Академический Документы
Профессиональный Документы
Культура Документы
McDonald To AG EPI - PEN - Letter
Загружено:
Matthew HamiltonОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
McDonald To AG EPI - PEN - Letter
Загружено:
Matthew HamiltonАвторское право:
Доступные форматы
THE ASSEMBLY
STATE OF NEW YORK
ALBANY
JOHN T. MCDONALD III
th
Assemblymember 108 District
COMMITTEES
Aging
Alcoholism and Drug Abuse
Cities
Insurance
Mental Health and
Developmental Disabilities
Real Property Taxation
September 21, 2016
Attorney General Eric Schneiderman
Office of the Attorney General
The Capitol
Albany, NY 12224-0341
Dear Attorney General Schneiderman:
First and foremost, I would like to extend my support for the recent investigation your office has opened in regard to the
potentially anti-competitive terms that the manufacturer of the EpiPen (Mylan) may have required in sales contracts with
school districts. The allegations, if true, are unacceptable and should be fixed. Public policy should be reviewed to correct
this type of behavior.
As you continue this investigation, I encourage you to expand this effort. I believe that there is more than a rogue
manufacturer in play in this game. As is widely known, the EpiPen has witnessed a 400% increase in price over the last
decade, while there has been no meaningful improvement to the product or expanded indications to justify a price increase.
During this time consumers, directly and indirectly have shouldered the burden of the cost. Directly in regard to their
copayments they have paid at the pharmacy register and indirectly through escalating health care premiums as abnormal
increased drug costs amongst other factors have played a role in the rising cost of health care. Government, employers and
consumers again, pay the price.
The lack of a generic alternative to EpiPen is an area that needs to be examined. Recently, a legislator introduced legislation
to enhance the substitution of EpiPen once a product comes to market. This legislation, while well intended, is not
necessary. Pharmacists have the opportunity already to substitute a less expensive alternative than the EpiPen. As a
pharmacist, I am aware of this product.
The product, Adrenaclick, has been on the market since 2013 and is a third of the price of EpiPen. The product and EpiPen
are both BX rated which means neither drug has an equivalent generic however; this does not prohibit generic substitution.
As background, most medications that are generically equivalent have an AB rating which by NYS law requires substitution
and therefore is mandatory unless a prescriber notates otherwise. For medications that are BX rated they are not required to
be substituted however, NYS Education Law allows a pharmacist, using his/her discretion, to substitute one product for the
other. Therefore, there is a generic for EpiPen. The issue is will anyone pay for it?
Knowing what is mentioned in the prior paragraph, one would logically assume that many EpiPen prescriptions are
substituted with the Adrenaclick brand, which is less expensive. Correct? Actually, it is not. I can attest to this fact first hand
as I practice pharmacy regularly. You will find it interesting to know that most prescription drug plans exclude the
Adrenaclick from coverage and therefore require the patient to secure the more costly EpiPen. Now at times the cost to the
patient may be negligible and at times it may not. But questions do arise including the following:
Room 417, Legislative Office Building, Albany, New York 12248 518-455-4474, FAX: 518-455-4727
EMAIL: mcdonaldj@assembly.state.ny.us
www.assembly.state.ny.us
Why are the brand name covered and the generic not?
What cost does the patient have attributed to their drug benefit when they receive the EpiPen vs the Adrenaclick,
many of which have plans that have medication cost ceilings?
What makes the more expensive medication less expensive when health insurance is involved?
Might it be the rebate that the manufacturer is guaranteeing to the Program Benefit Manager (PBM)?
Is the PBM sharing the rebate with the health plan?
Is the PBM sharing the rebate with the patient, or the employer or the governmental entity that is paying for the
EpiPen at the end of the day?
The questions above need to be asked because of the lack of transparency in the prescription drug benefit world. Now I am
not anti-PBM as they serve a role and purpose in regards to assisting management of prescription costs and also in measuring
outcomes which is what our health care system is moving in that direction. However, as a practicing pharmacist for over 32
years, it is clear that patient, employer, pharmacy and possibly even the health plan that contracts with the PBM are not
aware of what the true actual cost of the medication is at the end of the process. The issue is not just with EpiPen or Mylan.
This lack of knowledge, in my mind calls for your office to further the investigation. I would suggest a review of the New
York State government sponsored plans as well as NYSSHIP plans to acquire further information. I believe this issue is
larger than one would have originally thought. Recently, there have been reports about the middle class seeing for the first
time a rise in household income. That, unfortunately, is being negated by the rising cost of health care and the continued
pressure on employees to shoulder costs. This is impacting our working class families. We need to make sense of this issue,
especially as government continues to take on a more active role of subsidizing health care or managing it.
Thank you for your continued work and I am available for any further questions.
