Академический Документы
Профессиональный Документы
Культура Документы
Endocrine
Загружено:
أحمدالشحاتАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Endocrine
Загружено:
أحمدالشحاتАвторское право:
Доступные форматы
Describe the location of the
pituitary gland. Where does it sit?
Lies below the brain in a small cavity
on the sphenoid bone called the
sella turcica
Describe the embryonic origin of
the posterior pituitary.
The neurohypophyseal bud grows
down from the floor of the future
diencephalon as a stalk (or
infundibulum) that remains
attached to the brain.
Describe the embryonic origin of
the anterior pituitary.
An outpocketing of oral ectoderm from the
primitive mouth grows cranially, forming the
hypophyseal (Rathke) pouch. The base of this
pouch eventually constricts and separates
from the pharynx, and the pouch's anterior
wall thickens greatly, reducing the lumen to a
small fissure.
What are the 2 parts of the
neurohypophysis?
Pars nervosa = large part
Infundibulum = stalk attached to the
hypothalamus at the median
eminence
What are the 3 parts of the
adenohypophysis?
Pars distalis = large part or anterior
lobe
Pars tuberalis = wraps around the
infundibulum
Pars intermedia = thin; adjacent to
the posterior pars nervosa
What is the bundle of axons that
courses into the neurohypophysis
from 2 important hypothalamic
nuclei?
What are the 2 important
hypothalamic nuclei that send
axons to the neurohypophysis?
Describe the blood supply of the
pituitary gland.
Hypothalamic-hypophyseal tract
Supraoptic (mostly ADH) and
paraventricular (mostly oxytocin)
nuclei
Superior hypophyseal arteries:
Supply the median eminence and infundibular stalk
Divide into a primary plexus of fenestrated capillaries that irrigate
the stalk and median eminence
These capillaries rejoin to form venules that branch again as a
larger secondary capillary plexus in the adenohypophysis.
These vessels make up the hypothalamic-hypophyseal portal
system.
Inferior hypophyseal arteries:
Provides blood mainly for the neurohypophysis
What are 2 broad groups of cells in
the pars distalis?
What are the acidophilic
chromophils in the pars distalis?
Chromophils = secretory cells in which hormone
is stored in cytoplasmic granules; may be
basophilic or acidophilic
Chromophobes = stain weakly; few or no
secretory granules; include stem and
undifferentiated progenitor cells as well as any
degranulated cells present
Somatotrophs = secrete GH
Lactotrophs = secrete prolactin
What are the basophilic
chromophils in the pars distalis?
Most of the cells of the pars
tuberalis are of what kind?
Gonadotrophs = secrete LH and FSH
Corticotrophs = synthesize POMC;
secrete ACTH and beta-lipotropin
Thyrotrophs = secrete TSH
Gonadotrophs
Describe the histology and origin of
the pars intermedia.
Thin zone of basophilic cells between the pars
distalis and the pars nervosa; the pars
nervosa is often invaded by the basophilic
cells; develops from the dorsal wall of the
hypophyseal pouch and usually contains
colloid-filled cysts of various sizes that
represent remnants of that structure's lumen
What does the pars intermedia
produce?
During fetal life, these cells produce
POMC. Unlike corticotrophs, these
cells cleave the POMC into 2 forms
of MSH, gamma-lipotropin, and
beta-endorphin
What are the 2 cell types in the
posterior pituitary?
1. Unmyelinated axons of large secretory
neurons that have their cell bodies in the
supraoptic and paraventricular nuclei of the
hypothalamus
2. Pituicytes = highly branched glial cells that
resemble astrocytes; most abundant cell type in
the posterior pituitary
What are the axonal dilations in the
pars nervosa where hormones
accumulate?
Neurosecretory bodies or Herring
bodies
Faintly eosinophilic structures
Contain membrane-bound granules
with either oxytocin or ADH bound
to neurophysin I or II, respectively
Describe the embryonic origin of
the adrenal glands.
