Академический Документы
Профессиональный Документы
Культура Документы
PARA LEC Other Medically Important Protozoans 2
Загружено:
smcm11Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
PARA LEC Other Medically Important Protozoans 2
Загружено:
smcm11Авторское право:
Доступные форматы
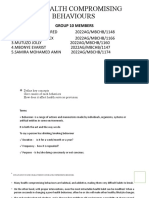
Other Medically Important Protozoans
PARASITOLOGY LECTURE (FLORES)
Babesia
spp.
-
-
-
-
-
-
-
-
-
Apicomplexan
o Intracellular
parasites
Blood
parasite
that
cause
malaria-like
infections
Zoonotic
infection;
transmitted
by
ticks
Causitive
agents
o Babesia
microti
o Babesia
divergens
Transovarian
parasite
can
be
transferred
to
the
offspring
of
the
tick
o Usually
seen
in
the
life
cycle
of
B.
divergens
IS
to
tick:
gametes
IS
to
man:
IS
to
mouse:
sporozoite
DH:
Tick
(Ixodes)
IH:
o White
footed
mouse
o Deer
o Livestock
o Cattle
o Humans
(accidental
host)
MOT:
o Bite
of
an
infected
tick
o Blood
transfusion
o Organ
transplant
o Vertical
transmission
SMCM EMT2017
has
been
documented
for
"large"
Babesia
spp.
but
not
for
the
"small"
babesiae,
such
as
B.
microti
.
Humans
enter
the
cycle
when
bitten
by
infected
ticks.
During
a
blood
meal,
a
Babesia-infected
tick
introduces
sporozoites
into
the
human
host
.
Sporozoites
enter
erythrocytes
and
undergo
asexual
replication
(budding)
.
Multiplication
of
the
blood
stage
parasites
is
responsible
for
the
clinical
manifestations
of
the
disease.
Humans
are,
for
all
practical
purposes,
dead-end
hosts
and
there
is
probably
little,
if
any,
subsequent
transmission
that
occurs
from
ticks
feeding
on
infected
persons.
However,
human
to
human
transmission
is
well
recognized
to
occur
through
blood
transfusions
Morphology
- Similar
to
malarial
parasite
o No
schizonts
or
gametocytes
- Up
to
4
parasites
per
cell
- Incubation
period:
1-12
months
- Gametocyte
has
no
hemozoin
pigment
- Merozoites:
o 4
in
a
cell
o Maltese
cross
appearance
- Immunocompetent
humans:
Asymptomatic
Life
Cycle
The
Babesia
microti
life
cycle
involves
two
hosts,
which
includes
a
rodent,
primarily
the
white-footed
mouse,
Peromyscus
leucopus,
and
a
tick
in
the
genus,
Ixodes.
During
a
blood
meal,
a
Babesia-
infected
tick
introduces
sporozoites
into
the
mouse
host
.
Sporozoites
enter
erythrocytes
and
undergo
asexual
reproduction
(budding)
.
In
the
blood,
some
parasites
differentiate
into
male
and
female
gametes
although
these
cannot
be
distinguished
at
the
light
microscope
level
.
The
definitive
host
is
the
tick.
Once
ingested
by
an
appropriate
tick
,
gametes
unite
and
undergo
a
sporogonic
cycle
resulting
in
sporozoites
.
