Академический Документы
Профессиональный Документы
Культура Документы
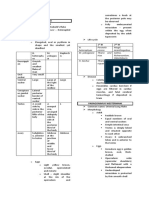
Genus Staphylococcus: Characteristic S.epidermidis S.saprophyticus
Загружено:
xxdrivexxОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Genus Staphylococcus: Characteristic S.epidermidis S.saprophyticus
Загружено:
xxdrivexxАвторское право:
Доступные форматы
GENUS STAPHYLOCOCCUS
The name staphyle (in Greek means bunch of grapes) is due to their appearance as
clusters as a result of division in many planes during replication.
Representants
It comprise more than 30 species, but 3 are medically important:
S.aureus responsible for most staphilococcal infections in humans
S.epidermidis causes opportunistic infections in immunosuppressed patients.
S.saprophyticus is opportunistic, cause urinary tract infections in women.
Differentiating characteristics of staphylococci
Characteristic
Color of colonies
S.aureus
S.epidermidis
yellow or white
white
S.saprophyticus
white or pale gray
Hemolysis
+/-
Coagulase production
Mannitol fermentation
Novobiocin sensitivity Sensitive
Sensitive
Cell wall teichoic acid
glycerol
ribitol
Resistant
S.aureus peptidoglycan is unique because of the pentaglycine bridges linking the
tetrapeptides.
S. aureus
Epidemiology
S.aureus colonizes the skin and mucous membranes of approximately 30% of normal
humans. (80-90% in healthcare personal). The anterior nares is the most commonly
populated site
-are implied in a lot of human infections
-human-to-human transmission is most common but nosocomial infection can also
occur (in hospitals to immunosupressed hosts and newborns)
-catalase positive
-prefer aerobic conditions but may behave as facultative anaerobes
-grow in presence of 7.5% sodium chloride (halotolerants)
Pathogenesis
Factors determining the occurrence of disease depend on:
-host: hormonal changes, devitalised tissues (wounds, burned areas, diabetus
mellitus), immunosupression due to iradiation, viral diseases, corticosteroids,
citostatic drugs, prolonged antibiotherapy.
-bacteria (S.aureus): number, determinants of pathogenicity
Determinants of pathogenicity
I.Surface (implied in the atachement of the staphylococcus to the host tissues)
-teichoic acids, peptidoglycan, capsula (present in young staphylococci), protein A
(covalently bound to the peptidoglycan layer of more than 90% of S.aureus isolates; it
binds to the Fc portion of Ig G, preventing specific antibodies from binding to the
bacteria and hindering Fc-mediated opsonization => complement is activated by the
protein A-bound immunoglobulins, which can contribute to a vigurous inflammatory
reaction.
II. Enzymes (determining both the invasive capacity and lesions)
*Coagulase = the most important marker of pathogenicity
-it helps the transformation of fibrinogen in fibrin
-2 tipes: free causes clotting of plasma
Linked forms a fibrine blanket over the group of staphilococci preventing
fagocytosis
*Fibrinolysin (staphylokinase)
*Hyaluronidase
*DNA-se
*Phospholipase: favour the instalation of staphylococcus in sebaceum regions where
they degrade lipids in fat acids, which can be used as carbon and energy sources. For
this reason they are also called FAME= fatty acids modifying enzymes)
*-lactamase (penicillinase)- they are easily transmitted from one strain to another
spreading the resistance to penicilins and other -lactamines.
III.Exotoxins
a.Pyrogenic exotoxins
-act as superantigens (the interaction with LT is not specific so that large numbers of
LT are implied, secreting a large amount of lymphokines).
1.Enterotoxins (A, B, C (1,2,3), D, E, F)
-heat stable proteins resistant to digestive enzymes
-responsible for the majority of food poisoning cases (in US and all over the world)
2.TSST-1 (toxic shock syndrome toxin-1)
-causes fever, multiple organ dysfunction and shock
-it is nearly identical with enterotoxin F
b. Citolytic exotoxins
1.Leukocidin kills PMN and macrophages
-immunogenic, because antibodies against this factor protect the host against
reinfection.
2.Hemolysins (,,, ) lyse erythrocytes
c.Exfoliatins
-cleave the stratum corneum, causing separation and loss of the most superficial
layers of the epidermis
-they are immunogenic => antibodies have been detected in recovering patients.
Clinical disease is primarily associated with S.aureus
I. Superficial infections occur most frequently and are characterized by intense
suppuration, local tissue necrosis and the formation of a pus filled local abscess.
