Академический Документы
Профессиональный Документы
Культура Документы
Effect of Fruit Restriction On Glycemic Control in Patients With Type 2 Diabetes - A Randomized Trial
Загружено:
Irfana EfendiОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Effect of Fruit Restriction On Glycemic Control in Patients With Type 2 Diabetes - A Randomized Trial
Загружено:
Irfana EfendiАвторское право:
Доступные форматы
Christensen et al.
Nutrition Journal 2013, 12:29
http://www.nutritionj.com/content/12/1/29
RESEARCH
Open Access
Effect of fruit restriction on glycemic control in
patients with type 2 diabetes a randomized trial
Allan S Christensen1*, Lone Viggers1, Kjeld Hasselstrm2 and Sren Gregersen3
Abstract
Background: Medical nutrition therapy is recognized as an important treatment option in type 2 diabetes. Most
guidelines recommend eating a diet with a high intake of fiber-rich food including fruit. This is based on the many
positive effects of fruit on human health. However some health professionals have concerns that fruit intake has a
negative impact on glycemic control and therefore recommend restricting the fruit intake. We found no studies
addressing this important clinical question. The objective was to investigate whether an advice to reduce the intake
of fruit to patients with type 2 diabetes affects HbA1c, bodyweight, waist circumference and fruit intake.
Methods: This was an open randomized controlled trial with two parallel groups. The primary outcome was a
change in HbA1c during 12 weeks of intervention. Participants were randomized to one of two interventions;
medical nutrition therapy + advice to consume at least two pieces of fruit a day (high-fruit) or medical nutrition
therapy + advice to consume no more than two pieces of fruit a day (low-fruit). All participants had two
consultations with a registered dietitian. Fruit intake was self-reported using 3-day fruit records and dietary recalls.
All assessments were made by the intention to treat principle.
Results: The study population consisted of 63 men and women with newly diagnosed type 2 diabetes. All patients
completed the trial. The high-fruit group increased fruit intake with 125 grams (CI 95%; 78 to 172) and the low-fruit
group reduced intake with 51 grams (CI 95%; -18 to 83). HbA1c decreased in both groups with no difference
between the groups (diff.: 0.19%, CI 95%; -0.23 to 0.62). Both groups reduced body weight and waist circumference,
however there was no difference between the groups.
Conclusions: A recommendation to reduce fruit intake as part of standard medical nutrition therapy in overweight
patients with newly diagnosed type 2 diabetes resulted in eating less fruit. It had however no effect on HbA1c,
weight loss or waist circumference. We recommend that the intake of fruit should not be restricted in patients with
type 2 diabetes.
Trial registration: www.clinicaltrials.gov; Identifier: NCT01010594.
Keywords: Glycemic control, Nutrition counseling, Weight loss, Fruit, Medical nutrition therapy, Type 2 diabetes
Background
The prevalence of type 2 diabetes (T2DM) is still rising
and has reached epidemic proportions in most countries
[1]. It is estimated that around 350 million people
worldwide have T2DM [1]. Individuals with T2DM have
increased morbidity and mortality and represent a huge
economic burden for society. The importance of medical nutrition therapy (MNT) is recognized as one of the
cornerstones in the treatment of T2DM [2-4]. Several
* Correspondence: allan.christensen@vest.rm.dk
1
Department of Nutrition, Regional Hospital West Jutland, Jutland, Denmark
Full list of author information is available at the end of the article
evidence-based nutrition guidelines have been published
and show that both diet quality and quantity have a huge
impact on T2DM [3-5]. A variety of fibre-rich food like
fruit and vegetables are generally recommended [4,5].
Fruit contain a wide range of specific bioactive substances which can act through multiple pathways in the
human body e.g. as antioxidants, reduce inflammation
and improve endothelial function [6-8]. High fruit intake
has been shown to reduce the risk of e.g. cardiovascular
disease [9,10] and some cancer types [11].
Health professionals often have concerns about the
sugar content of fruit and therefore advice individuals
2013 Christensen et al.; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the
Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use,
distribution, and reproduction in any medium, provided the original work is properly cited.
Christensen et al. Nutrition Journal 2013, 12:29
http://www.nutritionj.com/content/12/1/29
with T2DM to restrict their intake to a maximum of two
pieces a day. Few studies have addressed whether high
fruit intake is associated with glycemic control and these
have shown either no association [12-15] or an inverse
association [16] between fruit intake and either HbA1c
or blood glucose. However, these are all observational
studies and none are performed in subjects with T2DM.
Therefore sparse data exist to answer the question
whether or not fruit has a negative impact on blood glucose levels in subjects with T2DM. We carried out this
study to test the hypothesis that an advice to restrict
fruit intake to a maximum of two pieces a day compared
to at least two pieces a day results in an improved glycemic control in adults with type 2 diabetes.
Methods
Subjects
Volunteers were selected from patients referred to MNT
by their GP to the Outpatient Clinic at Department of
Nutrition, Regional Hospital West Jutland. Eligible patients were adults with T2DM (duration of T2DM < 12
months), HbA1c values 12.0% or less and who accepted
to adhere to the protocol. Exclusion criteria were clinically significant cardiovascular, renal or endocrine disease.
A total of 136 subjects were invited and 63 subjects were
randomized. Each subject gave informed, written consent and the study was approved by The Regional Committee on Biomedical Research Ethics.
