Академический Документы
Профессиональный Документы
Культура Документы
8 Full
Загружено:
Amar Mahesh KalluОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
8 Full
Загружено:
Amar Mahesh KalluАвторское право:
Доступные форматы
Eur J Echocardiography (2000) 1, 811
doi:10.1053/euje.2000.0006, available online at http://www.idealibrary.com on
HISTORICAL NOTE
Seeing the Invisible:
A Short History of Cardiac Ultrasound
Address all correspondence to: J. R. T. C. Roelandt, Thoraxcenter,
Room Bd 408, Dijkzigt Hospital, Dr Molewaterplein 40,
Rotterdam 3015 GD, The Netherlands
1525-2167/00/010008+04 $35.00/0
Downloaded from by guest on February 6, 2016
Cardiac ultrasound has been the most important
advance in diagnostic cardiology since the discovery
of X-rays by W. K. Rontgen[1]. Its development
closely paralleled the advances in electronic and
computer technology and is an example of interaction
and co-operative eorts of engineers, physicists and
clinicians.
The existence of ultrasound was recognized by L.
Spallanzani (17291799). He demonstrated that bats
who are blind navigate by means of echo-reflection
using inaudible sound. Spallanzani is, therefore, considered the father of ultrasound. In 1880, Jacques
and Piere Curie[2] discovered the piezo-electric eect,
a peculiar phenomenon observed in certain quartz
crystals which were the basis of the early ultrasound
systems and were later replaced by ferro-electric
materials. These were the basic ingredients, but the
technology for the ultrasound instruments was
derived from sound navigation and ranging
(SONAR) systems which were developed for the
military for ship navigation and remote submarine
detection.
The first suggestions of locating submerged objects
by echo-reflection probably came after the Titanic
disaster in 1912. During World War I, P. Langevin
(18721946) conceived in 1917 the idea to use a
piezo-electric quartz crystal as both the transmitter
and receiver, and this ultimately led to the development of sonar, which was completed with the invention of the cathode ray tube and extensively used in
World War II. Interestingly, Langevin equated mass
and energy independently of Einstein. The Austrian
K. T. Dussik was the first to apply ultrasound for
medical diagnosis in 1941[3] (Fig. 1). He tried to
outline the ventricles of the brain using echotransmission, a principle similar to X-ray imaging.
Dussik can be regarded the father of diagnostic
ultrasound. He also considered the use of echoreflection, but discontinued his idea after being
ridiculed. In 1950, the German W. D. Keidel, also
Figure 1. K. T. Dussik, the father of diagnostic ultrasound. He used an ultrasound transmission procedure to
visualize the ventricles of the brain and suggested the use
of reflected ultrasound.
using an echo-transmission technique, performed the
first cardiac examinations in an attempt to measure
cardiac output[4]. This sonocardiometric technique
was later used by R. F. Rushmer in his classic
cardiovascular experiments in awake animals.
The first experiments using ultrasonic echoreflection for examining the heart were initiated by I.
Edler and C. H. Hertz in Lund, Sweden[5] (Fig. 2).
These investigators were largely stimulated by their
surgical colleagues, who wanted a more accurate
2000 The European Society of Cardiology
A Short History of Cardiac Ultrasound
Figure 2. I. Edler and C. H. Hertz, who in 1953 recorded
the first M-mode echocardiograms of the heart using an
industrial reflectoscope for flaw detection. The picture
was taken at the Second Symposium on Echocardiology
in 1979 in Rotterdam.
diagnosis before surgery, cardiac catherization still
being in its infancy at that time. They produced the
first echocardiograms of the heart in 1953 (Fig. 3). An
industrial pulse-echo ultrasonic flaw detector to find
cracks in metals, and which they borrowed from a
shipyard to Malmo , was used. This industrial reflectoscope was only available during weekends. Fortuitously, this instrument had the wavelength and other
physical characteristics which were appropriate for
visualizing the heart. (Quite often, the story of a
scientific discovery is based on chance rather than
design). They identified many of the structures of the
heart. C. H. Hertz also devised the ink-jet recorder to
produce a strip chart recording of the echoes originating from a selected structure (time-motion or
M-mode recording) and the simultaneous recording
of ECG. In the late 1960s the fibre-optic recorder, a
spin-o from space technology, was introduced,
allowing the M-mode recording of all structures
along the ultrasound beam: this constituted the
definitive breakthrough in echocardiography. Today,
M-mode echocardiography remains an important
part of a complete cardiac ultrasound examination
because of its high temporal resolution, which allows
accurate analysis of fast-moving structures.
