Академический Документы
Профессиональный Документы
Культура Документы
OSCE Respiratory Examination Guide
Загружено:
M CubedИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
OSCE Respiratory Examination Guide
Загружено:
M CubedАвторское право:
Доступные форматы
Respiratory Examination
Respiratory System Examination
Steps:
1. Set up
2. Introduction
3. General inspection
4. Inspection of hands and pulse
5. Inspection of eyes, nose and mouth
6. Inspection of neck with JVP
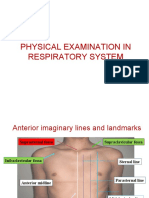
7. Closer Inspection of chest
8. Palpation of chest- Expansion, Apex Beat, Tactile Fremitus
9. Percussion of chest
10. Auscultation of chest
11. Closer inspection of back
12. Palpate of back
13. Percussion of back
14. Auscultation of back
15. Lymph node examination (optional thyroid examination)
16. Concluding exam and thank patient
17. Summary
Freenote OSCE Guide
Respiratory Examination
Freenote OSCE Guide
Respiratory Examination
Respiratory examination requires the patient to be seated at 45 degrees and exposed from
the the waist up. If this is not possible please indicate that these conditions are the ideal.
Before starting ensure you have a proper stethoscope with a bell and as usual a suitable
watch to check respiratory rate and possibly pulse. If possible sanitize hands before
beginning. A penlight and a tape measure are optional but recommended.
The main focus should be on proper technique as many unique procedures are required and
must be done systematically.
I.
* please note that this examination should include checking of JVP as well as lymph node
examination. These may saved for the end to ensure that time is not exceeded.
Start with introduction. Indicate intentions. Seek permission
- Good morning, My name is ________ and I'm a ________ year medical student. I have been
asked to perform a respiratory examination on you, it will basically involve me examining and
touching your chest area but will include other parts of your body. Is that okay with you sir/
madam?
II. Inquire persons name and age. ( Keep them in mind for the summary!)
- Could you please tell me you name sir/madam? And how old are you?
III. Ensure patient does not have any pain (this can be done later on before the person is touched)
- Do you have any pain anywhere? If you feel any pain as I examine you please let me know
IV. Stand by foot of the bed and begin general inspection:
A. Comment on general appearance (*begin pressing medial maleoli of ankles to save time when
checking for pedal edema later on)
1. Patient appears to be well
B. Comment on breathing. Indication breathlessness or respiratory distress if present. Indicate
movement of chest wall. Comment on abnormal breathing such as cough, wheeze or stridor.
Ideally respiratory rate must be checked but this may be done after checking pulse
1. Patient appears to be breathing comfortably without use of accessory muscle. No
presence of cough, wheezing or stridor.
2. Patient does not appear to be short of breath or in any respiratory distress
3. Patients chest wall seems to be moving symmetrically and together with breathing
C. Comment on patients color, checking for general cyanosis (indicate that it cannot be seen at
FOOT of bed)
1. At foot of bed patient does not seem to be cyanosed
D. Comment on any deformities of chest wall (you be general at this point and list specific
conditions on closer examination, just ensure that these conditions are stated). Abnormalities
include: obvious surgical scars, pectus carinatum, pectus excavatum, kyphosis and scoliosis
(better seen from behind), flailed chest or any recessions in chest. Also check for any vascular
anomalies.
2
Respiratory Examination
Freenote OSCE Guide
1. Examination of chest at foot of bed indicates no obvious surgical scars
2. No abnormal masses seen
3. No obvious chest wall deformities ( such as pectus carinatum, pectus excavatum. No
recessions in chest.)( No kyphosis or scoliosis) (No vascular anomalies seen)
E. Look around patient for signs of breathing apparatus or inhaler medication (*optional, more
important in hospital bedside setting)
1. No signs of breathing apparatus or inhaler.
F. Release hands and observe whether pedal edema is present
1. No signs of pedal edema
V. Approach patient and asks to see hands. Inspect both
1. Do you have any pain in your hands?
B. Begin by feeling palms. Indicate temperature. Note coloration or palms. Red palms, ie,
polycythemia, indicate patient is in a hypoxic state
1. Patients hands feel warm and moist
2. Palms are pink, no indication of hypoxia
C. Flip hand palm down. Check fingernails for tobacco tar staining. Check capillary refill and
check coloration of fingertips to see whether peripheral cyanosis is present.No signs of tar
staining
1. Capillary refill appears normal, no signs of peripheral cyanosis
VI. Check for clubbing. Some sources indicate checking for nail bed angle followed by Schamroth's
Window (nail angle diamond) as well as checking for nail fl is sufficient, if these are absent, then
the other tests are redundant as they check for later signs of clubbing. All tests are listed.
