Академический Документы
Профессиональный Документы
Культура Документы
A Method For Non-Invasive Determination
Загружено:
popeОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
A Method For Non-Invasive Determination
Загружено:
popeАвторское право:
Доступные форматы
Ph.D.
Thesis
Extended abstract
A METHOD FOR NON-INVASIVE DETERMINATION
OF THE HUMAN HEART ACTIVATION SEQUENCE
Stefan POPESCU
Politehnica University of Bucharest, ROMANIA
Ph.D. Thesis - Extended abstract. Translation from Romanian. The original paper was
published on March 1994 by the Politehnica University Bucharest Press.
1. Introduction
From the cardiologist point of view the classical 12-lead ECG is a simple, low cost
diagnostic tool. However the limited numbers of sampling points (9 active electrodes
spread over the entire body) and the way to display this information (time varying
signals) make the analysis process extreme complicated. The information content is low
comparing to the complexity of the 3-dimensional heart electrical phenomena. The
transfer from the spatial, time-varying heart potential field into a limited set of 12 signals
hides a lot of useful information. Long time training of the cardiologist for easy
recognition of typical waveform distortions, huge data bases for various heart diseases,
and sophisticated automatic analysis and diagnostic algorithms, make this tool
valuable. A further step forward, in order to acquire more primary information, is the
Body Surface Potential Mapping - BSPM technique. These systems use 32-90
electrodes to sample the thorax surface and build potential maps at relevant moments
within the cardiac cycle. The clinical use of these maps depends on the physician ability
to interpret them. Although a greater information content compared to classical ECG,
the BSP maps are yet hard to understand. The propagation process from the heart
surface to the thorax surface, makes the two potential fields total different, and the lack
of clinical expertise needed to interpret the BSPM leads to limited extend of its clinical
use. Other BSPM displaying methods as QRS area maps, ST segment maps, activation
time maps have limited application in diagnostic of the myocardial infraction, ectopic
beats, WPW syndrome or intra-vetricular blocks. A difficult point with both classical ECG
and BSPM is the mental effort needed to associate the heart electrical events with the
recorded patterns on the thorax. Under these circumstances a simpler way to see
directly whats happen on the heart surface is a more attractive concept.
The activation front concept
One of the most popular model for the electrical heart activity is the activation front [3].
The myocard cells are activated one by other or by the specialised nervous tissues of
the heart, change the electrical state and became negative (depolarisation process).
That part of the heart muscle that is already activated is negative related to the not yet
activated part. A potential step of 40 mV appears over this 0.5 mm wide separation
zone. This potential step travels across the myocard as more of the heart became
activated. The myocard depolarisation process begins at the upper side of the right
atrium in the vicinity of the sino-atrial node (SNA) and travels down and left thought the
right and left atrium. After a short delay, the activation front breaks out again near the
apex and then travels upwards toward the hearts base (see Fig.1). Maps with the time
evolution of this activation front where invasively recorded using epicardial electrodes
into opened thorax by Scher (1956), Durrer (1970) and Spach (1975). The ability to
1
Ph.D. Thesis
Extended abstract
SAN
PR
AVN
HISS
track the activation front over the
entire cardiac cycle helds a lot of
information about the electrical
state of both the myocard and the
nervous system of the heart.
These are comprehensive and
useful information in order to
elaborate
the
diagnostic.
Therefore a tool able to record in
real-time the epicardial potential
and to play it back as potential
maps or time evolution maps of
the
activation
front
is
a
comfortable, easy to understand
and interpret diagnostic mean.
All heart pathologies that produce
findings in the ECG recording are
associated with a particular
distorsion of the normal activation
front. However the projection of
this
distorsion
toward
the
Figure 1 The human heart activation sequence
unidimensional ECG signals is a
very complex process and makes
the backwards path (effect to cause) hard to track. Therefor we expect that the
representation of the activation front evolution will offer a better understanding of the
original tri-dimensional heart activation process. It will be a major step forward in
offering to the clinician a closer view of the electrical activity of the heart without being
necessary to open the patient thorax.
