Академический Документы
Профессиональный Документы
Культура Документы
Pediatric Hematology Oncology Ward Officer Handbook
Загружено:
Anonymous FSUnLYr4yАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Pediatric Hematology Oncology Ward Officer Handbook
Загружено:
Anonymous FSUnLYr4yАвторское право:
Доступные форматы
Paediatric Haematology/Oncology
Ward Officers
Handbook
Texas Childrens Cancer Center
&
Hematology Service
International Program
Editor: Parth S. Mehta, MD
Assistant Professor of Pediatrics
Baylor International Pediatric AIDS Initiative at Texas Childrens Hospital
Baylor College of Medicine
Texas Childrens Hospital
Houston, Texas USA
Baylor College of Medicine 2010
Paediatric Haematology/Oncology Ward Officers Handbook
Baylor College of Medicine 2010
Paediatric Haematology/Oncology Ward Officers Handbook
General
1. Pain control
2. Blood transfusion therapy
3. Transfusion reactions
4. Intravenous fluids, central lines & useful formulas
Oncology
1. Neutropenia
2. Fever & neutropenia
3. Anti-Fungal Therapy
4. Antiviral Therapy
5. Pneumocystis jerovecii (PCP) Prophylaxis
6. Anti-emetic Medications
7. Anaphylaxis Precautions
9. Oncologic Emergencies
10. Immunizations in Oncology Patients
11. Constipation
Hematology
1. Sickle cell disease
2. Sickle cell disease with fever
3. Sickle cell vaso-occlusive crisis
4. Pre-operative preparation of sickle cell patients
5. Transfusion therapy in sickle cell disease
7. Treatment of bleeding in patients with Hemophilia A
8. Treatment of bleeding in patients with Hemophilia B
9. Von Willebrands Disease
10. Immune Thrombocytopenic Purpura (ITP)
References
4
4
4
7
8
9
9
10
12
14
14
16
18
21
24
24
26
26
27
28
29
30
31
33
35
36
40
Baylor College of Medicine 2010
Paediatric Haematology/Oncology Ward Officers Handbook
General
1. Pain control
Intravenous medications
Morphine sulfate 0.1 - 0.2 mg/kg/dose every 2-4 hrs (Max single dose 15 mg)
Oral medications
Ibuprofen 10 mg/kg/dose every 6-8 hours (Max single dose 800 mg, 2400
mg/day)
Avoid this medication in patients with thrombocytopenia
GastrointestinaI prophylaxis with ranitidine recommended
Ranitidine 2-4 mg/kg/dose twice daily
Oral morphine sulfate
0.3 to 0.6 mg/kg/dose every 4-6 hrs
Intravenous (IV) to oral (PO) dosing conversion is 1:3; 1 mg IV is equivalent
to 3 mg PO
Different formulations exist including sustained release & immediate release; refer to prescribing information contained within medication packaging
2. Blood transfusion therapy
Infection risk of blood transfusion estimates
National transfusion centers ought to have more accurate incidence figures for
each setting
Incidence estimates taken from Transfusion 2002; 42:975-79
HIV 1:2,135,000
Hepatitis B 1:220,000
Hepatitis C 1:1,935,000
Bacterial contamination 1:2,000 platelet units
General Guidelines for Transfusion Therapy
Prior to initial transfusion, HIV & Hepatitis B & C screening is recommended
Premedication
Baylor College of Medicine 2010
Paediatric Haematology/Oncology Ward Officers Handbook
Used in patients with a history of prior allergic or febrile transfusion reaction
One or more of these medications can be used:
Paracetomol 15 mg/kg PO (Max dose 1000 mg)
Diphenhydramine 0.5 mg/kg (Max dose 50 mg)
Hydrocortisone 2 mg/kg (Max dose 100 mg)
Packed Red Blood Cell (pRBC) transfusion
Transfuse 10-15 ml/kg pRBC over 2-4 hours
Response varies depending on concentration of unit, but expect 2-3 g/dL
rise in hemoglobin for each 10-15 ml/kg transfusion given
Patients with long-standing anemia due to iron deficiency can often be managed without transfusion therapy
Pre- & post-transfusion diuretic therapy with furosemide is not routinely
recommended and should be given only if the clinical condition warrants it
(e.g. cardiac dysfunction)
Whole blood is frequently used where pRBC are not available. To achieve a
similar rise as noted above in hemoglobin, transfuse 20 ml/kg whole blood over
2-4 hours
Platelet transfusion
Dosing of transfusion volume
< 8 kg - give one unit (5 ml/kg)
> 8 kg - give one random unit/10 kg body weight
Maximum - 6 random donor units or 1 pheresis unit (where available)
1 single pheresis unit is equivalent to 6 random donor units
3
Expect increase in platelet count by 50,000/mm with above guidelines
If there is concern for poor response check platelet count from 10-60 minutes post-transfusion to assess response
Cautions
Contraindicated in patients with Thrombotic Thrombocytopenic Purpura
(TTP) and Heparin-Induced Thrombocytopenia (HIT)
No benefit in patients with Idiopathic thrombocytopenia purpura (ITP)
unless there is life-threatening bleeding
Baylor College of Medicine 2010
Paediatric Haematology/Oncology Ward Officers Handbook
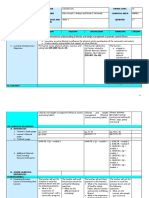
Platelet count (/mm3)
Transfusion Strategy
< 10,000
High risk for bleeding; transfusion likely indicated except in ITP without life-threatening
bleeding (see ITP section)
10,000 - 20,000
Transfusion likely needed if patient has infection, coagulopathy, splenomegaly, or bleeding
20,000 - 50,000
Transfusion for active bleeding, patients with
brain tumor, or for invasive procedures. Stable
patients rarely ever require transfusion
> 50,000
Transfusion only if there is an underlying platelet dysfunction or there is significant bleeding
Baylor College of Medicine 2010
Paediatric Haematology/Oncology Ward Officers Handbook
Plasma Transfusion
Indications for Fresh Frozen Plasma (FFP) use:
Massive transfusion of pRBC (greater than one blood volume within 24
hours)
Active bleeding or surgery in patient with prolonged Prothrombin Time
(PT) and/or activated partial thromboplastin time (aPTT) secondary to
factor deficiency for which specific factor replacement is not available
Dosing of Plasma
1 unit contains 200-250 ml
FFP contains 1 unit/mL of coagulation factors
10-15 ml/kg will result in 15-20% rise in factor level
Factor V & Factor VII may be exceptions as the former is labile & the
latter has a short half-life
3. Transfusion reactions
Signs & symptoms of transfusion reactions are varied, and can include any or all of
the following:
Chills & fever
Hemoglobinuria
Urticaria
Chest/spine pain
Shortness of breath
Anxiety or restlessness
Hypotension
Management of transfusion reaction
Stop transfusion, change IV tubing, flush line & start normal saline (NS) at 1600
ml/m2/day
If febrile or urticarial reaction give:
Diphenhydramine 1 mg/kg PO (Max dose 50 mg)
Paracetomol 15 mg/kg PO (Max dose 1000 mg)
Hydrocortisone 2 mg/kg IV (Max dose 100 mg)
In patients with anaphylaxis adrenaline should be given:
Adrenaline 1:1000, give 0.01 mL/kg IV
Adrenaline 1:10,000, give 0.1 mL/kg IV
Once patient is stable, consider transfusion of additional products unless patient experienced hemolytic reaction, in such a case, discuss with specialist first
Baylor College of Medicine 2010
Paediatric Haematology/Oncology Ward Officers Handbook
Patients with a history of transfusion reactions can be given pre-medication with
diphenhydramine, paracetomol, and hydrocortisone - doses noted above
If patient experiences only mild urticaria, give diphenhydramine & if symptoms
resolve, continue transfusion slowly
4. Intravenous fluids, central lines & useful formulas
2
Maintenance IV fluid rate - 1600 ml/m /day
Body surface area forumla:
square root (weight [kg] x height [cm] / 3600
Total Blood Volume (TBV)
Premature neonate:
Term neonate:
1 - 4 months age:
> 4 months age:
100 ml/kg
85 ml/kg
75 ml/kg
70 ml/kg
Plama Volume (PV)
TBV x (1-Hct)
Factor VIII Replacement
1 unit/kg raises level by 2%
In anemic patients: dose Factor VIII = (desired level - current level) x PV
Factor IX Replacement
1 unit/kg raises level by 1%
In anemic patients: dose Factor IX = (desired level - current level) x PV x 2
Central Lines: while frequently unavailable in the resource-limited setting, these do
come into use at times & sterile technique must be used in handling them
Hickman/Broviac
Flush lumens daily
Heparin 300 units in 5 ml NS
Dressing change twice per week
Port-a-Cath
Flush once per month
Heparin 500 units in 5 ml NS
Change dressing twice weekly while in use
Baylor College of Medicine 2010
Paediatric Haematology/Oncology Ward Officers Handbook
When central lines are in use, it is imperative to have anti-pseudomonal antibiotics such as piperacillin/tazobactam or ceftazidime if these patients are to
receive chemotherapy as pseudomonal line infections are more common & lifethreatening. These antibiotics also provide coverage of S. viridans, and therefore ciprofloxacin, while providing Pseudomonas coverage is not a suitable
substitute.
