Академический Документы
Профессиональный Документы
Культура Документы
497 Full
Загружено:
Arinta Purwi SuhartiОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
497 Full
Загружено:
Arinta Purwi SuhartiАвторское право:
Доступные форматы
Am. J. Trop. Med. Hyg., 76(3), 2007, pp.
497501
Copyright 2007 by The American Society of Tropical Medicine and Hygiene
ANTIPLASMODIAL INTERACTIONS BETWEEN ARTEMISININ AND TRICLOSAN
OR KETOCONAZOLE COMBINATIONS AGAINST BLOOD STAGES OF
PLASMODIUM FALCIPARUM IN VITRO
LOKESH C. MISHRA, AMIT BHATTACHARYA, AND VIRENDRA K. BHASIN*
Department of Zoology, University of Delhi, North Campus Delhi University, Delhi 110007, India
Abstract. Emergence of drug-resistant Plasmodium falciparum strains to conventional first-line antimalarial drugs
has compelled many countries to reorient their drug policies to adopt artemisinin-based combination therapies (ACTs)
for treatment of uncomplicated malaria. This has increased the demand of artemisinin, already a scarce commodity.
Synthesis of artemisinin is not yet commercially viable. Extensive use of available ACTs will invariably lead to emergence of resistance to these combinations. Thus, there is need to search for new artemisinin-based synthetic, inexpensive,
synergistic combinations to reduce dependence on artemisinin. In vitro cultures of P. falciparum provide an appropriate
system for identification of such new combinations. We evaluated interactions of artemisinin with triclosan or ketoconazole against blood stages of P. falciparum by a fixed-ratio isobologram method. Artemisinin shows mild synergistic
interaction with triclosan and slight to marked antagonism with ketoconazole in vitro. These antiplasmodial interactions,
however, require confirmation using in vivo model systems.
demonstrated antiplasmodial activity.26 In-depth studies of
interactions between drugs may also provide clues to their
mechanisms of action.7
INTRODUCTION
Hundreds of millions of people are at risk of drug-resistant
falciparum malaria infection. The worsening problems of
drug resistance in many parts of the world and the limited
number of antimalarial drugs available have led to increasing
difficulties for adequate disease management. Artemisinin
and its derivatives are among the most effective antimalarial
drugs known today. They rapidly cure even drug-resistant
falciparum infections. Artemisinin-based combination therapies (ACTs) are being used for treatment, instead of monotherapies, to delay the emergence of resistant strains of Plasmodium falciparum to this vital class of drugs. ACTs are increasingly being adopted as first-line treatments in malariaendemic regions of the world that are afflicted with P.
falciparum strains resistant to conventional antimalarial
drugs. The history of drug resistance is replete with instances
showing the uncanny ability of parasites to rapidly acquire
resistance to any chemotherapeutic assault deployed en
masse to treat uncomplicated malaria cases. Clinically artemisinin-resistant strains of P. falciparum have not yet been
encountered. Thus, the demand for ACTs is increasing. Artemisinin is obtained from aerial parts of an herb, and this
plant is globally scarce. Synthesis of artemisinin is not a commercially viable proposition at present. This makes ACT expensive for poor people in malaria-endemic regions. There is
also reason to believe that, sooner or later, resistance to existing ACTs will emerge. Thus, there is need to search for
synthetic synergistic drug partners of artemisinin and its derivatives to reduce dependence on this scarce natural product
in ACTs. Use of a P. falciparum in vitro system is very potent
in identifying novel lead compounds and combinations. We
have evaluated the in vitro antiplasmodial activity of the synthetic compounds triclosan and ketoconazole as partner drugs
in combination with artemisinin against erythrocytic stages of
P. falciparum using a modified fixed-ratio isobologram
method to study drugdrug interactions.1 Both of these combination partner drugs are FDA approved for human use and
MATERIALS AND METHODS
Parasite culture. Stock culture of malaria parasite P. falciparum 3D7 strain was continuously maintained in vitro using
the candle-jar method of Trager and Jensen.8 The parasites
were maintained on B+ human red blood cells suspended in a
complete culture medium. Each 960 mL of aqueous culture
medium consisted of 10.4 g of powdered RPMI-1640 (with
glutamine but without bicarbonate), 5.94 g of HEPES buffer,
and 40 mg of gentamicin. Complete medium was constituted
just before use by adding sterile 5% sodium bicarbonate at
the rate of 4 mL per 96 mL and supplemented with 10%
pooled B+ serum. The stock culture parasitemia was mostly
kept between 1% and 5% with subculturing every fourth day.
The starting hematocrit was 5%.