Transovarial
transmission
(also
known
as
vertical,
or
hereditary,
transmission)
Disease
Manifestation
and
Pathogenesis
- Causes
Babesiosis
or
Nantucket
Fever
or
Redwater
Fever,
Tick
Fever,
Texas
Cattle
Fever
- Most
cases
are
asymptomatc
and
usually
self-limiting
- Signs
and
symptoms:
o Mild
chills
and
fever
o Hemolytic
anemia
o Jaundice
o Hepatomegaly
o No
malarial
paroxysm
Risk
Factors
for
Severe
cases
of
Babesiosis
- Co-infection
with
Borrelia
burgdorferi
o Transmitted
with
the
same
tick
(vector)
o Causes
Lyme
disease
- Old
age
weak
immune
system
SMCM EMT2017
Other Medically Important Protozoans
PARASITOLOGY LECTURE (FLORES)
Absence of spleen: Splenectomy (removal of the spleen,
which removes abnormal or distorted RBCs)
Immunodeficiency
-
Diagnosis
- Examination
of
Giemsa
stained
smears
- Serology
o IFAT
(Diagnostic
titer
=
1:64)
o Inoculation
of
Animals
(Gold
Hamster
or
gerbil)
Positive results: if hamster is
susceptible to the infection
- History of tick bite
- Molecular methods:
o PCR: more sensitive in detecting the parasite
Epidemiology
- Zoonotic
- Europe: Babesia divergens
- North America: Babesia microti
o North East, East Coast
o cases also reported in West Coast
- Human infections usually occur during spring and summer
- No human infections reported yet in the country
Treatment
- Clindamycin
Prevention
- Avoid tick bites
- Screen blood donors
- Apply insect repellants
Blood and Tissue Flagellates
-
-
-
-
Hemoflagellates
Flagellates
that
are
found
in
the
blood
and
other
fluids
(CSF)
and
in
tissues
Vector
borne
parasites
Medically
important
genera
o Trypanosoma
o Leishmania
Generalities
- Only
Trypanosoma
and
Leishmania
infect
humans
- Transmitted
by
a
bite
of
an
infected
vector
- 4
morphological
forms/stages
o Amastigote
No flagella
Found inside the cell; intracellular
Donovan-Leishman form
Nucleus
Kinetoplast: energy source; primarly
composed of DNA
Axoneme: root of flagellum
Basal body
Found intracellularly only
Promastigote
Leptomonas stage
First time to see flagella
Longer and slender
First stage to have flagella
Axoneme
Basal body
Kinetoplast: anterior to the nucleus
o Epimastigote
Crithidia
First stage to have undulating
membrane (1/2 body length)
Kinetoplast: Anterior to the nucleus
o Trypomastigote
Structures: Nucleus
Undulating membrane: full body
length
Kinetoplast: posterior to the nucleus
C-shape / S-shape / U-shape
All forms are found in Trypanosoma cruzi infections
Only the epimastigote and trypomastigote are seen in
Trypanosoma brucei
Leishmania infections: seen amastigote and promastigote
Diagnostic stages: amastigote and promastigote
o
-
-
-
-
Trypanosoma
cruzi
- Hemoflagellate
- Causes
Chagas
Disease
or
American
Trypanosomiasis
- Final
host:
Human
- Diagnostic
stage:
trypomastigote
found
in
blood
- Final
host:
humans
- Reservoir
hosts:
o Armadillo
o Opossum
o Raccoon
o Dog
o Cat
- Intermediate
host
vector:
o Reduviid
Bug
(major)
Prefers lips during bug bite
o Triatomine bugs
o Kissing bug
- IS to humans: Metacyclic Trypomastigote
Life Cycle
SMCM EMT2017
Other Medically Important Protozoans
PARASITOLOGY LECTURE (FLORES)
o
o
An infected triatomine insect vector (or "kissing" bug) takes a blood
meal and releases trypomastigotes in its feces near the site of the
bite wound. Trypomastigotes enter the host through the wound or
through intact mucosal membranes, such as the conjunctiva .
