5 страницThe Effects of Using Hyaluronic Acid On The Extraction SocketssevattapillaiОценок пока нет
- SBV Dissertation Template 2017Документ22 страницыSBV Dissertation Template 2017sevattapillaiОценок пока нет
- Sterilization and AsepsisДокумент48 страницSterilization and AsepsissevattapillaiОценок пока нет
- Lymphangioma of The TongueДокумент3 страницыLymphangioma of The TonguesevattapillaiОценок пока нет
- DNA Probes and Primers in Dental PracticeДокумент6 страницDNA Probes and Primers in Dental PracticesevattapillaiОценок пока нет
- Oral Lesions in Neonates PDFДокумент8 страницOral Lesions in Neonates PDFsevattapillaiОценок пока нет
- Lymphangioma of The Tongue PDFДокумент3 страницыLymphangioma of The Tongue PDFsevattapillaiОценок пока нет
- Jackie ChanДокумент1 страницаJackie ChansevattapillaiОценок пока нет
- Congenital Sublingual CystДокумент5 страницCongenital Sublingual CystsevattapillaiОценок пока нет
- Oral Lesions in NeonatesДокумент8 страницOral Lesions in NeonatessevattapillaiОценок пока нет
- Congenital Ranula in A Newborn A Rare PresentationДокумент3 страницыCongenital Ranula in A Newborn A Rare PresentationsevattapillaiОценок пока нет
- Life of Gajanan Vijay Granthi UneditedДокумент63 страницыLife of Gajanan Vijay Granthi UneditedsevattapillaiОценок пока нет
- Oral LymphangiomaДокумент8 страницOral LymphangiomasevattapillaiОценок пока нет
- A Retrospective Study On The Use of A Dental Dressing To Reduce Dry Socket Incidence in SmokersДокумент5 страницA Retrospective Study On The Use of A Dental Dressing To Reduce Dry Socket Incidence in SmokerssevattapillaiОценок пока нет
- Post-Extraction Complication Course PDFДокумент11 страницPost-Extraction Complication Course PDFsevattapillai100% (1)
- Periapical Lesions - A Review of Clinical, Radiographic, and Histopathologic Features PDFДокумент7 страницPeriapical Lesions - A Review of Clinical, Radiographic, and Histopathologic Features PDFsevattapillaiОценок пока нет
- Nonsurgical Management of Periapical LesionsДокумент11 страницNonsurgical Management of Periapical LesionssevattapillaiОценок пока нет
- Sharma Et Al-2016-Journal of Applied MicrobiologyДокумент11 страницSharma Et Al-2016-Journal of Applied MicrobiologyJoanaОценок пока нет
- Breast Cancer Brachytherapy - More ChoicesДокумент5 страницBreast Cancer Brachytherapy - More ChoicesDr. Robert KuskeОценок пока нет
- Massage Therapy PDFДокумент1 страницаMassage Therapy PDFVirgilio BernardinoОценок пока нет
- Allergy Test PapersДокумент5 страницAllergy Test PapersDaniel MoncadaОценок пока нет
- Ijmrhs Vol 3 Issue 1Документ228 страницIjmrhs Vol 3 Issue 1editorijmrhsОценок пока нет
- The Japanese GMP Regulations 2003Документ46 страницThe Japanese GMP Regulations 2003John LyallОценок пока нет
- The Placebo EffectДокумент2 страницыThe Placebo EffectMeshack RutoОценок пока нет
- Respiratory Physiology: Control of The Upper Airway: Richard L. Horner University of TorontoДокумент8 страницRespiratory Physiology: Control of The Upper Airway: Richard L. Horner University of TorontoDopamina PsicoactivaОценок пока нет
- Hovenia Dulcis - Scientific Review On Usage, Dosage, Side Effects - ExamineДокумент5 страницHovenia Dulcis - Scientific Review On Usage, Dosage, Side Effects - Examineozman blooriОценок пока нет
- How To Control Hypertension (High Blood Pressure) - Nutrition StudiesДокумент3 страницыHow To Control Hypertension (High Blood Pressure) - Nutrition StudiesMatevž BrojanОценок пока нет
- Handbook: For Clinical Management of DengueДокумент124 страницыHandbook: For Clinical Management of DengueraattaiОценок пока нет
- The Information About EDSДокумент3 страницыThe Information About EDSAmber100% (1)
- Hyperosmolar Hyperglycemic State (HHS)Документ21 страницаHyperosmolar Hyperglycemic State (HHS)Malueth AnguiОценок пока нет
- (Trabajo) LRAMP - Linehan PDFДокумент7 страниц(Trabajo) LRAMP - Linehan PDFBreno PMОценок пока нет
- ScabiesДокумент5 страницScabiespakemainmainОценок пока нет
- ACM812 Ventilator - ASCFДокумент1 страницаACM812 Ventilator - ASCFMoussa ToudjaniОценок пока нет
- 5090 w12 QP 11Документ20 страниц5090 w12 QP 11mstudy123456Оценок пока нет
- Sample of An Expository EssayДокумент2 страницыSample of An Expository Essayfatin nadiaОценок пока нет
- Journal Abdominal SurgeryДокумент4 страницыJournal Abdominal SurgeryrizkaОценок пока нет
- Curosurf 120mg / Vial Endotracheopulmonary Instillation Suspension Curosurf 240mg / Vial Endotracheopulmonary Instillation SuspensionДокумент2 страницыCurosurf 120mg / Vial Endotracheopulmonary Instillation Suspension Curosurf 240mg / Vial Endotracheopulmonary Instillation SuspensionHerlinsye PurimahuaОценок пока нет
- Current Directions in ADHD and Its TreatmentДокумент314 страницCurrent Directions in ADHD and Its TreatmentSofía Lecter100% (1)
- 01 - Onsite Sanitation TechnologiesДокумент80 страниц01 - Onsite Sanitation TechnologiesDivyam ShreevatsalОценок пока нет