Академический Документы
Профессиональный Документы
Культура Документы
Jurnal Jantung
Загружено:
Diah Ayu AdiatiОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Jurnal Jantung
Загружено:
Diah Ayu AdiatiАвторское право:
Доступные форматы
Original Articles
IMAJ VOL 15 December 2013
Arterial Elasticity in Obese Subjects with Coronary Slow
Flow Phenomenon
Osamah Hussein MD1,4, Jamal Zidan MD2,4, Michael Plich MD4, Hana Gefen MD1, Roberto Klein MD4,5, Karina Shestatski MD1,5,
Kamal Abu-Jabal MD1,5 and Reuven Zimlichman MD6
Department of Internal Medicine A, 2Oncology Unit and 3Invasive Cardiology Unit, Ziv Medical Center, Safed, Israel
Bar-Ilan Faculty of Medicine, Safed, Israel
5
Department of Medicine and Hypertension, Wolfson Medical Center, Holon, Israel
6
Bruner Cardiovascular Research Institute, Sackler Faculty of Medicine, Tel Aviv University, Ramat Aviv, Israel
1
4
Abstract:
Background: Coronary slow flow phenomenon (CSFP) is a
functional and structural disease that is diagnosed by coronary angiogram.
Objectives: To evaluate the possible association between
CSFP and small artery elasticity in an effort to understand
the pathogenesis of CSFP.
Methods: The study population comprised 12 patients
with normal coronary arteries and CSFP and 12 with normal
coronary arteries without CSFP. We measured conjugated
diene formation at 234 nm during low density lipoprotein (LDL)
oxidation, as well as platelet aggregation. We estimated, noninvasively, arterial elasticity parameters. Mann-Whitney nonparametric test was used to compare differences between the
groups. Data are presented as mean standard deviation.
Results: Waist circumference was 99.2 8.8 cm and 114.9
10.5 cm in the normal flow and CSFP groups, respectively (P =
0.003). Four patients in the CSFP group and one in the normal
flow group had type 2 diabetes. Area under the curve in the
oral glucose tolerance test was 22% higher in the CSFP than
in the normal group (P = 0.04). There was no difference in
systolic and diastolic blood pressure, plasma concentrations
of total cholesterol, triglycerides, high density lipoprotein, LDL
and platelet aggregation parameters between the groups. Lag
time required until initiation of LDL oxidation in the presence
of CuSO4 was 17% longer (P = 0.02) and homocysteine fasting
plasma concentration was 81% lower (P = 0.05) in the normal
flow group. Large artery elasticity was the same in both
groups. Small artery elasticity was 5 1.5 ml/mmHgx100 in
normal flow subjects and 6.1 1.9 ml/mmHgx100 in the CSFP
patients (P = 0.02).
Conclusions: Patients with CSFP had more metabolic derangements. Arterial stiffness was not increased in CSFP.
IMAJ 2013; 15: 753757
Key words: coronary slow flow phenomenon (CSFP), metabolic
abnormalities, arterial elasticity, pulse wave contour
C mal or minimal atherosclerotic coronary arteries with
oronary slow flow phenomenon is characterized by nor-
delayed opacification of the distal vasculature [1]. Ninety
percent of patients complain of recurrent chest pain. Most
patients are men who smoke. In myocardial biopsy studies,
it was demonstrated that CSFP patients had microvascular
disease [2].
Ischemia demonstrated by electrocardiography and/or scintigraphy during stress provocation is found in less than 50%
of CSFP patients. However, many of them demonstrate ECG
evidence of ischemia during spontaneous chest pain, typically
during initial presentation with an acute coronary syndrome
[1]. ST segment elevation in the absence of epicardial artery
spasm was reported in association with CSFP [3].
CSFP patients show increased resting coronary vasomotor
tone with low coronary sinus oxygen saturation, reflecting an
increased myocardial oxygen extraction caused by delayed
resting coronary perfusion. Some patients fail to show CSFP
on repeated angiography, implying a significant dynamic component to the impaired coronary microvascular resistance [4]
beyond the structural (fixed) microvascular disease demonstrated in previous biopsy studies [2]. Angiographic resolution
of CSFP can be demonstrated with dipyridamole, but not with
nitrates [2]. Exercise perfusion SPECT showed reversible perfusion defect in 17 of 60 CSFP patients and was normal in 43
of 60 patients. Myocardial perfusion was normalized in all 17
patients with RPD after dipyridamole infusion. No correlation
was observed between the time needed to fill a native coronary
artery and RPD of the myocardium [5].
Since coronary blood flow increases with pacing tachycardia to the same extent in control patients and CSFP patients,
it was suggested that appropriate vasodilatory response is
present in CSFP patients [4]. Maximal coronary flow velocity
with adenosine was lower in CSFP patients compared with
control subjects [6]. Some patients experienced chest pain
and ST segment elevation during acetylcholine infusion in
the absence of pericardial artery spasm or myocardial lactate
production [4]. Thromboxane A2 release across the coronary
vascular bed is increased in patients with CSFP, suggesting
1
RPD = reversible perfusion defect
753
Original Articles
both the presence of intracoronary platelet activation and the
potential for coronary vasoconstriction [7].
As CSFP appears to have an abnormal systemic microvascular and metabolic component, we aimed to determine
whether measurement of small vessel elasticity can help us
understand and thus predict slow flow in the coronary arteries. In the present study we aimed to determine whether
patients with CSFP have a higher incidence of systemic
derangements of the components of metabolic syndrome,
oxidative stress and a platelet tendency to aggregation, and
whether CSFP is a general vascular abnormality that can be
predicted by measuring peripheral arterial elasticity.