Common triatomine vector species for trypanosomiasis belong to
the genera Triatoma, Rhodnius, andPanstrongylus. Inside the host,
the trypomastigotes invade cells near the site of inoculation, where
they differentiate into intracellular amastigotes . The amastigotes
multiply by binary fission and differentiate into trypomastigotes,
and then are released into the circulation as bloodstream
trypomastigotes . Trypomastigotes infect cells from a variety of
tissues and transform into intracellular amastigotes in new infection
sites. Clinical manifestations can result from this infective cycle. The
bloodstream trypomastigotes do not replicate (different from the
African trypanosomes). Replication resumes only when the
parasites enter another cell or are ingested by another vector. The
kissing bug becomes infected by feeding on human or animal
blood that contains circulating parasites
. The ingested
trypomastigotes transform into epimastigotes in the vectors
midgut
. The parasites multiply and differentiate in the
midgut
and differentiate into infective metacyclic
trypomastigotes in the hindgut .
Disease Manifestation and Pathogenesis
- Patients can be infected up to 20 years
- Chagoma: local inflammation; reddish nodule
o Found on site of bite / bite wound
- Romanas sign: early stages; type of periorbital swelling
(edema of eyelid and conjunctiva) (Eyelids: another site
that can be bitten)
- Acute phase
o Fever
o Lymphadenopathy (inflammation of lymph
nodes)
- Chronic phase
o No characteristic symptoms
- Manifestations of Chronic Phase
o Mega esophagus
o Mega colon
o Cardiomegaly
Cardiac arrhythmia / megacardium
Can lead to death
Pathogenesis
- Acute
inflammatory
reaction
on
bite
- Uses
lectin
like
carbohydrates
for
binding
- Direct
inflammatory
response
o Chaga
toxin
o Damage
to
infected
cells
o Destruction
of
autonomic
nerve
ganglions
- Target
cells:
o Cells
of
RES
o Cardiac
cells
o Skeletal
cells
o Smooth
muscles
o Neuroglia
cells
Diagnosis
- Cardiac
symptoms
are
present
if
living
in
endemic
regions
- Usually
in
South
America
(Brazil)
- Demonstration
of
trypanosomes
in
blood,
CSF,
tissues,
lymph
(staining
using
Giemsa)
- Xenodiagnosis:
to
confirm,
get
a
laboratory
reared
reduviid
bug;
bite
infected
patient
look
for
parasite
stages
in
the
bug
after
- Culture:
o Changs
o NNN
- Serology:
o IFAT
o Complement
fixation
o ELISA
Epidemiology
- Occurs
only
in
American
continent
o Highest
prevalence
in
Brazil
o More
common
in
rural
areas
o Chronic
disease
is
more
common
o Common
in
unsanitary
housing
conditions
o More
fatal
in
young
children
o Zoonotic
- Vector
is
found
in
Philippines
but
no
reported
cases
Treatment
- Nifurtimox
- Benznidazole
Prevention
and
Control
- Vector
control
- Screening
of
blood
- Health
education
Trypanosoma
brucei
complex
- 2
subspecies
o Trypanosoma
brucei
rhodesiense
o Trypanosoma
brucei
gambiense
3
SMCM EMT2017
Other Medically Important Protozoans
PARASITOLOGY LECTURE (FLORES)
Etiologic agents of African sleeping sickness
Trypanosoma brucei rhodesiense
a. Causes Rhodesian or East African Sleeping
Sickness
b. Endemic East and South Africa
2. Trypanosoma brucei gambiense
a. Causes Gambian or
- Under microscope, same morphology
- To differentiate:
- Vector Transmitted Parasitic Infections
o Vector: Tsetse Fly (Glossina spp.)
T.
b.
r.
G.
pallidipes,
G.
morsitans
Life
Cycle
2.
During
a
blood
meal
on
the
mammalian
host,
an
infected
tsetse
fly
(genus
Glossina)
injects
metacyclic
trypomastigotes
into
skin
tissue.
The
parasites
enter
the
lymphatic
system
and
pass
into
the
bloodstream
.
Inside
the
host,
they
transform
into
bloodstream
trypomastigotes
,
are
carried
to
other
sites
throughout
the
body,
reach
other
blood
fluids
(e.g.,
lymph,
spinal
fluid),
and
continue
the
replication
by
binary
fission
.
