Академический Документы
Профессиональный Документы
Культура Документы
Formulation and Evaluation of Bisoprolol Fumarate Buccal Patches by Using Selected Polymers
Загружено:
AlinaDianaИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Formulation and Evaluation of Bisoprolol Fumarate Buccal Patches by Using Selected Polymers
Загружено:
AlinaDianaАвторское право:
Доступные форматы
IJPCBS 2013, 3(3), 854-860
Sarath Chandran et al.
ISSN: 2249-9504
INTERNATIONAL JOURNAL OF PHARMACEUTICAL, CHEMICAL AND BIOLOGICAL SCIENCES
Research Article
Available online at www.ijpcbs.com
FORMULATION AND EVALUATION OF BISOPROLOL FUMARATE BUCCAL
PATCHES BY USING SELECTED POLYMERS
Sarath chandran C*, KV. Shijith, KV . Vipin and Ann Rose Augusthy
Department of Pharmaceutics, Academy of Pharmaceutical Sciences,
Pariyaram- 670 503, Kannur, Kerala, India.
ABSTRACT
This investigation mainly focused on the ability of polymer to release the Bisoprolol fumarate in
a controlled pre determined manner. The polymers selected for the investigation include
chitosan. HPMC, and sodium CMC. The polymers were selected on the basis of their property.
The muco adhesive buccal patches were prepared by solvent casting method with appropriate
modification. The prepared patches were subjected to physical evaluations, invitro diffusion
study, and stability study. The result obtained was satisfactory with all the formulation, but, the
patches prepared with 2% chitosan showed a better invitro diffusion result as it can diffuse 96%
of drug within 12 hour of the therapy. The result of physical evaluation and stability study
indicating that the Bisoprolol buccal patches with 2% chitosan could effectively treat the possible
anginal attack and hypertension.
Keywords: buccal patches, mucoadhesion, chitosan, HPMC, sodium CMC.
INTRODUCTION
Extensive effort has been made to focused on
targeting a drug or drug delivery system in a
particular region of the body not only for targeting
of drug, but also for better systemic delivery. One
amongst the best was mucoadhesive buccal drug
delivery. Mucoadhesive are synthetic or natural
polymer that can effectively interact with the
mucin layer, thus offers better results. Various
polymers are under investigation as carrier for
buccal drug delivery.
In this investigation three polymers, chitosan,
HPMC and sodium CMC, were selected on the
basis of their property. Chitosan is a natural bio
compatable and bio degradable polymer,
extensively used in the devolopement of
mucoadhesive buccal drug delivery. Chitosan has
a an excellent filim forming ability and better
muco adhesive property. The mucoadhesive
property of chitosan either due to its ability to
form secondary chemical bonds such as hydrogen
bonds or ionic interactions between the positively
charged amino groups of chitosan and the
negatively charged mucin. Appart from this
chitosan has a cell binding and membrane
permeation activity 21.
HPMC is a semisynthetic cellulose derivative,
biocompatable, has a variety of application in
novel
drug
delivery
systems
including
mucoadhesive property. The property of HPMC to
form a strong, flexible filim, made the polymer to
use in this investigation. It is stable over a pH
range of 3 to 11. Apart from this HPMC has the
ability to absorb water and swell, there by
enhancing the thickness of the filim, thus an ideal
candidate for mucoadhesive buccal systems1,2,21.
The other polymer used in this investigation is
sodium CMC, other cellulose derivative,
biocompatable polymer, already proven its ability
to form better mucoadhesive buccal drug delivery
system. It is an anionic polymer made by swelling
cellulose with NaOH and then reacting it with
monochloroacetic acid. It is stable over a pH
range of 4 to 10. The thixotropic behaviour of the
854
IJPCBS 2013, 3(3), 854-860
Sarath Chandran et al.
CMC solution made this polymer as an ideal
candidature for this study 1,2,21.
This investigation mainly focused on the ability of
polymer to release the Bisoprolol fumarate (BPL)
in a controlled pre-determined manner. Bisoprolol
fumarate is a beta adrenergic blocking agent, used
to treat cardiac disease. Bisoprolol is already
available in the market as 5mg, 10mg, and 20mg
tablet. The drug has a half life of 10 hrs and shows
a bio availability of more than 80 percentage. Even
though the drug has relatively high bio availability
and half-life, the controlled release formulation
has its own significance for improving the onset of
action, release characteristics and reducing the
side effects.
ISSN: 2249-9504
thickness was measured at five different spots of
the patch and average was taken.
Weight variation
Ten patches of 1cm2 were weighed individually
and average of those patches measured.
Surface pH7,8,9
Buccal patches were left to swell for 1 hour on the
surface of 2% agar plate, it was allowed to stand
until it is solidified to form a gel at room
temperature. The surface pH was measured by
means of pH paper placed on the surface of the
swollen patch.
% Swelling Index10,11
The developed buccal patches were cut in to small
sizes of 1.5 cm diameter. This patch was placed on
the surface of 2% agar plate and the diameter at
different time intervals where taken up to 5 hrs
and the percentage swelling index was calculated
using the formula,
MATERIALS AND METHODS
Bisoprololfumarate (BPL) was obtained as a gift
sample from Chethana Pharmaceuticals, Kerala,
chitosan and sodium CMC were obtained from
Balaji chemicals, Gujarat, HPMC was obtained
from Otto kemi, Mumbai. All other reagents and
chemicals were of analytical or pharmaceutical
grade.
% SD =
x 100
Where, % SD = % swelling by diameter method
Dt = diameter of swollen patch after time t
Do = original patch diameter.
