Академический Документы
Профессиональный Документы
Культура Документы
Recommendation
Загружено:
imthebossОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Recommendation
Загружено:
imthebossАвторское право:
Доступные форматы
RECOMMENDATION
Immediately after the diagnosis of acute primary angle closure, the patient
should receive the following medications, providing no contraindications exist:
The optometrist should review signs and symptoms of an acute angle closure in
detail with patients suspected of having ACG and those who have undergone an
iridotomy. Patients should be instructed to seek care immediately if any of these
signs or symptoms is noted. Because of the increased risk associated with a
positive family history, all first-degree relatives of the patient should be
encouraged to have a comprehensive eye and vision examination.
500 mg acetazolamide orally
One drop of 0.5% timolol
One drop of 2% pilocarpine
One drop of 1% apraclonidine.
While attempting to break an angle closure attack, the clinician should check IOP
readings every 15-30 minutes. If the attack is not broken 1 hour after institution of
treatment, oral hyperosmotics may be administered along with repeating all
topical medications. When an attack is unbroken after 2 hours, the patient should
have argon (or diode) laser gonioplasty. If the patient is still in angle closure 4-6
hours after initiation of treatment, emergency LPI or surgical iridectomy should
be attempted. When the IOP falls to 20 mm Hg or below, gonioscopy should be
performed to confirm that the angle is open.
An acute attack of angle closure glaucoma should not be considered broken until
the IOP has returned to normal levels, the pupil is miotic, and the angle is open.
Low pressure is not, by itself, indicative of a broken attack. When the angle is not
open, IOP will again rise to very high levels in hours to days. When the attack
can be broken medically, the patient should be maintained on 2% pilocarpine four
times a day bilaterally, and 1% prednisolone acetate four times daily in the
affected eye until a LPI is performed. Most clinicians also keep the patient on a
topical beta blocker twice a day in the affected eye. Miosis helps guard against
reclosure; topical steroids reduce the inflammation associated with angle closure;
and the beta blocker decreases aqueous production. It is customary to wait 2-7
days after breaking the attack before performing the LPI to allow resolution of the
iris congestion and the anterior chamber response.
Patient Education
The optometrist should review signs and symptoms of an acute angle closure in
detail with patients suspected of having ACG and those who have undergone an
iridotomy. Patients should be instructed to seek care immediately if any of these
signs or symptoms are noted. Because of the increased risk associated with a
positive family history, all first-degree relatives of the patient should be
encouraged to have a comprehensive eye and vision examination.
PROGNOSIS AND FOLLOW-UP
Patients with primary ACG should not be considered cured even after successful
LPI. Such patients should be considered glaucoma suspects for life and receive
appropriate followup care. Elevated pressure in the immediate postiridotomy
period can occur secondary to incomplete or closed iridotomy, inflammation or
extensive PAS, or in response to steroid therapy. Late-stage IOP rise may be due
to trabecular meshwork damage that occurred during the period of appositional
closure, or to nonpupillary block components of angle closure, such as plateau
iris and malignant glaucoma. The development of open angle glaucoma is also
possible in these patients.
Patients who have undergone LPI should be evaluated in the immediate
postprocedure period (1-7 days). The examination should be directed toward
establishing patency of the iridotomy, IOP measurement and control, and
gonioscopy to reaffirm that the anterior chamber angle remains open. These
patients should also be examined at 1, 2, and 6 months following LPI. Most
iridotomy closures occur within the first 2 months, almost never past 6 months;
therefore, evaluating patency of the iridotomy is critical in these examinations.
The 1-month visit should include dilation with stereoscopic evaluation of the optic
nerve head. Baseline photos of the optic nerve head and baseline threshold
visual fields may be conducted, if not previously obtained. Long-term followup of
patients who have undergone LPI should be every 6-12 months.
Primary ACG suspects should undergo baseline gonioscopy with standard
classification and drawing, careful biomicroscopic evaluation, stereoscopic
evaluation of the optic nerve head with baseline photos, and baseline threshold
visual fields. Clinicians should educate these patients regarding the signs and
symptoms of an acute angle closure attack and instruct them to seek care
immediately under those circumstances. Long-term monitoring of these patients
should be every 3-4 months for the first year and every 6-12 months thereafter.