The
entire
life
cycle
of
African
Trypanosomes
is
represented
by
extracellular
stages.
The
tsetse
fly
becomes
infected
with
bloodstream
trypomastigotes
when
taking
a
blood
meal
on
an
infected
mammalian
host
( ,
).
In
the
flys
midgut,
the
parasites
transform
into
procyclic
trypomastigotes,
multiply
by
binary
fission
,
leave
the
midgut,
and
transform
into
epimastigotes
.
The
epimastigotes
reach
the
flys
salivary
glands
and
continue
multiplication
by
binary
fission
.
The
cycle
in
the
fly
takes
approximately
3
weeks.
Humans
are
the
main
reservoir
host
for
Trypanosoma
brucei
gambiense,
but
this
species
can
also
be
found
in
animals.
Wild
game
animals
are
the
main
reservoir
host
of
T.
b.
rhodesiense.
Morphology
- Epimastigote
found
in
insect
- Trypomastigote
found
in
mammalian
host
Disease
Manifestation
1. Trypanosoma
brucei
gambiense
Causes Gambian or West African Sleeping
Sickness
o Earliest sign: Trypanosomal Chancre
Patients will appear healthy
Blood smear: negative in early stages,
+ trypomastigotes
Patients experience fever once the
lymph nodes are affected.
Other manifestations include malaise,
weakness, night sweats, dizziness and
nausea
o Winterbottoms sign
o Chronic disease
CNS invasion
Sleeping sickness stage initiated
Severe headache
Increasing mental deterioration
Apathy
Meningoencephalitis
Manifestation of Kerandels Sign:
delayed sensation to pain
o Terminal Phase
Coma leading to death
Trypanosoma brucei rhodesiense
o Causes Rhodesian and East African Sleeping
Sickness
o Similar to Gambian Sleeping Sickness
But acute and rapidly progressing
CNS stgae takes place in the early
stages
Glomerulonephritis may also be seen
o
-
1.
Pathogenesis
- Generalized
Lymphoid
Hyperplasia
- Anemia
- Thrombocytopenia
- Hypergammaglobulinemia
- Immune
evasion
though:
Variant
Surface
Glycoproteins
- Acute
infection
seen
in
Rhodesian
Sleeping
Sickness
- Chronic
Infection
seen
in
Gambian
Sleeping
Sickness
Diagnosis
- Physical
findings
and
patient
history
- Demonstration
of
trypomastogotes
in:
o Blood
o CSF
o Lymph
node
aspirate
- Concentration
of
buffy
coat
o Giemsa
stain
- Serology
o IHAT
o ELISA
o Rapid
tests
- Molecular
methods
- Animal
inculation
and
culture
4
Other Medically Important Protozoans
PARASITOLOGY LECTURE (FLORES)
Epidemiology
- Vectors
inhabit
areas
near
river
banks
and
streams
- Congenital
transmission
is
possible
- Low
prevalence
rate
(<1%)
Treatment
- Better
prognosis
if
treatment
started
before
CNS
stage
- Pentamidine
and
Suramine
(blood
and
lymphatic
stage)
- Melarsoprol
(late
stage)
Leishmania
spp.
- Vector
Borne
Parasitic
Disese
- Vector:
sandflies
(Phlebotomus
spp.)
- Obligate
intracellular
parasites
- Primarily
a
zoonotic
disease
- Humans
are
infected
by
bite
of
sandflies
o Other
MOT
Blood tranfusion
Contact
Contamination of bite wound
- Target cells: RE cells (Reticulo endothelial cells
macrophage)
- Leishmania tropica
- Leishmania braziliensis
- Leishmania donovani
- IS to man: promastigote
- IS to fly: amastigote
Life cycle
Leishmaniasis is transmitted by the bite of infected female
phlebotomine sandflies. The sandflies inject the infective stage (i.e.,
promastigotes) from their proboscis during blood meals
.