Study design
This study was a 12 week open randomized parallel diet
intervention trial. Sequentially numbered, sealed envelopes containing a computer-generated allocation were
used. The intervention consisted of standard MNT and
an advice to either: 1) Eat at least two pieces of fruit
each day (high-fruit) or 2) eat no more than two pieces
of fruit each day (low-fruit). Both groups had two consultations with an experienced registered dietitian at the
Outpatient Clinic. One consultation in the beginning
and one at the end of the study period. Shortly before
consultations in the Outpatient Clinic the subjects had a
blood sample drawn at their GP. During the intervention
subjects were treated at the GPs discretion. The primary outcome was change in HbA1c. Secondary outcomes were changes in fruit intake, body weight and
waist circumference.
Nutritional intervention
The MNT was given on an individual basis and focused
on the individual needs and personal preferences [3]. All
overweight subjects were advised to restrict the energy
intake. The only difference in the MNT between the
groups was the advice concerning fruit intake. The patients were recommended to eat fresh and whole fruit
Page 2 of 6
only and to exclude fruit juice, canned and dried fruit
from their diet or keep it as low as possible. One piece
of fruit was standardized to the amount of a fruit that
contained approximately 10 grams of carbohydrate e.g.
100 grams apple, 50 grams banana or 125 grams orange.
The patients were given written information and pictures about the amount of the most common fruit that
corresponded to one piece.
Anthropometry measurements
Height was measured at the first visit only. Body weight
and waist circumference were measured at both visits.
Subjects were weighed barefooted and in light clothing
on a calibrated scale. Height was measured using a wall
measuring stick scale. Waist circumference was measured horizontally at the level of the umbilicus in a relaxed standing position.
Biochemical analysis
Blood samples were taken at the subjects GP using
standard procedures. The blood samples were analyzed
at Department of Clinical Biochemistry, Regional Hospital West Jutland using standard laboratory procedures.
HbA1c was analyzed using HPLC.
Fruit intake
The subjects filled in a weighed 3-day fruit record before
and after the intervention. At each visit the fruit intake
was estimated using dietary recalls. Portion sizes were
estimated and translated to grams using pictures and
table values of mean weight for a given standard portion
[17,18]. This was compared with the fruit record to
avoid errors. Fruit intake was calculated at each visit as
mean intake using the 3-day fruit record.
Physical activity
A self-reported questionnaire was used at each visit to
estimate physical activity level [19].
Statistical analysis
Statistical analysis was performed using Stata statistical
software package 11.1 (Stata, College Station, TX, USA).
All analyses were performed on an intention-to-treat
basis, with a two-sided 0.05 significance level (=0.05).
We used paired t-test to analyze if a variable changed
significantly from before to after the intervention. For
each outcome we compared mean difference (after - before)
between the two groups using an unpaired t-test. For the
primary outcome we also used multiple regression analysis
controlling for potential confounders. Results are given as
mean standard error unless otherwise stated.
A sample of 38 subjects in each arm was estimated to
detect a difference of 0.7% in HbA1c. The sample size was
based on achieving an 80% power with = 0.05, SD = 1.0
Christensen et al. Nutrition Journal 2013, 12:29
http://www.nutritionj.com/content/12/1/29
and dropout = 10%. The inclusion rate was slower than
anticipated. The study was terminated prematurely due to
limited time and research funding. Fortunately, the variation in HbA1c was smaller than estimated in the power
calculation and there were no dropouts. Therefore the
actual power in the study was around 90% to detect a difference of 0.7% in HbA1c between the groups.
Results
Page 3 of 6
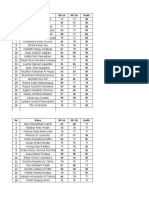
Table 1 Baseline characteristics of study participants*
Age (years)
High-fruit
Low-fruit
(n = 32)
(n = 31)
59 12
57 12
Sex (female)
14 (44)
18 (58)
Height (cm)
170 8
169 10
Body weight (kg)
92 17
91 17
32 5
32 6
BMI (kg/m2)
Baseline characteristics
Waist circumference (cm)
104 11
107 9
Recruitment took place from November 2009 to March
2011 with the last visit in June 2011. In total 63 T2DM
subjects were included. Baseline characteristics are shown
in Table 1. At baseline significantly more subjects were
taking oral antidiabetic drugs (OADs) on the high-fruit
diet than on the low-fruit diet (22 vs 12; p=0.02). There
were no significant differences between the groups for any
of the other baseline variables.
HbA1c (%)
6.7 1.2
6.5 1.1
Compliance to intervention
Based on the fruit records and recalls, the reported fruit
intake was altered as expected (Table 2). One subject on
the high-fruit diet kept the fruit intake steady just below
two pieces a day. The outcomes were unaffected by exclusion of this non-compliant subject.
HbA1c
As expected, there was a significant reduction in HbA1c
in both groups. The high-fruit group had a change from
6.74 0.2 to 6.26 0.1% and the low-fruit group a
change from 6.53 0.2 to 6.24 0.1%. The reductions
were 0.49 0.2 and 0.29 0.1% in the high-fruit and
low-fruit diet respectively. There was no significant
difference between the groups (Table 3). Adjusting for
use of OAD at baseline did not significantly change the
result (Table 3). Five subjects (high-fruit = 2; low-fruit = 3)
increased OAD dosage during the study period. They had
a significantly higher HbA1c at baseline and reduced their
HbA1c significantly more during the study (Figure 1).
