Академический Документы
Профессиональный Документы
Культура Документы
Gastric Schwannoma: MRI Findings: Case Report
Загружено:
jihaneОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Gastric Schwannoma: MRI Findings: Case Report
Загружено:
jihaneАвторское право:
Доступные форматы
The British Journal of Radiology, 75 (2002), 624626
2002 The British Institute of Radiology
Case report
Gastric schwannoma: MRI findings
N KARABULUT, MD, D R MARTIN, MD, PhD and M YANG, MD
Department of Radiology, West Virginia University Hospitals, Morgantown, WV, USA
Abstract. MRI features are described in a case of gastric schwannoma. A large, discretely
marginated, multilobular mass was seen adjacent to the gastric antrum with the epicentre of the
mass in the gastrocolic ligament. The overall signal pattern was low on T1 weighted images and
moderate to markedly elevated on T2 weighted images. Post-gadolinium sequences demonstrate
slow but fairly uniform enhancement throughout the mass.
Schwannomas are rare among the spindle
cell mesenchymal tumours of the digestive
tract, arising from the Schwann cells of the
neural plexus of the gastrointestinal wall. Gastric
schwannomas, most commonly sited in the
stomach, account for only 0.2% of all gastric
tumours [1] and have received little attention in
radiological literature. These tumours are usually
asymptomatic or may present as upper gastrointestinal bleeding or as mass lesions [17]. Upper
endoscopy is important in the initial evaluation
of these patients, but it may not be helpful in
the diagnosis of submucosal tumours growing
exophytically. Cross-sectional imaging findings
may be useful in the detection and characterization of the tumour and its relation with
surrounding organs. We describe here the MRI
features of gastric schwannoma in a 46-year-old
patient. To our knowledge, this case is the first to
be reported with MRI documentation.
Case report
A 46-year-old White male was seen in surgery
clinic with the complaint of inguinal hernia. On
physical examination the patient was found to
have a large abdominal mass in his right upper
quadrant. The patient denied any complaints or
any symptoms related to the mass. Laboratory
findings were within normal limits. Upper endoscopy showed large extrinsic bulges from both the
anterior and posterior walls in the gastric antrum.
Multiple biopsies taken from the site of extrinsic
mass revealed marked chronic active gastritis
without evidence of a malignancy. The patient
subsequently underwent abdominal MRI in order
to evaluate the mass, which showed a large,
Received 24 January 2002 and accepted 19 March 2002.
Address correspondence to N Karabulut, MD, Hastane
Cad. Umut Apt 5/3, 20010, Denizli, Turkey.
624
discretely marginated mass with innumerable
lobulations centered in the region of the gastrocolic ligament (Figure 1). The overall signal
pattern was low on T1 weighted images and
moderate to markedly elevated on T2 weighted
images (Figure 1a, b). Each of these lobulations
appeared to be encapsulated with moderately
well defined borders, which were seen as markedly
hypointense on T1 weighted images and hypointense, isointense and hyperintense on T2 weighted
images. Post-gadolinium sequences demonstrate
slow but fairly uniform marked enhancement
throughout the internal aspect of each of the
lobules (Figure 1c, d). However, the hypointense
borders around the lobulations remained unenhanced. There was no evidence of necrosis within
the tumour mass. The inferior aspect of the mass
was pushing on the transverse colon with the
transverse colon draped around the mass. The
superior aspect of the mass was seen extending
over the anterior aspect of the gastric antrum,
pylorus, duodenal cap and proximal part of the
second segment of the duodenum towards the
gall bladder fossa and porta hepatis. The distal
stomach appeared to be squeezed by the mass
(Figure 1a, b, d). The pancreas was pushed
posteriorly and inferiorly but was clearly separate
from the mass. The remainder of the abdomen
was unremarkable without evidence of direct
organ invasion, lymphadenopathy or solid organ
metastases. The celiac artery and major branches,
as well as the superior mesenteric artery and
major branches, were clearly identified but a
vascular supply to the mass was not well
demonstrated.