PATIENTS AND METHODS
The first consecutive 12 catheterized patients with normal
coronary arteries and CSFP in the three arteries and the first
consecutive 12 patients from the same period with normal
coronary arteries but without CSFP were included in the study.
Patients were not under the effect of nitrates and abstained from
consuming caffeine. Angiographic criteria for CSFP include
coronary angiography with normal or near-normal (< 40%
stenosis) coronary arteries and Thrombolysis in Myocardial
Infarction (TIMI) 0-1 flow, i.e., requiring three or more beats
to opacify the distal vasculature [8]. Secondary causes of CSFP
such as coronary emboli, no-reflow phenomenon or coronary
ectasia were excluded. All patients signed an informed consent,
and approval of the hospital internal review board was given.
TIMI frame counts were counted for each vessel in the left
anterior descending, circumflex and right coronary arteries.
Corrected TIMI frame counts were calculated as described by
Gibson and co-researchers [9]. The sum of TIMI frame counts
for the three arteries was divided by three. Coronary perfusion
pressures in mmHg (diastolic aortic pressure minus left ventricle
diastolic pressure) were available in six patients in the CSFP
group and seven patients in the coronary normal flow group.
Four days after the coronary angiography, blood samples
were drawn and oral glucose tolerance tests were done. Arterial
elasticity determinations were performed over 2 days . Patients
ingested 75 g glucose after an overnight fast. Serum glucose
was measured before, and 1 hour and 2 hours after ingestion.
Biochemical parameters including total cholesterol and low density lipoprotein cholesterol and triglycerides were measured by
specific kits (Olympus system reagents for clinical chemistry
analyzers, Olympus Diagnostic GmbH, Hamburg, Germany).
Serum levels for homocysteine were measured by AxSYM
homocysteine assay based on the Fluorescence Polarization
Immunoassay technology (Abbott laboratories, IL, USA). Blood
for LDL separation was drawn into sodium ethylene diamine
tetra acetic acid (NaEDTA) (1 mM) and centrifuged at 1500
rpm for 10 minutes at 4C. LDL was separated from plasma
by discontinuous density-gradient ultracentrifugation [10] and
754
IMAJ VOL 15 December 2013
dialyzed against saline-NaEDTA (1 mM). LDL protein concentration was determined by the method of Lowry et al. [11].
LDL oxidation studies were performed each time on fresh
samples. Prior to oxidation, LDL was dialyzed against saline
1.006 with Na2EDTA 1 mM, pH=7.4 and then dialyzed against
phosphate-buffered saline at 4C to remove Na2EDTA. It was
then diluted with PBS to 0.2 mg protein/ml. The lipoprotein was
incubated in the presence of 5 M CuSO4 at 37C. Measuring
conjugated diene formation at 234 nm continuously monitored
the kinetics of LDL oxidation. For each LDL sample we received
a curve consisting of three consecutive phases: lag phase (lag time
in minutes required for the initiation of CuSO4-induced LDL oxidation), propagation phase, and a final plateau phase [12].
2
Platelet separation
Washed platelets were chosen to measure isolated platelet reactivity with the influence of plasma components. For platelet
studies, venous blood (30 ml) was collected using siliconized
syringes into acid citrate dextrose solution (1.4% citric acid,
2.5% sodium citrate, and 2% dextrose) at a ratio of 9:1 (v:v) for
washed platelets preparation. Washed platelets were prepared by
centrifugation at 240 g for 20 min. The platelet ring was washed
twice in 5 mmol HEPES buffer, pH 7.4 (140 mmol NaCl, 2
mmol KCL, 1 mmol MgCl2, 5 mmol HEPES, 12 mmol NaHCO3
and 5.5 mmol glucose). For the preparation of washed platelets
suspension, 15 l of acetic acid (1 mmol) was added to 1 ml
of platelet suspension throughout WP preparation in order to
ensure acidic conditions required for platelet resuspension. This
procedure reduces the medium pH to 6.5 and does not influence
the aggregation response of the washed platelets.
Platelet aggregation
Collagen (Nycomed, Germany) was used as the aggregating
agent at a concentration of 4 g/ml (this concentration can
cause up to 60% aggregation amplitude in washed platelets).
Platelet aggregation was performed at 37C in an aggregometer (PACKS-4, Platelet aggregation chromogenic kinetic
system, Helena Laboratories, Beaumont, TX, USA) using
HEPES as a reference system. Results were expressed as the
extent of maximal aggregation (% of maximal amplitude) and
also as the slope of the aggregation curve (cm/min) [13].
Arterial elasticity determination
Diastolic pulse contour analysis (Windkessel model) demonstrates
arterial elastic properties. The wave form can be decomposed to
two main components: C1 is the main slope of the diastolic decay
function and is assumed to be related to the proximal compliance
(aorta and proximal part of carotids). C2 is the superimposed
decaying sinusoid function that represents the distal arteries and
is dependent on systemic vascular resistance [14].
PBS = phosphate-buffered saline
Original Articles
IMAJ VOL 15 December 2013
Measurements were performed in a quiet temperaturecontrolled environment after the patient rested in a supine
position. Radial arterial waveforms were recorded for 30
seconds for each subject in the supine position. The pressure
transducer amplifier system was connected to a specially
designed device (Model CR-2000, Hypertension Diagnostics
Inc. and Eagen, MN). The passive transient response of the
arterial vasculature to the initial loading conditions was
determined by analyzing the diastolic portion of the pressure
pulse wave form. This technique, which has been used extensively by us and others [15], was performed with a simple
non-invasive radial pulse wave recording and a computer
analysis of diastolic decay, thus providing a separate assessment of the large artery or capacitive compliance (C1) and
small artery reflective or oscillatory elasticity (C2).
