Академический Документы
Профессиональный Документы
Культура Документы
Cardiovascular Changes in Cardiogenic
Загружено:
Baso AgusofyangАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Cardiovascular Changes in Cardiogenic
Загружено:
Baso AgusofyangАвторское право:
Доступные форматы
Cardiovascular Changes in Cardiogenic
and Obstructive Shocks: Analysis Using
a Cardiopulmonary Simulation Model
M Giannessi1, NW Chbat2, A Albanese1, J Op Den Buijs3,
E Magosso1, M Ursino1
1
University of Bologna, Cesena, Italy
Philips Research North America, Briarcliff Manor, NY, USA
3
Mayo Clinic, Rochester, MN, USA
regulatory actions. Arterial hypotension activates the
baroreflex response, which causes an increase in
sympathetic drive and a reduction in vagal tone to the
heart, with consequent increase in total peripheral
resistance and heart rate (HR), as well as
venoconstriction. The fall in oxygen delivery, in turn,
may stimulate local regulatory mechanisms, able to
vasodilate coronary and brain circulations. In case of
severe heart failure resulting in arterial hypoxia, other
mechanisms can be put into action, such as the arterial
chemoreflex and the lung-stretch receptor mechanism
(consequent on respiratory changes). Of course, these
mechanisms interact in different ways, depending on the
severity of the cardiac insufficiency, on its aetiology and
on differences of the individuals.
The complexity of the relationships involved in shock
and the role of individual parameter changes, can be
better understood with the use of mathematical models
and computer simulations. In previous years, we
developed a comprehensive mathematical model of
systemic and pulmonary circulation integrated by the
short-term cardiorespiratory regulation [1]. The model is
able to simulate cardiovascular changes in different acute
stresses (like haemorrhage, hypoxia and hypercapnia)
[1,2].
In the last months, the previous work was further
developed to: i) include respiratory mechanics and
metabolic exchange; ii) use the extended model to
simulate conditions of clinical relevance in the ICU.
In the present work, the model is used to analyze the
cardiovascular changes occurring during two different
conditions leading to reduced cardiac efficiency: a
reduction in cardiac contractility (simulated decrease of
the end-systolic elastance of the left ventricle), and a
reduction in left-ventricle filling (simulated increase of
the pulmonary arterial resistance). Results illustrate the
correlation of the main cardiovascular changes with the
level of myocardial dysfunction and the size of the
pulmonary embolus.
Abstract
Conditions characterized by a fall in cardiac output
are associated with alterations in cardiopulmonary
variables and activation of cardiovascular and
respiratory control mechanisms. In order to study these
complex relationships, we developed a comprehensive
cardiopulmonary model consisting of a circulation, a
respiration and a metabolism block. In this work, the
model is used to simulate cardiovascular dynamics in
pathological conditions with an acute decrease in heart
function. In particular, two conditions are examined: the
first is characterized by a decrease in heart contractility,
simulated in the model via a reduction in the left
ventricular end-systolic elastance. The second consists in
an increase in pulmonary arterial resistance, associated
with pulmonary embolism. In conclusion, the proposed
model may be of value in clinical settings to illustrate the
complex relationship among cardiovascular variables.
1.
Introduction
Conditions characterized by a fall in cardiac output
(CO) represent a frequent cause of mortality and
morbidity, while their rapid diagnosis and efficient
treatment still represent a demanding task for physicians.
Shock, or acute hypotension, that accompanies this fall is
detectable in an intensive care unit (ICU) scenario.
However, shock can be caused by heart failure, or by
blood obstruction, loss, or infection. These four different
causes require very different therapeutic routes. Gaining
insight on the different shock types becomes then
clinically important. In this paper, we present simulation
results and analysis for cardiogenic shock (due to heart
failure) and compare it with published patient data, and
for obstructive shock (due to pulmonary emboli).
A reduction in CO induces a fall in systemic arterial
pressure and in oxygen transport, thus triggering
ISSN 02766574
457
Computers in Cardiology 2008;35:457460.
2.
used in building the model: inertances, which account for
inertial forces in blood (these are relevant in large arteries
only); resistances, which account for pressure energy
losses (this parameter is especially important in the
peripheral circulation) and capacitances, which represent
the blood volume stored in each compartment (this
parameter is especially relevant in the venous
circulation). Volume, in turn, is divided in an unstressed
volume, which does not stretch the vessel wall, and a
stressed volume (which causes stress in the wall, and
hence is associated with increase in internal pressure).
