Академический Документы
Профессиональный Документы
Культура Документы
Gracia Et Al-2004-Pharmacotherapy - The Journal of Human Pharmacology and Drug Therapy
Загружено:
ManuelaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Gracia Et Al-2004-Pharmacotherapy - The Journal of Human Pharmacology and Drug Therapy
Загружено:
ManuelaАвторское право:
Доступные форматы
Cyanide Poisoning and Its Treatment
Rebeca Gracia, Pharm.D., and Greene Shepherd, Pharm.D.
Cyanide is both widely available and easily accessible throughout the world.
Although the compound is not frequently encountered, it has been used as a
poison and contaminant in the past and is a potential terrorist agent. Cyanide
has the ability to cause significant social disruption and demands special
attention to public health preparedness. It can be obtained from a variety of
sources, including industrial, medical, and even common household products.
Another frequently encountered source of cyanide exposure is residential
fires. Exposure to high concentrations of the chemical can result in death
within seconds to minutes. Long-term effects from cyanide exposure can
cause significant morbidity. The only treatment for cyanide toxicity approved
for use in the United States is a kit consisting of amyl nitrite, sodium nitrite,
and sodium thiosulfate. Future research aims to find a faster-acting, more
effective, and better tolerated treatment for cyanide toxicity.
Key Words: cyanide, antidote, poisoning.
(Pharmacotherapy 2004;24(10):13581365)
OUTLINE
Sources
Toxic Dose and Onset of Toxicity
Mechanism of Toxicity
Acute Clinical Manifestations
Treatment
Antidote Therapy
Investigational and NonU.S.-Approved Antidotes and
Prophylaxis
Conclusion
Cyanide was used as a poison for centuries
before the chemical was isolated and identified.1, 2
Many, and often successful, attempts have been
made throughout history to exploit it as a poison
and contaminant against individuals as well as
targeted populations. Recent events have heightened concern about the use of chemical weapons
by terrorists. In addition to being highly toxic,
cyanide exposure can cause significant social
disruption and public panic. This threat
demands special attention to public health
From the North Texas Poison Center, Dallas, Texas (Dr.
Gracia); and the College of Pharmacy, University of Georgia
and the Department of Emergency Medicine, Medical
College of Georgia, Augusta, Georgia (Dr. Shepherd).
Address reprint requests to Rebeca Gracia, Pharm.D.,
North Texas Poison Center, 5201 Harry Hines Boulevard,
Dallas, TX 75235; e-mail: rgracia@parknet.pmh.org.
preparedness (e.g., antidote stocking). The only
treatment for cyanide toxicity approved for use in
the United States is a kit consisting of amyl
nitrite, sodium nitrite, and sodium thiosulfate
(Cyanide Antidote Kit; Acorn Inc., Buffalo Grove,
IL). It was formerly known as the Pasadena or
Lilly Kit. It is important for health professionals
to be aware of potential sources of cyanide, its
effects and treatment, and investigational as well
as nonU.S.-approved antidotes.
Sources
Cyanide is both widely available and easily
accessible in a variety of forms. Historically,
cyanide was used as a warfare agent in the
volatile, water-soluble, liquid forms of hydrogen
cyanide and cyanogen chloride. The highly
reactive salt forms are exploited for numerous
industrial applications, including chemical
synthesis, electroplating, tanning, metallurgy,
printing, agriculture, photography, manufacture
of paper and plastics, and for use as fumigants
and insecticides. These salts produce hydrogen
cyanide gas when mixed with strong acid and
thus pose a significant risk in industrial accidents
as well as for intentional exposures. The
insoluble salt forms of cyanidemercury
cyanide, copper cyanide, gold cyanide, and silver
CYANIDE ANTIDOTES Gracia and Shepherd
cyanidealso can be found in industrial
settings.3 Waste products from mining processes
produce vast amounts of cyanide complexes.
These chemicals are significantly less toxic than
their salt counterparts; however, they pose a
considerable risk to the environment due to
accumulation.4, 5
An additional form of cyanide is the chemical
group referred to as nitriles; the most frequently
encountered nitriles are acetonitrile and propionitrile.612 These chemicals are commonly used
in industry as solvents and in households as
artificial nail and glue removers. They do not
produce significant toxicity as parent compounds,
but they are metabolized to cyanide in the liver.
This metabolic process involves the cytochrome
P450 2E1 isoenzyme, which converts the
cyanohydrin metabolite into the actively toxic
cyanide molecule.1315 People exposed to these
organic cyanides experience delayed onset of
signs and symptoms, as a latent period of several
hours passes during which the toxin is transformed and liberated.
Another frequently encountered source of
cyanide exposure is fire. Many synthetic polymers,
such as nylon and plastics, may release hydrogen
cyanide gas during combustion; hydrogen
cyanide is also generated in the combustion of
certain natural materials, including wool and
silk. Any material that contains carbon and
nitrogen may release cyanide during pyrolysis.16
Victims of smoke inhalation are at risk for both
cyanide toxicity and carbon monoxide effects.17
Although the extent of carbon monoxide exposure
does not necessarily correspond to a specific
cyanide concentration, the likelihood of concurrent
toxicity is significant, especially in house fires.
Both carbon monoxide and cyanide cause
hypoxic damage; their effects are additive and
possibly synergistic.18 Some studies even suggest
that toxicity from cyanide is more contributory to
death in some fire victims than carbon monoxide.19
Early implementation of empiric treatment and
management of probable cyanide exposure may
be warranted in smoke inhalation victims who
are hypoxic or unconscious.2024
Cyanide poisoning also can result from
iatrogenic sources. Each molecule of the potent
antihypertensive nitroprusside can release up to
five cyanide groups; toxicity may develop as
cyanide accumulates. Caution is especially
warranted when this agent is administered at
high doses over an extended period of time.25, 26
Laetrile was investigated as a chemotherapeutic
drug and continues to be used in some countries,
1359
but it is banned by the Food and Drug Administration for use in the United States. It is the
purified form of the natural cyanide compound,
amygdalin. Amygdalin is a cyanogenic glucoside,
a sugar compound with cyanide attached. When
laetrile is given intravenously, it is mostly excreted
unchanged in the urine, and cyanide toxicity is
not a significant concern. However, when these
products are ingested, the enzyme b-glucosidase
in the gastrointestinal tract metabolizes amygdalin
into hydrogen cyanide, resulting in toxicity.