Promastigotes that reach the puncture wound are phagocytized by
SMCM EMT2017
macrophages and other types of mononuclear phagocytic cells.
Progmastigotes transform in these cells into the tissue stage of the
parasite (i.e., amastigotes) , which multiply by simple division and
proceed to infect other mononuclear phagocytic cells . Parasite,
host, and other factors affect whether the infection becomes
symptomatic and whether cutaneous or visceral leishmaniasis
results. Sandflies become infected by ingesting infected cells during
blood meals ( , ). In sandflies, amastigotes transform into
promastigotes, develop in the gut (in the hindgut for leishmanial
organisms in the Viannia subgenus; in the midgut for organisms in
the Leishmania subgenus), and migrate to the proboscis .
Morphology
- Amastigote form is seen in mammalian host
o Purple dots = amastigote
- Promastigote form is seen in sand fly
Disease Manifestations
1. Cutaneous Leishmaniasis
- Other names:
o Old World Leishmaniasis
o Aleppo Button
o Delhi Boil
o Baghdad Boil
o Jericho Boil
- Etiology: Leishmania tropica
- Incubation period: weeks to months
- Elevated skin ulcers (painless)
o leaves an ugly scar
o highly disfiguring
2. Mucocutaneous Leishmaniasis
- Other names:
o American Leishmaniasis
o New World Leishmaniasis
- Etiologic agent: Leishmania braziliensis
- Incubation: weeks to months
- Disease Manifestations
o Initial stage: ulcers similar to Old World
Leishmania
o Later stage: spread to oronasal and pharygneal
mucosa
Espundia
Tapir nose
Chiclero
ulcer
3. Visceral
leishmaniasis
- Other
names:
o Kala-azar
o Dumdum
fever
o Black
fever
- Etiology:
Leishmania
donovani
- Incubation
perios:
1-3
months
- Manifestation
o Dromedary
fever:
fever
with
twice
daily
elevations
o Splenomegaly
o Cachexia
5
Other Medically Important Protozoans
PARASITOLOGY LECTURE (FLORES)
o
o
o
SMCM EMT2017
Hepatomegaly
Darkening
of
skin
(forehead,
temples,
around
the
mouth)
Dermal
leishmanoid
lesions
may
be
rarely
seen
Epidemiology
- Endemic
in
88
countries
on
5
continents
- Endemic
areas:
o Visceral
Leishmaniasis:
Bangladesh,
Brazil,
India,
Nepal,
Sudan
o Cutaneous
Leishmaniasis:
Afganistan,
Brazil,
Iran,
Peru,
Saudi
Arabia,
Syria
o Mucotaneous
Leishmaniasis:
Brazil,
Eastern
Peru,
Bolivia,
Paraguay,
Ecuador,
Colombia,
Venezuela
Diagnosis
- Demonstration
of
Lesions
- Tissue
Biopsies
- Skin
Biopsies
- Examination
of
BM,
spleen,
lymph
node
- Montenegro
skin
test
Leishmanin
Skin
Test
- Serology:
IFAT
- Culture:
NNN
- Molecular
methods
Treatment
- Antimony
Compounds
o Soidum
Stibogluconate
o n-methyl-glucamine
antimonate
Вам также может понравиться
- Para Lab Demo Oct 15 2015Документ36 страницPara Lab Demo Oct 15 2015smcm11Оценок пока нет
- T Spiralis and FriendsДокумент4 страницыT Spiralis and Friendssmcm11Оценок пока нет
- Para Lab Lecture 2Документ6 страницPara Lab Lecture 2smcm11Оценок пока нет
- Carbohydrates 2Документ81 страницаCarbohydrates 2smcm11Оценок пока нет
- Lift CarryДокумент7 страницLift CarryBianca ThereseОценок пока нет
- Human ActДокумент21 страницаHuman Actsmcm11Оценок пока нет
- Christian AnthropologyДокумент17 страницChristian Anthropologysmcm11Оценок пока нет
