Академический Документы
Профессиональный Документы
Культура Документы
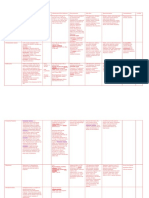
Gastrointestinal System: Antihistamine Half-Life: Onset: Peaks: Duration
Загружено:
syerly0 оценок0% нашли этот документ полезным (0 голосов)
26 просмотров3 страницыdfgh
Оригинальное название
c18 Antihistamine
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документdfgh
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
26 просмотров3 страницыGastrointestinal System: Antihistamine Half-Life: Onset: Peaks: Duration
Загружено:
syerlydfgh
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 3
1
CHAPTER 18 Gastrointestinal System
Antihistamine
Use
Provides symptomatic
relief of allergic symptoms;
sedative/antiemetic in
surgery/labor; decreases
post op nausea/vomiting;
adjunct to analgesics
in control of pain;
management of
motion sickness.
Example
Promethazine
hydrochloride
(Phenergan)
How it works
Half-life:
715 h
Route:
PO/IM/
Rectal/IV
Onset:
PO: 20 min
IM: 20 min
Rectal: 20 min
IV: 35 min
Pregnancy
category: C
Peaks:
2h
Duration:
PO/IM
Rectal/IV:
28 h
Pharmacokinetic:
Well absorbed from GI tract,
after IM administration:
Widely distributed;
metabolized in liver;
excreted in urine;
PB:6090%.
Antihistamine: Inhibits histamine at histamine receptor sites,
preventing, antagonizing most allergic effects (e.g., urticaria,
pruritus).
Antiemetic: Diminishes vestibular stimulation, depresses
labyrinthine function, acts on chemoreceptor trigger zone
(CTZ), producing antiemetic effect.
Sedative-hypnotic: Decreases stimulation to brain stem reticular
formation producing CNS depression.
Adult dose
Allergic symptoms: PO: 25 mg at bedtime of 12.5 mg
4 times/day; Rectal/IM/IV: 25 mg; may repeat in 2 hours.
Motion sickness: PO: 25 mg 3060 minutes before departure;
may repeat in 812 h, then every morning on arising and before
evening meal.
Antiemetic: PO/IM/IV/Rectal: 12.525 mg q46 h as needed.
Pre- and postop sedation; adjunct to analgesics: IM/IV: 2550 mg.
Before administration
Assess BP and pulse for bradycardia/tachycardia if patient is
given parenteral form.
If used as an antiemetic assess for dehydration (poor skin
turgor, dry mucous membranes, longitudinal furrows in tongue).
Obtain baseline blood work to include electrolyte levels.
Assess medical and drug history.
If used for pre-op sedation, have patient void before
administering medication and raise side rails to provide a
safe environment.
Pharmacology Demystified
Antihistamine
(continued)
Administration
PO: Give without regard to meals.
Scored tablets may be crushed.
IM: Note: Significant tissue necrosis may occur if given SubQ.
Inadvertent intra-arterial injection may produce severe
arteriospasm, resulting in severe circulation impairment.
Inject deep IM.
IV: May be given undiluted or dilute with 0.9% NaCl.
Final dilution should not exceed 25 mg/mL.
Administer at 25 mg/min rate through IV infusion tube.
A too rapid rate of infusion may result in transient fall in B/P,
producing orthostatic hypotension, reflex tachycardia; if patient
complains of pain at IV site, stop injection immediately
(possibility of intra-arterial needle placement/perivascular
extravasation).
Rectal: Refrigerate suppository; moisten with cold water before
inserting well into rectum.
After administration
Contraindications
Monitor vital signs.
Monitor serum electrolytes in patients with severe vomiting.
Assist with ambulation if drowsiness, lightheadedness occurs.
Maintain a safe environment.
Comatose, those receiving large doses of other CNS
depressants, acutely ill/dehydrated children, acute asthmatic
attack, vomiting of unknown etiology in children, Reyes
syndrome, those receiving MAO inhibitors.
Extreme caution: History of sleep apnea, young children,
family history of sudden infant death syndrome (SIDS), those
difficult to arouse from sleep.
Cautions: Narrow-angle glaucoma, peptic ulcer, prostatic
hypertrophy, pylorduodenal/ bladder neck obstruction, asthma,
COPD, increased intraocular pressure, cardiovascular disease,
hyperthyroidism, hypertension, seizure disorders.
CHAPTER 18 Gastrointestinal System
Antihistamine (continued)
Side effects/
adverse reaction
High incidence: drowsiness, disorientation. Hypotension,
confusion, syncope more likely in the elderly.