In 1968, R. Gramiak and P. M. Shah[6] described
contrast echocardiography, an accidental observation
during indocyanine green injections for cardiac output measurement. This technique was extremely helpful in further identifying and delineating the various
cardiac structures and is presently being refined for
myocardial perfusion studies.
In the 1960s, great progress was being made in
developing real-time two-dimensional (2D) echocardiography. In fact, it was the combination of
sonar technology with advanced radar circuitry which
improved ultrasonic instrument performance and
introduced the prospect of 2D echocardiography.
After the early pioneering work of J. J. Wild and
J. M. Reid[7] and D. H. Howry and W. R. Bliss[8] in
the early 1950s, both European and Japanese investigators introduced real-time 2D instruments based on
dierent principles. The practical use of these instruments, however, was limited because of the need for a
water bath contact, limited frame rates and large size
transducers. Indeed, the small precordial acoustic
windows to the heart dictate the use of a small
transducer. The large footprint of the bulky transducer was also the problem of the linear array system
developed at the Thoraxcentre, but the clinical results
with this instrument nevertheless stimulated the
interest of cardiologists[9]. In 1968, J. Somer[10] had
constructed the first electronic phased-array scanner
based on the wave-front theory formulated in the
17th century by C. Huygens and sonar technology,
but the advantages of 2D echocardiography over
M-mode echocardiography were yet to be realised. J.
Grith and W. Henry[11] introduced the mechanical
sector-scanner in 1974, in the same year that F. J.
Thurstone and O. T. von Ramm[12] constructed their
electronic phased-array scanner similar to the instrument developed by J. Somer. This instrument marked
the beginning of the revolutionary impact of ultrasound on clinical cardiology. Today, phased-array
scanners are the most widely available imaging instruments and have a greater impact on cardiac diagnosis
than electrocardiography, for which Einthoven was
awarded the Nobel prize in 1924.
The Austrian C. A. Doppler (18031853) worked
out the mathematical relationship between the frequency shift of sound and the relative motion of the
sound source and the observer, a theory tested in
Eur J Echocardiography, Vol. 1, issue 1, March 2000
Downloaded from by guest on February 6, 2016
Figure 3. One of the earliest M-mode echocardiograms
of the mitral valve, recorded by I. Edler and C. H. Hertz
in December 1953. The sensitivity of the transducers
used at that time allowed the recording of echoes from
diseased valves only, and not from normal valves.
10
J. R. T. C. Roelandt
Eur J Echocardiography, Vol. 1, issue 1, March 2000
definitive clinical breakthrough of transoesophageal
echocardiography[24,25].
As early as 1960, T. Ciezynski[26] mounted a single
element transducer on a catheter to obtain intracardiac echocardiograms, and 3 years later R. Omoto[27]
obtained intracardiac 2D images with a slowly rotating, single-element transducer mounted at a cathetertip. Two years later, N. Bom et al.[28] described a
real-time intracardiac scanner using an electronically
phased circular array of 32 elements at the tip of a 9F
catheter. These developments were discontinued
because of limitations of miniaturization and the
striking improvements in precordial image quality
making intracardiac imaging unnecessary. The rapid
progress in interventional cardiology renewed the
interest in imaging devices, allowing circumferential
imaging of the arterial wall under the endothelial
surface. Both mechanical single-element and multielement electronic systems are now increasingly
used.
Since the early 1970s numerous investigators have
explored the feasibility of three-dimensional (3D)
echocardiography. New computer technologies
recently have made volume rendered data which
make the display of tissue information possible[29,30]
even in real-time[31]. In the coming years this modality
will further strengthen the diagnostic capabilities of
cardiac ultrasound.
In this short history of cardiac ultrasound, credit is
given to the pioneers of this exciting non-invasive and
cost-eective diagnostic modality. Because of its
versatility of application in a wide variety of healthcare environments, the technique will continue to
grow along with advances in digital techniques and
miniaturization.
References
[1] Ro ntgen WK, U
} ber eine neue Art von Strahlen (Vorla nfige
Mitteilung). Sitzungsber. Physik Med Ges Wurzburg 1895:
132141.
[2] Curie J, Curie P. Sur lelectricite polaire dans les cristaus
he mie`dres a` faces incline es. Compt Rend Seances Acad Sci
1880; 91: 383389.
[3] Dussik KT. U
} ber die Moglichkeit Hochfrequente Mechanische Schwingungen als Diagnostisches Hilfsmitel zu
Verwerten. Z. Neurol 1941; 174: 153.
[4] Keidel von WD. Uber eine neue Methode zur Registrierung
ger Volumanderungen des herzens am Menschen. Zeitschr
Kreislauorschung 1950; 39: 257.
