Академический Документы
Профессиональный Документы
Культура Документы
Preeclampsia - Practice Essentials, Overview, Pathophysiology
Загружено:
Manuel LimaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Preeclampsia - Practice Essentials, Overview, Pathophysiology
Загружено:
Manuel LimaАвторское право:
Доступные форматы
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
Preeclampsia
Author:KeeHakLim,MDChiefEditor:RonaldMRamus,MDmore...
Updated:Feb03,2016
PracticeEssentials
Preeclampsiaisadisorderofwidespreadvascularendothelialmalfunctionand
vasospasmthatoccursafter20weeks'gestationandcanpresentaslateas46
weekspostpartum.Itisclinicallydefinedbyhypertensionandproteinuria,withor
withoutpathologicedema.
Definitions
Preeclampsiaisdefinedasthepresenceof(1)asystolicbloodpressure(SBP)
greaterthanorequalto140mmHgoradiastolicbloodpressure(DBP)greater
thanorequalto90mmHgorhigher,ontwooccasionsatleast4hoursapartina
previouslynormotensivepatient,OR(2)anSBPgreaterthanorequalto160mm
HgoraDBPgreaterthanorequalto110mmHgorhigher(Inthiscase,
hypertensioncanbeconfirmedwithinminutestofacilitatetimelyantihypertensive
therapy.). [1]
Inadditiontothebloodpressurecriteria,proteinuriaofgreaterthanorequalto0.3
gramsina24hoururinespecimen,aprotein(mg/dL)/creatinine(mg/dL)ratioof0.3
orhigher,oraurinedipstickproteinof1+(ifaquantitativemeasurementis
unavailable)isrequiredtodiagnosepreeclampsia. [1]
Preeclampsiawithseverefeaturesisdefinedasthepresenceofoneofthe
followingsymptomsorsignsinthepresenceofpreeclampsia[1]:
SBPof160mmHgorhigherorDBPof110mmHgorhigher,ontwo
occasionsatleast4hoursapartwhilethepatientisonbedrest(unless
antihypertensivetherapyhaspreviouslybeeninitiated)
Impairedhepaticfunctionasindicatedbyabnormallyelevatedblood
concentrationsofliverenzymes(todoublethenormalconcentration),severe
persistentupperquadrantorepigastricpainthatdoesnotrespondto
pharmacotherapyandisnotaccountedforbyalternativediagnoses,orboth.
Progressiverenalinsufficiency(serumcreatinineconcentration>1.1mg/dLor
adoublingoftheserumcreatinineconcentrationintheabsenceofother
renaldisease)
Newonsetcerebralorvisualdisturances
Pulmonaryedema
Thrombocytopenia(plateletcount<100,000/L)
Inapatientwithnewonsethypertensionwithoutproteinuria,thenewonsetofany
ofthefollowingisdiagnosticofpreeclampsia:
Plateletcountbelow100,000/L
Serumcreatininelevelabove1.1mg/dLordoublingofserumcreatininein
theabsenceofotherrenaldisease
Livertransaminaselevelsatleasttwicethenormalconcentrations
Pulmonaryedema
Cerebralorvisualsymptoms
Eclampsiaisdefinedasseizuresthatcannotbeattributabletoothercausesina
womanwithpreeclampsia.HELLPsyndrome(hemolysis,elevatedliverenzyme,low
platelets)maycomplicateseverepreeclampsia.
Riskfactors
Riskfactorsforpreeclampsiaandtheiroddsratiosareasfollows[2]:
Nulliparity(3.1)
Ageolderthan40years(3:1)
Blackrace(1.5:1)
Familyhistory(5:1)
Chronicrenaldisease(20:1)
Chronichypertension(10:1)
Antiphospholipidsyndrome(10:1)
Diabetesmellitus(2:1)
Twingestation(butunaffectedbyzygosity)(4:1)
Highbodymassindex(3:1)
HomozygosityforangiotensinogengeneT235(20:1)
HeterozygosityforangiotensinogengeneT235(4:1)
Signsandsymptoms
http://emedicine.medscape.com/article/1476919overview
1/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
Becausetheclinicalmanifestationsofpreeclampsiacanbeheterogeneous,
diagnosingpreeclampsiamaynotbestraightforward.Preeclampsiawithoutsevere
featuresmaybeasymptomatic.Manycasesaredetectedthroughroutineprenatal
screening.
