Академический Документы
Профессиональный Документы
Культура Документы
Cyanotic Heart Disease
Загружено:
mob3Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Cyanotic Heart Disease
Загружено:
mob3Авторское право:
Доступные форматы
Congenital heart disease final year lectures
September 2010
Cyanotic heart disease
Relevant terms
Percent O2 Saturation the proportion of RBC
sites which contain O2.
Partial pressure of O2 - indicates the availability
of O2 in alveolus and serum.
O2 dissociation curve shows the relation of O2
Sat and PO2.
Relevant terms
Oxygen content: 1 gm Hb carries approx
1.39ml of O2 if 100% sat.
O2 cont. adult Hb 15gmHb/dl, 100 % sat:
15 x 1.39 x 1(100% sat) x 10 = 208 O2/L.
O2 cont. adult Hb 15gm Hb, pO2 40(70%sat):
15 x 1.39 x .7 x 10 = 146 O2/L blood.
Relevant terms
Newborn O2 content:
20gm Hb, pO2 40(sat 75%)
20 x 1.39 x .75 x 10 = 208ml/L blood
Newborn O2 content:
12gm Hb, pO2 30(sat 60%)
12 x 1.39 x .60 x 10 = 100ml/L blood.
Congenital heart disease final year lectures
September 2010
Cyanotic CHD
Cyanosis - means blue blood a sign, not a
diagnosis - requires 5gm/dl reduced Hb.
Cyanosis - peripheral, central, differential.
Causes Cardiac, pulmonary, CNS,
haematological.
Approach to the cyanotic infant
PERIPHERAL
Pink mm
PO2 normal
Cool extremities
DD shock, sepsis,
cold
CENTRAL
Blue mm
Low pO2 & O2 sat
Warm extremities.
Cardiac or pulmonary cyanosis?
CARDIAC
PULMONARY
Increase on crying
Decrease on crying
+ or SOB
In resp. distress
Abnormal ECG
Normal ECG
Cxray changes
Cxray changes
pCO2 normal
pCO2 high
Small response to O2 Marked response to O2
Congenital heart disease final year lectures
September 2010
Laboratory studies
Pulse oximetry
Blood gas + 100% O2 challenge.
Pulm/hypovent paO2 <60 to > 200
R to L shunt
to >100
Pulm dis/CCF
to 100 200
Dextrostix. U&E. Hb PCV.
CXRay ECG 2DE
Classification cyanotic CHD
With incr. Pulm blood flow - TGA, TAPVR
truncus arteriosus.
With decr. PBF - TOF, PA, TA.
TGA is commonest cyanotic CHD in NB
period.
TOF is commonest cyanotic CHD at all ages.
Cyanotic CHD
Tetralogy of Fallot
Transposition of great arteries
Tricuspid atresia
Truncus arteriosus
Total anomalous pulmonary ven. Drainage
Hypoplastic left heart syndrome
Pulmonary atresia
Congenital heart disease final year lectures
September 2010
Complications - cyanotic CHD
Polycythemia
Thrombosis
Paradoxical emboli
Cerebral abscess
Infective endocarditis
Tetralogy of Fallot
Components
Ventricular septal defect
RV OT obstruction
RV hypertrophy
Overriding of Aorta
Congenital heart disease final year lectures
September 2010
TOF
Embryology
Anterior and superior displacement of conus
septum resulting in a nonalignment VSD in
the area of the membranous septum.
TOF - Haemodynamics
Large unrestrictive VSD.
Equal RV and LV and aortic pressures.
RVOT obstruction infundibular/valvular/
pulm art/branches.
R to L shunt through VSD to aorta.
Decreased pulmonary blood flow.
Congenital heart disease final year lectures
September 2010
TOF - Clinical features
Usually pink at birth unless defect is severe.
Signs similar to VSD at first
Blue on crying . Persistent cyanosis and
clubbing.
SOB on exercise. Squatting.
Growth and development affected.
Hypercyanotic spells.
