Академический Документы
Профессиональный Документы
Культура Документы
Causedoutbreak Klebsiella PDF
Загружено:
Jonathan WelchИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Causedoutbreak Klebsiella PDF
Загружено:
Jonathan WelchАвторское право:
Доступные форматы
Downloaded from http://bmjopen.bmj.com/ on September 27, 2016 - Published by group.bmj.
com
Open Access
Research
What caused the outbreak of ESBLproducing Klebsiella pneumoniae in a
neonatal intensive care unit, Germany
2009 to 2012? Reconstructing
transmission with epidemiological
analysis and whole-genome sequencing
Sebastian Haller,1,2 Christoph Eller,3,4 Julia Hermes,2 Martin Kaase,5
Matthias Steglich,3 Aleksandar Radonic,6 Piotr Wojtek Dabrowski,7
Andreas Nitsche,6 Yvonne Pfeifer,3 Guido Werner,3 Werner Wunderle,8
Edward Velasco,2 Muna Abu Sin,2 Tim Eckmanns,2 Ulrich Nbel3,9
To cite: Haller S, Eller C,
Hermes J, et al. What caused
the outbreak of ESBLproducing Klebsiella
pneumoniae in a neonatal
intensive care unit, Germany
2009 to 2012?
Reconstructing transmission
with epidemiological analysis
and whole-genome
sequencing. BMJ Open
2015;5:e007397.
doi:10.1136/bmjopen-2014007397
Prepublication history and
additional material is
available. To view please visit
the journal (http://dx.doi.org/
10.1136/bmjopen-2014007397).
SH, CE, TE and UN
contributed equally.
Received 7 December 2014
Revised 25 February 2015
Accepted 27 February 2015
For numbered affiliations see
end of article.
Correspondence to
Dr Sebastian Haller;
HallerS@rki.de
ABSTRACT
Objective: We aimed to retrospectively reconstruct the
timing of transmission events and pathways in order to
understand why extensive preventive measures and
investigations were not sufficient to prevent new cases.
Methods: We extracted available information from
patient charts to describe cases and to compare them
to the normal population of the ward. We conducted a
cohort study to identify risk factors for pathogen
acquisition. We sequenced the available isolates to
determine the phylogenetic relatedness of Klebsiella
pneumoniae isolates on the basis of their genome
sequences.
Results: The investigation comprises 37 cases and
the 10 cases with ESBL (extended-spectrum betalactamase)-producing K. pneumoniae bloodstream
infection. Descriptive epidemiology indicated that a
continuous transmission from person to person was
most likely. Results from the cohort study showed that
frequent manipulation (a proxy for increased exposure
to medical procedures) was significantly associated
with being a case (RR 1.44, 95% CI 1.02 to 2.19).
Genome sequences revealed that all 48 bacterial
isolates available for sequencing from 31 cases were
closely related (maximum genetic distance, 12 single
nucleotide polymorphisms). Based on our calculation
of evolutionary rate and sequence diversity, we
estimate that the outbreak strain was endemic since
2008.
Conclusions: Epidemiological and phylogenetic
analyses consistently indicated that there were
additional, undiscovered cases prior to the onset of
microbiological screening and that the spread of the
pathogen remained undetected over several years,
driven predominantly by person-to-person
transmission. Whole-genome sequencing provided
valuable information on the onset, course and size of
the outbreak, and on possible ways of transmission.
Strengths and limitations of this study
We highlight the complexity of nosocomial outbreaks and outbreak investigations.
We illustrate how microbiological and epidemiological methods may uncover pieces of a puzzle
that only when taken together can resolve the
whole picture of an outbreak situation.
Our study is limited to data and isolates collected
during the outbreak investigation. We could not
retrieve epidemiological data on all neonates and
had to make use of the available isolates collected during the investigation.
INTRODUCTION
On 28 February 2012, a German neonatal
intensive care unit (NICU) was closed due to
a large outbreak of ESBL-producing Klebsiella
pneumonia. It has remained closed ever since
(as on February 2015).1 In total, 37 infants
were affected by this outbreak. Among these,
10 cases developed a bloodstream infection.
Local public health authorities were rst
informed of the outbreak in September 2011
and convened an infection control team.
The hospital conducted a press conference
on 2 November 2011 to inform the public
about the outbreak. From then the outbreak
was discussed in the media for months, and a
parliamentary commission of the Bremen
parliament was established.1 2 By the time
the media was informed, the index case was
suspected to be a neonate who tested positive
for the outbreak strain in July 2011.
Throughout the outbreak, control measures were established with emphasis on
Haller S, et al. BMJ Open 2015;5:e007397. doi:10.1136/bmjopen-2014-007397
Downloaded from http://bmjopen.bmj.com/ on September 27, 2016 - Published by group.bmj.com
Open Access
hand hygiene, contact precautions, cohorting, personalisation of all medication and care products, and limiting
access to the units (eg, patient visits were restricted to
parents). Admission of new infants in the NICU was
ceased and the ward was closed on 5 November 2011 for
renovation; all movable material was discarded. The
NICU reopened on 9 January 2012; however, ve new
cases were detected in the NICU in February.
On 25 October 2011, a microbiological screening of
all infants in the NICU was introduced and then
extended to a twice weekly screening of all patients in
the paediatric clinic and an admission screening. More
than 270 staff members were screened twice, in
November 2011 and February 2012. Mothers on the
maternal ward were screened starting on 5 November
2011 ( perianal swabs). Mothers and staff were all
screened negative for the outbreak strain. More than
650 environmental samples were collected from the
NICU, other paediatric wards, the maternity ward and
the delivery room (>350 in 2011 and >300 in 2012),
including air, water, disinfectants and medical products.
Only ve environmental samples were ESBL-K. pneumoniae positive: a diaper scale, a sharps disposal, a baby
soother (used by a case) in 2011, a baby soother (used
by another case) and a cardboard box of gloves (9 days
after nal closure of the ward) in 2012.
Outbreaks due to multidrug-resistant K. pneumoniae
have been reported particularly in NICUs.35 They may
be difcult to control as K. pneumoniae can colonise the
gastrointestinal tract of patients without causing signs of
infections,6 acting as reservoirs for continued transmission.7 8 Other German hospitals have faced K. pneumoniae
outbreaks, but we are not aware of a nosocomial outbreak
in Germany that drew comparable public attention and
that has led to similar drastic consequences.
OBJECTIVE
We investigated this large, complex outbreak by combining epidemiological analysis with whole-genome sequencing. A combination of epidemiological analysis and
high-resolution, whole-genome sequencing has been
shown to be valuable for investigating outbreaks with
various bacterial pathogens, including K. pneumoniae.912
In particular, we aimed to retrospectively reconstruct the
timing of transmission events, date the start of the outbreak, and further elucidate possible sources in order to
understand why extensive measures and investigations
were insufcient to prevent new cases.1
METHODS
Setting
The paediatric clinic in Bremen, Germany, with about
160 beds, has more than 11 000 inpatients and about
40 000 outpatients per year, including paediatric surgery.
Neonates were treated in the NICU, the paediatric
intensive care unit (PICU), a paediatric surgical ward
and a rooming-in unit.
2
Confirmed case
Any patient treated in the paediatric clinic in Bremen
with the ESBL-K. pneumoniae outbreak strain (DNA
macrorestriction) detected prior to 15 May 2012.
Probable case
Patients having received treatment in the paediatric
clinic between 1 January 2011 and 15 May 2012, with
ESBL-K. pneumoniae record, but with no isolate available
for bacterial typing.