Weight and waist circumference
Both groups had a significant reduction in body weight
and waist circumference with no differences between
groups (Table 2). The reductions in body weight were
2.5 0.5 and 1.7 0.5 kg in the high-fruit and low-fruit
diet respectively. In waist circumference the reductions
were 4.3 0.6 and 3.0 0.6 cm in the high-fruit and
low-fruit group, respectively. Neither change in body
weight (r=0.07, p=0.61; r=0.17, p=0.19) nor in waist circumference (r=0.15, p=0.31; r=0.13, p=0.36) was associated with change in fruit intake or change in HbA1c
respectively.
Physical activity level (PAL)
1.7 0,1
1.6 0,1
Fruit intake (g)
194 87
186 82
22 (12107)
33 (1454)
Duration of diabetes (days)
Start on OAD prior to intervention
1-30 days
10 (45)
7 (58)
31-60 days
6 (27)
3 (25)
> 60 days
6 (27)
2 (17)
*Baseline values are presented as mean SD, median (25th-75th centile), and
number (%). OAD = oral antidiabetic drugs.
Physical activity
A significant change in physical activity was seen in the
high-fruit group (0.07 0.02 PAL; p=0.005) but not in the
low-fruit group (0.04 0.03 PAL; p=0.19). However, there
was no difference between the groups (0.04 PAL; p=0.31).
Side effects
One subject on the high-fruit diet, who increased fruit
intake from 145 to 310 grams, reported mild gastrointestinal side effects, but the subject remained compliant
throughout the study.
Discussion
Our pragmatic trial demonstrated that, in adults with
newly diagnosed T2DM, MNT with an advice to restrict
fruit intake resulted in a decreased fruit intake while
MNT with an advice to eat more fruit resulted in an increased fruit intake. However this difference in fruit intake
did not significantly affect glycemic control, body weight
or waist circumference.
To our knowledge, this is the first randomized intervention study examining the effects of dietary advice to
restrict fruit intake on glycemic control in T2DM. Most
intervention studies with fruit have investigated fruit as
a part of a whole diet, fruit mixed with vegetables
or only one type of fruit and often as a single meal study
e.g. glycemic index studies. Very few intervention studies
have tested a variety of fruit over several weeks and none
have investigated long-term glycemic control in T2DM
subjects.
In our study we found that restriction of fruit intake
does not significantly affect HbA1c. In a study by
Christensen et al. Nutrition Journal 2013, 12:29
http://www.nutritionj.com/content/12/1/29
Page 4 of 6
Table 2 Body weight, waist circumference and fruit intake before and after intervention
High-fruit
Body weight (kg)
Low-fruit
Differences between groups
Before
After
Before
After
Means (CI 95%)
p-value
92.4 2.9
89.9 3.0*
91.2 3.0
89.6 2.9*
0.9 (2.2 to 0.4)
0.18
Waist circumference (cm)
103 2
99 2*
107 2
103 2*
1.2 (3.0 to 0.5)
0.17
Fruit intake (grams)
194 15
319 24*
186 15
135 7*
175 (119 to 232)
< 0.0001
* Significant difference between before and after.
Body weight: high-fruit (n = 32), low-fruit (n = 31), waist circumference: high-fruit (n = 27), low-fruit (n = 22), fruit intake: high-fruit (n = 32), low-fruit (n = 31).
Rodriguez et al. 15 obese women randomized to either a
low-fruit or a high-fruit diet for 8 weeks a difference between the groups of 550 kJ from fructose was obtained
[20]. This is around twice the difference obtained in the
present study. The study reported no differences in
HOMA, glucose or insulin levels between the groups. In
another study by Madero et al. 131 obese subjects were
randomized to a low-fructose diet or a moderate-naturalfructose diet for 6 weeks [21]. The groups intake of fruit
corresponded to approximately 250 and 2200 kJ, respectively in low-fructose and moderate-natural-fructose which
corresponds to a difference between the groups about
three times as large as in the present study. Significant reductions in HOMA and glucose values were seen within
the moderate-natural-fructose group, but no difference
between the groups was seen. Cross-sectional studies have
shown that fruit intake is not associated [12-15] or inversely associated [16] with HbA1c or other parameters
reflecting glycemic control. Further, cohort studies addressing the impact of fruit intake on the incidence of
T2DM have shown either no association or an inverse association [22,23]. The evidence, including our present
study, therefore suggests that a high fruit intake does not
have a negative impact on glycemic control.
We found a tendency towards reduced body weight
and waist circumference in the group that ingested most
fruit 0.9 (CI 95%; 0.4 to 2.2) kg and 1.2 (CI 95%; 0.5
to 3.0) cm respectively. This corroborates with a few
intervention studies. The study by Rodriguez et al. in
which the high-fruit group had a significant reduction in
waist circumference compared to low-fruit group (5.5 vs.
2.4 cm; p=0.048) [20]. Weight loss was similar in the
two groups (6.1 vs. 6.4 kg; p=0.78). In another intervention study 49 obese women were randomized to add either three apples, three pears or three oat cookies to
their usual diet for 10 weeks [24]. The total energy and
fiber content of the supplements were matched. The two
groups with fruit supplements lost significantly more body
weight than the group with oat cookies (0.9 vs 0.8 vs
0.2 kg). In a third study by Madero et al. the moderatenatural-fructose group reduced body weight more than
the low-fructose group (4.1 vs 2.9 kg; p=0.02) [21]. A recent review study concluded that in most studies a higher
fruit intake has a beneficial effect on body weight and that
no studies have found a negative effect [25].