ENSURE YOU CHECK FOR VISUAL SIGNS AT EYE LEVEL.
A. Look across nail bed at nail bed for presence of nail bed angle at eye level
B. Ask patients to make a diamond with finger to view Schamroth's Window. Also to check
presence of nail bed angle. Also check at eye level.
C. Check for increased nail bed fluctuation. Place thumbs below patient finger. Place middle
fingers above patients finger at joint of the distal phalanx. use index fingers on either side of
nail bed to check for fluctuation
D. If the sign of early stages of clubbing are present, comment on presence of signs of later
stages(Check for increased curvature of nail)(Check for drumstick appearance)
1. Nail bed angle maintained. No signs of finger clubbing
2. No nail fluctuation
Respiratory Examination
Freenote OSCE Guide
VII. Check for tremor.
A. Ask patient to straighten hands in front of them and cock back their wrists whist
demonstrating the movement and ask them to keep their hands still as best as they can.
Flapping tremor aka asterixis is the most important and indicates CO2 retention, however, a
fine finger tremor may be seen in patients who use beta agonists such as asthmatics
1. Could you please stick out your arms like this and then tilt back your wrists like this?
2. No signs of asterixis/flapping tremor or fine tremor seen.
VIII. Check radial pulse, (radio-radial delay may be checked). If respiratory rate was not checked prior
to this point, do so now.
1. Patient has a pulse of ______. Rhythm and volume seem normal.
2. (Said before checking RR) please relax and breath normally.
3. Patient has a respiratory rate of _______.
IX. Check eyes of patient. Pull skin beneath eyelids down to check mucous membranes for signs of
anemia. Scleral icterus may also checked, however, this is not usually a part of respiratory
examination.
1. Mucous membranes are pink and moist, no signs of anemia
X. Ask patient to tilt back chin. View up nostrils, checking for the presence of polyps or nasal septal
deviation. (Penlight may be used to improve view). This step is not asked by all examiners but
may be deemed important by some.
1. Please tilt your chin back
2. No sign of nasal polyps or septal deviation
XI. At the neck there are two important steps that may be left for last to save time. They are testing
the JVP and palpation of lymph nodes and thyroid. JVP will be included here but neck palpation is
recommended at the end as access to the neck from behind is easier after examining the back.
A. Check JVP by asking patient to tilt head in the opposite direction.
1. Could you please tilt your head in that direction.
B. Get to eye level ( bend knees if necessary) with the patient's neck and view carefully along
the anterior border of the SCM looking for a pulsation. It can be distinguished from the carotid
pulse as it is not palpable. If it is not clearly seen, inform the patient and push down their
abdomen, to elicit hepatojugular reflex which should cause the JVP to become more
prominent.
C. Place ruler/tape measure vertically upward from sternal angle. Determine vertical distance of
JVP from sternal angle. Greater then 4cm indicates raised JVP, ie, increased pressure in right
side of heart, a sign of pulmonary edema or embolism.
1. JVP less than 4cm vertically from sternal angle. No sign or increased pressure in right side
of heart.
Respiratory Examination
Freenote OSCE Guide
XII. Check for tracheal deviation. Inform patient that the procedure is uncomfortable. Place ring finger
and index finder on the bony prominences of the medial ends of the clavicle. Then use middle
finger to palpate the trachea and along its sides.
1. Im going to feel your neck, it may feel uncomfortable. Is that alright?
2. The patients trachea lies along the midline and does not appear to be deviated
XIII.Conduct closer inspection of chest. Ask patient to breath deeply once and observe chest
A. If conditions were not listed at foot of the bed fill them in now
1. On closer inspection of chest, findings were consistent with those seen at the foot of the
bed.