The reader can find more details, equations and
parameter values in former publications [1,2].
Short term regulatory mechanisms work via local
metabolic factors on peripheral resistances and through
the action of the autonomic nervous system. The latter
modulates several parameters via two major efferent
neural branches, i.e., the sympathoadrenergic and the
vagus. Vagal stimulation rises heart period. Sympathetic
stimulation causes vasoconstriction in arterioles and veins
(thus increasing peripheral resistances and decreasing
venous volumes), raises heart contractility, and increases
heart rate. Some vascular beds (splanchnic circulation,
skeletal muscle circulation and circulation in the other
extrasplanchnic districts) are very sensitive to
sympathetic stimulation. Conversely, the cerebral and
coronary circulations are independent of the autonomic
control mechanism. Finally, the sympathetic and vagal
neural branches, respond to several groups of afferent
influences, triggered by baroreceptors, chemoreceptors
and lung-stretch receptors.
The cardiopulmonary model (see Fig. 2) also includes
lung mechanics (with distinction among larynx, trachea,
bronchi and alveoli), metabolic exchange equations at the
alveoli and capillaries, and the control of respiratory rate
and tidal volume by central and peripheral
chemoreceptors.
Methods
The model includes four cardiac chambers with
ventricular contractility, pulmonary and systemic
circulations (see Fig. 1). The latter is subdivided into five
districts arranged in parallel (brain, coronary, skeletal
muscle, splanchnic and the remaining extrasplanchnic
vascular beds).
Figure 1. Hydraulic analog of the model in which
resistances are represented with restrictions and
compliances with expanded spaces. P, pressures; R,
hydraulic resistances; C, compliances; L, inertances; F,
flows; sa, systemic arteries; sp and sv, splanchnic
peripheral and splanchnic venous circulation; ep and ev,
extrasplanchnic peripheral and extrasplanchnic venous
circulation; mp and mv, peripheral and venous circulation
in the skeletal muscle vascular bed; bp and bv, peripheral
and venous circulation in the brain; hp and hv, peripheral
and venous circulation in the heart (coronary vascular
bed); la, left atrium; lv, left ventricle; pa, pulmonary
arteries; pp and pv, pulmonary peripheral and pulmonary
venous circulation; ra, right atrium; rv, right ventricle.
According to Fig. 1, the different compartments
include hemodynamics in the large arteries (systemic and
pulmonary), the peripheral circulation, and the venous
circulation. Three main kinds of lumped parameters are
Figure 2. Cardiopulmonary model diagram.
458
3.
step changes to the end-systolic elastance. Model results
(continuous line with dots) are compared with data from
Webb JG. et al. [3] (dashed line). The dashed lines
represent mean values of the different variables
monitored for 816 patients suffering cardiogenic shock.
Results
Though the model represents cardiopulmonary
dynamics with associated neural regulatory mechanisms,
here we are only perturbing the cardiovascular part of the
model and analyzing its response. Let us first clarify the
convention that variables means blood pressures, flows
and volumes, and parameters pertains to blood vessel
properties and geometry, i.e. the R, L, and C of the
different compartments defined earlier. The two shock
scenarios that were simulated refer to acute conditions,
and acute response only is what we analyze.
The first scenario is one of a cardiogenic shock. Please
refer to Fig. 3 for abbreviations of variables and results.
Six variables are shown which are important in assessing
the condition of an ICU patient in such a shock (acute
hypotension). The cardiopulmonary model has
parameters that would correspond to a 70 Kg male with
initial variables in the quasi-normal range (EF 55%, CO
5.3 L/min, HR 72 beats/min, and slightly elevated
systolic/diastolic 128/87 and PCWP 15 mmHg) and so
representing relatively stable patient conditions. The
parameters of the model may be changed manually or
automatically to represent different classes of patients or
a particular patient with changing conditions. In this
study, however, the parameters are held constant as to
represent a general nominal ICU population.