Drug solutions. Artemisinin, triclosan, and ketoconazole
were obtained from Sigma-Aldrich (St. Louis, MO), Vivimed
Laboratories Ltd. (Hyderabad, India), and Yanshu Chemicals
Ltd. (Mumbai, India), respectively. Artemisinin and triclosan
were dissolved separately in DMSO, and ketoconazole was
dissolved in redistilled water to obtain stock solutions of 0.2,
1, and 1 mg/mL concentrations, respectively. The stock solutions were diluted on the day of experiment to obtain the
desired concentrations for each drug. The amount of DMSO
in the diluted concentrations used had no effect on parasite
growth.
Inhibitory concentrations assay. The inhibitory concentration of each individual drug needed to prevent the growth and
multiplication of P. falciparum was determined in vitro using
a doseresponse assay in 24-well tissue culture plates in triplicates. Synchronous parasites were prepared9 and challenged
with a graded concentration of a drug solution for 48 hours at
37C by the candle-jar method.8 The medium was changed in
each well after 24 hours with or without drug. The percentage
inhibition of parasitemia in relation to control was calculated
by examining thin-smear Giemsa-stained slides. Assay results
were computed to determine the IC50 value of each drug.
* Address correspondence to Virendra K. Bhasin, Department of
Zoology, University of Delhi, North Campus Delhi University, Delhi
110007, India. E-mail: virendrabhasin@hotmail.com
497
498
MISHRA AND OTHERS
Drug combination preparations. For each combination assay, drug strength was made so that IC50 of the individual
drugs fell between third and fourth 2-fold serial dilutions,
while the other four drug combinations were made in fixed
ratios (Tables 2 and 3). Six combinations prepared in nM
ratios of artemisinin/triclosan were 32:0, 25.6:1780, 19.2:3560,
12.8:5340, 6.4:7120, and 0:8900, respectively; and six concentrations of artemisinin (nM)/ketoconazole (M) combinations were 32:0, 25.6:3.36, 19.2:6.72, 12.8:10.08, 6.4:13.44, and
0:16.8, respectively.
Combination plate preparation. Drug dilutions of combinations were made in sterile, flat-bottom, 96-well tissue culture
plates as described elsewhere.1 Each microtiter plate contains
wells in eight rows (AH) and 12 columns. Wells in row H,
columns 3 to 11, contained a 2 stock concentration, and
serial dilutions were made from solutions in these wells upward to wells in row B. Each well contained a total volume of
200 L of drug, presynchronized infected RBCs (0.8% parasitemia at 2.5% hematocrit), and complete culture medium.
Simultaneously, parasite control wells without drug were prepared in row A, columns 3 to 11, and rows A to H, columns
2 and 12, although only column 2 was taken for IC50 calculations. The wells in column 1, rows A to H, were kept with a
normal RBC suspension in complete medium, without drug.
Six combinations (in triplicate) were tested in two plates. Except for row H, columns 3 to 11, in all wells 100 L of complete medium was added. Serial dilution was done from row
H to row B, with transfer of 100 L each time after mixing,
and 100 L from the wells in row B was discarded finally. The
plates were kept in a candle jar and candle-lighted to increase
CO2 concentration.8 The plates were incubated at 37C for 48
hours with a brief interruption after 24 hours, and re-gassed
by burning the candle.
Slide preparation and staining. The plates were removed
from candle jar, and the material from each test well was
transferred into the corresponding well numbered 1.5-mL microcentrifuge tube. After a fast spin, the supernatant was removed and the pellet was mixed thoroughly to prepare thin
blood smear slide for each test well. The slides were air-dried,
methanol-fixed, and stained in Giemsa stain for 40 minutes.
After they were stained, slides were removed from the coupling jar, washed in running tap water, and air-dried. The
Giemsa-stained slides were examined to count the number of
parasites in random adjacent microscopic fields, equivalent to
3000 erythrocytes at 1000 magnification. Percent parasitemia was calculated.
Construction of isobologram. For the combination assay,
IC50 was calculated from two sets of doseresponse graphs
(Figures 1 and 2), each containing a drug-alone curve and
four drug-combination curves. Fractional inhibitory concentration (FIC) values were calculated separately for each drug
concentration present in the combination by the following
formula:
FIGURE 1. Doseresponse curves of artemisinin (A) and triclosan
(B) are presented for six different combination solutions with their
serial dilutions. IC50 values were calculated for both of the drugs
present in combinations 1 to 6 separately. In these examples, two sets
of curves of the first replicate are presented. Six sets of such curves
were obtained.
Sum FIC FIC =
IC50 of A in mixture
IC50 of A alone
+
IC50 of B in mixture
IC50 of B alone
RESULTS
Sensitivity of P. falciparum. The sensitivity of malaria
parasite, strain 3D7, to artemisinin, triclosan, and ketoconazole was assessed in vitro against erythrocytic stages. The
computed IC50 values given in Table 1 were used for combination assays.