2. The inverse problem in cardiology - IPC
The aim to solve for the cardiac sources knowing the thorax potential is the so called
Inverse Problem in Cardiology - IPC. As opposed to the direct problem, the inverse
problem has not necessary a unique solution unless some initial knowledge about
distribution, orientation or number of the cardiac sources is available [1,3]. This imposes
limits to the degree of freedom for the inverse solution in order to keep the inversion
stable. As long as the 3-dimensional electric heart phenomenon is observed from a 2dimensional thorax surface, neither model can completely describe the cardiac sources.
A better approach is to limit the inverse solution to the determination of the epicardial
potential. The transfer relationship between the potential on the thorax surfaces and
heart surfaces is reciprocal and the inverse solution, according to the Helmhotz
theorem, is always possible and unique [3]. Using this information the evolution of the
heart activation front can be easily computed. There are many possibilities to solve for
the heart surface potential when knowing the thorax potential: the finite difference
method (FDM), the finite elements method (FEM), the boundary elements method
(BEM). In this work we preferred the BEM due to the efficient precision-speed
performance factor.
Ph.D. Thesis
Extended abstract
Still an electrical model for the medium between the heart and body surface is needed.
We used a simplified thorax model in order to keep the calculation's complexity low. The
internal structure between thorax surface and
heart surface is built from a finite number of
entities, bounded by closed surface and having
an electrical conductivity approximately
constant in their volume. With a certain degree
of accuracy, these entities can be associated
with various anatomic parts of the thorax
(bones, lungs, liver, spinal cord, kidney...).
Useful prior information about the geometry
(electrode position, thorax shape and organ
size and position) could be measured using an
imaging method like CT, MRI or ultrasound
tomography. A better division of the thorax and
Figure 2 Electrical model of the a greater number of homogeneous volumes,
thorax. The actual electrodes give a better precision for the inverse solution.
position depends upon the patient The glue medium that fills the space between
the homogeneous volumes is the thorax volume
thorax topology.
VT with the mean conductivity T and bounded
outside the thorax by the surface ST and inside by the heart surface SH and the surface
of the homogeneous entities Si (i=1..M). Therefore VT does not includes the heart
volume VH neither the volumes Vi. The 2nd Green equation applied to this volume
gives:
VT ( )dV
S T ( n T n T )dST S H ( n T n T )dS H
M
i 1
(1)
S i ( n T n T )dSi
where ( r ) is the electric potential and ( r ) the tridimensional Green function ( r, ro )
= ( 4 | r - ro | )-1, with ro a mobile point outside the thorax. Inside VT there are no
sources for the potential (=0) and =0 because ro VT. Also the current that
leaves the thorax normal to its surface is null : on ST.
Inside the homogeneous entities Vi there are no sources for the potential and then the
2nd Green equation applied to the Vi volumes gives:
S i ( n i n i )dSi 0
(2)
Replacing (2) in (1) and considering the continuity of the potential and its normal
derivate at entity surface, results the final potential equation:
Ph.D. Thesis
Extended abstract
ST n T dS T SH n T n T dS H
M
1
dS i 0
T Si n T
i 1
(3)
Equation (3) can be transformed from continue to discrete by digitising the surfaces. We
choose a number of N discrete nodes for every surface of interest (thorax, heart and
entities. By using a numeric integration method, the integrals are now finite sums over N
points of the numerical values in nodes, and (3) is now:
N
( rTj )
j1
n T
Tj
N
( r Hj )
Hj
Hj
( r Hj )
n
n
T
T
j1
N
( rij )
0
k i (Sij)
T
i 1
j1
M
(4)
with ki = 1-i/T the conductivity step at the Vi interfaces. We can use this equation in
order to find the unknown electric potential on the heart surface. Additionally we have
as supplementary unknowns the potential on the entity's surface and its normal
derivative on the heart surface up to a total number of N(M+2) unknowns. In order to
solve for these unknowns, we have to write N(M+2) equations for N(M+2) different ro
positions. A simple approach is to let ro to travel through the N(M+2) digitising nodes.
However these nodes are on the boundary, not outside VT. The Boundary Elements
Method chose the position of ro inside the VT volume in points very close to the nodes.
However we found the mathematical and numerical problems associated with the huge
Green function values in points ro near the integral surface difficult to handle. Therefore
we chose these positions outside VT uniformly spread over a cylinder, 1m height, 1m
diameter, centred around the thorax in order to avoid the singularity of the Green
function and its derivative in the nodes. Equation (4) builds a linear system of N(M+2)
algebraic equations with N(M+2) unknowns, which allow us to solve for the potential and
normal current on the heart surface.
