Академический Документы
Профессиональный Документы
Культура Документы
1989 Moller
Загружено:
Irfan MohammadАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
1989 Moller
Загружено:
Irfan MohammadАвторское право:
Доступные форматы
Int. J. Gynecol. Obstet.
, 1989,30: 123-131
123
International Federation of Gynecology and Obstetrics
A study of antenatal care at village level in rural Tanzania
B. Moller*, 0. Lushinod,
0. Meirikb, M. Gebre-Medhin
and G. Lindmark
Apartments of Obstetrics and Gynecology, %cial Medicine and =Pediatrics, Uppsala University, Akademiska Sjukhuset, Uppsala
(Sweden) and *Muga Regional Hmpitai, Iringa (Tanzania)
(Received August 31s~ 1988)
(Revised and accepted November 4th. 1988)
Abstract
Antenatal care is an acknowledged measure for the reduction of maternal and
perinatal mortality. In the rural village of
Ilula, Tanzania, the possible impact of
antenatal care on mortality was studied longitudinally on the basis of the 707 women delivered in the study period. Ninety-five percent
of the antenatal records were available.
Anemia, malaria and anticipated obstetric
problems were the most frequent reasons for
interventions. Among the women from the
area who were delivered in hospital, 90% had
been referred there. No relationship was
found between the number of antenatal visits
and the pregnancy outcome, but perinatal
mortality was correlated to a low birth
weight. Even with a mean attendance rate of
six visits and full coverage by antenatal care
maternal and perinatal mortality remains
high.
Keywords: Prenatal care; Developing country; Health care research; Perinatal mortality;
Twin diagnosis; Breech presentation.
Introduction
Antenatal care (ANC) emerged in its basic
form 50 years ago in Europe [l]. Although
0020- 7292/ 89/ $03. 50
0 1989 International Federation of Gynecology and Obstetrics
Published and Printed in Ireland
this model generally has been adopted in
developing countries, the health problems
noted there are quite different. In Tanzania,
for example, the maternal and child health
(MCH) services operate with limited material
and manpower resources. At a time when the
effectiveness of ANC is being questioned in
European countries by consumers and care
providers alike [2,3], it is prudent to assess the
effectiveness and relevance of various parts of
the ANC part of the MCH organization in
developing countries, including Tanzania.
In 1984 a joint WHO/Tanzanian study on
primary health care [4] reported a mean 95%
registration rate to ANC in seven regions,
with at least one visit to the MCH during
pregnancy. The average number of visits during pregnancy was 4.3, with pronounced
variations between the studied regions. Shears
and Mkerenga [5] analyzed the impact of
mobile MCH services on the maternal health
and pregnancy outcome in several villages of
Tanzania, mainly in the northern part. They
concluded that the MCH services had only
limited influence on the principal problems of
maternal health and nutrition.
The present study analyzes antenatal care
service at the village level in an area where
ANC coverage and attendance are good. It is
based on an evaluation of the actual contents
of the care in terms of detection of complicaClinical and Clinical Research
124
Moller et al.
tions, interventions and patient compliance
relative to pregnancy outcome. To our knowledge such an area-based, prospective study
has not been performed in Tanzania or, for
that matter, in any other developing country.
Materials and methods
Subjects
Between June 1, 1983 to November 30,
1985 all women from the village of Ilula who
delivered at, or attended the antenatal clinic
in Ilula were eligible for enrollment. Of a
total 719 women, 685 were enrolled at a visit
to the antenatal care clinic in Ilula and 34
when they were delivered, shortly after the
study commenced.
The Ilula mission dispensary is staffed by a
village midwife, trained as an MCH aide,
assisted by another MCH aide and the locally
All women
trained
MCH
attendants.
delivered at home (230/o), in the dispensary
(68%) or in the Iringa Regional Hospital
(9Vo) 47 km away. The distance from the
mothers home to the dispensary did not
exceed 6 km for any of the women in the
study population.
Methods
The village midwife undertook the data
collection. She was known by the villagers for
many years, and she knew the women in the
two villages well and enjoyed their respect.
The national antenatal record was used. After
childbirth an extensive questionnaire
was
completed by the midwife during an interview
with the mother. This information served to
validate some data from the antenatal card.
The obstetric history was recorded at the
first antenatal visit. The national Swahili
action-oriented antenatal card [6] has tick
boxes to note risk factors present at
registration or detected at subsequent visits.