At exploratory laparatomy, the abdominal
mass was found to be adhered to the greater
curvature in the anterior wall of the distal
stomach. Since the mass was arising from the
distal portion of the stomach, a partial gastrectomy with Billroth I gastroduodenostomy was
The British Journal of Radiology, July 2002
Case report: MRI of gastric Schwannoma
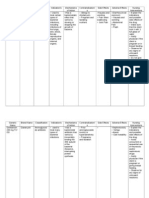
(a)
(b)
(c)
(d)
Figure 1. 46-year-old man with gastric schwannoma. (a) Axial fat-suppressed T1 weighted fast spoiled gradient
echo MR image (FLASH: TR/TE, 258/5.9 msec) at the level of the gall bladder shows a hypointense mass in the
region of gastrocolic and gastrohepatic ligaments squeezing the gastric antrum (arrows). (b) Coronal T2 weighted
fast steady state MR image (True FISP: TR/TE 4.6/2.3 msec) through the stomach shows a multilobulated mass
centred in the gastrocolic ligament exhibiting areas of moderate to markedly elevated signal. Note the close relation of the mass to gastric antrum. (c) Axial fat-suppressed T1 weighted fast spoiled gradient echo MR image
(FLASH: TR/TE, 168/5.9 msec) after iv administration of gadolinium demonstrates fairly uniform intense
enhancement throughout the internal aspect of each of the lobules. The hypointense borders surrounding the
lobules remain unenhanced. (d) Axial fat-suppressed T1 weighted volumetric three-dimensional gradient echo MR
image (TR/TE, 3.7/1.7 msec) at the level of the gastric antrum after iv administration of gadolinium delineates the
relationship between the mass and the stomach to a better degree.
performed in order to remove the mass. Macroscopic examination revealed a yellowtan bosselated tumour, which measured 15 cm612 cm6
11 cm in size. The cut surface of this tumour
was yellowtan and focally haemorrhagic with a
fish flesh appearance. Sections from the gastric
tumour showed a spindle cell neoplasm arranged
in a palisading fashion with numerous Verocay
bodies. In addition, more cellular Antoni type A
patterns were seen alternating with looser Antoni
type B areas. Mitoses were not seen and cytologic
atypia was not appreciated. The tumour cells
were strongly positive for S100 and vimentin, and
negative for smooth muscle actin, keratin and
The British Journal of Radiology, July 2002
CD34. The histological and immunohistochemical features were consistent with a benign
Schwannoma.
Discussion
Schwannomas, also known as neurinoma and
neurilemmoma, are benign, slow growing neoplasms originating in any nerve that has a
Schwann cell sheath. They rarely occur in the
digestive tract, but when they do the most
common site is the stomach, and represent 0.2%
of all gastric tumours [1]. Gastric schwannomas
occur more frequently in the third to fifth decade
of life and are usually solitary tumours arising
625
N Karabulut, D R Martin and M Yang
from the fundus, body or antrum of the stomach
[17]. However, they can occur in children and,
rarely, can be malignant [8]. Commonly they are
intramural, although they can be extraluminal
or endoluminal [2]. Gastric schwannomas are
usually covered by intact mucosa and principally
involve the submucosa and muscularis propria.
Tumours vary from 0.5 cm to 11 cm diameter
and are spherical or ovoid, occasionally with a
multinodular pattern [37]. They can be distinguished from other gastric mesenchymal tumours
based on immunohistochemical or ultrastructural
findings [6, 7]. Patients are usually asymptomatic, however, they may present with the symptoms of abdominal pain or discomfort, occult
or overt upper gastrointestinal bleeding from
the ulceration of the overlying mucosa. A palpable mass may be present when the tumour is
larger and predominantly exophytic. Diagnosis
is usually delayed owing to subclinical tumour
growth. Endoscopic evaluation may be normal
or only show non-specific secondary findings
such as extrinsic mass effect or ulceration if the
schwannoma is mainly exophytic. Furthermore,
as occurred in this case, endoscopic biopsy may
not be adequate for definite diagnosis because
schwannomas are submucosal tumours and
mucosal abnormality may be minimal.
In this case, the abdominal mass appeared to
be centred in the gastrocolic ligament and its
site of origin could not be confirmed initially,
although close relation of the tumour with the
gastric antrum was depicted, particularly on threedimensional volumetric MRI. When a large
intraabdominal mass is present next to several
organs, its exact site of origin cannot be determined based on the location of its epicentre on
cross-sectional imaging, as in this case. However,
the benign nature of the tumour and its relation
to adjacent structures are well delineated on MRI.