Data source
We extracted information from patient charts, the hospital information system and the laboratory information
system, and performed a retrospective case search within
these data sources. Variables such as gestational age,
birth weight, sex, exposures (eg, alimentation, procedures), outcomes (eg, microbiological ndings), as well
as information on the mother and the delivery of all
cases belonging to the outbreak and all non-cases in the
cohort study were extracted.
Descriptive epidemiology was applied to all cases for
whom information was retrieved. Subsequently, we compared cases born and identied between 1 January and
31 October 2011 to all neonates born during the same
time span, who received treatment in the paediatric
clinic for more than 12 h within the rst 7 days of life
(standard data set for quality assessment).
A retrospective cohort study included infants who were in
the NICU between 9 February and 28 February 2012 to
analyse reoccurrence of the outbreak strain. The time of
exposure for cases was dened as time since birth or last
negative screening until 1 day before rst detection of
ESBL-K. pneumoniae. The time of exposure for non-cases
was the length of hospital stay within the study period.
We tested the association of single exposures with being
a case, and tested combined variables as invasive measures and those exposures that led to frequent
manipulation.
Statistical analyses
We calculated relative risks and p values (signicance
level of p<0.05) using Poisson regression in Stata (Stata
V.12: StataCorp LP; 2011).
Bacterial strain typing
All conserved ESBL-K. pneumoniae that had been isolated
were analysed using DNA macrorestriction with XbaI and
subsequent pulsed-eld gel electrophoresis (PFGE) was
performed as previously described13 (see online supplementary methods).
Genome sequencing
We generated a reference genome sequence for the outbreak strain from isolate K. pneumoniae 234/12 (Pacic
Biosciences, 454/Roche, and Illumina technologies; see
online supplementary methods). For annotation, we
Haller S, et al. BMJ Open 2015;5:e007397. doi:10.1136/bmjopen-2014-007397
Downloaded from http://bmjopen.bmj.com/ on September 27, 2016 - Published by group.bmj.com
Open Access
used the RAST web pipeline (http://rast.nmpdr.org/)14
and the PHAST tools.15
Resequencing of DNA from 46 K. pneumoniae isolates
was performed by applying Illumina technology (see
online supplementary methods). We mapped the resulting paired-end reads to the reference genome sequence
to identify sequence variation (see online supplementary
methods). We inferred multilocus sequence types (STs)
from genome sequences. Sequence data were submitted
to the Sequence Read Archive at NCBI (BioProject
PRJNA 235888; http://www.ncbi.nlm.nih.gov/sra).
Phylogenetic analyses
An alignment of core genome single nucleotide polymorphisms (SNPs) assisted in the reconstruction of the
isolates phylogeny using the PhyML module in Seaview,
V.4.2.3. We then estimated evolutionary rates and divergence dates from an alignment of genome sequence
dates with the isolates recovery dates, by using BEAST
V.1.7.4 (http://beast.bio.ed.ac.uk; see online supplementary methods).
Ethics
A formal ethical review process and approval was not
required for this outbreak investigation in accordance
with article 25, section 1 of the German Infection
Protection Act of 2001.
RESULTS
Descriptive epidemiological analysis
In total, we identied 37 cases (31 (84%) conrmed
cases and 6 (16%) probable cases (epidemiological data
were retrievable for 35 (95%) cases)). Using retrospective case search we identied 6 cases (2 conrmed and 4
probable) that were tested ESBL-K. pneumoniae positive
prior to the supposed index case (case 12, July 2011).
There were 46 isolates available for sequencing: 38 isolates from 31 cases, 5 environmental isolates and 2 isolates from patients from the hospital without
epidemiological link and 1 isolate of a similar strain
from Poland.
The majority (n=33, 89%) of cases was born preterm
(gestational age, <37+0), 10 (27%) cases developed a
bloodstream infection with the outbreak strain, and 7
(19%) died (all-cause mortality).
Between 30 April 2011 and 28 February 2012, at least
one case was permanently hospitalised in the paediatric
clinic; 65% of cases were on the same ward as another
case within 7 days prior to rst detection, and 90% of
cases had been treated in the NICU (gure 1).
We analysed a data set of neonates born between
January and November 2011 and treated in the paediatric clinic (n=310, including 20 cases). The cases had a
lower birth weight and a lower gestational age, and
developed sepsis signicantly more often than non-cases
(table 1). However, when adjusted for birth weight and
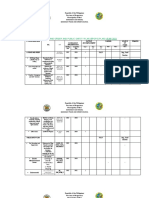
Figure 1 Timeline of the outbreak. The index patient (case 1), isolate from 01.01.2009 (day 1 of the outbreak) was
retrospectively found to belong to the outbreak. Eight hundred and fifty days later the second case was tested positive. Black line
between day 1 and day 827 represents time span with no additional information on cases. Time intervals of 10 days between
vertical lines compressed whenever additional information was not lost. Data on case 37 are not presented in this figure. (Note:
After discharge many infants came back to hospital for day hospital visits during which they were treated by members of the
same team treating infants on neonatal intensive care unit (NICU) and paediatric intensive care unit. Sixty-five per cent of cases
were on the same ward as another case within 7 days prior to first detection. Thirty-three cases were exposed to the NICU.)
Haller S, et al. BMJ Open 2015;5:e007397. doi:10.1136/bmjopen-2014-007397
Downloaded from http://bmjopen.bmj.com/ on September 27, 2016 - Published by group.bmj.com
Open Access
Table 1 Comparison of cases with non-cases
Sex
Multiples
Birth weight (g)
Gestational age (weeks)
Fatalities
Sepsis
Male
Yes
Median (range)
Median (range)
Yes
Yes/no
Cases (n=20)
Non-cases (n=290)
RR*
95% CI
p Value
13 (65%)
8 (40%)
1105 (6202640)
27+5 (24+236+2)
4 (20%)
9 (45%)
149 (51%)
76 (26%)
2400 (4684,87)
35+6 (24+342+6)
22 (8%)
41 (14%)
1.69
1.79
0.26
0.77
2.73
4.25
0.63 to 5.02
0.64 to 4.77
0.14 to 0.49
0.695 to 0.858
0.66 to 8.46
1.56 to 11.29
0.36
0.30
<0.001
<0.001
0.16
0.005
Twenty cases born and identified between 1 January and 31 October 2011, and 290 non-cases born in the same time period treated in the
paediatric clinic, univariable analysis.
*Relative risk (RR) and p values calculated using Poisson regression or exact Poisson regression (where possible) and corresponding 95% CI.
All fatalities among cases and non-cases counted, not differentiating causes.
gestational age, the association with sepsis was no longer
signicant (RR 1.50; 95% CI 0.56 to 4.02).
Cohort study
Twenty infants were included in this cohort, comprising
5 cases and 15 non-cases. One case had a Klebsiella sepsis
and two cases died. Birth weight, gestational age and
gender did not differ signicantly between cases and
controls. Analysing exposures we found a signicant
association with the combined variables as proxy for frequent manipulation (RR 1.44; 95% CI 1.02 to 2.19 for 1
point increase). Infants had up to 10 points in the combined variable, indicating an increased risk up to 14-fold
of becoming a case (table 2).
Genetic population structure
ST514 had not been observed in Germany previously, but
was reported in two neonatal patients at a university hospital in Poland in 1996.16 De novo genome sequencing of
our isolate 234/12 by combining Pacic Biosciences and
Illumina sequencing technologies revealed that the outbreak strain displayed large-scale genomic differences to
the historic ST514 isolate (316/12) from 1996, including the acquisition and/or restructuring of prophages.