Patientswithpreeclampsiawithseverefeaturesdisplayendorganeffectsandmay
complainofthefollowing:
Headache
Visualdisturbances:Blurred,scintillatingscotomata
Alteredmentalstatus
Blindness:Maybecortical [3]orretinal
Dyspnea
Edema:Suddenincreaseinedemaorfacialedema
Epigastricorrightupperquadrantabdominalpain
Weaknessormalaise:Maybeevidenceofhemolyticanemia
Clonus:Mayindicateanincreasedriskofconvulsions
Diagnosis
Allwomenwhopresentwithnewonsethypertensionshouldhavethefollowing
tests:
CBC
Serumalanineaminotransferase(ALT)andaspartateaminotransferase
(AST)levels
Serumcreatinine
Uricacid
24hoururinecollectionforproteinandcreatinine(criterionstandard)orurine
dipstickanalysis
AdditionalstudiestoperformifHELLPsyndromeissuspectedareasfollows:
Peripheralbloodsmear
Serumlactatedehydrogenase(LDH)level
Indirectbilirubin
Althoughacoagulationprofile(prothrombintime[PT],activatedpartial
thromboplastintime[aPTT],andfibrinogen)shouldalsobeevaluated,itsclinical
valueisunclearwhentheplateletcountis100,000/mm3ormorewithnoevidence
ofbleeding. [4]
HeadCTscanningisusedtodetectintracranialhemorrhageinselected
patientswithanyofthefollowing:
Suddensevereheadaches
Focalneurologicdeficits
Seizureswithaprolongedpostictalstate
Atypicalpresentationforeclampsia
Otherprocedures
Ultrasonography:Transabdominal,toassessthestatusofthefetusand
evaluateforgrowthrestrictionumbilicalarteryDopplerultrasonography,to
assessbloodflow
Cardiotocography:Thestandardfetalnonstresstestandthemainstayof
fetalmonitoring
Management
Deliveryistheonlycureforpreeclampsia.Patientswithpreeclampsiawithout
severefeaturesareofteninducedafter37weeks'gestation.Beforethis,thepatient
isusuallyhospitalizedandmonitoredcarefullyforthedevelopmentofworsening
preeclampsiaorcomplicationsofpreeclampsia,andtheimmaturefetusistreated
withexpectantmanagementwithcorticosteroidstoacceleratelungmaturityin
preparationforearlydelivery.
Inpatientswithpreeclampsiawithseverefeatures,inductionofdeliveryshouldbe
consideredafter34weeks'gestation.Inthesecases,theseverityofdiseasemust
beweighedagainsttherisksofinfantprematurity.Intheemergencysetting,control
ofBPandseizuresshouldbepriorities.
Criteriafordelivery
Womenwithpreeclampsiawithseverefeatureswhoaremanagedexpectantlymust
bedeliveredunderthefollowingcircumstances:
Nonreassuringfetaltestingincluding(nonreassuringnonstresstest,
biophysicalprofilescore,and/orpersistentabsentorreverseddiastolicflow
onumbilicalarteryDopplervelocimetry)
Rupturedmembranes
UncontrollableBP(unresponsivetomedicaltherapy)
Oligohydramnios,withamnioticfluidindex(AFI)oflessthan5cm
Severeintrauterinegrowthrestrictioninwhichtheestimatedfetalweightis
lessthan5%
Oliguria(<500mL/24hr)
Serumcreatininelevelofatleast1.5mg/dL
Pulmonaryedema
http://emedicine.medscape.com/article/1476919overview
2/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
Shortnessofbreathorchestpainwithpulseoximetryof<94%onroomair
Headachethatispersistentandsevere
Rightupperquadranttenderness
DevelopmentofHELLPsyndrome
Eclampsia
Plateletcountlesstha100,000cells/microL
Placentalabruption
Unexplainedcoagulopathy
Seizuretreatmentandprophylaxis
Thebasicprinciplesofairway,breathing,andcirculation(ABC)should
alwaysbefollowed
Magnesiumsulfateisthefirstlinetreatmentforprimaryandrecurrent
eclampticseizures
TreatactiveseizureswithIVmagnesiumsulfate [5]:Aloadingdoseof4gis
givenbyinfusionpumpover510minutes,followedbyaninfusionof1g/hr
maintainedfor24hoursafterthelastseizure
Treatrecurrentseizureswithanadditionalbolusof2goranincreaseinthe
infusionrateto1.5or2gperhour
Prophylactictreatmentwithmagnesiumsulfateisindicatedforallpatients
withpreeclampsiawithseverefeatures
Lorazepamandphenytoinmaybeusedassecondlineagentsforrefractory
seizures
Acutetreatmentofseverehypertensioninpregnancy
Antihypertensivetreatmentisrecommendedforseverehypertension(SBP>160
mmHgDBP>110mmHg).ThegoalofhypertensiontreatmentistomaintainBP
around140/90mmHg.