B. Now that the chest can be viewed from the side, the presence of barrel chest is more easily
seen. Inspect the antero-posterior diameter and picture cross-section of the chest. Ideally it
should be elliptical. Circular cross section indicate barrel-chest, which is a sign of Air trapping,
eg, in COPD.
1. The cross section of the patients chest appears to have a normal elliptical shape.
C. Ask patient to life arms and check lateral wall for signs of laproscopy scars
1. No signs of surgical scars on the lateral walls of the chest
XIV. Before proceeding to palpate the chest Remind the patient you are going to touch their chest
and that when you give the indication you need them to breath in and out. Palpation has three
important aspects: chest expansion, vocal fremitus and localisation of apex beat
1. I'm going to touch your chest now. When I say "in" I'll need you to breath in as deeply as
you can and when i say "out" I'll need you to breath out as much as you can. is that okay with
you?
A. Chest expansion- place palms on the patients chest so that thumbs point at midline but fingers
cup the lateral sides of the chest. Ask patient to breath out as deeply as they can and pull rib
cage in as much as possible, whilst slide thumbs toward midline. This is to ensure the ribcage
is close to the lung, so that if it expands, your hands will be forced apart. Ask patient to breath
in deeply. Note whether the chest wall is expanding symmetrically in the lateral plane.
B. Chest expansion cont'd- to check for vertical expansion symmetry of the lungs place hands on
the patients chest so that your fingers are parallel to each other and your middle finger is right
below the clavicle, pointing upward. Allow tips of thumbs to touch. This helps compare both
sides. Once again ask the patient to breath out deeply and then breath in.
1. Chest wall expansion was found to be symmetrical
C. Apex Beat- place both hands on either side of chest to ensure beat is on the left. Once this is
established, adjust hand placement until the exact spot where the beat is greatest is found.
Leave finger in this position. Use other hand to find second intercoastal space at sternal
angles lateral border. Then palpate downwards using the ribs as markers to indicate which
ICS you are palpate. Go down until you are lateral to your apex beat marking finger and
palpate across until your fingers meet to ensure point lies in the same ICS. Note how lateral
Respiratory Examination
Freenote OSCE Guide
the beat is as well. It should normally lie at the 5th intercoastal space and the mid-clavicular
line.
1. Apex beat was found to be within the LEFT side at the 5th intercoastal space along the
mid-clavicular line.
D. Vocal fremitus- instruct the patient to say "99" when your hand is touching them. Start at the
top right of the chest and place the ulnar border of your hand into the 2nd ICS at least 2cm
away from the midline. Note the feeling of vibration as the patient speaks. Then place your
hand on the other side at the reflection oft he first position. Compare the vibration and note
whether they are different. Move your hand a few cm downwards and repeat process 6
postions total have been checked. The last position should not be lower than the
xiphisternum. Ask patient to raise arms to allow access to their sides and then repeat the
procedure at 6 positions along the lateral chest wall.
1. Each time i place my hand on you, please clearly say the words "99"
2. Vocal fremitus is symmetrical at each position tested on the patient.
XV. Percuss, first the apices of the lung. This can be done on the clavicle, however, some tutors state
that this is painful for the patient and do not advise it. Percussing in the supraclavicular notches is
recommended but is a bit tricky. Practice can improve this. After the apices, percuss the chest in
the same 12 spots (6 in front, 3 on each side) that were checked for fremitus. REMEMBER that
the intercoastal SPACES must be percussed and make to a point to demonstrate to your
examiner you have placed you finger correctly. Also ensure that you COMPARE SIDES, ie, after
checking one spot, always move ACROSS to the other side, NOT downwards. Only move down,
once both sides have been checked. This is also true for percussion of the lateral aspect of the
chest.
1. Percussion of lungs reveals them to be resonant and symmetrical
XVI. Turn Stethoscope to bell side. Place once on either side of chest, ensuring it is placed at least 5
cm away from the midline to ensure breath sounds are from lung filling and not passage of air
through trachea. Instruct the patient to breath deeply. Auscultate the apices as well as multiple (at
least 6) places on the anterior chest and 3 places on each side of the patient. Listen carefully for
signs of wheeze.
