Академический Документы
Профессиональный Документы
Культура Документы
Stroke Journal
Загружено:
Eufrasia VictaИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Stroke Journal
Загружено:
Eufrasia VictaАвторское право:
Доступные форматы
Page 1 of 7
View this article online at: patient.info/health/stroke-leaflet
Stroke
A stroke causes damage to the brain. A common cause of stroke is a blood clot that forms in a brain
blood vessel (artery). Immediate treatment may include a clot-busting medicine to dissolve the blood
clot. Other treatments include medication to reduce risk factors for further strokes. Rehabilitation is a
major part of treatment. Disability following a stroke depends on factors such as the part of the brain
affected, how quickly treatment was given and the extent of the damage to the brain. Call for an
ambulance immediately if you suspect someone is having a stroke. Common symptoms are listed
below.
What is a stroke and what causes it?
A stroke means that the blood supply to a part of the brain is suddenly cut off. The brain cells need a constant
supply of oxygen from the blood. Soon after the blood supply is cut off, the cells in the affected area of brain
become damaged or die. A stroke is sometimes called a brain attack.
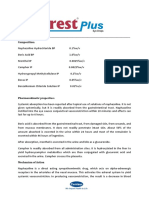
The blood supply to the brain comes mainly from four blood vessels (arteries) - the right and left carotid arteries
and the right and left vertebrobasilar arteries (see diagram below). These branch into many smaller arteries
which supply blood to all areas of the brain. The area of brain affected and the extent of the damage depend on
which blood vessel is affected.
For example, if you lose the blood supply from a main carotid artery then a large area of your brain is affected,
which can cause severe symptoms or death. In contrast, if a small branch artery is affected then only a small
area of brain is damaged which may cause relatively minor symptoms.
There are two main types of stroke - ischaemic and haemorrhagic.
Page 2 of 7
Ischaemic stroke - caused by a blood clot
Ischaemic means a reduced blood and oxygen supply to a part of the body. It is usually caused by blood clot in an
artery, which blocks the flow of blood. This occurs in about 7 in 10 cases.
The blood clot often forms within the artery itself. This commonly occurs over a patch of fatty material
called atheroma. Atheroma is often called furring or hardening of the arteries. Small patches of
atheroma form on the inside of arteries in most older people. If a patch of atheroma becomes thick, it
can trigger the blood to clot.
In some cases, the blood clot forms in another part of the body and then travels in the bloodstream this is called an embolus. The most common example is a blood clot which forms in a heart chamber
as a result of abnormal turbulent blood flow. This may occur in a condition called atrial fibrillation. See
separate leaflet called Atrial Fibrillation for more detail. The blood clot is then carried in the bloodstream
until it gets stuck in an artery in the brain.
There are other rare causes of ischaemic stroke.
Haemorrhagic stroke - caused by bleeding
A damaged or weakened artery may burst and bleed:
An intracerebral haemorrhage occurs when the blood vessel bursts inside the brain. The blood then
spills into the nearby brain tissue. This can cause the affected brain cells to lose their oxygen supply.
They become damaged or die. This happens in about 1 in 10 strokes.
A subarachnoid haemorrhage occurs when a blood vessel bursts in the subarachnoid space. This is
the narrow space between the brain and the skull. This space is normally filled with a fluid called the
cerebrospinal fluid. About 1 stroke in 20 is due to a subarachnoid haemorrhage.
Uncertain cause
The cause is uncertain in a small number of strokes.
Who is affected by stroke?
Each year around 120,000 people in the UK have a first stroke and about 30,000 have a recurrent stroke. Stroke
is the largest cause of disability in the UK and the third most common cause of death (after heart disease and
cancer). Most cases occur in people aged over 65. Each year about 1 in 100 people over the age of 75 will have a
stroke. But a stroke can occur at any age - even in babies. About one million people in the UK are living with the
effects of stroke. Half of these people depend on others for help with everyday activities.
What are the symptoms of a stroke?