In spite of a difference in fruit intake of about two
pieces daily between the groups we did not find any effect on HbA1c, body weight or waist circumference. The
most likely explanation is that fruit is eaten as a part of
a daily diet and therefore when changing the fruit intake
it will lead to other changes in the diet. We did not
measure total energy intake, but weight and physical activity were similar between the groups and therefore energy intake must have been more or less the same in
both groups too. When changing the fruit intake other
changes in the diet most likely occur and this would explain that there was no difference in HbA1c, body weight
and waist circumference despite the significant difference in fruit intake.
Table 3 Mean difference between the groups in HbA1c (%)
Difference*
CI 95%
p-value
Unadjusted
0.19
0.23 to 0.62
0.37
Adjusted for baseline OAD
0.06
0.38 to 0.49
0.80
* Difference between the diets (high-fruit (n = 32) low-fruit (n = 31))
analyzed by multiple regression. OAD = oral antidiabetic drugs.
Figure 1 HbA1c values before and after intervention by groups.
Each thin line represents one subject. Thick line represents
mean change.
Christensen et al. Nutrition Journal 2013, 12:29
http://www.nutritionj.com/content/12/1/29
Our study has several strengths. It is the first randomized controlled study investigating the relevant scientific
question: does fruit intake matter in relation to glycemic
control in T2DM subjects? We chose to do this in a
real life setting. Thus, almost all subjects were fully
compliant and there were no drop-outs.
However, our study also has some weaknesses. First, it
can be argued that a greater difference in fruit intake between the high and low fruit groups would have resulted
in a significant effect, positive or negative. However, we
consider a difference of about two pieces of fruit as clinically relevant and we think it reflects a real life situation. We admit that testing whether an even higher
fruit intake may impact significantly the glycemic control would be interesting, but this was not the intention
in this pragmatic trial. Secondly, we did not control (and
had no pre-trial intention to do so) the intake of medication. A difference in baseline use of OADs could bias
the results. However, adjustments did not significantly
change the results (Table 3). Therefore we do not believe
it has biased the results. Thirdly, fruit intake and physical activity were self-reported and therefore could have
been subject to under or over-reporting. Measurement
of biomarkers of fruit intake, e.g. plasma vitamin C and
plasma carotenoids would have strengthened the study.
Conclusions
We conclude that an advice to restrict fruit intake as part
of standard MNT in overweight adults with newly diagnosed TDM2 does not improve glycemic control, body
weight or waist circumference. Considering the many possible beneficial effects of fruit, we recommend that fruit
intake should not be restricted in T2DM subjects.
Page 5 of 6
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
Competing interests
The authors declare that they have no competing interests.
16.
Authors' contributions
All authors were involved in the development of the study protocol. ASC
performed subject recruitment, data collection and was responsible for the
day-to-day running of the study. ASC and SG performed statistical analysis
and drafted the final version of the manuscript. All authors approved and
read the final manuscript.
Author details
1
Department of Nutrition, Regional Hospital West Jutland, Jutland, Denmark.
2
Medical Department, Regional Hospital West Jutland, Jutland, Denmark.
3
Department of Endocrinology and Metabolism, Aarhus University Hospital,
Aarhus, Denmark.
Received: 4 September 2012 Accepted: 27 February 2013
Published: 5 March 2013
References
1. Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, Lin JK,
Farzadfar F, Khang YH, Stevens GA, Rao M, Ali MK, Riley LM, Robinson CA,
Ezzati M: National, regional, and global trends in fasting plasma glucose
and diabetes prevalence since 1980: systematic analysis of health
examination surveys and epidemiological studies with 370 country-years
and 2.7 million participants. Lancet 2011, 378:3140.
17.
18.
19.
20.
21.
22.
Morris SF, Wylie-Rosett J: Medical Nutrition Therapy: A Key to Diabetes
Management and Prevention. Clinical diabetes 2010, 28:1218.
Franz MJ, Powers MA, Leontos C, Holzmeister LA, Kulkarni K, Monk A,
Wedel N, Gradwell E: The evidence for medical nutrition therapy for
type 1 and type 2 diabetes in adults. J Am Diet Assoc 2010,
110:18521889.
Bantle JP, Wylie-Rosett J, Albright AL, Apovian CM, Clark NG, Franz MJ,
Hoogwerf BJ, Lichtenstein AH, Mayer-Davis E, Mooradian AD, Wheeler ML:
Nutrition recommendations and interventions for diabetes: a position
statement of the American Diabetes Association. Diabetes Care 2008,
31(Suppl 1):S6178.
Mann JI, De Leeuw I, Hermansen K, Karamanos B, Karlstrom B, Katsilambros N,
Riccardi G, Rivellese AA, Rizkalla S, Slama G, Toeller M, Uusitupa M, Vessby B:
Evidence-based nutritional approaches to the treatment and prevention of
diabetes mellitus. Nutr Metab Cardiovasc Dis 2004, 14:373394.
Gonzalez-Gallego J, Garcia-Mediavilla MV, Sanchez-Campos S, Tunon MJ: Fruit
polyphenols, immunity and inflammation. Br J Nutr 2010, 104(Suppl 3):S1527.
Chong MF, Macdonald R, Lovegrove JA: Fruit polyphenols and CVD
risk: a review of human intervention studies. Br J Nutr 2010,
104(Suppl 3):S2839.
Feeney MJ: Fruits and the prevention of lifestyle-related diseases. Clin Exp
Pharmacol Physiol 2004, 31(Suppl 2):S1113.