1. Please breath in/out deeply
2. No abnormal breath sounds heard
A. *Note that there are two ways of checking fremitus. The first was done using the ulnar border
of hand. However, it can also be checked using a stethoscope instead. Though some tutors
advise executing both to demostrate you are familiar with the technique. However, if you are
short on time, this is not recommended as it is redundant. Auscultate the same areas once
more. This time asking patient to say "99" each time you place the stethoscope on them
1. Vocal fremitus is symmetrical and sounds normal
XVII.Instruct patient to sit up.
A. Then instruct and demonstrate that they should "hug" themselves to retract the scapula
enough to allow access to ribcage.
1. Please sit up. Wrap your arms around yourself like this please
6
Respiratory Examination
Freenote OSCE Guide
B. Inspect back for surgical scars or abnormalities including scoliosis or kyphosis
1. On inspection of the back, no signs of any surgical scars, abnormal masses or spine
deformities such as scoliosis and kyphosis
C. Proceed to check chest expansion by place hands on back similarly to before, however,
movement of your hands apart from each other is expected during expiration rather than
inspiration (*this step is recommended by some tutors but deemed redundant by others. If
chest expansion is normal anteriorly, abnormal expansion from behind is unlikely. Step
included simply for the sake of completion)
1. Could you please inhale as deeply as you can. Now exhale
2.
chest expansion is symmetrical
D. Check fremitus similarly to how it was done in the front at 6 positions in ICS. Ensure you
remind patient to say the words "99".
1. Once again, could you please say "99" when you feel my hand rest on your back.
E. Percuss back in a similar fashion as before on 6 spots. Once again keep in mind to find the
ICS.
1. Percussion of lungs reveals that they are also resonant posteriorly.
F. Auscultate the back of the rib cage. Once again keeping 5 cm away from the midline and
asking the patient to breath deeply. Check at least 6 spots
1. Please breath deeply
2. No abnormal breath sounds heard
XVIII.At this point, if Checking of JVP and/or lymph nodes has not been completed, do so now. If time
has been exceeded, at least inform the examiner that ideally you would have done them. It is
recommended that you save lymph node exam for this point as the nodes as more accessible
from the back of the patient. The steps are as follows
A. Instruct the patient that you are going to check their lymph nodes in their neck region. Let
them know that it may be uncomfortable. Instruct them to lift their chin up to allow access. It is
highly recommended that you speak to you patient while palpating as you are standing behind
them and silence during this is awkward and uncomfortable for the patient.
1. Now I'm going to check your lymph nodes which are in your neck. It may feel a bit
uncomfortable but will not take long. Please tilt you chin up for me
B. Start below the tip and mandible and palpate back along the chin until you reach the angle.
Palpate along the anterior of the SCM from top to bottom. Then palpate along the posterior of
the SCM from bottom to top. Palpate from the mastoid to the back of the ear. Palpate above
the ear and in front of the ear. Palpate along the back of the head from the occiput
downwards.
1. * speak to the patient throughout. Simply telling them that they are doing well and that your
are almost finished
2. Lymph nodes in neck were not palpable
Respiratory Examination
Freenote OSCE Guide
XIX.State that ideally you would like to conduct a peak expiratory flow test.
1. Ideally, i would like to conduct a peak expiratory flow test or spirometry to complete
examination
XX.THANK PATIENT. Some tutors look for signs such as shaking the patients hand and maintaining
eye contact when speaking to patient as signs of good rapport. Cover patient!
A. Thank you very much Mr./Mrs. ______. You've done very well.
XXI.If requested and time is adequate, give summary of findings to examiner. Don't be too specific
and just state the general findings each test has given you.
A. On examination, we have a well looking ____ year old male/female patient, breathing normally
and in no signs of respiratory distress. No surgical scars or abnormalities of any kind were
seen on inspection. Respiratory rate and pulse were normal. No signs of hypoxia or cyanosis.
Chest walls moves symmetrically with breathing. Lungs were found to be resonant with no
abnormal conduction of sound. Breath sounds were normal. In summary findings indicative of
a normal respiratory examination.