Preparation of bisoprolol fumarate buccal
patches3
The buccal patches containing BPL were prepared
by solvent casting method with required
modification. The desired percentage of polymer
(chitosan, HPMC or sodium CMC) was dissolved in
1% acetic acid by stirring in a mechanical stirrer
for 2 hours. This solution was filtered through a
muslin cloth to remove debris. The above solution
was added with calculated amount of BPL and10
% ethanol and stirred in a mechanical stirrer for 2
hours. This solution was kept overnight to remove
air bubbles and poured in to a glass mould having
a surface area of 40 cm2, to which glycerin added
as plasticizer. It was dried in an oven at 450C, cut
in to desired size, and packed in to aluminium foil
for further studies.
% Moisture content4,5
The buccal patches were weighed accurately and
kept in desiccators containing anhydrous calcium
chloride. After three days, the patches were taken
out and weighed. The moisture content (%) was
determined by the formula
% Moisture content =
Initial weight Final weight 100
Initial weight
Tensile Strength12,13
The instrument used to measure the tensile
strength was designed in pharmaceutics
laboratory especially for this project work. The
instrument is a modification of chemical balance
used in the normal laboratory. One pan of the
balance was replaced with one metallic plate
having a hook for attaching the film. The
equilibrium of the balance was adjusted by adding
weight to the right pan of balance. The instrument
was modified in such a way that the patch can be
fixed up between two hooks of horizontal beams
to hold the test film. A film of 2.5cm length was
attached to one side hook of the balance and the
Folding Endurance4,5
Folding endurance of the patches was determined
by repeatedly folding a small strip of the patch
(approximately 2x2 cm) at the same place till it
broke. The number of times patch could be folded
at the same place, without breaking gives the
value of folding endurance.
Patch thickness6
The thickness of the buccal patch was measured
by using screw gauge with a least count of 0.01
mm at different spots of the patches. The
855
IJPCBS 2013, 3(3), 854-860
Sarath Chandran et al.
other side hook was attached to plate fixed up to
the pan as shown in the figure.
Tensile strength,
T=
ISSN: 2249-9504
RESULTS AND DISCUSSION
Buccal patch is a category of controlled DDS in
which the release of drug was controlled in a predetermined rate by using suitable polymeric
systems. All the selected polymers were well
established for designing various novel drug
delivery systems. 1% acetic acid (AA) was used as
solvent for developing the formulations. The
concentrations for selected polymers and AA were
optimized during the investigation (Table No.1).
10% ethanol was incorporated as the permeation
enhancer for all the developed patches and
glycerin was selected as plasticizer. Developed
patches were cut in to suitable size and packed in
aluminum foil and used for further evaluations.
The visual inspection confirmed that the prepared
patches had satisfactory physical attributes in
terms of color and clarity. Patches developed
using chitosan had pale yellow in color, whereas
the HPMC and sodium CMC based patches had
white colour. In spite of the application of heat
during the development of the formulations,
colour of developed patches were almost same as
that of pure polymers incorporated 22. The results
of physical characteristics were satisfactory for a
buccal patches developed using selected
polymers.
Folding endurance for developed buccal patches
were ranging between 165-255 for all the
developed patches (Table No.2). Lowest folding
endurance was calculated for the patches
prepared using sodium CMC, where highest
folding endurance of 255 was obtained for HPMC
based patches. All the patches, irrespective of
polymers used, showed good folding endurance
and ensured good flexibility 23.
All the developed patches had a thickness in
between 0.5-0.7mm (Table No.2). Data for patch
thickness were matching with the desired level of
thickness for buccal patches. The average weight
of drug loaded patches was calculated to ensure
the weight uniformity 24. Data obtained during
evaluation of weight variation proved the
uniformity of contents in the developed
formulations. Higher the weight variation, higher
will be the variation in contents which make the
formulation therapeutically unacceptable 25. The
average weight obtained for the patches were
ranging between 9.8-10.8 mg. The patches
prepared using sodium CMC (F3) had the lowest
average weight in comparison with patches
developed using other two polymers, this may be
due to the lower molecular weight of sodium CMC
in comparison with HPMC and chitosan.
Dynes/cm
T= force at break/ initial cross-sectional area of sample.
Where,
M = mass in grams
g = acceleration due to gravity 980 cm/sec
B = breadth of the specimen in cm
t = thickness of sample in cm.
%Drug content14,15,16
Prepared buccal patch was dissolved in 100ml of
Phosphate buffer solution (PBS) of pH 6.8 using a
magnetic stirrer for 12 hours and then sonicated
for 30 minutes. The solution was centrifuged and
then filtered. The drug content determination was
done by using UV spectroscopy at 223 nm.
In vitro diffusion study17.18
In vitro diffusion study was performed by using
modified franz diffusion cell across cellophane
membrane. Phosphate buffer solution (PBS) of pH
6.8 was used as medium for diffusion study.
Patches of dimension 2x2cm2were placed on the
membrane, which was placed between donor and
receptor compartment of franz diffusion cell.
Cellophane membrane was brought in contact
with PBS of pH 6.8 filled in receptor compartment.
Temperature was maintained at 370C with stirring
at 50 rpm using magnetic beed stirrer. 1ml of
sample
was
withdrawn
from
receptor
compartment at pre-determined interval and was
replaced with fresh PBS of pH 6.8. With suitable
dilution, samples were measured for absorbance
at 223nm using UV visible spectrophotometer.
Stability study 19,20
Stability studies were performed in accordance
with ICH guidelines for accelerated stability
testing. Patches (2x2 cm2) were wrapped
individually in aluminium foil and maintained at
refrigerated
temperature(420C),
room
temperature(3020C) and oven temperature
(45
) and 75
RH for a period of 1
month. Changes in the appearance and drug
content of the stored patches were investigated
after storage period.
856
IJPCBS 2013, 3(3), 854-860
Sarath Chandran et al.