Sincerely,
Member of Assembly
John T. McDonald III
Room 417, Legislative Office Building, Albany, New York 12248 518-455-4474, FAX: 518-455-4727
EMAIL: mcdonaldj@assembly.state.ny.us
www.assembly.state.ny.us
Вам также может понравиться
- Joint Budget Schedule 2018 Release FINALДокумент1 страницаJoint Budget Schedule 2018 Release FINALMatthew HamiltonОценок пока нет
- 2018-19 Executive Budget Briefing BookДокумент161 страница2018-19 Executive Budget Briefing BookMatthew Hamilton100% (1)
- FY 18-19 Budget School Aid RunsДокумент15 страницFY 18-19 Budget School Aid RunsMatthew HamiltonОценок пока нет
- State of The State BingoДокумент5 страницState of The State BingoMatthew Hamilton100% (1)
- SNY0118 Crosstabs011518Документ3 страницыSNY0118 Crosstabs011518Matthew HamiltonОценок пока нет
- New York State Plastic Bag Task Force ReportДокумент88 страницNew York State Plastic Bag Task Force ReportMatthew Hamilton100% (1)
- SNY0118 Crosstabs011618Документ7 страницSNY0118 Crosstabs011618Nick ReismanОценок пока нет
- IDC Leader Jeff Klein Legal Memo Re: Sexual Harassment Allegation.Документ3 страницыIDC Leader Jeff Klein Legal Memo Re: Sexual Harassment Allegation.liz_benjamin6490Оценок пока нет
- 11-29-17 Heastie Letter To McLaughlin Re: McLaughlin InvestigationДокумент2 страницы11-29-17 Heastie Letter To McLaughlin Re: McLaughlin InvestigationMatthew HamiltonОценок пока нет
- 6-21-17 Ethics Committee Letter To Heastie Re: McLaughlin InvestigationДокумент3 страницы6-21-17 Ethics Committee Letter To Heastie Re: McLaughlin InvestigationMatthew HamiltonОценок пока нет
- Approval #64-66 of 2017Документ3 страницыApproval #64-66 of 2017Matthew HamiltonОценок пока нет
- 11-27-17 LetterДокумент5 страниц11-27-17 LetterNick ReismanОценок пока нет
- DiNapoli Debt Impact Study 2017Документ30 страницDiNapoli Debt Impact Study 2017Matthew HamiltonОценок пока нет
- 2018 State of The State BookДокумент374 страницы2018 State of The State BookMatthew HamiltonОценок пока нет
- 6-22-17 Heastie Letter To Ethics Committee Re: McLaughlin InvestigationДокумент1 страница6-22-17 Heastie Letter To Ethics Committee Re: McLaughlin InvestigationMatthew HamiltonОценок пока нет
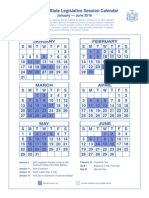
- 2016 Legislative Session CalendarДокумент1 страница2016 Legislative Session CalendarMatthew HamiltonОценок пока нет
- Rockefeller Instittue 106 Ideas For A Constitutional ConventionДокумент17 страницRockefeller Instittue 106 Ideas For A Constitutional ConventionMatthew HamiltonОценок пока нет
- Faso Scaffold Law BillДокумент4 страницыFaso Scaffold Law BillMatthew HamiltonОценок пока нет
- Comptroller's Fiscal Update: State Fiscal Year 2017-18 Receipts and Disbursements Through The Mid-YearДокумент10 страницComptroller's Fiscal Update: State Fiscal Year 2017-18 Receipts and Disbursements Through The Mid-YearMatthew HamiltonОценок пока нет
- DiNapoli Wall Street Profits Report 2017Документ8 страницDiNapoli Wall Street Profits Report 2017Matthew HamiltonОценок пока нет
- Gov. Andrew Cuomo Law Approval Message #6 - 2017Документ1 страницаGov. Andrew Cuomo Law Approval Message #6 - 2017Matthew HamiltonОценок пока нет
- Andrew Cuomo Letter To Jeff Bezos Re HQ2Документ2 страницыAndrew Cuomo Letter To Jeff Bezos Re HQ2Matthew HamiltonОценок пока нет
- USA V Pigeon 100617Документ29 страницUSA V Pigeon 100617Matthew HamiltonОценок пока нет
- SNY1017 CrosstabsДокумент6 страницSNY1017 CrosstabsNick ReismanОценок пока нет
- OSC Municipal Water Systems ReportДокумент14 страницOSC Municipal Water Systems ReportMatthew HamiltonОценок пока нет
- DiNapoli Federal Budget ReportДокумент36 страницDiNapoli Federal Budget ReportMatthew HamiltonОценок пока нет
- NYS DFS Credit Reporting Agency RegulationsДокумент6 страницNYS DFS Credit Reporting Agency RegulationsMatthew HamiltonОценок пока нет
- Gov. Andrew Immigration Status Executive OrderДокумент2 страницыGov. Andrew Immigration Status Executive OrderMatthew HamiltonОценок пока нет
- Siena College October 2017 PollДокумент8 страницSiena College October 2017 PollMatthew HamiltonОценок пока нет