Вам также может понравиться
- Respiratory Examination OSCE GuideДокумент14 страницRespiratory Examination OSCE GuideSam James100% (1)
- Essential Examination, third edition: Step-by-step guides to clinical examination scenarios with practical tips and key facts for OSCEsОт EverandEssential Examination, third edition: Step-by-step guides to clinical examination scenarios with practical tips and key facts for OSCEsРейтинг: 3 из 5 звезд3/5 (5)
- Osce Abdominal ExaminationДокумент1 страницаOsce Abdominal ExaminationNairobipaeds Madakitari WatotoОценок пока нет
- Cardiology - CVS OSCE ChecklistДокумент5 страницCardiology - CVS OSCE ChecklistPraveenaОценок пока нет
- General Rules of Abdomenal ExaminationДокумент22 страницыGeneral Rules of Abdomenal ExaminationSamuel Sebastian SirapanjiОценок пока нет
- Thyroid Exam OSCEДокумент4 страницыThyroid Exam OSCEJon Mark LimОценок пока нет
- Abdominal Exam 2020Документ6 страницAbdominal Exam 2020InhoОценок пока нет
- Osce ChecklistДокумент11 страницOsce Checklistgemgem06Оценок пока нет
- Physical ExaminationДокумент10 страницPhysical ExaminationChristine NaОценок пока нет
- PD OSCE GuideДокумент19 страницPD OSCE GuideChorong ParkОценок пока нет
- Approach To Heart MurmursДокумент57 страницApproach To Heart MurmursRadley Jed PelagioОценок пока нет
- Theme 4 - HTN in The OSCEДокумент1 страницаTheme 4 - HTN in The OSCEShannon RamsumairОценок пока нет
- OSCE SkillsДокумент9 страницOSCE SkillsgoodbyethereОценок пока нет
- August - September - 2002 Osce Stations MelbourneДокумент12 страницAugust - September - 2002 Osce Stations Melbournemnigam64Оценок пока нет
- pGALS Examination OSCE GuideДокумент18 страницpGALS Examination OSCE GuideFanny PritaningrumОценок пока нет
- OSCE Skills 2013 1Документ141 страницаOSCE Skills 2013 1Haseeb RayhanОценок пока нет
- LMCC Part 2 - Shoulder ExamДокумент6 страницLMCC Part 2 - Shoulder Exampsandrew1_88338763Оценок пока нет
- Medicine: CardiorespiratoryДокумент56 страницMedicine: CardiorespiratoryWalaa abo foolОценок пока нет
- CardiologyДокумент6 страницCardiologyFrancis FransОценок пока нет
- Typhon Cases 2Документ7 страницTyphon Cases 2api-483865455Оценок пока нет
- Congenital Heart Defects Test Five Nursing FourДокумент6 страницCongenital Heart Defects Test Five Nursing FourTiffany D'Alessandro GordonОценок пока нет
- Cardiology A. Woo PDFДокумент52 страницыCardiology A. Woo PDFiuliОценок пока нет
- Cardiovascular Examination - OSCE Guide - Geeky MedicsДокумент6 страницCardiovascular Examination - OSCE Guide - Geeky MedicsJahangir AlamОценок пока нет
- History and Physical Exam GuidelinesДокумент5 страницHistory and Physical Exam GuidelinesPrincella MonicaОценок пока нет
- Cardiovascular Examination Checklist OSCEДокумент1 страницаCardiovascular Examination Checklist OSCESteve TanОценок пока нет
- Common Histories and Red Flags Presentation Noninteractive VersionДокумент21 страницаCommon Histories and Red Flags Presentation Noninteractive VersionesmarОценок пока нет
- A Clinical Approach To SyncopeДокумент8 страницA Clinical Approach To Syncopepuskesmas tarik100% (1)
- History Taking: DR - Ahmed Gaber Ass. Prof of Neurology Ain Shams UniversityДокумент81 страницаHistory Taking: DR - Ahmed Gaber Ass. Prof of Neurology Ain Shams UniversityKhaled OssamaОценок пока нет
- Cardiovascular History Taking - Geeky MedicsДокумент6 страницCardiovascular History Taking - Geeky MedicsJahangir AlamОценок пока нет