Although definite diagnosis of digestive tract
schwannoma is made by microscopic examination and immunohistochemical staining, crosssectional imaging, particularly MRI with direct
multiplanar imaging capability, is important in
defining the exact location and extent of the
tumour with displacement of surrounding organs
or vessels, providing valuable information for
surgical planning. The imaging findings of gastric
schwannoma have rarely been documented [6,
8]. Usually they appear as spherical, ovoid or
626
multilobulated solid masses adjacent to gastric
wall, hypoechoic on ultrasound, hypodense on
CT and show contrast enhancement. They
rarely appear cystic, although large tumours
may undergo cystic degeneration. Calcification
is uncommon.
The MRI appearance of schwannomas arising from cranial or spinal nerves has been well
described in the literature, but that of a gastric
schwannoma has not been reported previously.
Typically, these lesions are sharply demarcated,
strongly enhancing tumours, having low to
medium signal intensity on T1 weighted images
and high signal intensity on T2 weighted images.
The MRI findings in our case are consistent
with the literature on cranial or spinal nerve
schwannomas, except for unenhanced borders
surrounding the lobules. Schwannomas should
be included in the differential diagnosis of
intramural or exophytic gastric masses when
imaging findings show a well defined multilobulated solid mass adjacent to the stomach.
References
1. Melvin WS, Wilkinson MG. Gastric Schwannoma.
Clinical and pathologic considerations. Am Surg
1993;59:2936.
2. Bruneton JN, Drouillard J, Roux P, Ettore F,
Lecomte P. Neurogenic tumors of the stomach.
Report of 18 cases and review of the literature.
ROFO Fortschr Geb Rontgenstr Nuklearmed 1983;
139:1928.
3. Miettinen M, Lasota J. Gastrointestinal stromal
tumorsdefinition, clinical, histological, immunohistochemical, and molecular genetic features and
differential diagnosis. Virchows Arch 2001;438:112.
4. Daimaru Y, Kido H, Hashimoto H, Enjoji M.
Benign schwannoma of the gastrointestinal tract: a
clinicopathologic and immunohistochemical study.
Hum Pathol 1988;19:25764.
5. Sarlomo-Rikala M, Miettinen M. Gastric schwannomaa clinicopathological analysis of six cases.
Histopathology 1995;27:35560.
6. Rymarczyk G, Hartleb M, Boldys H, Kajor M,
Wodolazski A. Neurogenic tumors of the digestive
tract: report of two cases. Med Sci Monit 2000;
6:3835.
7. Prevot S, Bienvenu L, Vaillant JC, de Saint-Maur
PP. Benign schwannoma of the digestive tract: a
clinicopathologic and immunohistochemical study of
five cases, including a case of esophageal tumor. Am
J Surg Pathol 1999;23:4316.
8. Bees NR, Ng CS, Dicks-Mireaux C, Kiely EM.
Gastric malignant schwannoma in a child. Br
J Radiol 1997;70:9525.
The British Journal of Radiology, July 2002
Вам также может понравиться
- Adult Intussussception Int J Student Res 2012Документ3 страницыAdult Intussussception Int J Student Res 2012Juan De Dios Diaz-RosalesОценок пока нет
- Gastrointestinal Stromal Tumor FirdausДокумент8 страницGastrointestinal Stromal Tumor FirdausFarizka FirdausОценок пока нет
- Primary Pure Squamous Cell Carcinoma of The Duodenum: A Case ReportДокумент4 страницыPrimary Pure Squamous Cell Carcinoma of The Duodenum: A Case ReportGeorge CiorogarОценок пока нет
- Nephroblastoma: Radiological and Pathological Diagnosis of A Case With Liver MetastasesДокумент5 страницNephroblastoma: Radiological and Pathological Diagnosis of A Case With Liver MetastasesfifahcantikОценок пока нет
- Intussusception of Rectosigmoid Colon Cancer Mimicking A Pedunculated Tumor 2014Документ5 страницIntussusception of Rectosigmoid Colon Cancer Mimicking A Pedunculated Tumor 2014吳醫師Оценок пока нет