TOF - Haemodynamics
R to L shunt increased by a fall in systemic
resistance and an increase in RVOT
obstruction (e g infundibular spasm).
If RVOT obstruction is mild, shunt is L to R
across VSD but ECG shows RVH.
Systemic resistance increases with
squatting, decreases with exercise.
TOF - Blue Spell
Congenital heart disease final year lectures
September 2010
TOF- Physical examination
- classical
General Growth impaired, cyanosis,
clubbing.
Pulses and BP normal.
Heart quiet praecordium, diffuse apex,
RV heave, single S2, ejection SM ULSE
No evidence of CCF.
TOF - Investigations
Hb PCV Pulse oximetry
ECG RAD RVH
Cxray Heart size normal. Decreased PBF.
Boot shaped heart. 25% R aortic arch.
2DE all features demonstrated.
Cardiac catheter preferred by some
surgeons.Coronary art. & pulm art (br) size.
TOF - Boot shaped heart
Congenital heart disease final year lectures
September 2010
Treatment of TOF
Maintain hydration
Treat Fe deficiency. Plebotomy if PCV>65
Anticipate and manage blue spells
Treatment of blue spells
Anticipate. Prevention propanolol p.o.
Knee chest position. Oxygen(not helpful)
IV access - bolus N saline / Hartmanns
- Propranolol / morphine
- Na HCO3, phenylephrine
If severe/persistent - anaesthetise/ventilate
- urgent Sx.
TOF BT shunt
Congenital heart disease final year lectures
September 2010
TOF - Total correction
TOF - Complications
Polycythemia. Infective endocarditis.
Hypercyanotic spells. Failure to thrive
Brain abscesses. Seizures. CVA.
Bleeding disorders.
Decreased development.
Death/ brain damage in blue spell.
Post op complications.
Congenital heart disease final year lectures
September 2010
Transposition of the great arteries
Aorta arises from the RV anterior to and to the R
of the
Pulmonary artery which arises from LV
In the normal heart there is a single circulation in
series
In TGA there are 2 circulations in parallel
Survival depends on a communication between
parallel circulations.
TGA Features
Cyanosis at birth, NB becomes hypoxic and
acidotic.
Cardiac failure in NB period.
When the ductus closes severe hypoxia,
cyanosis and death ensue if there is no other
communication.
10
Congenital heart disease final year lectures
September 2010
TGA
Treatment
maintain ductal patency by IV
prostaglandin E1 in the early NB period or
Perform balloon atrial septostomy until
Definitive surgery - e.g. arterial switch
Balloon atrial septostomy
b
11
Congenital heart disease final year lectures
September 2010
Arterial switch
Truncus arteriosus
Tricuspid atresia
12
Congenital heart disease final year lectures
September 2010
TAPVR
Pulmonary atresia
HYPOLASTIC LH SYN
13
Congenital heart disease final year lectures
September 2010
14
Вам также может понравиться
- Hanan Fathy Pediatric Nephrology UnitДокумент59 страницHanan Fathy Pediatric Nephrology UnitdrhananfathyОценок пока нет
- Cyanotic Heart Disease: Dr.B.BalagobiДокумент38 страницCyanotic Heart Disease: Dr.B.BalagobiGomathi ShankarОценок пока нет
- Cardio-Respiratory Conditions: by DR Priscus MushiДокумент73 страницыCardio-Respiratory Conditions: by DR Priscus MushiMusaОценок пока нет
- Neonatal Central CyanosisДокумент4 страницыNeonatal Central CyanosisRosdiana Elizabeth SiburianОценок пока нет