Central lines should only be used if adequate skill in caring for them is available, otherwise they present a greater risk than benefit
Oncology
1. Neutropenia
Neutropenia is defined as a decrease in Absolute Neutrophil Count (ANC):
ANC < 1500
Mild Neutropenia
ANC < 1000
Moderate Neutropenia
ANC < 500
Severe Neutropenia
ANC = total WBC * (% neutrophils + % bands)
Patients with neutropenia are at higher risk for serious infection and therefore:
No suppositories or enemas with oncologist approval
No rectal temperature or exam
No incision & drainage of lesions without oncologist approval
No NG tube, urine catheter, or LP without oncologist approval
Prior to blood work or IV, area should be prepped with betadine
Baylor College of Medicine 2010
Paediatric Haematology/Oncology Ward Officers Handbook
2. Fever & neutropenia
1. Assessment
Patients should be assessed immediately upon arrival to the clinic/emergency center, and antibiotic therapy instituted immediately after
obtaining blood work.
2. Work Up
Complete physical exam including visual perianal exam remembering
that physical signs of infection may be subtle in the neutropenic patient.
Full Blood Count (FBC), Blood Culture
Obtain according to the presence of symptoms other than fever:
Renal Function Tests (RFT), urinalysis (UA), urine culture, Chest xray (CXR), stool, and throat cultures
3. Therapy
Monotherapy: Patients meeting the following criteria may be placed on
monotherapy with cefotaxime:
All patients EXCEPT those with infant Acute lymphocytic leukemia (ALL), acute mylogenous leukemia (AML), aplastic anemia
and bone marrow transplant
Normal vital signs
No chills
No localizing symptoms or findings on physical exam
Cefotaxime dosing:
1 month 12 years: 50 mg/kg/dose IV q 8 hours
adults: 1-2 gm IV q 8 hours
(Max. Dose: 2 gm/dose)
Baylor College of Medicine 2010
10
Paediatric Haematology/Oncology Ward Officers Handbook
Multiagent therapy:
Patients not eligible for monotherapy should be started on one of
the following drug combinations:
If isolated fever and neutropenia without evidence of cardiovascular compromise or specific PE findings, and patient not allergic to
the drugs:
Gentamicin: infants/children: 2-2.5 mg/kg/dose IV q 8 hrs
(Max Initial Dose: 120 mg/dose)
Cefotaxime: 1 month 12 years: 75 mg/kg/dose every 8 hrs
adults: 2 gm IV q6 hours
Vancomycin can be added where clinically indicated (e.g. persistent
fever despite 48 hrs antibiotics)
Vancomycin dosing: children: 10-15 mg/kg/dose IV q6 hrs
(Max Dose: 500 mg/dose)
adults: 1 gm IVq 12 hrs or 750 mg IV q 8
hrs (Max Dose: 2 gm/day)
4. Other Considerations:
When using aminoglycosides and/or vancomycin monitor BUN, Cr at initiation then twice weekly as these agents are nephrotoxic. Where available, drugs levels can be obtained in therapy will continue for more than 3
days with either agent.
All toxic appearing patients should be treated with a three-drug combination such as vancomycin, cefotaxime and gentamicin.
Patients with specific infectious concerns such as interstitial pneumonitis
or acute abdomen should have antibiotic selections modified as the clinical situation warrants.
If the patient has a positive blood culture, daily cultures should be ordered and continued until negative x 3. Orders should also state to rotate
lumens for antibiotic infusion in patients with central lines.
Baylor College of Medicine 2010
11
Paediatric Haematology/Oncology Ward Officers Handbook
Where indwelling central lines (e.g. Broviac or Port-a-Cath) are available
& used, ready access to anti-pseudomonal antibiotics must be assured.
These agents include piperacillin/tazobactam, ticarcillin/clavulanic acid,
and ceftazidime. Without these medications, surgically placed central
lines should be used only with due regard to the risk incurred.
3. Anti-Fungal Therapy
Consider in the persistently febrile patient with negative cultures, or the patient
with fever who has been neutropenic for greater than five days.
Nystatin
used for thrush
infants 1 mL applied to each side of the mouth four times per day
children and adults 5 mL PO four times per day swish and swallow
Fluconazole
used for prophylaxis in AML and for the treatment of candidiasis
monitor liver function tests (AST/ALT q 2-3 weeks)
Children (>14 days): Prophylatic and treatment doses: 6 mg/kg/day
Max. Prophylactic Dose=200 mg/day
Max. Treatment Dose=400 mg/day
Baylor College of Medicine 2010
12
Paediatric Haematology/Oncology Ward Officers Handbook
Fluconazole Indication
Day One
Daily Therapy
Minimum Duration
Oropharyngeal Candidiasis
6 mg/kg
3 mg/kg
14 days
Esophageal Candidiasis
6 mg/kg
3 - 12 mg/kg
21 days
Systemic Candidiasis
6 - 12 mg/kg
28 days
Amphotericin B
follow BUN/Cr daily initially until full dose reached, then 3 x per week
follow serum K+ daily
Dosing: 0.25 mg/kg/day for the first dose
Escalate up to 0.5-1 mg/kg/day as indicated by the clinical situation
Follow Mg twice/wk ; more frequently if hypokalemia or hypomagnesemia
May bolus NS 10 mL/kg (Max. 500 ml IV) over 1-2 hours prior ampho B
Minimizes renal toxicity
Tubuloglomerular feedback system regulates renal blood flow
To prevent a drug reaction may use as premedication:
Paracetomol 15 mg/kg dose (Max. Dose: 4000 mg/day; 1 gm/dose)
Diphenhydramine (or Chlorpheniramine) 1 mg/kg IV/PO (Max. Dose: 50 mg)
Hydrocortisone 2 mg/kg IV (Max. Dose: 100 mg)
To treat rigors with chills:
Meperidine (Pethidine) 0.5 mg/kg (Max. Dose: 25 mg) may use this dose to
premedicate in the future.
Baylor College of Medicine 2010
13
Paediatric Haematology/Oncology Ward Officers Handbook
4. Antiviral Therapy
Diagnosis made using cultures or polymerase chain reaction (PCR), or antigenemia where available, otherwise herpes simplex virus (HSV) and varicella zoster virus (VZV) can be diagnosed clinically.
Acyclovir:
Baseline chemistries prior to therapy, then monitor BUN/Cr 2x week
Maintain adequate hydration:
High-dose acyclovir IV, use 2400 mL/m2/day
Standard-dose, use maintenance IV Fluid rate
Adjust dose for renal impairment
In immuno-compromised patients with varicella zoster (shingles) who are afebrile and stable, may use oral dosing.