When risk factors are present, instructions
adjacent to the boxes explain the nature and
timing of appropriate actions, namely referral
for consultation or for institutional delivery
at a hospital or a health center. Specified risk
Int J Gynecol Obstet 30
factors include previous cesarean section or
poor pregnancy outcome, grand multiparity,
maternal bleeding or hypertensive disorders,
maternal height under 150 cm, fetal malpresentation and post-term pregnancy. The card
also provides separate space for notes on the
dispensing of iron, folic acid and antimalarials. Reasons for referral are noted
and the back of the card is used as the delivery
record. The mothers keep their antenatal card
themselves. The women were instructed to
give the antenatal card to the village midwife
subsequent to delivery or abortion.
The mothers were examined at each visit,
and their weight, blood pressure, any edema,
general health status and the date of their next
visit were noted.
Blood pressure
was
measured in the sitting position with an
aeroid sphygmomanometer.
Complications
and interventions are noted as they occur.
Tetanus
vaccinations
and
prophylactic
medication with iron, folic acid and antimalarial agents are formally parts of the
List of complications during pregnancy divided in
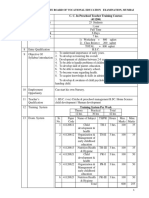
Table I.
symptoms and signs as noted at the 4392 antenatal visits to the
MCH.
No.
of
notes
notes
100
38
10
9
16
34
13
3
3
7
5
14
53
2
18
1
30
10
Symtoms
(a)Abdominal pain, backache, headache,
leg pain
(b) Fever, malaria
General illness, other
Vaginal bleeding
Vaginal discharge, local vaginal disorder
Urinary tract infection, diarrhea
Premature labor, premature rupture of
the membranes
g&W
(c) Anemia, clinicrd diagnosis
Hb<8.5g/lOOml
Pre-eclampsia
Fetal complications: malpresentation.
twinning, fetal distress etc.
Total
20
292
Frenatat care evaluation
Table II.
125
Documented interventions during pregnancy related to length of gestation.
Interventions
Gestational age (weeks)
32-35
Total
Qs of
total
21
28-3 1
Medication (at Ilula dispensary)
Admitted to Hula dispensary
Referrals
For blood transfusion
For consultation of doctor
For hospital admission
For hospital delivery
12
3
10
2
9
4
8
2
3
2
42
13
30
9
2
1
I
3
1
1
2
11
7
2
21
7
5
1
2
18
3
38
18
26
2
27
13
19
Total
18
18
35
43
26
140
100%
program. Fever and general malaise are
regarded as malaria. The diagnosis of anemia
is usually made on clinical impression. Laboratory determination
of hemoglobin most
often was not available.
At the conclusion of the study period,
antenatal cards were scrutinized for notes on
symptoms
and signs, complications
of
pregnancy and interventions.
The information
was coded
and computerized.
Complications were classified in symptoms
and signs, according to Table I. Interventions
were categorized as local interventions or
referrals to hospital (Table II). Referral to a
doctor in the Iringa Regional Hospital for
assessment or admission was a common intervention, either during pregnancy or from the
delivery ward of the dispensary, mostly during labor.
36-39
Data analysis
This analysis is based on the 683 available
antenatal cards, which corresponds to 95% of
the 719 pregnant women enrolled in the
study. The reasons for missing cards were as
follows: six patients had mislaid their cards,
five mothers were lost to follow-up, four
mothers had moved from the area, one
negated antenatal care and 20 cards were lost
in other ways. Judging from other sources of
information, such as the questionnaire, the
log-book and personal communication with
the staff, the utilization of antenatal care in
these groups did not seem to be different
from that of the analyzed population.
Information on hospital deliveries was supplemented with followup information when
the card was not available. Five of the women
with a lost card had hospital deliveries.
Length of gestation at successive visits for all attenders and for attenders divided into two groups according to the
Table III.
number of visits (gw = gestational week).
Length of gestation (weeks) at visit
For all attenders
For women attending five times
or less
For women attending six times
or more
1st gw
Zndgw
3rdgw
4thgw
5thgw
6thgw
7thgw
8thgw
!Jthgw
1Othgw
22
26
30
33
35
36
38
39
40
41
25
29
33
35
31
20
25
29
32
35
36
38
39
40
41
Clinical and Clinical Research
126
Moller et al.
Results
Registration and intervals between visits
The mean
length
of gestation
on
enrollment was 23 weeks, with a range of 634. The number of visits averaged 6.4, with a
range from 1 to 14. Eighty-six percent of the
women had made more than two visits. The
average week of pregnancy for each successive visit is given in Table III. The average
weeks of the visits have been tabulated separately for women with six visits or more and
for those with five visits or fewer. Women
who made five visits or fewer during the span
of pregnancy registered at the ANC clinic in
the 25th week, on average, and delivered at an
average of 38.2 weeks. Half the visits were
made before 33 weeks, and half after.