Fraction of drug concentration required to produce
IC50 when used in combination
FIC =
Fraction of drug concentration required to produce
IC50 when used alone
Drug interaction assessment. The sum of the fractional inhibitory concentrations ( FICs) of both the drugs for a particular combination shows the interaction pattern10 between
the two drugs.
FIGURE 2. Doseresponse curves of artemisinin (A) and ketoconazole (B) are presented for six different combination solutions with
their serial dilutions. In these examples, two sets of curves of the first
replicate are presented. Six sets of such curves were obtained.
ARTEMISININ AND TRICLOSAN ANTIPLASMODIAL INTERACTIONS
TABLE 1
Baseline sensitivity of P. falciparum (strain 3D7) to artemisinin, triclosan, and ketoconazole in terms of IC50
Drug
Mean IC50 SE*
Artemisinin
Triclosan
Ketoconazole
3.97 0.08 nM
1.105 0.059 M
2.101 0.0253 M
* Standard error (n 3).
Sensitivity to drug combinations. From combination experiments, the observed IC50 values were analyzed in relation
to data obtained with the single compounds by using the
method of Berenbaum,11 which yielded FICs for the drug
combination. Mean FIC values were calculated separately for
both the drugs present in combinations 1 to 6. In these six
preparations, combinations 1 and 6 contain drug A and drug
B alone, respectively, so their IC50 corresponded to the IC50
obtained by their individual doseresponse assay. From each
triplicate, six sets of doseresponse curves were obtained. The
mean FICs of interaction between artemisinin/triclosan (Figure 3A) and artemisinin/ketoconazole (Figure 3B) were
plotted in an isobologram for combination preparations 1
through 6.
Interaction between artemisinin and triclosan. The FIC
values of artemisinin and triclosan fixed-ratio combinations
showed a synergistic interaction with combination 2 and
trends toward mild synergism with combinations 3, 4, and 5
(Table 2).
Interaction between artemisinin and ketoconazole. Interaction of artemisinin with ketoconazole showed an additive pattern with combination 2, moderate antagonism with combination 3 and 4, and marked antagonism with combination 5
(Table 3).
DISCUSSION
Artemisinin and its four derivatives (dihydroartemisinin,
artesunate, artemether, and arteether) are rapidly acting an-
FIGURE 3. (A) Isobologram showing the interaction between artemisinin and triclosan. (B) Isobologram showing the interaction between artemisinin and ketoconazole. Mean FICs of drugs A and B
were taken on the y and x axes, respectively, along with X and Y error
bars. The straight line joining both axes shows additive interaction.
499
timalarial drugs effective against even chloroquine-resistant
malaria infections. To improve their efficacy and delay the
onset of resistance to this vital class of antimalarial drugs, they
are used in combination with other effective antimalarial
drugs. At present, they play an essential role in malaria management and control. This, however, depends on ensuring
that they are affordable, readily available, and of acceptable
quality. Unfortunately, the quality and effectiveness of these
antimalarials have been declining, and the supply is often
inefficient and unreliable. Fake preparations of the frequently
used ACTartemether and lumefantrine combinationhave
hit some of the Southeast Asian markets.12 The global scarcity of artemisinin, leading to its high cost, and the lack of
quality control in resource-poor countries where malaria is
rampant are some of the factors for these maladies. The widespread misuse of ACTs suggests that they will succumb to
resistance sooner rather than later. The current grim situation
demands reduced dependence on artemisinins and a search
for synthetic, inexpensive partner drugs to augment the antiplasmodial activity of new combinations.
In vitro cultures of P. falciparum blood stages form a good
first screen for identifying potential partner drugs for ACTs
to be developed as anti-malaria therapies. Combining artemisinin with another in vitro-effective schizonticidal drug may
lead to altered pharmacokinetics, decreases in efficacy, and
modified toxicity levels of combined drugs. Many of these
aspects cannot be predicted using this system. However, an in
vitro drugdrug interactions interpretation for antiplasmodial
activity by an isobologram is obtainable and can provide information regarding synergistic, additive (indifferent), or antagonistic outcomes in inhibiting parasite growth and multiplication. Isobolograms are prepared either by the fixed-ratio
method,1 where concentration ratios of both drugs differ by a
fixed ratio, or by the checkerboard method,13 where one drug
concentration is kept constant while the other is varied. Both
of these methods have been used in drug-combination studies
for antitumor, antibacterial, and antifungal agents.1416 The
fixed-ratio method using known synergistic antimalarial
drugssulfadoxine and pyrimethaminein combination assay was validated (data not presented) and found to be accurate, simple, and straightforward. In-depth study of antimalarial drug interactions is of great significance to both development of combination therapies and understanding the
mode of action of these drugs.7
The candidate partner drug in ACT should have an independent mode of action to delay the selection of resistance.