If febrile institute IV therapy.
In immuno-compromised patients with chicken pox institute IV therapy
Patients with herpes simplex may be treated using the oral acyclovir
Intravenous
HSV (sick/toxic patient): 20 mg/kg/dose q 8 hours
HSV (well-appearing): 10 mg/kg/dose q8 hours
Varicella: 20 mg/kg/dose q 8 hours (Max. Dose: None)
Oral
HSV or shingles: 250-600 mg/m2/dose 4-5 x/day (Max. Dose: 800
mg/dose)
5. Pneumocystis jerovecii (PCP) Prophylaxis
All patients on chemotherapy should receive PCP prophylaxis that continues until 6
months after completion of chemotherapy.
Baylor College of Medicine 2010
14
Paediatric Haematology/Oncology Ward Officers Handbook
Trimethoprim/sulfamethoxazole (TMP/SMX) can be given once daily or three times per
week twice daily using the dosing below:
BSA (m2)
Regular Strength Tab
Liquid (mL)
< 0.3
N/A
2.5
0.3-0.79
0.5
0.8-1.39
10
1.4-1.89
1.5
15
>1.9
20
Intolerance to TMP/SMX can occur. In such cases use either dapsone or, where
available pentamidine can be used as per the dosing schedule below:
Dapsone 2 mg/kg PO qAM (Max dose 100 mg)
Pentamidine given once monthly either aerosolized or IV:
Aerosolized
< 5 yrs: 8 mg/kg/dose in 5mL sterile water (Max Dose 300 mg)
> 5 yrs: 300 mg/dose in 5 mL sterile water
Administer with salbutomol 2 puffs pre & post pentamidine
Intravenous
4 mg/kg given once monthly
Baylor College of Medicine 2010
15
Paediatric Haematology/Oncology Ward Officers Handbook
6. Anti-emetic Medications
5HT3 Receptor Inhibitors: These medications are expensive & not readily available
in the resource-limited setting. However, they can be found at times & hence the
dosing is given here.
Give these medications 30 minutes prior to chemotherapy
Scheduled dosing is recommended especially for platinum-containing chemotherapy regimens
(1)
Ondansetron
PO
IV
< 4 yrs
0.2 mg/kg/dose
4-12 yrs
4 mg/dose
> 12 yrs
8 mg/dose
Wt (kg)
m2
Dose
< 10
<0.4
0.15 mg/kg/dose
10-50
0.4-1.2
4 mg/dose
> 50
> 1.2
8 mg/dose
Granisetron: Pediatric dosing is not well established
PO
Adult dose is 2 mg once daily or 1 mg twice daily
Pediatric dosing: 1 mg twice daily
IV
Pediatric dosing: 20-40 mcg/kg/day divided once or twice daily
Max dose 3 mg/dose or 9 mg/day
Dexamethasone
2
2
2 mg/m IV or PO with each ondansetron dose or a single 6 mg/m dose
given with the first ondansetron dose
Promethazine
Baylor College of Medicine 2010
16
Paediatric Haematology/Oncology Ward Officers Handbook
0.25 - 0.5 mg/kg/dose IV every 6 hours as needed
This can be given on a scheduled basis especially when 5HT3 Receptor
inhibitor agents are unavailable
Lorazepam
0.03 - 0.05 mg/kg/dose IV or PO every 6 hours
This drug is particularly beneficial for anticipatory nausea/vomiting
Baylor College of Medicine 2010
17
Paediatric Haematology/Oncology Ward Officers Handbook
Emetogenicity of Chemotherapy Agents
Note: sd - standard dose
hd - high dose (often difficult to give in resource-poor setting)
None
Mild
Moderate
Severe
6-mercaptopurine
5-fluorouracil
Cytarabine (sd)
Nitrogen mustards
Vincristine/Vinblastine
Etoposide/Teniposide
Methotrexate (hd)
Dacarbazine
6-thioguanine
Cyclophophamide
(sd)
Carboplatin
Cyclophosphamide
(hd)
L-asparaginase
Intrathecal chemotherapy
Daunomycin/Doxorubicin
Cytarabine (hd)
Bleomycin
Methotrexate (sd)
Actinomycin-D
Cisplatin
Hydroxyurea
Ifosfamide
7. Anaphylaxis Precautions
Use as a standard protocol when administering the following medications:
Etoposide or Teniposide
Carboplatin
L-Asparaginase
Reaction Grading Scale for Carboplatin, Etoposide, & Teniposide
Grade I - transient hives
Grade II - hives, pruritis, lip/tongue swelling, mild wheezing, anxiety
Grade III - serum sickness, chest tightness, severe bronchospasm, cough, chills,
vomiting, tachycardia, cyanosis
Grade IV - anaphylaxis with shock & hypotension
Baylor College of Medicine 2010
18
Paediatric Haematology/Oncology Ward Officers Handbook
Reaction Grading Scale for L-Asparaginase
Grade I - Local reaction at injection site with hives < 6 cm occuring < 6 hrs after
administration of medication
Grade II - Generalized reaction with hives < cm occurring < 6 hrs after administration of medication
Grade III - serum sickness, chest tightness, severe bronchospasm, cough, chills,
vomiting, tachycardia, cyanosis
Grade IV - anaphylaxis with shock & hypotension
Treatment of Reactions:
Grade I - II
2
Stop infusion, start NS at 100 ml/m /hr
Diphenhydramine 1 mg/kg Stat dose (Max dose: 50 mg)
Hydrocortisone 2 mg/kg IV Stat dose
Grade III-IV
2
Stop infusion, start NS at 100 ml/m /hr
Epinephrine (Adrenaline) 1:10,000 give 0.1 ml/kg IV Push Stat dose
Epinephrine (Adrenaline) 1:1,000 give 0.01 ml/kg IV Push Stat dose
After epinephrine given, give diphenhyrdamine & hydrocortisone
Monitor patient closely & repeat medications as needed given clinical condition
For any reaction monitor vital signs every 2-5 minutes until patient is stable including
heart rate, respiratory rate, blood pressure, & pulse oximetry (where available)
Medications that cause a reaction must not be repeated as a repeat dose can be fatal.
A pediatric oncologist ought to be consulted to determine if an alternate medication
would be possible.