The functions of the different parts of the body are controlled by different parts of the brain. So, the symptoms
vary depending on which part of the brain is affected and on the size of the damaged area. Symptoms develop
suddenly and usually include one or more of the following:
Weakness of an arm, leg, or both. This may range from total paralysis of one side of the body to mild
clumsiness of one hand.
Weakness and twisting of one side of the face. This may cause you to drool saliva.
Problems with balance, co-ordination, vision, speech, communication or swallowing.
Dizziness or unsteadiness.
Numbness in a part of the body.
Headache.
Confusion.
Loss of consciousness (occurs in severe cases).
Page 3 of 7
What is a mini-stroke?
A mini-stroke is a set of symptoms similar to a stroke but which last for less than 24 hours. It is due to a
temporary lack of blood to a part of the brain. It is more correctly called a transient ischaemic attack (TIA). In most
cases, a TIA is caused by a tiny blood clot that becomes stuck in a small blood vessel (artery) in the brain. This
blocks the blood flow and a part of the brain is starved of oxygen. The affected part of the brain is without oxygen
for just a few minutes and soon recovers. This is because the blood clot either breaks up quickly or nearby blood
vessels are able to compensate.
Unlike a stroke, the symptoms of a TIA soon go. However, you should see a doctor urgently if you have a TIA, as
you are at increased risk of having a full stroke. See separate leaflet called Transient Ischaemic Attack for more
detail.
A quick guide for the general public to remember
Both a stroke and a TIA are medical emergencies and need immediate medical attention. As a way of helping the
general public to become more aware of the symptoms of a stroke or TIA, a simple symptom checklist to
remember has been devised and publicised. This is to think of the word FAST. That is:
F - Facial weakness. Can the person smile? Has their mouth or eye drooped?
A - Arm weakness. Can the person raise both arms?
S - Speech disturbance. Can the person speak clearly? Can they understand what you say?
T - Time to call 999/112/911.
If any of these symptoms suddenly develop then the person needs to see a doctor urgently. So call an ambulance
FAST. The FAST checklist does not cover every possible symptom of stroke or TIA. However, it is easy to
remember and it is estimated that about 8 or 9 in 10 people with a stroke or TIA will have one or more FAST
symptoms.
What are the long-term effects from having a stroke?
The type and extent of disability caused by a stroke can vary greatly. It depends on the extent of the damage to
the brain.
A large stroke can cause death. A small stroke may cause minor problems, which may go completely over time.
In many cases the effects are somewhere in between these two extremes.
The sort of problems that may occur include one or more of the following:
Weakness of one side of the body. This may cause problems with walking if a leg is affected or
problems using an arm or hand properly.
Problems with balance and co-ordination.
Page 4 of 7
Swallowing problems are common. In some cases this can be dangerous, as food may go down
the windpipe rather than down the gullet when you eat. Because of this, it is usual to do a swallow test
on all people with a stroke before they are allowed to eat or drink. This is to make sure that swallowing
is safe. If there is severe difficulty with swallowing then you may need to have food and drinks passed
into your stomach via a tube.
Speech and communication difficulties. This may range from a difficulty in finding the correct
words to say in the middle of a sentence to being completely unable to speak. Also, understanding
speech, reading or writing may be affected.
Difficulty with vision. If a part of the brain that deals with vision is affected then problems may arise.
For example, some people who have had a stroke have double vision. Some people lose half of their
field of vision.
Difficulties with mental processes. For example, difficulty in learning, concentrating, remembering,
etc.
Inappropriate emotions. For example, following a stroke, some people cry or laugh at times for no
apparent reason.
Tiredness.
The above are just some examples of what may occur following a stroke. Every stroke is different and the
problems and difficulties have to be assessed for each affected person.
In the first few weeks after a stroke the swelling and inflammation around the damaged brain tissue settles down.
Some symptoms may then improve. In time, sometimes other parts of the brain can compensate for the
damaged part of the brain. With rehabilitation and appropriate therapy, there may be a gradual improvement.
Of those people who survive a stroke, about 3 in 10 are fully independent within three weeks. This rises to about
5 in 10 within six months. However, it is common for some degree of disability to remain.