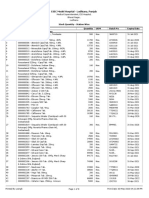
Appendix Figure 2 provides a summary of the frequency and composition of
evaluations for patients with primary ACG.
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- New IELTS Writing Answer SheetДокумент4 страницыNew IELTS Writing Answer Sheetraaj2240% (5)
- August Complete (Compressed)Документ447 страницAugust Complete (Compressed)Dr-Qazi Ejaz AhmadОценок пока нет
- Useful Mother Tinctures in My Homoeopathic PracticeДокумент8 страницUseful Mother Tinctures in My Homoeopathic PracticeAbhijit100% (1)
- Imci Chart Booklet 2011 - 1 PDFДокумент64 страницыImci Chart Booklet 2011 - 1 PDFDanny Irung100% (2)
- Peritonitis: Presentan: FAUZAN AKBAR YUSYAHADI - 12100118191Документ21 страницаPeritonitis: Presentan: FAUZAN AKBAR YUSYAHADI - 12100118191Fauzan Fourro100% (1)
- Meds Quick RefДокумент134 страницыMeds Quick RefPopa D. SilviuОценок пока нет
- FluphenazineДокумент4 страницыFluphenazineimthebossОценок пока нет
- IELTS Reading Answer SheetДокумент1 страницаIELTS Reading Answer Sheetskuppal50% (2)
- SVTДокумент8 страницSVTJulieОценок пока нет
- Medical MCQ Center - Tuberculosis MCQsДокумент4 страницыMedical MCQ Center - Tuberculosis MCQsnarendrakumar9450% (2)
- RubellaДокумент26 страницRubellaAndré BrincatОценок пока нет
- Home Visit Plans: Pregnant Woman Post Partum Well-Baby MorbidДокумент1 страницаHome Visit Plans: Pregnant Woman Post Partum Well-Baby MorbidimthebossОценок пока нет
- My Boracay Guide Map 27th EditionДокумент2 страницыMy Boracay Guide Map 27th EditionimthebossОценок пока нет
- CUES1Документ1 страницаCUES1Emman Carl Ely RubinОценок пока нет
- Name of Drug General Action Specific Action Indications Contraindicati ONS Side/Adverse Effects Nursing Responsibilitie SДокумент1 страницаName of Drug General Action Specific Action Indications Contraindicati ONS Side/Adverse Effects Nursing Responsibilitie SimthebossОценок пока нет
- Compare Contrast IntroДокумент1 страницаCompare Contrast IntroAsma AlthawadiОценок пока нет
- Criteria BlablahДокумент5 страницCriteria BlablahimthebossОценок пока нет
- Deficient Fluid Volume R/T Inadequate Fluid Volume Intake Aeb Dry Mucous MembraneДокумент2 страницыDeficient Fluid Volume R/T Inadequate Fluid Volume Intake Aeb Dry Mucous MembraneimthebossОценок пока нет
- Prof Ad2Документ2 страницыProf Ad2imthebossОценок пока нет
- Management Process PlanningДокумент4 страницыManagement Process PlanningimthebossОценок пока нет
- Dengue FeverДокумент10 страницDengue FeverimthebossОценок пока нет
- CuesДокумент11 страницCuesimthebossОценок пока нет
- Atrial FibrillationДокумент1 страницаAtrial FibrillationimthebossОценок пока нет
- Abuse and Violence - OdtДокумент3 страницыAbuse and Violence - OdtimthebossОценок пока нет
- Course in The Ward Date/Time Doctor'S Order Rationale Nursing ResponsibilitiesДокумент3 страницыCourse in The Ward Date/Time Doctor'S Order Rationale Nursing ResponsibilitiesimthebossОценок пока нет
- Audience: Floor Plan: September 2, 2016 at Rooms 207 and 208Документ1 страницаAudience: Floor Plan: September 2, 2016 at Rooms 207 and 208imthebossОценок пока нет
- Score Sheets Copy 15Документ5 страницScore Sheets Copy 15imthebossОценок пока нет
- Master Score SheetДокумент6 страницMaster Score SheetimthebossОценок пока нет
- Drug Name General Action Specific Action Indication Contraindication Adverse Effects NSG Responsibilities Acetazolamide 250mg/tab 1 Tab Now Then TIDДокумент8 страницDrug Name General Action Specific Action Indication Contraindication Adverse Effects NSG Responsibilities Acetazolamide 250mg/tab 1 Tab Now Then TIDimthebossОценок пока нет