Baylor College of Medicine 2010
19
Paediatric Haematology/Oncology Ward Officers Handbook
8. Mucositis & Oral Hygiene
Mucositis Grading System
Grade
Symptoms
Painless ulcers, erythema, mild soreness
II
Painful erythema, edema, ulcers; patient able to eat
III
As per Grade II but patient is unable to eat
IV
Requires parenteral or NG tube nutritional support
Medication options for mouthcare
Mouthwash - 1 L NS + 1 teaspoon table salt + 1 teaspoon NaHCO3 + 5 ml glycerin
10 ml swish & spit out four times daily
Nystatin: can be used as prophylaxis or if there is evidence of thrush
Infants: 1 ml of 100,000 units/ml solution applied to each side of mouth four
times daily
Children: 5 ml swish & swallow four times daily
Magnesium or Aluminum Hydroxide + Chlorpheniramine or diphenhyrdamine
Mix in a 1:1 ratio (e.g. 50 ml of each), and swish & spit four times daily
Maximum 5 ml per dose
Baylor College of Medicine 2010
20
Paediatric Haematology/Oncology Ward Officers Handbook
Chemotherapy Agents & Mucositis Severity
Minimal or No Mucositis
Mild Mucositis
Moderate-Severe Mucositis
Asparaginase
Bleomycin
Cytarabine
Etoposide (VP-16)
Cisplatin
Daunorubicin
Ifosfamide
6-mercaptopurine
5-fluorouracil
Vincristine
Procarbazine
Methotrexate
6-thioguanine
Doxorubicin
Vinblastine
Cyclophosphamide
9. Oncologic Emergencies
Tumor Lysis Syndrome (TLS)
Lysis of tumor cells releases electrolytes & urea cycle products resulting in
hyperuricemia, hyperkalemia, hyperphosphatemia & resultant hypocalcemia
Severe TLS seen with large tumor burden including (but not limited to):
Burkitts Lymphoma
3
Acute Lymphoblastic Leukemia with WBC count >100,000/mm
AML
Neuroblastoma
TLS Labs: minimum daily up to every 6hrs as resources allow
Urea & Electrolytes
Calcium
Magnesium
Baylor College of Medicine 2010
21
Paediatric Haematology/Oncology Ward Officers Handbook
Phosphate
Uric Acid
Maintain urine output at > 2.5 ml/kg/hr
Hemodialysis reserved for severe TLS, prevention of severe disease will
obviate requiring this invasive & expensive intervention
Specific Management
Hyperuricemia Management
2
Hydration with 3000 ml/m /day with fluids not containing potassium
1
(e.g. D5 /2 NS)
Consider adding 40 mEq NaHCO3/L to aid in uric acid excretion
Need to monitor calcium & phosphate several times daily if adding
NaCO3, where this is not feasible, do not add NaHCO3 to fluids
2
Allopurinol 100 mg/m /dose PO given three times daily
Max dose 600 mg/day for age <10 yrs, 800 mg/day for >10 yrs
Rasburicase:
currently not available in the resource-limited setting
Hyperkalemia
ECG: T wave elevation (peaked T wave), loss of P wave, widened
QRS complex
Avoid potassium in fluids to help prevent this complication
Stop any potassium supplementation if present
Dextrose 0.5 g/kg with 0.3 units insulin/gm dextrose, infuse over 2
hours
Kayexalate 1 g/kg/dose PO four times daily
1 g/kg lowers potassium by 1 mEq
Hyperphosphatemia/Hypocalcemia
Remove NaHCO3 from fluids if Ca x PO4 > 60
Where calcium & phosphate levels cannot be checked several times
daily, do not add NaHCO3 to fluids
Hyperphosphatemia - treat with aluminum hydroxide 25 mg/kg/dose
four times daily & avoid foods containing large amounts of phosphate
Hypocalcemia: 10% calcium gluconate 500 mg/kg IV infusion through
a central line
Maximum dose 2000 mg/dose
Monitor calcium level closely including ionized calcium where
available
Hyperleukocytosis
3
Defined as WBC > 100,000/mm
High risk for pulmonary & CNS complications due to viscosity & stasis
Baylor College of Medicine 2010
22
Paediatric Haematology/Oncology Ward Officers Handbook
2
IV fluid rate 3600 ml/m /day
Monitor WBC counts along with TLS labs
Monitor pulse oximetry for evidence of pulmonary complications, continuous
monitoring where possible
Do not transfuse above Hg 8.5 g/dL as pRBC or whole blood may increase
viscosity
3
May transfuse platelets for active bleeding or platelets <50,000/mm
Although not available in resource-limited settings, leukopheresis is recommended if possible
Space occupying lesions
Mediastinal mass/upper airway lesion
Avoid sedation
Elevate head of bed
Avoid procedures that may compromise airway & consult anesthesia for
procedures
Obtain diagnostic tissue with the least invasive method - e.g. peripheral
lymph node biopsy preferred over thoracotomy to biopsy chest mass
May need emergency chemotherapy and/or radiation therapy as a lifesaving measure, even prior to full diagnostic work-up
Intracranial mass/spinal cord compression
Intracranial pressure elevation can be treated with dexamethasone;
mannitol can be added for severe cases
Dexamethasone up to 4 mg IV every 4 hours can be given for cerebral
edema
Where required, substitution with hydrocortisone or prednisone can
be done, but effects on cerebral edema are much less potent as
compared to dexamethasone
Any central nervous system involvement by tumor requires immediate
involvement of neurosurgery
May need emergency chemotherapy and/or radiation therapy as a lifesaving measure, even prior to full diagnostic work-up
Baylor College of Medicine 2010
23
Paediatric Haematology/Oncology Ward Officers Handbook
10. Immunizations in Oncology Patients
Live vaccines, especially oral polio must be avoided for patient & family members
during chemotherapy
Yellow fever vaccine must be avoided in the patient; however, family members can
receive this vaccine where indicated
Killed or recombinant vaccines can be administered to the patient & family members; response is generally seen despite immunosuppression, however patients
undergoing bone marrow transplant generally require re-immunization 1 year posttransplant
Live vaccines can be resumed 6 months after chemotherapy is completed
Annual injectable influenza vaccine is recommended for immunosuppressed patients where the vaccine is available
11. Constipation
Most commonly caused by vincristine, inactivity & opiod medications
No rectal exam, enemas, or suppositories for patients on chemotherapy unless
discussed with specialist
Even minor trauma to the rectal mucosa can introduce a life-threatening infection in patients with neutropenia
Patients with normal absolute neutrophil count who did not receive chemotherapy in the previous 2 weeks are less likely to have complications
Management
A bowel regimen is recommended for all patients on vincristine therapy as preventing constipation is preferred to treating after it has started
Docusate sodium (stool softener)
Age < 3 yrs: 10-40 mg/day divided into 1-4 doses
Age 3 - 6 yrs: 20-60 mg/day divided into 1-4 doses
Age 6 - 12 yrs: 40-150 mg/day divided into 1-4 doses
Age > 12 yrs: 50-400 mg/day divided into 1-4 doses
Bisacodyl (Oral doing only; laxative)
3 - 12 yrs: 5 mg PO once daily
> 12 yrs: 10 mg PO once daily
Baylor College of Medicine 2010
24
Paediatric Haematology/Oncology Ward Officers Handbook
Magnesium hydroxide (laxative)
< 2 yrs: 0.5 ml/kg/dose
2 - 5 yrs: 10-15 ml PO once daily (can be given in divided doses)
6 - 12 yrs: 15-30 ml PO once daily (can be given in divided doses)
> 12 yrs: 30-60 ml PO once daily (can be given in divided doses)
Baylor College of Medicine 2010
25
Paediatric Haematology/Oncology Ward Officers Handbook
Hematology
1. Sickle cell disease
Patients should be receiving prophylaxis penicillin
Penicillin VK 125 mg PO twice daily for age < 3 years
Penicillin VK 250 mg PO twice daily for age > 3 years
Penicillin prophylaxis can be stopped for patients who these criteria:
No prior documented pneumococcal infection or pneumonia
Has not had surgical splenectomy
Has received vaccination with both the 7-valent conjugate pneumococcal vaccine and polysaccharide based 23-valent pneumococcal vaccine
Diagnostics: ideally hemoglobin (Hg) electrophoresis ought to be monitored, however this is often difficult to obtain routinely in the resource-limited setting
Where available, Hg S level ought to be followed & checked particularly when
exchange transfusion is available as the goal of exchange is to reduce the Hg S
level usually to < 30%
Folic Acid supplementation
Patients with chronic hemolysis, as with sickle cell disease, benefit from folic
acid supplementation in certain cases
For patients with Hg < 9 g/dL and reticulocyte count > 5%, give:
0.5 mg PO daily (age < 2 years age)
1 mg PO daily (age > 2 years age)
In the resource-limited setting, folic acid is often only available as 5 mg tablets,
in this case, give 5 mg for age > 2 years as folate is relatively benign
5 mg tablet can be crushed and a suspension made for infants
5 mg in 10 ml - 1 ml equals 0.5 mg