The surface pH for the developed formulations
were approximately 7.0(Table No.2). The pH at
mucosal surface is approximately 6.8. The pH
between 6.5-6.7 of the developed patches
indicates that the patches may be safe enough for
the regular application in the mucosal region. The
% swelling index were calculated after 5 hours
and recorded highest for sodium CMC and lowest
for chitosan. Since chitosan is a natural bio
degradable polymer, which takes much time to
swell in the AA medium and erode slowly which
might have reflected through low swelling index
value. The swelling property of chitosan may
contributes to its improved release profile as a
controlled release formulation. No significant
difference was found between the patches in
terms of moisture content.
Tensile strength value of chitosan based
formulations were 2.87-2.95 kg/cm2 which was
highest in comparison with other formulations.
Tensile strength proves the resistance power of
the patch from breaking apart. The high tensile
strength of chitosan may be due to the nature of
polymeric chain present in the structure of
chitosan. Lowest average tensile strength was
recorded for sodium CMC based buccal patches.
Drug content of more than 90% in the formulation
shows the high amount of drug present in the
formulation, without causing any change in the
ideal property of buccal patches Highest % drug
content was calculated for formulation F1 which
was chitosan based, lowest %Drug content was
obtained for HPMC based formulation F2. The
high % Drug content of chitosan may be due to the
high molecular weight of the chitosan as
compared to HPMC and sodium CMC which results
in high entrapment efficiency of drug within the
polymer structure of chitosan.
The in vitro diffusion study may be used as an
indirect measurement of drug solubility,
especially in the preliminary assessment of
formulation factors and manufacturing methods
that are likely to influence the bioavailability. In
vitro diffusion study was carried out using
modified franz diffusion cell across cellophane
membrane using PBS of pH6.8 as medium. When
ISSN: 2249-9504
the diffusion profile for F1,F2 and F3 were cross
compared, the diffusion profile of F2,ie 2%
chitosan buccal patches showed much improved
results in comparison to F4 and F6. During the
initial stages of the diffusion study ,ie within 1
hour, 25% of drug has been diffused from F2. %
Drug diffused from F2 after 1hour was much
higher than the % diffusion of drug from
formulation F4 and F6. This data proves that BPL
may experience good initial burst release when
formulated as buccal patch with 2% chitosan. The
diffusion data obtained was impressive when
compared with % drug release profile of US
patented multiparticulate tablet of BPL which is
already existing in US market26. After the good
initial burst release, the formulation F1 showed a
controlled release profile upto a period of 12 hour.
At the end of 12th hour of the diffusion study, the
% drug diffused from F1 was 93.96, at the same
period of study, F2 and F3 had 87.09% and
78.77% drug diffused (Table No.3) & (Fig No.1).
Since HPMC and sodium CMC, being a
semisynthetic derivative of cellulose, when these
polymers comes in contact with saliva forms a
gelatinous barrier layer at the surface of patches,
which may result in its lower rate of diffusion in
comparison with chitosan based buccal patch27,28.
Apart from this, chitosan possess inherent
permeation enhancing property29, which might
have resulted in a synergistic effect with 10%
ethanol incorporated in formulation for improved
release properties of chitosan based buccal patch.
There was no significant change reported in
colour, thickness, and pH of all the developed
formulations at the end of one month period
irrespective of the temperature difference (Table
No.4). The % drug content calculated for
formulation F1 was 84.5 0.04% which was much
better than the other formulations during the
study hence chitosan may be the best suitable
polymer to design and develop a stable buccal
patche containing BPL. Based on available results,
these developed buccal patches may be more
stable between a temperature range of 0-300C,
whereas higher temperature may cause
deleterious effect on patches.
Table 1: Composition of formulation
Ingredients
Bisoprololfumarate
Chitosan(%) in acetic acid 1%
HPMC(%) in acetic acid 1%
Sodium CMC(%) in acetic acid 1%
Ethanol 10%
Glycerine
857
Formulation code
F1
F2
F3
100
100
100
2%
2%
2%
1
1
1
0.5
0.5
0.5
IJPCBS 2013, 3(3), 854-860
Sarath Chandran et al.
ISSN: 2249-9504
Table 2: Characterization of developed formulations
FORMULATION CODE
Appearance
Texture
Folding endurance
Thickness(mm)
Average weight (mg)
Surface Ph
%Swelling index
(after 5 hours)
% Moisture content
Tensile strength
(Kg/cm2)
% Drug content
F1
Smooth
Flexible
2102
0.70.2
11.3
6.7
F2
Smooth
Flexible
2553
0.60.2
10.8
6.6
F3
Smooth
Flexible
1852
0.60.2
10.1
6.6
36
34
35
1.7
3.3
2.5
2.950.03
2.650.03
2.610.02
98.79
94.52
95.01
Table 3: In vitro diffusion data of
developed formulations
TIME (Hrs)
0
0.5
1
2
3
4
5
6
8
12
% Drug diffused
F2
F4
F6
0
0
0
11.95
8.35
7.47
25.5
16.07
14.95
33.4
28.68
21.66
40.36
36.48
27.13
49.91
45.58
38.4
62
55.43
45.99
74.73
60.63
61.1
89.17
81.52
72.24
93.96
87.09
78.77
Table 4: Stability data of all formulation
Formulation code
F1
F2
F3
Physical appearance
420C
3020C
4520C
+
+
++
++
+
+++
++
+
+++
420C
98.60
93.58
94.35
% Drug content
3020C
4520C
98.75
84.5
93.95
71.11
94.85
72.95
+ - no change, ++ - marginal change, +++ - significant change.
IN VITRO RELEASE PLOT OF FORMULATIONS F1- F6
100
90
80
% Release
70
60
50
F1
40
F2
30
F3
20
10
0
0
10
12
14
Time (hrs)
Fig. 1: In vitro diffusion plot of developed formulation F1- F3
858
IJPCBS 2013, 3(3), 854-860
Sarath Chandran et al.