1.Pyoderma (impetigo):
-etiology: S.aureus, S.epidermidis or Streptococcus
-highly communicable superficial skin infection: vesicles filled with clear to
yellowish fluid, most often on the extremities following infections of previous
mosquito bites or skin trauma.
2.Folliculitis, furuncles (boils) and sties result from infection of the hair follicles
3.Abscesses and carbuncles
II. Deep infections
1.Osteomyelitis
2.Pneumonia
3.Acute endocarditis
4.Arthritis, bacteremia, septicemia and deep organ (brain, kidney, lung) abscesses
III. Staphylococcal toxin diseases
1.Scalded skin syndrome
-manifestation of an exfoliatin producing strain of S.aureus
-involves infants and children younger than 5 years of age.
a)Bullous impetigo: few large localized blisters
b)Staphylococcal scarlet fever: erythematous rash but do not involves tongue
and palate
2.Staphylococcal food poisoning
-explosive vomiting and diarrhea and NO fever !!!
-occurs 1-5 hours after ingestion of contaminated food (e.g. meat, cream-filled
pastries, mayonnaise-containing salads)
-self-limiting, with proper hydration complete recovery occurs within 24-48 hours.
3.TSS
-febrile illness that may progress to organ failure and death.
Laboratory diagnosis
A. Direct diagnosis
1.Sample collection: pus, blood, nasal and pharyngeal exudates, urine, etc.
2.Microscopic examination: Gram smear : clusters of gram positive cocci on a
background formed by fibrin, necrotic descoamated cells.
3.Inoculation on media
-grow well under condition that are usually inhibitory to other bacteria (e.g. 7.5%
sodiumchloride or 40% bile)
-blood agar preferred for isolation from samples with little or no other microbial
contamination
-selective media with 7-10% sodium shloride, polymyxin, or bile.
-manitol salt agar (Chapman media) is selective and differential for staph.because
S.aureus ferments manitol => yellow colonies, whereas S.epidermidis does not =>
unmodified colonies.
Staphylococcus grow best at 37 C but become pigmented best at 20-25 C
4.Identification based on:
-morphology and staining: G (+) cocci arranged in clusters, non-motile, nonsporulated, the young stapylococci are capsulated
-cultural properties: in liquid media produce an uniform opalescence and on solid
media grow as big (2-3 mm), smooth, shiny colonies (S) with different pigmentation
depending on the species: white (S.epidermidis), white or yellow (S.aureus) and white
or gray (S.saprophyticus).
S.aureus produce hemolysis (incomplete = ), which can transform into complete
hemolysis () at 4 C.
-biochemical properties: catalase +, coagulase + (S.aureus), manitol fermentation and
oxidation + (S.aureus)
-pathogenic properties (production of toxic and non/toxic determinants of
pathogenicity)
a)in vitro
Coagulase test: a suspension of S.aureus is mixed with a drop of plasma, fibrin
clots form almost immediately.
Fibrinolysin test: in a media with fibrin they determine a clear area where the
colony grow
b)in vivo
Hemolysin is dermonecrotic: injected in rabbit (48-72 h) => lesion
Exfoliatin will cause exfoliation at the inoculation place in suckling mice.
Enterotoxin Dolman test: filtrate of a bacterial culture boiled for 20 min. is
injected intraperitoneal in kitten; after 10 to 60 minutes the kitten become agitated
has sialorhea, abdominal contractions, diarrhea. After 1 hour everything becomes
to normal.
5. Sensitivity to antibiotics and treatment
-must be performed because the resistance is very frequent and easily acquired from
one strain to another
-if treatment has to be done before isolation Oxacillin, Nafcillin and Meticillin are the
drugs of choice. For meticillin resistant strains vancomicin is preffered.
Cephalosporins, erythromycin or clindamycin may be used for patients allergic to
penicillin.
Control and prevention
Suppressing the carrier state population and implementing diligent aseptic practices
are the most effective measures of infection control. No vaccine is available.