3. The electrical impedance tomography - EIT
The coefficients in equation (4) depend upon the thorax geometry and electrical thorax
parameters expressed by the constants ki. A way to specify the values for ki is to use
typical values measured in vitro by different authors [1,2]. However the technique of
Electrical Impedance Imaging allows a better approach, namely to measure these
parameters in vivo, using the same electrodes that measure the thorax potential and a
suitable auxiliary hardware and software. An EIT instrument as described in [5] uses a
number of electrodes uniformly spread over the thorax and a number of programmable
current generators that source or sink alternate current into -from thorax. Different
current patterns produce different voltage patterns on the thorax surface. Processing
this information allow the non-invasive measurement of electrical parameters of the
thorax. The exploring current is around 100A and the frequency around 100kHz in
order to separate the heart potential from the measurement voltage and to avoid nerve
4
Ph.D. Thesis
Extended abstract
or muscle somestesic stimulation. For the reconstruction process most of the authors
use the Finite Element Method [5,6] in order to avoid the fact that the internal geometry
of the thorax is initially unknown. Therefore the number of initial unknowns is bigger as
the number of finite elements used to describe the thorax is greater. The reconstruction
process is very difficult especially for the 3-dimensional case [5,6]. To simplify the
complexity of the calculus we used the Boundary Elements Methods and an identical
thorax model with the one used for the inverse problem in cardiology. In this case we
have to find only the conductivity of the homogeneous entities that build-up the thorax.
In order to apply the reconstruction algorithm one needs to know the transfer
relationship which gives the resulted thorax voltages produced by the injected currents.
In the frequency range used for exploration, tissues are mainly resistive and the
electromagnetic field produced inside the thorax is stationary harmonic. We wrote the
Green equation using effective values for currents and voltages. Similar with (4) the
following conditions holds true: inside the thorax there are no sources for the voltage
(=0) and =0 because ro VT and the current normal to thorax surface is null
everywhere except electrode's surface. We agree also that the electrodes are small
compared to ro and hence is constant over one electrodes surface. Equation (3) will
have the new form:
N
S T n T dST I j ( rej )
j 1
M 1
1 i
dS i 0
T S i n T
i 1
(5)
where Ij is the current, rej is the position vector of the jth electrode and SM+1 SH.
The discrete version when considering a number of N nodes for each surface will be:
N
( rTj )
j 1
n T
Tj
M 1
I j ( rej )
j 1
( rij )
0
k i Sij
T
i 1 j 1
N
(6)
Equation (6) allows us to build a consistent system of equations for the total number of
U = N(N-1)/2 independent current patterns and resulted voltages. Hence U is the
maximum number of unknown conductivity values possible to find when using N
exploring electrodes. Similar to the IPC we have to deal with N(M+1) additionally
unknowns for each test pattern, associated with the resulted potentials in the
homogeneous entities' nodes. We handle this problem by sweeping ro position over the
above mentioned cylinder.
5. Implementation and results
In order to verify the procedure described above, we built a special hardware system
and we wrote suitable software.
Ph.D. Thesis
Extended abstract
Description of the hardware
As depicted in Fig.3 the hardware system consists of 32 floating ECG amplifiers,
multiplexed through 4 differential isolation amplifiers to a specially developed data
acquisition system [7]. A separate amplifier provides the signal for the Wilson central
reference.
8 channels
amplifier
8 channels
amplifier
8 channels
amplifier
8 channels
amplifier
Reference
amplifier
Multiplexed
isolation amplifier
Multiplexed
isolation amplifier
Data aqusition board.
12 bit multiplexed
A/D converter.
IBM PC compatible
computer.
Multiplexed
isolation amplifier
Multiplexed
isolation amplifier
Figure 3 The body surface potential measurement system
All channel amplifiers have the same structure as depicted in Fig.4. The amplifiers' band
is 0.05Hz...250Hz and the overall gain is programmable in steps of x1...x16 V/mV under
computer control. The amplifier inputs are protected against damage caused by
defibrillator discharges. An automatic zero circuit reduces the time required for the
amplifiers capacitors to reach the steady operation conditions.