We then resequenced the genomes from 46 K. pneumoniae isolates by applying Illumina sequencing technology
(see online supplementary table S1), and polymorphisms
in the core genome were identied by mapping sequencing reads to the genome sequence from the reference
isolate 234/12. All 44 ST514 outbreak isolates carried the
ESBL gene blaCTX-M-15 and the -lactamase genes blaTEM-1
and blaSHV-63. All these isolates were resistant to ampicillin, cefotaxime and ceftazidime, but they were susceptible
to carbapenems (see online supplementary table S1).
Among ST514 isolates from the outbreak in the paediatric clinic, we discovered a total of only 61 SNPs, illustrating their close relationship. Two short runs of adjacent
SNPs (each consisting of 2 SNPs with a distance on the
chromosome of 84 and 358 base pairs, respectively) and
one homoplasious SNP (see online supplementary
table S2) were signatures of potential recombination
events. For phylogenetic analyses, we removed these ve
potentially recombined SNPs from the data set to avoid
any obfuscation of the phylogenetic signal. Of the
remaining 56 SNPs, 13 were parsimony-informative (ie,
they occurred in >1 haplotype), enabling the reconstruction of a unique phylogenetic tree (homoplasy index, 0.0;
gure 2). When this tree was rooted with the genome
from an older ST514 isolate (316/12, Poland, 1996), the
earliest isolate from the paediatric clinic (267/12, from
2009) sat closest to the root (see online supplementary
gure S1). In a minimum spanning tree for our data set
Table 2 Cohort study 2012; selected devices and procedures during the study period (9 February to 28 February 2012)
Personal characteristics, exposure
Cases (n=5)
Non-cases (n=15)
RR
CI
Sex
Multiples
Birth weight (g)
Gestational age (weeks+days)
Central venous catheter
Umbilical catheter
Arterial catheter
Mechanical ventilation
Surfactant
Frequent manipulation (010)*
3 (60%)
0 (0%)
1800 (4983000)
31+2 (24+236+3)
4 (80%)
4 (80%)
3 (60%)
3 (60%)
3 (60%)
7 (410)
7 (47%)
2 (13%)
2300 (6134210)
34+2 (24+142+1)
6 (40%)
2 (13%)
0 (0%)
4 (27%)
2 (13%)
4 (07)
1.5
1.3
1.0
0.9
4.0
9.3
8.5
2.8
4.5
1.4
0.2
0.0
1.0
0.7
0.4
0.9
1.0
0.3
0.5
1.0
Male
Yes/no
Median (range)
Median (range)
Yes
Yes
Yes
Yes
Yes
Median (range)
p Value
to 18.0
to 9.82
to 1.0
to 1.1
to 197.0
to 459.6
to 101.8
to 33.4
to 53.9
to 2.2
1.00
1.00
0.50
0.21
0.38
0.06
0.05
0.47
0.21
0.04
Univariable exact Poisson regression and corresponding 95% CI.
*Combined variables as proxy for frequent manipulation (administration of eye drops (1)+continuous positive airway pressure (1)+radiograph
(1)+ECG (1)+physiotherapy (1)+umbilical catheter (1)+central venous catheter (1)+arterial catheter (1)+urinary catheter (1)+administration of
surfactant (1)+mechanical ventilation (1)+blood transfusion (1)).
Haller S, et al. BMJ Open 2015;5:e007397. doi:10.1136/bmjopen-2014-007397
Downloaded from http://bmjopen.bmj.com/ on September 27, 2016 - Published by group.bmj.com
Open Access
Figure 2 Maximum-likelihood phylogenetic tree based on sequence variation in the core genome (5.2 Mio base pairs) from
ESBL-producing Klebsiella pneumoniae isolates representing the outbreak investigated. The tree was rooted by using isolate
316/12 (ST514, collected in Poland in 1996). Patient numbers, environmental sample numbers and isolation dates are indicated.
Where multiple isolates from individual patients were available, these are numbered consecutively. Phylogenetic clades 1, 2 and
3 are indicated. SNP, single nucleotide polymorphism; ST, sequence type.
of 43 isolates, 40 isolates clustered in three clades (clades
1, 2 and 3; gure 3) that were fully congruent with clades
in a maximum-likelihood tree (gure 2). However, the
minimum spanning tree allowed ancestral isolates to
occupy internal nodes, which may reect the underlying
transmission tree more closely.17 While DNA macrorestriction (PFGE) enabled identication of the outbreak
strain, pulsotype subgroups differing from each other by
one or two bands were not concordant with SNP-based
phylogeny, since several of these subgroups were found in
more than one of the three phylogenetic clades
(gure 2).
Evolutionary rate and age of outbreak strain
Based on our set of genome sequences from isolates
that had been sampled serially over time, we estimated
that this K. pneumoniae strain has accumulated point
mutations in its core genome at a rate of three mutations per genome and year (5.5107 substitutions per
nucleotide site and year; 95% CI 2.9107 to 8.4107).
This short-term evolutionary rate is similar to rates
recently reported for Clostridium difcile,18 Mycobacterium
tuberculosis19 and Vibrio cholerae,20 but lower than that of
Staphylococcus aureus.21 22 Based on this evolutionary rate
and the sequence diversity of our data set, the time
Haller S, et al. BMJ Open 2015;5:e007397. doi:10.1136/bmjopen-2014-007397
estimation of the most recent common ancestor of the
K. pneumoniae outbreak strain was the beginning of 2008
(95% CI 2006 to 2009). Of note, virtually the same rate
and dates were calculated after removal of the single
isolate from 2009.
Diversity of K. pneumoniae within individual patients
From each of six individual patients, two to three isolates
were available. In two of these cases ( patients 16 and
35), two to three isolates collected up to 65 days apart
had fully identical genomes, and in two cases ( patients
34 and 29), the isolates sampled 93 and 112 days apart,
respectively, differed by one to two SNPs (gure 2). This
result is consistent with the average short-term evolutionary rate and suggests that the diversity within individual
patients may be low. In contrast, two isolates from
patient 17 collected 127 days apart differed by ninepoint mutations, yet clustered together in the phylogenetic tree (gure 2). Two isolates from patient 12
sampled 138 days apart were afliated with separate clusters in the phylogenetic tree (gure 2). These ndings
could be due to reinfection with a related strain and/or
the continuous presence of diverse pathogen populations within these individuals.
5
Downloaded from http://bmjopen.bmj.com/ on September 27, 2016 - Published by group.bmj.com
Open Access
Figure 3 Minimum spanning tree (constructed by using Bionumerics software) based on the same sequence data as the
maximum-likelihood tree in figure 2. The root of the tree was determined by comparison to the genome from isolate 316/12
(ST514, collected in Poland in 1996). Colours indicate isolation dates. Where multiple isolates from individual patients were
available, these are numbered consecutively. Phylogenetic clades 1, 2 and 3 are indicated. The asterisk marks the multifurcation
point in the tree that is referred to in the text (ST, sequence type).
DISCUSSION
Epidemiological links and microbiological results
suggest an outbreak of 37 affected infants
(31 conrmed cases). ST514 has not been reported
from other sites in Germany, including hospitals, which
indicates that this ST is rare. We provide evidence for a
person-to-person transmission and for undetected cases,
which helps to better understand why the extensive
hygiene measures may have been insufcient to stop
transmission.
Extent of the outbreak
Our investigation indicates that undetected cases must
have occurred within the paediatric clinic prior to the
onset of microbiological screening. Before screening was
introduced, cases were identied only if they had developed signs of infection or if mechanical ventilation had
prompted a microbiological screening (it was current
practice on the ward to perform microbiological screening of sputum in mechanically ventilated infants).