Artemisinins are sesquiterpene lactones containing an endoperoxide bridge. There are several views regarding the mode
of action of artemisinin on P. falciparum. The mechanism of
action is considered to be at least two-step processes, involving an activation step and alkylation. In the activation step,
intraparasitic iron catalyzes cleavage of the endoperoxide
bridge and generates a highly reactive free radical, which in
the second step forms a covalent bond with parasite proteins
and incapacitates them,17,18 eventually killing the parasite. It
seems to act on many targets within a nanodomain vicinity of
the parasite. Perhaps this is one reason why resistance to this
vital class of drug has not emerged despite its long historic use
for fever resolution in China. A yeast model showed artemisinin to interact with the electron transport chain, generating a
local reactive oxygen species and causing depolarization of
the mitochondrial membrane.19 It has also been shown that
500
MISHRA AND OTHERS
TABLE 2
Interaction between artemisinin and triclosan against P. falciparum (strain 3D7) at different combination solutions
Ratio of drugs (in 100 L)
Mean FIC50 SE*
Combination
solution
Drug A
Drug B
Drug A (artemisinin)
Drug B (triclosan)
FICs, interaction
1
2
3
4
5
6
5
4
3
2
1
0
0
1
2
3
4
5
1.0 0.029
0.416 0.0078
0.568 0.0087
0.3233 0.0047
0.1483 0.00145
0.0
0.0
0.1093 0.0027
0.386 0.0079
0.494 0.006
0.666 0.0245
1.0103 0.0399
1.0, ADD
0.525, SYN
0.954, SLT-SYN
0.817, SLT-SYN
0.824, SLT-SYN
1.0103, ADD
* Standard error (n 3).
SYN, synergistic; SLT-SYN, slightly synergistic; ADD, additive.
artemisinins exert their antimalarial action by disrupting calcium homeostasis; they promote discharge of calcium ions
from intracellular stores of malaria parasite by specifically
inhibiting a metabolic enzyme: the malarial, calciumdependent, endoplasmic reticulum ATPase.20 Inhibition of
this enzyme causes uncontrolled release of calcium stored in
the endoplasmic reticulum into cytoplasm, causing parasite
death.
Triclosan is synthetic 2-hydroxydiphenyl ether that has
been evaluated as a drug partner with artemisinin. Triclosan
has a favorable safety profile and is well tolerated by humans.2 It is neither an acute oral toxicant nor does it act as a
carcinogen, mutagen, or teratogen.2 It is found in many commercial products, such as mouthwashes and deodorants. Its
use as a systemic antimicrobial has not been established, but
antimalarial activity was demonstrated when it was administered subcutaneously6 in an in vivo system. Triclosan also
inhibits the growth of the blood stages of P. falciparum in
vitro and is effective against chloroquine-resistant and chloroquine-sensitive strains.6 Triclosan inhibits the fatty acid biosynthesis II (FAS II) pathway in P. falciparum through inhibition of Fab enzyme, which is necessary for the conversion
of crotonyl-ACP (acyl carrier protein) in butyryl-ACP.6,21
The FAS II pathway is completely lacking in humans and is,
therefore, potentially an attractive target for antimalarial
therapeutics.22 On the basis of these facts, triclosan was considered to be a suitable partner drug for evaluation with artemisinin. A modified fixed-ratio isobologram method1 was
used to determine the effect of triclosan in combination with
artemisinin in strain 3D7 of P. falciparum. The experiments
conducted in combination showed a mild synergistic interaction in each combination ratio (Table 2), with synergism at
combination 2. But even a weak synergistic interaction may
be of importance for its mechanistic implications in the design
and development of new agents.15 Both artemisinin and tri-
closan also showed differential stage-specific inhibitions with
high mortality of schizont and trophozoite blood stages, respectively (data not shown). This observation substantiates
the fact that they have different modes of action on the parasite. The pharmacokinetic characteristics of the partner drug
are important considerations in determining the suitability of
the drug for practical use. Both partners in drug combinations
should have similar pharmacokinetic characteristics, so as not
to leave any drug alone in circulation unprotected by the
other drug for extended period of time; otherwise, it will defeat the purpose of combination therapy. It is known that
artemisinin has a short half-life of a few hours.23 Similar studies with triclosan in humans are lacking. Intravenous administration of radiolabeled triclosan to rats showed that the
plasma elimination half-time was 9 hours.24 It will be of
interest to evaluate this combination in vivo malaria model
systemas well as triclosan in combination with different artemisinin derivativesto establish the synergistic effects of
this new antimalarial agent.