CONCLUSION
The above investigation reveals that the property
of developed patches greatly depends on the
nature of the selected polymer use in the
formulations. From overall investigation data, it
can be concluded that 2% chitosan may be the
best polymer to develop a stable mucoadhesive
patches to deliver Bisoprololfumarate. Design and
development of such buccal patches may be highly
beneficial which can deliver drug up to a period of
12hrs duration. Hence application of buccal
patches at bed time may assure maximum
concentration of Bisoprolol fumarate in the early
mornings, which can avoid the possible angina
attack for hypertensive patients.
10.
11.
12.
13.
REFERENCES
1. Sarathchandran.C, Shijith.k.v, A conscise
insight on mucoadhesivebuccal drug
delivery system, Lamb.Acad.Pub.2012: 1-65
2. KV. Shijith, SarathChandran C, KV. Vipin,
Ann Rose Augusty, K. Premaletha, A review
on basics behind development of muco
adhesive buccal drug delivery systems,
IJAPBC.2013; 2(2): 310-317.
3. S. Roy, K. Pal, A. Anis, K. Pramanik and
B.Prabhakar, Polymers in mucoadhesive
drug delivery system, A brief note, designed
monomers and polymers.2009; 12: 483495.
4. Y Indira Muzib, K SrujanaKumari,
Mucoadhesivebuccal films of glibenclamide:
Development and evaluation, Int. J. Pharma.
Ivn.2011; 1(1):42-47
5. Vinod R, Ashok kumar P, SomeswaraRao B,
Suresh V. kulkarni and Shankar MS, Design
and evaluation of miconazole nitrate
buccalmucoadhesive patches, J. Pharmacy
Res.2010; 3 (6): 1338-1341
6. G. A. Khairnar, F. J. Sayyad, Development of
buccal drug delivery system based on
mucoadhesive polymers, Int.J. PharmTech
Res.2010; 2(1): 719-735
7. N.K. Jain, Controlled and novel drug
delivery, CBS Publishers and Distributors,
1st Edition.2010:52-81
8. RaghavendraRao N. G. and Suryakar V. B,
Formulation and evaluation of montelukast
sodium mucoadhesivebuccal patches for
chronic asthma attacks,Int.J. Pharma and
Bio Sci.2010: 1(2)
9. M. Balamurugan, V.S. Saravanan, P. Ganesh,
S.P.
Senthil,
P.V.
Hemalatha
and
SudhirPandya, Development and In-vitro
Evaluation of MucoadhesiveBuccal Tablets
14.
15.
16.
17.
18.
19.
20.
859
ISSN: 2249-9504
of Domperidone, Res.J Pharmacy and
Tech.2008; 1(4).
A Semalty, Mona Semalty, and U Nautiyal,
Formulation
and
evaluation
of
mucoadhesivebuccal films of Enalapril
maleate, Ind. J.Pharma. Sci.2010; 72(5):
571575
M Nappinnai, R chandanbala, R Balajirajan,
Formulation
and
evaluation
of
nitrendipinebuccal films, Ind.J. Pharm.
Sci.2008;70 (5): 631-635.
Wong CF, Yuen KH, Peh KK. Formulation
and evaluation of controlled release
Eudragitbuccal patches. Int J Pharm. 1999
Feb 1; 178(1): 11-22.
Balamurugan K, Pandit JK, Choudary PK,
Balasubramaniam J. Systemic absorption of
Propranolol
Hydrochloride
from
buccoadhesive films. Ind J Pharm Sci. 2001;
63(6): 473-480.
Nafee NA, Ismail FA, Boraie NA, Mortada
LM. Mucoadhesivebuccal patches of
Miconazole nitrate: in vitro/in vivo
performance and effect of ageing. Int J
Pharm. 2003 Oct; 264(1-2): 1-14.
Panigrahi L, Pattnaik S, Ghosal SK. Design
and
characterization
of
mucoadhesivebuccal patches of Diclofenac
Sodium. Ind J Pharm Sci. 2005; 67(3): 319326.
Pavankumar GV, Ramakrishna V, William GJ,
Konde A. Formulation and evaluation of
buccal films of Salbutamol Sulphate. Ind J
Pharm Sci. 2005; 67(2):
160-164.
Chinna Reddy Palem, Ramesh Gannu,
Vamshi Vishnu Yamsani, Shravan Kumar
Yamsani and MadhusudanRaoYamsani,
Development of bilayeredmucoadhesive
patches for buccal delivery of felodipine: in
vitro and ex vivo characterization, Cur.
trends in Biotech. and Pharmacy. 2010
April; 4(2).
J. Thimmasetty, G. S. Pandey, P. R.
SatheshBabu, Design and evaluation of
carvidilolbuccalmucoadhesive
patches,
Pak.J.Pharm. Sci. 2008 July;21(3): 241-248.
Garry Kerch, VadimKorkhov, Effect of
storage time and temperature on structure,
mechanical and barrier properties of
chitosan-based films, Euro. Food Res. and
Tech.2012; 232(1):17-22.
Kristine
Romren,
Astrid
Aaberge,
GroSmistad, Beate J Thu, OysteinEvensen,
Long-term stability of chitosan-based
IJPCBS 2013, 3(3), 854-860
21.
22.
23.
24.
25.
Sarath Chandran et al.
polyplexes,
PubMedPharm.
Res.2005;21(12):2340-2346
Punitha S, Girish Y, Polymers in
mucoadhesive buccal drug delivery system
A review, Int. J. Res. Pharm. Sci. 2010;1(2):
170-186.
J. Varshosaz, Z. Dehghan, Development and
characterization
of
buccoadhesiveNifedipine tablets, Eur. J. of
Pharma. and Biopharm.2002; 54: 135141.