Accordingly, the proportion of cases with Klebsiella sepsis
was 50% before implementation of screening, decreasing to 10% after. When microbiological screening
started in the NICU (25 October 2011), seven new cases
were detected within 12 days, also suggesting a formerly
high prevalence of undetected cases. One case, a termborn infant who had stayed in the NICU in June 2011,
in whom the colonisation with the outbreak strain was
6
only detected in December 2011, after the infant had
been actively screened for ESBL-K. pneumoniae months
after discharge. No other risk factors had been reported
for this case, leaving the stay in the NICU the most
plausible time of outbreak strain acquisition (gure 1).
Accordingly, outbreak isolates sampled in 2011 displayed considerable genomic diversity, since all three
clades (gure 3) were already present, and the multifurcation point in the minimum spanning tree (labelled
with an asterisk in gure 3) reects the lack of specimens from before 2011.
Before the introduction of microbiological screening,
the timeframe during which transmission could occur
was often long (up to 445 days). Extensive barrier precautions were not in place during time periods in which
carriers of the outbreak strain remained undetected.
Risk factors for being a case in our investigation were
low gestational age and low birth weight, which conrms
risk factors identied in previous outbreak reports.11
Beginning of the outbreak
The spread of the pathogen remained undetected for
approximately 3 years. Prior to our retrospective case
search, the outbreak was assigned a start date of 22 July
2011. However, we were able to identify earlier cases,
including one from 2009: Based on genome sequence
variation that we found among outbreak isolates and
considering the evolutionary rate at which point
Haller S, et al. BMJ Open 2015;5:e007397. doi:10.1136/bmjopen-2014-007397
Downloaded from http://bmjopen.bmj.com/ on September 27, 2016 - Published by group.bmj.com
Open Access
mutations accumulated over time, we estimated that the
outbreak strain had been endemic in the hospital since
2008.
Pathogen reservoir and transmission pathways
Person-to-person pathogen spread is most likely, although
we could not directly identify a responsible vehicle of
transmission. The outbreak strain was continuously
present in the NICU during the study period (gure 1).
Genome sequence data supported patient-to-patient
transmission as the principle route of pathogen spread,
since in the minimum spanning tree (gure 3) all but
one furcation nodes in clades 1, 2 and 3 are occupied by
isolates sampled from patients, rather than from parents,
staff or any environmental source. In contrast, repeated
introductions of the pathogen from a common source
would have resulted in a star-like tree, and introductions
from multiple external sources would have resulted in
greater diversity that would have been only partially
represented by the strain collection from the ward.
Evidence of the critical role of hand hygiene was provided by the cohort study, which showed a signicant
association with the compound score for frequent
manipulation (table 2). When environmental investigations were intensied, increased numbers of pathogens
(not the outbreak strain) were detected on personnel
hands, gowns and hand contact places (ie, pager or box
of gloves).
Understafng and overcrowding have repeatedly been
described as risk factors for increased infection rates
and the occurrence of outbreaks.23 Nonetheless, the
median patient/nurse ratio in the NICU in 2011 was
3.0, and repeatedly one nurse had to take care of more
than ve neonates (data not shown).
Drastic measures were implemented to control the
outbreak during the last months of 2011, including stopping admissions, closure and renovation of the NICU.
Nevertheless, phylogenetic clades 2 and 3 were present
before and after reopening of the NICU (gures 2
and 3). Moreover, the positions of isolates from 2012
in the minimum spanning tree show that at least two
different genotypes (cases 3236, clades 2 and 3;
gure 3) were introduced into the ward following the
renovation.
Repeated screenings of staff did not detect any
ESBL-producing K. pneumoniae. Likewise, the outbreak
strain was neither detected among mothers on the
maternal ward nor among patients from other wards, or
from other hospitals within the area. It is unlikely that
the outbreak clone was endemic in the wider geographic
area. Genomic relatedness of K. pneumoniae isolates supported the notion that patients constituted a reservoir
for the pathogen, as several neonates were colonised
with unique strains for several months (gure 2).
Notably, closely related isolates were collected from each
of two patients (cases 17 and 29) before and after renovation of the NICU (gure 2), suggesting that the pathogen may have been reintroduced into the NICU by
Haller S, et al. BMJ Open 2015;5:e007397. doi:10.1136/bmjopen-2014-007397
person-to-person transmission. Case 29 was rehospitalised in the PICU 20 days before birth of case 32. Case
17 was rehospitalised in the PICU only 1 day before
birth of case 32. Further undetected cases hospitalised
in 2012 may have reintroduced the outbreak strain
through outpatient visits in 2012.
Environmental investigation
Environmental screenings yielded ve K. pneumoniae
isolates that were closely related to the outbreak strain
(see online supplementary table S1). Coincidentally,
genomes from these isolates (sampled from a box of
gloves, a diaper scale, a sharps disposal and baby soothers, respectively) occupied peripheral positions of the
minimum spanning tree (gure 2), ruling out these contaminated materials as spreading hubs. The nding of
the outbreak strain in a box of gloves 9 days after closure
of the ward demonstrates the remarkable viability of
Klebsiella on inanimate surfaces. Additional boxes of
gloves (including unopened ones) tested negative, suggesting that the single positive tested box of gloves was
most likely contaminated by insufciently disinfected
hands. Tests performed by a specialised laboratory
showed that the outbreak strain was sensitive to the disinfectants used in the clinic.
LIMITATIONS
Most data on exposures were collected from patient
records. Within these we found systematic inconsistencies in documentation and missing data on epidemiologically important information, like room number,
attending personnel and incubator number. Use of skin
disinfectant (eg, for umbilical cord care) was more frequently documented in known cases than in non-cases,
even though a standard procedure applied to all newborns. Furthermore, by extending barrier precautions
and moving the NICU, medical procedures and thereby,
the exposures may have changed.
While genome sequencing provided improved discriminatory power when compared with other typing
methods,9 11 12 the short-term evolutionary rate in
K. pneumoniae of three base substitution per genome per
year on average, as measured here, is unlikely to allow the
reliable tracking of specic transmission events between
individuals, which occur on much shorter time scales.
Resolution could have likely been improved by including
multiple isolates from each individual neonate, which
were not sufciently available in the present investigation.
CONCLUSIONS AND RECOMMENDATIONS
Late detection and thereby, delayed extensive response
may have contributed to the difculties in controlling
this outbreak. Our analyses suggest that there were
numerous unknown cases and that measures, such as
cohorting and barrier nursing, were only applied to
known cases. The outbreak spread from the NICU to
other wards of the paediatric clinic, and readmissions of
7
Downloaded from http://bmjopen.bmj.com/ on September 27, 2016 - Published by group.bmj.com
Open Access
known and unknown cases may have reintroduced the
outbreak strain into the NICU.
While in the present analysis, extensive sequencing
was applied retrospectively only, genomic diversity of K.
pneumoniae isolates from patients and environmental
samples clearly indicated that the duration and extent of
the outbreak had been underestimated. Further,
sequence data provided evidence for the patients being
the reservoir of the pathogen and it ruled out environmental contamination as a major route of spread.
Surveillance systems for outbreak detection with standardised evaluation of pathogen clusters should be
established, especially on wards with highly susceptible
populations. Having this valuable information during
real-time outbreak situations would improve infection
control and prevention measures by elucidating the start
and extent of the outbreak, conrming possible transmission routes and identifying most probable sources.