Ketoconazole was also evaluated for drug interactions with
artemisinin. This synthetic compound is an imidazole and has
wide-spectrum antimicrobial activity, including P. falciparum.5 Ketoconazole inhibits the enzyme 14--demethylase,
thereby interrupting the synthesis of ergosterol, an important
component of plasma membrane of apicomplexan parasites
like P. falciparum.25 This enzyme is also necessary for conversion of lanosterol into zymosterol, which is converted to
ergosterol.25 It also inhibits growth of falcipain (FP) crystals
by a surface-binding mechanism and interferes with other
heme crystal-sensitive pathways in P. falciparum, leading to
death of the parasite.3 Falcipain-2 (FP-2) plays an important
role in degradation of erythrocyte proteins like hemoglobin,
thus rendering an important target in the design of novel
antimalarial drugs.26 These considerations led to selection of
this compound in the present studies. Our experiments
TABLE 3
Interaction between artemisinin and ketoconazole against P. falciparum (strain 3D7) at different combination solutions
Ratio of drugs (in 100 L)
Mean FIC50 SE*
Combination
solution
Drug A
Drug B
Drug A (artemisinin)
Drug B (ketoconazole)
FICs, interaction
1
2
3
4
5
6
5
4
3
2
1
0
0
1
2
3
4
5
1.019 0.01266
1.217 0.03037
1.233 0.03851
1.208 0.05028
0.780 0.01472
0.0
0.0
0.301 0.005686
0.809 0.02771
1.793 0.06917
3.110 0.03166
1.001 0.004096
1.019, ADD
1.518, ADD
2.042, SLT-ANT
3.001, SLT-ANT
3.890, MKD-ANT
1.001, ADD
* Standard error (n 3).
ADD, additive; SLT-ANT, slightly antagonistic; MKD-ANT, markedly antagonistic.
ARTEMISININ AND TRICLOSAN ANTIPLASMODIAL INTERACTIONS
showed a combination of artemisinin and ketoconazole to be
largely antagonistic in antiplasmodial activity in vitro (Table
3). The antimalarial activity of ketoconazole is enhanced with
an increase in oxygen concentration.27 Older P. falciparuminfected erythrocytes are more susceptible to ketoconazole
than younger infected RBCs, as older RBCs are more susceptible to oxidative stress.28 Because we used the candle-jar
method, where the concentration of oxygen in the cultures
could not be controlled, it would be premature to conclude
that interactions between artemisinin and ketoconazole were
antagonistic without supporting evidence from in vivo or in
vitro model system wherein oxygen levels could be controlled. Although the concentrations of gentamicin used in
the experiments do not affect the parasite growth in vitro,29
even small amounts may affect drug interactions.
Received September 26, 2006. Accepted for publication November 7,
2006.
Financial support: This work was supported in part by the Department of Biotechnology, Ministry of Science and Technology, Government of India. L.C.M. and A.B. received fellowships from the
Council of Scientific and Industrial Research, New Delhi. The American Society of Tropical Medicine and Hygiene (ASTMH) assisted
with publication expenses.
Authors address: Lokesh C. Mishra, Amit Bhattacharya, and Virendra K. Bhasin, Department of Zoology, University of Delhi, Delhi
110007, India, Telephone: +91-11-27667989, E-mail: virendrabhasin@
hotmail.com.
REFERENCES
1. Fivelman QL, Adagu IS, Warhurt DC, 2004. Modified fixed ratio
isobologram method for studying in vitro interactions between
atovaquone and proguanil or dihydroartemisinin against drug
resistant strains of Plasmodium falciparum. Antimicrob Agents
Chemother 48: 40974102.
2. Bhargava HN, Leonard PA, 1996. Triclosan: applications and
safety. Am J Infect Control 6: 209218.
3. Chong CR, Sullivan DJ Jr, 2003. Inhibition of heme crystal
growth by antimalarials and other compounds: implications for
drug discovery. Biochem Pharmacol 66: 22012212.
4. Pfaller MA, Krogstad DJ, 1981. Imidazole and polyene activity
against chloroquine-resistant Plasmodium falciparum. J Infect
Dis 144: 372375.
5. Pfaller MA, Segal JJ, Krogstad DJ, 1982. Activity of ketoconazole and its deacyl derivative against Plasmodium falciparum
and Candida isolates. Antimicrob Agents Chemother 22: 917
919.
6. Surolia N, Surolia A, 2001. Triclosan offers protection against
blood stages of malaria by inhibiting enoyl-ACP of plasmodium falciparum. Nat Med 7: 167173.
7. Bell A, 2005. Antimalarial drug synergism and antagonism:
mechanistic and clinical significance. FEMS Microbiol Lett
253: 171184.
8. Trager W, Jensen JB, 1976. Human malaria parasites in continuous culture. Science 193: 673675.
9. Lambros C, Vanderberg JP, 1979. Synchronization of Plasmodium falciparum erythrocytic stages in culture. J Parasitol 65:
418420.