Frequent: Dry mouth, urinary retention, thickening of bronchial
secretions.
Occasional: Epigastric distress, flushing, visual disturbances,
hearing disturbances, wheezing, paresthesia, sweating, chills.
Rare: Dizziness, urticaria, photosensitivity, nightmares.
Fixed-combination form with pseudoephedrine may produce
mild CNS stimulation.
Adverse/toxic:
Paradoxical reaction (particularly in children) manifested as
excitation, nervousness, tremors, hyperactive reflexes,
convulsions. CNS depression has occurred in infants and
young children (respiratory depression, sleep apnea, SIDS).
Long-term therapy may produce extrapyramidal symptoms
noted as dystonia (abnormal movements), pronounced motor
restlessness (most frequently occurs in children), and
Parkinsonian symptoms (esp. noted in elderly). Blood
dyscrasias, particularly agranulocytosis, have occurred.
Patient education
Drowsiness and dry mouth may be an expected response to
drug. Sugarless gum, sips of tepid water may relieve dry
mouth. Coffee/tea may help reduce drowsiness.
Report visual disturbances.
Avoid tasks that require alertness and motor skills until
response to drug is established.
Avoid alcohol and other CNS depressants.
Вам также может понравиться
- Drug StudyДокумент7 страницDrug StudyJoy Jarin100% (1)
- Atropine SulfateДокумент5 страницAtropine Sulfateapi-3797941100% (1)
- Atropine Sulfate (Drug Study)Документ3 страницыAtropine Sulfate (Drug Study)Franz.thenurse6888100% (1)
- Therapeutic: Urinary Tract Stimulants Pharmacologic: CholinergicДокумент37 страницTherapeutic: Urinary Tract Stimulants Pharmacologic: CholinergicApple MaeОценок пока нет
- NCP DrugДокумент13 страницNCP DrugMhar CamposanoОценок пока нет
- PhenobarbitalДокумент5 страницPhenobarbitalapi-3797941100% (1)
- Drug Study ShenДокумент12 страницDrug Study ShenLass KazeОценок пока нет
- 5 MG Iv BidДокумент17 страниц5 MG Iv BidhanzreinherОценок пока нет
- Drug StudyДокумент9 страницDrug StudyShiara Ruth EdrosoloОценок пока нет
- Gastrointestinal System: Anticholinergic Half-Life: Onset: Peaks: DurationДокумент2 страницыGastrointestinal System: Anticholinergic Half-Life: Onset: Peaks: DurationsyerlyОценок пока нет
- Drug Study Gentamicin Sulfate and SalbutamolДокумент7 страницDrug Study Gentamicin Sulfate and SalbutamolEduardОценок пока нет
- DrugsДокумент5 страницDrugsnurse_nurseОценок пока нет
- Drug Study 2Документ8 страницDrug Study 2rey_tengОценок пока нет
- High Alert MedicationsДокумент17 страницHigh Alert MedicationsJoanna Marie Datahan EstomoОценок пока нет
- c18 Serotonin AntagonistДокумент2 страницыc18 Serotonin AntagonistsyerlyОценок пока нет
- Drug StudyДокумент8 страницDrug Studykarenkaren09Оценок пока нет
- Drugs ErДокумент7 страницDrugs EreyesidphОценок пока нет
- Ciprofloxacin CiproДокумент1 страницаCiprofloxacin CiproKristi WrayОценок пока нет
- Morphine SulfateДокумент3 страницыMorphine SulfateConn_Casipe_8158100% (3)
- Nursing Considerations Assessment: History: Infections Kidney Disease Liver Disease, Hypothyroidism UlcerativeДокумент5 страницNursing Considerations Assessment: History: Infections Kidney Disease Liver Disease, Hypothyroidism UlcerativeSophia limОценок пока нет
- Drugs For EmergencyДокумент25 страницDrugs For EmergencyJunathan L. DelgadoОценок пока нет
- Drug Study For FractureДокумент4 страницыDrug Study For FractureitsmeayaОценок пока нет
- 1430 Drug CardsfinalДокумент7 страниц1430 Drug CardsfinalLizSherman100% (1)
- AntitussiveДокумент7 страницAntitussiveCucumber WarriorОценок пока нет