The results show that as the left ventricular (LV)
elastance worsens, blood pressure and corresponding CO
and EF fall precipitously, while the PCWP increases due
to blood backing up all the way to the pulmonary
circulation. HR also increases, which includes baroreflex
action trying to compensate for arterial blood pressure
drop. With a further deterioration of the LV contractility,
PCWP enters the 20 mmHg zone, which could cause
interstitial edema to be likely followed by pulmonary
edema. It is intuitively helpful to correlate the level of LV
contractility loss to corresponding values of the PCWP,
EF, and CO. No CO results were reported in the patient
study. The simulation results fall well within the range of
the population study. However, this real patient study has
only averaged values for all five variables shown in
dashed lines. According to the model, the patient
population had an average of more than 50% loss in LV
contractility. This loss could also be interpreted as
equivalent loss of contractility as other factors could have
contributed to the deterioration of these patients. A
population breakdown would have been helpful to assess
the severity of myocardial infarcts, comorbidities,
demographic information, etc.
Figure 4. Systemic pulse pressure vs contractility of the
left ventricle, computed with the model in steady state
conditions by performing several step changes to the endsystolic left ventricular elastance.
Figure 4 represents the pulse pressure, the difference
between systolic and diastolic pressures. Because the
contractility of the left ventricle is affected, then the endsystolic pressure and volume will worsen more than the
end-diastolic pressure and volume. Hence, the pulse
pressure, and EF, as expected, will fall. No pulse pressure
data was given in the patient study; however, a difference
between the two dashed lines of the systolic and diastolic
pressures of Fig. 3 would give an approximation of the
Figure 3. Plots of systolic arterial blood pressure (systolic
ABP), diastolic arterial blood pressure (diastolic ABP),
heart rate (HR), pulmonary capillary wedge pressure
(PCWP), ejection fraction (EF) and cardiac output (CO)
vs the contractility of the left ventricle, computed by the
model at steady state conditions by performing several
459
pressures, a reduction in CO and EF, and an increase in
heart rate up to 100-110 beats/min. PCWP increases with
worsening LV contractility but decreases with increasing
upstream pulmonary embolism. These changes make
physiological and clinical sense.
The cardiogenic shock results are further compared
(Fig. 3) with average values taken from a large data set of
cardiogenic shock patients [3]. This comparison shows
that the model can simulate the average cardiovascular
variables, not only in a qualitative but also in a
quantitative manner, assuming that the end-systolic
elastance is decreased to 1/4 or 1/5 of its normal value.
The results provide a quantitative indication of the degree
of ventricular contractility impairment, which can occur
in a typical cardiogenic shock patient, as a function of
important hemodynamic variables such as CO, EF, and
PCWP.
The present simulations describe only acute events
with corresponding short-term hemodynamic response at
different levels of parameter derangement (either in
systolic elastance or Rpa). However, long-term shock
effects which can progressively evolve with time and
involve a downstream spiral, in which ischemia could
progressively deteriorates heart function, which in turn
further worsens ischemia [4] may be attempted in future
work.
The present model can have various potential clinical
applications in cardiology by providing insight into:
interactions of cardiovascular variables (pressures, flows,
volumes), effect of parameters (vessel properties and
geometry) on hemodynamic stability, patient variability,
correlation of parameter impairment severity with crucial
cardiovascular variables, and finally possible therapeutic
what-if scenarios.
patients average pulse pressure value: around 30 mmHg.
Figure 5. Plots of the main cardiovascular variables vs
pulmonary arterial resistance (Rpa), computed with the
model in steady state conditions by increasing 50, 100
and 150 times the Rpa. Rpa values are normalized at the
basal value. Meaning of symbols is the same as in Fig. 3.
The second scenario is one of an obstructive shock,
where the pulmonary artery resistance (Rpa) is acutely
increased. An example of this condition would be a
saddle embolus, i.e. clogging of both pulmonary
arteries, while a lesser severity shock would block a
correspondingly lesser area of these arteries. The
diameter of the pulmonary artery is implicit in the
resistance (resistance is inversely proportional to the
fourth power of the diameter.) In this shock the acute
hypotension is not due to a malfunction of the left heart,
as in the previous simulated scenario. So we see from the
results in Fig. 5 that the EF falls only to 45% even after
150% increase in Rpa, while the CO falls much more (5.3
to 3 L/min), and so does blood pressure, due to the fact
that less blood is reaching the left heart. HR also
increases here in order to compensate for the hypotensive
condition. PCWP falls since the obstruction occurs
upstream from it, and hence less blood reaches the
pulmonary capillaries. There were no patient results
available in the literature for this scenario. However, a
search is underway to obtain more patient data.