501
10. Gupta S, Thapar MM, Wernsdorfer WH, Bjorkman A, 2002. In
vitro interaction of artemisinin with atovaquone, quinine, and
mefloquine against Plasmodium falciparum. Antimicrob
Agents Chemother 46: 15101515.
11. Berenbaum MC, 1978. A method for testing synergy with any
number of agents. J Infect Dis 137: 122130.
12. Newton PN, McGready R, Fernandez F, Green MD, Sunjio M,
Bruneton C, Phanouvong S, Millet P, Whitty CJM, Talisuna
AO, Proux S, Christophel EM, Malenga G, Singhasivanon P,
Bojang K, Kaur H, Palmer K, Day NPJ, Greenwood BM, Nosten F, White NJ, 2006. Manslaughter by fake artesunate in
Asiawill Africa be next? PLoS Med 3: e197.
13. Martinez-Irujo JJ, Villahermosa ML, Alberdi E, Santiago E,
1996. A checkerboard method to evaluate interactions between drugs. Biochem Pharmacol 51: 635644.
14. Ryungsa K, Tanabe K, Inoue H, Toge T, 2002. Mechanism(s) of
antitumor action in protracted infusion of low dose 5-fluorouracil and cisplatin in gastric carcinoma. Int J Oncol 20: 549
555.
15. Hall MJ, Middleton RF, Westmacott D, 1983. The fractional inhibitory concentration (FIC) index as a measure of synergy. J
Antimicrob Chemother 11: 427433.
16. Meletiadis J, Mouton JW, Meis JFGM, Verweij PE, 2003. In vitro
drug interaction modeling of combinations of azoles with terbinafine against clinical Scedosporium prolificans isolates. Antimicrob Agents Chemother 47: 106117.
17. Meshnick SR, 1994. The mode of action of antimalarial endoperoxides. Trans R Soc Trop Med Hyg 88: 3132.
18. Ridley RG, 2003. Malaria: to kill a parasite. Nature 424: 887889.
19. Li W, Mo W, Shen D, Sun L, Wang J, 2005. Yeast model uncovers
dual roles of mitochondria in the action of artemisinin. PLoS
Genet 1: e36.
20. Ludwig UE, Webb RJ, van Goethem IDA, East JM, Lee AG,
Kimura M, ONeill PM, Bray PG, Ward SA, Krishna S, 2003.
Artemisinins target the SERCA of Plasmodium falciparum.
Nature 424: 957961.
21. Beeson JG, Winstanley PA, McFadden GI, Brown GV, 2001.
New agents to combat malaria. Nat Med 7: 149150.
22. Rao SP, Surolia A, Surolia N, 2003. Triclosan: a shot in the arm
for antimalarial chemotherapy. Mol Cell Biochem 253: 5563.
23. White NJ, 1997. Assessment of the pharmacodynamic property of
antimalarial drugs in vivo. Antimicrob Agents Chemother 41:
14131422.
24. Siddiqui WH, Buttar HS, 1979. Pharmacokinetics of triclosan in
rat after intravenous and intravaginal administration. J Environ Pathol Toxicol 2: 861871.
25. Docampo R, Moreno SNJ, 2001. Bisphosphonates as chemotherapeutic agents against trypanosomatid and apicomplexan
parasites. Curr Drug Targets Infect Disord 1: 5161.
26. Hogg T, Nagarajan K, Herzberg S, Chen L, Shen X, Jiang H,
Wecke M, Blohmke CJ, Hilgenfeld R, Schmidt CL, 2006.
Structural and functional characterization of falcipain-2, a hemoglobinase from the malarial parasite Plasmodium falciparum. J. Boil. Chem. 281: 2542525437.
27. Pfaller MA, Krogstad DJ, 1983. Oxygen enhances the antimalarial activity of the imidazoles. Am J Trop Med Hyg 32: 660
665.
28. Tiffert TH, Ginsburg H, Krugliak M, Elford BC, Lew VL, 2000.
Potent antimalarial activity of clotrimazole in in vitro cultures
of Plasmodium falciparum. Proc Natl Acad Sci USA 97: 331
336.
29. McClom AA, McHardy N, 1984. Evaluation of a range of antimicrobial agents against the parasitic protozoa, Plasmodium
falciparum, Babesia rodhaini and Theileria parva in vitro. Ann
Trop Med Parasitol 78: 345354.