Dauchet L, Amouyel P, Hercberg S, Dallongeville J: Fruit and vegetable
consumption and risk of coronary heart disease: a meta-analysis of
cohort studies. J Nutr 2006, 136:25882593.
Martinez-Gonzalez MA, Lamuela-Raventos RM: The unparalleled benefits of
fruit. Br J Nutr 2009, 102:947948.
Aune D, Lau R, Chan DS, Vieira R, Greenwood DC, Kampman E, Norat T:
Nonlinear reduction in risk for colorectal cancer by fruit and vegetable
intake based on meta-analysis of prospective studies. Gastroenterology
2011, 141:106118.
Overby NC, Margeirsdottir HD, Brunborg C, Andersen LF, Dahl-Jorgensen K:
The influence of dietary intake and meal pattern on blood glucose
control in children and adolescents using intensive insulin treatment.
Diabetologia 2007, 50:20442051.
Gulliford MC, Ukoumunne OC: Determinants of glycated haemoglobin in
the general population: associations with diet, alcohol and cigarette
smoking. Eur J Clin Nutr 2001, 55:615623.
Buyken AE, Toeller M, Heitkamp G, Irsigler K, Holler C, Santeusanio F, Stehle
P, Fuller JH: Carbohydrate sources and glycaemic control in Type 1
diabetes mellitus. EURODIAB IDDM Complications Study Group. Diabet
Med 2000, 17:351359.
Panagiotakos DB, Tzima N, Pitsavos C, Chrysohoou C, Papakonstantinou E,
Zampelas A, Stefanadis C: The relationship between dietary habits,
blood glucose and insulin levels among people without cardiovascular
disease and type 2 diabetes; the ATTICA study. Rev Diabet Stud 2005,
2:208215.
Sargeant LA, Khaw KT, Bingham S, Day NE, Luben RN, Oakes S, Welch A,
Wareham NJ: Fruit and vegetable intake and population glycosylated
haemoglobin levels: the EPIC-Norfolk Study. Eur J Clin Nutr 2001,
55:342348.
Andersen LT, Jensen H, Haraldsdottir J: Typiske vgte for madvarer. Scand
J Nutr 1996, 40:S129152.
The Danish Diabetes Association: Sund mad - nr du har diabetes. Odense;
2001.
Johansson G, Westerterp KR: Assessment of the physical activity level with
two questions: validation with doubly labeled water. Int J Obes (Lond)
2008, 32:10311033.
Rodriguez MC, Parra MD, Marques-Lopes I, De Morentin BE, Gonzalez A,
Martinez JA: Effects of two energy-restricted diets containing different
fruit amounts on body weight loss and macronutrient oxidation. Plant
Foods Hum Nutr 2005, 60:219224.
Madero M, Arriaga JC, Jalal D, Rivard C, McFann K, Perez-Mendez O, Vazquez
A, Ruiz A, Lanaspa MA, Jimenez CR, Johnson RJ, Lozada LG: The effect of
two energy-restricted diets, a low-fructose diet versus a moderate
natural fructose diet, on weight loss and metabolic syndrome
parameters: a randomized controlled trial. Metabolism 2011,
60:15511559.
Carter P, Gray LJ, Troughton J, Khunti K, Davies MJ: Fruit and vegetable
intake and incidence of type 2 diabetes mellitus: systematic review and
meta-analysis. BMJ 2010, 341:c4229.
Christensen et al. Nutrition Journal 2013, 12:29
http://www.nutritionj.com/content/12/1/29
Page 6 of 6
23. Hamer M, Chida Y: Intake of fruit, vegetables, and antioxidants and risk of
type 2 diabetes: systematic review and meta-analysis. J Hypertens 2007,
25:23612369.
24. de Oliveira MC, Sichieri R, Venturim Mozzer R: A low-energy-dense diet
adding fruit reduces weight and energy intake in women. Appetite 2008,
51:291295.
25. Alinia S, Hels O, Tetens I: The potential association between fruit intake
and body weighta review. Obes Rev 2009, 10:639647.
doi:10.1186/1475-2891-12-29
Cite this article as: Christensen et al.: Effect of fruit restriction on glycemic
control in patients with type 2 diabetes a randomized trial. Nutrition
Journal 2013 12:29.