Baylor College of Medicine 2010
26
Paediatric Haematology/Oncology Ward Officers Handbook
2. Sickle cell disease with fever
Common pathogens
S. pneumoniae
H. influenza type b
E. coli
Salmonella
Mycoplasma pneumoniae and hominis
Chlamydophila pneumoniae
Diagnostics
Full blood count with differential & reticulocyte count
Blood culture
CXR - cannot rely on symptoms or physical exam findings
Where clinically needed - blood chemistries, urinalysis, urine culture
Management/Treatment
Admit for intravenous antibiotics if any of the following is found:
Age < 1 year
o
T > 40 C
Toxic or ill-appearing patient
Any infiltrate on CXR
Pulse oximeter reading < 92% on room air
History of bacteremia or pneumonia
Hg < 6 g/dL or reticulocyte count > 4%
3
3
WBC < 5,000/mm or > 30,000/mm
3
Platelet count < 100,000/mm
Non-toxic patient
Cefuroxime 50 mg/kg/dose IV every 8 hours
Toxic
patient
Vancomycin 15 mg/kg/dose IV every 8 hours
Cefotaxime 200 mg/kg/day divided every 8 hours
Patient with chest syndrome/pneumonia, add azithromycin
Patients who do not require admission
Minimum phone follow-up within 24 hours to check culture results & clinical
condition
Ceftriaxone 50 mg/kg IV/IM x 1 prior to discharge
Cefprozil 15 mg/kg/dose every 12 hour for 3 days (or local equivalent) or
Baylor College of Medicine 2010
27
Paediatric Haematology/Oncology Ward Officers Handbook
Erythromycin 50 mg/kg/day divided 4 times daily for 3 days (for patients allergic to cephalosporin)
If blood culture positive, adjust treatment based on culture & sensitivity
3. Sickle cell vaso-occlusive crisis
Pain crisis
Diagnostics: Full blood count with differential & reticulocyte count
Management
Pain control with opioid analgesic (see Pain Control section)
2
Hydration: 2000 - 2400 ml/m /day (if no cardiopulmonary disease)
Priapism
Diagnostics: Full blood count with differential & reticulocyte count
Management
Pain control with opioid analgesics (see Pain control section)
2
Hydration: 2000 - 2400 ml/m /day (if no cardiopulmonary disease)
Consult urology immediately for aspiration & irrigation if 4 hours since onset
Transfusion only if no detumescence within 12 hours
There is no indication for oxygen therapy in such cases
Splenic sequestration
Diagnostics: Full blood count with differential & reticulocyte count, type & cross
Management
2
Hydration: 1600 ml/m /day
Transfusion with pRBC urgently; transfusion rate dependent on hemodynamic status
Aplastic crisis
Diagnostics: Full blood count with differential & reticulocyte count, type & cross
Management
Hydration: maintenance PO fluids, IV fluids if not able to take PO
Transfusion with pRBC as clinically indicated
Acute Chest Syndrome/Pneumonia
Diagnostics: Full blood count with differential & reticulocyte count, type & cross,
chemistries, Blood culture, pulse oximetery, CXR
Baylor College of Medicine 2010
28
Paediatric Haematology/Oncology Ward Officers Handbook
Management
2
Hydration: IV fluids + PO total at maintenance (1600 ml/m /day)
3
Consider IV fluids at /4 maintenance to avoid fluid overload even if not
taking PO well
Pain management - cautious but do not withhold. Balance between pain
control & sedation required as either may lead to respiratory distress
Respiratory care
Oxygen therapy with pulse oximetry monitoring
Salbutomol inhaler/nebulized every 4 hours
Incentive spirometry 10 puffs every 2 hours while awake
10-15 ml/kg pRBC transfusion if significant anemia
Exchange transfusion often considered ideal; however it is rarely available in resource-limited setting
Antibiotics for pneumonia
Cefuroxime (dosage as above)
Azithromycin - M. pneumoniae frequent cause of acute chest syndrome
Stroke
Diagnostics: Full blood count with differential & reticulocyte count, type & cross,
emergent CT or MRI (where available)
Consider omitting contrast as it may exacerbate sickling
Management
Exchange transfusion is standard management where available
4. Pre-operative preparation of sickle cell patients
Diagnostics: Full blood count, type & cross
Ideally, patients ought to receive exchange transfusion to reduce Hg S < 30%
prior to most surgical procedures
Where exchange is unavailable, simple transfusions can be utilized to reduce Hg S, usually this will require multiple simple transfusion
Occasional low risk procedures can be done with a simple transfusion and IV
hydration without a Hg S goal level
Baylor College of Medicine 2010
29
Paediatric Haematology/Oncology Ward Officers Handbook
5. Transfusion therapy in sickle cell disease
Sickle cell patients should not be transfused to Hg > 11 g/dL or Hct > 30% as this
results in increased risk for vaso-occlusion and stroke
Where available, phenotyping should be performed to match blood for Rh and Kell
antigen groups
6. Hemophilia
Patients with hemophilia can have spontaneous bleeding and/or excessive bleeding with trauma, it is imperative to treat hemophilia patients within 30 minutes
of presentation and then consider diagnostic testing
Factor VIII deficiency (Hemophilia A)
1 unit/kg increases Factor VIII activity by 2%
Factor IX deficiency (Hemophilia B)
1 unit/kg increases Factor IX activity by 1%
Severity
Factor Level
Severe
<1%
Moderate
1-4%
Mild
5-25%
Baylor College of Medicine 2010
30
Paediatric Haematology/Oncology Ward Officers Handbook
7. Treatment of bleeding in patients with Hemophilia A
It is important to dose Factor VIII to a unit vial dose whenever possible to avoid
waste
For example, if unit vial is 500 units & patients dose is 400 units, order 500
units Factor VIII
Where
available, use recombinant product, otherwise factor concentrate ought to
be given
Where Factor VIII is unavailable or not immediately available in emergency situations, FFP at 10-15 ml/kg may be used
Inhibitor Screen
Where available, screening for inhibitor should be performed
If screen positive, defined as > 5 Bethesda Units, recombinant and concentrate
products will not be sufficient even at high doses
Where available Factor VIIa, Anti-Inhibitor Coagulant Complex, or Porcine
Factor VIII will be required
Baylor College of Medicine 2010
31
Paediatric Haematology/Oncology Ward Officers Handbook
The following table gives general guidelines, however specific cases should be
discussed with the specialist
Event
Hemarthrosis
First Factor Dose
(% correction)
50 U/Kg (100)
Subsequent Doses
25-35 U/Kg (50-70)
q12-24h x 2-5 days
Comments
Ice for 20 mins
immobilize x 48hr
Soft tissue bleed
30 U/Kg (60)
25 U/kg (50) daily x 2
days
Ice for 20 mins
Hematuria
35 U/Kg (70)
25 U/Kg (50) q12-24h x
2-7 days
IV hydration
prednisone 1-2 mg/kg/d
x 1-2 wks
GI Bleed
50 U/Kg (100)
25-35 U/Kg (50-70)
q12h x 2-7 days
Monitor FBC, transfuse
as required
Mucosal bleeding
35-50 U/Kg (75-100)
25 U/Kg (50) daily x 12 days
Amicar 100 mg/kg q6h
x 3-5 days where available
Head Trauma
50 U/Kg (100)
35 U/Kg (70) q8-12h
Do not wait for neurologic signs
CT scan after 1st dose
Maintain factor VIII level
> 80%
Major Surgery
50 U/Kg (100)
25-35 U/Kg (50-70)
q12h x 7-10 days
Maintain factor VIII level
> 50%
Dental Extractions
50 U/Kg (100)
25-35 U/Kg (50-70)
daily x 3 days
Amicar 100 mg/kg q6h
x 3-5 days where available
Baylor College of Medicine 2010
32
Paediatric Haematology/Oncology Ward Officers Handbook
8. Treatment of bleeding in patients with Hemophilia B
FFP 10-15 ml/kg where factor concentrate is not available or not immediately
available in emergency situations
Doses > 50 U/Kg may be associated with thromboembolic complications when less
pure Factor IX concentrates are used
This requires awareness of risk, this does not mean higher doses should not
be used
High purity Factor IX can result in anaphylaxis
Risk should be communicated to family if factor will be given at home
Anaphylaxis precautions should be followed in the hospital setting
Baylor College of Medicine 2010
33
Paediatric Haematology/Oncology Ward Officers Handbook
The following table gives general guidelines, however specific cases should be
discussed with the specialist
If using recombinant Factor IX, the dose must be increased by factor of 1.2
For example, dose of 100 U/Kg will be 120 U/Kg for recombinant factor
Event
Hemarthrosis
First Factor Dose
(% correction)
100 U/Kg (100)
Subsequent Doses
50-70 U/Kg (50-70)
q12-24h x 1-3 days
Comments
Ice for 20 mins
immobilize x 48hr
Soft tissue bleed
60 U/Kg (60)
50 U/kg (50) daily x 2
days
Ice for 20 mins
Hematuria
70 U/Kg (70)
50 U/Kg (50) q12-24h x
2-7 days
IV hydration
prednisone 1-2 mg/kg/d
x 1-2 wks
GI Bleed
100 U/Kg (100)
50-70 U/Kg (50-70)
q12h x 2-7 days