Since January 2012, the German Commission for
Hospital Hygiene and Infectious Disease Prevention
(KRINKO) recommends weekly microbiological screening for multiresistant Gram-negative pathogens and
Methicillin-resistant Staphylococcus aureus (MRSA) in all
very low birthweight infants (<1500 g) in Germany.24 25
Author affiliations
1
Postgraduate Training for Applied Epidemiology, Berlin, Germany, affiliated to
the European Programme for Intervention Epidemiology Training, European
Centre for Disease Prevention and Control, Stockholm, Sweden
2
Division of Healthcare-Associated Infections, Surveillance of Antimicrobial
Resistance and Consumption, Department for Infectious Disease
Epidemiology, Robert Koch Institute, Berlin, Germany
3
Division of Nosocomial Pathogens and Antibiotic Resistances, Department
for Infectious Diseases, Robert Koch Institute, Wernigerode, Germany
4
Department of Laboratory Medicine, University Hospital Halle, Halle,
Germany
5
Department of Medical Microbiology, Ruhr-University Bochum, Bochum,
Germany
6
Centre for Biological Threats and Special Pathogens, Highly Pathogenic
Viruses, Robert Koch Institute, Berlin, Germany
7
Central Administration Department, Information Technology, Robert Koch
Institute, Berlin, Germany
8
Department of Public Health, Gesundheitsamt Bremen (Local Public Health
Service), Bremen, Germany
9
DZIF Group on Microbial Genome Research, Leibniz Institute DSMZ
(Deutsche Sammlung von Mikroorganismen und Zellkulturen), Braunschweig,
Germany
Acknowledgements The authors want to thank the personnel of the
paediatric clinic, and especially the NICU and PICU team without whom the
outbreak investigation would have been impossible. They thank Susanne
Schink, Anja Takla, Cornelius Remschmidt, Kristin Tolksdorf, Katharina Alpers
and all other members of the outbreak investigation team. They are grateful to
Marek Gniadkowski and Janusz Fiett for the provision of Klebsiella
pneumoniae ST514 isolate (316/12, Poland, 1996) and to Jule Hinzmann for
excellent technical assistance. They also thank Sybille Mller-Bertling and
Christine Gnther for their excellent technical assistance and Ren W Rollet
for help with Spades software. Further they thank Brbel Christiansen for
analysing sensitivity of the outbreak strain to disinfectant, and Rainer
Podschun for analysis of the Klebsiella capsule.
Contributors SH, JH, WW, EV, MAS and TE were part of the outbreak team
and conducted the epidemiological outbreak investigations. MK, MS, AR,
PWD, AN, YP, GW and UN conducted the microbiological investigations. SH,
CE, TE and UN conceptualised the studies. SH, CE, TE and UN drafted the
manuscript. All authors critically revised the manuscript and approved the
final version. SH is corresponding author and guarantor.
Funding This work was partially funded by a grant from the Federal Ministry
for Research and Technology (BMBF), Germany (no. 01KI1013E to G. W.).
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement No additional data are available.
Open Access This is an Open Access article distributed in accordance with
the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license,
which permits others to distribute, remix, adapt, build upon this work noncommercially, and license their derivative works on different terms, provided
the original work is properly cited and the use is non-commercial. See: http://
creativecommons.org/licenses/by-nc/4.0/
REFERENCES
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
Tuffs A. Neonatal ward in Bremen is closed down again after two
more deaths of babies. BMJ 2012;344:e1680.
Tuffs A. Poor hospital hygiene is blamed for deaths of three babies
in Bremen. BMJ 2011;343:d7396.
Benenson S, Levin PD, Block C, et al. Continuous surveillance to
reduce extended-spectrum beta-lactamase Klebsiella pneumoniae
colonization in the neonatal intensive care unit. Neonatology
2013;103:15560.
Harris AD, McGregor JC, Johnson JA, et al. Risk factors for
colonization with extended-spectrum beta-lactamase-producing
bacteria and intensive care unit admission. Emerg Infect Dis
2007;13:11449.
Sumer S, Turk Dagi H, Findik D, et al. Two outbreaks due to
Esbl-producing Klebsiella pneumoniae in a neonatal intensive care
unit. Pediatr Int 2014;56:2226.
Selden R, Lee S, Wang WL, et al. Nosocomial klebsiella infections:
intestinal colonization as a reservoir. Ann Intern Med
1971;74:65764.
Gastmeier P, Vonberg RP. Klebsiella spp. in endoscopy-associated
infections: we may only be seeing the tip of the iceberg. Infection
2014;42:1521.
Jarvis WR, Munn VP, Highsmith AK, et al. The epidemiology of
nosocomial infections caused by Klebsiella pneumoniae. Infect
Control 1985;6:6874.
Koser CU, Holden MT, Ellington MJ, et al. Rapid whole-genome
sequencing for investigation of a neonatal MRSA outbreak. N Engl J
Med 2012;366:226775.
Eyre DW, Cule ML, Wilson DJ, et al. Diverse sources of C. difficile
infection identified on whole-genome sequencing. N Engl J Med
2013;369:1195205.
Nbel U, Nachtnebel M, Falkenhorst G, et al. MRSA transmission on
a neonatal intensive care unit: epidemiological and genome-based
phylogenetic analyses. PLoS ONE 2013;8:e54898.
Snitkin ES, Zelazny AM, Thomas PJ, et al. Tracking a hospital
outbreak of carbapenem-resistant Klebsiella pneumoniae with
whole-genome sequencing. Sci Transl Med 2012;4:148ra16.
Tenover FC, Arbeit RD, Goering RV, et al. Interpreting chromosomal
DNA restriction patterns produced by pulsed-field gel
electrophoresis: criteria for bacterial strain typing. J Clin Microbiol
1995;33:22339.
Aziz RK, Bartels D, Best AA, et al. The RAST Server: rapid
annotations using subsystems technology. BMC Genomics
2008;9:75.
Zhou Y, Liang Y, Lynch KH, et al. PHAST: a fast phage search tool.
Nucleic Acids Res 2011;39(Web Server issue):W34752.
Fiett J, Palucha A, Miaczynska B, et al. A novel complex mutant
beta-lactamase, TEM-68, identified in a Klebsiella pneumoniae
isolate from an outbreak of extended-spectrum
beta-lactamase-producing Klebsiellae. Antimicrob Agents
Chemother 2000;44:1499505.
Jombart T, Eggo RM, Dodd PJ, et al. Reconstructing disease
outbreaks from genetic data: a graph approach. Heredity
2011;106:38390.
He M, Miyajima F, Roberts P, et al. Emergence and global spread of
epidemic healthcare-associated Clostridium difficile. Nat Genet
2013;45:10913.
Roetzer A, Diel R, Kohl TA, et al. Whole genome sequencing versus
traditional genotyping for investigation of a Mycobacterium
Haller S, et al. BMJ Open 2015;5:e007397. doi:10.1136/bmjopen-2014-007397
Downloaded from http://bmjopen.bmj.com/ on September 27, 2016 - Published by group.bmj.com
Open Access
20.
21.
22.
23.
tuberculosis outbreak: a longitudinal molecular epidemiological
study. PLoS Med 2013;10:e1001387.
Mutreja A, Kim DW, Thomson NR, et al. Evidence for several waves
of global transmission in the seventh cholera pandemic. Nature
2011;477:4625.
Harris SR, Feil EJ, Holden MT, et al. Evolution of MRSA during
hospital transmission and intercontinental spread. Science
2010;327:46974.
Nbel U, Dordel J, Kurt K, et al. A timescale for evolution, population
expansion, and spatial spread of an emerging clone of methicillinresistant Staphylococcus aureus. PLoS Pathog 2010;6:e1000855.
Clements A, Halton K, Graves N, et al. Overcrowding and
understaffing in modern health-care systems: key determinants in
Haller S, et al. BMJ Open 2015;5:e007397. doi:10.1136/bmjopen-2014-007397
24.
25.
methicillin-resistant Staphylococcus aureus transmission. Lancet
Infect Dis 2008;8:42734.