- Pathophysiology: Modifiable Non-ModifiableДокумент3 страницыPathophysiology: Modifiable Non-ModifiableimthebossОценок пока нет
- Physical Examination and Review of SystemДокумент10 страницPhysical Examination and Review of SystemimthebossОценок пока нет
- Physical Examination and Review of SystemДокумент10 страницPhysical Examination and Review of SystemimthebossОценок пока нет
- Fabi AnatomyДокумент4 страницыFabi AnatomyimthebossОценок пока нет
- Scope and LimitationДокумент1 страницаScope and LimitationimthebossОценок пока нет
- Nursing Health HistoryFINALLYДокумент6 страницNursing Health HistoryFINALLYimthebossОценок пока нет
- Cues Nursing Diagnosis Scientific Rationale Goals Nursing Intervention Rationales Evaluation Subjective CuesДокумент2 страницыCues Nursing Diagnosis Scientific Rationale Goals Nursing Intervention Rationales Evaluation Subjective CuesimthebossОценок пока нет
- Generic Name Action Indication Contraindication Adverse and Side Effect Nursing ConsiderationsДокумент2 страницыGeneric Name Action Indication Contraindication Adverse and Side Effect Nursing ConsiderationsimthebossОценок пока нет
- Diseases ListДокумент49 страницDiseases ListChandra Sekhar GajulaОценок пока нет
- Ogilvie SyndromeДокумент4 страницыOgilvie Syndromedrnareshkumar3281Оценок пока нет
- 8 Causes of Periumbilical Pain and When To Seek Emergency HelpДокумент8 страниц8 Causes of Periumbilical Pain and When To Seek Emergency HelpJohn Rodney PicaОценок пока нет
- Soal ArithmiaДокумент13 страницSoal Arithmiaeka rahmawatiОценок пока нет
- Immunization Poster LifespanДокумент1 страницаImmunization Poster Lifespanapi-533830260Оценок пока нет
- OB Hypertension in PregnancyДокумент5 страницOB Hypertension in PregnancyIsabel CastilloОценок пока нет
- Hypersensitivity Reaction/ AllergyДокумент23 страницыHypersensitivity Reaction/ AllergyCharity Grace MagnoОценок пока нет
- Clinical Practice Guidelines 11-18Документ20 страницClinical Practice Guidelines 11-18Feroz RaZa SoomrOoОценок пока нет
- Viral MeningitisДокумент4 страницыViral MeningitisLucky PuspitasariОценок пока нет
- Brochure RotavirusДокумент4 страницыBrochure RotavirusMaria Chacón CarbajalОценок пока нет
- Pediatrics - VaccinationsДокумент2 страницыPediatrics - VaccinationsJasmine Kang100% (1)
- Drugs Used To Treat AnemiaДокумент36 страницDrugs Used To Treat AnemiaMoxie Macado100% (1)
- Pareto Apotek NuhrintamaДокумент70 страницPareto Apotek NuhrintamaNur Insani JОценок пока нет
- Immunization During PregnancyДокумент7 страницImmunization During PregnancyNur SulistiyaningsihОценок пока нет
- 4RT Exam Mapeh 7Документ4 страницы4RT Exam Mapeh 7Marivic LabuacОценок пока нет
- DAY 2 Febrile Seizure Kuliah MHSДокумент45 страницDAY 2 Febrile Seizure Kuliah MHSAdhi WiratmaОценок пока нет
- Hemorrhoids - Causes, Treatments, and PreventionДокумент5 страницHemorrhoids - Causes, Treatments, and PreventionSAIFUL ISLAMОценок пока нет
- Fluticasone PropionateДокумент1 страницаFluticasone PropionateRPh Krishna Chandra JagritОценок пока нет
- ESIC Model Hospital - Ludhiana, PunjabДокумент8 страницESIC Model Hospital - Ludhiana, PunjabPushpinder Singh SandhuОценок пока нет
- Kti DMДокумент117 страницKti DMYudhis BamsОценок пока нет
- Dyspepsia GuidelinesДокумент3 страницыDyspepsia Guidelinesmeong_sweetОценок пока нет
- St. Paul College of Ilocos SurДокумент5 страницSt. Paul College of Ilocos SurCharina AubreyОценок пока нет