Submit your next manuscript to BioMed Central
and take full advantage of:
Convenient online submission
Thorough peer review
No space constraints or color gure charges
Immediate publication on acceptance
Inclusion in PubMed, CAS, Scopus and Google Scholar
Research which is freely available for redistribution
Submit your manuscript at
www.biomedcentral.com/submit
Вам также может понравиться
- Effects of Diet and Simvastatin On Serum Lipids, Insulin, and Antioxidants in Hypercholesterolemic MenДокумент8 страницEffects of Diet and Simvastatin On Serum Lipids, Insulin, and Antioxidants in Hypercholesterolemic MenAranel BomОценок пока нет
- Research: Cite This As: BMJ 2010 341:c3337Документ7 страницResearch: Cite This As: BMJ 2010 341:c3337Deepak DahiyaОценок пока нет
- Research Article Perceived Stress and Adherence To The Dietary Recommendations and Blood Glucose Levels in Type 1 DiabetesДокумент8 страницResearch Article Perceived Stress and Adherence To The Dietary Recommendations and Blood Glucose Levels in Type 1 DiabetesAisiri RaoОценок пока нет
- Drug Literature ReviewДокумент9 страницDrug Literature Reviewabenezer g/kirstosОценок пока нет
- New-Guthrie2015Документ10 страницNew-Guthrie2015Ser Eldrin GarciaОценок пока нет
- Siegel 2018Документ8 страницSiegel 2018indah puspitaОценок пока нет
- Toward Improved Management of NIDDM: A Randomized, Controlled, Pilot Intervention Using A Lowfat, Vegetarian DietДокумент5 страницToward Improved Management of NIDDM: A Randomized, Controlled, Pilot Intervention Using A Lowfat, Vegetarian DietpepeОценок пока нет
- Low Carb StudyДокумент15 страницLow Carb StudycphommalОценок пока нет
- A Randomized Trial of A Low-Carbohydrate Diet For Obesity - NEJMДокумент16 страницA Randomized Trial of A Low-Carbohydrate Diet For Obesity - NEJMMateo PeychauxОценок пока нет
- dc14-0018 FullДокумент8 страницdc14-0018 FullLo RakОценок пока нет
- Wiliam Yancy PDFДокумент7 страницWiliam Yancy PDFDeaz Fazzaura PutriОценок пока нет
- DMSO 27665 Randomized Double Blind Placebo Controlled Linear Dose Cross 011712Документ7 страницDMSO 27665 Randomized Double Blind Placebo Controlled Linear Dose Cross 011712Perfero CaffeОценок пока нет
- Effects of High Performance Inulin Supplementation On Glycemic Control and Antioxidant Status in Women With Type 2 DiabetesДокумент9 страницEffects of High Performance Inulin Supplementation On Glycemic Control and Antioxidant Status in Women With Type 2 DiabetesNia Tiffany HarrkaОценок пока нет
- Beneficial Effects of Viscous Dietary Fiber From Konjac-Mannan in Subjects With The Insulin Resistance Syndro M eДокумент6 страницBeneficial Effects of Viscous Dietary Fiber From Konjac-Mannan in Subjects With The Insulin Resistance Syndro M eNaresh MaliОценок пока нет
- Hypertension 2012 West 58 63Документ7 страницHypertension 2012 West 58 63Rully SyahrizalОценок пока нет
- New England Journal Medicine: The ofДокумент10 страницNew England Journal Medicine: The ofRussell BeckОценок пока нет
- NIH Public Access: Author ManuscriptДокумент18 страницNIH Public Access: Author ManuscriptKevinJuliusTanadyОценок пока нет
- Journal Medicine: The New EnglandДокумент11 страницJournal Medicine: The New EnglandYancy Erazo DoradoОценок пока нет
- 2699 PDFДокумент4 страницы2699 PDFSeptya widhiafniОценок пока нет
- DASH Eating Plan: An Eating Pattern For Diabetes Management: From Research To PracticeДокумент6 страницDASH Eating Plan: An Eating Pattern For Diabetes Management: From Research To PracticeSari SaryonoОценок пока нет
- Weight Management Clinical TrialsДокумент7 страницWeight Management Clinical TrialschuariwapoohОценок пока нет
- InsulinaДокумент8 страницInsulinaClaudiu SufleaОценок пока нет
- Nfs 774 Case StudyДокумент37 страницNfs 774 Case Studyapi-533845626Оценок пока нет
- Contribution of Liraglutide in The Fixed-Ratio Combination of Insulin Degludec and Liraglutide (Ideglira)Документ8 страницContribution of Liraglutide in The Fixed-Ratio Combination of Insulin Degludec and Liraglutide (Ideglira)rakolovaОценок пока нет
- Bean and Rice MealsДокумент7 страницBean and Rice MealsTeky WidyariniОценок пока нет
- Nurul ArfinaДокумент9 страницNurul ArfinaNurul ArfinaОценок пока нет
- Research ArticleДокумент93 страницыResearch Articlearyan batangОценок пока нет
- Efficacy of Glyburide/Metformin Tablets Compared With Initial MonotherapyДокумент7 страницEfficacy of Glyburide/Metformin Tablets Compared With Initial MonotherapyriphqaОценок пока нет
- NEJMoa1200111 (Bariatric Surgery Versus Conventional Medical Therapy For Type 2 Diabetes)Документ9 страницNEJMoa1200111 (Bariatric Surgery Versus Conventional Medical Therapy For Type 2 Diabetes)Daniel Domínguez AldereteОценок пока нет
- Diabetes - EditedДокумент11 страницDiabetes - EditedIssah Issah100% (1)