This method evaluates the components of the arterial
pulse by waveform analysis, enabling differentiation between
small and large arterial elasticity parameters.
Statistical analysis
Mann-Whitney non-parametric test was used to compare
differences between normal and slow flow groups. Data are
presented as mean standard deviation. Multiple linear
regressions were performed to predict TIMI flow by metabolic
parameters and arterial elasticity.
RESULTS
Table 1 presents the clinical characteristics of the subjects with
coronary normal and slow flow phenomenon. The number of
patients treated by statins, beta-blocker, angiotensin-converting enzyme inhibitor, nitrate, alpha-blocker or acetyl salicylic
acid was 4, 5, 3, 2, 1 and 3 in the CSFP group and 5, 5, 3, 3, 1
and 3 in the normal flow group, respectively. The number of
atherosclerotic plaques < 40% in LAD, Cx and RCA in the normal flow and CSFP groups were 2, 1, 1 and 2, 2, 1, respectively.
Table 2 describes the angiographic parameters including TIMI flow grade and corrected TIMI frame count as an
average for three arteries. Corrected TIMI frame count was
significantly higher in the CSFP group by 91% compared
3
LAD = left anterior descending artery
Cx = circumflex artery
RCA = right coronary artery
Table 1. Clinical presentations in subjects with coronary normal
and slow flow phenomenon
Clinical
presentation
Angina
at rest
ST segment
depression
by ECG
Positive
exercise
stress test
with the normal flow group. There were no differences in
coronary perfusion pressures (which were available in 50%
of the patients) between the two groups.
There was no difference in mean age, number of smokers or
body mass index between the two groups. Waist circumference
was significantly higher by 16% in the CSFP group compared
with the normal flow group. Four patients in the CSFP group
and one in the normal flow group had type 2 diabetes mellitus.
The mean area under the curve in the oral glucose tolerance
tests was significantly higher by 22% in the CSFP compared with
the normal flow group. The systemic systolic and diastolic blood
pressure measured before the coronary catheterization were not
significantly different from the systolic and diastolic blood pressure measured in the aorta during the coronary catheterization,
Table 2. Metabolic parameters and elasticity in subjects with coronary normal and
slow flow phenomenon
Normal flow
(n=12)
Slow flow
(n=12)
P value
TIMI flow grade
3.0 0.00
1.9 0.2
< 0.001
Gender (male)
Corrected TIMI frame count (average for three arteries)
23.2 2.7
44.2 11.1
0.001
Age (yr)
49.5 5.3
50.3 8.6
NS
Smokers
Body mass Index (kg/m2)
30.0 3.8
31.8 4.2
NS
Waist circumference (cm) (combined average)
99.2 8.8
114.9 9.3
< 0.001
Type 2 diabetes mellitus
Arterial hypertension
NS
Hyperlipidemia or lipid modifying drugs
11
NS
Area under curve in oral glucose tolerance test (mmol/L/hr)
14.3 2.4
17.5 0.7
< 0.050
Systolic blood pressure mmHg (at enrolment)
132.3 23.2
133.2 15.4
NS
Diastolic blood pressure mmHg (at enrolment)
88.1 12.7
86.1 11.3
NS
Systolic blood pressure mmHg (before coronary catheterization)
126 8
134 10
NS
Diastolic blood pressure (mmHg)
(before coronary catheterization)
77 8
79 9
NS
Systolic blood pressure mmHg (aorta, during angiography)
132 8
128 18
NS
Diastolic blood pressure (mmHg) (aorta, during angiography)
76 9
77 9
NS
Coronary perfusion pressure (mmHg)
56 19 (n=7)
57 4 (n=6)
NS
Plasma total cholesterol (mg/dl)
212 36
213 48
NS
Plasma LDL-cholesterol (mg/dl)
135 22
134 47
NS
Plasma triglycerides (mg/dl)
171 125
189 86
NS
Plasma HDL-cholesterol (mg/dl)
42 10
41 8
NS
Homocysteine plasma levels (mol/L)
11.4 3.1
20.6 14.2
p<.050
Positive
stress
perfusion
imaging
Lag time required to initiation of LDL oxidation (min)
41.1 8.8
34.2 7.4
NS
Maximal platelet aggregation (% of maximal amplitude)
Slope of aggregation curve (cm/min)
89.8 5.3
140.6 21.4
90.8 5.4
146.0 35.8
NS
NS
Normal flow subjects
Large artery elasticity C1 (ml/mmHgx10)
16.2 6.0
15.7 5.8
NS
Slow flow subjects
10
Small artery elasticity C2 (ml/mmHgx100)
4.51.5
6.11.3
P<.050
755
Original Articles
IMAJ VOL 15 December 2013
nor from systolic and diastolic blood pressure measured during
enrolment of the patients to the study, both within and between
the two groups. Three patients in each group were under treatment with aspirin 75 mg/day. Excluding these patients did not
alter the conclusion that there was no difference in maximal
platelet aggregation as a percent of maximal amplitude or slope
of aggregation curve between the two groups. There was no difference in the serum levels of total cholesterol, LDL-cholesterol,
HDL -cholesterol and triglycerides between the two groups.
Homocysteine serum level was 81% higher (P = 0.05) and lag
time required until initiation of LDL oxidation was significantly
shorter by 17% in the CSFP group compared to the normal
flow group. There was no difference in large artery elasticity
(C1) between the two groups, but small artery elasticity (C2)
was 22% significantly higher in the CSFP group compared with
the normal flow group. Both homocysteine and area under the
curve in the oral glucose tolerance test predicted TIMI flow by
multiple linear regressions [Table 3].