Clinical findings at antenatal visits
At the 4392 visits by the 685 women, 292
complaints or complications
were noted.
Complaints such as abdominal pain, headache, backache and heaviness without accompanying objective signs were noted in 100
cases, but were not premonitory signs of an
adverse outcome, except in one case of prematurity in week 31. Abdominal pain was
Table IV.
Noted complications related to length of gestation
at diagnosis.
Complications
Fever, general
illness
Vaginal bleeding
Rupture of
membranes
Anemia
Hypertension
Twins, breech
presentation
Total
Gestational age (weeks)
Total
UP
to
28-31
21
32-35
36-39
40
12
3
12
1
10
3
4
1
48
9
8
11
2
9
1
14
53
2
2
21
10
1
12
1
24
41
29
41
31
150
Int J Gynecol Obstet 30
generally poorly defined and might mean discomfort, anxiety or uterine contractions.
Only when accompanied by other symptoms
or signs was it associated with an adverse outcome. The distribution of complications over
time is shown in Table IV.
In addition, 12 women had had a cesarean
section in a previous pregnancy. Seven of
these were delivered in hospital, and four had
a cesarean section delivery this time. Of all
parturients, primigravidae constituted 17%.
Thirteen percent of primigravidae were delivered in the hospital and 71% in the dispensary. Of all pregnant women, 24 (3.4%) were
shorter than 150 cm. Forty percent of the 24
were delivered in hospital.
There were 38 febrile episodes presumed to
be malarial attacks in the antenatal cards, but
at the interview after delivery 171 patients
gave a history of having had malaria during
pregnancy. In this regard, less than a quarter
of malarial attacks were treated at the
antenatal clinic; most patients were treated at
other times at the out-patient department of
the dispensary.
A total of 4240 blood pressure (BP) measurements were made in the study period.
Readings were nearly always recorded to the
nearest multiple of ten. The mean antenatal
pressure was 100/65 mmHg and this did not
vary over pregnancy. Throughout pregnancy
8-10070 of the diastolic readings were 80
mmHg or over, but only 14 readings (0.3%)
were 85 or more. Twenty-nine (0.6%) of the
systolic pressure readings were over 120
mmHg.
Only two patients were referred to hospital
because of an elevated BP reading at a regular
visit. An additional four patients were sent
from the dispensary in labor because of
hypertensive complications. The diastolic BP
at the previous visit to MCH had not
exceeded 80 mmHg for any of the four. However, two of these women had had eclampsia
at the dispensary.
Sixty-four percent of the 58 diagnoses of
anemia were made before the 32nd week, the
majority by inspection of the mucous mem-
Prenatal care evaluation
Hemoglobin values obtained from 152 consecutive
Table V.
antenatal care attenders in Ilula.
Hemoglobin value (g/l)
Readings 070
<85
85-99
100-114
115-129
> 130
33
38
19
branes and not confirmed by laboratory
measurements.
Hemoglobin
values were
checked in a group of patients (n = 152)
participating in concomitant nutritional studies. The distribution of the hemoglobin values
recorded in this group is given in Table V.
Most anemic patients were prescribed
ferrous tablets, generally in inadequate
amounts, as the supplies seldom matched the
demands. Three patients had blood transfusions at the hospital because of anemia
[l] and antepartum hemorrage [2].
Interventions
Interventions resulted from symptoms or
findings. A total of 140 interventions were
documented (Table II). Local interventions
were most commonly medication for malaria,
anemia and other illnesses. Of a total of 95
Table VI.
Hospital deliveries (n = 67, 61 referred, 6 not
referred) and the indications for referral.
Reasons for referral
Referred
From ANC
Malposition, twins, big baby
Previous cesarean section
Anemia
Premature rupture of membranes
Hypertension (2 eclampsia)
Lack of progress in labor
Postmaturity
Local vaginal disorder
Miscellaneous
Unknown
Referred
4
1
6
3
43
referrals, only 85 were actually activated
(Table II). The main indications for referral
to a doctor were pelvic assessment of
primigravidae, twinning, malpositions and
anemia.
Twenty-two of 119 primigravidae
had
pelvic assessment. Of 13 primigravidae 150
cm or under, two had pelvic assessment and
later were delivered by cesarean section at the
hospital. Among 11 remaining short women,
four had normal delivery at home, five delivered at the dispensary, and two delivered at
hospital, one having cesarean section and one
vacuum extraction.
Of all referred patients, 43 delivered in
hospital (Table VI). Another 18 referrals for
hospital delivery were made from the
dispensary of patients in labor. Six of the 67
mothers delivered in hospital had gone there
of their own choice without having been
referred.