Вам также может понравиться
- Aaaaaa KKДокумент1 страницаAaaaaa KKArinta Purwi SuhartiОценок пока нет
- NPH 12325Документ17 страницNPH 12325Arinta Purwi SuhartiОценок пока нет
- (2004, Bailey DKK) Prediction of Anti-Plasmodial Activity of A Annua - Application of 1H NMR Spectroscopy and ChemometricsДокумент10 страниц(2004, Bailey DKK) Prediction of Anti-Plasmodial Activity of A Annua - Application of 1H NMR Spectroscopy and ChemometricsArinta Purwi SuhartiОценок пока нет
- (2012 Ye & Bhatia) REVIEW - Metabolic Engineering For The Production of Clinically Important Molecules - Omega-3 Fatty Acids, Artemisinin, and TaxolДокумент14 страниц(2012 Ye & Bhatia) REVIEW - Metabolic Engineering For The Production of Clinically Important Molecules - Omega-3 Fatty Acids, Artemisinin, and TaxolArinta Purwi SuhartiОценок пока нет
- IJAMSCR 14 205 SreenagavalliДокумент3 страницыIJAMSCR 14 205 SreenagavalliArinta Purwi SuhartiОценок пока нет
- (2009, Anthony DKK) Optimization of The Mevalonate-Based Isoprenoid Biosynthetic in E Coli For Production Amorpha-4,11-DieneДокумент7 страниц(2009, Anthony DKK) Optimization of The Mevalonate-Based Isoprenoid Biosynthetic in E Coli For Production Amorpha-4,11-DieneArinta Purwi SuhartiОценок пока нет
- Molecules 15 00040Документ18 страницMolecules 15 00040Arinta Purwi SuhartiОценок пока нет
- (2002 Wentzinger DKK) Inhibition of Squalene Synthase and Squalene Epoxidase in Tobacco Cells Triggers An Up-Regulation of 3-Hydroxy-3-Methylglutaryl Coenzyme A Reductase PDFДокумент13 страниц(2002 Wentzinger DKK) Inhibition of Squalene Synthase and Squalene Epoxidase in Tobacco Cells Triggers An Up-Regulation of 3-Hydroxy-3-Methylglutaryl Coenzyme A Reductase PDFArinta Purwi SuhartiОценок пока нет
- 03 AДокумент10 страниц03 AArinta Purwi SuhartiОценок пока нет
- (2013 Pu DKK) Expression and Localization of Amorpha-4,11-Diene Synthase in Artemisia Annua L.Документ6 страниц(2013 Pu DKK) Expression and Localization of Amorpha-4,11-Diene Synthase in Artemisia Annua L.Arinta Purwi SuhartiОценок пока нет
- Inhibitory Effects of Artemisinin On Voltage-Gated Ion Channels in Intact Nodose Ganglion Neurones of Adult RatsДокумент8 страницInhibitory Effects of Artemisinin On Voltage-Gated Ion Channels in Intact Nodose Ganglion Neurones of Adult RatsArinta Purwi SuhartiОценок пока нет
- Journal Pone 0068231Документ8 страницJournal Pone 0068231bhatubimОценок пока нет
- Antimicrobial Activity of Crude Extracts 2Документ6 страницAntimicrobial Activity of Crude Extracts 2Arinta Purwi SuhartiОценок пока нет
- Ni Hms 135180Документ19 страницNi Hms 135180Arinta Purwi SuhartiОценок пока нет
- Medicinal PlantsДокумент151 страницаMedicinal Plantsallanquartermaine0% (1)
- Finding Out About Cystic Fibrosis - A Guide For Parents: Factsheet - March 2013Документ22 страницыFinding Out About Cystic Fibrosis - A Guide For Parents: Factsheet - March 2013Arinta Purwi SuhartiОценок пока нет
- Antibiotic Treatment For Cystic FibrosisДокумент102 страницыAntibiotic Treatment For Cystic Fibrosischar1356Оценок пока нет
- Ni Hms 135180Документ19 страницNi Hms 135180Arinta Purwi SuhartiОценок пока нет
- KhawajaДокумент4 страницыKhawajaArinta Purwi SuhartiОценок пока нет
- FS Physio Babies and Toddlers Mar 13Документ7 страницFS Physio Babies and Toddlers Mar 13Arinta Purwi SuhartiОценок пока нет
- Antimicrobial Activity of Crude Extracts 2Документ6 страницAntimicrobial Activity of Crude Extracts 2Arinta Purwi SuhartiОценок пока нет
- MeleДокумент4 страницыMeleArinta Purwi SuhartiОценок пока нет
- Medicinal PlantsДокумент151 страницаMedicinal Plantsallanquartermaine0% (1)
- 5 Ajps 3 1 2013Документ4 страницы5 Ajps 3 1 2013Arinta Purwi SuhartiОценок пока нет
- HarrДокумент11 страницHarrArinta Purwi SuhartiОценок пока нет
- The Pathogenesis and Pathophysiology of Type 1 and PDFДокумент12 страницThe Pathogenesis and Pathophysiology of Type 1 and PDFasmawatiОценок пока нет