- CTSU Presentation PDAДокумент41 страницаCTSU Presentation PDAEdwin OkonОценок пока нет
- Approach To A Child With Cyanosis GRP E FINALДокумент37 страницApproach To A Child With Cyanosis GRP E FINALdua.11864Оценок пока нет
- Blalock Taussig Shunt PDFДокумент4 страницыBlalock Taussig Shunt PDFzuraini_mdnoorОценок пока нет
- #5 Neonatal Cardiac AnomaliesДокумент93 страницы#5 Neonatal Cardiac AnomaliesSittie Hania100% (2)
- Neonatology #30-41Документ36 страницNeonatology #30-41Daanish KhorasaniОценок пока нет
- Anaesthetic Concern For One Lung Ventilation: By-Dr - Bhushan Kinge, M.D. Ims - Bhu, VaranasiДокумент57 страницAnaesthetic Concern For One Lung Ventilation: By-Dr - Bhushan Kinge, M.D. Ims - Bhu, VaranasifaisalnaseemkhanОценок пока нет
- CardiacДокумент43 страницыCardiacStephanie TalbotОценок пока нет
- Penyakit Jantung KongenitalДокумент30 страницPenyakit Jantung KongenitalrintiikОценок пока нет
- TOF Diagnosis and ManagementДокумент49 страницTOF Diagnosis and ManagementPrazОценок пока нет
- INNOCENT HEART MURMURSДокумент10 страницINNOCENT HEART MURMURSlindsay_weiss_6Оценок пока нет
- DR Manish Pagaria - Top Tips On Respiratory Calls - 0 - 0 - 0 PDFДокумент56 страницDR Manish Pagaria - Top Tips On Respiratory Calls - 0 - 0 - 0 PDFMadalina OtiliaОценок пока нет
- Management of Cyanotic Child BivinДокумент48 страницManagement of Cyanotic Child BivinChippy BivinОценок пока нет
- Harrison CHapter Summaries - Cadua, Norman VryneДокумент21 страницаHarrison CHapter Summaries - Cadua, Norman VryneNorman Vryne CaduaОценок пока нет
- Gerry B. Acosta, MD, FPPS, FPCC: Pediatric CardiologistДокумент51 страницаGerry B. Acosta, MD, FPPS, FPCC: Pediatric CardiologistChristian Clyde N. ApigoОценок пока нет
- Cyanotic Heart LesionsДокумент40 страницCyanotic Heart LesionsRaison D'etreОценок пока нет
- ucu-CHDs_240114_230618 (2)Документ68 страницucu-CHDs_240114_230618 (2)BrianОценок пока нет
- Pda TofДокумент56 страницPda TofPritam PanigrahiОценок пока нет
- Cor Pulmonale (Pneumoconiosis)Документ23 страницыCor Pulmonale (Pneumoconiosis)Sai charithaОценок пока нет
- Gerry B. Acosta, MD, FPPS, FPCC: Pediatric CardiologistДокумент51 страницаGerry B. Acosta, MD, FPPS, FPCC: Pediatric CardiologistChristian Clyde N. ApigoОценок пока нет
- Cyanotic Congenital Heart DiseasesДокумент9 страницCyanotic Congenital Heart DiseasesGubara Mohamed ZainОценок пока нет
- Interventions For Critically Ill Patients With Respiratory Problems LectureДокумент118 страницInterventions For Critically Ill Patients With Respiratory Problems LecturedeebertoОценок пока нет
- Ductus Arteriosus Dependent Congenital Heart Disease: Amjad Kouatli MD. FAAP. FACCДокумент28 страницDuctus Arteriosus Dependent Congenital Heart Disease: Amjad Kouatli MD. FAAP. FACCKartik KumarasamyОценок пока нет
- Final Anesthesia Reviw Flash CardsДокумент217 страницFinal Anesthesia Reviw Flash Cardsaljuhanita100% (1)
- Atrial Septial DefectДокумент22 страницыAtrial Septial DefectJulie MckinneyОценок пока нет
- KP 2.5.5.3 Cor PulmonaleДокумент17 страницKP 2.5.5.3 Cor Pulmonalenurul ramadhiniОценок пока нет