Antitetanus vaccination is provided as a
basic immunization for those previously not
vaccinated and as a booster dose for
previously vaccinated women. The coverage
by immunization was 80%. Prophylactic antimalarials and hematinics were provided very
irregularly and clearly not to the extent
intended in the national ANC program.
Twins, breech presentation
Of the 25 twin pregnancies (Table VII), 16
were correctly suspected or diagnosed at an
Table VII.
Twins and breech presentations.
In labor
14
6
5
2
2
1
2
18
127
Correctly diagnosed in
antenatal clinic (olo)
Diagnoses at delivery (olo)
Hospital delivery (Vo)
Birth weight < 2000 g
Mean birth weight (g)
Perinatal mortality rate (Vo)
Twin
pregnancies
(n = 25)
Breech
presentations
(n = 17)
64
36
20
15
21m
28 (14150)
47
53
53
3
2635
53 (9/17)
*Birthweight was known for 44 twins and 12 breech-delivered
infants.
Clinical and Clinical Research
128
Moller ef al.
Table VIII.
Number of antenatal visits in relation to
pregnancy outcome. The table is based on the 683 women for
whom an antenatal card was available (PMR = perinatal mortality rate).
Visits
l-2
No. of patients
Abortions
Deliveries
Mean gestational age at
delivery (weeks)
Birth weight < 2000 g
Mean birth weight (g)
Perinatal deaths
PMR/lOOO
41
7
34
3-4
126
3
123
5-6
187
0
187
>6
329
0
329
Total
6.4
(mean)
683
10
673
37
38
39
40
39.4
8
8
5
0
21
2492 2877 2958 3195 3011
9
9
12
12
42
260
73
64
37
63
average gestational age of 31 weeks. Five
mothers had an X-ray to confirm the diagnosis. Of the 16 women with twin pregnancies
diagnosed antepartum, six delivered at home,
and five (20%) were sent to the referral hospital.
Breech presentation was correctly diagnosed in 8 of 17 cases. Five of these 8 women
had hospital delivery. Because four women
with undiagnosed breech presentation were
referred to hospital for other reasons and
delivered there, nine of the 17 breech presentations (53%) were delivered in hospital.
Number of visits andpregnancy outcome
The outcome related to the numbers of visits is shown in Table VIII. As half of the visits
took place before 33 weeks and subsequent
visits were more closely spaced, women with
premature deliveries had fewer visits. The
high perinatal mortality rate in the low birth
weight groups occurred in women with few
visits. Eight of the nine perinatal deaths in the
group with one or two visits to the ANC clinic
occurred in babies with a birth weight below
2000 g. Evidently the high mortality in the
groups with few visits was associated with a
low birth weight and prematurity.
There were four maternal deaths in this
study. They all occurred in term deliveries
Int J Gynecol Obstet 30
around the time of delivery. In no case could
the outcome
be linked to insufficient
antenatal care, nor was any abnormality
noted during pregnancy.
Discussion
Many components of antenatal care, especially health education and social support, are
difficult to evaluate. In contrast, other
components such as the correct diagnosis of
breech presentation
and twins, site of
delivery, referral patterns and the numbers of
antenatal visits can easily be quantitated. The
Tanzanian national antenatal card [6] was
designed as an instrument to help reduce
maternal and perinatal deaths. This study
demonstrates its additional use for health
service research. Ninety-five per cent of the
cards were available for analysis in this study,
compared with 87% in a similar study in
Aberdeen [7].
Clinical findings at antenatal visits
Some complication or complaint was noted
in 7% (292/4392) of antenatal visits. One
third
concerned
mainly
physiological
inconveniences of pregnancy of no clinical
importance (Table IIa), usually eliciting no
action other than possibly short courses of
symptomatic medication. In general, staff of
busy clinics in many countries pay little heed
to these problems
[3] although
it is
important for the women to be treated with
sympathy in this respect. In 107 instances,
however, symptomatic complications
were
noted (Table IIb). These conditions led the
patient to seek medical care even though a
visit was not scheduled. Eighty-five women
(Table 11~)had a diagnosis of generally symptomless conditions,
mainly
anemia
or
abnormal presentation detected through the
routine monitoring of pregnancy.
Unfortunately
clinical examination does
not always lead to identification of multifetal
pregnancy
or breech presentation.
For
example, the frequency of correct twin
diagnosis in antenatal care was 60% in Swe-
Prenatal care evaluation
den in 1971 [8], before ultrasound or biochemical indicators were used routinely,
suggesting that the 64% detection rate of
twins in Ilula is the rate that can be attained in
routine clinical work without the use of
sophisticated techniques. The breech detection rate of 47% is comparable to the
61% detection rate of term breeches in San
Francisco between 1976 and 1984 [9].