- 29051-Texto Do Trabalho-123037-2-10-20221229Документ3 страницы29051-Texto Do Trabalho-123037-2-10-20221229Luis Curvo SemedoОценок пока нет
- Journal of Pediatric Surgery Case Reports: Wandering Mesenteric CystДокумент4 страницыJournal of Pediatric Surgery Case Reports: Wandering Mesenteric CysthilalОценок пока нет
- MRI Features of Rare Mesenteric Lipoblastoma in a ChildДокумент4 страницыMRI Features of Rare Mesenteric Lipoblastoma in a ChildjamesfkpОценок пока нет
- Case Report: Urachal Adenocarcinoma: A Case Report With Key Imaging Findings and Radiologic-Pathologic CorrelationДокумент6 страницCase Report: Urachal Adenocarcinoma: A Case Report With Key Imaging Findings and Radiologic-Pathologic Correlationchristian hansОценок пока нет
- بحث 8Документ4 страницыبحث 8Ossama Abd Al-amierОценок пока нет
- Dynamic CT Findings of A Polypoid Gastric - ChrisnaДокумент4 страницыDynamic CT Findings of A Polypoid Gastric - ChrisnaferonicaОценок пока нет
- Obstruccion Intestinal MalignaДокумент11 страницObstruccion Intestinal MalignaMaria Del PilarОценок пока нет
- Journalarticle 0185Документ2 страницыJournalarticle 0185Mahmood AdelОценок пока нет
- Protruding LesionsДокумент10 страницProtruding LesionsJenniffer FlorenciaОценок пока нет
- Laparoscopy and Primary Diffuse MalignantДокумент5 страницLaparoscopy and Primary Diffuse Malignantmalvina.sekolonik911Оценок пока нет
- 48 Devadass EtalДокумент4 страницы48 Devadass EtaleditorijmrhsОценок пока нет
- Metastatic Breast Cancer Presenting As A Gallstone Ileus: Case ReportДокумент3 страницыMetastatic Breast Cancer Presenting As A Gallstone Ileus: Case ReportMaghfirah MahmuddinОценок пока нет
- An Unusual Cause of Duodenojejunal IntussusceptionДокумент2 страницыAn Unusual Cause of Duodenojejunal IntussusceptionVictoria HОценок пока нет
- The Robotic Approach For Enucleation of A Giant Esophageal LipomaДокумент3 страницыThe Robotic Approach For Enucleation of A Giant Esophageal LipomaPatricia JaramilloОценок пока нет
- Jurnal 1Документ5 страницJurnal 1Anida ShofianaОценок пока нет
- Nej M CPC 079007Документ10 страницNej M CPC 079007Pandu Nugroho KantaОценок пока нет
- Successful Treatment of A 14-Year-Old Patient With Intestinal Malrotation With Laparoscopic Ladd Procedure: Case Report and Literature ReviewДокумент5 страницSuccessful Treatment of A 14-Year-Old Patient With Intestinal Malrotation With Laparoscopic Ladd Procedure: Case Report and Literature ReviewHendry JohannesОценок пока нет
- Recurrent Adenocarcinoma of Colon Presenting As Duo-Denal Metastasis With Partial Gastric Outlet Obstruction: A Case Report With Review of LiteratureДокумент5 страницRecurrent Adenocarcinoma of Colon Presenting As Duo-Denal Metastasis With Partial Gastric Outlet Obstruction: A Case Report With Review of LiteratureVika RatuОценок пока нет
- Imaging Techniques for Diagnosing Inflammatory Bowel DiseaseДокумент16 страницImaging Techniques for Diagnosing Inflammatory Bowel DiseaseJEFFERSON MUÑOZОценок пока нет
- Uterine Fibroid Mimicking Ovarian TumorДокумент3 страницыUterine Fibroid Mimicking Ovarian Tumorasshagab04Оценок пока нет
- Adenocarcinoma of The DuodenumДокумент2 страницыAdenocarcinoma of The DuodenumDeba P SarmaОценок пока нет
- CA Stomach OverviewДокумент84 страницыCA Stomach OverviewDr Shafiq Ahmad ChughtaiОценок пока нет
- Casereports 18 125 PDFДокумент6 страницCasereports 18 125 PDFAstrianti Kusuma WardaniОценок пока нет
- Adenocarcinoma at Angle of Treitz: A Report of Two Cases With Review of LiteratureДокумент3 страницыAdenocarcinoma at Angle of Treitz: A Report of Two Cases With Review of LiteratureRijal SaputroОценок пока нет