Many published case reports describe deaths after
use of illegally acquired laetrile.2729
Amygdalin can be found in food, although it
rarely poses a risk of acute toxicity due to its very
low concentrations. The most well-known food
source of cyanide is the amygdalin in seeds and
fruit pits from the Prunus species (e.g., apple
seeds, chokecherries, bitter almonds, apricot
pits).30, 31 Of note, apricot pits and bitter almonds
have the highest concentrations of amygdalin.
Other relevant food sources include dietary
staples such as lima beans and cassava.32 Acute
cyanide toxicity can occur from exposure to the
wastewater from factories that process these
foods.33, 34
Toxic Dose and Onset of Toxicity
Cyanide is well known for its high degree of
lethality. It is estimated that the lethal dose in
adults is 50200 mg. This potency is a product
of cyanides rapid diffusion into tissues and
irreversible binding to target sites. It is the rapidity
of action rather than the minuteness of a dose
that makes cyanide lethal. In fact, the lethal dose
of cyanide is actually relatively high when compared
with other potential chemical weapons, such as
botulinum toxin, ricin, and sarin. The form of
cyanide significantly influences the toxic dose.35
Intravenous and inhalational exposures to cyanide
produce the most rapid onset of symptoms. Death
can occur within seconds to minutes. Apparent
toxicity from ingestion may be delayed for
several minutes until significant concentrations
have accumulated in the bloodstream. It may
take several hours before manifestations are seen
after a dermal exposure to intact skin. Significant
delay in clinical presentation of toxicity from
cyanogenic compounds that require metabolic
activation, such as the nitriles and amygdalin,
has been noted to occur.
Mechanism of Toxicity
The purported mechanisms of toxicity are
1360
PHARMACOTHERAPY Volume 24, Number 10, 2004
fairly well supported by the literature; however,
there are modes left to be discovered. Sulfane
and cyanocobalamin reactions, which occur
primarily within the liver, metabolize the low
concentrations of cyanide encountered normally.
The enzyme rhodanase catalyzes the conversion
of cyanide to thiocyanate. Reactions between 3mercaptopyruvate sulfurtransferase, thiosulfate
reductase (in the liver), and cystathionase also
may act to convert cyanide to thiocyanate. The
body can detoxify about 0.017 mg of cyanide/
kilogram/minute. These enzymatic routes are
highly effective, but they are insufficient for the
large quantities of cyanide encountered in
poisonings due to depletion of sulfur donors. In
the acute poisoning situation, endogenous
pathways of cyanide metabolism are rapidly
overwhelmed and conjugate substrates are
depleted, allowing for accumulation and
progression of toxic effects.36
Cyanide inhibits many metabolic processes,
but its most notable toxic effects seem to originate
from inhibition of the terminal enzyme in the
respiratory chain.36 The most commonly cited
mechanism is binding of cytochrome oxidase
within the mitochondria, resulting in abrupt
cessation of cellular respiration (Figure 1).
ATP
Cyanide has a high binding affinity for the ferric
ion on the cytochrome a3 portion of the enzyme.
This effectively stops electron transport and
inhibits oxidative phosphorylation. This
inhibition in essence terminates the synthesis
pathway of adenosine triphosphate. The
mitochondria continue to be exposed to an
adequate oxygen supply; however, there is
impaired oxygen extraction and use.37, 38 This
disruption of aerobic metabolism leads to
increased glycolysis by anaerobic pathways.
Acute Clinical Manifestations
Exposure to high concentrations of cyanide
can result in death within seconds to minutes. In
cases of more prolonged onset of toxicity, signs
and symptoms reflect a progressive intracellular
hypoxia. The hallmark presentation is hypoxia
and acidosis. Cyanosis may occur as a later
finding. Acute cyanide toxicity lacks characteristic
symptoms, and the diagnosis often is missed in
absence of a reasonable index of suspicion. The
constellation of initial transient symptoms often
mimics anxiety. The victim may complain of
dizziness, headache, weakness, flushing,
diaphoresis, dyspnea, hyperventilation, and
hyperpnea. 39 Cyanogen chloride gas and
(2)
Oxyhemoglobin
++
Cytochrome a3
NO2
(3)
Methemoglobin
(1)
Fe3+
Cytochrome a3+++
O2 + 2H2O
Cyanide
Cyanomethemoglobin
Cyanide + methemoglobin
(4)
Thiocyanate
(5)
Oxyhemoglobin
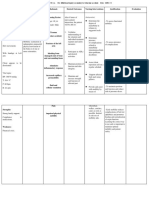
Figure 1. Binding of the cytochrome oxidase within the mitochondria, resulting in abrupt cessation of cellular respiration. (1)
Step 1 shows cyanide bindings to the ferric ion (Fe3+) in the cytochrome a3+ complex. (2) Step 2 illustrates that the electron
transport chain is inhibited, resulting in loss of aerobic metabolism and generation of adenosine triphosphate (ATP). (3) In
step 3, nitrites (NO2) react with oxyhemoglobin to form methemoglobin, which draws cyanide out of mitochrondria and forms
cyanomethemoglobin. (4) In step 4, the enzyme rhodanase combines thiosulfate with cyanomethemoglobin to form the less
toxic thiocyanate, which is excreted by the kidneys. (5) Finally, in step 5, methemoglobin is converted back to oxyhemoglobin
by the enzyme methemoglobin reductase.