Are any tests needed?
A doctor can usually diagnose a stroke by the typical symptoms and signs which develop suddenly. Tests which
are commonly done include:
A brain scan (CT scan or MRI scan). This can determine the type of stroke (ischaemic or
haemorrhagic) and may detect rarer conditions which may have caused the stroke or which may
mimic a stroke.
Blood tests to check on such things as blood sugar level and cholesterol level. High levels can
increase the risk of a further stroke.
Chest X-ray and a heart tracing (electrocardiogram, or ECG) to check for heart or lung conditions
which may be a cause of stroke (for example, atrial fibrillation).
Ultrasound scan of the carotid blood vessels (arteries) in the neck to check if there are large patches
of atheroma in these arteries.
What treatment and care are usual for people who have a stroke?
If you suspect that you (or a person you are with) are having a stroke then call for an ambulance immediately. You
should be admitted to hospital.
Immediate care
Ideally, you will be assessed quickly by a doctor. Commonly, a scan of the brain is organised as soon as
possible. The aim of the scan is to confirm the diagnosis and to tell whether the stroke is an ischaemic or
haemorrhagic stroke. This is very important to know, as the initial treatment of the two is very different.
If an ischaemic stroke is diagnosed and it has been less than four and a half hours since symptoms started, you
may be given a medicine directly into a vein, called alteplase. This is a clot-busting medicine which aims to
dissolve the blood clot. The medical word for this is thrombolysis. If the blood clot that caused the stoke can be
dissolved shortly after symptoms begin, it can improve the eventual outcome. This is because brain cells that
would have died are able to survive.
Page 5 of 7
Further early treatment
A plan for any other treatments should be devised and started as soon as possible. Treatments should be tailored
to the particular need of the individual. The treatment plan can depend on factors such as the severity of the
stroke, the effects it has, the cause of the stroke, and other diseases that may be present. Treatments that may
be considered include the following:
Antiplatelet medication. Platelets are tiny particles in the blood which help blood to clot. Antiplatelet medication is
usually advised if you have had an ischaemic stroke (due to a blood clot). Antiplatelet medication reduces the
stickiness of platelets. This helps to prevent blood clots forming inside arteries, which helps to prevent a further
stroke. Aspirin (low-dose) is the most commonly used antiplatelet medicine when the stroke has just happened.
Another antiplatelet medicine, clopidogrel, is usually given long-term after the initial treatment.
If you are unable to swallow, you will be given food and fluids via a tube that is passed into your stomach. As
mentioned earlier, a swallowing test is usually done early after being admitted to hospital.
Medication may be advised to reduce any risk factors for having a further stroke (as discussed later in this
leaflet). For example, medication to lower a raised blood pressure, sugar level or cholesterol level.
If you have atrial fibrillation, you have an increased risk of a blood clot forming in a heart chamber and travelling to
the brain to cause a stroke. If you have atrial fibrillation (or certain other heart conditions), a medicine called
warfarin may be prescribed. Warfarin helps to prevent blood clots forming. Warfarin is an anticoagulant.
If you have carotid stenosis then you have an increased risk of having a stroke. Carotid stenosis means a
narrowing of one of your carotid arteries, due to atheroma. If the narrowing is severe, you may be advised to have
surgery to strip out the atheroma. Your doctor will advise if this is an option.
If you have a bleeding (haemorrhagic) stroke and are taking an anticoagulant medicine such as warfarin,
treatment to reverse the effect of the anticoagulation is given.
If a subarachnoid haemorrhage is the cause of the stroke, an operation to fix the leaking blood vessel (artery) is
sometimes an option.
Other operations are occasionally done. For example, sometimes surgery is considered to ease the pressure
within the skull if the pressure becomes high following certain types of stroke.
As soon as possible after having a stroke you should be helped to sit up in bed and to get out of bed and move
around if you are able to do so. This is to start the process of rehabilitation as soon as possible. Also, this
reduces the risk of having a deep vein thrombosis (DVT) in a leg vein, which is a risk if you are inactive in bed for
long periods.