- OSCE Note 1Документ2 страницыOSCE Note 1Presley Omorodion100% (1)
- Bates Physical Exam Video NotesДокумент3 страницыBates Physical Exam Video Notesdulcedeleche12359Оценок пока нет
- OSCE Marksheet 1Документ7 страницOSCE Marksheet 1Elias PetrouОценок пока нет
- HPI For History and Physical ExamДокумент2 страницыHPI For History and Physical Examv-santОценок пока нет
- Radiological Chest SignsДокумент15 страницRadiological Chest SignsEzekiel ArtetaОценок пока нет
- Community MedicineДокумент77 страницCommunity MedicineSharon DanielОценок пока нет
- HB PT Osce SPДокумент10 страницHB PT Osce SPAli NofalОценок пока нет
- JVP - WL GanДокумент1 страницаJVP - WL GanWeh Loong GanОценок пока нет
- 02 The Abdominal Exam Lab - CopДокумент6 страниц02 The Abdominal Exam Lab - CopBhumiShahОценок пока нет
- Paediatrics OSCE BookletДокумент3 страницыPaediatrics OSCE BookletJohn TangОценок пока нет
- Musculoskeletal Assessment: (10 Digit Number)Документ5 страницMusculoskeletal Assessment: (10 Digit Number)David Gomes0% (1)
- Past Years OSCE Answers - 2012Документ30 страницPast Years OSCE Answers - 2012christietwongОценок пока нет
- Congenital Heart DiseasesДокумент6 страницCongenital Heart Diseasestheglobalnursing100% (2)
- OSCE Station SampleДокумент7 страницOSCE Station Sampledragon6650% (2)
- List of OSCE Neurology StationsДокумент10 страницList of OSCE Neurology StationsHamo Refaat100% (1)
- Physical Examination in Respiratory SystemДокумент58 страницPhysical Examination in Respiratory SystemMarian0% (1)
- OSCE - Chest PainДокумент2 страницыOSCE - Chest PaincgalongОценок пока нет
- History Taking OSCE Example 4Документ6 страницHistory Taking OSCE Example 4worlddoctor2012Оценок пока нет
- Pulmonary Function TestДокумент77 страницPulmonary Function TestMohammed Saad NabhanОценок пока нет
- Osce Revision Questions 2017Документ21 страницаOsce Revision Questions 2017Leong Tung OngОценок пока нет
- Clinical Log 111713Документ3 страницыClinical Log 111713api-242065432Оценок пока нет
- Ace The OSCE2 BookДокумент126 страницAce The OSCE2 BookalexОценок пока нет
- Bates Physical Examination RED NOTESДокумент2 страницыBates Physical Examination RED NOTESAmanda Gomez100% (1)
- The OSCE OrientationДокумент25 страницThe OSCE OrientationginadaisluОценок пока нет
- Classic Radiology SignsДокумент9 страницClassic Radiology SignsJui DirDapОценок пока нет
- Cardio-Physiology Exam QuestionsДокумент17 страницCardio-Physiology Exam Questionsjimmy100% (2)
- Achieving Excellence in The OSCE Part 2Документ465 страницAchieving Excellence in The OSCE Part 2Sultan AlexandruОценок пока нет
- Shoulder Examination Mark SchemeДокумент1 страницаShoulder Examination Mark Schemegus_lionsОценок пока нет
- Case Report - CC - Uraemic EncephalopathyДокумент11 страницCase Report - CC - Uraemic EncephalopathyM CubedОценок пока нет
- Differential Diagnosis List For Various ConditionsДокумент45 страницDifferential Diagnosis List For Various ConditionsM CubedОценок пока нет
- Pure Mathematics Specimen Paper U1 Paper 03-BДокумент5 страницPure Mathematics Specimen Paper U1 Paper 03-BM CubedОценок пока нет
- Specimen Paper Unit 1 Paper 02Документ6 страницSpecimen Paper Unit 1 Paper 02M CubedОценок пока нет
- CAPE Chemistry Syllabus - CompleteДокумент74 страницыCAPE Chemistry Syllabus - CompleteM Cubed100% (2)
- 99 NazdirusДокумент4 страницы99 NazdirusJay-King Tut Guy100% (2)