CYANIDE ANTIDOTES Gracia and Shepherd
hydrogen cyanide may cause mucus membrane
irritation. The victim may have an odor of bitter
almonds, but only about 4060% of the
population possesses the gene necessary to detect
this odor, and it is not a reliable sign.40, 41
Although cyanide historically is associated
with a cherry red flush, the dramatic color
alteration is more often a postmortem finding.
However, a rapid indicator is visualization of
equally red retinal arteries and veins. Poor
oxygen extraction leads to abnormally increased
oxygen in the venous supply and a more notable
red color.42 As cellular hypoxia worsens, victims
experience loss of consciousness progressing to
coma, with fixed dilated pupils, hemodynamic
compromise, arrhythmias, seizures, apnea,
cardiac arrest, and finally death.
The most prominent laboratory finding in
cyanide toxicity is a metabolic acidosis with
dramatically elevated lactate concentrations. The
shift from aerobic to anaerobic metabolism
ultimately results in marked production of lactate
as a profound high anion gap acidosis ensues.
Several reports indicate that lactate concentrations
may be used as markers of severity of cyanide
toxicity.21, 43 Although these studies demonstrate
impressive correlations, numerous processes in a
critically ill patient contribute to elevations in
lactate and may confound the clinical picture.
In the case of an unknown exposure, it is
useful to check both venous and arterial blood
gases for supranormal venous oxygen content or
arteriolization of venous blood; these findings
strongly indicate cyanide toxicity. 44, 45 As
mitochondria cease to use the supplied oxygen, a
disproportionate oxygen concentration builds up
in the venous blood supply. Oxygen saturation
measurements by pulse oximetry will remain
high because the blood has good oxygen content;
rather, the problem in cyanide toxicity lies in
oxygen use and extraction. Of note, once therapy
has been started to induce methemoglobinemia,
pulse oximetry will depict a higher than actual
oxygen concentration, as both oxyhemoglobin
and methemoglobin deflect light at similar
wavelengths.46, 47
Cyanide tests are not readily available and
often require a few days for the results to be
available. The significant time lag in obtaining
results of cyanide concentrations in blood
precludes the use of these tests for indicating
treatment in acute exposures. Although many
sources report attempts to correlate expected
signs and symptoms at various cyanide concentrations, this approach may be misleading.
1361
Patient care should be based on clinical
presentation, regardless of what the cyanide
concentration may or may not be. Cyanide
concentrations only should be used to confirm
exposure; management of the victim should be
based on index of suspicion and clinical
presentation. Red blood cells have the highest
concentration of cyanide, and whole blood
specimens should be collected for analysis.38
Long-term effects from an acute exposure are
not frequently addressed, but cyanide exposure
can contribute to significant morbidity. Cyanide
induces cellular hypoxia, leading to oxidative
stress and lipid membrane peroxidation.48, 49 The
effects seem related to, and are synonymous with,
those effects seen from hypoxia, as with carbon
monoxide poisoning. Several neurologic diseases
are thought to be due to chronic cyanide toxicity.
Examples are tobacco amblyopia, retrobulbar
neuritis, Leber optic atrophy (a disorder of
defective cyanide metabolism), and Nigerian
nutritional ataxic neuropathy, otherwise known
as tropical ataxic neuropathy.38, 50, 51 Management
of an acute exposure is well defined; however,
little is known about prevention of long-term
effects from low-dose cyanide exposure.
Treatment
Cyanide is extremely quick to act, and there is
often limited time for treatment. All patients
should undergo decontamination appropriate to
the type of exposure. Remove clothing and
accessories for inhalational exposures. Proceed
to dermal decontamination with water for liquid
and solid exposures. If a patients external
decontamination may have been inadequate, it is
advisable to use double gloves, replacing them
often, and a mask.35, 52, 53 Several case reports
describe secondary contamination due to offgassing from victims. Cyanide may be exhaled
from the affected individuals lungs, or it can
emanate from heavily soaked clothing, skin, or
toxic vomitus.53
Cyanide salts are rapidly absorbed by the
gastrointestinal tract. Gastrointestinal decontamination measures may prove futile due to
cyanides high potency and rapid onset of
toxicity. However, some forms of cyanide may
have prolonged absorption kinetics. For patients
presenting within 1 hour of ingestion, it is
reasonable to consider performing an orogastric
lavage and administering activated charcoal in
attempt to recover any amount of the cyanide.
One gram of activated charcoal binds to only 35
1362
PHARMACOTHERAPY Volume 24, Number 10, 2004
mg of cyanide. 54 Despite this low level of
binding, administration of activated charcoal may
be helpful, as the lethal dose of cyanide is
relatively small.55
Supplemental oxygen is a crucial part of
supportive care in cyanide poisoning. Ventilation
with 100% oxygen increases tissue oxygen
delivery. However, it might seem useless to
employ enhanced oxygen as a therapy, given that
the mechanism of toxicity involves oxygen use
rather than availability.56 Theoretically, increased
oxygen may have a synergistic effect with
antidotes. Oxygen may serve to increase respiratory excretion of cyanide, restore cytochrome
oxidase activity by displacing cyanide, stimulate
activation of other oxidative systems (such as
those enzymes not yet poisoned by cyanide), and
perhaps facilitate the rhodanase enzyme
indirectly.5759
The use of hyperbaric oxygen for cyanide
toxicity remains controversial. Published
literature on the topic offers little corroboration,
as some investigations have found positive
effects, whereas others have failed to demonstrate
correlations between hyperbaric oxygen and
improved clinical status.6063 The Undersea and
Hyperbaric Medicine Society recommends
administering hyperbaric oxygen to patients with
carbon monoxideinduced hypoxia complicated
by cyanide poisoning.64
Additional supportive therapies that address
acidosis, hemodynamic compromise, and
seizures should be employed as needed
throughout the clinical course. Seizures resulting
from cyanide poisoning may be refractory and
require aggressive management. Hemodialysis
has been advocated in some cases of cyanide
toxicity; it would be particularly beneficial in the
face of worsening acidosis and failing renal
function, which would cause thiosulfate to
accumulate and induce its own additional
toxicity.65
Antidote Therapy
The cyanide antidote kit available in the
United States contains three constituents: amyl
nitrite, sodium nitrite, and sodium thiosulfate.