Вам также может понравиться
- Staphylococcus LectureДокумент66 страницStaphylococcus LectureFarhan Azmain FahimОценок пока нет
- 18 Staphylococci, Streptococci, Meningococci, GonococciДокумент72 страницы18 Staphylococci, Streptococci, Meningococci, GonococciManisanthosh KumarОценок пока нет
- Immuno Virology BacteriologyДокумент309 страницImmuno Virology BacteriologyJulianna MacintyreОценок пока нет
- Mycology 1 PrelimДокумент4 страницыMycology 1 PrelimKaye Angel VillonОценок пока нет
- Virology - S1: Abbas Adel Group 4Документ38 страницVirology - S1: Abbas Adel Group 4William BufОценок пока нет
- Chapt01 Notes Q PDFДокумент13 страницChapt01 Notes Q PDFamor magtibayОценок пока нет
- Review 1 BacteДокумент9 страницReview 1 BacteJibz MiluhonОценок пока нет
- Isolation and Identification of Enteric OrganismsДокумент7 страницIsolation and Identification of Enteric OrganismsCzarina Charmaine DiwaОценок пока нет
- RMTnotes PARASITOLOGYДокумент68 страницRMTnotes PARASITOLOGYArvin O-CaféОценок пока нет
- Opportunistic MycosesДокумент3 страницыOpportunistic MycosesMaryОценок пока нет
- Lab Practical UrinalysisДокумент7 страницLab Practical UrinalysisHeatherIz AwwsomeОценок пока нет
- Medical MycologyДокумент1 страницаMedical MycologyHairul AnuarОценок пока нет
- Heterophyid: ST NDДокумент3 страницыHeterophyid: ST NDIvan ChuaОценок пока нет
- Urine CrystallДокумент4 страницыUrine Crystallpartho1432513Оценок пока нет
- Types of Mycoses According To SiteДокумент8 страницTypes of Mycoses According To SiteAlyanna ManguerraОценок пока нет
- ParasitologyДокумент7 страницParasitologySherine Mohamed OmarОценок пока нет
- Routine UrinalysisДокумент74 страницыRoutine UrinalysisGARON KlarizzaОценок пока нет
- VirologyДокумент131 страницаVirologyvaidyamОценок пока нет
- Medical Parasitology: Medina & Albano - Lecture & LaboratoryДокумент9 страницMedical Parasitology: Medina & Albano - Lecture & LaboratoryabigailОценок пока нет
- Urine Case 2010-2Документ9 страницUrine Case 2010-2hendra_darmawan_4Оценок пока нет
- Medical MycologyДокумент14 страницMedical Mycologyhawkar omerОценок пока нет
- General Virology 3.doc - 0Документ14 страницGeneral Virology 3.doc - 0Isak Isak IsakОценок пока нет
- Blood SmearsДокумент4 страницыBlood SmearsAmor KourdouliОценок пока нет
- Characteristics: Description: Ascaris Lumbricoides Trichuris Trichiura Enterobius Vermicularis Capillaria PhilippinensisДокумент8 страницCharacteristics: Description: Ascaris Lumbricoides Trichuris Trichiura Enterobius Vermicularis Capillaria PhilippinensisAlcera JemОценок пока нет
- 15medically Important Viruses PDFДокумент75 страниц15medically Important Viruses PDFdan ghaОценок пока нет
- Entamoeba SPPДокумент21 страницаEntamoeba SPPragnabulletinОценок пока нет
- What Is CoagulationДокумент6 страницWhat Is CoagulationKang Wenn LeeОценок пока нет
- Campylobacter & Plesiomonas - Bacter ReportДокумент55 страницCampylobacter & Plesiomonas - Bacter ReportRona SalandoОценок пока нет
- 5 Basic VirologyДокумент71 страница5 Basic VirologyErdemОценок пока нет
- Medical VirologyДокумент136 страницMedical VirologysoundharyaОценок пока нет
- Analysis of Urine and Other Body: Central Luzon Doctors' Hospital Educational InstitutionДокумент63 страницыAnalysis of Urine and Other Body: Central Luzon Doctors' Hospital Educational InstitutionRenaОценок пока нет
- Types of MycosesДокумент8 страницTypes of MycosesTimothy John ValenciaОценок пока нет
- Lesson 3Документ71 страницаLesson 3Angel joyce ValenciaОценок пока нет
- Introduction To UrinalysisДокумент8 страницIntroduction To UrinalysisKyle PicocОценок пока нет