- Alasan Ke ManusiaДокумент12 страницAlasan Ke ManusiaafiwahyuОценок пока нет
- World J DiabetesДокумент60 страницWorld J DiabetesSheila AurelliaОценок пока нет
- tmp2475 TMPДокумент7 страницtmp2475 TMPFrontiersОценок пока нет
- Mntcasestudy 2Документ25 страницMntcasestudy 2api-309963538Оценок пока нет
- Diabetes DietДокумент8 страницDiabetes DietkitchaaОценок пока нет
- Comparison of High-Fat and High-Protein Diets With A High-Carbohydrate Diet in Insulin-Resistant Obese WomenДокумент9 страницComparison of High-Fat and High-Protein Diets With A High-Carbohydrate Diet in Insulin-Resistant Obese WomenDanielle AliceОценок пока нет
- Physical Activity Intensity and Type 2 Diabetes Risk in Overweight Youth A Randomized TriaДокумент27 страницPhysical Activity Intensity and Type 2 Diabetes Risk in Overweight Youth A Randomized TriaMilenckaVidalConsiglieriОценок пока нет
- Lit ReviewДокумент19 страницLit Reviewapi-240895351Оценок пока нет
- A Very Low Carbohydrate, Low Saturated Fat Diet For Type 2 Diabetes Management: A Randomized TrialДокумент10 страницA Very Low Carbohydrate, Low Saturated Fat Diet For Type 2 Diabetes Management: A Randomized TrialvicenteОценок пока нет
- Barnard, Et Al.,2009Документ9 страницBarnard, Et Al.,2009Kiaraliz Rivera RosaОценок пока нет
- Pistachio Nut Consumption and Serum Lipid Levels: Original ResearchДокумент8 страницPistachio Nut Consumption and Serum Lipid Levels: Original ResearchMônica BatalhaОценок пока нет
- Nutritional Update For Physicians: Plant-Based DietsДокумент6 страницNutritional Update For Physicians: Plant-Based DietsAria Marta KornasОценок пока нет
- Bai & Kumari, 2020Документ5 страницBai & Kumari, 2020larissa matosОценок пока нет
- Type 2 Diabetes Mellitus (Article) Author United States Department of Veterans AffairsДокумент9 страницType 2 Diabetes Mellitus (Article) Author United States Department of Veterans Affairsnaljnaby9Оценок пока нет
- Research: Mediterranean Diets and Metabolic Syndrome Status in The PREDIMED Randomized TrialДокумент9 страницResearch: Mediterranean Diets and Metabolic Syndrome Status in The PREDIMED Randomized TrialDINO ECOОценок пока нет
- Nejmoa2032183 - STEP 1Документ14 страницNejmoa2032183 - STEP 1นันทสิทธิ์ ศิริวิชญ์ไมตรีОценок пока нет
- Ramachandran 2006Документ9 страницRamachandran 2006Dharsheena Seshadri ManogaranОценок пока нет
- ANNALS-Diabetes Tipo IIДокумент16 страницANNALS-Diabetes Tipo IIewb100% (2)
- 05 Iajps05062017Документ6 страниц05 Iajps05062017Baru Chandrasekhar RaoОценок пока нет
- Nutrients 12 00055 v2Документ27 страницNutrients 12 00055 v2Luciano MirianiОценок пока нет
- Human Nutrition and MetabolismДокумент7 страницHuman Nutrition and MetabolismMisyani MisyaniОценок пока нет
- Glycemic Index of Common Malaysian FruitsДокумент5 страницGlycemic Index of Common Malaysian FruitsJia Jun VooОценок пока нет
- Effect of Diet On Type 2 Diabetes Mellitus: A Review.: Sami, W Ansari, T Butt, N.S Hamid, M.R. 2017Документ5 страницEffect of Diet On Type 2 Diabetes Mellitus: A Review.: Sami, W Ansari, T Butt, N.S Hamid, M.R. 2017Yayang SavitaОценок пока нет
- Example 6Документ4 страницыExample 6Tutor BlairОценок пока нет
- Diets Among Obese IndividualsДокумент26 страницDiets Among Obese IndividualsjuanpabloefОценок пока нет
- Dr. Poon's Metabolic Diet Program Improves Clinical and Laboratory Outcomes in Obese Patients With Metabolic SyndromeДокумент5 страницDr. Poon's Metabolic Diet Program Improves Clinical and Laboratory Outcomes in Obese Patients With Metabolic SyndromeasclepiuspdfsОценок пока нет
- Effect of Diets Enriched in Almonds On Insulin Action and Serum Lipids in Adults With Normal Glucose Tolerance or Type 2 DiabetesДокумент7 страницEffect of Diets Enriched in Almonds On Insulin Action and Serum Lipids in Adults With Normal Glucose Tolerance or Type 2 DiabetesLyly SelenaОценок пока нет
- JETIR1905867 - Reduction in Drug Dosage - DR - BiswaroopRoyChowdhury PDFДокумент12 страницJETIR1905867 - Reduction in Drug Dosage - DR - BiswaroopRoyChowdhury PDFSudhir YadavОценок пока нет
- Sitagliptin vs. Pioglitazone As Add-On Treatments in Patients With Uncontrolled Type 2 Diabetes On The Maximal Dose of Metformin Plus SulfonylureaДокумент9 страницSitagliptin vs. Pioglitazone As Add-On Treatments in Patients With Uncontrolled Type 2 Diabetes On The Maximal Dose of Metformin Plus SulfonylureaFebi FernandaОценок пока нет
- Faktor-Faktor Yang Berpengaruh Terhadap Keberadaan Jentik AedesДокумент6 страницFaktor-Faktor Yang Berpengaruh Terhadap Keberadaan Jentik AedesIrfana EfendiОценок пока нет
- DAFTAR PUSTAKA ReferatДокумент3 страницыDAFTAR PUSTAKA ReferatIrfana EfendiОценок пока нет
- Jurnal Irfana EfendiДокумент6 страницJurnal Irfana EfendiIrfana EfendiОценок пока нет