The combination of nitrites and thiosulfate has
been used in this country with relative success
since the 1930s.6668 The differential diagnosis
for acute cyanide poisoning is relatively small,
and the antidote should be administered
empirically. It is important to administer the
antidote even when a patients condition appears
fatal.38 Early studies with the nitrite thiosulfate
combination found that patients were responsive
to therapy up to 2.5 hours after cyanide
exposure.66
Nitrites are used to induce methemoglobinemia.
Amyl nitrite is administered by inhalation and
generates approximately 5% methemoglobin.
Sodium nitrite is given intravenously and
increases methemoglobin by about 820%.69 In
children, the dosage of sodium nitrite should be
adjusted based on hemoglobin levels.70
Cyanide appears to bind preferentially to the
ferric iron of methemoglobin, rather than to the
ferric iron of the cytochrome in mitochondria. It
is thought that an increased amount of cyanide
will transfer to the extracellular space and be
displaced from the cytochrome, enabling the
mitochondria to reactivate electron transport.66
It has been proposed that methemoglobin
formation may not be the sole mechanism of
action of nitrites. 71 Several studies have
demonstrated that many agents with vasoactive
properties, presumably via nitric oxide, also
afford protection against cyanide toxicity.72 They,
in fact, may alleviate toxicity through a
vasodilatory mechanism. Several other agents,
including promethazine and chlorpromazine,
also have beneficial effects by way of vasodilatory
actions.73
The nitrites do cause significant adverse
effects, namely vasodilatation and hypotension.
These effects can be problematic, especially if
compounded by coingestants or preexisting
medical conditions. Although methemoglobin is
the desired end point of therapy, it may
exacerbate the condition of certain patients,
including those with poor cardiopulmonary
reserve and those with concomitant carbon
monoxide poisoning. It is recommended to
avoid nitrites in smoke inhalation victims due to
the risk of worsening the oxygen-carrying
capacity deficit.74
The antidote for methemoglobinemia is
methylene blue. This agent will counteract
excess methemoglobin formation, but it may
subsequently release bound cyanide. It is of
interest that very high (oxidizing) doses of
methylene blue were identified as an early
antidote; this finding led to the development of
the current regimen.66
The third component of the cyanide antidote
kit is sodium thiosulfate. This agent enhances
clearance of cyanide by acting as a sulfhydryl
donor. Thiosulfate reversibly combines with
cyanide in the extracellular space to form the
1363
CYANIDE ANTIDOTES Gracia and Shepherd
Table 1. Investigational and Non.S.-Approved Cyanide Antidotes and Prophylaxis
Agent
Mechanism
Proposed Use
Advantages
Antidote,
Documented
Hydroxycobalamin7883
Chelates cyanide in
equimolar amounts
adjunct therapy
efficacy;
with thiosulfate
rare, minor
adverse reactions
Concerns
Large dose required,
short half-life,
light sensitive,
tachyphylaxis
4-Dimethylaminophenol8486
Induces
methemoglobinemia
Antidote,
adjunct therapy
Documented
efficacy,
i.m. injection
Necrosis at injection
site, excessive
methemoglobinemia
Stroma-free
methemoglobin
Binds to cyanide
Investigational
Uncompromised
oxygen-carrying
capacity
Investigational
Dicobalt edetate88
Chelates cyanide
to cobalticyanide
Antidote
Conflicting reports
on efficacy
Extreme toxicity
a-Ketoglutarate
and related
cyanohydrinforming drugs8991
Amino group scavenger
Prophylaxis,
adjunct therapy,
acute and chronic
exposures
Few adverse effects
Investigational
Dihydroxycetone92
Binds cyanide, enhances
adenosine triphosphate
Antidote,
adjunct therapy
Both i.v. and p.o.
administration
Short duration of
action, investigational
minimally toxic and renally excreted thiocyanate.
It also may augment mitochondrial sulfurtransferase reactions. The effectiveness of sodium
thiosulfate as an antidote is limited by its delay to
onset of action, short half-life, and small volume
of distribution. However, in smoke inhalation
with a suspected cyanide component, sodium
thiosulfate can be administered without nitrite
therapy.74
In contrast to its counterparts, the nitrites,
sodium thiosulfate has very few adverse effects.
The only significant adverse reaction is the rare
hypersensitivity reaction and infusion rate
dependent hypotension. However, chronic exposure to thiocyanates can cause toxicity because
thiocyanates and cyanide exist in equilibrium.
The effects seen from acute treatment of cyanide
exposure are virtually nonexistent, but they
should be kept in mind. It is important to note
that thiocyanate toxicity may be pronounced in
renal insufficiency, but it is dialyzable.66
Investigational and NonU.S.-Approved
Antidotes and Prophylaxis
Different antidotes are available in other
countries, and some novel antidotes are under
investigation (Table 1). 7593 Investigations of
potential antidotes have been complicated by the
fact that cyanide toxicity changes the
pharmacokinetics of the individual agent, making
it difficult to predict antidote efficacy and
toxicity. Other cyanide antidotes, particularly
hydroxycobalamin, warrant further investigation.