+0,6V
2x
Dp
E
R1
C1
C2
A1
A2
R2
R4
-0,6V
D1
D2
R3
R5
2x
DZ
C3
Figure 4 The floating electrode amplifier
To build the reference voltage for the isolated differential amplifiers a circuit as that
depicted in Fig.5 was used. The same circuit is used to apply a negative drive voltage to
the patient right leg to minimise the common mode noise that appears between patient
body and the floating amplifiers inputs. The circuit achieves a rejection of the common
mode voltage of at least 100dB. Additionally, the isolated differential amplifier add at
least 80dB of common mode rejection. The global figure of 180 dB is high enough for
every operating condition eliminating the interference produced by the parasitic coupling
between patient body and the 50Hz power lines.
Ph.D. Thesis
Extended abstract
R1
A1
R1
A2
C1
R
C2
Vref
A2
R2
R4
R1
A3
D1
D2
R3
R5
2x
DZ
C3
Cc
A4
Figure 5 The reference amplifier and right leg drive circuit
In order to isolate the patient and the input amplifiers from the computer ground we
used isolation amplifiers as depicted in Fig.6.
MUX
8
canale
ADG
508
Amplificator diferenial AD621
C1
Modulator
factor
de umplere
Rg
Vref
UWilson x 100
C2
Demod
factor
de umplere
Burr Brown ISO 121
Figure 6 The isolated multiplexed differential amplifier
The isolated differential amplifiers negative input is connected to the Wilson central
terminal reference [8] provided by the circuit depicted in Fig.5.
The data acquisition system was designed as a extension board for a IBM - PC
compatible computer. We used a relative fast 12 bits ADC to sample each channel
every millisecond (1kHz/channel sampling rate) [8]. The acquisition process and data
storing are controlled by an IBM PC-286 computer. The board support DMA transfer
and the firmware is interrupt driven.
Description of the reconstruction software
The acquired signals are first pre-processed by dedicated software to eliminate the
wandering of the base line. Special regression methods are used to eliminate the
7
Ph.D. Thesis
Extended abstract
wandering synchronous to the respiration movements that are due to a poor electrode
contact. The constant base line shifting is eliminated based on a statistical procedure.
The histogram of the signal discrete amplitudes is used to find the deviation from null of
the base line. A linear interpolation procedure eliminates the time aperture error
introduced by the delays between the sampling moments at each electrode appearing
due the use of a single AD converter.
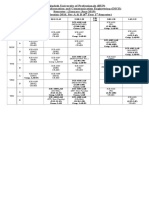
For both IPC and EIT problems we used a thorax model with 5 homogeneous entities
(lungs, liver, stomach and spinal cord) each digitised with 32 nodes.
In the first attempt we used typical values for
the electrical parameters measured in vitro"
by Kim [2]:
Tissue type
Thorax - mean
Heart muscle
Lungs
Spinal cord
Liver
Stomach
[.cm]
300
450
1200
2000
625
800
The inversion was made using an IBM PC-486
computer and a special developed Pascal
Figure 7 Boundary element model of program. The outer thorax geometry was
the thorax used for both IPC and EIT measured for each patient and the internal
geometry was generated using anatomical
problems.
maps and standard geometrical relations.
We used the Gauss quadrature method to evaluate the integrals in (4-7) and the 7 point
integration method over an elementary triangle as suggested by Albrecht and Collatz
[3]. The discrete version of the equation 4, will be in this case:
M
T T ( r0 ) H H ( r0 ) H H ( r0 ) I I ( r0 ) 0
(7)
I 1
We used this equation as descried above to build a linear system of equation that we
solved to find the unknowns associated with the potential on the heart surface. Because
of the ill-posed nature of the problem we had to use a Tikhonov first order regularisation
procedure to keep the inverse solution stable.
Figures 5 and 6 show the evolution of the signals measured on the thorax of a healthy
29-year old male subject and the reconstructed signals on the heart surface.
Additionally the analysis software has the possibility to display an animated image that
reproduces at reduced speed the evolution of potential on heart surface by coding the
potential values as different grey levels or different colours.
Ph.D. Thesis
Extended abstract
Figure 8 The ECG signals recorded on the torso surface (Wilson Central
Reference) for a young healthy patient
Figure 9 The signals reconstructed on the patients heart surface.