Robert Koch Institute. Mitteilung der Kommission fr
Krankenhaushygiene und Infektionsprvention: Ergnzende
Empfehlung (2011) zur Prvention nosokomialer Infektionen
bei neonatologischen Intensivpflegepatienten mit einem
Geburtsgewicht unter 1.500 g (2007). Epidemiologisches Bull
2012;2/2012:1315.
Christoph J, Dame C, Eckmanns T, et al. Praktische Umsetzung
sowie krankenhaushygienische und infektionsprventive
Konsequenzen des mikrobiellen Kolonisationsscreenings bei
intensivmedizinisch behandelten Frh- und Neugeborenen.
Epidemiologisches Bull 2013;42/2013:42131.
Downloaded from http://bmjopen.bmj.com/ on September 27, 2016 - Published by group.bmj.com
What caused the outbreak of
ESBL-producing Klebsiella pneumoniae in a
neonatal intensive care unit, Germany 2009 to
2012? Reconstructing transmission with
epidemiological analysis and whole-genome
sequencing
Sebastian Haller, Christoph Eller, Julia Hermes, Martin Kaase, Matthias
Steglich, Aleksandar Radonic, Piotr Wojtek Dabrowski, Andreas Nitsche,
Yvonne Pfeifer, Guido Werner, Werner Wunderle, Edward Velasco, Muna
Abu Sin, Tim Eckmanns and Ulrich Nbel
BMJ Open 2015 5:
doi: 10.1136/bmjopen-2014-007397
Updated information and services can be found at:
http://bmjopen.bmj.com/content/5/5/e007397
These include:
Supplementary Supplementary material can be found at:
Material http://bmjopen.bmj.com/content/suppl/2015/05/11/bmjopen-2014-007
397.DC1.html
References
This article cites 22 articles, 6 of which you can access for free at:
http://bmjopen.bmj.com/content/5/5/e007397#BIBL
Open Access
This is an Open Access article distributed in accordance with the Creative
Commons Attribution Non Commercial (CC BY-NC 4.0) license, which
permits others to distribute, remix, adapt, build upon this work
non-commercially, and license their derivative works on different terms,
provided the original work is properly cited and the use is
non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Email alerting
service
Receive free email alerts when new articles cite this article. Sign up in the
box at the top right corner of the online article.
Topic
Collections
Articles on similar topics can be found in the following collections
Epidemiology (1700)
Genetics and genomics (96)
Infectious diseases (461)
Paediatrics (485)
Public health (1757)
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/
Downloaded from http://bmjopen.bmj.com/ on September 27, 2016 - Published by group.bmj.com
Notes
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/
Вам также может понравиться
- Petersen 2001Документ30 страницPetersen 2001Bianca MagnelliОценок пока нет
- Extensively Drug-Resistant Tuberculosis in Children With HumanДокумент12 страницExtensively Drug-Resistant Tuberculosis in Children With Humanromeoenny4154Оценок пока нет
- Ped PCR PL PedДокумент8 страницPed PCR PL PedjhonellyОценок пока нет
- 33 Sneha EtalДокумент7 страниц33 Sneha EtaleditorijmrhsОценок пока нет
- Infectious Mononucleosis Due To Epstein-Barr Virus Infection in Children - A Profile From Eastern IndiaДокумент7 страницInfectious Mononucleosis Due To Epstein-Barr Virus Infection in Children - A Profile From Eastern IndiaEmilia LunguОценок пока нет
- My Paper PDFДокумент8 страницMy Paper PDFSinh TranОценок пока нет
- Antecedentes INFECTOLOGYДокумент40 страницAntecedentes INFECTOLOGYDr. Claro RichardОценок пока нет
- Jurnal InfeksiДокумент10 страницJurnal InfeksiIkhsan AliОценок пока нет
- Epidemiologi of HFMDДокумент16 страницEpidemiologi of HFMDJimmy AmbaritaОценок пока нет
- Pneumonia Etiology Research for Child Health Project: A 21st Century Childhood Pneumonia Etiology StudyДокумент9 страницPneumonia Etiology Research for Child Health Project: A 21st Century Childhood Pneumonia Etiology StudyZuna QaziОценок пока нет
- N.sepsis 2Документ129 страницN.sepsis 2cooldude_secbad1712100% (1)
- Research Article: The Analysis of Etiology and Risk Factors For 192 Cases of Neonatal SepsisДокумент7 страницResearch Article: The Analysis of Etiology and Risk Factors For 192 Cases of Neonatal Sepsisflorentina lulutОценок пока нет
- Neumonia Complicada PDFДокумент9 страницNeumonia Complicada PDFadriana gallardoОценок пока нет
- Community-Acquired Pneumonia Requiring Hospitalization Among U.S. ChildrenДокумент11 страницCommunity-Acquired Pneumonia Requiring Hospitalization Among U.S. ChildrenParasОценок пока нет
- CMV, Tosoplasma, Rubeóla, Herpes SimpleДокумент13 страницCMV, Tosoplasma, Rubeóla, Herpes SimplePau PuenteОценок пока нет
- Dengue Hemorrhagic Fever in Infants: A Study of Clinical and Cytokine ProfilesДокумент12 страницDengue Hemorrhagic Fever in Infants: A Study of Clinical and Cytokine ProfilesYono FabiandiОценок пока нет
- Etiology of Acute Otitis Media in Children Less Than 5 Years of AgeДокумент9 страницEtiology of Acute Otitis Media in Children Less Than 5 Years of AgeadyОценок пока нет
- Neonatal Infections PerspectiveДокумент13 страницNeonatal Infections PerspectiveYUDY LORENA GIRALDO ALFONSOОценок пока нет
- The Aetiology and Antibiotic Management of Community-Acquired Pneumonia in Adults in Europe: A Literature ReviewДокумент15 страницThe Aetiology and Antibiotic Management of Community-Acquired Pneumonia in Adults in Europe: A Literature ReviewPutu Sukma RadhanaОценок пока нет
- Probiotics and Carriage of Streptococcus PneumoniaeДокумент9 страницProbiotics and Carriage of Streptococcus Pneumoniaeanita awОценок пока нет
- Charlier Et Al. Lancet Infectious Diseases 2017Документ47 страницCharlier Et Al. Lancet Infectious Diseases 2017werwrОценок пока нет
- Herpes Simplex Congenital Infections, Part I: Cytomegalovirus, Toxoplasma, Rubella, andДокумент13 страницHerpes Simplex Congenital Infections, Part I: Cytomegalovirus, Toxoplasma, Rubella, andSyahrialОценок пока нет
- Hematological Scoring for Early Neonatal Sepsis DiagnosisДокумент5 страницHematological Scoring for Early Neonatal Sepsis DiagnosisNabila NatasyaОценок пока нет
- THT - 12 Acute Otitis Media and Other Complication of Viral Respiratory InfectionДокумент12 страницTHT - 12 Acute Otitis Media and Other Complication of Viral Respiratory InfectionWelly SuryaОценок пока нет
- Hematologic Scoring for Early Neonatal Sepsis DiagnosisДокумент5 страницHematologic Scoring for Early Neonatal Sepsis DiagnosisrantiadrianiОценок пока нет