Of interest, many agents are being explored as
prophylactic cyanide antagonists. These agents
may prove beneficial in situations where cyanide
is used as a chemical weapon. The cyanide
antidotes currently available in the United States
are not suitable as prophylactic agents. Amyl
nitrite and sodium nitrite have unacceptable
adverse effects, and sodium thiosulfate, although
quite safe, acts too slowly to be of prophylactic
benefit.66
Because cyanide inhibits numerous enzyme
systems, many potential mechanisms of detoxification have yet to be exploited. Exogenous
administration of enzymes or substrates normally
involved in cyanide metabolism and detoxification may prove beneficial.92 A few investigations report treatments such as carrier erythrocytes containing rhodanase and thiosulfate to
reverse cyanide toxicity.93, 94
Conclusion
Cyanide is widely available throughout the
world and may be harmful to humans in the
settings of poisoning, suicide attempts,
occupational hazards, fires, or as a chemical
weapon. Medical facilities are urged to maintain
an adequate antidote store to respond rapidly to
cyanide exposures. The mainstay of treatment in
the United States is decontamination, oxygen,
and a combination of nitrites and thiosulfate.
Future research efforts should be directed toward
finding faster acting, more effective, and better
tolerated treatments for cyanide toxicity.
1364
PHARMACOTHERAPY Volume 24, Number 10, 2004
References
1. Gettler AO, St George AV. Cyanide poisoning. Am J Clin
Pathol 1934;4(5):42937.
2. Kunkel D. The toxic emergencycyanide: looking for the
source. Emerg Med 1987;May 15:11525.
3. Blanc P, Hogan M, Mallin K, Hryhorczuk D, Hessl S, Bernard
B. Cyanide intoxication among silver-reclaiming workers.
JAMA 1985;253(3):36771.
4. Kovac C. Cyanide spill threatens health in Hungary. BMJ
2000;320(7234):536.
5. Kovac C. Cyanide spill could have long term impact. BMJ
2000;320(7245):1294.
6. Willhite CC. Inhalation toxicology of acute exposure to
aliphatic nitriles. Clin Toxicol 1981;18(8):9911003.
7. Vogel RA, Kirkendall WM. Acrylonitrile (vinyl cyanide)
poisoning: a case report. Tex Med 1984;80(5):4851.
8. Caravati EM, Litovitz TL. Pediatric cyanide intoxication and
death from an acetonitrile-containing cosmetic. JAMA
1988;260(23):34703.
9. Kurt TL, Day LC, Reed WG, Gandy W. Cyanide poisoning
from glue-on nail remover. Am J Emerg Med 1991;9(3):2712.
10. Geller RJ, Ekins BR, Iknoian RC. Cyanide toxicity from
acetonitrile-containing false nail remover. Am J Emerg Med
1991;9(3):26870.
11. Losek JD, Rock AL, Boldt RR. Cyanide poisoning from a
cosmetic nail remover. Pediatrics 1991;88(2):33740.
12. Bismuth C, Baud FJ, Djeghout H, Astier A, Aubriot D.
Cyanide poisoning from propionitrile exposure. J Emerg Med
1987;5(3):1915.
13. Wang H, Chanas B, Ghanayem BI. Cytochrome P450 2E1
(CYP2E1) is essential for acrylonitrile metabolism to cyanide:
comparative studies using CYP2E1-null and wild-type mice.
Drug Metab Dispos 2002;30(8):91117.
14. Freeman JJ, Hayes EP. Microsomal metabolism of acetonitrile
to cyanide: effects of acetone and other compounds. Biochem
Pharmacol 1988;37(6):11539.
15. Feierman DE, Cederbaum AI. Role of cytochrome P-450 IIE1
and catalase in the oxidation of acetonitrile to cyanide. Chem
Res Toxicol 1989;2(6):35966.
16. Alarie Y. The toxicity of smoke from polymeric materials
during thermal decomposition. Ann Rev Pharmacol Toxicol
1985;25:32547.
17. Silverman SH, Purdue GF, Hunt JL, Bost RO. Cyanide toxicity
in burned patients. J Trauma 1988;28(2):1716.
18. Pitt BR, Radford EP, Gurtner GH, Traystman RJ. Interaction of
carbon monoxide and cyanide on cerebral circulation and
metabolism. Arch Environ Health 1979;34(5):3459.
19. Lundquist P, Rammer L, Sorbo B. The role of hydrogen
cyanide and carbon monoxide in fire casualties: a prospective
study. Forensic Sci Int 1989;43(1):914.
20. Hall AH, Rumack BH, Karkal SS. Increasing survival in acute
cyanide poisoning. Emerg Med Rep 1988;9(17):12936.
21. Baud FJ, Barriot P, Toffis V, et al. Elevated blood cyanide
concentrations in victims of smoke inhalation. N Engl J Med
1991;325(25):17616.
22. Koschel MJ. Where theres smoke, there may be cyanide. Am J
Nurs 2002;102(8):3942.
23. Clark CJ, Campbell D, Reid WH. Blood carboxyhaemoglobin
and cyanide levels in fire survivors. Lancet 1981;1(8234):
13325.
24. Becker CE. The role of cyanide in fires. Vet Hum Toxicol
1985;27(6):48790.
25. Curry SC, Arnold-Capell P. Toxic effects of drugs used in the
ICU. Nitroprusside, nitroglycerin, and angiotensin-converting
enzyme inhibitors. Crit Care Clin 1991;7(3):55581.
26. Rindone JP, Sloane EP. Cyanide toxicity from sodium
nitroprusside: risks and management. Ann Pharmacother
1992;26(4):51519.
27. Rauws AG, Olling M, Timmerman A. The pharmacokinetics of
amygdalin. Arch Toxicol 1982;49(34):31119.
28. Beamer WC, Shealy RM, Prough DS. Acute cyanide poisoning
from laetrile ingestion. Ann Emerg Med 1983;12(7):44951.
29. Braico KT, Humbert JR, Terplan KL, Lehotay JM. Laetrile
intoxication: report of a fatal case. N Engl J Med 1979;300(5):
23840.
30. Rubino MJ, Davidoff F. Cyanide poisoning from apricot seeds
[letter]. JAMA 1979;241(4):359.
31. Morse DL, Harrington JM, Heath CW Jr. Laetrile, apricot pits,
and cyanide poisoning [letter]. N Engl J Med 1976;295(22):
1264.