MedicationsusedforBPcontrolincludethefollowing:
Hydralazine
Labetalol
Nifedipine
Sodiumnitroprusside(inseverehypertensiveemergencyrefractorytoother
medications)
Fluidmanagement
Diureticsshouldbeavoided
Aggressivevolumeresuscitationmayleadtopulmonaryedema
Patientsshouldbefluidrestrictedwhenpossible,atleastuntiltheperiodof
postpartumdiuresis
Centralvenouspressure(CVP)orpulmonaryarterypressuremonitoringmay
beindicatedincriticalcases
ACVPof5mmHginwomenwithnoheartdiseaseindicatessufficient
intravascularvolume,andmaintenancefluidsalonearesufficient
Totalfluidsshouldgenerallybelimitedto80mL/hror1mL/kg/hr
Postpartummanagement
Manypatientswillhaveabrief(upto6hours)periodofoliguriafollowing
delivery
Magnesiumsulfateseizureprophylaxisiscontinuedfor24hourspostpartum
Liverfunctiontestsandplateletcountsmustdocumentdecreasingvalues
priortohospitaldischarge
ElevatedBPmaybecontrolledwithnifedipineorlabetalolpostpartum
IfapatientisdischargedwithBPmedication,reassessmentandaBPcheck
shouldbeperformed,atthelatest,1weekafterdischarge
Unlessawomanhasundiagnosedchronichypertension,inmostcasesof
preeclampsia,theBPreturnstobaselineby12weekspostpartum
Patientsshouldbecarefullymonitoredforrecurrentpreeclampsia,whichmay
developupto4weekspostpartum,andforeclampsiathathasoccurredup
to6weeksafterdelivery
Overview
Preeclampsiaisadisorderofwidespreadvascularendothelialmalfunctionand
vasospasmthatoccursafter20weeks'gestationandcanpresentaslateas46
weekspostpartum.Itisclinicallydefinedbyhypertensionandproteinuria,withor
withoutpathologicedema. [6]
TheincidenceofpreeclampsiaintheUnitedStatesisestimatedtorangefrom2%
to6%inhealthy,nulliparouswomen. [7,8,9]Amongallcasesofthepreeclampsia,
10%occurinpregnanciesoflessthan34weeks'gestation.Theglobalincidenceof
preeclampsiahasbeenestimatedat514%ofallpregnancies.
Indevelopingnations,theincidenceofthediseaseisreportedtobe418%, [10,11]
withhypertensivedisordersbeingthesecondmostcommonobstetriccauseof
stillbirthsandearlyneonataldeathsinthesecountries. [12]
Medicalconsensusislackingregardingthevaluesthatdefinepreeclampsia,but
reasonablecriteriainawomanwhowasnormotensivebefore20weeks'gestation
includeasystolicbloodpressure(SBP)greaterthan140mmHgandadiastolicBP
(DBP)greaterthan90mmHgontwosuccessivemeasurements,4hoursapart.
http://emedicine.medscape.com/article/1476919overview
3/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
Preeclampsiaandpreeclampsiawithseverefeatures
Severepreeclampsiaaccountsforapproximately25%ofallcasesofpreeclampsia.
[5]Initsextreme,thediseasemayleadtoliverandrenalfailure,disseminated
intravascularcoagulopathy(DIC),andcentralnervoussystem(CNS)abnormalities.
Ifpreeclampsiaassociatedseizuresdevelop,thedisorderhasdevelopedintothe
conditioncalledeclampsia.
Preeclampsiaisdefinedasthepresenceof(1)asystolicbloodpressure(SBP)
greaterthanorequalto140mmHgoradiastolicbloodpressure(DBP)greater
thanorequalto90mmHgorhigher,ontwooccasionsatleast4hoursapartina
previouslynormotensivepatient,OR(2)anSBPgreaterthanorequalto160mm
HgoraDBPgreaterthanorequalto110mmHgorhigher(Inthiscase,
hypertensioncanbeconfirmedwithinminutestofacilitatetimelyantihypertensive
therapy.). [1]
Inadditiontothebloodpressurecriteria,proteinuriaofgreaterthanorequalto0.3
gramsina24hoururinespecimen,aprotein(mg/dL)/creatinine(mg/dL)ratioof0.3
orhigher,oraurinedipstickproteinof1+(ifaquantitativemeasurementis
unavailable)isrequiredtodiagnosepreeclampsia. [1]
Preeclampsiawithseverefeaturesisdefinedasthepresenceofoneofthe
followingsymptomsorsignsinthepresenceofpreeclampsia[1]:
SBPof160mmHgorhigherorDBPof110mmHgorhigher,ontwo
occasionsatleast4hoursapartwhilethepatientisonbedrest(unless
antihypertensivetherapyhaspreviouslybeeninitiated)
Impairedhepaticfunctionasindicatedbyabnormallyelevatedblood
concentrationsofliverenzymes(todoublethenormalconcentration),severe
persistentupperquadrantorepigastricpainthatdoesnotrespondto
pharmacotherapyandisnotaccountedforbyalternativediagnoses,orboth.