6
DISCUSSION
Patients with CSFP have more risk factors for atherosclerosis
than patients with normal coronary flow, including obesity,
increased homocysteine and increased tendency of LDL to oxidation. As anticipated, most of the patients were men [1] and
presented because of angina at rest. For metabolic parameters in
the present study, there were no differences in serum total cholesterol, LDL-C, HDL-C or triglyceride concentrations between
the two groups. On the other hand, there was increased oxidative stress in the serum of the CSFP group, as demonstrated
by shorter lag time to LDL peroxidation in comparison to the
normal flow group. We did not find a difference in systolic or
diastolic blood pressures that were measured before and during
coronary catheterization and during patients enrolment; therefore, corrected TIMI frame counts difference between the two
groups cannot be explained by changes in blood pressure or
coronary perfusion pressures during coronary catheterization.
Waist circumference as a measure for abdominal obesity was
higher in the CSFP group. In the CSFP group, both men and
HDL = high density lipoprotein
Table 3. Multiple regression to predict TIMI flow by homocysteine
and area under the curve in the oral glucose tolerance test
B
SEB
Homocysteine
-0.023
0.007
-0.443*
Area under the curve
Glucose tolerance test
0.007
0.002
0.613**
R2
0.585
14.787**
*P < 0.01, ** P < 0.001
SEB = standard error of B
756
women had a waist circumference that fit the criteria for metabolic syndrome (Adult Treatment Panel III: waist circumference
> 102 cm for men and > 88 cm for women) [16]. Area under the
curve of the glucose tolerance test was significantly high in the
CSFP group. This is in line with other studies in which insulin
resistance was an independent risk factor for CSFP [17].
For prothrombotic tendency, it has been postulated that
there is increased intracoronary platelet activation in CSFP
patients [7]. In the present study, no increase in systemic
platelet activity was found in the CSFP group as compared to
the normal flow group. It seems that the different results in
other studies are due to different methods of measuring platelet
activity. Platelet aggregation is still considered the gold standard for platelet activity. The increased thromboxane A2 release
across the coronary vascular bed in patients with CSFP may
be secondary to sluggish intracoronary flow [7]. The increased
plasma levels of homocysteine in CSFP patients together with
coronary slow blood flow may affect endothelial function in
coronary arteries, thus activating intracoronary platelets.
In the present study, CSFP patients presented with more
metabolic derangements than did the normal flow group,
which may affect endothelial function in this group beyond the
structural pathology [2]. In various studies humoral factors were
explored to understand the pathogenesis of CSFP. Endothelin-1
plasma concentrations were higher and nitric oxide plasma
concentrations lower at baseline and peak exercise in CSFP
patients [18]. The metabolic abnormalities suggest that CSFP is
a generalized endothelial dysfunction state. Patients with coronary heart disease may have abnormalities of remote systemic
arterial function [19]. Indeed, it was demonstrated in CSFP
patients that there is a close relation between coronary artery
endothelium-dependent vasomotor responses to acetylcholine
and flow-mediated dilatation of the brachial artery [20] and
elevated ascending aortic pulse pressure and aortic pulsatility
[21]. Despite these findings, it was demonstrated that large
artery stiffness and arterial wave reflection characteristics are
normal in CSFP patients between their acute episodes [22].
To evaluate the possibility that CSFP is caused by or is associated with generalized increased small artery stiffness we analyzed the pulse wave contour in the radial artery. Pulse wave
contour analysis can detect preclinical vascular disease of both
small and large arteries [23]. In the present study, small artery
elasticity was lower in the normal flow group and unrelated to
passive decrease in elasticity frequently associated with higher
arterial pressure. In a previous study there was no difference in
augmentation index between CSFP and controls in response
to either salbutamol or glyceryl trinitrate [24]. Augmentation
index is a measure of endothelial function in small arteries.
Even close to the acute episode, small artery elasticity was not
impaired in CSFP.
In contrast to the suggestion that CSFP is always a systemic
abnormality, it can be both a systemic and a regional phenom-
Original Articles
IMAJ VOL 15 December 2013
enon. Heterogeneity of response in conduit arteries in different
regions of the vascular tree [25] has been shown.
The present study found no correlation between small
artery elasticity and CSFP, which may be explained by the
differing hemodynamic parameters at various sites. Regional
variations, such as low shear stress, oscillatory flow or turbulent flow, may prime the local vascular wall and geneexpression profile to interact differentially with systemic
factors, thereby resulting in the potential for local variations
in arterial elasticity. CSFP can be a heterogeneous condition,
as a local vascular abnormality or as a part of generalized
endothelial dysfunction.
Study limitations
Arterial elasticity was determined by two technicians from
another hospital (Wolfson Medical Center) and the laboratory workup was performed by laboratory personnel who
were blinded to the results of the coronary arteries angiogram; the first author, however, was not blinded. Another
limitation was the small number of patients. The ideal control
group would be of healthy persons with no history of chest
pain or cardiac disease and with normal cardiac angiogram
and normal coronary flow, but they would not be candidates
for cardiac angiogram. On the other hand, without cardiac
angiography it would not be possible to exclude coronary
artery disease or the CSFP.
Conclusions
Patients with CSFP show a higher incidence of metabolic
abnormalities and oxidative stress but do not demonstrate
increased platelet tendency to aggregation. On the other hand,
the finding of normal elasticity in the small vessels excludes
the possibility that small artery stiffness plays a pathogenetic
role in the mechanism of the coronary slow flow phenomenon.
The contribution of the study is that CSFP is not a homogenous syndrome and not every method of measurement in the
peripheral arterial system can detect CSFP.