32. Akintonwa A, Tunwashe OL. Fatal cyanide poisoning from
cassava-based meal. Hum Exp Toxicol 1992;11(1):479.
33. Okafor PN, Okorowkwo CO, Maduagwu EN. Occupational
and dietary exposures of humans to cyanide poisoning from
large-scale cassava processing and ingestion of cassava foods.
Food Chem Toxicol 2002;40(7):10015.
34. Oliveira MA, Reis EM, Nozaki J. Biological treatment of
wastewater from the cassava meal industry. Environ Res
2001;85(2):17783.
35. Bogucki S, Weir S. Pulmonary manifestations of intentionally
released chemical and biological agents. Clin Chest Med
2002;23(4):77794.
36. Way JL, Leung P, Cannon E, et al. The mechanism of cyanide
intoxication and its antagonism. Ciba Found Symp 1988;
140:23243.
37. Keilin D. Cytochrome and respiratory enzymes. Proc R Soc
Lond B Biol Sci 1929;104:20652.
38. Vogel SN, Sultan TR, Ten Eyck RP. Cyanide poisoning. Clin
Toxicol 1981;18(3):36783.
39. Mokhlesi B, Leikin JB, Murray P, Corbridge TC. Adult
toxicology in critical care: part II: specific poisonings. Chest
2003;123(3):897922.
40. Bonnichsen R, Maehly AC. Poisoning by volatile compounds.
J. Forensic Sci 1966;11(4):51647.
41. Hall AH, Rumack BH. Clinical toxicology of cyanide. Ann
Emerg Med 1986;15:106774.
42. Peters CG, Mundy JV, Rayner PR. Acute cyanide poisoning:
the treatment of a suicide attempt. Anaesthesia 1982;37(5):
5826.
43. Baud FJ, Borron SW, Megarbane B, et al. Value of lactic
acidosis in the assessment of the severity of acute cyanide
poisoning. Crit Care Med 2002;30(9):204450.
44. Johnson RP, Mellors JW. Arteriolization of venous blood gases:
a clue to the diagnosis of cyanide poisoning. J Emerg Med
1988;6(5):4014.
45. Yeh MM, Becker CE, Arieff AI. Is measurement of venous
oxygen saturation useful in the diagnosis of cyanide poisoning?
Am J Med 1992;93(5):5823.
46. Barker SJ, Tremper KK. The effect of carbon monoxide
inhalation on pulse oximetry and transcutaneous PO 2 .
Anesthesiology 1987;66(5):6779.
47. Gonzalez A, Gomez-Arnau J, Pensado A. Carboxyhemoglobin
and pulse oximetry [letter]. Anesthesiology 1990;73(3):573.
48. Johnson JD, Conroy WG, Burris KD, Isom GE. Peroxidation
of brain lipids following cyanide intoxication in mice.
Toxicology 1987;46(1):218.
49. Ardelt BK, Borowitz JL, Maduh EU, Swain SL, Isom GE.
Cyanide-induced lipid peroxidation in different organs:
subcellular distribution and hydroperoxide generation in
neuronal cells. Toxicology 1994;89(2):12737.
50. Freeman AG. Optic neuropathy and chronic cyanide
intoxication: a review. J R Soc Med 1988;81(2):1036.
51. Bismuth C, Baud FJ, Pontal PG. Hydroxycobalamin in chronic
cyanide poisoning. J Toxicol Clin Exp 1988;8(1):358.
52. Brueske PJ. ED management of cyanide poisoning. J Emerg
Nurs 1997;23(6):56973.
53. Shenoi R. Disaster medicine: chemical warfare agents. Clin Ped
Emerg Med 2002;3(4):23947.
54. Andersen A. Experimental studies on the pharmacology of
activated charcoal. I. Adsorption power of charcoal in aqueous
solutions. Acta Pharmacol 1946;2:6978.
55. Lambert RJ, Kindler BL, Schaeffer DJ. The efficacy of
superactivated charcoal in treating rats exposed to a lethal oral
dose of potassium cyanide. Ann Emerg Med 1988;17(6):
5958.
CYANIDE ANTIDOTES Gracia and Shepherd
56. Way JL. Cyanide antagonism. Fundam Appl Toxicol
1983;3(5):3836.
57. Way JL, Gibbon SL, Sheehy M. Cyanide intoxication:
protection with oxygen. Science 1966;152(3719):21011.
58. Sheehy M, Way JL. Effect of oxygen on cyanide intoxication. 3.
Mithridate. J Pharmacol Exp Ther 1968;161(1):1638.
59. Isom GE, Way JL. Effect of oxygen on cyanide intoxication. VI.
Reactivation of cyanide-inhibited glucose metabolism. J
Pharmacol Exp Ther 1974;189(1):23543.
60. Litovitz TL, Larkin RF, Myers RA. Cyanide poisoning treated
with hyperbaric oxygen. Am J Emerg Med 1983;1(1):94101.
61. Goodhart GL. Patient treated with antidote kit and hyperbaric
oxygen survives cyanide poisoning. South Med J 1994;87(8):
81416.
62. Scolnick B, Hamel D, Woolf AD. Successful treatment of lifethreatening propionitrile exposure with sodium nitrite/sodium
thiosulfate followed by hyperbaric oxygen. J Occup Med
1993;35(6):57780.
63. Trapp WG. Massive cyanide poisoning with recovery: a boxingday story. Can Med Assoc J 1970;102(5):517.
64. Weiss LD, Van Meter KW. The applications of hyperbaric
oxygen therapy in emergency medicine. Am J Emerg Med
1992;10(6):55868.
65. Wesson DE, Foley R, Sabatini S, Wharton J, Kapusnik J,
Kurtzman NA. Treatment of acute cyanide intoxication with
hemodialysis. Am J Nephrol 1985;5(2):1216.