- Researcharticle Open Access: Alexandra Hagen, Anna Eichinger, Melanie Meyer-Buehn, Tilmann Schober and Johannes HuebnerДокумент10 страницResearcharticle Open Access: Alexandra Hagen, Anna Eichinger, Melanie Meyer-Buehn, Tilmann Schober and Johannes HuebneramaliaОценок пока нет
- Neonatal Sepsis in The Very Low Birth Weight Preterm Infants: Part 1: Review of Patho-PhysiologyДокумент10 страницNeonatal Sepsis in The Very Low Birth Weight Preterm Infants: Part 1: Review of Patho-PhysiologyjukunkОценок пока нет
- MAKALAH Keputusasan-1Документ7 страницMAKALAH Keputusasan-1ARINAОценок пока нет
- Vertical Transmission of Dengue Virus in The Peripartum Period and Viral Kinetics in Newborns and Breast Milk: New DataДокумент8 страницVertical Transmission of Dengue Virus in The Peripartum Period and Viral Kinetics in Newborns and Breast Milk: New DataMarcelo QuipildorОценок пока нет
- Ebn RespiДокумент17 страницEbn RespilablabkurmОценок пока нет
- Clinical Characteristic and Pathogen Spectrum of Neonatal Sepsis in Guangzhou City From June 2011 To June 2017Документ9 страницClinical Characteristic and Pathogen Spectrum of Neonatal Sepsis in Guangzhou City From June 2011 To June 2017PSIK sarimuliaОценок пока нет
- Jurnal 2Документ12 страницJurnal 2zingioОценок пока нет
- Ang LW Et Al. Epidemiology and Control of Hand, Foot and Mouth Disease in Singapore, 2001-2007. Ann Acad Med Singapore 2009 38 106-12Документ7 страницAng LW Et Al. Epidemiology and Control of Hand, Foot and Mouth Disease in Singapore, 2001-2007. Ann Acad Med Singapore 2009 38 106-12chaer assofiОценок пока нет
- Risk Factors For and Outcomes of Multidrug-Resistant Escherichia Coli Infections in ChildrenДокумент17 страницRisk Factors For and Outcomes of Multidrug-Resistant Escherichia Coli Infections in ChildrenLihaniUltifaОценок пока нет
- Risk Factors for Suppurative Complications in Children with PneumoniaДокумент6 страницRisk Factors for Suppurative Complications in Children with PneumoniaWilson LeccaОценок пока нет
- Pattern of Infectious Morbidity in Hiv-Exposed Uninfected Infants and ChildrenДокумент8 страницPattern of Infectious Morbidity in Hiv-Exposed Uninfected Infants and Childrenmiss betawiОценок пока нет
- Etiologic and Epidemiologic Analysis of Hand FootДокумент9 страницEtiologic and Epidemiologic Analysis of Hand FootAisah AisahОценок пока нет
- Bronchiolitis High Risk ApneaДокумент7 страницBronchiolitis High Risk ApneaclikgoОценок пока нет
- ARTICULO Estudio de CasoДокумент14 страницARTICULO Estudio de Casowhmticona2002Оценок пока нет
- Neonatal Mastitis: Controversies in Management: October 2012Документ5 страницNeonatal Mastitis: Controversies in Management: October 2012ditaОценок пока нет
- Diarrea en QuimioterapiaДокумент6 страницDiarrea en QuimioterapiaPaola DiazОценок пока нет
- Group 1 InfographicsДокумент2 страницыGroup 1 Infographicscabahugjabez192Оценок пока нет
- Neonatal GAS Meningitis Case Report and Literature ReviewДокумент6 страницNeonatal GAS Meningitis Case Report and Literature ReviewJessyMomoОценок пока нет
- Review Article: Choice and Duration of Antimicrobial Therapy For Neonatal Sepsis and MeningitisДокумент10 страницReview Article: Choice and Duration of Antimicrobial Therapy For Neonatal Sepsis and MeningitisjessicacookОценок пока нет
- fcimb-11-694093Документ12 страницfcimb-11-694093Marketable StudioОценок пока нет
- TB in ChildrenДокумент9 страницTB in Childrenparamita nindyaОценок пока нет
- Neonatal Pneumonia Incidence and Outcomes in BangladeshДокумент6 страницNeonatal Pneumonia Incidence and Outcomes in BangladeshAnonymous Us5v7C6QhОценок пока нет
- 1 s2.0 S1896112615000498 MainДокумент6 страниц1 s2.0 S1896112615000498 MainNELSON VIDIGALОценок пока нет
- Etiology of Neonatal Sepsis in Five Urban Hospitals in The PhilippinesДокумент11 страницEtiology of Neonatal Sepsis in Five Urban Hospitals in The PhilippinesAlexandra Duque-DavidОценок пока нет
- Articulo MicroДокумент8 страницArticulo Microliliana ospinaОценок пока нет
- Infecciones Neonatale IДокумент13 страницInfecciones Neonatale IFidel RamonОценок пока нет
- Acute Histologic Chorioamnionitis at Term: Nearly Always NoninfectiousДокумент7 страницAcute Histologic Chorioamnionitis at Term: Nearly Always NoninfectiousSri AgustinaОценок пока нет
- Achten 2018Документ6 страницAchten 2018bram AyuОценок пока нет
- BMJ c4978 FullДокумент6 страницBMJ c4978 Fulljesusm_115Оценок пока нет
- HTTP Journals - Plos.org Plosmedicine Article Asset Id 10.1371 Journal - Pmed.1001444 PDFДокумент12 страницHTTP Journals - Plos.org Plosmedicine Article Asset Id 10.1371 Journal - Pmed.1001444 PDFferОценок пока нет
- Diag BronchiolitisДокумент2 страницыDiag BronchiolitisoussamamusОценок пока нет
- Variations in Mortality in Children Admitted With Pneumonia To Kenyan HospitalsДокумент7 страницVariations in Mortality in Children Admitted With Pneumonia To Kenyan HospitalsAyunda HardiyantiОценок пока нет
- Effects of One-Dose Varicella Vaccination On Disease Severity in Children During Outbreaks in Seoul, KoreaДокумент5 страницEffects of One-Dose Varicella Vaccination On Disease Severity in Children During Outbreaks in Seoul, KoreaNur WahyuningsihОценок пока нет
- Community-Acquired Pneumonia in Children: Myths and FactsДокумент4 страницыCommunity-Acquired Pneumonia in Children: Myths and FactsFranciscoDelgadoОценок пока нет
- Influenza vaccination: What does the scientific proof say?: Could it be more harmful than useful to vaccinate indiscriminately elderly people, pregnant women, children and health workers?От EverandInfluenza vaccination: What does the scientific proof say?: Could it be more harmful than useful to vaccinate indiscriminately elderly people, pregnant women, children and health workers?Оценок пока нет
- Jurnal Gastroenterology, Hepatology, and Nutrition PediatricДокумент71 страницаJurnal Gastroenterology, Hepatology, and Nutrition PediatricJonathan WelchОценок пока нет
- TB SimulationДокумент15 страницTB SimulationJonathan WelchОценок пока нет
- Pediatric Gastroenterology Algorithme PDFДокумент118 страницPediatric Gastroenterology Algorithme PDFJonathan Welch100% (1)
- J. Clin. Microbiol.-2000-Haque-3235-9Документ5 страницJ. Clin. Microbiol.-2000-Haque-3235-9Jonathan WelchОценок пока нет
- Amebic Liver Abscess in ChildrenДокумент5 страницAmebic Liver Abscess in ChildrenJonathan WelchОценок пока нет
- Pediatric Neurology PDFДокумент301 страницаPediatric Neurology PDFJonathan WelchОценок пока нет
- Jact03i2p107 PDFДокумент5 страницJact03i2p107 PDFJonathan WelchОценок пока нет