- Phys Chem Exam of Urine PPT Handout 2012 (Compatibility Mode)Документ12 страницPhys Chem Exam of Urine PPT Handout 2012 (Compatibility Mode)smcm11Оценок пока нет
- Connective TissueДокумент65 страницConnective Tissuesmcm11Оценок пока нет
- Carbohydrates 2Документ81 страницаCarbohydrates 2smcm11Оценок пока нет
- RNA Isolation From YeastsДокумент1 страницаRNA Isolation From Yeastssmcm11Оценок пока нет
- LIT Quiz #1Документ7 страницLIT Quiz #1smcm11Оценок пока нет
- 25 Amino AcidsДокумент3 страницы25 Amino AcidsAkramul HaqueОценок пока нет
- Mutation and DNA RepairДокумент14 страницMutation and DNA Repairsmcm11Оценок пока нет
- Chapter 2: The Effective Teacher: - Mastery of The Subject MatterДокумент3 страницыChapter 2: The Effective Teacher: - Mastery of The Subject Mattersmcm11Оценок пока нет
- Ip Manual 01Документ42 страницыIp Manual 01smcm11Оценок пока нет
- Benedict Anderson - Imagined CommunitiesДокумент8 страницBenedict Anderson - Imagined CommunitiesSaurav DattaОценок пока нет
- Digestive SystemДокумент95 страницDigestive Systemsmcm11Оценок пока нет
- Chapter 5 Stereochemistry Chiral MoleculesДокумент29 страницChapter 5 Stereochemistry Chiral Moleculessmcm11Оценок пока нет
- Exp6 - Comparative Investigation of Organic CompoundsДокумент3 страницыExp6 - Comparative Investigation of Organic Compoundssmcm11Оценок пока нет
- HETARДокумент25 страницHETARsmcm11Оценок пока нет
- Ip Manual 01Документ42 страницыIp Manual 01smcm11Оценок пока нет
- Chap23 Powerpoint LДокумент63 страницыChap23 Powerpoint Lsmcm11100% (1)
- Table 1. Solubility of Alcohols in WaterДокумент1 страницаTable 1. Solubility of Alcohols in Watersmcm11Оценок пока нет
- Chapter 4 Lec NewtonДокумент40 страницChapter 4 Lec Newtonsmcm11Оценок пока нет
- Respiratory SystemДокумент70 страницRespiratory Systemsmcm11Оценок пока нет
- HydrocarbonsДокумент36 страницHydrocarbonsdan_petre_popescu100% (2)
- Applications of Newton - S LawsДокумент11 страницApplications of Newton - S Lawssmcm11Оценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Overview of hemostasis antiplatelets, anticoagulants & fibrinolytic agentsДокумент21 страницаOverview of hemostasis antiplatelets, anticoagulants & fibrinolytic agents黄資元100% (1)
- Adult Idiopathic Hypertrophic Pyloric Stenosis A Common Presentation With An Uncommon DiagnosisДокумент5 страницAdult Idiopathic Hypertrophic Pyloric Stenosis A Common Presentation With An Uncommon DiagnosiszapomannОценок пока нет
- Flowchart Clinic Management SystemДокумент1 страницаFlowchart Clinic Management SystemAbhijit KulkarniОценок пока нет
- Cancer NursingДокумент42 страницыCancer NursingXaa YaaОценок пока нет
- IWU Nursing Care Plan for 81-Year-Old Female with CHF and PneumoniaДокумент6 страницIWU Nursing Care Plan for 81-Year-Old Female with CHF and PneumoniaclarimerОценок пока нет
- Diseases of The MouthДокумент4 страницыDiseases of The MouthAhmed Gh Al-zechrawiОценок пока нет
- 16) Facial Diplegia With ParesthesiaДокумент2 страницы16) Facial Diplegia With ParesthesiaRoxana AndreeaОценок пока нет