Progressiverenalinsufficiency(serumcreatinineconcentration>1.1mg/dLor
adoublingoftheserumcreatinineconcentrationintheabsenceofother
renaldisease)
Newonsetcerebralorvisualdisturances
Pulmonaryedema
Thrombocytopenia(plateletcount<100,000/L)
Also,apatientwithnewonsethypertensionwithoutproteinuriacanbediagnosedif
anyofthefollowingispresent [1]:
Plateletcountbelow100,000/L
Serumcreatininelevelabove1.1mg/dLordoublingofserumcreatininein
theabsenceofotherrenaldisease
Livertransaminaselevelsatleasttwicethenormalconcentrations
Pulmonaryedema
Cerebralorvisualsymptoms
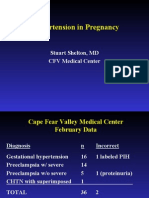
Classificationandcharacteristicsofhypertensivedisorders
Preeclampsiaispartofaspectrumofhypertensivedisordersthatcomplicate
pregnancy.AsspecifiedbytheNationalHighBloodPressureEducationProgram
(NHBPEP)WorkingGroup,theclassificationisasfollows[13]:
Gestationalhypertension
Chronichypertension
Preeclampsia/eclampsia
Superimposedpreeclampsia(onchronichypertension)
Althougheachofthesedisorderscanappearinisolation,theyarethoughtofas
progressivemanifestationsofasingleprocessandarebelievedtoshareacommon
etiology.
Gestationalhypertension
Thecharacteristicsofgestationalhypertensionareasfollows:
BPof140/90mmHgorgreaterforthefirsttimeduringpregnancy
Noproteinuria
BPreturnstonormallessthan12weeks'postpartum
Finaldiagnosismadeonlypostpartum
Chronichypertension
Chronichypertensionischaracterizedbyeither(1)aBP140/90mmHgorgreater
beforepregnancyordiagnosedbefore20weeks'gestationnotattributableto
gestationaltrophoblasticdiseaseor(2)hypertensionfirstdiagnosedafter20weeks'
gestationandpersistentafter12weekspostpartum.
Preexistingchronichypertensionmaypresentwithsuperimposedpreeclampsia
presentingasnewonsetproteinuriaafter20weeks'gestation.
Preeclampsia/eclampsia
Preeclampsia/eclampsiaischaracterizedbyaBPof140/90mmHgorgreaterafter
20weeks'gestationinawomenwithpreviouslynormalBPandwhohave
http://emedicine.medscape.com/article/1476919overview
4/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
proteinuria(0.3gproteinin24hurinespecimen).
Eclampsiaisdefinedasseizuresthatcannotbeattributabletoothercauses,ina
womanwithpreeclampsia
Superimposedpreeclampsia
Superimposedpreeclampsia(onchronichypertension)ischaracterizedby(1)new
onsetproteinuria(300mg/24h)inawomanwithhypertensionbutnoproteinuria
before20weeks'gestationand(2)asuddenincreaseinproteinuriaorBP,ora
plateletcountoflessthan100,000/mm3,inawomanwithhypertensionand
proteinuriabefore20weeks'gestation.
HELLPsyndrome
HELLPsyndrome(hemolysis,elevatedliverenzyme,lowplatelets)maybean
outcomeofseverepreeclampsia,althoughsomeauthorsbelieveittohavean
unrelatedetiology.Thesyndromehasbeenassociatedwithparticularlyhigh
maternalandperinatalmorbidityandmortalityratesandmaybepresentwithout
hypertensionor,insomecases,withoutproteinuria.
Proteinuria
Proteinuriaisdefinedasthepresenceofatleast300mgofproteinina24hour
urinecollection,aprotein(mg/dL)/creatinine(mg/dL)ratiogreaterthanorequalto
0.3,oraurinedipstickproteinof1+(ifaquantitativemeasurementisunavailable).