Corresponding author:
Dr. O. Hussein
Head, Dept. of Internal Medicine A, Ziv Medical Center, Safed 13100, Israel
Phone: (972-4) 682-8943
Fax: 972-4) 682-8944
email: osama.h@ziv.health.gov.il
References
1. Hawkins BM, Stavrakis S, Rousan TA, Abu-Fadel M, Schechter E. Coronary
slow flow: prevalence and clinical correlation. Circ J 2012; 76: 936-42.
2. Mangieri E, Macchiarelli G, Ciavolella M, et al. Slow coronary flow: clinical
and histopathological features in patients with otherwise normal epicardial
coronary arteries. Cathet Cardiovasc Diagn 1996; 37: 375-81.
3. Beltrame JF, Horowitz JD. ST elevation secondary to microvascular dysfunction. J Am Coll Cardiol 1999; 34: 312-13.
4. Beltrame JF, Limaye SB, Wuttke RD, Horowitz JD. Coronary hemodynamic
and metabolic studies of the coronary slow flow phenomenon. Am Heart J
2003; 146: 84-90.
5. Demirkol MO, Yaymaci B, Mutlu B. Dipyridamole myocardial perfusion
single photon emission computed tomography in patients with slow coronary
flow. Coron Artery Dis 2002; 13: 223-9.
6. Ge J, Simon HU, Jeremias A, Shah V, Caspari G. Angiographic coronary slow
flow phenomenon indicates microvascular dysfunction: an intracoronary
Doppler study [Abstract]. Circulation 1997; 8: I-273.
7. Di Donato M, Fantini F, Maioli M, Prisco D, Rogasi PG, Neri Serneri GG.
Blood velocity in the coronary artery circulation: relation to thromboxane A2
levels in coronary sinus in patients with angiographically normal coronary
arteries. Cathet Cardiovasc Diagn 1987; 13: 162-6.
8. Chesebro JH, Knatterud G, Roberts R, et al. Thrombolysis in Myocardial
Infarction (TIMI) Trial, Phase I: A comparison between intravenous tissue
plasminogen activator and intravenous streptokinase. Clinical findings
through hospital discharge. Circulation 1987; 76: 142-54.
9. Gibson CM, Cannon CP, Daley WL, et al. TIMI frame count: a quantitative
method of assessing coronary artery flow. Circulation 1996; 93: 879-88.
10. Aviram M. Plasma lipoprotein separation by discontinuous density gradient
ultracentrifugation in hyperlipoproteinemic patients. Biochem Med 1983; 30:
111-18.
11. Lowry OH, Rosebrough NJ, Farr AL, Randall RJ. Protein measurement with
the Folin phenol reagent. J Biol Chem 1951; 193: 265-75.
12. Esterbauer H, Striegl G, Puhl H, Rotheneder M. Continuous monitoring of
in vitro oxidation of human low density lipoprotein. Free Radic Res Commun
1989; 6: 67-75.
13. Hussein O, Rosenblat M, Schlezinger S, Keidar S, Aviram M. Reduced platelet
aggregation after fluvastatin therapy is associated with altered platelet lipid
composition and drug binding to the platelets. Br J Clin Pharmocol 1997; 44: 77-84.
14. ORourke MF, Staessen JA, Vlachopoulos C, Duprez D, Plante GE. Clinical
applications of arterial stiffness; definitions and reference values. Am J Hypertens
2002; 15: 426-44.
15. Shargorodsky M, Leibovitz E, Lubimov L, Gavish D, Zimlichman R.
Prolonged treatment with the AT1 receptor blocker, valsartan, increases small
and large artery compliance in uncomplicated essential arterial hypertension.
Am J Hypertens 2002; 15: 1087-91.
16. Executive Summary of the third report of the National Cholesterol Education
Program (NCEP) expert panel on detection, evaluation, and treatment of high
blood cholesterol in adults (adult treatment panel III). JAMA 2001; 285: 2486-97.
17. Ozcan T, Gen R, Akbay E, et al. The correlation of thrombolysis in myocardial
infarction frame count with insulin resistance in patients with slow coronary
flow. Coron Artery Dis 2008; 19: 591-5.
18. Camsari A, Pekdemir H, Cicek D, et al. Endothelin-1 and nitric oxide
concentrations and their response to exercise in patients with slow coronary
flow. Circ J 2003; 67: 1022-8.
19. Werns SW, Walton JA, Hsia HH, Nabel EG, Sanz ML, Pitt B. Evidence of
endothelial dysfunction in angiographically normal coronary arteries of
patients with coronary artery disease. Circulation 1989; 79: 287-91.
20. Anderson TJ, Uehata A, Gerhard MD, et al. Close relation of endothelial function
in the human coronary and peripheral circulations. J Am Coll Cardiol 1995; 26:
1235-41.
21. Guray U, Guray Y, Yilmaz MB, et al. Aortic pulse pressure and aortic pulsatility
in patients with coronary slow flow. Cardiology 2007; 107: 233-8.
22. Sharman JE, Moir S, Kostner KM, Haluska B, Marwick TH. Patients with
coronary slow flow phenomenon demonstrate normal myocardial blood flow
and arterial wave reflection between acute episodes. Int J Cardiol 2009; 131: 321-5.
23. Heagerty AM, Aalkjaer C, Bund SJ, Korsgaard N, Mulvany MJ. Small artery
structure in hypertension. Dual processes of remodeling and growth. Hypertension
1993; 21: 391-7.
24. Kopetz V, Kennedy J, Heresztyn T, et al. Endothelial function, oxidative
stress and inflammatory studies in chronic coronary slow flow phenomenon
patients. Cardiology 2012; 121: 197-203.
25. Kawasaki T, Sasayama S, Yagi S, Asakawa T, Hiari T. Non-invasive assessment
of the age related changes in stiffness of major branches of the human arteries.