A very useful representation is the map of iso-potential lines. These are the lines
connecting points on the heart surface having the same potential at a certain moment
(see Fig.7). The position of the activation front can be defined either as the line of 0 mV
or as the line connecting the points on the heart surface having the maximum negative
local gradient. The second has the advantage of being reference independent (4).
Ph.D. Thesis
Extended abstract
4
0.189
0.811
0.433
1.056
1.678
1.678
0.433
0.433
1.056
1.433
2.056
0.811
2.678
0.189
2.056
1.433
1
Figure 10 The isopotential map of the heart surface at
20 ms after QRS onset for a healthy patient
The resulted evolution of the activation front was compared to the apriori available
physiological knowledge and showed a good match. A total of 15 different patients
suffering form major heart damages (Myocardial Infarction with Different Location, Early
Activation, Wolf-Parkinson-White Syndrome, Ectopic Beats, Supra-Ventricular
Activation, Right / Left Bundle Branch Block ) where investigated with the above
described system to acquire the minimum clinical skill required to efficiently operate the
system and for further enhancing of both hardware and software [8]. Presently we work
on a modified hardware which allow both ECG measurements and EIT reconstruction
using the same electrodes allowing to build a better thorax model for each patient in
useful time.
5. Claims for original contributions
proof of the Helmholtz theorem for equivalent sources in 2 cases: unipolar current
layer and bipolar current layer
proof of the reciprocal relationship between thorax surface potential distribution and
heart surface potential distribution in the case of a non-homogenous thorax volume
situated into a bounded region
the original method of injected currents used to proof the reciprocal relationship
between thorax potential and heart surface potential
deducing of the discrete transfer matrix between the potential measured on the
thorax and the potential inside the thorax.
the combination of IPC and EIT problems using the same discrete model of the
thorax used to build the inversion matrix from a single patient examination
method to reconstruct the internal thorax impedance parameters from current
measurements and using the boundary element method
simplified impedance image reconstruction algorithm based on the NewtonKantorovich method and on the inversion of non-rectangular tall matrix (notion
introduced by the author)
method and instrument to non-invasive determination of the activation sequence of
the human heart based on the activation front concept
hardware system used to measure the thorax potential evolution
software to pre-process the measured signals
10
Ph.D. Thesis
Extended abstract
software to describe and model the real patient thorax based on geometrical
measurements
software to display the acquired and reconstructed signals, the potential maps, the
animated evolution of potential field and the 3-dimensional activation maps
Selected References
[1] H.Geertjan and Adriaan van Oosterom, The depolarisation sequence of the human heart
surface computed from measured body potentials, IEEE TBME, pp. 1047-1058, Dec 1988.
[2] W.K.Kim., W.Desk, L.E.Bakar and J.Pearce, Origins of the impedance change in impedance
cardiography by a tree-dimensional finite element model, IEEE TBME, pp. 993-1000, Dec
1988.
[3] Adrianus Antonius Hubertus Damen, On the observability of electrical cardiac sources,
Ph.D. Dissertation, Technische Hogeschool Eindhoven.
[4] M.Shenasa, M.Borggrefe and G.Breithart, Cardiac Mapping, Mount Kisco, NY: Futura, 1993.