- Anatomy, Lecture 5, Pleurae & Lungs (Slides)Документ21 страницаAnatomy, Lecture 5, Pleurae & Lungs (Slides)Ali Al-Qudsi100% (1)
- Margaret Roy A First Materia Medica For Homoeopathy: Reading ExcerptДокумент7 страницMargaret Roy A First Materia Medica For Homoeopathy: Reading ExcerptSohail LatifОценок пока нет
- Manual AspergerДокумент309 страницManual AspergerCindy Ramona FaluvegiОценок пока нет
- Piquet 2021Документ8 страницPiquet 2021Manuel Amade OvalleОценок пока нет
- Anti-Dsdna-Ncx Elisa (Igg) Test Instruction: Summary and ExplanationДокумент12 страницAnti-Dsdna-Ncx Elisa (Igg) Test Instruction: Summary and Explanationanahh ramakОценок пока нет
- Scleroderma in The Common Orthopaedic Practice A Review KZ2tДокумент3 страницыScleroderma in The Common Orthopaedic Practice A Review KZ2tMagdaОценок пока нет
- CBIC Free Test 2023Документ7 страницCBIC Free Test 2023cPanelОценок пока нет
- Serological Test On Bacterial Infections-Streptococcal InfectionДокумент5 страницSerological Test On Bacterial Infections-Streptococcal InfectionMarlon BauagОценок пока нет
- Om Health Campus Affiliated To Purbanchal University Gopikrishnanagar, KathmanduДокумент107 страницOm Health Campus Affiliated To Purbanchal University Gopikrishnanagar, KathmanduAdditi SatyalОценок пока нет
- Pediatric Nursing IДокумент2 страницыPediatric Nursing IFilipino Nurses CentralОценок пока нет
- Shyamal Neuronal Migration DisorderДокумент3 страницыShyamal Neuronal Migration Disorderapi-228136529Оценок пока нет
- Group 10Документ12 страницGroup 10Esdras DountioОценок пока нет
- National Mediclaim Policy (NMP)Документ20 страницNational Mediclaim Policy (NMP)Binode SarkarОценок пока нет
- International Ayurvedic Medical JournalДокумент7 страницInternational Ayurvedic Medical JournalChandu PanditОценок пока нет
- Taenia Saginata Taenia Solium: "Beef Tapeworm"Документ6 страницTaenia Saginata Taenia Solium: "Beef Tapeworm"Gela ReyesОценок пока нет
- Mental Status: Ateneo de Zamboanga UniversityДокумент7 страницMental Status: Ateneo de Zamboanga UniversityMaha AmilОценок пока нет
- Antistreptolysin oДокумент3 страницыAntistreptolysin oces8bautistaОценок пока нет
- 2020-Indian Journal of Public Health Research and Development (Scopus Q-4)Документ5 страниц2020-Indian Journal of Public Health Research and Development (Scopus Q-4)NoniAndayaniОценок пока нет
- Medicine Question Bank RS4Документ26 страницMedicine Question Bank RS4Unnathi TОценок пока нет
- Cerebral Palsy: Signs & Symptoms / Pathophysiology / Drug Studies / Ncps / Health TeachingsДокумент22 страницыCerebral Palsy: Signs & Symptoms / Pathophysiology / Drug Studies / Ncps / Health TeachingsGeoffrey Sintaan RiveraОценок пока нет
- Information Sheet For CandidateДокумент3 страницыInformation Sheet For CandidatejljoioiuОценок пока нет
- Forthcoming Grand Chamber Case Vavricka and Others v. Czech RepublicДокумент3 страницыForthcoming Grand Chamber Case Vavricka and Others v. Czech RepublicZiarul de GardăОценок пока нет
- Pharmacotherapeutics For Advanced Practice A Practical Approach Ebook PDFДокумент62 страницыPharmacotherapeutics For Advanced Practice A Practical Approach Ebook PDFrosanne.hahn846100% (39)