[14]Serialconfirmations6hoursapartincreasethepredictivevalue.Althoughmore
convenient,aurinedipstickvalueof1+ormore(30mg/dL)isnotreliableinthe
diagnosisofproteinuria.
Pathophysiology
Anestimated28%ofpregnanciesarecomplicatedbypreeclampsia,with
associatedmaternofetalmorbidityandmortality. [15]Inthefetus,preeclampsiacan
leadtoischemicencephalopathy,growthretardation,andthevarioussequelaeof
prematurebirth.
Eclampsiaisestimatedtooccurin1in200casesofpreeclampsiawhen
magnesiumprophylaxisinnotadministered.(SeeSeizureProphylaxis.)[16,17]
Cardiovasculardisease
Aspreviouslymentioned,preeclampsiaischaracterizedbyendothelialdysfunction
inpregnantwomen.Therefore,thepossibilityexiststhatpreeclampsiamaybea
contributortofuturecardiovasculardisease.Inametaanalysis,severalassociations
wereobservedbetweenanincreasedriskofcardiovasculardiseaseandapregnancy
complicatedbypreeclampsia.Theseassociationsincludedanapproximately4fold
increaseintheriskofsubsequentdevelopmentofhypertensionandan
approximately2foldincreaseintheriskofischemicheartdisease,venous
thromboembolism,andstroke. [18]Moreover,womenwhohadrecurrent
preeclampsiaweremorelikelytosufferfromhypertensionlaterinlife. [18]
Inareviewofpopulationbasedstudies,HarskampandZeemannoteda
relationshipbetweenpreeclampsiaandanincreasedriskoflaterchronic
hypertensionandcardiovascularmorbidity/mortality,comparedwithnormotensive
pregnancy.Moreover,womenwhodeveloppreeclampsiabefore36weeks'gestation
orwhohavemultiplehypertensivepregnancieswereathighestrisk. [19]
HarskampandZeemanalsofoundthattheunderlyingmechanismfortheremote
effectsofpreeclampsiaiscomplexandprobablymultifactorial.Theriskfactorsthat
aresharedbycardiovasculardiseaseandpreeclampsiaareasfollows:
Endothelialdysfunction
Obesity
Hypertension
Hyperglycemia
Insulinresistance
Dyslipidemia
Metabolicsyndrome,theinvestigatorsnoted,maybeapossibleunderlying
mechanismcommontocardiovasculardiseaseandpreeclampsia.
Mechanismsbehindpreeclampsia
Althoughhypertensionmaybethemostcommonpresentingsymptomof
preeclampsia,itshouldnotbeviewedastheinitialpathogenicprocess.
Themechanismsbywhichpreeclampsiaoccursisnotcertain,andnumerous
maternal,paternal,andfetalfactorshavebeenimplicatedinitsdevelopment.The
factorscurrentlyconsideredtobethemostimportantincludethefollowing[20]:
Maternalimmunologicintolerance
Abnormalplacentalimplantation
Genetic,nutritional,andenvironmentalfactors
Cardiovascularandinflammatorychanges
http://emedicine.medscape.com/article/1476919overview
5/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
ImmunologicFactorsinPreeclampsia
Immunologicfactorshavelongbeenconsideredtobekeyplayersinpreeclampsia.
Oneimportantcomponentisapoorlyunderstooddysregulationofmaternal
tolerancetopaternallyderivedplacentalandfetalantigens. [21]Thismaternalfetal
immunemaladaptationischaracterizedbydefectivecooperationbetweenuterine
naturalkiller(NK)cellsandfetalhumanleukocyteantigen(HLA)C,andresultsin
histologicchangessimilartothoseseeninacutegraftrejection.
Theendothelialcelldysfunctionthatischaracteristicofpreeclampsiamaybe
partiallyduetoanextremeactivationofleukocytesinthematernalcirculation,as
evidencedbyanupregulationoftype1helperTcells.
PlacentationinPreeclampsia
Placentalimplantationwithabnormaltrophoblasticinvasionofuterinevesselsisa
majorcauseofhypertensionassociatedwithpreeclampsiasyndrome. [22,23]Infact,
studieshaveshownthatthedegreeofincompletetrophoblasticinvasionofthe
spiralarteriesisdirectlycorrelatedwiththeseverityofsubsequentmaternal
hypertension.Thisisbecausetheplacentalhypoperfusionresultingfromthe
incompleteinvasionleadsbyanunclearpathwaytothereleaseofsystemic
vasoactivecompoundsthatcauseanexaggeratedinflammatoryresponse,
vasoconstriction,endothelialdamage,capillaryleak,hypercoagulability,andplatelet
dysfunction,allofwhichcontributetoorgandysfunctionandthevariousclinical
featuresofthedisease. [6]
Normalplacentationandpseudovascularization
Innormalpregnancies,asubsetofcytotrophoblastscalledinvasivecytotrophoblasts
migratethroughtheimplantationsiteandinvadedeciduatunicamediaofmaternal
spiralarteriesandreplaceitsendotheliuminaprocesscalledpseudovascularization.