Considering that some breech deliveries in
Ilula were preterm, this detection rate is
reasonable. The value of prelabor diagnosis is
particularly great in view of the perinatal
mortality of 50% and the skill required to
handle breech and multifetal deliveries in the
best of circumstances. As this skill generally is
available only at institutions, patients with
breech presentation or multifetal pregnancy
should be made aware of the importance of
institutional delivery.
Antenatal referrals
Only every fifth primigravida was sent to a
medical officer for pelvic assessment, and
only two of the 13 short primigravidae were
assessed. That all but one of the assessed
women
also had institutional
delivery
probably better indicates that these women
were prone to comply with staff recommendations
than that they were especially at risk. The majority of primigravidae
did not have pelvic assessment, and its value
as part of antenatal monitoring of pregnancy
must be questionned.
Medical actions at the MCH clinic
The prophylaxis and treatment of anemia
and malaria are important ingredients of
ANC. Most febrile illnesses are considered to
be malaria and treated accordingly without
examination. Three quarters of all febrile episodes occurred outside scheduled visits to the
MCH and were treated elsewhere. When
defined according
to WHO (< lOOg/l),
anemia was found to be present in 14 women,
or 10% of the sample. This frequency is considerably lower than the 45% reported from
Mozambique [lo] and the 20% from the
129
Ivory Coast [ 111. Although the diagnosis of
anemia by clinical inspection is inaccurate
[12], laboratory confirmation is often not
feasible. The use of prophylactic medication
by all pregnant women or at least those displaying signs of anemia, should constitute a
more important part of antenatal care than
was seen here.
Weight and blood pressure recordings
A considerable amount of time and effort
is spent on recording the body weight and
blood pressure of every expectant mother at
each visit. Maternal weight and its relation to
birth weight will be reported elsewhere [ 131.
In routine clinical work, the findings at
weighing mothers at each visit rarely alter
their management, and this practise was even
discarded by Essex et al. [6].
The yield of blood pressure measurements
was particularly low. Ilula is an area with a
relatively low rate of eclampsia. The two
cases of eclampsia were not detected in the
pre-eclamptic
stage. The remaining
few
hypertensive patients were identified through
concomitant or incidental clinical symptoms
rather than by blood pressure recordings. The
detection rate might be increased, with less
waste of time, by performing blood pressure
recordings at each visit only in risk groups,
namely primigravidae, women with previous
pregnancy hypertension and those with a high
blood pressure at the first visit. Tests for
albuminuria in these cases should be given
priority, and when diagnostic tools are scarce,
they should be saved for these cases.
Prophylactic medication
One of the stated purposes of antenatal
care is to provide prophylactic medication for
the prevention of some complications such as
anemia and malaria. Also, neonatal tetanus is
prevented by maternal immunization. Logistic problems make this part of ANC vulnerable and insufficient [14]. Of medications and
vaccinations, only the antitetanus vaccination
program worked fairly well, while hematinics
and anti-malarial agents very often were not
Clinical and Clinical Research
130
Moller et al.
available. This important goal of the national
preventive program has not nearly been
reached.
Number and timing of antenatal visits
Several reports [15-171 show a correlation
between frequent attendance at an antenatal
clinic and a good pregnancy outcome.
However, these studies suffer from two major
weaknesses. One is the problem of self-selection by mothers registering for antenatal care,
and the other is that the quality of the care is
not assessed [ 181. In most European countries
a full antenatal program comprises lo-12
visits. The recommendations for the spacing
of visits vary considerably, however, but
according to Blonde1 [19] outcome as measured in national perinatal mortality is not
related to the number of antenatal visits.
In this study we found an association
between the outcome of pregnancy and the
number of antenatal visits. We question,
however, the causality of this association. If
the preterm and low birth weight babies with
their high mortality are taken into account,
an independent effect of the number of
antenatal visits is no longer obvious. Unfortunately, prematurity and low birth weight
are usually not preventable through antenatal
care other than possibly by treating malarial
episodes and other infections.
Early enrollment for antenatal care has
long been encouraged. The purpose of this
early attendance is to permit the detection and
treatment of maternal diseases such as anemia, syphilis and tuberculosis and to allow a
better dating of pregnancy. Unless screening
for these conditions is actually practised, the
justification of early enrollment fails.
Structured programs
To improve results within the framework
of programs with limited resources, greater
emphasis should be placed on quality rather
than on quantity in antenatal care. Structured
programs based on local priorities ideally
should optimize the use of scarce resources.