[5] Edler I, Hertz CH. Use of ultrasonic reflectoscope for continuous recording of movements of heart walls. Kurgl.
Fysiogr. Salad i Lund Forhandl 1954; 24: 5.
[6] Gramiak R, Shah PM. Echocardiography of the aortic root.
Invest Radiol 1968; 3: 356.
[7] Wild JJ, Reid JR. Application of echo-ranging techniques to
the determination of structure of biological tissues. Science
1952; 115: 226.
[8] Howry DH, Bliss WR. Ultrasonic visualisation of soft tissue
structures of the body. J Lab Clin Med 1952; 40: 579.
Downloaded from by guest on February 6, 2016
practice in 1845 by C. H. D. Buys Ballot (18171890)
in Utrecht.
Investigation of blood flow velocity using Doppler
frequency shifts to measure motion of cardiac structures, and later of the velocity of red blood cells,
started with the work of S. Satomura and his colleagues in 1957.[13]. The pulsed-wave Doppler technique was almost simultaneously introduced by P. N.
T. Wells[14], P. A. Peronneau et al.[15,16] and D. W.
Baker[17]. The method allowed depth selection for
blood flow velocity interrogation, but the major step
forward for its clinical acceptance was its combination with imaging: the duplex scanner published by
F. E. Barber et al. in 1974[18]. This development ultimately led to the integration of pulsed-wave
Doppler with 2D phased-array systems and allow
blood flow to be studied at selected regions within
the image plane. The Bernouilli equation is now the
cornerstone of the Doppler assessment of cardiac
haemodynamics and was published by the Dutchborn D. Bernouilli (17001782) in his treatise Hydrodynamica in 1738. He formulated the relationship of
the pressure drop across the inlet of an obstruction in
a flow channel to the flow rate through it.
J. Holen et al.[19] showed in 1977 that the Bernouilli
equation could be applied to estimate the pressure
drop across a stenotic orifice from the jet flow
velocity. In 1978, the Swiss-born M. A. Brandestini
et al.[20] produced a 128-channel digital multigate
Doppler instrument, allowing the imaging of cardiac
structures and blood flow in colour and in real-time.
Based on similar principles, C. Kasai et al.[21] constructed in 1982 the revolutionary colour Doppler
flow imaging system based on autocorrelation
detection, providing a non-invasive angiogram of
normal and abnormal blood flow on a beat-to-beat
basis. At present, M-mode, 2D, pulsed-wave,
continuous-wave and colour Doppler flow are all
combined in one diagnostic console, and represent
the most comprehensive cardiac diagnostic modality
by providing integrated structural, functional and
haemodynamic information. A modern echo/Doppler
laboratory can nowadays be appropriately referred to
as the non-invasive imaging and haemodynamic
laboratory.
Although the idea of transoesophageal ultrasound
to circumvent chest wall problems dates back to the
early 1970s, clinical application started with anaesthetists using a M-mode system introduced by
L. Frazin et al. in 1976[22]. The Japanese engineer
K. Hisanaga and co-workers[23] first reported transoesophageal 2D imaging with a mechanical scanning
system 1 year later. The mono- and biplane electronic
phased-array probes developed by J. Souquet in 1982
and his multiplane probe in 1985 represented the
A Short History of Cardiac Ultrasound
[22]
[23]
[24]
[25]
[26]
[27]
[28]
[29]
[30]
[31]
correlation technique. IEEE Trans Sonics Ultrason 1985; 32:
460463.
Frazin L, Talan JV, Stephanides L et al. Esophageal echocardiography (abstr.). Circulation 1976; 54: 102.
Hisanaga K, Hisanaga A, Ichie Y. A new transesophageal
real-time linear two-dimensional echocardiographic system
using a flexible tube and is clinical application. Proc Jpn Soci
of Ultrasonics in Med 1977; 32: 4344.
Souguet J, Hanrath P, Zitelli L et al. Transesophageal phased
array for imaging the heart. IEEE Trans Biomed Eng 1982; 29:
707.
Harui N, Souquet. Transesophageal echocardiography
scanhead. United States patent no. 4.543.960, October 1,
1995.
Cieszynski T. Intracardiac method for the investigation of
structure of the heart with the aid of ultrasonics. Arch Immun
Ter Dow 1960; 8: 551557.
Omoto R. Intracardiac scanning of the heart with the aid of
ultrasonic intravenous probe. Jpn Heart J 1967; 8: 569581.
Bom N, Lancee CT, Egmond van FC. An ultrasonic intracardiac scanner. Ultrasonics 1972; 10: 7276.