Adrenal cortex = comes from
mesoderm
Adrenal medulla = comes from
neural crest
Describe the blood supply of the
adrenal glands.
Arteries --> cortical arterioles --> capillaries and
sinusoids that irrigate the cortex --> join medullary
capillaries and medullary arterioles that penetrate
directly to the medulla --> central medullary veins -->
suprarenal vein
Blood supply of medulla is dual: arterial blood from
medullary arterioles and venous blood from cortical
capillaries
Steroid-secreting cells:
Describe the ultrastructure of cells
of the adrenal cortex.
Acidophilic cytoplasm rich in lipid droplets
Central nuclei
Profuse SER with enzymes for cholesterol synthesis and
conversion of pregnenolone into steroid hormones
Spherical mitochondria with tubular (rather than shelf-like)
cristae; synthesize ATP, convert cholesterol to pregnenolone, and
perform some steps in steroid synthesis
What are the 3 concentric zones of
the adrenal cortex?
Zona glomerulosa
Zona fasciculata
Zona reticularis
Describe the zona glomerulosa.
Describe the zona fasciculata.
Describe the zona reticularis.
Immediately inside the capsule
15% of the cortex
Closely packed, rounded or arched
cords of columnar or pyramidal
cells with many capillaries
Main product = aldosterone
65-80% of the cortex
Long cords of large polyhedral cells; cords are
1-2 cells thick and are separated by
fenestrated sinusoidal capillaries
Products = mainly glucocorticoids (esp
cortisol); small amounts of weak androgens
are also produced here
Innermost
10% of the cortex
Smaller cells in a network of irregular cords
interspersed with wide capillaries
Cells are more heavily stained because they contain
fewer lipid droplets and more lipofuscin pigment
Products = mainly DHEA and androstenedione; small
amounts of glucocorticoids (cortisol)
Chromaffin cells
What are parenchymal cells of the
adrenal medulla called? What is
their origin?
What are pheochromocytomas?
Arise from neural crest cells, as do the postganglionic
neurons of sympathetic and parasympathetic ganglia
Chromaffin cells can be considered modified
sympathetic postganglionic neurons that lack axons
and dendrites and are specialized as secretory cells
Benign growths in the adrenal
medulla that secrete high levels of
catecholamines that affect blood
pressure
Describe the ultrastructure of
chromaffin cells.
Contain many electron-dense granules for
storage and secretion of catecholamines (Epi
and NE)
Both Epi and NE, together with Ca2+ and ATP,
are bound in granular storage complexes with
proteins called chromogranins
Islets of Langerhans are mostly
found in what part of the pancreas?
Tail of the pancreas
Only constitute 1-2% of the organ's
total volume
What is the embryonic origin of the
pancreatic islets?
Same as the exocrine pancreas:
originate as epithelial outgrowths
from the endoderm of the
developing gut tube
Delta cells = secrete somatostatin
Besides alpha and beta cells, what
other 3 cell types do islets of
Langerhans contain?
PP cells = secrete pancreatic polypeptide;
these cells are more common in islets located
within the head of the pancreas
Enterochromaffin cells
How do sympathetic and
parasympathetic fibers affect
glucagon and insulin release?
Sympathetic = stimulates glucagon
release; inhibits insulin release
Parasympathetic = stimulates
release of both insulin and glucagon
What is the embryonic origin of the
thyroid gland?
Describe the parenchyma of the
thyroid gland.
What protein does thyroid colloid
contain?
What are the main cells of the
thyroid gland? Describe them.
What is the second endocrine cell
type found in the thyroid gland?
What is their origin?