Monitor FBC, transfuse
as required
Mucosal bleeding
75-100 U/Kg (75-100)
50 U/Kg (50) daily x 1-2
days
Amicar 100 mg/kg q6h x
3-5 days where available
Head Trauma
100 U/Kg (100)
70 U/Kg (70) q12-24h
Do not wait for neurologic signs
CT scan after 1st dose
Maintain factor IX level
> 80%
Major Surgery
100 U/Kg (100)
50-70 U/Kg (50-70) daily x 7-10 days
Maintain factor IX level
>50%
Dental Extractions
100 U/Kg (100)
50-70 U/Kg (50-70) daily x 2-7 days
Amicar 100 mg/kg q6h x
3-5 days if available
Baylor College of Medicine 2010
34
Paediatric Haematology/Oncology Ward Officers Handbook
9. Von Willebrands Disease
Most commonly patients have mucocutaneous bleeding
Heavy menses in adolescent females and older females in the family is common
It is important to ask specifically about number of days & amount of bleeding
as many women & adolescents will think their heavy menses are normal
Diagnostics: FBC, PTT, Factor VIII, vWF activity & antigen, ristocetin cofactor activity, vWF multimers
Where vWF testing is not available, FBC, PTT, and Factor VIII should be
checked and results & case discussed with specialist
Treatment
Desmopressin Acetate can be given for patients who are sensitive (contraindicated in Type 2B vWD)
Avoid in patients less than 2 years or less than 10 kg
Potential side effects: headache, flushing, tachyphylaxis, fluid retention, hyponatremia
Restrict fluid intake following treatment
Dosing
0.3 micrograms/kg infused over 15 mins q12-24 hr (maximum 3 doses)
Intranasal - 150 micrograms/puff
< 50 kg: one puff q12-24 hr (maximum 3 doses)
> 50 kg: 2 puffs q12-24 hr (maximum 3 doses)
Certain Factor VIII concentrates do contain vWF depending on the preparation
e.g. Factor VIII from BioProducts Institute in RSA has 500 U vWF per vial
along with 500 U Factor VIII
Treat with 50 units/kg q12-24 hrs depending on severity of bleeding
Prophylaxis treatment is not generally indicated
Cryoprecipitate 1 bag/5 kg body weight can be given in emergency settings
where available and can be repeated every 8, 12, or 24 hrs depending on the
severity of bleeding
FFP does not contain vWF to any level that will be therapeutic and is not
indicated for vWD
Baylor College of Medicine 2010
35
Paediatric Haematology/Oncology Ward Officers Handbook
10. Immune Thrombocytopenic Purpura (ITP)
History
History of mucocutaneous bleeding & bruising
Previous viral infection
Recent vaccination
Atypical findings (may suggest disease other than ITP)
Systemic symptoms
Current infection
Evidence of immunodeficiency
HIV exposure or HIV+ status (although ITP is not uncommon with HIV)
Family history of low platelets or bleeding disorder
Medication exposure including antibiotics, anticonvulsants, heparin, antiarrhytmia medications, sulfa drugs, aspirin
Physical exam findings
Signs of bleeding including active bleeding or old clotted blood (e.g. nares)
Petechiae
Bruising
Atypical findings (may suggest disease other than ITP)
Evidence of active infection
Arthralgia
Bone pain
Hepatomegaly, splenomegaly, lymphadenopathy
Dysmorphic features, skeletal abnormalities, growth delay, failure to thrive
Known specific congenital condition
Fanconi anemia
Thrombocytopenia Absent Radii (TAR) syndrome
Platelet disorder: Bernard-Soulier, May-Hegglin, Gray Platelet syndrome
vWD Type 2B
Thrombocytopenic Thrombotic Purpura (TTP)
Diagnostics
FBC, reticulocyte count, smear examination
Results consistent with ITP
Platelet size normal or large in size
Occasional giant platelets seen
normal RBC & WBC morphology
In the resource-limited setting, microcytic, hypochromic red cells due
to underlying iron deficiency anemia is not uncommon
Baylor College of Medicine 2010
36
Paediatric Haematology/Oncology Ward Officers Handbook
Occasional activated lymphocytes can also be seen
Results not consistent with ITP
Predominant giant platelets
Abnormal RBC morphology
Leukocytosis or leukopenia
Immature leukocyte forms
Small platelets
Children with atypical features may have ITP but other diagnostics should be
performed as clinically indicated including, but not limited to:
LDH, uric acid
Bone marrow examination
Anti-Nuclear Antibody Titer
Coombs Test
Coagulation Panel: PT/INR, aPTT
Chemistries, urinalysis
Treatment Recommendations
Various recommendations exist for treatment, the following is based primarily
on recommendations from the American Society of Hematology (ASH) & various articles (see references)
3
Asymptomatic patients with platelets > 30,000/mm
Observation without treatment
3
Repeat platelet count weekly for 3 weeks then monthly if < 150,000/mm
If patient becomes symptomatic at any time refer to appropriate category
below
3
Asymptomatic, or minor symptoms with platelets 20-30,000/mm
If asymptomatic observation is appropriate
Minor symptoms including bruising & petechiae can also be observed, however outpatient treatment with prednisone is acceptable as well
Refer to treatment schedules below for details on prednisone therapy
Monitor platelets at day 7 & day 28 after treatment or weekly as above if no
treatment
3
Minor symptoms with platelets > 30,000/mm
Observation without treatment is recommended with platelet count monitoring as noted above for observation group
Alternatively, where there is clinical concern or follow-up concerns, treatment with prednisone with repeat platelet count day 7 & 28 post-treatment
Baylor College of Medicine 2010
37
Paediatric Haematology/Oncology Ward Officers Handbook
3
Minor symptoms (e.g. bruising) with no bleeding & platelets < 20,000/mm
Treatment for these patients is advised
Monitor platelet count at day 7 & 28 after treatment
Treatment with prednisone, IVIG, or anti-D antibody can be given
3
Mucous membrane bleeding with platelets < 50,000/mm
Treatment for these patients is advised
3
Active bleeding with platelets < 20,000/mm
Hospitalize, treat with IVIG or high-dose steroids or both
Discharge when bleeding controlled & platelet count rising (~ 2-3 days)
3
Bleeding with platelet > 30,000/mm
Treat with IVIG or high-dose steroids
Hospitalization based on stability of bleeding, accessibility to care. Stable patients with fast access to care can be managed as outpatients
Severe, life-threatening bleeding regardless of platelet count
Hospitalization & rapid treatment that should begin in Accident & Emergency
Treatment with IVIG and high-dose steroids with or without platelet transfusion therapy
Rule-out TTP prior to platelet therapy as this condition can be worsened
by platelet transfusion
Emergency splenectomy can be performed in select cases but the patients
condition & response to medical therapy must be considered
Follow-up after 1st month
3
Asymptomatic patients with platelet > 30,000/mm , monitor platelet count
3
monthly until > 150,000/mm
3
Patients with platelet count < 20,000/mm must be monitored as clinically
indicated
Treatment Schedules for Acute ITP
Chronic ITP is generally reserved for patients with persistent thrombocytopenia
beyond 6 months & management is best done with hematologist consultation
Prednisone therapy
Eligible patients
The importance of excluding ALL prior to prednisone therapy cannot be
stressed enough
Typical history & physical exam
No fever, adenopathy, hepatosplenomegaly or arthralgia/bone pain
FBC with normal WBC differential & RBC morphology
Peripheral smear shows no immature forms
Baylor College of Medicine 2010
38
Paediatric Haematology/Oncology Ward Officers Handbook
Schedule Options
Prednisone 4 mg/kg/day divided three times daily for 4 days
Prednisone 1-2 mg/kg/day divided three times daily for 14 days with 7
days taper
Methylprednisolone 30 mg/kg once daily for 3 days
Ranitidine is recommended when treating with corticosteroids
Intavenous Immunoglobulin (IVIG)
Eligible patients
Typical history & physical exam
No fever, significant adenopathy, hepatosplenomegaly
Mild to moderate bleeding
3
Platelet count < 30,000/mm
Schedule Options
Patients < 50 kg
0.8 - 1 g/kg once or
0.5 g/kg daily for 2 days
Patients > 50 kg
0.5 g/kg daily for two days
Patients with severe, life-threatening bleeding should receive up to 2 g/kg
given over 2-5 days
Adverse reactions including headache, fever, nausea, & flushing can be
treated by slowing infusion and/or giving:
Diphenhydramine 0.5-1 mg/kg IV or PO (max dose 50 mg)
Hydrocortisone 1 mg/kg (max dose 100 mg)
Paracetomol 15 mg/kg once (max dose 1000 mg)
Patients
with IgA deficiency should not receive standard IVIG preparations
Baylor College of Medicine 2010
39
Paediatric Haematology/Oncology Ward Officers Handbook
References
1.