- Lecture 11 SCI 8007SEF Medical Microbiology & Virology Topic 5 - Introduction of Mycology - 12 Nov 2023Документ80 страницLecture 11 SCI 8007SEF Medical Microbiology & Virology Topic 5 - Introduction of Mycology - 12 Nov 2023YY CheungОценок пока нет
- Cultivation Media For BacteriaДокумент4 страницыCultivation Media For BacterialapetitefilleОценок пока нет
- Pre-Analytical Considerations in PhlebotomyДокумент56 страницPre-Analytical Considerations in PhlebotomyAngel joyce ValenciaОценок пока нет
- Blood Loss: Acute Chronic Inadequate Production of Normal Blood CellsДокумент11 страницBlood Loss: Acute Chronic Inadequate Production of Normal Blood CellsSheila Amor BodegasОценок пока нет
- Parasitology: By: Jahre Mark Toledo, RMT, Maed BioДокумент50 страницParasitology: By: Jahre Mark Toledo, RMT, Maed BioJahre Mark Toledo100% (1)
- Rickettsial Diseases: DR Sajan Christopher Assistant Professor of Medicine Medical College, ThiruvananthapuramДокумент40 страницRickettsial Diseases: DR Sajan Christopher Assistant Professor of Medicine Medical College, ThiruvananthapuramYogya MandaliОценок пока нет
- Family Neisseriaceae: Joy P. Calayo, RMT, MSMT UST Faculty of Pharmacy Dept. of Medical TechnologyДокумент18 страницFamily Neisseriaceae: Joy P. Calayo, RMT, MSMT UST Faculty of Pharmacy Dept. of Medical Technologypixholic100% (1)
- DermatophytesДокумент1 страницаDermatophytesKoo ThaОценок пока нет
- 2.01 Diagnostic VirologyДокумент6 страниц2.01 Diagnostic VirologyMaria MikaelaОценок пока нет
- Fungal Infections in IcuДокумент195 страницFungal Infections in IcubhumikaОценок пока нет
- Superficial MycosisДокумент61 страницаSuperficial MycosisBrightKinglySweetDomsonОценок пока нет
- Rickettsia eДокумент10 страницRickettsia eDeep Iyaz100% (1)
- Microbiology - ParasitologyДокумент34 страницыMicrobiology - ParasitologySasi DharanОценок пока нет
- (OS 217 - IDS) LEC 04 Diagnostic MycologyДокумент6 страниц(OS 217 - IDS) LEC 04 Diagnostic MycologyErtyWitalayaL.ToruanОценок пока нет
- Introduction To Microbiology Taxonomy Morphology: Dr. José L. Navarro Clinical Microbiologist, (Madrid, Spain)Документ49 страницIntroduction To Microbiology Taxonomy Morphology: Dr. José L. Navarro Clinical Microbiologist, (Madrid, Spain)ImaPratiwiОценок пока нет
- Foundations in Microbiology: Nonspecific Host Defenses TalaroДокумент35 страницFoundations in Microbiology: Nonspecific Host Defenses TalaroOdurОценок пока нет
- My CologyДокумент3 страницыMy CologyAbdul Samad NoonariОценок пока нет
- Helicobacter Pylori: Dr.B.BoyleДокумент35 страницHelicobacter Pylori: Dr.B.BoyleTammy AdjaОценок пока нет
- Diagnostic Microbiology - : University of Santo Tomas - Medical TechnologyДокумент6 страницDiagnostic Microbiology - : University of Santo Tomas - Medical TechnologyWynlor AbarcaОценок пока нет
- Microbial GrowthДокумент96 страницMicrobial GrowthJenniferОценок пока нет
- Sir Alvin Rey Flores: Echinococcus Granulosus, Taenia Solium)Документ5 страницSir Alvin Rey Flores: Echinococcus Granulosus, Taenia Solium)Corin LimОценок пока нет
- Week 1 Day 1 LessonДокумент143 страницыWeek 1 Day 1 LessonTRIXIE CYRAH MIRANDA SALAVIAОценок пока нет
- 29th ChapДокумент129 страниц29th ChapJoshОценок пока нет
- CompilationДокумент3 страницыCompilationBelle Cherlette FelipeОценок пока нет
- Guidlines Pregnancy and Heart DiseaseДокумент52 страницыGuidlines Pregnancy and Heart DiseasePanggih Sekar Palupi IIОценок пока нет
- Pregnancy PDFДокумент18 страницPregnancy PDFNada MotahharОценок пока нет
- Managing Complications in Pregnancy and ChildbirthДокумент390 страницManaging Complications in Pregnancy and ChildbirthxxdrivexxОценок пока нет
- Pregnancy MonographДокумент81 страницаPregnancy Monographwrite2hannanОценок пока нет