- Christophe Glass Executive Profile PDFДокумент1 страницаChristophe Glass Executive Profile PDFIrfana EfendiОценок пока нет
- BBBBBBNNNДокумент6 страницBBBBBBNNNIrfana EfendiОценок пока нет
- DSFJNFJGNSFNBДокумент1 страницаDSFJNFJGNSFNBIrfana EfendiОценок пока нет
- FalseДокумент7 страницFalseIrfana EfendiОценок пока нет
- Daftar Pustaka: (Accessed: April 28, 2010)Документ3 страницыDaftar Pustaka: (Accessed: April 28, 2010)Irfana EfendiОценок пока нет
- Accepted Manuscript: 10.1016/j.nut.2014.07.005Документ43 страницыAccepted Manuscript: 10.1016/j.nut.2014.07.005Irfana EfendiОценок пока нет
- OUTPUTДокумент31 страницаOUTPUTIrfana EfendiОценок пока нет
- Jurnal Politik Dan Cinta Tanah Air Dalam Perspektif IslamДокумент9 страницJurnal Politik Dan Cinta Tanah Air Dalam Perspektif Islamalpiantoutina12Оценок пока нет
- MOtivating Your Teenager PDFДокумент66 страницMOtivating Your Teenager PDFElleMichelle100% (1)
- (Music of The African Diaspora) Robin D. Moore-Music and Revolution - Cultural Change in Socialist Cuba (Music of The African Diaspora) - University of California Press (2006) PDFДокумент367 страниц(Music of The African Diaspora) Robin D. Moore-Music and Revolution - Cultural Change in Socialist Cuba (Music of The African Diaspora) - University of California Press (2006) PDFGabrielОценок пока нет
- Statistical MethodsДокумент4 страницыStatistical MethodsYra Louisse Taroma100% (1)
- Conversational Maxims and Some Philosophical ProblemsДокумент15 страницConversational Maxims and Some Philosophical ProblemsPedro Alberto SanchezОценок пока нет
- Applied Mechanics-Statics III PDFДокумент24 страницыApplied Mechanics-Statics III PDFTasha AОценок пока нет
- Talent Development - FranceДокумент6 страницTalent Development - FranceAkram HamiciОценок пока нет
- Bab 3 - Soal-Soal No. 4 SD 10Документ4 страницыBab 3 - Soal-Soal No. 4 SD 10Vanni LimОценок пока нет
- Easter in RomaniaДокумент5 страницEaster in RomaniaDragos IonutОценок пока нет
- Peter Lehr Militant Buddhism The Rise of Religious Violence in Sri Lanka Myanmar and Thailand Springer International PDFДокумент305 страницPeter Lehr Militant Buddhism The Rise of Religious Violence in Sri Lanka Myanmar and Thailand Springer International PDFIloviaaya RegitaОценок пока нет
- Social Awareness CompetencyДокумент30 страницSocial Awareness CompetencyudaykumarОценок пока нет
- Assignment 1 Front Sheet: Qualification BTEC Level 5 HND Diploma in Computing Unit Number and Title Submission DateДокумент18 страницAssignment 1 Front Sheet: Qualification BTEC Level 5 HND Diploma in Computing Unit Number and Title Submission DatecuongОценок пока нет
- Hibbeler, Mechanics of Materials-BendingДокумент63 страницыHibbeler, Mechanics of Materials-Bendingpoom2007Оценок пока нет
- PETE 689 Underbalanced Drilling (UBD) : Well Engineering Read: UDM Chapter 5 Pages 5.1-5.41Документ74 страницыPETE 689 Underbalanced Drilling (UBD) : Well Engineering Read: UDM Chapter 5 Pages 5.1-5.41Heris SitompulОценок пока нет
- 2,3,5 Aqidah Dan QHДокумент5 страниц2,3,5 Aqidah Dan QHBang PaingОценок пока нет
- CV Michael Naughton 2019Документ2 страницыCV Michael Naughton 2019api-380850234Оценок пока нет
- Personal Philosophy of Education-Exemplar 1Документ2 страницыPersonal Philosophy of Education-Exemplar 1api-247024656Оценок пока нет
- Unidad 12 (libro-PowerPoint)Документ5 страницUnidad 12 (libro-PowerPoint)Franklin Suarez.HОценок пока нет
- How To Create Partner Function in SAP ABAPДокумент5 страницHow To Create Partner Function in SAP ABAPRommel SorengОценок пока нет
- Spring94 Exam - Civ ProДокумент4 страницыSpring94 Exam - Civ ProGenUp SportsОценок пока нет
- Cognitive ApprenticeshipДокумент5 страницCognitive ApprenticeshipRandall RobertsОценок пока нет
- Final Box Design Prog.Документ61 страницаFinal Box Design Prog.afifa kausarОценок пока нет
- Hero Cash Cash Lyrics - Google SearchДокумент1 страницаHero Cash Cash Lyrics - Google Searchalya mazeneeОценок пока нет
- Ottley Sandra 2009Документ285 страницOttley Sandra 2009Lucas Fariña AlheirosОценок пока нет
- Ielts Reading Whale CultureДокумент4 страницыIelts Reading Whale CultureTreesa VarugheseОценок пока нет
- Created By: Susan JonesДокумент246 страницCreated By: Susan JonesdanitzavgОценок пока нет
- AdvacДокумент13 страницAdvacAmie Jane MirandaОценок пока нет
- THE LAW OF - John Searl Solution PDFДокумент50 страницTHE LAW OF - John Searl Solution PDFerehov1100% (1)
- Copper Reaction: Guillermo, Charles Hondonero, Christine Ilao, Ellaine Kim, Yumi Lambrinto, Arl JoshuaДокумент6 страницCopper Reaction: Guillermo, Charles Hondonero, Christine Ilao, Ellaine Kim, Yumi Lambrinto, Arl JoshuaCharles GuillermoОценок пока нет
- Ancestral Healing PrayersДокумент4 страницыAncestral Healing Prayerssuperhumannz100% (13)