Originates in early embryonic life
from the foregut endoderm near
the base of the developing tongue
Millions of rounded epithelial
thyroid follicles, each with a simple
epithelium and a central lumen
densely filled with gelatinous
acidophilic colloid
Thyroglobulin
Contains 140 Tyr residues critical for
thyroid hormone synthesis
Released as an exocrine product
from apical vesicles of thyrocytes
into the follicular lumen
Thyrocytes
Apical junctional complexes
Rest on a basal lamina
Round, central nuclei
Basal RER
Apical Golgi, secretory granules, phagosomes,
and lysosomes
Apical microvilli
Parafollicular cells = C cells = secrete calcitonin
Located inside the basal lamina of the follicular
epithelium or as isolated clusters btw follicles
Neural crest origin
What transporters are involved in
iodine uptake by thyrocytes?
Basolateral Na+/I- symporter (NIS) =
uptake of iodide from the blood;
decreased plasma iodide triggers
increased NIS synthesis
Apical I-/Cl- transporter (pendrin) =
pumps I- from thyrocytes into the colloid
1. Secretion of thyroglobulin and iodide into the colloid
List the steps of thyroid hormone
synthesis.
2. Oxidation of iodide to iodine by membrane-bound thyroid peroxidase on the
microvilli surface of thyrocytes
3. Iodination of tyrosyl residues in thyroglobulin to form MIT or DIT
4. Formation of T3 (MIT + DIT) and T4 (2 DIT) in covalently conjugated coupling
reactions
5. Endocytosis of iodinated thyroglobulin and degradation of thyroglobulin by
lysosomal proteases, freeing T3 and T4
6. Secretion of T3 and T4 at the basolateral surface
Which thyroid hormone is more
abundant in the blood? Which is
more active? How is the more active
form generated by the tissues?
What is the embryologic origin of
the parathyroid glands?
What are the endocrine cells of the
parathyroid gland called? Describe
these cells.
More abundant = T4
More potent = T3
Tissues use the enzyme 5'-iodinase
to convert T4 to T3
Pharyngeal pouches:
Superior glands come from the 4th pouch
Inferior glands come from the 3rd pouch
Their migration to the developing thyroid gland is
sometimes misdirected. Up to 10% of people have
parathyroid tissue attached to the thymus, which
originates from the same pharyngeal pouches
Principal (chief) cells
Small polygonal cells with round
nuclei and pale-staining, slightly
acidophilic cytoplasm and
irregularly shaped granules
containing PTH
Oxyphil cells
What cell type may appear in the
parathyroid glands of older people?
Describe these cells.
Much larger than the principal cells;
characterized by very acidophilic cytoplasm filled
with abnormally shaped mitochondria
What is the pineal gland also known
as?
Epiphysis cerebri
Where is the pineal gland located?
What is its origin?
What is the pineal gland covered
by?
What are the secretory cells of the
pineal gland called?
Some oxyphil cells show low levels of PTH
synthesis
Develops from neuroectoderm in
the posterior wall of the 3rd
ventricle and remains attached to
the brain by a short stalk
Pia mater
Pinealocytes
Basophilic cytoplasm; irregular
euchromatic nuclei; secretory vesicles;
mitochondria; long cytoplasmic
processes that extend to the
vascularized septa, where they end in
dilatations near capillaries
What do pinealocytes produce?
Melatonin
Release is promoted by darkness
and inhibited by daylight
Melatonin is a derivative of what?
Tryptophan
How is light stimuli info relayed to
the pineal gland?
Detection within the retinas
Transmission to the pineal via the
retinohypothalamic tract, the
suprachiasmatic nucleus, and the
tracts of sympathetic fibers that
enter the pineal gland
What other cell type, besides
pinealocytes, is present in the
pineal gland?
Modified Astrocytes (GFAP +)
5% of the cells
Usually found in perivascular areas
and btw groups of pinealocytes
What are the characteristic
concretions of calcium and
magnesium salts in the pineal gland
called?