4.
References
[1] Ursino M, Magosso E, Acute cardiovascular response to
isocapnic hypoxia. I. A mathematical model, Am. J.
Physiol Heart Circ. Physiol, vol. 279, no. 1, p. H149-H165,
July2000.
[2] Magosso E, Ursino M, A mathematical model of CO2
effect on cardiovascular regulation, Am. J. Physiol Heart
Circ. Physiol, vol. 281, no. 5, p. H2036-H2052, Nov.2001.
[3] Webb JG, Kelly RF, Epidemiology of Cardiogenic Shock.
In: Hollenberg SM and Bates ER. Cardiogenic Shock.
United Kingdom: Blackwell Futura, 2002: chapter 1.
[4] Hollenber SM, Cardiogenic shock, Crit Care Med. 17: 391410, 2001.
Address for correspondence:
Massimo Giannessi
via Venezia 52, 47023 Cesena (FC), Italy
massimo.giannessi@unibo.it
Discussion and conclusions
The presented results demonstrate that the model is
able to simulate the main acute cardiovascular changes
due to cardiogenic and obstructive shocks quite well.
These include a fall in systolic, diastolic, and pulse
460
Вам также может понравиться
- (O. Nelson) Small Animal CardiologyДокумент208 страниц(O. Nelson) Small Animal CardiologyLoredana Gutu100% (1)
- Department of Education: Summative Test in Science ViДокумент5 страницDepartment of Education: Summative Test in Science Viricsha masanay100% (4)
- Small Animal Cardiology PDFДокумент208 страницSmall Animal Cardiology PDFRoberto AmpueroОценок пока нет
- Gastrointestinal Physiology, JohnsonДокумент310 страницGastrointestinal Physiology, JohnsonSubhajit Chakraborty80% (5)
- 2.1.1 Reproductive Systems Teacher Answer SheetДокумент3 страницы2.1.1 Reproductive Systems Teacher Answer SheetFerdi Hasan100% (1)
- Nervous System Practice QuestionsДокумент7 страницNervous System Practice QuestionsOsama AlhumisiОценок пока нет
- Abdo Pelvis McqsДокумент21 страницаAbdo Pelvis Mcqsmohankseb100% (2)
- Nervous System NotesДокумент21 страницаNervous System NotesLasalle BenavidesОценок пока нет
- Central Venous Pressure: Its Clinical Use and Role in Cardiovascular DynamicsОт EverandCentral Venous Pressure: Its Clinical Use and Role in Cardiovascular DynamicsОценок пока нет
- Controlled Hypotensive AnesthesiaДокумент24 страницыControlled Hypotensive AnesthesiaSuresh Kumar100% (1)
- Assessment of Systemic Lupus ErythematosusДокумент13 страницAssessment of Systemic Lupus ErythematosusBaso AgusofyangОценок пока нет
- 5 - Cardiac Output - Ass. Prof. Dalia Abd El-Salam - 2020Документ6 страниц5 - Cardiac Output - Ass. Prof. Dalia Abd El-Salam - 2020Hossam BaniisОценок пока нет
- Pathophysiology of Cardiogenic Pulmonary EdemaДокумент8 страницPathophysiology of Cardiogenic Pulmonary EdemaLili Fiorela CRОценок пока нет
- Lecture 14-Oct.23 Haemodynamics of Circulation, Circulatory Mechanics, ResistanceДокумент29 страницLecture 14-Oct.23 Haemodynamics of Circulation, Circulatory Mechanics, ResistanceAparmitОценок пока нет
- 15 CerebrumДокумент32 страницы15 CerebrumMédecin Adrian TGОценок пока нет
- Funk2013 1Документ7 страницFunk2013 1BiancaPancuОценок пока нет
- Cardiovascular and Autonomic Influences On Blood Pressure: John E. Jones,, Aruna R. Natarajan,,, and Pedro A. JoseДокумент23 страницыCardiovascular and Autonomic Influences On Blood Pressure: John E. Jones,, Aruna R. Natarajan,,, and Pedro A. JoseLulu LuwiiОценок пока нет
- Pathophysiology / Pharmacology: Cardiac PhysiologyДокумент6 страницPathophysiology / Pharmacology: Cardiac Physiologyjazzdoc007Оценок пока нет