Wollschlager H. Transesophageal echo computer tomography: a new method for dynamic three-dimensional imaging of
the heart. In: Computers in Cardiology 1989. IEEE Computer
Society 1990: 39.
Roelandt J, ten Cate FJ, Bruining N, Salustri A, Vletter WB,
Mumm B, van der Putten N. Transesophageal rotoplane
echo-CT. A novel approach to dynamic three-dimensional
echocardiography. Thoraxcentre J 1993; 6: 48.
Von Ramm OT, Smith SW, Pavy HG Jr. High-speed ultrasound volumetric imaging system. Part II. Parallel processing
and image display. IEEE Trans Ultrason Ferroelec Freq Cont
1991; 38: 109115.
Eur J Echocardiography, Vol. 1, issue 1, March 2000
Downloaded from by guest on February 6, 2016
[9] Bom N, Lancee CT, Honkoop J, Hugenholtz PC. Ultrasonic
viewer for cross-sectional analysis of moving cardiac structures. Biomedical Eng 1971; 6: 500.
[10] Somer JC. Electronic sector scanning for ultrasonic diagnosis.
Ultrasonics 1968; 6: 153159.
[11] Grith JM, Henry WL. A sector scan for real time twodimensional echocardiography. Circulation 1974; 49: 1147
1152.
[12] Thurstone FL, von Ramm OT. A new ultrasound imaging
technique employing two dimensional electronic beam steering. In: Green PS (ed.). Acoustical Holography. Plenum Press,
New York 1974; 5: 149159.
[13] Satomura S. Ultrasonic Doppler method for the inspection of
cardiac function. J Acoust Soc Am 1957; 29: 11811185.
[14] Wells PNT. A range-gated ultrasonic Doppler system. Med
Biol Eng 1969; 7: 641652.
[15] Peronneau PA, Leger F. Doppler Ultrasonic pulsed blood
flow meter. Proc Int Conf Med Engng 1969: 10.
[16] Peronneau PA, Hinglais JR, Pellett MM, Leger F. Ve locimetre sanguin par eet Doppler a` e mission ultrasonore pulse e.
Onde Elect 1970; 50: 369384.
[17] Baker DW. Pulsed ultrasonic Doppler blood flow sensing.
IEEE Trans Sonics Ultrason 1970; 17: 170185.
[18] Barber FE, Baker DW, Nation AWC, Strandness De, Reid
JM. Ultrasonic duplex echo-Doppler scanner. IEEE Trans
Biomed Eng 1974; 21: 109113.
[19] Holen J, Aaslid R, Landmark K, Simonsen S, Ostrem T.
Determination of eective orifice area in mitral stenosis from
noninvasive Doppler data and mitral flow rate. Acta Med
Scand 1977; 201: 8388.
[20] Brandestini MA. Topoflow: a digital full range Doppler
velocity meter. IEEE Son Ultrason SU25-5 1978; 287293.
[21] Kasai C, Namekawa K, Koyano A, Omoto R. Realtime two-dimensional blood flow imaging using an auto-
11
Вам также может понравиться
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
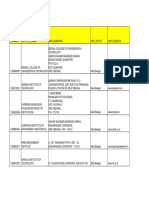
- EHS ActiveHospitals 551 14-03-2016Документ19 страницEHS ActiveHospitals 551 14-03-2016Amar Mahesh KalluОценок пока нет
- EHS ActiveHospitals 551 14-03-2016Документ19 страницEHS ActiveHospitals 551 14-03-2016Amar Mahesh KalluОценок пока нет
- Knobology Image Optimization and Trans Views - ShookДокумент5 страницKnobology Image Optimization and Trans Views - ShookAmar Mahesh KalluОценок пока нет
- Mechanical EngineДокумент23 страницыMechanical EngineAmar Mahesh KalluОценок пока нет
- Facial Fractures ClassificationДокумент72 страницыFacial Fractures ClassificationAmar Mahesh KalluОценок пока нет
- Aiims May 2015 QaДокумент222 страницыAiims May 2015 QaRexArtemОценок пока нет
- The "I Form", (The "Ich Form") The "We Form", (The "Wir" Form)Документ2 страницыThe "I Form", (The "Ich Form") The "We Form", (The "Wir" Form)Amar Mahesh KalluОценок пока нет
- Middle Ear Tumours: - Dr.P.Krishna Soumya ReddyДокумент19 страницMiddle Ear Tumours: - Dr.P.Krishna Soumya ReddyAmar Mahesh KalluОценок пока нет
- Approach To VERTIGOДокумент18 страницApproach To VERTIGOAmar Mahesh Kallu100% (1)
- Anaesthesia Drugs Used CommonlyДокумент6 страницAnaesthesia Drugs Used CommonlyAmar Mahesh KalluОценок пока нет