In her account of the setting in Scotland, Hall
Int J Gynecol Obstet 30
[2] suggests a reduction in the number of
planned visits for normal multigravidae to
four. Primigravidae should be followed up
according to the traditional
programme
because of their higher risk of hypertensive
disorders.
In the case of Tanzania, programs may be
worked out along the same goal-oriented
lines. A few visits will be enough to detect
most risk factors. Some women with risk
factors will need closer monitoring.
All
women
should
be advised
to report
immediately should complications such as
bleeding occur. Most gravidae will benefit
from a program in which the aim of all
scheduled visits is defined and clearly stated.
Improved attention to individual and group
instruction, especially of women at high risk
such as women with multifetal pregnancies
and breech presentations,
should assist in
improving pregnancy outcome. To increase
compliance, women should be made aware of
their personal risk factors [20].
The present organization of MCH clinics in
Tanzania is such that women bring their
children and all parties receive regular health
education. Visitors to MCH clinics have been
found to be very receptive audiences [5]. An
appropriately compiled collection of centrally
prepared short health education programs
will help the MCH staff in this task [21].
Limits of antenatal care
In this study, the main causes of perinatal
death were prematurity and LBW births. In
the absence of resources for referral to a hospital and/or of an effective preventive medication program, one can speculate if perinatal
mortality rates can be lowered by significantly
more frequent routine antenatal visits.
Other determinants of pregnancy outcome
clearly are present. Social factors such as
female work load and nutrition, from childhood onwards, also influence the outcome of
pregnancy and probably are just as important
as those risk factors that might be mitigated
by specific actions taken in antenatal care.
In conclusion, our assessment of the effec-
Prenatal care evaluation
tiveness of the antenatal services in a rural
setting in Tanzania has shown that despite
good coverage of the pregnant population by
a popular antenatal service, maternal and
perinatal mortality rates remain high, apparently not affected by the frequent antenatal
monitoring. One probable reason for this is
that perinatal mortality is largely associated
with prematurity and low birth weight, both
of which cannot be easily influenced simply
by checking mothers for risk factors.
On the other hand, the present system
of
antenatal
care
provides
excellent
opportunities to reach mothers with prophylactic medication, vaccinations, and diagnosis
and treatment of infectious diseases, and also
health education programs.
The present study suggests that more
emphasis should be placed on preventive
medical and social measures. Strengthening
of the referral capacity is also a necessity if
obstetric risk screening is to be made
worthwhile.
Acknowledgment
This study was supported by SAREC grant
81/79. We are indebted
to UNICEF,
Tanzania, for logistical support.
References
Wagner MG: Health services for pregnancy care in
Europe. Int J Technol Assess Health Care I: 789,1985.
Hall M: Antenatal care in practice. Spastics Int Med Public, London, 1982.
Garcia JO: Womens views of antenatal care. Spastics Int
Med Public, London, 1982.
Government of Tanzania/UNICEF:
An analysis of the
situation of women and children. Dar Es Salaam, 1985.
Shears F, Mkerenga R: Evaluating the impact of mother
and child health (MCH) services at village level, a survey
in Tanzania, and lessons for elsewhere. Ann Trop Pediatr
5: 55.1985.
131
6 Essex BJ, Everett J: Use of an action oriented record for
antenatal screening. Trop Dot 7: 134.1977.
7 Hall MH, Chng PK, MacGillivray I: Is routine antenatal
care worth while? Lancet ii: 78, 1980.
8 Grennert L, Persson PH, Gennser G, Kullander S:
Ultrasound and human placental-lactogcn
for early
detection of twin pregnancies. Lancet i: 4, 1976.
9 Flanagan TA, Mulchahey KM, Korenbrot CC, Green JR,
Laros KL: Management of term breech presentation. Am
J Obstet GynecolZ56: 1492,1987.
10 Boatin BA, Bulsara MK. Wurpa FK: Evaluation of
conjunctival pallor in the diagnosis of anaemia. J Trop
Med Hyg89: 33.1986.
11 Reinhart MC: A survey of mothers and their newborns in
Abijan, Ivory Coast. Helv Paediatr Acta Suppl 41, 33:
1978.
12 Wurapa FK, Bulsara MK, Boatin SA: Evaluation of conjunctival pallor in the diagnosis of anemia. J Trop Med
Hyg 89: 33,1986.
13 Moller BJ, Gebre-Medhin M, Lindmark G: Maternal
weight, weight gain and birth weight at term in the rural
Tanzanian village of Ilula. Br J Obstet Gynecol, in press.
14 Ministry of Health: Report on a study on patient
management, essential drugs and equipment supply. Tanzania, 1985.
15 Ryan GM: Prenatal care and pregnancy outcome. Am J
Obstet Gynecol137: 876. 1980.