[24]Thetrophoblastdifferentiationalongtheinvasivepathwayinvolvesalterationin
theexpressionofanumberofdifferentclassesofmolecules,includingcytokines,
adhesionmolecules,extracellularmatrix,metalloproteinases,andtheclassIbmajor
histocompatibilitycomplex(MHC)molecule,HLAG. [25,26]
Forexample,duringnormaldifferentiation,invadingtrophoblastsaltertheir
adhesionmoleculeexpressionfromthosethatarecharacteristicofepithelialcells
(integrinsalpha6/beta1,alphaV/beta5,andEcadherin)tothoseofendothelial
cells(integrinsalpha1/beta1,alphaV/beta3,andVEcadherin).
Asaresultofthesechanges,thematernalspiralarteriesundergotransformation
fromsmall,musculararteriolestolargecapacitance,lowresistancevessels.This
allowsincreasedbloodflowtothematernalfetalinterface.Remodelingofthese
arteriolesprobablybeginsinthefirsttrimesterandendsby1820weeks'gestation.
However,theexactgestationalageatwhichtheinvasionstopsisunknown.
Failureofpseudovascularizationinpreeclampsia
Theshallowplacentationnotedinpreeclampsiaresultsfromthefactthatthe
invasionofthedecidualarteriolesbycytotrophoblastsisincomplete.Thisisduetoa
failureinthealterationsinmolecularexpressionnecessaryforthedifferentiationof
thecytotrophoblasts,asrequiredforpseudovascularization.Forexample,the
upregulationofmatrixmetalloproteinase9(MMP9)andHLAG,2moleculesnoted
innormallyinvadingcytotrophoblasts,doesnotoccur.
Theinvasivecytotrophoblaststhereforefailtoreplacetunicamedia,whichmeans
thatmostlyintactarterioles,whicharecapableofvasoconstriction,remain.
Histologicevaluationoftheplacentalbeddemonstratesfewcytotrophoblasts
beyondthedeciduallayer.
Theprimarycauseforthefailureoftheseinvasivecytotrophoblaststoundergo
pseudovascularizationandinvadematernalbloodvesselsisnotclear.However,
immunologicandgeneticfactorshavebeenproposed.Earlyhypoxicinsultto
differentiatingcytotrophoblastshasalsobeenproposedasacontributingfactor.
EndothelialDysfunction
Datashowthatanimbalanceofproangiogenicandantiangiogenicfactorsproduced
bytheplacentamayplayamajorroleinmediatingendothelialdysfunction.
Angiogenesisiscriticalforsuccessfulplacentationandthenormalinteraction
betweentrophoblastsandendothelium.(SeeAngiogenicFactorsinPreeclampsia,
below.)
Severalcirculatingmarkersofendothelialcellinjuryhavebeenshowntobe
elevatedinwomenwhodeveloppreeclampsiabeforetheybecamesymptomatic.
Theseincludeendothelin,cellularfibronectin,andplasminogenactivatorinhibitor1,
withanalteredprostacyclin/thromboxaneprofilealsopresent. [3,27]
Evidencealsosuggeststhatoxidativestress,circulatorymaladaptation,
inflammation,andhumoral,mineral,andmetabolicabnormalitiescontributetothe
endothelialdysfunctionandpathogenesisofpreeclampsia.
AngiogenicFactorsinPreeclampsia
http://emedicine.medscape.com/article/1476919overview
6/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
Thecirculatingproangiogenicfactorssecretedbytheplacentaincludevascular
endothelialgrowthfactor(VEGF)andplacentalgrowthfactor(PlGF).The
antiangiogenicfactorsincludesolublefmsliketyrosinekinaseIreceptor(sFlt1)
(otherwiseknownassolubleVEGFreceptortypeI)andsolubleendoglin(sEng).
VEGFandPlGF
VEGFandPlGFpromoteangiogenesisbyinteractingwiththeVEGFreceptor
family.Althoughbothgrowthfactorsareproducedbyplacenta,theserumlevelof
PlGFrisesmuchmoresignificantlyinpregnancy.Inastudy,Tayloretal
demonstratedthattheserumlevelofPlGFdecreasedinwomenwholater
developedpreeclampsia. [28]Thefallinserumlevelwasnotableasearlyasthe
secondtrimesterinwomenwhodevelopedpreeclampsiaandintrauterinegrowth
restriction.