- Case Pres PREECLAMPSIA Drugs NCPДокумент12 страницCase Pres PREECLAMPSIA Drugs NCPDanica May Galvez100% (1)
- Drug Study No.1 Brand Name: Paracetamol Generic Name: Tempra Classification: Anti-Infectives Dosage: 100mg, 1ml Drops q4hrДокумент7 страницDrug Study No.1 Brand Name: Paracetamol Generic Name: Tempra Classification: Anti-Infectives Dosage: 100mg, 1ml Drops q4hrMary EnsomoОценок пока нет
- EMERGENCY DRUGS: A Drug StudyДокумент33 страницыEMERGENCY DRUGS: A Drug StudyNicole GarciaОценок пока нет
- Morphine SulfateДокумент5 страницMorphine Sulfateapi-3797941100% (4)
- 508 Medication PreAssignmentДокумент9 страниц508 Medication PreAssignmentMikeОценок пока нет
- Preoperative PremedicationsДокумент90 страницPreoperative PremedicationsMorad SatariОценок пока нет
- Classification: 1. Natural AlkaloidsДокумент14 страницClassification: 1. Natural AlkaloidsManikanta GupthaОценок пока нет
- FentanylДокумент4 страницыFentanylapi-3797941Оценок пока нет
- EMERGENCY DRUGS: A Drug StudyДокумент8 страницEMERGENCY DRUGS: A Drug StudyShaine WolfeОценок пока нет
- Drug Study On Emergency DrugsДокумент14 страницDrug Study On Emergency DrugsRene John FranciscoОценок пока нет
- Drug StudyДокумент9 страницDrug StudyVicenia BalloganОценок пока нет
- Drug Study ProjectДокумент7 страницDrug Study ProjectMaRic Gabutin Guerra100% (1)
- Delivery Room Drug StudyДокумент9 страницDelivery Room Drug Studymacel sibayan100% (9)
- Drug StudyДокумент3 страницыDrug StudyJaylean Abrigo AguinaldoОценок пока нет
- Nclex NotesДокумент67 страницNclex Notesjanet roosevelt94% (65)
- Epinephrine Classifications: Therapeutic: Antiasthmatics, Bronchodilators, Vasopressors Pharmacologic: Adrenergics IndicationsДокумент14 страницEpinephrine Classifications: Therapeutic: Antiasthmatics, Bronchodilators, Vasopressors Pharmacologic: Adrenergics IndicationsLindy Shane BoncalesОценок пока нет
- Drug Study DRДокумент6 страницDrug Study DRBheigh Lomitao AlbueraОценок пока нет
- Nursing Care Plan: Assessment Diagnosis Planning Implementation Rationale EvaluationДокумент4 страницыNursing Care Plan: Assessment Diagnosis Planning Implementation Rationale Evaluationthomasfinley44Оценок пока нет
- Drug StudyДокумент11 страницDrug StudyKaloy KamaoОценок пока нет
- Drug Study On Emergency DrugsДокумент34 страницыDrug Study On Emergency DrugsMei-mei ZhuangОценок пока нет
- Medications Sheet PreopДокумент37 страницMedications Sheet Preopapi-503879428Оценок пока нет
- Drug 25Документ17 страницDrug 25carol_gigliotti24100% (1)
- Drug Name General Action Specific Action Indication Contraindication Adverse Effect Nursing ResДокумент9 страницDrug Name General Action Specific Action Indication Contraindication Adverse Effect Nursing ResDustin JohnОценок пока нет
- PhenytoinДокумент6 страницPhenytoinapi-3797941100% (1)
- Drugs ORДокумент17 страницDrugs ORCatherine ZamoraОценок пока нет
- Emergency Drugs: (A Drug Study)Документ13 страницEmergency Drugs: (A Drug Study)Marichu BajadoОценок пока нет
- MetoprololДокумент3 страницыMetoprololapi-3797941100% (3)
- Drug Study HydralazineДокумент10 страницDrug Study HydralazineLuige AvilaОценок пока нет
- Drug Study JrodДокумент8 страницDrug Study JrodGaez ﭢ UlpindoОценок пока нет
- Gastrointestinal System: GI Osmotic: Laxative/Antacid, Anticonvulsant, Electrolyte Half-Life: Onset: Peaks: DurationДокумент4 страницыGastrointestinal System: GI Osmotic: Laxative/Antacid, Anticonvulsant, Electrolyte Half-Life: Onset: Peaks: DurationsyerlyОценок пока нет
- Gastrointestinal System: Anticholinergic Half-Life: Onset: Peaks: DurationДокумент2 страницыGastrointestinal System: Anticholinergic Half-Life: Onset: Peaks: DurationsyerlyОценок пока нет