- Chapter 7 Regulation of Arterial Blood Pressure and MicrocirculationДокумент20 страницChapter 7 Regulation of Arterial Blood Pressure and Microcirculationaisyahasrii_Оценок пока нет
- Previous Sectionnext SectionДокумент19 страницPrevious Sectionnext Sectionbaiq_permataОценок пока нет
- Venous Return in Critical IllnessДокумент15 страницVenous Return in Critical IllnessInês MendonçaОценок пока нет
- Blood Pressure RegulationДокумент3 страницыBlood Pressure RegulationiMaibelle BelleОценок пока нет
- Bondgraph Published CardioVascular 5Документ24 страницыBondgraph Published CardioVascular 5AhmedОценок пока нет
- Heart Failure and AnaesthesiaДокумент7 страницHeart Failure and AnaesthesiaShinta RizkyОценок пока нет
- Peer Review Process: Author: Section Editor: Deputy EditorДокумент14 страницPeer Review Process: Author: Section Editor: Deputy EditorLuis Enrique Caceres AlavrezОценок пока нет
- Distribution of Blood Flow at Rest and at ExerciseДокумент5 страницDistribution of Blood Flow at Rest and at ExerciseMohammad AliОценок пока нет
- Dar o No Dar Fluidos 2012Документ8 страницDar o No Dar Fluidos 2012césar_campos_45Оценок пока нет
- Blood Flow ECMДокумент31 страницаBlood Flow ECMirene :]Оценок пока нет
- Central Mechanisms Cardiovascular System Short and Long TermДокумент12 страницCentral Mechanisms Cardiovascular System Short and Long Termsilvio da costa guerreiroОценок пока нет
- Pleth Variability Index (PVI)Документ4 страницыPleth Variability Index (PVI)leagagaОценок пока нет
- 2007 Vol2 (5) No1 pg56-64Документ9 страниц2007 Vol2 (5) No1 pg56-64Vebby 'bee' AstriОценок пока нет
- II-A ShockДокумент5 страницII-A ShockMuhammad075Оценок пока нет
- Congestive Heart Failure: Martin M. ZdanowiczДокумент6 страницCongestive Heart Failure: Martin M. ZdanowiczAnonymous wpUzJBОценок пока нет
- Fisiopatologia Del Shock Cardiogenico Por Iam PDFДокумент12 страницFisiopatologia Del Shock Cardiogenico Por Iam PDFYESSICA CARENALGAОценок пока нет
- CHF PathophysiologyДокумент4 страницыCHF PathophysiologyVirtudazo JessaОценок пока нет
- The Conduit Artery Functional Endpoint CAFE StudyДокумент6 страницThe Conduit Artery Functional Endpoint CAFE StudyKaren AmolozaОценок пока нет
- Sirosis Kardiomiopati Journal 2006Документ0 страницSirosis Kardiomiopati Journal 2006Chindia BungaОценок пока нет
- Cardiovascular Physiology: The Autonomic Nervous SystemДокумент8 страницCardiovascular Physiology: The Autonomic Nervous SystemRidha Surya NugrahaОценок пока нет
- Assessment and Management of Shock A Nursing PerspectiveДокумент21 страницаAssessment and Management of Shock A Nursing PerspectiveDiane Abanilla100% (1)
- Front Page: Effects of Systemic Vascular Resistance On The BodyДокумент1 страницаFront Page: Effects of Systemic Vascular Resistance On The BodyRodel Aguila SañoОценок пока нет
- Neurohormonal Hypothesis in Heart FailureДокумент11 страницNeurohormonal Hypothesis in Heart FailureCypress Trixia Mananquil MacapagalОценок пока нет
- Reviews: Hyperventilation in Head InjuryДокумент16 страницReviews: Hyperventilation in Head InjurySani Widya FirnandaОценок пока нет
- Cardiac Toxic ResponsesДокумент10 страницCardiac Toxic ResponsesDaismar ArenasОценок пока нет
- Hypertension: A Comparative Review Based On Fractal Wave Theory of ContinuumДокумент8 страницHypertension: A Comparative Review Based On Fractal Wave Theory of ContinuumAdaptive MedicineОценок пока нет