Wong CF, Yuen KH, Peh KK. Formulation
and evaluation of controlled release
Eudragitbuccal patches. Int J Pharm. 1999
Feb 1; 178(1): 11-22.
Subhash V. Deshmane, Madhuri A.
Channawar,
Anil
V.
Chandewar1,
UnmeshM.Joshi, Kailash R. Biyani, Chitosan
based
sustained
release
mucoadhesivebuccal patches containing
verapamil HCl, Int.J. Pharmacy and Pharma.
Sci.(Nov.-Dec. 2009); 1(1)
Liji Jacob, C. I. Sajeeth, K. Santhi, Design,
Development and Evaluation
of the
26.
27.
28.
29.
860
ISSN: 2249-9504
Mucoadhesive Patches of Nifedipine for
Buccal Delivery, Int. J. of Pharmacy and
Techn.2012;4 (1): 3883-3900.
Stark etal, multiparticulate Bisoprolol
formulation, United state patent, patent
no.US 6733789B1, patented date. May 11,
2004.
VipinBansal, Pramod Kumar Sharma, Nitin
Sharma, Om Prakash Pal, RishabhaMalviya,
Applications of Chitosan and Chitosan
Derivatives in Drug Delivery, Adv. in Biolog.
Res.2011; 5 (1): 28-37.
InampudiAjit, AdimoolanSemthil, Bhosale
Rahul, V.B.NarayanaSwamy, Formulation
and evaluation of VelnafaxineHClbuccal
tablet, Int.Res. J. of Pharmacy.2012;3(1):
226-231.
Muralikrishna K, Nagaraju T, Gowthami R,
Rajashekar M, Sandeep S, Himabindu S,
ShravankumarYamsani,
Comprehensive
review on buccal delivery, . Int J Pharm.
2012; 2(1): 205-217.
Вам также может понравиться
- Flow charts of pharmaceutical quality control tests for different dosage formsОт EverandFlow charts of pharmaceutical quality control tests for different dosage formsОценок пока нет
- Bisopr MucoДокумент5 страницBisopr Mucovipinkv99Оценок пока нет
- A Laboratory Manual of Physical PharmaceuticsОт EverandA Laboratory Manual of Physical PharmaceuticsРейтинг: 2.5 из 5 звезд2.5/5 (2)
- Pandit Et Al HPMC Karbopol 2%Документ6 страницPandit Et Al HPMC Karbopol 2%kristinedp92Оценок пока нет
- Mukoadesif Timolol2Документ6 страницMukoadesif Timolol2Isma UddinОценок пока нет
- Design and Evaluation of Buccal Patches Containing Combination of Hydrochlorothiazide and AtenololДокумент8 страницDesign and Evaluation of Buccal Patches Containing Combination of Hydrochlorothiazide and Atenololshamma shahulhameedОценок пока нет
- Methods of Formulation and Evaluation of BDDS: Presented ToДокумент40 страницMethods of Formulation and Evaluation of BDDS: Presented ToAkhilesh M SОценок пока нет
- Formulation, Evaluation, and Comparison of Bilayered and Multilayered Mucoadhesive Buccal Devices of Propranolol HydrochlorideДокумент8 страницFormulation, Evaluation, and Comparison of Bilayered and Multilayered Mucoadhesive Buccal Devices of Propranolol HydrochlorideNarendra BhupatiОценок пока нет
- Captopril FloatingДокумент6 страницCaptopril FloatingMira TjakkuduОценок пока нет
- 2017 PLA-PVP Membranes Produced by Solution Blow SpinningpdfДокумент9 страниц2017 PLA-PVP Membranes Produced by Solution Blow SpinningpdfEliton Medeiros Candido de MacêdoОценок пока нет
- Development and Evaluation of Poloxamer Based Nanogel of Rutin by Using Simplex-Lattice Mixture DesignДокумент9 страницDevelopment and Evaluation of Poloxamer Based Nanogel of Rutin by Using Simplex-Lattice Mixture DesignRAPPORTS DE PHARMACIEОценок пока нет
- Ijpras 2018 7 1 33 40 PDFДокумент8 страницIjpras 2018 7 1 33 40 PDFAmina AhmadyОценок пока нет
- ISSN: 0975-766X Available Online Through Development of Mucoadhesive Films For Buccal Administration of MontelukastДокумент15 страницISSN: 0975-766X Available Online Through Development of Mucoadhesive Films For Buccal Administration of MontelukastrahatulislamОценок пока нет
- 2008 Article 730152Документ10 страниц2008 Article 730152Mari Fei LagmayОценок пока нет
- Ijapr: S.RamkanthДокумент10 страницIjapr: S.RamkanthRahmat RizaldiОценок пока нет
- International Journal of Current Pharmaceutical ResearchДокумент4 страницыInternational Journal of Current Pharmaceutical Researchiin eirkaОценок пока нет
- Formulation and Characterization of Clarithromycin Floating Tablets by Using Various PolymersДокумент11 страницFormulation and Characterization of Clarithromycin Floating Tablets by Using Various PolymersIJAR JOURNALОценок пока нет
- Accepted Manuscript: International Journal of Biological MacromoleculesДокумент40 страницAccepted Manuscript: International Journal of Biological MacromoleculesKhoa DuyОценок пока нет
- HPMC/CMC Based Fast Dissolvable Oral Films of An Anxiolytic: Drug Release and Texture AnalysisДокумент9 страницHPMC/CMC Based Fast Dissolvable Oral Films of An Anxiolytic: Drug Release and Texture Analysisthomas cookОценок пока нет
- 3420 PDFДокумент11 страниц3420 PDFreskyОценок пока нет
- Development and Evaluations of Transdermal Delivery of Selegiline HydrochlorideДокумент14 страницDevelopment and Evaluations of Transdermal Delivery of Selegiline HydrochlorideInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- 1 s2.0 S0928493120334664 MainДокумент15 страниц1 s2.0 S0928493120334664 MainAnggun NurhidayahОценок пока нет
- Chitosan-Carboxymethylcellulose BasedДокумент7 страницChitosan-Carboxymethylcellulose BasedRaghav MehraОценок пока нет
- Influence of The Changed USP Specifications On Disintegration Test PerformanceДокумент5 страницInfluence of The Changed USP Specifications On Disintegration Test Performancelejla7Оценок пока нет