Cardiovasc Res 1987; 21: 678-87.
757
Вам также может понравиться
- Blood Chemistry and CBC Analysis - Clinical Laboratory Testing From A Functional Perspective - Quick Reference GuideДокумент29 страницBlood Chemistry and CBC Analysis - Clinical Laboratory Testing From A Functional Perspective - Quick Reference Guidejamesilluminare73% (15)
- Transfusion in Emergency Room by DR Prannoy George, Department of Emergency Medicine, Amrita Institute of Medical Sciences, Kochi, KeralaДокумент41 страницаTransfusion in Emergency Room by DR Prannoy George, Department of Emergency Medicine, Amrita Institute of Medical Sciences, Kochi, KeralaAETCM Emergency medicineОценок пока нет
- Chapter 4Документ29 страницChapter 4starykОценок пока нет
- Jcu 17 127 PDFДокумент8 страницJcu 17 127 PDFRezkyFYОценок пока нет
- Sharawey2011 PDFДокумент7 страницSharawey2011 PDFIkram DibОценок пока нет
- Relation Between Progression and Regression of ... Coronary Artery Disease and Serum Cholesterol LevelsДокумент19 страницRelation Between Progression and Regression of ... Coronary Artery Disease and Serum Cholesterol LevelsJОценок пока нет
- Arteriovenous Thrombosis in Chronic Renal Failure Patients Receiving Renal Replacement TherapyДокумент6 страницArteriovenous Thrombosis in Chronic Renal Failure Patients Receiving Renal Replacement TherapyMaya RustamОценок пока нет
- Ischemia-Modified Albumin Use As A Prognostic Factor in Coronary Bypass SurgeryДокумент5 страницIschemia-Modified Albumin Use As A Prognostic Factor in Coronary Bypass SurgerySarah KemalasariОценок пока нет
- Angina Pectoris in Patients With Aortic Stenosis and Normal Coronary Arteries - CirculationДокумент24 страницыAngina Pectoris in Patients With Aortic Stenosis and Normal Coronary Arteries - CirculationOscar F RojasОценок пока нет
- Journal 2Документ3 страницыJournal 2Anis Rita PratiwiОценок пока нет
- Abstracts / Atherosclerosis 252 (2016) E1 Ee196 E185Документ2 страницыAbstracts / Atherosclerosis 252 (2016) E1 Ee196 E185MaulОценок пока нет
- Relatia Dintre Arteroscleroza Si Colesterol SericДокумент7 страницRelatia Dintre Arteroscleroza Si Colesterol SericBeniamin BorotaОценок пока нет
- Impact of Albumin RL For BTДокумент10 страницImpact of Albumin RL For BTSandeep BhaskaranОценок пока нет
- Siadh vs. CSWДокумент6 страницSiadh vs. CSWFadiah Izzati SalimОценок пока нет
- Evaluation of Factors Affecting Liver Function Test in Patients Underwent Coronary Artery Bypass Graft SurgeryДокумент7 страницEvaluation of Factors Affecting Liver Function Test in Patients Underwent Coronary Artery Bypass Graft SurgeryajmrdОценок пока нет
- JURNALДокумент8 страницJURNALICHWANUDDINBUCHORIОценок пока нет
- Citrate in CRRTДокумент8 страницCitrate in CRRTAshish PandeyОценок пока нет
- Ojsadmin, 176Документ4 страницыOjsadmin, 176Signor 2019Оценок пока нет
- JASN SDHD Paper 2005Документ11 страницJASN SDHD Paper 2005Carlos EghiОценок пока нет
- Trombosit Dan D-Dimer (Inggris)Документ8 страницTrombosit Dan D-Dimer (Inggris)lidawatiОценок пока нет
- Rediana Murti N, Suryono, Jauhar FirdausДокумент6 страницRediana Murti N, Suryono, Jauhar Firdausrediana murti noviaОценок пока нет
- Fluid Resuscitation - Dita AditianingsihДокумент48 страницFluid Resuscitation - Dita AditianingsihGalih Wicaksono100% (1)
- Plasma Homocysteine and Total Thiol Content in Patients With Exudative Age-Related Macular DegenerationДокумент5 страницPlasma Homocysteine and Total Thiol Content in Patients With Exudative Age-Related Macular DegenerationAnonymous 1jCVqQuОценок пока нет
- Pathophysiology of COPDДокумент4 страницыPathophysiology of COPDrinieeeОценок пока нет
- Addison K May, MD John P Reilly, MD, Msce Scott Manaker, MD, PHD Arthur J Silvergleid, MD Geraldine Finlay, MD Contributor DisclosuresДокумент12 страницAddison K May, MD John P Reilly, MD, Msce Scott Manaker, MD, PHD Arthur J Silvergleid, MD Geraldine Finlay, MD Contributor DisclosuresAlvaro HaroОценок пока нет
- Original Article Coagulation Abnormalities in Patients With Chronic Liver Disease in PakistanДокумент5 страницOriginal Article Coagulation Abnormalities in Patients With Chronic Liver Disease in PakistanAsfandyar RoghaniОценок пока нет
- Cardio Resource UnitsДокумент31 страницаCardio Resource Unitsgraveheart11Оценок пока нет
- Stroke and LipidДокумент4 страницыStroke and LipidvenniariskiaОценок пока нет
- S64 FullДокумент3 страницыS64 FullkarenafiafiОценок пока нет
- Cardiorenal Syndrome: SciencedirectДокумент10 страницCardiorenal Syndrome: SciencedirectDwiFitriaAnggrainiОценок пока нет