- Quiz Blessings #5Документ3 страницыQuiz Blessings #5Rachel LiuОценок пока нет
- Cardiopulmonary Dynamics:The Role of Oxygen in HemodialysisДокумент46 страницCardiopulmonary Dynamics:The Role of Oxygen in Hemodialysiskamel6Оценок пока нет
- Respiratory Case StudiesДокумент6 страницRespiratory Case Studiesadom09Оценок пока нет
- Tetralogy of Fallot with Multiple Caries and Patent Ductus ArteriosusДокумент44 страницыTetralogy of Fallot with Multiple Caries and Patent Ductus ArteriosusBella MartadipuraОценок пока нет
- Tetralogy of Fallot-16 Sept 2014Документ21 страницаTetralogy of Fallot-16 Sept 2014aYie_30Оценок пока нет
- Tetralogy of FallotДокумент18 страницTetralogy of FallotAaronMaroonFive100% (1)
- Congenital Heart Diseases ExplainedДокумент27 страницCongenital Heart Diseases ExplainedShreyas KotadiyaОценок пока нет
- Pediatric ObjectivesДокумент18 страницPediatric Objectivesasheehan17Оценок пока нет
- BronchiectasisДокумент6 страницBronchiectasisdrpaviОценок пока нет
- Cyanotic Congenital Heart DiseaseДокумент22 страницыCyanotic Congenital Heart DiseaseRaviОценок пока нет
- Cyanotic Congenital Heart DiseaseДокумент50 страницCyanotic Congenital Heart DiseaseSasi KumarОценок пока нет
- Cyanotic Congenital Heart DiseaseДокумент20 страницCyanotic Congenital Heart DiseaseCabdi IshakОценок пока нет
- Cyanotic Congenital Heart DiseaseДокумент20 страницCyanotic Congenital Heart DiseaseCabdi IshakОценок пока нет
- 7) Acute Pulmonary EmbolismДокумент2 страницы7) Acute Pulmonary EmbolismAris PaparisОценок пока нет
- Dr. Shaker's Guide to Managing Cyanotic Heart DiseaseДокумент66 страницDr. Shaker's Guide to Managing Cyanotic Heart DiseasePrasanth SankarОценок пока нет
- Cardiopatias CianoticasДокумент9 страницCardiopatias CianoticasAngie CalderónОценок пока нет
- Cyanotic CHDДокумент64 страницыCyanotic CHDKUMARAVELОценок пока нет
- Ventilasi PerfusiДокумент44 страницыVentilasi PerfusiIdahrachman515100% (1)
- Cardiology FMДокумент25 страницCardiology FMtrushaОценок пока нет
- CCHDДокумент69 страницCCHDchebetnaomi945Оценок пока нет
- Pulmonary Atresia With Ventricular Septal DefectДокумент23 страницыPulmonary Atresia With Ventricular Septal Defectluulamthangtai0105Оценок пока нет
- Peds Exam 3Документ25 страницPeds Exam 3Yu Yu ChenОценок пока нет
- Manage Acute Pulmonary Oedema in 38 CharactersДокумент4 страницыManage Acute Pulmonary Oedema in 38 CharactersTze SiangОценок пока нет
- PJ KritikalДокумент38 страницPJ KritikalnafisyarifahОценок пока нет
- Pulmonary Embolism Guide: Causes, Symptoms & DiagnosisДокумент60 страницPulmonary Embolism Guide: Causes, Symptoms & DiagnosisRafika RaraОценок пока нет
- 1.conginital Cardiac DefectsДокумент39 страниц1.conginital Cardiac DefectsJõsëph Jåy MîthОценок пока нет
- Medicine in Brief: Name the Disease in Haiku, Tanka and ArtОт EverandMedicine in Brief: Name the Disease in Haiku, Tanka and ArtРейтинг: 5 из 5 звезд5/5 (1)
- 10 1542@pir 12-11-333Документ13 страниц10 1542@pir 12-11-333mob3Оценок пока нет
- SSD Buying GuideДокумент16 страницSSD Buying Guidemob3Оценок пока нет
- BrestДокумент79 страницBrestseidkeОценок пока нет
- Caribbean Asthma Guidelines - Revised March 2011Документ77 страницCaribbean Asthma Guidelines - Revised March 2011mob3Оценок пока нет