- Recovery of Protein & Microbial Cells Using Adsorptive Bubble Separation TechniqueДокумент9 страницRecovery of Protein & Microbial Cells Using Adsorptive Bubble Separation Techniqueromita duttaОценок пока нет
- Agnihotri 2004Документ15 страницAgnihotri 2004Abdul QadirОценок пока нет
- Admin Articles Formulation and Evaluation of Hydroxy Propyl Methyl Cellulose Transdermal Drug Delivery SystemsДокумент4 страницыAdmin Articles Formulation and Evaluation of Hydroxy Propyl Methyl Cellulose Transdermal Drug Delivery SystemsKristine Dwi PuspitasariОценок пока нет
- Formulationandin vitroEvaluationofBuccalTabletsofPiroxicam PDFДокумент11 страницFormulationandin vitroEvaluationofBuccalTabletsofPiroxicam PDFFransisca Cornelia PutriОценок пока нет
- 6 Vol. 8 Issue 1 January 2017 IJPSR RA 6983Документ10 страниц6 Vol. 8 Issue 1 January 2017 IJPSR RA 6983vinayОценок пока нет
- Comparative Investigations On Different PolymersДокумент7 страницComparative Investigations On Different PolymersKhoa DuyОценок пока нет
- Formulation and Evaluation of in Situ Gels Containing Clotrimazole For Oral CandidiasisДокумент7 страницFormulation and Evaluation of in Situ Gels Containing Clotrimazole For Oral CandidiasisAndika DikaОценок пока нет
- Formulation and Invitro Characterisation of Mucoadhesive Microspheres of Oseltamivir by Ionic Gelation MethodДокумент12 страницFormulation and Invitro Characterisation of Mucoadhesive Microspheres of Oseltamivir by Ionic Gelation MethodSriram NagarajanОценок пока нет
- International Journal of Pharma and Bio Sciences V1 (2) 2010Документ10 страницInternational Journal of Pharma and Bio Sciences V1 (2) 2010Richard MoralesОценок пока нет
- Floating FilmДокумент13 страницFloating Filmchittam suvarnaОценок пока нет
- Continuous Fluidized Bed Drying: Residence Time Distribution Characterization and Effluent Moisture Content PredictionДокумент13 страницContinuous Fluidized Bed Drying: Residence Time Distribution Characterization and Effluent Moisture Content PredictionKelvin WahyudiОценок пока нет
- Chitosan and Guar Gum Composite FilmДокумент5 страницChitosan and Guar Gum Composite FilmMutiara Putri Utami SusantoОценок пока нет
- Pharmaceutical Characterization of Amoxicillin Trihydrate As Mucoadhesive Microspheres in Management of H. PyloriДокумент11 страницPharmaceutical Characterization of Amoxicillin Trihydrate As Mucoadhesive Microspheres in Management of H. PyloriYuda ArifОценок пока нет
- Effect of Isopropyl Myristate On The ViscoelasticiДокумент6 страницEffect of Isopropyl Myristate On The ViscoelasticiNofi Lutfiah SfaОценок пока нет
- Research Article Mucoadhesive Microspheres For Gastroretentive Delivery of Acyclovir: in Vitro and in Vivo EvaluationДокумент9 страницResearch Article Mucoadhesive Microspheres For Gastroretentive Delivery of Acyclovir: in Vitro and in Vivo EvaluationmarinasiraitОценок пока нет
- ProposalДокумент8 страницProposalNouran ElbadawiОценок пока нет
- Preparation and Evaluation of Buccal Drug Delivery SystemДокумент2 страницыPreparation and Evaluation of Buccal Drug Delivery SystemKeerthi KomaragiriОценок пока нет
- Design and Evaluation of Transdermal Patches of Olmesartan MedoxomilДокумент9 страницDesign and Evaluation of Transdermal Patches of Olmesartan MedoxomilmasrorohОценок пока нет
- Shivanand 1998Документ14 страницShivanand 1998handikajati kusumaОценок пока нет
- Preparation and Evaluation of Ofloxacin Loaded Polymer Composite Film For Wound Healing ActivityДокумент9 страницPreparation and Evaluation of Ofloxacin Loaded Polymer Composite Film For Wound Healing ActivitydattusinghsОценок пока нет
- 2016 Bonan Et Al PLApdfpdfДокумент11 страниц2016 Bonan Et Al PLApdfpdfEliton Medeiros Candido de MacêdoОценок пока нет
- Review of Related LiteratureДокумент11 страницReview of Related Literaturekyle javierОценок пока нет
- International Journal of Pharma and Bio Sciences V1 (2) 2010Документ14 страницInternational Journal of Pharma and Bio Sciences V1 (2) 2010Ka KaaОценок пока нет
- Tds 4Документ4 страницыTds 4Neha YadavОценок пока нет
- Advance in The Applications of Konjac Glucomannan and Its DerivativesДокумент5 страницAdvance in The Applications of Konjac Glucomannan and Its DerivativesLoo Chong SianОценок пока нет
- Research ArticleДокумент8 страницResearch ArticleGabriela SolanoОценок пока нет
- John 2013Документ5 страницJohn 2013Fhyrdha Slaluw ZetiaaОценок пока нет
- Ketoprofen-Carboxymethyl Chitosan Microparticles Prepared by Spray Drying: Optimization and EvaluationДокумент3 страницыKetoprofen-Carboxymethyl Chitosan Microparticles Prepared by Spray Drying: Optimization and EvaluationAgusОценок пока нет
- International Journal of Current Pharmaceutical ResearchДокумент5 страницInternational Journal of Current Pharmaceutical ResearchImranОценок пока нет
- International Research Journal of PharmacyДокумент5 страницInternational Research Journal of PharmacycristinaviiuОценок пока нет