Rehabilitation
The aim of rehabilitation is to maximise activity and quality of life following a stroke. Hospitals which deal with
stroke patients have various specialists who help in rehabilitation. These include physiotherapists, occupational
therapists, speech therapists, dieticians, psychologists, specialist nurses and doctors. One or more of these
may be required, depending on how the stroke has affected you. Good-quality rehabilitation is vital following a
stroke and can make a big difference to your eventual outcome.
Can strokes be prevented?
As described above, a common reason why a blood clot forms is because it develops over a patch of atheroma
on the lining of a blood vessel (artery). Certain risk factors increase the chance of atheroma forming - which
increase your risk of having a stroke (and heart attack). You can reduce the risk of having a stroke (or a further
stroke) if you reduce your risk factors. These are briefly mentioned below but are dealt with in more detail in a
separate leaflet called Preventing Cardiovascular Diseases. Briefly, risk factors that can be modified are:
Smoking. If you smoke, you should make every effort to stop. The chemicals in tobacco are carried in
your bloodstream and can damage your arteries. If you smoke, stopping smoking can greatly cut your
risk of having a stroke.
Page 6 of 7
High blood pressure. Make sure your blood pressure is checked at least once a year. If it is high it
can be treated. High blood pressure usually causes no symptoms but can be damaging to the
arteries. If you have high blood pressure, treatment of the blood pressure is likely to have the greatest
effect on reducing your risk of having a stroke.
If you are overweight , losing some weight is advised.
Ahigh cholesterol level . This can be treated if it is high.
Inactivity. If able, you should aim to do some moderate physical activity on most days of the week for
at least 30 minutes. For example, brisk walking, swimming, cycling, dancing, gardening, etc.
Diet. You should aim to eat a healthy diet. Briefly, a healthy diet means:
AT LEAST five portions or ideally 7-9 portions of a variety of fruit and vegetables per day.
A THIRD OF MOST MEALS should be starch-based foods (such as cereals, wholegrain
bread, potatoes, rice, pasta), plus fruit and vegetables.
NOT MUCH fatty food such as fatty meats, cheeses, full-cream milk, fried food, butter, etc.
Use low-fat, mono- or poly-unsaturated spreads.
INCLUDE 2-3 portions of fish per week. At least one of these should be oily (such as
herring, mackerel, sardines, kippers, pilchards, salmon or fresh tuna).
If you eat red meat, it is best to eat lean red meat or poultry such as chicken.
If you do fry, choose a vegetable oil such as sunflower, rapeseed or olive.
Try not to add salt to food, and limit foods which are salty.
Alcohol. Do not drink more than the recommended limits. That is, men should drink no more than 21
units of alcohol per week, no more than four units in any one day and have at least two alcohol-free
days a week. Women should drink no more than 14 units of alcohol per week, no more than three
units in any one day and have at least two alcohol-free days a week. Pregnant women should not drink
at all. One unit is in about half a pint of normal strength beer, or two thirds of a small glass of wine, or
one small pub measure of spirits.
Diabetes is a risk factor. If you have diabetes, treatment to keep your blood sugar as near normal as
possible is important.
People with atrial fibrillation have an increased risk of having a stroke. This increased risk can also be reduced.
See the separate leaflet called Preventing Stroke When You Have Atrial Fibrillation for more details.