- The Effect of Cilostazol On Right Heart FunctionДокумент43 страницыThe Effect of Cilostazol On Right Heart FunctionGunawan YogaОценок пока нет
- Cardiorenal SyndromeДокумент18 страницCardiorenal Syndromedauz3017Оценок пока нет
- 1 Hemofiltración RMH 1994Документ9 страниц1 Hemofiltración RMH 1994PILARICA201263Оценок пока нет
- Arterio-Venous Fistula Recirculation in Hemodialysis: Causes and PrevalencesДокумент8 страницArterio-Venous Fistula Recirculation in Hemodialysis: Causes and PrevalencesMashiur RahmanОценок пока нет
- 1 s2.0 073510979390668Q Main PDFДокумент9 страниц1 s2.0 073510979390668Q Main PDFPribac RamonaОценок пока нет
- Molecular Adsorbent Recirculating System and Single-Pass Albumin Dialysis in Liver Failure - A Prospective, Randomised Crossover StudyДокумент13 страницMolecular Adsorbent Recirculating System and Single-Pass Albumin Dialysis in Liver Failure - A Prospective, Randomised Crossover StudyRicardo RodriguezОценок пока нет
- 1757 7241 21 86Документ12 страниц1757 7241 21 86Nicco MarantsonОценок пока нет
- Acute Hypercalcemic Hypertension in Man: Role of Hemodynamics, Catecholamines, and ReninДокумент5 страницAcute Hypercalcemic Hypertension in Man: Role of Hemodynamics, Catecholamines, and ReninRo KohnОценок пока нет
- The Perindopril in Elderly PeopleДокумент8 страницThe Perindopril in Elderly PeopleluchititaОценок пока нет
- 8931 26614 2 PB PDFДокумент7 страниц8931 26614 2 PB PDFMaferОценок пока нет
- High Risk of Coagulopathy Among Type-2 Diabetes Mellitus Clients at A Municipal Hospital in GhanaДокумент7 страницHigh Risk of Coagulopathy Among Type-2 Diabetes Mellitus Clients at A Municipal Hospital in GhanaLovi AnaОценок пока нет
- Chiu 2016Документ7 страницChiu 2016alan arroyoОценок пока нет
- Jurnal Yang DipakeДокумент8 страницJurnal Yang DipakeEsy LОценок пока нет
- Syntax Score and Its Relation To Lipoprotein A - LP (A) and Extended Lipid Parameters in Non-Diabetic Patients With Acute Coronary Syndrome Having Age Below 55 YearsДокумент7 страницSyntax Score and Its Relation To Lipoprotein A - LP (A) and Extended Lipid Parameters in Non-Diabetic Patients With Acute Coronary Syndrome Having Age Below 55 YearsPremier PublishersОценок пока нет
- bb5 ClassifsofttissueДокумент5 страницbb5 ClassifsofttissueMuhammad MaulanaОценок пока нет
- Low Alt CKDДокумент5 страницLow Alt CKDFebianti RukmanaОценок пока нет
- QT Dispersion in Patients With Systemic Lupus Erythematosus: The Impact of Disease ActivityДокумент5 страницQT Dispersion in Patients With Systemic Lupus Erythematosus: The Impact of Disease ActivityWahyubudi PratamaОценок пока нет
- The Effect of Aerobic Exercise On Blood and Plasma Viscosity On Cardiac Health Club ParticipantsДокумент4 страницыThe Effect of Aerobic Exercise On Blood and Plasma Viscosity On Cardiac Health Club ParticipantsDedy SavradinataОценок пока нет
- Revisiting The Role of Oxygen Therapy in Cardiac Patients: Raman Moradkhan, MD, Lawrence I. Sinoway, MDДокумент4 страницыRevisiting The Role of Oxygen Therapy in Cardiac Patients: Raman Moradkhan, MD, Lawrence I. Sinoway, MDIda LemonОценок пока нет
- AnaemiaДокумент27 страницAnaemiaSamahir F HusseinОценок пока нет
- Hemodynamic Support in Fluid-Refractory Pediatric Septic ShockДокумент6 страницHemodynamic Support in Fluid-Refractory Pediatric Septic ShockJosé Pepo Apey ReinosoОценок пока нет
- Anemia and Thrombocytopenia in Acute and Chronic Renal Failure PDFДокумент6 страницAnemia and Thrombocytopenia in Acute and Chronic Renal Failure PDFSatriyo Dwi SuryantoroОценок пока нет
- Levosimendan in Perioperative Cardiothoracic Practice - A Narrative Review-FirstДокумент22 страницыLevosimendan in Perioperative Cardiothoracic Practice - A Narrative Review-FirstNehemias MD GuevaraОценок пока нет
- Mitrovic 2009Документ10 страницMitrovic 2009Lucas BragaОценок пока нет
- Bahan Referat Miocardial Stunning Perit Dial Int-2011-Selby-27-33Документ7 страницBahan Referat Miocardial Stunning Perit Dial Int-2011-Selby-27-33viniganorОценок пока нет
- A Randomized, Double Blind Comparison of Lactated.61Документ7 страницA Randomized, Double Blind Comparison of Lactated.61Temoc TemocОценок пока нет
- Comparison of The Plasma Levels of Apolipoproteins B and A-L, and Other Risk Factors in Men and Women With Premature Coronary Artery DiseaseДокумент7 страницComparison of The Plasma Levels of Apolipoproteins B and A-L, and Other Risk Factors in Men and Women With Premature Coronary Artery DiseaseCamilo HernándezОценок пока нет