Inanotherinvestigation,MaynardetalobservedthattheserumlevelsofVEGFand
PlGFweredecreasedinwomenwithpreeclampsia. [29]However,themagnitudeof
decreasewaslesspronouncedforVEGF,asitsserumlevelwasnotashighasthat
ofPlGF,eveninnormalpregnancy.Otherinvestigatorshaveconfirmedthisfinding
andhaveshownthattheserumlevelofPlGFdecreasedinwomenbeforethey
developedpreeclampsia. [30,31]
BillsetalsuggestthatcirculatingVEGFAlevelsinpreeclampsiaarebiologically
activebecauseofalossofrepressionofVEGFreceptor1signalingbyPlGF1,and
VEGF165bmaybeinvolvedintheincreasedvascularpermeabilityofpreeclampsia.
[32]
Solublefmsliketyrosinekinase1receptor
ThereceptorsFlt1isasolubleisoformofFlt1,whichisatransmembranereceptor
forVEGF.AlthoughsFlt1lacksthetransmembranedomain,itcontainstheligand
bindingregionandiscapableofbindingcirculatingVEGFandPlGF,preventing
thesegrowthfactorsfrombindingtotransmembranereceptors.Thus,sFlt1hasan
antiangiogeniceffect.
Inadditiontoangiogenesis,VEGFandPlGFareimportantinmaintaining
endothelialhomeostasis.SelectiveknockoutoftheglomerularVEGFgenehas
beenshowntobelethalinrats,whereastheheterozygoteswerebornwith
glomerularendotheliosis(therenallesioncharacteristicofpreeclampsia)and
eventuallyrenalfailure.Furthermore,sFlt1,wheninjectedintopregnantrats,
producedhypertensionandproteinuriaalongwithglomerularendotheliosis. [29]
Inadditiontoanimalstudies,multiplestudiesinhumanshavedemonstratedthat
excessproductionofsFlt1isassociatedwithanincreasedriskofpreeclampsia.In
acasecontrolstudythatmeasuredlevelsofsFlt1,VEGF,andPlGF,investigators
foundanearlierandgreaterincreaseintheserumlevelofsFlt1inwomenwho
developedpreeclampsia(2124wk)thaninwomenwhodidnotdevelop
preeclampsia(3336wk),whereastheserumlevelsofVEGFandPlGFdeceased.
Furthermore,theserumlevelofsFlt1washigherinwomenwhodevelopedsevere
preeclampsiaorearlypreeclampsia(<34wk)thanitwasinwomenwhodeveloped
mildpreeclampsiaatterm. [30]
Solubleendoglin
sEngisasolubleisoformofcoreceptorfortransforminggrowthfactorbeta(TGF
beta).EndoglinbindstoTGFbetainassociationwiththeTGFbetareceptor.
BecausethesolubleisoformcontainstheTGFbetabindingdomain,itcanbindto
circulatingTGFbetaanddecreasecirculatinglevels.Inaddition,TGFbetaisa
proangiogenicmolecule,sotheneteffectofhighlevelsofsEngisantiangiogenic.
SeveralobservationssupporttheroleofsEnginthepathogenesisofpreeclampsia.
Itisfoundinthebloodofwomenwithpreeclampsiaupto3monthsbeforethe
clinicalsignsofthecondition,itslevelinmaternalbloodcorrelateswithdisease
severity,andthelevelofsEngintheblooddropsafterdelivery. [33]
Instudiesonpregnantrats,administrationofsEngresultsinvascularpermeability
andcauseshypertension.Thereisalsoevidencethatithasasynergistic
relationshipwithsFlt1,becauseitincreasestheeffectsofsFlt1inpregnantrats
thisresultsinHELLPsyndrome,asevidencedbyhepaticnecrosis,hemolysis,and
placentalinfarction. [34]Moreover,sEnginhibitsTGFbetainendothelialcellsand
alsoinhibitsTGFbeta1activationofnitricoxidemediatedvasodilatation.
GeneticFactorsinPreeclampsia
Preeclampsiahasbeenshowntoinvolvemultiplegenes.Over100maternaland
paternalgeneshavebeenstudiedfortheirassociationwithpreeclampsia,including
thoseknowntoplayaroleinvasculardiseases,BPregulation,diabetes,and
immunologicfunctions.