Further help & information
Stroke Association
Stroke Association House, 240 City Road, London, EC1V 2PR
Tel: (Helpline) 0303 303 3100, (General) 020 7566 0300
Web: www.stroke.org.uk
Chest, Heart and Stroke Northern Ireland
21 Dublin Road, Belfast, BT2 7HB
Tel: 028 9032 0184
Web: www.nichs.org.uk
Chest Heart and Stroke Scotland
Third Floor, Rosebery House, 9 Haymarket Terrace, Edinburgh, EH12 5EZ
Tel: (Advice Line) 0845 077 6000, (General) 0131 225 6963
Web: www.chss.org.uk
Different Strokes
9 Canon Harnett Court, Wolverton Mill, Milton Keynes, MK12 5NF
Tel: 01908 317618 or 0845 130 7172
Web: www.differentstrokes.co.uk
Page 7 of 7
Further reading & references
Stroke: The diagnosis and acute management of stroke and transient ischaemic attack (TIA); NICE Clinical Guideline (July
2008)
Prevention of cardiovascular disease - Guidance on the prevention of cardiovascular disease at the population level ; NICE
Public Health Guideline (June 2010)
National clinical guidelines for stroke (fourth edition); Royal College of Physicians (2012)
Sandercock PA, Counsell C, Gubitz GJ, et al; Antiplatelet therapy for acute ischaemic stroke. Cochrane Database Syst Rev.
2008 Jul 16;(3):CD000029.
The evidence base for alcohol guidelines; Royal College of Physicians (2011)
Young J, Forster A; Review of stroke rehabilitation. BMJ. 2007 Jan 13;334(7584):86-90.
UK Stroke Contacts Map; Stroke Association
Disclaimer: This article is for information only and should not be used for the diagnosis or treatment of medical
conditions. EMIS has used all reasonable care in compiling the information but make no warranty as to its
accuracy. Consult a doctor or other health care professional for diagnosis and treatment of medical conditions.
For details see our conditions.
Original Author:
Dr Tim Kenny
Current Version:
Dr Colin Tidy
Peer Reviewer:
Dr John Cox
Document ID:
4338 (v44)
Last Checked:
29/05/2015
Next Review:
28/05/2018
View this article online at: patient.info/health/stroke-leaflet
Discuss Stroke and find more trusted resources at Patient.
EMIS Group plc - all rights reserved.
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Conceptual Foundations of Occupational Therapy PracticeДокумент332 страницыConceptual Foundations of Occupational Therapy PracticeGabi Timo94% (16)
- A Case-Based Guide To Clinical Endocrinology (October 23, 2015) - (1493920588) - (Springer)Документ434 страницыA Case-Based Guide To Clinical Endocrinology (October 23, 2015) - (1493920588) - (Springer)AbdulraHman KhalEd100% (2)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Psychiatric Case History NotesДокумент8 страницPsychiatric Case History NotesTysle100% (1)
- Chemicals Zetag MSDS Powder Zetag 4139 - 1010Документ6 страницChemicals Zetag MSDS Powder Zetag 4139 - 1010PromagEnviro.comОценок пока нет
- Einstein's Theory of Relativity Explained Through His Life and CareerДокумент4 страницыEinstein's Theory of Relativity Explained Through His Life and Careeray2004jan29% (7)
- Essential hygiene and safety practices for body, home and cookingДокумент3 страницыEssential hygiene and safety practices for body, home and cookingNorma Nieves QuesadaОценок пока нет
- Mini Question Bank - Vety Sci - For Students PDFДокумент106 страницMini Question Bank - Vety Sci - For Students PDFRakesh Prajapati100% (3)
- Wound Closure ManualДокумент127 страницWound Closure ManualDougyStoffell100% (5)
- Yoga Decreases Kyphosis in Senior WomenДокумент19 страницYoga Decreases Kyphosis in Senior WomenEufrasia VictaОценок пока нет
- Understanding Cycle Threshold (CT) in Sars-Cov-2 RT-PCR: A Guide For Health Protection TeamsДокумент12 страницUnderstanding Cycle Threshold (CT) in Sars-Cov-2 RT-PCR: A Guide For Health Protection TeamsDika 20152016Оценок пока нет