- Pathophysiology and Etiology of Edema - IДокумент9 страницPathophysiology and Etiology of Edema - IBrandy MaddoxОценок пока нет
- Blood Pressure Management in Acute StrokeДокумент19 страницBlood Pressure Management in Acute StrokeTamara LopezОценок пока нет
- Vasculopathy Emulation and Its Influence On The Cardiac Output Curve-Franyi Lorena DiazДокумент7 страницVasculopathy Emulation and Its Influence On The Cardiac Output Curve-Franyi Lorena Diazfranyi lorenaОценок пока нет
- Pathophysiology of COPDДокумент4 страницыPathophysiology of COPDrinieeeОценок пока нет
- Stochastic Model For Blood Pressure AnalysisДокумент9 страницStochastic Model For Blood Pressure AnalysisRakeshconclaveОценок пока нет
- Articol 2 Pentru PublicareДокумент6 страницArticol 2 Pentru PublicarePOPESCU LUCIANОценок пока нет
- Case 2 SlosДокумент7 страницCase 2 SlosNamarОценок пока нет
- Pinsky1997 Article TheHemodynamicConsequencesOfMeДокумент11 страницPinsky1997 Article TheHemodynamicConsequencesOfMeAlvaro EstupiñánОценок пока нет
- BaroreseptorДокумент3 страницыBaroreseptorHaziq GanuОценок пока нет
- Cardiac Output HandoutДокумент10 страницCardiac Output Handoutsac50900Оценок пока нет
- Congestive Heart Failure: Diagnosis, Pathophysiology, Therapy, and Implications For Respiratory CareДокумент10 страницCongestive Heart Failure: Diagnosis, Pathophysiology, Therapy, and Implications For Respiratory CareKevinDilianSugandaОценок пока нет
- Chronic Interactions Between Carotid Baroreceptors and Chemoreceptors in Obesity HypertensionДокумент14 страницChronic Interactions Between Carotid Baroreceptors and Chemoreceptors in Obesity HypertensionCaesar Catalin CaratasuОценок пока нет
- Pleiotropic Effects of Calcium Channel BlockersДокумент11 страницPleiotropic Effects of Calcium Channel BlockersSabdiah Eka SariОценок пока нет
- CVS QuesДокумент8 страницCVS QuesTan Ann JeeОценок пока нет
- Hypertension: SMF Saraf Rsud Bangli Fakultas Kedokteran Universitas Islam Al-Azhar 2018Документ49 страницHypertension: SMF Saraf Rsud Bangli Fakultas Kedokteran Universitas Islam Al-Azhar 2018Muhammad HidayatullahОценок пока нет
- Heart FailureДокумент10 страницHeart FailureJajangОценок пока нет
- CV PathoДокумент32 страницыCV PathoSaif AliОценок пока нет
- Pathophysiology of Heart Failure - Neurohumoral Adaptations PDFДокумент10 страницPathophysiology of Heart Failure - Neurohumoral Adaptations PDFcristianamihailaОценок пока нет
- Shock and Critical Care: Presented BY: Palwasha KhanДокумент23 страницыShock and Critical Care: Presented BY: Palwasha KhanPalwasha KhanОценок пока нет
- Monitoreo Hemodinamico Funcional PinskyДокумент23 страницыMonitoreo Hemodinamico Funcional PinskyJuan CarrascoОценок пока нет
- Chronic Baroreflex Activation Restores Spontaneous Baroreflex Control and Variability of Heart Rate in Obesity-Induced HypertensionДокумент10 страницChronic Baroreflex Activation Restores Spontaneous Baroreflex Control and Variability of Heart Rate in Obesity-Induced HypertensionCaesar Catalin CaratasuОценок пока нет
- IISRT Jaisre Kamaraj (EC)Документ5 страницIISRT Jaisre Kamaraj (EC)IISRTОценок пока нет
- Pathophysiology of Congestive Heart FailureДокумент6 страницPathophysiology of Congestive Heart FailurenevandraОценок пока нет
- Assignment 1 BM-331 Modeling and SimulationДокумент6 страницAssignment 1 BM-331 Modeling and SimulationeraОценок пока нет