Nathan D, Orkin S, Ginsburg D, Look A. Nathan and Oski's Hematology of Infancy and Childhood, Sixth Edition. 2003.
2.
Pizzo P, Poplack D. Principles and Practices of Pediatric Oncology. 2006.
3.
Suell M, Bomgaars L. Texas Children's Caner Center & Hematology Service
Resident Handbook. 2005.
4.
Dodd RY, Notari EPt, Stramer SL. Current prevalence and incidence of infectious
disease markers and estimated window-period risk in the American Red Cross blood
donor population. Transfusion 2002;42(8):975-9.
Baylor College of Medicine 2010
40
Вам также может понравиться
- Pediatric Hematology-Oncology Ward Officers HandbookДокумент78 страницPediatric Hematology-Oncology Ward Officers HandbookMarcela Catalina Fandiño VargasОценок пока нет
- Understanding Jaundice: Causes, Treatment and PreventionДокумент33 страницыUnderstanding Jaundice: Causes, Treatment and Preventionmbishara20100% (1)
- Antibiotics in Pediatrics (Vancomycin, Quinolones, Aminoglycosides, Tetracyclines, Chloramphenicol, Clindamycin, Macrolides)Документ90 страницAntibiotics in Pediatrics (Vancomycin, Quinolones, Aminoglycosides, Tetracyclines, Chloramphenicol, Clindamycin, Macrolides)Jill PОценок пока нет
- Quiz YourselfДокумент154 страницыQuiz YourselfKandykane05Оценок пока нет
- Haematology and Oncology MockДокумент7 страницHaematology and Oncology MockAung Myint HtunОценок пока нет
- NICU Standing Orders KFAFHДокумент36 страницNICU Standing Orders KFAFHallysonviernes100% (1)
- Diagnostic Pediatric Hematopathology - 2011Документ588 страницDiagnostic Pediatric Hematopathology - 2011Omar SarvelОценок пока нет
- Approach To Abdominal Masses in ChildrenДокумент36 страницApproach To Abdominal Masses in ChildrenMia Lesaca-Medina100% (3)
- Handbook of Pediatric Hematology and Oncology 3rd Edition 2021Документ492 страницыHandbook of Pediatric Hematology and Oncology 3rd Edition 2021pgginecologiahospirioОценок пока нет
- Sepsis Neonatal 2012 PeiatricsДокумент12 страницSepsis Neonatal 2012 PeiatricsWalter LojaОценок пока нет
- Approach To Sick NeonateДокумент47 страницApproach To Sick NeonateblitheleevsОценок пока нет
- Pediatric TransfusionДокумент82 страницыPediatric TransfusionMia Lesaca-Medina100% (2)
- HEMATOLOGY MCQS QUESTIONS WITH ANSWERS PDF Hematology Mcqs Questions With Answers PDFДокумент2 страницыHEMATOLOGY MCQS QUESTIONS WITH ANSWERS PDF Hematology Mcqs Questions With Answers PDFSrinivas PingaliОценок пока нет
- Anemia of PrematurityДокумент14 страницAnemia of PrematurityMariel HuamancayoОценок пока нет
- Myeloproliferative Diseases 2020Документ105 страницMyeloproliferative Diseases 2020Marc FosterОценок пока нет
- Intrauterine Fetal Transfusion of Red Blood CellsДокумент16 страницIntrauterine Fetal Transfusion of Red Blood CellsHervi LaksariОценок пока нет
- Paediatric History TakingДокумент6 страницPaediatric History Takingsubramaniam krishnamoorthiОценок пока нет
- Post Antibiotic Era Emerging Concern To HumanityДокумент47 страницPost Antibiotic Era Emerging Concern To Humanitytummalapalli venkateswara raoОценок пока нет
- Clinical PediatricДокумент214 страницClinical PediatricRogerОценок пока нет
- Pediatrics AnswersДокумент28 страницPediatrics Answersjaini_patel23Оценок пока нет
- Oxford Pediatric Oncology PDFДокумент593 страницыOxford Pediatric Oncology PDFmondderОценок пока нет
- Keyes Neonatal Emergencies FinalДокумент108 страницKeyes Neonatal Emergencies FinalthanyunОценок пока нет
- Serum Protein ElectrophoresisДокумент9 страницSerum Protein Electrophoresiskiedd_04100% (4)
- Pediatric Hematology Oncology CaseДокумент107 страницPediatric Hematology Oncology CaseSayyed Ahmad KhursheedОценок пока нет
- MRCPCH Guide NeonateДокумент4 страницыMRCPCH Guide NeonateRajiv Kabad100% (1)
- Fetus & Neoborn-3Документ25 страницFetus & Neoborn-3Mateen Shukri100% (1)
- The Following Drugs Are Safe in Breast-Feeding:: AccidentsДокумент2 страницыThe Following Drugs Are Safe in Breast-Feeding:: AccidentsRajiv KabadОценок пока нет
- Dr. Ashok Deorari - Non Invasive Ventilation Way Forward For IndiaДокумент11 страницDr. Ashok Deorari - Non Invasive Ventilation Way Forward For IndiaKalyan DamisettiОценок пока нет
- Educational Guide: 2nd EditionДокумент130 страницEducational Guide: 2nd EditionEdin HamzicОценок пока нет
- HemaДокумент7 страницHemaLean Ashly Tuddao MacarubboОценок пока нет
- Gastroentrology LastДокумент48 страницGastroentrology LastAbdallah K. RamadanОценок пока нет
- Basic Sciences For MRCPCH ExamДокумент11 страницBasic Sciences For MRCPCH ExamMahmoud Abul AtaОценок пока нет
- Antibiotic Use in Critical Care: DR Radha Sundaram Lead Clinician RAH PaisleyДокумент36 страницAntibiotic Use in Critical Care: DR Radha Sundaram Lead Clinician RAH PaisleyHidayati IdaОценок пока нет
- MRCPCH SyllabusДокумент3 страницыMRCPCH SyllabusKanthi Sagar100% (1)
- Pediatrics Review: MOC - CME - Board ReviewДокумент56 страницPediatrics Review: MOC - CME - Board ReviewTalib AdilОценок пока нет
- Pediatric Reference RangesДокумент9 страницPediatric Reference RangesmmmmmmОценок пока нет
- Neonatal PolycythemiaДокумент13 страницNeonatal PolycythemiaMariel HuamancayoОценок пока нет
- Clinical Pathology Handbook (Weblinks 1 Jan 2017)Документ66 страницClinical Pathology Handbook (Weblinks 1 Jan 2017)sam214100% (1)
- Pae-Central Nervous SystemДокумент17 страницPae-Central Nervous SystemMegha ProjectsОценок пока нет
- Thalassemia & Treatment: Hematology Oncology Sub Division Padjadjaran University - Hasan Sadikin Hospital Bandung 2011Документ24 страницыThalassemia & Treatment: Hematology Oncology Sub Division Padjadjaran University - Hasan Sadikin Hospital Bandung 2011Galantry Ahmad AzhariОценок пока нет