- Intubation ChartДокумент4 страницыIntubation ChartAmar Mahesh KalluОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- 1 in 8.5 60KG PSC Sleepers TurnoutДокумент9 страниц1 in 8.5 60KG PSC Sleepers Turnoutrailway maintenanceОценок пока нет
- Catedral de SevillaДокумент28 страницCatedral de SevillaAnonymous LkgNmKeОценок пока нет
- Chapter - I Introduction and Design of The StudyДокумент72 страницыChapter - I Introduction and Design of The StudyramОценок пока нет
- Topic 3Документ21 страницаTopic 3Ivan SimonОценок пока нет
- CV Augusto Brasil Ocampo MedinaДокумент4 страницыCV Augusto Brasil Ocampo MedinaAugusto Brasil Ocampo MedinaОценок пока нет
- Friction: Ultiple Hoice UestionsДокумент5 страницFriction: Ultiple Hoice Uestionspk2varmaОценок пока нет
- Food ResourcesДокумент20 страницFood ResourceshiranОценок пока нет
- Illustrating An Experiment, Outcome, Sample Space and EventДокумент9 страницIllustrating An Experiment, Outcome, Sample Space and EventMarielle MunarОценок пока нет
- Module 2 MANA ECON PDFДокумент5 страницModule 2 MANA ECON PDFMeian De JesusОценок пока нет
- Nadee 3Документ1 страницаNadee 3api-595436597Оценок пока нет
- WBДокумент59 страницWBsahil.singhОценок пока нет
- Cisco BGP ASPATH FilterДокумент115 страницCisco BGP ASPATH FilterHalison SantosОценок пока нет
- Department of Education: Republic of The PhilippinesДокумент1 страницаDepartment of Education: Republic of The PhilippinesJonathan CayatОценок пока нет
- Intellirent 2009 CatalogДокумент68 страницIntellirent 2009 Catalograza239Оценок пока нет
- Week 4 - Theoretical Framework - LectureДокумент13 страницWeek 4 - Theoretical Framework - LectureRayan Al-ShibliОценок пока нет
- Where We Are in Place and Time "We Are Part of The Universe and Feel Compelled To Explore It."Документ1 страницаWhere We Are in Place and Time "We Are Part of The Universe and Feel Compelled To Explore It."Safia-umm Suhaim- FareedОценок пока нет
- DeliciousDoughnuts Eguide PDFДокумент35 страницDeliciousDoughnuts Eguide PDFSofi Cherny83% (6)
- Aleutia Solar Container ClassroomДокумент67 страницAleutia Solar Container ClassroomaleutiaОценок пока нет
- Physics Blue Print 1 Class XI Half Yearly 23Документ1 страницаPhysics Blue Print 1 Class XI Half Yearly 23Nilima Aparajita SahuОценок пока нет
- Development Developmental Biology EmbryologyДокумент6 страницDevelopment Developmental Biology EmbryologyBiju ThomasОценок пока нет
- Phytotherapy On CancerДокумент21 страницаPhytotherapy On CancerSiddhendu Bhattacharjee100% (1)
- Activity Title: Learning Targets: Reference (S)Документ5 страницActivity Title: Learning Targets: Reference (S)Jhev LeopandoОценок пока нет
- JIS G 3141: Cold-Reduced Carbon Steel Sheet and StripДокумент6 страницJIS G 3141: Cold-Reduced Carbon Steel Sheet and StripHari0% (2)
- How To Block HTTP DDoS Attack With Cisco ASA FirewallДокумент4 страницыHow To Block HTTP DDoS Attack With Cisco ASA Firewallabdel taibОценок пока нет
- Assessment of The Genitourinary System: GeneralДокумент2 страницыAssessment of The Genitourinary System: GeneralMaharani UtamiОценок пока нет
- Z-Purlins: Technical DocumentationДокумент11 страницZ-Purlins: Technical Documentationardit bedhiaОценок пока нет
- Modlist - Modlist 1.4Документ145 страницModlist - Modlist 1.4Tattorin vemariaОценок пока нет
- 2022 WR Extended VersionДокумент71 страница2022 WR Extended Versionpavankawade63Оценок пока нет
- Pathology of LiverДокумент15 страницPathology of Liverערין גבאריןОценок пока нет
- Miguel Augusto Ixpec-Chitay, A097 535 400 (BIA Sept. 16, 2013)Документ22 страницыMiguel Augusto Ixpec-Chitay, A097 535 400 (BIA Sept. 16, 2013)Immigrant & Refugee Appellate Center, LLCОценок пока нет