- Pregnancy PDFДокумент18 страницPregnancy PDFNada MotahharОценок пока нет
- Clinical Practice Guidelines For The Use of Anti D Immunoglobin For The Prevention of RHD Haemolytic Disease of The NewbornДокумент18 страницClinical Practice Guidelines For The Use of Anti D Immunoglobin For The Prevention of RHD Haemolytic Disease of The NewbornxxdrivexxОценок пока нет
- Nutrition in PregnancyДокумент15 страницNutrition in PregnancyxxdrivexxОценок пока нет
- Healthy Pregnancy GuideДокумент56 страницHealthy Pregnancy Guideprince168Оценок пока нет
- Chickenpox in PregnancyДокумент23 страницыChickenpox in PregnancyxxdrivexxОценок пока нет
- Irish Maternity Early Warning System (IMEWS)Документ27 страницIrish Maternity Early Warning System (IMEWS)xxdrivexxОценок пока нет
- Resuscitation For The Pregnant WomanДокумент18 страницResuscitation For The Pregnant WomanxxdrivexxОценок пока нет
- Fetal Growth Restriction - Recognition, Diagnosis and ManagementДокумент28 страницFetal Growth Restriction - Recognition, Diagnosis and ManagementxxdrivexxОценок пока нет
- Management of Obstetric Anal Sphincter InjuryДокумент20 страницManagement of Obstetric Anal Sphincter InjuryxxdrivexxОценок пока нет
- Nutrition During PregnancyДокумент48 страницNutrition During PregnancyxxdrivexxОценок пока нет
- The Diagnosis and Management of Pre-Eclampsia and EclampsiaДокумент22 страницыThe Diagnosis and Management of Pre-Eclampsia and EclampsiaxxdrivexxОценок пока нет
- Parvovirus B19 Exposure Infection During PregnancyДокумент16 страницParvovirus B19 Exposure Infection During PregnancyxxdrivexxОценок пока нет
- Management of Multiple PregnancyДокумент14 страницManagement of Multiple PregnancyxxdrivexxОценок пока нет
- Management of Pelvic Girdle Pain in Pregnancy and Post-PartumДокумент27 страницManagement of Pelvic Girdle Pain in Pregnancy and Post-PartumxxdrivexxОценок пока нет
- Management of Pelvic Girdle Pain in Pregnancy and Post-PartumДокумент27 страницManagement of Pelvic Girdle Pain in Pregnancy and Post-PartumxxdrivexxОценок пока нет
- Management of Breech PresentationДокумент26 страницManagement of Breech PresentationxxdrivexxОценок пока нет
- Preterm Prelabour Rupture of Membranes (PPROM)Документ19 страницPreterm Prelabour Rupture of Membranes (PPROM)xxdrivexxОценок пока нет
- Nutrition During PregnancyДокумент48 страницNutrition During PregnancyxxdrivexxОценок пока нет
- Obesity and PregnancyДокумент39 страницObesity and PregnancyxxdrivexxОценок пока нет
- The Management of Second Trimester MiscarriageДокумент30 страницThe Management of Second Trimester MiscarriagexxdrivexxОценок пока нет
- Ultrasound Diagnosis of Early Pregnancy LossДокумент18 страницUltrasound Diagnosis of Early Pregnancy LossxxdrivexxОценок пока нет
- Oxytocin To Accelerate or Induce LabourДокумент20 страницOxytocin To Accelerate or Induce LabourxxdrivexxОценок пока нет
- Tocolytic Treatment in PregnancyДокумент21 страницаTocolytic Treatment in PregnancyxxdrivexxОценок пока нет
- Resuscitation For The Pregnant WomanДокумент18 страницResuscitation For The Pregnant WomanxxdrivexxОценок пока нет
- Listeriosis in PregnancyДокумент18 страницListeriosis in PregnancyxxdrivexxОценок пока нет
- Intrapartum Fetal Heart Rate MonitoringДокумент15 страницIntrapartum Fetal Heart Rate MonitoringxxdrivexxОценок пока нет
- I. Objectives:: Semi-Detailed Lesson Plan in Reading and Writing (Grade 11)Документ5 страницI. Objectives:: Semi-Detailed Lesson Plan in Reading and Writing (Grade 11)Shelton Lyndon CemanesОценок пока нет