- Development and Characterization of Transdermal Patch For Controlled Release of Fluocinolone AcetonideДокумент12 страницDevelopment and Characterization of Transdermal Patch For Controlled Release of Fluocinolone AcetonideJOURNAL CLUB FOR PHARMACEUTICAL SCIENCES (JCPS)Оценок пока нет
- Kubo Et Al. - 2010 - Three-Year Clinical Evaluation of A Flowable and A Hybrid Resin Composite in Non-Carious Cervical LesionsДокумент10 страницKubo Et Al. - 2010 - Three-Year Clinical Evaluation of A Flowable and A Hybrid Resin Composite in Non-Carious Cervical Lesionsjanvier_89Оценок пока нет
- Research Journal of Pharmaceutical, Biological and Chemical SciencesДокумент14 страницResearch Journal of Pharmaceutical, Biological and Chemical SciencesArinta Purwi SuhartiОценок пока нет
- JDDR 127 PDFДокумент23 страницыJDDR 127 PDFEarthjournal PublisherОценок пока нет
- Article in Press: International Journal of Biological MacromoleculesДокумент10 страницArticle in Press: International Journal of Biological MacromoleculesFatoş Kabak ÖzçelikОценок пока нет
- FTS SemisolidaДокумент11 страницFTS SemisolidaEdi SaputraОценок пока нет
- TramadolДокумент8 страницTramadolAlinaDianaОценок пока нет
- LC-MS 1Документ7 страницLC-MS 1AlinaDianaОценок пока нет
- Determination of Enalapril Maleate From Tablets Using A New HPLC MethodДокумент6 страницDetermination of Enalapril Maleate From Tablets Using A New HPLC MethodAlinaDianaОценок пока нет
- Codul Divin Al VietiiДокумент94 страницыCodul Divin Al VietiiAlinaDianaОценок пока нет
- Development and Validation of A Method For Quantitative Determination of Amiodarone Hydrochloride in Blood Serum by HPLC-MS-MДокумент6 страницDevelopment and Validation of A Method For Quantitative Determination of Amiodarone Hydrochloride in Blood Serum by HPLC-MS-MAlinaDianaОценок пока нет
- Antiinflammatory Activity of An N, N'-DisalicylidenemethylendiamineДокумент4 страницыAntiinflammatory Activity of An N, N'-DisalicylidenemethylendiamineAlinaDianaОценок пока нет
- A New High Performance Liquid Chromatographic Analysis Method For CiprofloxacinДокумент4 страницыA New High Performance Liquid Chromatographic Analysis Method For CiprofloxacinAlinaDianaОценок пока нет
- A HPLC Method For The Determination of Bisoprolol in Tablets and Its Application To A Bioequivalence StudyДокумент5 страницA HPLC Method For The Determination of Bisoprolol in Tablets and Its Application To A Bioequivalence StudyAlinaDianaОценок пока нет
- Validation of A New Spectrophotometric Method For The Assay of Bisoprolol FumarateДокумент4 страницыValidation of A New Spectrophotometric Method For The Assay of Bisoprolol FumarateAlinaDianaОценок пока нет
- Study of Physico-Chemical Characteristics and Pharmacological Effects of 1-Ethyl-Salicyldene-bis-Ethylene - Diamine and Its Complex With MN (II)Документ4 страницыStudy of Physico-Chemical Characteristics and Pharmacological Effects of 1-Ethyl-Salicyldene-bis-Ethylene - Diamine and Its Complex With MN (II)AlinaDianaОценок пока нет
- In Vitro Characterization of Polyvinyl Alcohol/ Chitosan Hydrogels As Modified Release Systems For BisoprololДокумент5 страницIn Vitro Characterization of Polyvinyl Alcohol/ Chitosan Hydrogels As Modified Release Systems For BisoprololAlinaDianaОценок пока нет
- Fast HPLC Method For The Determination of Piroxicam and Its Application To Stability StudyДокумент6 страницFast HPLC Method For The Determination of Piroxicam and Its Application To Stability StudyAlinaDianaОценок пока нет
- Molecular Networking As A Drug Discovery, Drug Metabolism, and Precision Medicine StrategyДокумент12 страницMolecular Networking As A Drug Discovery, Drug Metabolism, and Precision Medicine StrategySam SonОценок пока нет
- Analgesic Agents: Maya Ganda Ratna Department of Pharmacology and Pharmacy Faculty of Medicine - Lampung UniversityДокумент46 страницAnalgesic Agents: Maya Ganda Ratna Department of Pharmacology and Pharmacy Faculty of Medicine - Lampung UniversityMuhammad GilangОценок пока нет
- Lioresal: (Baclofen)Документ11 страницLioresal: (Baclofen)ddandan_2Оценок пока нет
- Patente Info FenilefrinaДокумент14 страницPatente Info Fenilefrinadesarrollo farma19Оценок пока нет
- Consumos Medicamentos 2020Документ568 страницConsumos Medicamentos 2020LUCERO LOPEZОценок пока нет
- The Significance of Acid:base Properties in Drug DiscoveryДокумент12 страницThe Significance of Acid:base Properties in Drug DiscoveryBen ZoeОценок пока нет
- Richard Gerster: 19-Ganesh Kale 29-Sachin Naik 39-Amol Patel 49 - Vivek SargaonkarДокумент21 страницаRichard Gerster: 19-Ganesh Kale 29-Sachin Naik 39-Amol Patel 49 - Vivek SargaonkarSachin NaikОценок пока нет
- HistaminicsДокумент3 страницыHistaminicsgentianbreguОценок пока нет
- Imbong V Hon. Ochoa, Jr. GR NO. 204819 APRIL 8, 2014 FactsДокумент8 страницImbong V Hon. Ochoa, Jr. GR NO. 204819 APRIL 8, 2014 FactsJack NumosОценок пока нет
- 10 Herbal Medicine-DohДокумент5 страниц10 Herbal Medicine-DohJuna RoallosОценок пока нет
- Mapeh 6: Quarter 4 - Module 1Документ10 страницMapeh 6: Quarter 4 - Module 1ALEX CORPORALОценок пока нет
- Antipsychotic Treatment A Systematic Literature Review and Meta Analysis of Qualitative StudiesДокумент12 страницAntipsychotic Treatment A Systematic Literature Review and Meta Analysis of Qualitative StudiesmafeОценок пока нет