- Gastrointestinal Bleeding in Infants and ChildrenДокумент16 страницGastrointestinal Bleeding in Infants and ChildrenaandakuОценок пока нет
- Apert SyndromeДокумент2 страницыApert SyndromeJonathan WelchОценок пока нет
- Combination Measles Mumps Rubella Varicella.9Документ12 страницCombination Measles Mumps Rubella Varicella.9Jonathan WelchОценок пока нет
- Jurnal LeukapharesisДокумент6 страницJurnal LeukapharesisJonathan WelchОценок пока нет
- Jurnal Nefro Madya - Achmad YudhaДокумент15 страницJurnal Nefro Madya - Achmad YudhaJonathan WelchОценок пока нет
- International Journal of Pathology and Clinical Research Ijpcr 2 023Документ9 страницInternational Journal of Pathology and Clinical Research Ijpcr 2 023Jonathan WelchОценок пока нет
- Practical Algorithms in Pediatric NephrologyДокумент126 страницPractical Algorithms in Pediatric NephrologyJonathan Welch100% (2)
- Causedoutbreak Klebsiella PDFДокумент11 страницCausedoutbreak Klebsiella PDFJonathan WelchОценок пока нет
- Glasgow Meningococcal Septicaemia Prognostic Score (GMPS) : Arrival 1 Hour 1 Systolic Blood PressureДокумент1 страницаGlasgow Meningococcal Septicaemia Prognostic Score (GMPS) : Arrival 1 Hour 1 Systolic Blood PressureJonathan WelchОценок пока нет
- Measles DifferentialDiagnosisTable PDFДокумент1 страницаMeasles DifferentialDiagnosisTable PDFJonathan WelchОценок пока нет
- Apneu, CafeinДокумент8 страницApneu, CafeinJonathan WelchОценок пока нет
- Antibiotik Pada Anak: Achmad Yudha ApДокумент23 страницыAntibiotik Pada Anak: Achmad Yudha ApJonathan WelchОценок пока нет
- ESBL UptodateДокумент12 страницESBL UptodateJonathan WelchОценок пока нет
- JB Drugs ToolbookДокумент272 страницыJB Drugs ToolbookOrion JohnОценок пока нет
- Gejala Klinis Apa Sajakah Yang Bisa Digunakan UntukДокумент2 страницыGejala Klinis Apa Sajakah Yang Bisa Digunakan UntukKenОценок пока нет
- ESBL UptodateДокумент12 страницESBL UptodateJonathan WelchОценок пока нет
- Efek Meropenem Pada NeoДокумент5 страницEfek Meropenem Pada NeoJonathan WelchОценок пока нет
- ESBLДокумент7 страницESBLJonathan WelchОценок пока нет
- Multivitamin, TBC, Tanzanian Children PDFДокумент9 страницMultivitamin, TBC, Tanzanian Children PDFJonathan WelchОценок пока нет
- New Approach for Evaluating LV Diastolic Function Using Color M-Mode DopplerДокумент7 страницNew Approach for Evaluating LV Diastolic Function Using Color M-Mode DopplerJonathan WelchОценок пока нет
- Roti, Gizi Arrabinoxylan OligosakaridaДокумент11 страницRoti, Gizi Arrabinoxylan OligosakaridaJonathan WelchОценок пока нет
- @2000 The Most Important Changes Guidelines 2000Документ7 страниц@2000 The Most Important Changes Guidelines 2000nurmauliarizkyОценок пока нет
- Neelakantan V Thesis PDFДокумент299 страницNeelakantan V Thesis PDFNur HafidzОценок пока нет
- Worksheet 1.1 Department of Health Area Program-Based Health PlanningДокумент7 страницWorksheet 1.1 Department of Health Area Program-Based Health PlanningNik Rose ElОценок пока нет
- Bloodborne Pathogens TrainingДокумент102 страницыBloodborne Pathogens Trainingapi-311432115Оценок пока нет
- ZODДокумент1 страницаZODJeric Miguel Raquel TabionОценок пока нет
- ANTIBIOTIC POLICY FOR Sassoon Hospital & BJGMC, PuneДокумент32 страницыANTIBIOTIC POLICY FOR Sassoon Hospital & BJGMC, Puneshah007zaadОценок пока нет
- Cosh ReviewerДокумент3 страницыCosh ReviewerDRACONIAN DEVIL100% (11)
- EENC (Early Essential Newborn Care)Документ74 страницыEENC (Early Essential Newborn Care)Jennifer AlamonОценок пока нет
- Bpops Plan 2023Документ6 страницBpops Plan 2023Nenita TravillaОценок пока нет
- Maternal Mortality in Papua New Guinea and Australia: Max Brinsmead MB Bs PHD December 2017Документ24 страницыMaternal Mortality in Papua New Guinea and Australia: Max Brinsmead MB Bs PHD December 2017DrChauhanОценок пока нет
- 03 4.3.1 IRAR PROCEDURE RevДокумент10 страниц03 4.3.1 IRAR PROCEDURE RevYousaf RichuОценок пока нет
- Declaration of Anthony MillerДокумент4 страницыDeclaration of Anthony MillerLawrence Lessig100% (1)
- Per Axelsson - Epidemia de Polio en Suecia 1880-1940Документ15 страницPer Axelsson - Epidemia de Polio en Suecia 1880-1940KarlosTrusikОценок пока нет
- 2020 11 07 XII Economics 1Документ17 страниц2020 11 07 XII Economics 1Sjft6hd FfОценок пока нет
- Obesity Is The Most Nutritional Among Children Developed CountriesДокумент14 страницObesity Is The Most Nutritional Among Children Developed CountriesBulanBiruОценок пока нет
- Ectopic Pregnancy Management - 280720Документ10 страницEctopic Pregnancy Management - 280720SUPRIYA SINGHОценок пока нет
- POGI Preclampsia 2022Документ52 страницыPOGI Preclampsia 2022SDM RSTIОценок пока нет
- Thesis On Wellness ProgramДокумент28 страницThesis On Wellness ProgramGemma GuemoОценок пока нет
- Community Health NursingДокумент1 страницаCommunity Health NursingNeenu RajputОценок пока нет
- SMA Bahasa Inggris 11 Summative AssessmentДокумент9 страницSMA Bahasa Inggris 11 Summative Assessmentalberthoal588Оценок пока нет
- Kirke Tiziana Terenzi Extrait de Parfum 100ML - Gümrüksüz ParfümДокумент1 страницаKirke Tiziana Terenzi Extrait de Parfum 100ML - Gümrüksüz ParfümSema RutbilОценок пока нет
- Family Nursing Care Plan: Bicol University Tabaco Campus Nursing DepartmentДокумент5 страницFamily Nursing Care Plan: Bicol University Tabaco Campus Nursing DepartmentCelline Isabelle ReyesОценок пока нет
- Obstetrics and Gynecology HighlightsДокумент18 страницObstetrics and Gynecology Highlightsvk100% (1)
- TCL BHS 14Документ38 страницTCL BHS 14maroseg21Оценок пока нет
- Urban Health and Health Seeking Behaviour - A Case Study of Slums in India and PhilippinesДокумент193 страницыUrban Health and Health Seeking Behaviour - A Case Study of Slums in India and Philippineskarl_poorОценок пока нет
- TB LAM Training MaterialsДокумент24 страницыTB LAM Training MaterialsBenedict OkotОценок пока нет
- CHN Week 1 Day 2 and 3 Activity Initial Data BaseДокумент6 страницCHN Week 1 Day 2 and 3 Activity Initial Data BaseGailОценок пока нет
- CHN Exercise 1 - Paola Mariz P. CeroДокумент3 страницыCHN Exercise 1 - Paola Mariz P. CeroPaola Mariz P. CeroОценок пока нет
- Pengaruh Beban Kerja Dokter Gigi Terhadap Tingkat Kepuasan Kerja Dan Kinerja Saat Pandemi Covid Di Klinik Kimia Farm Kota MakassarДокумент12 страницPengaruh Beban Kerja Dokter Gigi Terhadap Tingkat Kepuasan Kerja Dan Kinerja Saat Pandemi Covid Di Klinik Kimia Farm Kota MakassarBu YantiОценок пока нет