66. Baskin SI, Horowitz AM, Nealley EW. The antidotal action of
sodium nitrite and sodium thiosulfate against cyanide
poisoning. J Clin Pharmacol 1992;32(4):36875.
67. Yen D, Tsai J, Wang LM, et al. The clinical experience of acute
cyanide poisoning. Am J Emerg Med 1995;13(5):5248.
68. Chen KK, Rose CL. Nitrite and thiosulfate therapy in cyanide
poisoning. JAMA 1952;149(2):11315.
69. Tanen DA, LoVecchio F, Curry SC. Failure of intravenous Nacetylcysteine to reduce methemoglobin produced by sodium
nitrite in human volunteers: a randomized controlled trial. Ann
Emerg Med 2000;35(4):36973.
70. Berlin CM Jr. The treatment of cyanide poisoning in children.
Pediatrics 1970;46(5):7936.
71. Way JL, Sylvester D, Morgan RL, Isom GE, Burrows GE,
Tamulinas CB. Recent perspectives on the toxicodynamic basis
of cyanide antagonism. Fundam Appl Toxicol 1984;4(2 pt
2):S2319.
72. Baskin SI, Nealley EW, Lempka JC. Cyanide toxicity in mice
pretreated with diethylamine nitric oxide complex. Hum Exp
Toxicol 1996;15(1):1318.
73. Way JL, Burrows G. Cyanide intoxication: protection with
chlorpromazine. Toxicol Appl Pharmacol 1976;36(1):937.
74. Moore SJ, Norris JC, Walsh DA, Hume AS. Antidotal use of
methemoglobin forming cyanide antagonists in concurrent
carbon monoxide/cyanide intoxication. J Pharmacol Exp Ther
1987;242(1):703.
75. Sauer SW, Keim ME. Hydroxycobalamin: improved public
health readiness for cyanide disasters. Ann Emerg Med
2001;37(6):63541.
76. Brouard A, Blaisot B, Bismuth C. Hydroxycobalamine in
1365
cyanide poisoning. J Toxicol Clin Exp 1987;7(3):15568.
77. Hall AH, Rumack BH. Hydroxycobalamin/sodium thiosulfate
as a cyanide antidote. J Emerg Med 1987;5(2):11521.
78. Houeto P, Hoffman JR, Imbert M, Levillain P, Baud FJ.
Relation of blood cyanide to plasma cyanocobalamin concentration after a fixed dose of Hydroxycobalamin in cyanide
poisoning. Lancet 1995;346(8975):6058.
79. Zerbe NF, Wagner BK. Use of vitamin B12 in the treatment and
prevention of nitroprusside-induced cyanide toxicity. Crit Care
Med 1993;21(3):4657.
80. Forsyth JC, Mueller PD, Becker CE, et al. Hydroxycobalamin
as a cyanide antidote: safety, efficacy and pharmacokinetics in
heavily smoking normal volunteers. J Toxicol Clin Toxicol
1993;31(2):27794.
81. Cottrell JE, Casthely P, Brodie JD, Patel K, Klein A, Turndorf
H. Prevention of nitroprusside-induced cyanide toxicity with
Hydroxycobalamin. N Engl J Med 1978;298(15):80911.
82. Mushett C, Kelley KL, Boxer GE, et al. Antidotal efficacy of
vitamin B 12 (Hydroxycobalamin) in experimental cyanide
poisoning. Proc Soc Exp Biol 1952;81:2347.
83. Weger NP. Treatment of cyanide poisoning with 4dimethylaminophenol (DMAP): experimental and clinical
overview. Middle East J Anesthesiol 1990;10(4):389412.
84. Bhattacharya R, Jeevaratnam K, Raza SK, Das Gupta S.
Protection against cyanide poisoning by the co-administration
of sodium nitrite and hydroxylamine in rats. Hum Exp Toxicol
1993;12(1):336.
85. Bhattacharya R. Antidotes to cyanide poisoning: present status.
Indian J Pharmacol 2000;32:94101.
86. Breen PH, Isserles SA, Tabac E, Roizen MF, Taitelman UZ.
Protective effect of stroma-free methemoglobin during cyanide
poisoning in dogs. Anesthesiology 1996;85(3):55864.
87. Nagler J, Provoost RA, Parizel G. Hydrogen cyanide poisoning:
treatment with cobalt EDTA. J Occup Med 1978;20(6):41416.
88. Hume AS, Mozingo JR, McIntyre B, Ho IK. Antidotal efficacy
of a-ketoglutaric acid and sodium thiosulfate in cyanide
poisoning. J Toxicol Clin Toxicol 1995;33(6):7214.
89. Bhattacharya R, Vijayaraghavan R. Promising role of aketoglutarate in protecting against the lethal effects of cyanide.
Hum Exp Toxicol 2002;21(6):297303.
90. Dulaney MD Jr, Brumley M, Willis JT, Hume AS. Protection
against cyanide toxicity by oral a-ketoglutaric acid. Vet Hum
Toxicol 1991;33(6):5715.
91. Niknahad H, Ghelichkhani E. Antagonism of cyanide
poisoning by dihydroxyacetone. Toxicol Lett 2002;132(2):
95100.
92. Schwartz C, Morgan RL, Way LM, Way JL. Antagonism of
cyanide intoxication with sodium pyruvate. Toxicol Appl
Pharmacol 1979;50(3):43741.
93. Cannon EP, Leung P, Hawkins A, Petrikovics I, DeLoach J,
Way JL. Antagonism of cyanide intoxication with murine
carrier erythrocytes containing bovine rhodanese and sodium
thiosulfate. J Toxicol Environ Health 1994;41(3):26774.
94. Petrikovics I, Pei L, McGuinn WD, Cannon EP, Way JL.
Encapsulation of rhodanese and organic thiosulfonates by
mouse erythrocytes. Fundam Appl Toxicol 1994;23(1):705.