- Naskah Roleplay Bahasa InggrisДокумент6 страницNaskah Roleplay Bahasa InggrisIlhamОценок пока нет
- 050c2d93fc8616 - PMP Catalouge-Jan-2013 PDFДокумент52 страницы050c2d93fc8616 - PMP Catalouge-Jan-2013 PDFUmaima faizОценок пока нет
- En Investors1 Annual Reports 2002-03 Dabur MDA 02 03Документ13 страницEn Investors1 Annual Reports 2002-03 Dabur MDA 02 03mishra_shashishekhar97Оценок пока нет
- Peter Goadsby - Treatment of Cluster Headache PDFДокумент3 страницыPeter Goadsby - Treatment of Cluster Headache PDFharunОценок пока нет
- Cilinary Set UpДокумент32 страницыCilinary Set UpOla Kareem100% (1)
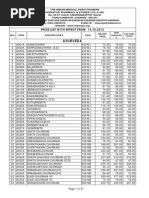
- Price List From 14.10.2013Документ27 страницPrice List From 14.10.2013jasoneinsteinОценок пока нет
- Oxoferin Ward PPT UPDATEDДокумент27 страницOxoferin Ward PPT UPDATEDdrusmanjamilhcmdОценок пока нет
- SuspensionsДокумент20 страницSuspensionsK3nsh1nXОценок пока нет
- GDHHДокумент40 страницGDHHnaelarizqiОценок пока нет
- Ayurvedic Medicines PDFДокумент24 страницыAyurvedic Medicines PDFRamling PatrakarОценок пока нет
- IV Infusion NumericalsДокумент2 страницыIV Infusion NumericalsYarfa KhurramОценок пока нет
- S&P Pharma Industry Overview - 11252010Документ49 страницS&P Pharma Industry Overview - 11252010earajesh100% (1)
- ACIДокумент4 страницыACISalina HillОценок пока нет
- Daftar Alat-Alat Yang Ada Diruangan Instalasi Gawat Darurat RS Bina Kasih Pekanbaru Lemari High AlertДокумент5 страницDaftar Alat-Alat Yang Ada Diruangan Instalasi Gawat Darurat RS Bina Kasih Pekanbaru Lemari High AlertRiwiyoko YrsОценок пока нет
- Good Dispensing PracticeДокумент59 страницGood Dispensing Practicechalii100% (1)
- Drug StudyДокумент3 страницыDrug StudyatchiekОценок пока нет
- Processing The PrescriptionДокумент66 страницProcessing The PrescriptionRose Ann100% (1)
- D Watson Chemists:: Pakistan German Business ForumДокумент3 страницыD Watson Chemists:: Pakistan German Business ForumareebОценок пока нет
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)От EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Рейтинг: 3 из 5 звезд3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedРейтинг: 4.5 из 5 звезд4.5/5 (82)
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (32)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionОт EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionРейтинг: 4 из 5 звезд4/5 (404)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDОт EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDРейтинг: 5 из 5 звезд5/5 (3)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОт EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОценок пока нет
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsОт EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsРейтинг: 5 из 5 звезд5/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsОт EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsРейтинг: 4 из 5 звезд4/5 (4)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisОт EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisРейтинг: 3.5 из 5 звезд3.5/5 (2)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeРейтинг: 2 из 5 звезд2/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisОт EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisРейтинг: 4.5 из 5 звезд4.5/5 (42)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.От EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Рейтинг: 4.5 из 5 звезд4.5/5 (110)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeОт EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeРейтинг: 4.5 из 5 звезд4.5/5 (254)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsОт EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsРейтинг: 4.5 из 5 звезд4.5/5 (170)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesОт EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesРейтинг: 4.5 из 5 звезд4.5/5 (1412)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaОт EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- To Explain the World: The Discovery of Modern ScienceОт EverandTo Explain the World: The Discovery of Modern ScienceРейтинг: 3.5 из 5 звезд3.5/5 (51)
- The Obesity Code: Unlocking the Secrets of Weight LossОт EverandThe Obesity Code: Unlocking the Secrets of Weight LossРейтинг: 4 из 5 звезд4/5 (6)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryОт EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryРейтинг: 4 из 5 звезд4/5 (46)
- The Marshmallow Test: Mastering Self-ControlОт EverandThe Marshmallow Test: Mastering Self-ControlРейтинг: 4.5 из 5 звезд4.5/5 (60)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessОт EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessРейтинг: 4.5 из 5 звезд4.5/5 (328)
- Why We Die: The New Science of Aging and the Quest for ImmortalityОт EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityРейтинг: 4.5 из 5 звезд4.5/5 (6)
- How to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingОт EverandHow to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingРейтинг: 1 из 5 звезд1/5 (1)