- Efficacy and Safety of Topical AntifungalsДокумент17 страницEfficacy and Safety of Topical AntifungalsEufrasia VictaОценок пока нет
- Efficacy and Safety of Topical AntifungalsДокумент17 страницEfficacy and Safety of Topical AntifungalsEufrasia VictaОценок пока нет
- Scoliosis and Kyphosis PDFДокумент5 страницScoliosis and Kyphosis PDFEufrasia VictaОценок пока нет
- Postural Variables in Girls Practicing VolleyballДокумент2 страницыPostural Variables in Girls Practicing VolleyballEufrasia VictaОценок пока нет
- Guide to Stroke: Causes, Symptoms, and TreatmentДокумент13 страницGuide to Stroke: Causes, Symptoms, and TreatmentEufrasia VictaОценок пока нет
- Adult Scoliosis - A Quantitative Radiographic and Clinical AnalysisДокумент1 страницаAdult Scoliosis - A Quantitative Radiographic and Clinical AnalysisEufrasia VictaОценок пока нет
- Development Os A Smart Garment To Reduce Kyphosis During Daily LivingДокумент9 страницDevelopment Os A Smart Garment To Reduce Kyphosis During Daily LivingEufrasia VictaОценок пока нет
- GPAQ Instrument and Analysis Guide v2 PDFДокумент25 страницGPAQ Instrument and Analysis Guide v2 PDFEufrasia VictaОценок пока нет
- Epidemiology of Autism in Adult Across Age Groups and Ability LevelsДокумент20 страницEpidemiology of Autism in Adult Across Age Groups and Ability LevelsEufrasia VictaОценок пока нет
- Guidelines For Data Processing and Analysis of The International Physical Activity Questionnaire (IPAQ)Документ15 страницGuidelines For Data Processing and Analysis of The International Physical Activity Questionnaire (IPAQ)Nicola Pendleton100% (2)
- Correlation of Back Extensor Strength With Kyphosis and LordosisДокумент1 страницаCorrelation of Back Extensor Strength With Kyphosis and LordosisEufrasia VictaОценок пока нет
- Curve Patterns in Idiopathic ScoliosisДокумент1 страницаCurve Patterns in Idiopathic ScoliosisEufrasia VictaОценок пока нет
- Thoracic Kyphosis in Women With OsteoporosisДокумент1 страницаThoracic Kyphosis in Women With OsteoporosisEufrasia VictaОценок пока нет
- Relationship Between Temprament and Character and Psychotic Like Experiences in Healthy Children and Adolescent PDFДокумент6 страницRelationship Between Temprament and Character and Psychotic Like Experiences in Healthy Children and Adolescent PDFEufrasia VictaОценок пока нет
- Urban Adolescents - Role of Physical Activity, Diet, and GeneticsДокумент1 страницаUrban Adolescents - Role of Physical Activity, Diet, and GeneticsEufrasia VictaОценок пока нет
- Predicting Suicide Following Self-Harm - Systematic Review of Risk Factors and Risk ScalesДокумент27 страницPredicting Suicide Following Self-Harm - Systematic Review of Risk Factors and Risk ScalesEufrasia VictaОценок пока нет
- Sleep, Life, and InterventionДокумент2 страницыSleep, Life, and InterventionEufrasia VictaОценок пока нет
- Treatment of Opioid Use DisordersДокумент12 страницTreatment of Opioid Use DisordersEufrasia VictaОценок пока нет
- Lifestyle Medicine For Prevention of Cognitive Decline - Focus On Green TeaДокумент3 страницыLifestyle Medicine For Prevention of Cognitive Decline - Focus On Green TeaEufrasia VictaОценок пока нет
- Relationship Between Temprament and Character and Psychotic Like Experiences in Healthy Children and Adolescent PDFДокумент6 страницRelationship Between Temprament and Character and Psychotic Like Experiences in Healthy Children and Adolescent PDFEufrasia VictaОценок пока нет
- Sleep, Life, and InterventionДокумент2 страницыSleep, Life, and InterventionEufrasia VictaОценок пока нет