Corpora arenacea
Appear during childhood and
increase in number and size with
age with no apparent effect on
function
Вам также может понравиться
- Wdhllohb Ihbknjk KJJGKJVM, MBJHV.L ., KBKJB, NGKJV,,.N, V HJKДокумент1 страницаWdhllohb Ihbknjk KJJGKJVM, MBJHV.L ., KBKJB, NGKJV,,.N, V HJKأحمدالشحاتОценок пока нет
- MNBДокумент1 страницаMNBأحمدالشحاتОценок пока нет
- Physiology of The Kidey NMMMMMMMMM N, MBNV NMBNN NMBNMBNДокумент1 страницаPhysiology of The Kidey NMMMMMMMMM N, MBNV NMBNN NMBNMBNأحمدالشحاتОценок пока нет
- MCQ Bacteriology 31Документ9 страницMCQ Bacteriology 31أحمدالشحات100% (1)
- Ent CaseДокумент1 страницаEnt CaseأحمدالشحاتОценок пока нет
- New Text DocumentДокумент3 страницыNew Text DocumentأحمدالشحاتОценок пока нет
- اشهر اسئله لدكتور دينا شكرىДокумент6 страницاشهر اسئله لدكتور دينا شكرىأحمدالشحاتОценок пока нет
- MSSBДокумент1 страницаMSSBأحمدالشحاتОценок пока нет
- OphthslДокумент1 страницаOphthslأحمدالشحاتОценок пока нет
- New Text DocumentДокумент1 страницаNew Text DocumentأحمدالشحاتОценок пока нет
- New Text DocumentДокумент7 страницNew Text DocumentأحمدالشحاتОценок пока нет
- New Text DocumentДокумент6 страницNew Text DocumentأحمدالشحاتОценок пока нет
- Cell Injury and AdaptationДокумент33 страницыCell Injury and AdaptationأحمدالشحاتОценок пока нет
- New Text DocumentДокумент3 страницыNew Text DocumentأحمدالشحاتОценок пока нет
- New Text DocumentДокумент10 страницNew Text DocumentأحمدالشحاتОценок пока нет
- New Text DocumentДокумент4 страницыNew Text DocumentأحمدالشحاتОценок пока нет
- New Text DocumentДокумент2 страницыNew Text DocumentأحمدالشحاتОценок пока нет
- MRCP Material Drive PDFДокумент2 страницыMRCP Material Drive PDFأحمدالشحات100% (1)
- Causes Symptoms Treatment Orthostatic HypotensionДокумент9 страницCauses Symptoms Treatment Orthostatic HypotensionأحمدالشحاتОценок пока нет
- Pass & SketchyДокумент1 страницаPass & Sketchyأحمدالشحات100% (1)
- Accessory GI OrgansДокумент10 страницAccessory GI OrgansأحمدالشحاتОценок пока нет
- FalcoДокумент1 страницаFalcoأحمدالشحاتОценок пока нет
- RespiratoryДокумент14 страницRespiratoryأحمدالشحاتОценок пока нет
- UsbnvДокумент1 страницаUsbnvأحمدالشحاتОценок пока нет
- Set 3c271ab3Документ12 страницSet 3c271ab3أحمدالشحاتОценок пока нет
- ReproductiveДокумент28 страницReproductiveأحمدالشحاتОценок пока нет
- PharmacologyДокумент9 страницPharmacologyRVDОценок пока нет
- SkinДокумент6 страницSkinأحمدالشحاتОценок пока нет
- UrinaryДокумент10 страницUrinaryأحمدالشحاتОценок пока нет
- GitДокумент20 страницGitأحمدالشحاتОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- CHB1 Assignmen5Документ2 страницыCHB1 Assignmen5anhspidermenОценок пока нет
- Lecture 6-Design For ShearДокумент14 страницLecture 6-Design For ShearMarkos DanielОценок пока нет
- U-PJT WASHER-MD SimpleUX WEB SSEC-01 EU EnglishДокумент76 страницU-PJT WASHER-MD SimpleUX WEB SSEC-01 EU EnglishszerenguettiОценок пока нет