- Thyroid GlandДокумент110 страницThyroid Glandmob3Оценок пока нет
- Small Victories, New Challenges Two Decades of Maternal Mortality Surveillance in JamaicaДокумент15 страницSmall Victories, New Challenges Two Decades of Maternal Mortality Surveillance in Jamaicamob3Оценок пока нет
- History of The Suture Personal Suture Preference Suture CharacteristicsДокумент33 страницыHistory of The Suture Personal Suture Preference Suture Characteristicsmob3Оценок пока нет
- Review Diseases of The Thyroid GlandДокумент21 страницаReview Diseases of The Thyroid Glandmob3Оценок пока нет
- Management of Sickle Cell Disease in PregnancyДокумент20 страницManagement of Sickle Cell Disease in Pregnancymob3Оценок пока нет
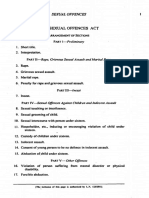
- Sexual Offences Act PDFДокумент34 страницыSexual Offences Act PDFmob3Оценок пока нет
- Pediatrics-in-Review 1989 - Acute Diarrhea in Children PDFДокумент10 страницPediatrics-in-Review 1989 - Acute Diarrhea in Children PDFmob3Оценок пока нет
- Impetigo: Staphylococcus Au-ReusДокумент7 страницImpetigo: Staphylococcus Au-Reusmob3Оценок пока нет
- 7Документ6 страниц7Yoser ThamtonoОценок пока нет
- Aiims Pge 2004Документ24 страницыAiims Pge 2004mob3Оценок пока нет
- Acute Stridor in ChildrenДокумент6 страницAcute Stridor in Childrenmob3Оценок пока нет
- RCOG Guidelines - Gestational Trophoblastic DiseaseДокумент12 страницRCOG Guidelines - Gestational Trophoblastic Diseasemob3100% (1)
- Approach To Cardiac MurmursДокумент11 страницApproach To Cardiac Murmurstouthang0074085Оценок пока нет
- 14 ReportNationalHighBloodPressureДокумент22 страницы14 ReportNationalHighBloodPressurebetzaОценок пока нет
- Case Study - Seizures and HypoglycemiaДокумент2 страницыCase Study - Seizures and Hypoglycemiamob3Оценок пока нет
- Inhaled Diuretic Frusemide's Role in Treating AsthmaДокумент2 страницыInhaled Diuretic Frusemide's Role in Treating Asthmamob3Оценок пока нет
- Standards of Medical Care in Diabetes 2015Документ99 страницStandards of Medical Care in Diabetes 2015Juan Carlos Sánchez Suárez100% (1)
- AsthmaДокумент73 страницыAsthmamob3Оценок пока нет
- Post-Exposure Prophylaxis For HivДокумент12 страницPost-Exposure Prophylaxis For Hivmob3Оценок пока нет
- Quincke's Pulse PDFДокумент1 страницаQuincke's Pulse PDFmob3Оценок пока нет
- Evaluation of Hospital Inpatient ComplicationsДокумент12 страницEvaluation of Hospital Inpatient Complicationsmob3Оценок пока нет
- HIV Prophylaxis Following Occupational ExposureДокумент39 страницHIV Prophylaxis Following Occupational Exposuremob3Оценок пока нет
- Creeping Fat in Crohn's DiseaseДокумент1 страницаCreeping Fat in Crohn's Diseasemob3Оценок пока нет
- Guideline ADA 2010 in Hyperglicemia CrisisДокумент9 страницGuideline ADA 2010 in Hyperglicemia CrisisAissyiyah Nur An NisaОценок пока нет
- Diagnosis, Evaluation, and Treatment of Hyponatremia - Expert Panel RecommendationsДокумент42 страницыDiagnosis, Evaluation, and Treatment of Hyponatremia - Expert Panel Recommendationsmob3Оценок пока нет
- Ocular Manifestations of Systemic Lupus Erythematosus A Review of The LiteratureДокумент10 страницOcular Manifestations of Systemic Lupus Erythematosus A Review of The Literaturemob3Оценок пока нет