- Gastrointestinal System: Antidiarrheals Half-Life: Onset: Peaks: DurationДокумент2 страницыGastrointestinal System: Antidiarrheals Half-Life: Onset: Peaks: DurationsyerlyОценок пока нет
- c18 Serotonin AntagonistДокумент2 страницыc18 Serotonin AntagonistsyerlyОценок пока нет
- Diphenhydramine Drug TabulationДокумент2 страницыDiphenhydramine Drug TabulationMeriyah EdzyleОценок пока нет
- mc-2 cmptd30-12-2019 3-1 SEC-B PDFДокумент37 страницmc-2 cmptd30-12-2019 3-1 SEC-B PDFvijay100% (1)
- Slides AUTACOIDSДокумент29 страницSlides AUTACOIDSStrange eeОценок пока нет
- Top 200 Brand Name DrugsДокумент1 страницаTop 200 Brand Name DrugsLen HuaОценок пока нет
- Aerius Syrup PIДокумент9 страницAerius Syrup PITerrence LiОценок пока нет
- Histamine, Serotonin & The Ergot AlkaloidsДокумент31 страницаHistamine, Serotonin & The Ergot AlkaloidsnicewanОценок пока нет
- NCLEX Cram Sheet: 1. Lab ValuesДокумент7 страницNCLEX Cram Sheet: 1. Lab ValuesReema Akberali noorani50% (2)
- Ap 201220 1019 1Документ9 страницAp 201220 1019 1Anisa RahmaОценок пока нет
- Sedilix-Rx Linctus: What Is in This LeafletДокумент2 страницыSedilix-Rx Linctus: What Is in This LeafletWei HangОценок пока нет
- Allergic Rhinitis in ChildrenДокумент7 страницAllergic Rhinitis in ChildrenTina MorleyОценок пока нет
- LabadДокумент8 страницLabadAndriati RahayuОценок пока нет
- AutacoidsДокумент23 страницыAutacoidsdrjahangirkaboutari100% (3)
- AntihistamineДокумент2 страницыAntihistamineMichelle CasilangОценок пока нет
- HYPEREMESIS GRAVIDARUM GT 69 NotesДокумент6 страницHYPEREMESIS GRAVIDARUM GT 69 NotesFara WakeshimaОценок пока нет
- DiphenhydramineДокумент6 страницDiphenhydramineAndrea BroccoliОценок пока нет
- Mehu525 U4 T3 INTOXICACIONES2-4Документ32 страницыMehu525 U4 T3 INTOXICACIONES2-4jorgealonsosaavedraОценок пока нет
- Allergic RhinitisДокумент38 страницAllergic RhinitisDr-Firas Nayf Al-ThawabiaОценок пока нет
- Defn: Periodic Spasm of Bronchial Smooth Muscles, Increased Secretion, andДокумент5 страницDefn: Periodic Spasm of Bronchial Smooth Muscles, Increased Secretion, andSambit BeheraОценок пока нет
- 2nd Generation AntihistamineДокумент4 страницы2nd Generation AntihistamineJohn Christopher LucesОценок пока нет
- Stem Definition & Substem (If Available)Документ15 страницStem Definition & Substem (If Available)nasadsasdОценок пока нет
- Antihistamine - WikipediaДокумент39 страницAntihistamine - WikipediaMuhammadafif SholehuddinОценок пока нет
- Acute Angioedema Overview of Angioedema TreatmentДокумент5 страницAcute Angioedema Overview of Angioedema TreatmentGiorgiana pОценок пока нет
- Anti Ulcer 2Документ55 страницAnti Ulcer 2Amra ahmedОценок пока нет
- Histamine and Antihistamines LatestДокумент28 страницHistamine and Antihistamines LatestAjay KumarОценок пока нет
- Edema Auricular Inducido Por TPA Art BaseДокумент7 страницEdema Auricular Inducido Por TPA Art BaseCINTIA MARIANA MALDONADO GONZALEZОценок пока нет
- LCZ ColdДокумент5 страницLCZ ColdManmohan SinghОценок пока нет
- The Healing Power of WaterДокумент22 страницыThe Healing Power of WaterMОценок пока нет
- Antihistaminic & Antiallergic Drugs: Biosynthesis of HistamineДокумент18 страницAntihistaminic & Antiallergic Drugs: Biosynthesis of HistamineSara MohamedОценок пока нет
- Schizophrenia (10 Questions) : Psychiatric DisordersДокумент21 страницаSchizophrenia (10 Questions) : Psychiatric DisordersYaj Cruzada100% (1)
- UG Graphs-1Документ74 страницыUG Graphs-1Rakshith S AradhyaОценок пока нет