- 3000 Most Common Words in EnglishДокумент85 страниц3000 Most Common Words in Englishapi-575590272100% (1)
- Kavanaugh On Philosophical EnterpriseДокумент9 страницKavanaugh On Philosophical EnterprisePauline Zoi RabagoОценок пока нет
- 713 Catalog PagesДокумент2 страницы713 Catalog PagesJosé AcostaОценок пока нет
- Travel Agency ManagementДокумент47 страницTravel Agency ManagementKatherine BarretoОценок пока нет
- Dewatering Well PointsДокумент4 страницыDewatering Well Pointssalloum3Оценок пока нет
- EtomДокумент1 страницаEtomarthryxОценок пока нет
- Sewer CadДокумент10 страницSewer CadAlvaro Jesus Añazco YllpaОценок пока нет
- Mock DataДокумент56 страницMock DataAnonymous O2bvbOuОценок пока нет
- Mock PPT 2023 TietДокумент22 страницыMock PPT 2023 Tiettsai42zigОценок пока нет
- Excel Data AnalysisДокумент30 страницExcel Data AnalysisРоман УдовичкоОценок пока нет
- MST 2 ReviewerДокумент4 страницыMST 2 ReviewerAizha NarioОценок пока нет
- CLOZE TEST Fully Revised For SSC, Bank Exams & Other CompetitiveДокумент57 страницCLOZE TEST Fully Revised For SSC, Bank Exams & Other CompetitiveSreenu Raju100% (2)
- The Effects of Self-Esteem On Makeup InvolvementДокумент9 страницThe Effects of Self-Esteem On Makeup InvolvementMichelle Nicole Tagupa SerranoОценок пока нет
- Running Head:: Describe The Uses of Waiting Line AnalysesДокумент6 страницRunning Head:: Describe The Uses of Waiting Line AnalysesHenry AnubiОценок пока нет
- Electromagnetic Braking SystemДокумент14 страницElectromagnetic Braking SystemTanvi50% (2)
- Stage TwoДокумент34 страницыStage TwoThar LattОценок пока нет
- Investigation of Twilight Using Sky Quality Meter For Isha' Prayer TimeДокумент1 страницаInvestigation of Twilight Using Sky Quality Meter For Isha' Prayer Timeresurgam52Оценок пока нет
- Smell Detectives: An Olfactory History of Nineteenth-Century Urban AmericaДокумент35 страницSmell Detectives: An Olfactory History of Nineteenth-Century Urban AmericaUniversity of Washington PressОценок пока нет
- 2002 AriДокумент53 страницы2002 AriMbarouk Shaame MbaroukОценок пока нет
- Wiley Wesleyan UniversityДокумент36 страницWiley Wesleyan UniversityBirunda SilvaОценок пока нет
- Crafting and Executing StrategyДокумент33 страницыCrafting and Executing Strategyamoore2505Оценок пока нет
- A Hirshfeld Surface Analysis and Crystal StructureДокумент8 страницA Hirshfeld Surface Analysis and Crystal StructureLidiane MicheliniОценок пока нет
- Radiograph Evaluation ChecklistДокумент2 страницыRadiograph Evaluation ChecklistZulfadli Haron100% (1)
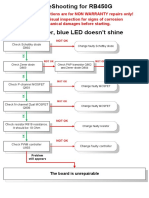
- RB450G Trouble ShootingДокумент9 страницRB450G Trouble Shootingjocimar1000Оценок пока нет
- 3.1-Pile Design Calculation For Boundary (p1 To p50)Документ24 страницы3.1-Pile Design Calculation For Boundary (p1 To p50)layaljamal2Оценок пока нет
- 31 Legacy of Ancient Greece (Contributions)Документ10 страниц31 Legacy of Ancient Greece (Contributions)LyreОценок пока нет