- JensenДокумент26 страницJensenBaso AgusofyangОценок пока нет
- Effectifeness of Managing Suspected Pulmonary Embolism Using An Algorithm Combining Clinical ProbabilityДокумент140 страницEffectifeness of Managing Suspected Pulmonary Embolism Using An Algorithm Combining Clinical ProbabilityBaso AgusofyangОценок пока нет
- Effectifeness of Managing Suspected Pulmonary Embolism Using An Algorithm Combining Clinical ProbabilityДокумент140 страницEffectifeness of Managing Suspected Pulmonary Embolism Using An Algorithm Combining Clinical ProbabilityBaso AgusofyangОценок пока нет
- Quality of Life of SLE PatientsДокумент8 страницQuality of Life of SLE PatientsBaso AgusofyangОценок пока нет
- Correlation Between SLEDAI, C3, C4 Dan Anti-dsDNA AntibodiesДокумент6 страницCorrelation Between SLEDAI, C3, C4 Dan Anti-dsDNA AntibodiesBaso AgusofyangОценок пока нет
- Ictal Vomiting LocalisationДокумент4 страницыIctal Vomiting LocalisationmayankОценок пока нет
- Anatomy and PhysiologyДокумент23 страницыAnatomy and PhysiologyRusca De MedikoОценок пока нет
- LUNG-OVERVIEW (Autosaved)Документ132 страницыLUNG-OVERVIEW (Autosaved)Thivashinie Kandy Nazan VelloОценок пока нет
- Endocrine System DiseasesДокумент8 страницEndocrine System DiseasesPrincess Xzmae Ramirez100% (1)
- Herniation Flash CardДокумент4 страницыHerniation Flash CardAin GhazaliОценок пока нет
- 4mm Frog EmbryoДокумент3 страницы4mm Frog EmbryoIvy CruzОценок пока нет
- Important McQs For Clinical and BNSДокумент3 страницыImportant McQs For Clinical and BNSAbrar AhmadОценок пока нет
- WLP Science q2 w3 Nov 28 Dec 2Документ6 страницWLP Science q2 w3 Nov 28 Dec 2Maria Aurea BorjaОценок пока нет
- 1.23 Liver DiseaseДокумент2 страницы1.23 Liver DiseaseDr-Dalya ShakirОценок пока нет
- By Parashie Sidhwani, Grade 10: "Transplant, Also Known As Graft or Organ Transplant, Is AДокумент2 страницыBy Parashie Sidhwani, Grade 10: "Transplant, Also Known As Graft or Organ Transplant, Is AParashie SidhwaniОценок пока нет
- P9mi9p6lx - Lesson 3.3-The Integumentary System 3Документ23 страницыP9mi9p6lx - Lesson 3.3-The Integumentary System 3Precious RoxasОценок пока нет
- Pyelonephritis: Dr.P.SravaniДокумент70 страницPyelonephritis: Dr.P.SravaniSravani Peddagangannagari100% (1)
- Chapter 19Документ34 страницыChapter 19Sahithya MОценок пока нет
- Edexcel Circulary System Past Paper Questions 1Документ10 страницEdexcel Circulary System Past Paper Questions 1binura desilvaОценок пока нет
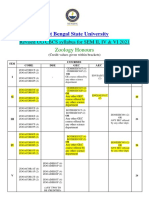
- Revised ZOOLOGY HONOURS UG CBCS Syllabus Sem II, IV, VI-editedДокумент5 страницRevised ZOOLOGY HONOURS UG CBCS Syllabus Sem II, IV, VI-editedRidhi ChoudharyОценок пока нет
- CH 01Документ12 страницCH 01TahmidОценок пока нет
- Brain StudyДокумент57 страницBrain StudyJoeОценок пока нет
- Pex 02 02Документ13 страницPex 02 02Febriano SuwartoОценок пока нет
- Pancreatic Solid LeasionsДокумент24 страницыPancreatic Solid LeasionsEliza CrăciunОценок пока нет
- Tutor: Prof. Dr. H. Syakroni Daud Rusdi, SP - OGДокумент53 страницыTutor: Prof. Dr. H. Syakroni Daud Rusdi, SP - OGAna Abadi Al IndОценок пока нет
- The Heart and PericardiumДокумент40 страницThe Heart and PericardiumMartha Orendu Oche AttahОценок пока нет
- Endocrin E Diseases: by Group 3Документ53 страницыEndocrin E Diseases: by Group 3Ash AshОценок пока нет
- Cardiac ExaminationДокумент23 страницыCardiac ExaminationAreza Eka PermanaОценок пока нет