- Herbal Cosmetics for Beautiful Skin and HairДокумент9 страницHerbal Cosmetics for Beautiful Skin and HairBogdanОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Integrated disease management conceptsДокумент8 страницIntegrated disease management conceptsNidhi SinghОценок пока нет
- Ophthalmology - Diseases of CorneaДокумент18 страницOphthalmology - Diseases of CorneajbtcmdtjjvОценок пока нет
- MedChem10 Antiviral PDFДокумент85 страницMedChem10 Antiviral PDFMартин ДончевОценок пока нет
- RIZAL TECHNOLOGICAL UNIVERSITY NATIONAL SERVICE TRAINING PROGRAM MODULESДокумент9 страницRIZAL TECHNOLOGICAL UNIVERSITY NATIONAL SERVICE TRAINING PROGRAM MODULESJULIUS CAEZAR CHAVEZОценок пока нет
- Michael G. Glasspool FRCS, DO (Auth.) - Atlas of Ophthalmology-Springer Netherlands (1982) PDFДокумент117 страницMichael G. Glasspool FRCS, DO (Auth.) - Atlas of Ophthalmology-Springer Netherlands (1982) PDFInna BujorОценок пока нет
- Hepatitis B: DR Tanmay Vyas (DM Hepatology)Документ37 страницHepatitis B: DR Tanmay Vyas (DM Hepatology)Sreekanth VattikondaОценок пока нет
- Exually Tran Mitted Disease: Rean Jane EscabarteДокумент14 страницExually Tran Mitted Disease: Rean Jane EscabarteRan Jung EscabarteОценок пока нет
- Protein Calorie MalnutritionДокумент97 страницProtein Calorie Malnutritionnshaikh56Оценок пока нет
- SiriДокумент1 страницаSirisrinivasОценок пока нет
- India Today 18 March 2013Документ124 страницыIndia Today 18 March 2013Ravi SinghОценок пока нет
- Introduction and Neoplasia - PathologyДокумент20 страницIntroduction and Neoplasia - PathologyjmosserОценок пока нет
- ImpactionДокумент11 страницImpactionKhalid AgwaniОценок пока нет
- Gelect3 5Документ3 страницыGelect3 5Mhartin OrsalОценок пока нет
- Cancer ImmunologyДокумент12 страницCancer ImmunologyFreddy TorresОценок пока нет
- The Prevalence of Parasitic Protozoan Diseases in Iraq, 2016Документ5 страницThe Prevalence of Parasitic Protozoan Diseases in Iraq, 2016Jeremia AnkesaОценок пока нет
- Odessa National Medical University: Surgical InfectionsДокумент34 страницыOdessa National Medical University: Surgical InfectionsDrRajneesh ShastriОценок пока нет
- Herpes Simplex Type 1&2Документ15 страницHerpes Simplex Type 1&2ulfah febyОценок пока нет
- MycotoxinsДокумент20 страницMycotoxinsibraheem aboyadak100% (1)
- Expanded Program On Immunization Philippines)Документ8 страницExpanded Program On Immunization Philippines)Mark AcuzarОценок пока нет
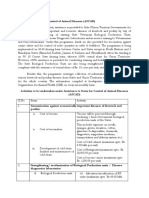
- Assistance To States For Control of Animal Diseases (ASCADДокумент6 страницAssistance To States For Control of Animal Diseases (ASCADMonal DaptardarОценок пока нет
- People at Virology: Dmitri Iosifovich Ivanovsky - Founders of VirologyДокумент2 страницыPeople at Virology: Dmitri Iosifovich Ivanovsky - Founders of VirologyFae BladeОценок пока нет
- NematodesДокумент4 страницыNematodesPrincess Shaina CanapeОценок пока нет
- Tuberculosis Lab ReportДокумент4 страницыTuberculosis Lab ReportJullian Clare CreusОценок пока нет
- Hot Topics in Internal MedicineДокумент9 страницHot Topics in Internal Medicinekhangsiean89Оценок пока нет
- Chikungunya - DINKES - RS UNAIR 22 November 2017Документ24 страницыChikungunya - DINKES - RS UNAIR 22 November 2017Mojo PuskesmasОценок пока нет
- Sanitary Engineering2 (Repaired)Документ95 страницSanitary Engineering2 (Repaired)ronnel mauzar100% (2)
- Litchi Heart Disease and It's ControlДокумент23 страницыLitchi Heart Disease and It's Controlpracholi lamp100% (1)
- Kumar Indoor Air Quality Study Summary - Proffer SweepsДокумент1 страницаKumar Indoor Air Quality Study Summary - Proffer SweepsAnonymous Pb39klJОценок пока нет
- Feline Dermatophytosis Treatment RecommendationsДокумент21 страницаFeline Dermatophytosis Treatment RecommendationsFrancisca Thenée SerranoОценок пока нет
- Causes of Sterile Pyuria Infection RelatedДокумент2 страницыCauses of Sterile Pyuria Infection RelatedSarah AhmedОценок пока нет