- Reading ComprehensionДокумент2 страницыReading ComprehensioncameliaОценок пока нет
- картки для читанняДокумент12 страницкартки для читанняОксана ХмільОценок пока нет
- Fear by H. E. BatesДокумент9 страницFear by H. E. BatesMont Sumthing100% (1)
- Sol2e ELEM Progress Test 5BДокумент4 страницыSol2e ELEM Progress Test 5BMihaela DrimbareanuОценок пока нет
- Bubblehe PDFДокумент3 страницыBubblehe PDFHenny Kim100% (1)
- Alter Self UsesДокумент3 страницыAlter Self UsesMiguel ColodroОценок пока нет
- Australian Goat Manual For Malaysian Farmers: A Guide To Successful Goat Production From Australian Goats in MalaysiaДокумент56 страницAustralian Goat Manual For Malaysian Farmers: A Guide To Successful Goat Production From Australian Goats in MalaysiaAsuranОценок пока нет
- Ancient Civilizations DBQДокумент6 страницAncient Civilizations DBQapi-327647329Оценок пока нет
- Thilatharpanapuri or Adhi Vinayakar Temple - Temples of TamilnaduДокумент3 страницыThilatharpanapuri or Adhi Vinayakar Temple - Temples of TamilnadusureshОценок пока нет
- W S The Lost CamelДокумент3 страницыW S The Lost CamelSammy SamОценок пока нет
- Careers in Agriculture (1) - 3Документ50 страницCareers in Agriculture (1) - 3keronОценок пока нет
- Ectoparasites of ReptilesДокумент8 страницEctoparasites of ReptilesJohnLyndonLunnayОценок пока нет
- VillageworksheetДокумент3 страницыVillageworksheetapi-239157948Оценок пока нет
- Picture Index: Adams, Jim Boudias, ChristopheДокумент6 страницPicture Index: Adams, Jim Boudias, ChristopheHữu TríОценок пока нет
- TissueДокумент54 страницыTissueNicole EncinaresОценок пока нет
- Extra Photocopiable Material 1 Final Assessment: Unit 1 Unit 4Документ2 страницыExtra Photocopiable Material 1 Final Assessment: Unit 1 Unit 4Constanza Rojas BurgosОценок пока нет
- Personality and Individual Differences: J. Philippe Rushton, Donald I. TemplerДокумент5 страницPersonality and Individual Differences: J. Philippe Rushton, Donald I. TemplerYmeОценок пока нет
- Maciocia Patterns - Review 1Документ91 страницаMaciocia Patterns - Review 1keiraku100% (4)
- Romania Fact SheetДокумент2 страницыRomania Fact SheetEmeseDengОценок пока нет
- JSR 43-3 Book Reviews PDFДокумент4 страницыJSR 43-3 Book Reviews PDFmargaridasolizОценок пока нет
- Dna Genetics Test 7thgradeДокумент7 страницDna Genetics Test 7thgradeCorradОценок пока нет
- Body Condition of Dairy Cows PDFДокумент44 страницыBody Condition of Dairy Cows PDFfranky100% (1)
- Dragon Monk PDFДокумент1 страницаDragon Monk PDFfishguts4ever100% (1)
- Pub - Colin Wilson Spider World 01 The DesertДокумент148 страницPub - Colin Wilson Spider World 01 The DesertAlex ZavyalovaОценок пока нет
- Grade 4, Prompt For Opinion Writing: Common Core Standard W.CCR.1Документ5 страницGrade 4, Prompt For Opinion Writing: Common Core Standard W.CCR.1Daniela CorneciОценок пока нет
- Bricks Reading 150 - 2 Review Test 1: (1-5) Write The Correct Word For Each SentenceДокумент4 страницыBricks Reading 150 - 2 Review Test 1: (1-5) Write The Correct Word For Each SentenceMichael Christopher Calderon EscanoОценок пока нет
- Quantock HillsДокумент2 страницыQuantock HillsMurray DickensОценок пока нет
- Worksheet 2 Semester 2-1Документ2 страницыWorksheet 2 Semester 2-1Setya AptasariОценок пока нет
- Chemistry Project Part 1 Caseins in Milk.....Документ38 страницChemistry Project Part 1 Caseins in Milk.....prem malviОценок пока нет