16 Gorthmaker S: The effects of prenatal care upon the
health of the newborn. Am J Public Health 69: 653, 1979.
17 Greenberg R: The impact of prenatal care in different
social groups. Am J Obstet Gynecol145: 797,1982.
18 Helliger FJ: Prenatal care, neonatal intensive care and
infant mortality. J Technol Assess Health Care I: 934,
1985.
19 Blonde1 B: Some characteristics of antenatal care in 13
European countries. Br J Obstet Gynaecol 92: 565,1985.
20 WHO/UNICEF Joint Statement: Maternal care for the
reduction of perinatal and neonatal mortality. WHO,
Geneva, 1986.
21 Morley D: Communication and learning. In Pediatric
Priorities in Developing Countries, p 3%. Butterworth,
London, 1975.
Address for reprints:
G. Ltodmark
Dejnutment of Obstetrks and Gynecology
tJPplul8univemity
AludemisluS]nkbnset
s 75185 Sweden
Clinical and Clinical Research
Вам также может понравиться
- Jurnal GH TambuntaДокумент6 страницJurnal GH TambuntaIrfan MohammadОценок пока нет
- Dia Care-2015-Huang-746-51 PDFДокумент6 страницDia Care-2015-Huang-746-51 PDFMohammad IrfanОценок пока нет
- Antibiotic Treatment Strategies For Community Acquired Pneumonia in AdultsДокумент12 страницAntibiotic Treatment Strategies For Community Acquired Pneumonia in AdultsCumbelia PrimaОценок пока нет
- Introduction To Metabolism: Departemen Fisiologi Fakultas Kedokteran USUДокумент22 страницыIntroduction To Metabolism: Departemen Fisiologi Fakultas Kedokteran USUAnditha Namira RSОценок пока нет
- Managing Immune Thrombocytopenic Purpura: An UpdateДокумент7 страницManaging Immune Thrombocytopenic Purpura: An UpdateApriliza RalasatiОценок пока нет
- Diagnosis and Management of Clinical ChorioamnionitisДокумент18 страницDiagnosis and Management of Clinical ChorioamnionitisIrfan MohammadОценок пока нет
- Itp Periop1Документ4 страницыItp Periop1Irfan MohammadОценок пока нет
- Dia Care 2015 Krul Poel 1420 6Документ7 страницDia Care 2015 Krul Poel 1420 6Irfan MohammadОценок пока нет
- K 19 20 Metabolism RegulationДокумент29 страницK 19 20 Metabolism RegulationIrfan MohammadОценок пока нет
- Itp Periop1Документ4 страницыItp Periop1Irfan MohammadОценок пока нет
- Dia Care 2015 Bellido 2211 6Документ6 страницDia Care 2015 Bellido 2211 6Irfan MohammadОценок пока нет
- Dia Care-2015-Siraj-2000-8Документ9 страницDia Care-2015-Siraj-2000-8Irfan MohammadОценок пока нет
- 1994 Al NasserДокумент9 страниц1994 Al NasserIrfan MohammadОценок пока нет
- CH08 Vaginal Breech DeliveryДокумент25 страницCH08 Vaginal Breech DeliveryShintaPuspitasariОценок пока нет
- Terapi AntiretroviralДокумент13 страницTerapi AntiretroviralthiamuthiaОценок пока нет
- 2005 HildingssonДокумент7 страниц2005 HildingssonIrfan MohammadОценок пока нет
- Normal Newborn CareДокумент49 страницNormal Newborn CareIrfan MohammadОценок пока нет
- 1987 ReebДокумент7 страниц1987 ReebIrfan MohammadОценок пока нет
- Maternal Anatomy WilliamsДокумент52 страницыMaternal Anatomy WilliamsIrfan MohammadОценок пока нет
- 1987 ReebДокумент7 страниц1987 ReebIrfan MohammadОценок пока нет
- Dia Care-2015-Zeitler-2285-92Документ8 страницDia Care-2015-Zeitler-2285-92Irfan MohammadОценок пока нет
- Dia Care 2015 Bellido 2211 6Документ6 страницDia Care 2015 Bellido 2211 6Irfan MohammadОценок пока нет
- ITP BJH 2003Документ23 страницыITP BJH 2003Mohammad IrfanОценок пока нет
- Antibiotic Treatment Strategies For Community Acquired Pneumonia in AdultsДокумент12 страницAntibiotic Treatment Strategies For Community Acquired Pneumonia in AdultsCumbelia PrimaОценок пока нет
- Guidline EndocarditisДокумент54 страницыGuidline EndocarditisIrfan MohammadОценок пока нет
- Copd NICE GuidlinesДокумент61 страницаCopd NICE GuidlinesIrfan MohammadОценок пока нет