- Transabdominalultrasoundfor Bowelevaluation: Peter M. Rodgers,, Ratan VermaДокумент16 страницTransabdominalultrasoundfor Bowelevaluation: Peter M. Rodgers,, Ratan VermaAle SosaОценок пока нет
- Dematos 1997Документ6 страницDematos 1997Ali AmokraneОценок пока нет
- GistДокумент4 страницыGistMada IacobОценок пока нет
- Tumores NeuroendocrinosДокумент8 страницTumores NeuroendocrinosGabriela Zavaleta CamachoОценок пока нет
- Liang 2016Документ4 страницыLiang 2016danielleclimacoОценок пока нет
- cLINICAL PRACTICE GUIDELINESДокумент7 страницcLINICAL PRACTICE GUIDELINESdrmolinammОценок пока нет
- Breast vs. Gastric Cancer: PicturesДокумент4 страницыBreast vs. Gastric Cancer: PicturesMa-Kur'z LeonesОценок пока нет
- Recurrent Acute Pancreatitis and Massive Hemorrhagic Ascites Secondary To A Duodenal Duplication in A Child: A Case ReportДокумент4 страницыRecurrent Acute Pancreatitis and Massive Hemorrhagic Ascites Secondary To A Duodenal Duplication in A Child: A Case ReportHarnadi WonogiriОценок пока нет
- Css CT Scan AbdomenДокумент54 страницыCss CT Scan AbdomenUlfa DiyaОценок пока нет
- Retroperitoneal Tumor - NcbiДокумент6 страницRetroperitoneal Tumor - NcbiWidya Eka WardhaniОценок пока нет
- Junk For Junk SiteДокумент5 страницJunk For Junk SitejwthreeОценок пока нет
- Yang Et Al. - 2020 - Blunt Abdominal Trauma Resulting in Ovarian Mucinous Cystadenoma RuptureДокумент2 страницыYang Et Al. - 2020 - Blunt Abdominal Trauma Resulting in Ovarian Mucinous Cystadenoma RuptureJamesLeeОценок пока нет
- 3Fwjfx "Sujdmf &BSMZ %jbhoptjt PG (Bmmcmbeefs $bsdjopnb "O "Mhpsjuin "QqspbdiДокумент6 страниц3Fwjfx "Sujdmf &BSMZ %jbhoptjt PG (Bmmcmbeefs $bsdjopnb "O "Mhpsjuin "QqspbdiabhishekbmcОценок пока нет
- Cureus 0012 00000011874Документ6 страницCureus 0012 00000011874Arsen NitОценок пока нет
- A Complicated Ileal Duplication Cyst in A Young Adult: The Value of The "Gut Signature"Документ5 страницA Complicated Ileal Duplication Cyst in A Young Adult: The Value of The "Gut Signature"naufal12345Оценок пока нет
- 2016 Article 1454 PDFДокумент3 страницы2016 Article 1454 PDFHerlinda Puji LОценок пока нет
- Esophageal Carcinoma InfoДокумент4 страницыEsophageal Carcinoma InfoCamilofonoОценок пока нет
- Angiomatous Leiomyoma of The Urachus: A Rare Entity Masquerading As Extraluminal Gastrointestinal Stromal TumorДокумент4 страницыAngiomatous Leiomyoma of The Urachus: A Rare Entity Masquerading As Extraluminal Gastrointestinal Stromal Tumordella elvira rosaОценок пока нет
- s40792 018 0489 1Документ7 страницs40792 018 0489 1Laura PredescuОценок пока нет
- Pancreatic Acinar Cell Carcinoma - Literature Review and Case of A 56-Year-Old Man Presenting With Abdominal PainДокумент5 страницPancreatic Acinar Cell Carcinoma - Literature Review and Case of A 56-Year-Old Man Presenting With Abdominal PainAndra KurniantoОценок пока нет
- Case ReportДокумент5 страницCase ReportIntan HaddadОценок пока нет
- Macronodular Hepatosplenic Tuberculosis: Case ReportДокумент3 страницыMacronodular Hepatosplenic Tuberculosis: Case ReportEnda RafiqohОценок пока нет
- Small Intestine TumorsДокумент8 страницSmall Intestine TumorspkotaphcОценок пока нет
- Omental RhabdoДокумент4 страницыOmental RhabdoDaisuke KiritoОценок пока нет
- LeíomaДокумент6 страницLeíomaStephanie OdriozolaОценок пока нет
- Aghiz 3Документ12 страницAghiz 3nandaaa aprilОценок пока нет
- Presentation of A Case of Mesenteric CystДокумент5 страницPresentation of A Case of Mesenteric CystAthenaeum Scientific PublishersОценок пока нет
- Fulltext 1Документ6 страницFulltext 1pathologyguruОценок пока нет