[5] Gadd R., P.M.Record and P.Rolfe: Finite element modelling for electrical impedance
tomography - AIC of BME vol-12 pag.133-134 / 1990;
[6] Murai T. and Y.Kagawa: Electrical Impedance Computed Tomography Based On A Finite
Element Model - TBME vol BME-32, pag. 177-184 / 1985;
[7] Cristescu A., Stefan POPESCU, K.Schob, and M.Hancu, An integrated system for body
surface heartpotential distribution maps, in Timisoara medicala Tom 32/1987 Supplement,
pp.21-27;
[8] S.Pasca and Stefan POPESCU, Sistem de achizitie de date si sontrol pentru aplicatii
biomedicale - in volumul REP, Snagov 6-7 IX 1990, pag.V20-V25
11
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- HP Scanjet N9120 (Service Manual) PDFДокумент394 страницыHP Scanjet N9120 (Service Manual) PDFcamilohto80% (5)
- A First Etymological Dictionary of BasquДокумент29 страницA First Etymological Dictionary of BasquDaily MailОценок пока нет
- SemДокумент583 страницыSemMaria SantosОценок пока нет
- National Pension System (NPS) - Subscriber Registration FormДокумент3 страницыNational Pension System (NPS) - Subscriber Registration FormPratikJagtapОценок пока нет
- Angle ModulationДокумент26 страницAngle ModulationAtish RanjanОценок пока нет
- Optimizing Stata For Analysis of Large Data SetsДокумент29 страницOptimizing Stata For Analysis of Large Data SetsTrần Anh TùngОценок пока нет
- Void Engineers (Convention: Mage The Ascension)Документ6 страницVoid Engineers (Convention: Mage The Ascension)Beth0% (1)
- Slide 7 PV NewДокумент74 страницыSlide 7 PV NewPriyanshu AgrawalОценок пока нет
- 1.2 The Basic Features of Employee's Welfare Measures Are As FollowsДокумент51 страница1.2 The Basic Features of Employee's Welfare Measures Are As FollowsUddipta Bharali100% (1)
- Gates Crimp Data and Dies Manual BandasДокумент138 страницGates Crimp Data and Dies Manual BandasTOQUES00Оценок пока нет
- T54125AДокумент64 страницыT54125ARaúl FroddenОценок пока нет
- Tecsun Pl310et PDFДокумент30 страницTecsun Pl310et PDFAxel BodemannОценок пока нет
- تأثير العناصر الثقافية والبراغماتية الأسلوبية في ترجمة سورة الناس من القرآن الكريم إلى اللغة الإ PDFДокумент36 страницتأثير العناصر الثقافية والبراغماتية الأسلوبية في ترجمة سورة الناس من القرآن الكريم إلى اللغة الإ PDFSofiane DouifiОценок пока нет
- Green ThumbДокумент2 страницыGreen ThumbScarlet Sofia Colmenares VargasОценок пока нет
- Visual Metaphor Process BookДокумент18 страницVisual Metaphor Process Bookmatt8859Оценок пока нет
- Class Routine Final 13.12.18Документ7 страницClass Routine Final 13.12.18RakibОценок пока нет
- LQZLQM ) So"L/L6H Klans LN : Sfof (No K - Of) HGSF) Nflu DFQДокумент5 страницLQZLQM ) So"L/L6H Klans LN : Sfof (No K - Of) HGSF) Nflu DFQSAJAL KOIRALAОценок пока нет
- Formulae HandbookДокумент60 страницFormulae Handbookmgvpalma100% (1)
- TOEFL-Reading Question Type Definitions and ExplanationДокумент5 страницTOEFL-Reading Question Type Definitions and ExplanationSamara SampaioОценок пока нет
- Program of ActivitiesДокумент2 страницыProgram of ActivitiesVon Limuel LopezОценок пока нет
- Hexoloy SP Sic TdsДокумент4 страницыHexoloy SP Sic TdsAnonymous r3MoX2ZMTОценок пока нет
- International Supply Chain ManagementДокумент2 страницыInternational Supply Chain ManagementPRASANT KUMAR SAMALОценок пока нет
- Hemax-530 PDFДокумент2 страницыHemax-530 PDFNice BennyОценок пока нет
- Tekla SoakwayДокумент2 страницыTekla SoakwayBalaji Naik100% (1)
- Evidence MODULE 1 Evidence DefinitionДокумент8 страницEvidence MODULE 1 Evidence Definitiondave BarretoОценок пока нет
- InterviewДокумент8 страницInterviewswapnadip kumbharОценок пока нет
- Unit 1 - Plant & Eqpt. Safety Apprisal & Control Techq.Документ147 страницUnit 1 - Plant & Eqpt. Safety Apprisal & Control Techq.Madhan MОценок пока нет
- "Large Quote Goes Here.": Title or Heading HereДокумент2 страницы"Large Quote Goes Here.": Title or Heading HereHesti RianaОценок пока нет
- 74 Series Logic ICsДокумент6 страниц74 Series Logic ICsanon-466841Оценок пока нет
- 2018-2019 Annual Algebra Course 1 Contest: InstructionsДокумент2 страницы2018-2019 Annual Algebra Course 1 Contest: InstructionsNaresh100% (1)