- Bleeding in A NeonateДокумент36 страницBleeding in A NeonateDrBibek AgarwalОценок пока нет
- Hanan Fathy Pediatric Nephrology UnitДокумент59 страницHanan Fathy Pediatric Nephrology UnitdrhananfathyОценок пока нет
- Pediatric 6th Year 2016Документ30 страницPediatric 6th Year 2016motasem alsharifОценок пока нет
- WBC Pathology: Lecturer: Associate Professor T. A. GrekovaДокумент49 страницWBC Pathology: Lecturer: Associate Professor T. A. GrekovaFaheem MusthafaОценок пока нет
- Managing the Unconscious Pregnant PatientДокумент12 страницManaging the Unconscious Pregnant PatientmasterchipОценок пока нет
- Hemoglobin Electrophoresis1Документ19 страницHemoglobin Electrophoresis1nidaats100% (1)
- MBChB Year 4 & 5 Past Papers + AnswersДокумент170 страницMBChB Year 4 & 5 Past Papers + AnswersHariharan NarendranОценок пока нет
- IVMS - General Pathology, InflammationДокумент94 страницыIVMS - General Pathology, InflammationMarc Imhotep Cray, M.D.Оценок пока нет
- Nephrology Best RДокумент6 страницNephrology Best Rfrabzi100% (1)
- The Bleeding Child OSCE HaemophiliaДокумент3 страницыThe Bleeding Child OSCE HaemophiliaJJ LimОценок пока нет
- How Long Do Partial Thickness Burns Typically Take To Heal?Документ49 страницHow Long Do Partial Thickness Burns Typically Take To Heal?Farah FarahОценок пока нет
- Nutrition Board ReviewДокумент52 страницыNutrition Board ReviewWaleed AlakbariОценок пока нет
- MCQ Nelson 20Документ588 страницMCQ Nelson 20della mouradОценок пока нет
- Case Study #1: History and Exam of a Critically Ill NewbornДокумент39 страницCase Study #1: History and Exam of a Critically Ill Newbornleonzon_ben442296Оценок пока нет
- AAO READING ON RETINOPATHY OF PREMATURITYДокумент34 страницыAAO READING ON RETINOPATHY OF PREMATURITYUNHAS OphthalmologyОценок пока нет
- Lec1 Introduction To Immunohematology1Документ20 страницLec1 Introduction To Immunohematology1Dalia M. MohsenОценок пока нет
- Hemat.Q - 1Документ27 страницHemat.Q - 1aliaaОценок пока нет
- HematologyДокумент34 страницыHematologyAnne Angue GonzalesОценок пока нет
- Rhetorical Analysis Essay-4Документ5 страницRhetorical Analysis Essay-4api-545696216Оценок пока нет
- Menstrual DisordersДокумент45 страницMenstrual DisordersMegat Mohd Azman Adzmi100% (1)
- Report On AganwadiДокумент5 страницReport On AganwadiAkansha JohnОценок пока нет
- Ayurveda Tongue Analysis Dr. Rama PrasadДокумент34 страницыAyurveda Tongue Analysis Dr. Rama PrasadSanjay Soni100% (2)
- PPIs and Kidney DiseaseДокумент6 страницPPIs and Kidney DiseaseSonia jolandaОценок пока нет
- F1000research 8 20413Документ7 страницF1000research 8 20413miss betawiОценок пока нет
- Indian Polity: Constitution, Governance & Social JusticeДокумент8 страницIndian Polity: Constitution, Governance & Social JusticeXylo MartyОценок пока нет
- USCE Database Compiled by Usmlesarthi TeamДокумент12 страницUSCE Database Compiled by Usmlesarthi Teamagar agarОценок пока нет
- Jurnal IMD 2Документ11 страницJurnal IMD 2weniОценок пока нет
- Mid-Term Presentation OutlineДокумент16 страницMid-Term Presentation Outlineapi-526664901Оценок пока нет
- Hospital ExamplesДокумент10 страницHospital ExamplesArmand Kyle AbadОценок пока нет
- Iacta 2011 Janak Mehta Award Winning PresentationДокумент56 страницIacta 2011 Janak Mehta Award Winning PresentationDr.Sandeep Kumar KarОценок пока нет
- Lessons Learnt During Malaysia's MCOДокумент2 страницыLessons Learnt During Malaysia's MCOYEW SIAU JING MoeОценок пока нет
- Missed Nursing Care in Pediatric and Neonatal Care Settings: An Integrative ReviewДокумент2 страницыMissed Nursing Care in Pediatric and Neonatal Care Settings: An Integrative ReviewMikaela Gabrielle GERALIОценок пока нет
- Garcia Rudea v. Pascasio PDFДокумент2 страницыGarcia Rudea v. Pascasio PDFerxha ladoОценок пока нет
- Candida albicans Gram StainingДокумент3 страницыCandida albicans Gram StainingNida RidzuanОценок пока нет
- Bhagandara NidanaДокумент5 страницBhagandara NidanaSachintha WijesiriwardhanaОценок пока нет
- Early Clinical Exposure: Dr. Varun Sisodia Secretary MEU KDMCHRCДокумент19 страницEarly Clinical Exposure: Dr. Varun Sisodia Secretary MEU KDMCHRCFrank NobodОценок пока нет
- Hospital AdventistДокумент6 страницHospital AdventistGina Hong HongОценок пока нет
- JSS Guide for Community HIV Care and Treatment ActivityДокумент47 страницJSS Guide for Community HIV Care and Treatment Activityishdo ishdoОценок пока нет
- Temporomandibular Joint Disorders: Coverage RationaleДокумент14 страницTemporomandibular Joint Disorders: Coverage RationaleVitalii RabeiОценок пока нет
- Name: Ni Made Ayu Candra Dewi NIM: 18C10083 Class: Ilmu Keperawatan BДокумент2 страницыName: Ni Made Ayu Candra Dewi NIM: 18C10083 Class: Ilmu Keperawatan BVira Permata SariОценок пока нет
- Treatment GuidelineДокумент28 страницTreatment Guidelinev_vijayakanth7656Оценок пока нет
- Uva-Dare (Digital Academic Repository)Документ237 страницUva-Dare (Digital Academic Repository)F FreitasОценок пока нет
- Hair and Health Lifestyle ManualДокумент39 страницHair and Health Lifestyle Manualmenna hassanОценок пока нет
- Hospital Transfer PoliceДокумент4 страницыHospital Transfer PoliceMahmoud NaggarОценок пока нет
- Daily Lesson Log on Lifestyle and Weight ManagementДокумент8 страницDaily Lesson Log on Lifestyle and Weight ManagementNoel Isaac Maximo100% (2)
- Policies and Schemes of Central and State Governments For People With DisabilitiesДокумент128 страницPolicies and Schemes of Central and State Governments For People With Disabilitiesmanjunatha tОценок пока нет
- سندДокумент82 страницыسندAshkan AbbasiОценок пока нет
- Factors of Alcohol Consumption ThesisДокумент34 страницыFactors of Alcohol Consumption ThesisLowie Jay Mier Orillo100% (1)