- PIIS0016508597003843Документ8 страницPIIS0016508597003843Mudassar SattarОценок пока нет
- Shock Five Point ZeroДокумент78 страницShock Five Point ZeroprashsubbuОценок пока нет
- Alternatives to Blood Transfusion in Transfusion MedicineОт EverandAlternatives to Blood Transfusion in Transfusion MedicineAlice ManiatisОценок пока нет
- HDL PDFДокумент10 страницHDL PDFDiah Ayu AdiatiОценок пока нет
- CV MS 071209Документ5 страницCV MS 071209Diah Ayu AdiatiОценок пока нет
- Jurnal JantungДокумент11 страницJurnal JantungDiah Ayu AdiatiОценок пока нет
- Jurnal JantungДокумент9 страницJurnal JantungDiah Ayu AdiatiОценок пока нет
- Jurnal JantungДокумент10 страницJurnal JantungDiah Ayu AdiatiОценок пока нет
- Jurnal JantungДокумент11 страницJurnal JantungDiah Ayu AdiatiОценок пока нет
- Jurnal JantungДокумент14 страницJurnal JantungDiah Ayu AdiatiОценок пока нет
- Jurnal JantungДокумент7 страницJurnal JantungDiah Ayu AdiatiОценок пока нет
- Jurnal JantungДокумент11 страницJurnal JantungDiah Ayu AdiatiОценок пока нет
- Jurnal JantungДокумент7 страницJurnal JantungDiah Ayu AdiatiОценок пока нет
- SchizophreniaДокумент32 страницыSchizophreniaHerlina SihalohoОценок пока нет
- PJK JurnalДокумент4 страницыPJK JurnalDiah Ayu AdiatiОценок пока нет
- NeurotransmittersДокумент16 страницNeurotransmittersKiyomasa KatoОценок пока нет
- Corneal InfectionsДокумент8 страницCorneal InfectionsDiah Ayu AdiatiОценок пока нет
- JADASSmanagement Main PDFДокумент10 страницJADASSmanagement Main PDFPragatiОценок пока нет
- Nursing Practice IvДокумент24 страницыNursing Practice IvJohn wewОценок пока нет
- Gonad in The BodyДокумент10 страницGonad in The Bodyjuliana leonОценок пока нет
- Catecholamines and The Effects of Exercise, Training and GenderДокумент24 страницыCatecholamines and The Effects of Exercise, Training and GenderMenna Tesfaye MigbarОценок пока нет
- Group 2 Culture TechniqueДокумент38 страницGroup 2 Culture TechniqueBartazal dawaganОценок пока нет
- Digoxin Drug CardДокумент1 страницаDigoxin Drug CardMahsa Ahmadzadeh100% (2)
- Metabolic AlkalosisДокумент15 страницMetabolic AlkalosisMenna ElesawyОценок пока нет
- Nama BHP & Kode Barang Lab EkadaДокумент3 страницыNama BHP & Kode Barang Lab EkadaPipit latuОценок пока нет
- Lact2 2018-11 v12Документ4 страницыLact2 2018-11 v12Kouame FrancisОценок пока нет
- Infographic Folic Acid Vs FolateДокумент1 страницаInfographic Folic Acid Vs FolateKaterina PoposkaОценок пока нет
- 2021 Article 1063Документ15 страниц2021 Article 1063Raúl LópezОценок пока нет
- Lipid Catabolism: Overview of Lipid MetabolismДокумент3 страницыLipid Catabolism: Overview of Lipid Metabolismninafatima allamОценок пока нет
- Review of Digestion MetabolismДокумент4 страницыReview of Digestion MetabolismAntonia SalvadorОценок пока нет
- Efeito Browning Nos Adipócitos ApostilaДокумент31 страницаEfeito Browning Nos Adipócitos ApostilaRachel RodriguesОценок пока нет
- Adrenal Gland - Physiology, Pathology, and Pharmacology - Lecturio PDFДокумент8 страницAdrenal Gland - Physiology, Pathology, and Pharmacology - Lecturio PDFfaiz alamОценок пока нет
- 1700 Mock 2 PDFДокумент37 страниц1700 Mock 2 PDFSiraj Ul IslamОценок пока нет
- Male Reproductive SystemДокумент9 страницMale Reproductive SystemSarilyn Simon50% (2)
- John K. Mathai, Yanhong Liu and Hans H. SteinДокумент10 страницJohn K. Mathai, Yanhong Liu and Hans H. SteinDébora Giaretta ZattaОценок пока нет
- Bahasa Inggris 1.13Документ5 страницBahasa Inggris 1.13Rizky AdiОценок пока нет
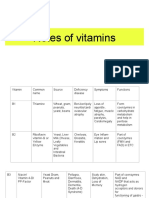
- Notes of VitaminsДокумент8 страницNotes of VitaminsEllyОценок пока нет
- Ang Tunay Na Excretory SystemДокумент17 страницAng Tunay Na Excretory SystemcjОценок пока нет
- GravoiДокумент6 страницGravoiPam Barboza100% (1)
- Week 6-7 - Environmental Health and ToxicologyДокумент33 страницыWeek 6-7 - Environmental Health and ToxicologyLorenz GarciaОценок пока нет
- Filesugd66484b .PDF 2Документ75 страницFilesugd66484b .PDF 2صاحب القلمОценок пока нет
- Endocrine SystemДокумент11 страницEndocrine Systemshannon c. lewisОценок пока нет
- Biology (Zoology, Botany, Health), Environment & AgricultureДокумент1 страницаBiology (Zoology, Botany, Health), Environment & AgriculturerjtbtbtbОценок пока нет
- A Wearable Electrochemical Biosensor For The Monitoring of Metabolites and NutrientsДокумент13 страницA Wearable Electrochemical Biosensor For The Monitoring of Metabolites and NutrientsBAUTISTA DIPAOLA100% (1)
- Notes For PediatricsДокумент38 страницNotes For PediatricsadamsamillionОценок пока нет