- The Teachings of DiogenesДокумент14 страницThe Teachings of Diogenesryanash777100% (1)
- Subject: Telugu Tejam FactsДокумент5 страницSubject: Telugu Tejam FactsAum RaoОценок пока нет
- Honey Bee Complaint As Community Policing For Scouting Against PCA Act, 1960: Restoring 5 FreedomsДокумент31 страницаHoney Bee Complaint As Community Policing For Scouting Against PCA Act, 1960: Restoring 5 FreedomsNaresh KadyanОценок пока нет
- Conjunctivitis - PinkeyeДокумент3 страницыConjunctivitis - PinkeyeJenna HenryОценок пока нет
- 2013 Skin and Wound Infections - StudentДокумент35 страниц2013 Skin and Wound Infections - Studentmicroperadeniya0% (1)
- 7 Principles of Leave No TraceДокумент2 страницы7 Principles of Leave No TraceDiether100% (1)
- Tissue Eng ToolsДокумент20 страницTissue Eng ToolsVijay RajОценок пока нет
- Module 3 Developmental Stages in Middle and Late AdolescenceДокумент21 страницаModule 3 Developmental Stages in Middle and Late Adolescencejulietpamintuan100% (5)
- Anatomy of the Lymph and Immune SystemsДокумент5 страницAnatomy of the Lymph and Immune SystemsHebsiba PonnayyanОценок пока нет
- Solved CAT 2000 Paper With Solutions PDFДокумент80 страницSolved CAT 2000 Paper With Solutions PDFAravind ShekharОценок пока нет
- Paed HistДокумент123 страницыPaed HistG VenkateshОценок пока нет
- 2nd QRTR Anet ReteachДокумент13 страниц2nd QRTR Anet Reteachapi-310709379Оценок пока нет
- Darwin Comes To TownДокумент7 страницDarwin Comes To TownTadeoОценок пока нет
- The Five-Minute Daily Energy RoutineДокумент4 страницыThe Five-Minute Daily Energy RoutineSatinder Bhalla100% (1)
- Cs Study GuideДокумент380 страницCs Study Guide6436407fm100% (2)
- Lower Genital Tract InfectionДокумент51 страницаLower Genital Tract InfectionSarisa SupawimonОценок пока нет
- 5090 s14 QP 11 PDFДокумент16 страниц5090 s14 QP 11 PDFruesОценок пока нет
- Eucoelomates Lab ReportДокумент13 страницEucoelomates Lab Reportsatvindar singhОценок пока нет
- Creative ParkДокумент14 страницCreative ParkAli SimsekОценок пока нет
- Reading Dragons and Dinos PDFДокумент27 страницReading Dragons and Dinos PDFBobTomsОценок пока нет
- Horse Picture BooksДокумент3 страницыHorse Picture BooksCallibraryОценок пока нет
- Vence Ferrell - The Vaccination CrisisДокумент177 страницVence Ferrell - The Vaccination CrisisIna Hasim100% (1)
- Hidronefrosis Fetal: Urología PediátricaДокумент17 страницHidronefrosis Fetal: Urología PediátricaZule YepezОценок пока нет
- 100 Gross Anatomy ConceptionsДокумент228 страниц100 Gross Anatomy Conceptionscrsoriano2011Оценок пока нет
- Pet Agreement and Indemnification RotaДокумент1 страницаPet Agreement and Indemnification RotaLuis Bernal NevaОценок пока нет
- Types of ClaimsДокумент14 страницTypes of ClaimsCatherine Joy ManaloОценок пока нет
- Hep AДокумент2 страницыHep Aapi-237098034Оценок пока нет
- Cat Breeds & Types GuideДокумент13 страницCat Breeds & Types Guideprabhakar_n1Оценок пока нет
- Colonic LesionsДокумент89 страницColonic Lesionsjagadeesan_ushaОценок пока нет
- Animal Aloksan PDFДокумент14 страницAnimal Aloksan PDFTrias Ilmi PramudikaОценок пока нет