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Sing With Distortion - 10 TipsДокумент10 страницSing With Distortion - 10 TipstjoodleОценок пока нет
- EHS ManualДокумент426 страницEHS ManualUnme Vr100% (2)
- Informed Consent Form and Interview ProtocolДокумент4 страницыInformed Consent Form and Interview ProtocolAdonis BesaОценок пока нет
- The Sacred Mushroom "Reishi"-A ReviewДокумент4 страницыThe Sacred Mushroom "Reishi"-A ReviewDinesh Babu PugalenthiОценок пока нет
- The Hypothesis and Assumptions of The StudyДокумент12 страницThe Hypothesis and Assumptions of The StudyMaria Arlene67% (3)
- Reading Sub-Test: Answer Key - Part AДокумент23 страницыReading Sub-Test: Answer Key - Part AAlwin BrightОценок пока нет
- Ectropion & EntropionДокумент2 страницыEctropion & EntropionAhmed ShafikОценок пока нет
- Catatan Koas THT 1Документ5 страницCatatan Koas THT 1MEDS easyОценок пока нет
- Neuro Oncol 2016 Patil 1487 97Документ11 страницNeuro Oncol 2016 Patil 1487 97ManuelaОценок пока нет
- Cyanides and their toxicity: A literature reviewДокумент12 страницCyanides and their toxicity: A literature reviewManuela100% (1)
- Modeling CyanideДокумент362 страницыModeling CyanideManuelaОценок пока нет
- C 0845132105Документ8 страницC 0845132105ManuelaОценок пока нет
- Cyanide Poisoning PDFДокумент14 страницCyanide Poisoning PDFGilbert OfeiОценок пока нет
- Reviews: Are Technetium-99m-Labeled Myocardial Pehsion Agents Adequate For Detection of Myocardial Viability?Документ8 страницReviews: Are Technetium-99m-Labeled Myocardial Pehsion Agents Adequate For Detection of Myocardial Viability?ManuelaОценок пока нет
- 1 s2.0 S0010482514001024 MainДокумент10 страниц1 s2.0 S0010482514001024 MainManuelaОценок пока нет
- CianuriДокумент7 страницCianuriManuelaОценок пока нет
- CianuriДокумент24 страницыCianuriManuelaОценок пока нет
- CianuriДокумент5 страницCianuriManuelaОценок пока нет
- Minimizing Social Desirability Bias in Measuring Sensitive Topics: The Use of Forgiving Language in Item DevelopmentДокумент14 страницMinimizing Social Desirability Bias in Measuring Sensitive Topics: The Use of Forgiving Language in Item DevelopmentKillariyPortugalОценок пока нет
- Chapter1 Intro of Biomedical Signal ProcessingДокумент50 страницChapter1 Intro of Biomedical Signal ProcessingShafayet Uddin100% (3)
- PCRL 627: Clinical Microbiology and Immunology 2016: Email: Shilling@uic - EduДокумент45 страницPCRL 627: Clinical Microbiology and Immunology 2016: Email: Shilling@uic - Edui24youОценок пока нет
- Post MBBS - Second Round Allotment Details PDFДокумент89 страницPost MBBS - Second Round Allotment Details PDFRamaniОценок пока нет
- Mudravig PDFДокумент24 страницыMudravig PDFJai KanthОценок пока нет
- Medical Charges Reimbursement Form: Item Names Charges Details of Cash-Memos EtcДокумент2 страницыMedical Charges Reimbursement Form: Item Names Charges Details of Cash-Memos EtcAmit KumarОценок пока нет
- Chemicals Zetag MSDS Powder Zetag 4139 - 1010Документ6 страницChemicals Zetag MSDS Powder Zetag 4139 - 1010PromagEnviro.comОценок пока нет
- Tza STG Neml 2007 PDFДокумент220 страницTza STG Neml 2007 PDFJohnny EmperorОценок пока нет
- 2001 PP No 22Документ10 страниц2001 PP No 22tarОценок пока нет
- IPE Zoology Model Paper 1 Question PaperДокумент2 страницыIPE Zoology Model Paper 1 Question PaperFgkew DjgsОценок пока нет
- Akf Stok 13Документ67 страницAkf Stok 13Grace Riani Pongsipulung TariganОценок пока нет
- Cutera Laser Genesis Patient BrochureДокумент6 страницCutera Laser Genesis Patient BrochureRogier van der HeideОценок пока нет
- Q4 Health 6 Week3Документ4 страницыQ4 Health 6 Week3Ethelyn Joy FarquerabaoОценок пока нет
- Medical 1 PDFДокумент5 страницMedical 1 PDFsuresh balajiОценок пока нет
- 13497-Texto Del Artículo-48998-1-10-20150925Документ7 страниц13497-Texto Del Artículo-48998-1-10-20150925Pipe Contecha BernatteОценок пока нет
- Synthesis of Novel Amino Acid Derivative of 7-AVCAДокумент4 страницыSynthesis of Novel Amino Acid Derivative of 7-AVCAIOSRjournal0% (1)
- NCP OrthoДокумент2 страницыNCP OrthoJeyser T. GamutiaОценок пока нет
- Disturbing Art Exposes Modern Culture AbsurditiesДокумент15 страницDisturbing Art Exposes Modern Culture Absurdities2aethicusОценок пока нет
- Doctors Roadmap To The UkДокумент10 страницDoctors Roadmap To The Uksryh2012Оценок пока нет
- CPR and Aed: Quiz #2 ResultsДокумент2 страницыCPR and Aed: Quiz #2 ResultsNathan WhiteОценок пока нет
- Malabon Hospital Admission GuideДокумент2 страницыMalabon Hospital Admission GuideJose BernelОценок пока нет
- 3 Azarpour Et Al. JNBR 4 (1) 2015 PDFДокумент9 страниц3 Azarpour Et Al. JNBR 4 (1) 2015 PDFKamailОценок пока нет