- 2010 Aetiological Diagnosis of Ischaemic Stroke in Young AdultsДокумент12 страниц2010 Aetiological Diagnosis of Ischaemic Stroke in Young AdultsHenri PurnomoОценок пока нет
- Journal StrokeДокумент13 страницJournal StrokeEufrasia VictaОценок пока нет
- Correlation of Back Extensor Strength With Kyphosis and LordosisДокумент1 страницаCorrelation of Back Extensor Strength With Kyphosis and LordosisEufrasia VictaОценок пока нет
- The Etiology and Pathogenesis of Idiopathic Scoliosis.Документ1 страницаThe Etiology and Pathogenesis of Idiopathic Scoliosis.Eufrasia VictaОценок пока нет
- Correlation Between Backpack Weight and Way of CarryingДокумент2 страницыCorrelation Between Backpack Weight and Way of CarryingEufrasia VictaОценок пока нет
- Postural Variables in Girls Practicing VolleyballДокумент2 страницыPostural Variables in Girls Practicing VolleyballEufrasia VictaОценок пока нет
- Chapter 11 2012 EditionДокумент215 страницChapter 11 2012 EditionLuis Soriano MitraОценок пока нет
- Parental Alienation Is SERIOUS Child Abuse 2018 Wilfrid Von Boch-Galhau Parental Alienation Is in The DSMДокумент15 страницParental Alienation Is SERIOUS Child Abuse 2018 Wilfrid Von Boch-Galhau Parental Alienation Is in The DSML9at100% (6)
- Unipex - Technical - Exo-PДокумент6 страницUnipex - Technical - Exo-PFelpnilОценок пока нет
- Mink Dissection InstructionsДокумент15 страницMink Dissection InstructionsMark PenticuffОценок пока нет
- History of Science and Technology in The PhilippinesДокумент12 страницHistory of Science and Technology in The PhilippinesQuerobin Gampayon100% (1)
- The Six-Step Formula for Hypnotic PersuasionДокумент24 страницыThe Six-Step Formula for Hypnotic Persuasionmajadb100% (12)
- Vit KДокумент22 страницыVit KKimbek BuangkeОценок пока нет
- 3 Azarpour Et Al. JNBR 4 (1) 2015 PDFДокумент9 страниц3 Azarpour Et Al. JNBR 4 (1) 2015 PDFKamailОценок пока нет
- Dressing and BandagingДокумент5 страницDressing and BandagingMaricar Gallamora Dela CruzОценок пока нет
- Ocurest Plus2018Документ4 страницыOcurest Plus2018rotastrainОценок пока нет
- NCP OrthoДокумент2 страницыNCP OrthoJeyser T. GamutiaОценок пока нет
- American Society For Biochemistry and Molecular BiologyДокумент23 страницыAmerican Society For Biochemistry and Molecular BiologyShishui UchihaОценок пока нет
- Thyroid Gland AnatomyДокумент11 страницThyroid Gland AnatomyRem AlfelorОценок пока нет
- The Incredible Journey: A Baby's Development from Conception to 1 YearДокумент40 страницThe Incredible Journey: A Baby's Development from Conception to 1 YearEli Abram CabilinОценок пока нет
- Acute Care TestingДокумент222 страницыAcute Care TestingAdel ChaabaneОценок пока нет
- 01 M039 43754Документ16 страниц01 M039 43754DrDeepak PawarОценок пока нет
- Acute Appendicitis in Adults: Clinical Manifestations and DiagnosisДокумент37 страницAcute Appendicitis in Adults: Clinical Manifestations and DiagnosisDaniela MuñozОценок пока нет
- DiaDENS-Cardio Operations ManualДокумент37 страницDiaDENS-Cardio Operations Manualgetdenas100% (4)
- List of Firms Having Who (Own)Документ1 страницаList of Firms Having Who (Own)Ksusha ChernobrovaОценок пока нет
- Pediatric PulmonologyДокумент250 страницPediatric Pulmonologyshankargoudachildicu100% (4)
- Abdominal Aortic AneurysmДокумент20 страницAbdominal Aortic AneurysmPortia Rose RodriguezОценок пока нет
- De Gruchys Clinical Haematology PDFДокумент1 страницаDe Gruchys Clinical Haematology PDFShivanshi K0% (1)
- Aims and Applications: Aims: The Three Aims of Pharmacoepidemiology AreДокумент10 страницAims and Applications: Aims: The Three Aims of Pharmacoepidemiology Aregowtham0% (1)