- USA v. Skelos Appellate DecisionДокумент12 страницUSA v. Skelos Appellate DecisionMatthew HamiltonОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Steps To SuccessДокумент188 страницSteps To SuccessOmar Branch100% (2)
- English for Nurses GuidebookДокумент18 страницEnglish for Nurses GuidebookainigucciiОценок пока нет
- Family Health Dispute InfoДокумент1 страницаFamily Health Dispute InfoAzeem AhmedОценок пока нет
- Income Tax Midterm Exam KeyДокумент16 страницIncome Tax Midterm Exam KeyanggandakonohОценок пока нет
- HCA Letter Re DHCS Mitigation PlanДокумент6 страницHCA Letter Re DHCS Mitigation PlanPaul GlickmanОценок пока нет
- John Q Application Paper - EditedДокумент11 страницJohn Q Application Paper - EditedPaul WahomeОценок пока нет
- Hdi Forcasting v2 2Документ26 страницHdi Forcasting v2 2DannyMartinОценок пока нет
- Salve Vs Carague-Non-liability of Approving Authority On Disallowed PaymentsДокумент10 страницSalve Vs Carague-Non-liability of Approving Authority On Disallowed PaymentsattyleoimperialОценок пока нет
- 01 - Internal Audit Report - SecurityДокумент9 страниц01 - Internal Audit Report - SecurityVincent OngОценок пока нет
- List of Schemes of The Government of India - WikipediaДокумент12 страницList of Schemes of The Government of India - WikipediaKARTHIKEYAN MОценок пока нет
- Massachusetts Tattooing Statute ChallengedДокумент19 страницMassachusetts Tattooing Statute ChallengedsrwunschОценок пока нет
- Flyer - Taiwhakaea Airport Hui - Full VersionДокумент3 страницыFlyer - Taiwhakaea Airport Hui - Full VersionKarl TakotohiwiОценок пока нет
- Medical Certificate FormatДокумент1 страницаMedical Certificate FormatdevaismynameОценок пока нет
- Legal Research On Whether or Not A Barangay Has The Power To Temporarily Close A RoadДокумент2 страницыLegal Research On Whether or Not A Barangay Has The Power To Temporarily Close A RoadJoanne DiezОценок пока нет
- Literature Review On Family Planning Method in Slum Dwellers-AlamgirДокумент4 страницыLiterature Review On Family Planning Method in Slum Dwellers-AlamgirAuny Alamgir অনি আলমগীর100% (1)
- Health Facility Upgrade ProposedДокумент4 страницыHealth Facility Upgrade ProposedLGU PadadaОценок пока нет
- Operational Guidelines RBSKДокумент43 страницыOperational Guidelines RBSKanunad100% (1)
- Materiality and Sustainability Disclosure - SGX Top50 - Ernst & Young Thought Leadership Oct2015Документ20 страницMateriality and Sustainability Disclosure - SGX Top50 - Ernst & Young Thought Leadership Oct2015Krishna SadashivОценок пока нет
- Nabh Tertiary CareДокумент7 страницNabh Tertiary CareGold PANDIОценок пока нет
- Community Mental Health Current Scenario Dr. Manish KumarДокумент63 страницыCommunity Mental Health Current Scenario Dr. Manish KumarManish KumarОценок пока нет
- Infographic Violence Against Women en 11x17 No BleedsДокумент1 страницаInfographic Violence Against Women en 11x17 No BleedsEdward NoriaОценок пока нет
- Powers and Duties of Officers and Employees G.O.Ms - No.375 Animal Husbandry and Fisheries (AH-7) Department, Dated 13.07.1990Документ7 страницPowers and Duties of Officers and Employees G.O.Ms - No.375 Animal Husbandry and Fisheries (AH-7) Department, Dated 13.07.1990Patrick SaravananОценок пока нет
- Offer Letter Sasken Nancharaiah GudavalliДокумент3 страницыOffer Letter Sasken Nancharaiah GudavalliNancharaiah SandyОценок пока нет
- Dokumen - Tips - Hse P 44607 Hse Audit Inspection and Management VisitДокумент6 страницDokumen - Tips - Hse P 44607 Hse Audit Inspection and Management VisiteliОценок пока нет
- Quality, Costs, and Policy Factors InfluencingДокумент1 страницаQuality, Costs, and Policy Factors InfluencingRubi ZimmermanОценок пока нет
- Final Legal ResearchДокумент22 страницыFinal Legal ResearchIyleОценок пока нет
- Shouldice PDFДокумент2 страницыShouldice PDFRizvi SyedОценок пока нет
- January 2009 Room Assignments For Pharmacy Licensure ExaminationДокумент35 страницJanuary 2009 Room Assignments For Pharmacy Licensure ExaminationdericОценок пока нет
- BlotterДокумент6 страницBlotterrori ragaasОценок пока нет
- Philippines health insurance report details employee premium contributionsДокумент2 страницыPhilippines health insurance report details employee premium contributionsSuzette SubicoОценок пока нет