- Colon Adenocarcinoma With Metastasis To The GingivaДокумент3 страницыColon Adenocarcinoma With Metastasis To The GingivaSafira T LОценок пока нет
- Inverted Meckel's Diverticulum Causing Intussusception in An AdultДокумент2 страницыInverted Meckel's Diverticulum Causing Intussusception in An Adultlorenz_gtlОценок пока нет
- Optic Nerve PathologiesДокумент64 страницыOptic Nerve Pathologieshasan aslamОценок пока нет
- Verrucous CarcinomaДокумент12 страницVerrucous Carcinomaanatomimanusia100% (1)
- NCPДокумент2 страницыNCPNikai PabayoОценок пока нет
- Tog 12685Документ3 страницыTog 12685saeed hasan saeedОценок пока нет
- DUTY SDH + CKDДокумент6 страницDUTY SDH + CKDadelia putri wirandaniОценок пока нет
- Varicose VeinsДокумент4 страницыVaricose VeinsNur Hanani KhanОценок пока нет
- LESSON PLAN 6 MALARIA IN PREGNANCYjjДокумент13 страницLESSON PLAN 6 MALARIA IN PREGNANCYjjjrkedridgemwanakalandoОценок пока нет
- Cri Du ChatДокумент16 страницCri Du ChatJet LeeОценок пока нет
- Final NCP PediaДокумент2 страницыFinal NCP PediaKuro HanabusaОценок пока нет
- Listening A07Документ4 страницыListening A07qartzzОценок пока нет
- Health Assessment 21Документ4 страницыHealth Assessment 21shannon c. lewisОценок пока нет
- Psychotropic medications guide for depression, OCD and anxietyДокумент17 страницPsychotropic medications guide for depression, OCD and anxietyMJ Torralba100% (1)
- Nursing Case Analysis: Laparoscopic CholecystectomyДокумент19 страницNursing Case Analysis: Laparoscopic CholecystectomyChristopher MaОценок пока нет
- Pharmacotherapy of heart failureДокумент79 страницPharmacotherapy of heart failureAbera JamboОценок пока нет
- Abdomen in Acute-Critical Care MedicineДокумент50 страницAbdomen in Acute-Critical Care MedicineBejinaruOanaSiCristiОценок пока нет
- Older People - Patterns of IllnessДокумент4 страницыOlder People - Patterns of IllnessTweenie DalumpinesОценок пока нет
- .Au Files Dysbiosis ScoreДокумент2 страницы.Au Files Dysbiosis ScorekenetmartinОценок пока нет
- Feline Scabies, Case Report Pramodh Bernard 17BVM89Документ10 страницFeline Scabies, Case Report Pramodh Bernard 17BVM89pramodh bernardОценок пока нет
- T Alimentacion LibroДокумент485 страницT Alimentacion LibrodeadelcarmenОценок пока нет
- Consumer Chemistry: Quarter 4 - Module 4: Anticancer DrugsДокумент24 страницыConsumer Chemistry: Quarter 4 - Module 4: Anticancer DrugsShekina Joy SungaОценок пока нет
- NCMB 312 Rle Week 14 Dengue FeverДокумент3 страницыNCMB 312 Rle Week 14 Dengue FeverMada mada DaneОценок пока нет
- Retinal Detachment SlideДокумент54 страницыRetinal Detachment SlideHerin NataliaОценок пока нет
- Kista Bartholine NewДокумент12 страницKista Bartholine NewZulfy AzharyОценок пока нет
- Perceived Awareness of Clozapine Associated With Socio - Demographic Status, Clinical, and Side Effect Profile Among Patients From Mental Health Hospital, Taif, Saudi ArabiaДокумент8 страницPerceived Awareness of Clozapine Associated With Socio - Demographic Status, Clinical, and Side Effect Profile Among Patients From Mental Health Hospital, Taif, Saudi ArabiaJAVED ATHER SIDDIQUIОценок пока нет
- PPT Inggris DMДокумент9 страницPPT Inggris DMtria WidiastutiОценок пока нет
- Tumor of The EyeДокумент30 страницTumor of The EyenenyririОценок пока нет
- Coronavirus Reading ComprehensionДокумент1 страницаCoronavirus Reading ComprehensionMarianita TamagnoОценок пока нет
- Drug Study - OBДокумент10 страницDrug Study - OBArdhel LoslosoОценок пока нет
- TSO Medical GuidelinesДокумент42 страницыTSO Medical GuidelinesEmilio SantiagoОценок пока нет
- Clean CVДокумент25 страницClean CVassssadfОценок пока нет