- Propp Function's Types:: 1-Absentation: One of The Members of A Family Absents Himself From HomeДокумент10 страницPropp Function's Types:: 1-Absentation: One of The Members of A Family Absents Himself From HomeRohith KumarОценок пока нет
- The Dust Bunnies COL FKBДокумент36 страницThe Dust Bunnies COL FKBPradeep ManralОценок пока нет
- GSM Radio ConceptsДокумент3 страницыGSM Radio ConceptsMD SahidОценок пока нет
- Internal Gear Pump: Replaces: 03.08 Material No. R901216585 Type PGH.-3XДокумент36 страницInternal Gear Pump: Replaces: 03.08 Material No. R901216585 Type PGH.-3XbiabamanbemanОценок пока нет
- Enhancing Guest Experience and Operational Efficiency in Hotels Through Robotic Technology-A Comprehensive Review.Документ8 страницEnhancing Guest Experience and Operational Efficiency in Hotels Through Robotic Technology-A Comprehensive Review.Chandigarh PhilosophersОценок пока нет
- Cs205-E S3dec18 KtuwebДокумент2 страницыCs205-E S3dec18 KtuwebVighnesh MuralyОценок пока нет
- Laporan Keuangan TRIN Per Juni 2023-FinalДокумент123 страницыLaporan Keuangan TRIN Per Juni 2023-FinalAdit RamdhaniОценок пока нет
- MFD16I003 FinalДокумент16 страницMFD16I003 FinalAditya KumarОценок пока нет
- II. Put The Verbs in The Correct FormsДокумент3 страницыII. Put The Verbs in The Correct FormsNguyễn Bích DiệpОценок пока нет
- FMO ESG Toolkit (AutoRecovered)Документ149 страницFMO ESG Toolkit (AutoRecovered)me.abhishekpОценок пока нет
- Silk Road Ensemble in Chapel HillДокумент1 страницаSilk Road Ensemble in Chapel HillEmil KangОценок пока нет
- Enemies Beyond Character Creation SupplementДокумент8 страницEnemies Beyond Character Creation SupplementCain BlachartОценок пока нет
- NASA Gemini 4 Press KitДокумент94 страницыNASA Gemini 4 Press KitOrion2015100% (1)
- Merchant Shipping MINIMUM SAFE MANNING Regulations 2016Документ14 страницMerchant Shipping MINIMUM SAFE MANNING Regulations 2016Arthur SchoutОценок пока нет
- One Foot in The Grave - Copy For PlayersДокумент76 страницOne Foot in The Grave - Copy For Playerssveni meierОценок пока нет
- De On Tap So 4-6Документ8 страницDe On Tap So 4-6Quy DoОценок пока нет
- Brachiocephalic Artery: AnteriorДокумент37 страницBrachiocephalic Artery: AnteriorFarah FarahОценок пока нет
- Choosing An Effective Visual ToolДокумент9 страницChoosing An Effective Visual ToolAdil Bin KhalidОценок пока нет
- EstoqueДокумент56 страницEstoqueGustavo OliveiraОценок пока нет
- Thesis Topics in Medicine in Delhi UniversityДокумент8 страницThesis Topics in Medicine in Delhi UniversityBecky Goins100% (2)
- A Project Report On "A Comparative Study Between Hero Honda Splendor+ and Its Competitors To Increase The Market Share in MUDHOL RegionДокумент70 страницA Project Report On "A Comparative Study Between Hero Honda Splendor+ and Its Competitors To Increase The Market Share in MUDHOL RegionBabasab Patil (Karrisatte)Оценок пока нет
- Best of The Photo DetectiveДокумент55 страницBest of The Photo DetectiveSazeed Hossain100% (3)
- Fike ECARO-25 Frequently Asked Questions (FAQ)Документ8 страницFike ECARO-25 Frequently Asked Questions (FAQ)Jubert RaymundoОценок пока нет
- Grammar Practice #2Документ6 страницGrammar Practice #2Constantin OpreaОценок пока нет
- DS SX1280-1-2 V3.0Документ143 страницыDS SX1280-1-2 V3.0bkzzОценок пока нет
- Datalogic tl46 A Manual - 230104 - 140343Документ2 страницыDatalogic tl46 A Manual - 230104 - 140343Emmanuel Baldenegro PadillaОценок пока нет
- Eureka Math Grade 2 Module 3 Parent Tip Sheet 1Документ2 страницыEureka Math Grade 2 Module 3 Parent Tip Sheet 1api-324573119Оценок пока нет
- NDT HandBook Volume 10 (NDT Overview)Документ600 страницNDT HandBook Volume 10 (NDT Overview)mahesh95% (19)
- DescriptiveДокумент1 страницаDescriptiveRizqa Anisa FadhilahОценок пока нет