- 2007 NiceДокумент249 страниц2007 NiceIrfan MohammadОценок пока нет
- HipoglikemiaДокумент12 страницHipoglikemiaIrfan MohammadОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- RCPI Diabetes GuidelinesДокумент88 страницRCPI Diabetes GuidelinesJohn Smith100% (1)
- Thesis Statement Opposing AbortionДокумент5 страницThesis Statement Opposing Abortionaflnbwmjhdinys100% (2)
- NCP Pain - OBДокумент5 страницNCP Pain - OBSandra Guimaray50% (2)
- Childbirth Education Then and NowДокумент5 страницChildbirth Education Then and Nowazida90Оценок пока нет
- Maternal Mortality 1-5Документ36 страницMaternal Mortality 1-5Samuel CrewzОценок пока нет
- 2B-C - Why Did Mrs X Died PDFДокумент19 страниц2B-C - Why Did Mrs X Died PDFReyna Chame GarcinezОценок пока нет
- Pre School Teacher Training Course. 1Документ19 страницPre School Teacher Training Course. 1MithileshОценок пока нет
- Safe Prevention of The Primary Cesarean Delivery - ACOGДокумент16 страницSafe Prevention of The Primary Cesarean Delivery - ACOGAryaОценок пока нет
- 05-Insurance Companies Policy-NewДокумент18 страниц05-Insurance Companies Policy-NewIBRAHIM ELSHOURAОценок пока нет
- Stugeron DosageДокумент5 страницStugeron Dosagetarcher1987Оценок пока нет
- Susana O. Pabinguit, B.S.N., R.N. DOH-Central VisayasДокумент58 страницSusana O. Pabinguit, B.S.N., R.N. DOH-Central VisayasRnheals Central Visayas100% (8)
- ANC Guideline PresentationДокумент42 страницыANC Guideline PresentationDeepak BamОценок пока нет
- AEMT - Obstetrics and Pediatrics Exam PracticeДокумент26 страницAEMT - Obstetrics and Pediatrics Exam PracticeEMS DirectorОценок пока нет
- ScizopheniaДокумент20 страницScizopheniaGogea GabrielaОценок пока нет
- Why Antenatal Care is EssentialДокумент4 страницыWhy Antenatal Care is EssentialChennulОценок пока нет
- Nihms 940015Документ50 страницNihms 940015Maria Salome Olortegui AceroОценок пока нет
- Duty Report 5.12.1978Документ55 страницDuty Report 5.12.1978Riyan W. PratamaОценок пока нет
- Lecture 10 - Reproductive SystemДокумент83 страницыLecture 10 - Reproductive SystemNiyanthesh Reddy100% (1)
- Stonecoal v3 Guidelines 2023-06-09Документ77 страницStonecoal v3 Guidelines 2023-06-09Entertainment Buddy'sОценок пока нет
- Determinants of First Antenatal Visit Timing Among Pregnant Women in Antenatal Care at Kampala International University Teaching Hospital, Western UgandaДокумент19 страницDeterminants of First Antenatal Visit Timing Among Pregnant Women in Antenatal Care at Kampala International University Teaching Hospital, Western UgandaKIU PUBLICATION AND EXTENSIONОценок пока нет
- OC Set B NEWДокумент18 страницOC Set B NEWmatrixtrinityОценок пока нет
- Calculation of Concentrate Requirement of A Dairy Cattle On The Basis of FatДокумент4 страницыCalculation of Concentrate Requirement of A Dairy Cattle On The Basis of Fatfarid khan100% (1)
- Assessing Fetal Wellbeing in PregnancyДокумент8 страницAssessing Fetal Wellbeing in PregnancyViviane Ńíáshéè Basod100% (1)
- Sepsis Neonatorum UpdatedДокумент87 страницSepsis Neonatorum Updated'Eduard Laab AlcantaraОценок пока нет
- Rle NST PPT DraftДокумент4 страницыRle NST PPT DraftJingie Leigh EresoОценок пока нет
- Prenatal Chart 2022Документ3 страницыPrenatal Chart 2022Dheeraj ChopadaОценок пока нет
- Midwifery and ObstetricsДокумент16 страницMidwifery and ObstetricsOdette Wayne BalatbatОценок пока нет
- Abortion Case StudyДокумент18 страницAbortion Case StudyJuan Miguel T. Magdangal33% (3)
- Sss Gsis LawДокумент57 страницSss Gsis LawBroy D Brium100% (1)
- Rheumatological Disorders in PregnancyДокумент61 страницаRheumatological Disorders in Pregnancydrsyan hamzahОценок пока нет