Importantly,theriskofpreeclampsiaispositivelycorrelatedbetweencloserelatives
astudyshowedthat2040%ofdaughtersand1137%ofsistersofwomenwith
preeclampsiaalsodevelopedthedisease. [21]Twinstudieshaveshownahigh
correlationaswell,approaching40%.
http://emedicine.medscape.com/article/1476919overview
7/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
Becausepreeclampsiaisageneticallyandphenotypicallycomplexdisease,itis
unlikelythatanysinglegenewillbeshowntoplayadominantroleinits
development.
AdditionalFactorsinPreeclampsia
Othersubstancesthathavebeenproposed,butnotproven,tocontributeto
preeclampsiaincludetumornecrosisfactor,interleukins,variouslipidmolecules,
andsyncytialknots. [35]
RiskFactorsforPreeclampsia
Theincidenceofpreeclampsiaishigherinwomenwithahistoryofpreeclampsia,
multiplegestations,andchronichypertensionorunderlyingrenaldisease.In
addition,Lykkeetalfoundthatpreeclampsia,spontaneouspretermdelivery,orfetal
growthdeviationinafirstsingletonpregnancypredisposeswomentothose
complicationsintheirsecondpregnancy,especiallyifthecomplicationswere
severe. [36]
Gestationalage
Inaregistrybasedcohortstudyof536,419Danishwomen,deliverybetween32and
36weeksgestationincreasedtheriskofpretermdeliveryinthesecondpregnancy
from2.7%to14.7%andincreasedtheriskofpreeclampsiafrom1.1%to1.8%.A
firstdeliverybefore28weeksincreasedtheriskofasecondpretermdeliveryto26%
andincreasedtheriskofpreeclampsiato3.2%.
Preeclampsiainafirstpregnancy,withdeliverybetween32and36weeks'
gestation,increasedtheriskofpreeclampsiainasecondpregnancyfrom14.1%to
25.3%.Fetalgrowth23standarddeviationsbelowthemeaninafirstpregnancy
increasedtheriskofpreeclampsiafrom1.1%to1.8%inthesecondpregnancy. [36]
Primigravidpatientsinparticularseemtobepredisposedtopreeclampsia.
Maternalage
Womenaged35yearsandolderhaveamarkedlyincreasedriskofpreeclampsia.
Race
IntheUnitedStates,theincidenceofpreeclampsiais1.8%amongwhitewomen
and3%inblackwomen.
Additionalriskfactors
Someriskfactorscontributetopoorplacentation,whereasotherscontributeto
increasedplacentalmassandpoorplacentalperfusionsecondarytovascular
abnormalities. [2]
Inadditiontothosediscussedabove,preeclampsiariskfactorsalsoincludethe
following:
Hydatidiformmole
Obesity
Thrombophilia
Oocytedonationordonorinsemination
Urinarytractinfection
Diabetesmellitus:Womenwithpregnancyrelatedhypertensiveconditions,
includingpreeclampsia,pluspreexistingdiabetesorearlygestational
diabetesappeartoremainatincreasedriskforpoorpregnancyoutcomes
evenwhenthegestationaldiabeteswasidentifiedearlyandtreated. [37]
Collagenvasculardisease
Periodontaldisease [38]
OneliteraturereviewsuggeststhatmaternalvitaminDdeficiencymayincreasethe
riskofpreeclampsiaandfetalgrowthrestriction.Anotherstudydeterminedthat
vitaminDdeficiency/insufficiencywascommoninagroupofwomenathighriskfor
preeclampsia.However,itwasnotassociatedwiththesubsequentriskofan
adversepregnancyoutcome. [39]
Studieshavesuggestedthatsmokingduringpregnancyisassociatedwithareduced
riskofgestationalhypertensionandpreeclampsiahowever,thisiscontroversial. [26]
Placentapreviahasalsobeencorrelatedwithareducedriskofpreeclampsia.
Bodyweightisstronglycorrelatedwithprogressivelyincreasedpreeclampsiarisk,
rangingfrom4.3%forwomenwithabodymassindex(BMI)below20kg/m2to
13.3%inthosewithaBMIover35kg/m2.AUnitedKingdomstudyonobesity
showedthat9%ofextremelyobesewomenwerepreeclamptic,comparedwith2%
ofmatchedcontrols. [40]
Ananalysisof456,668singletonbirthsfoundthatearlyonset(<34weeks'gestation)
andlateonset(34weeks'gestation)preeclampsiasharedsomeetiologicfeatures,
buttheirriskfactorsandoutcomesdiffered.Sharedriskfactorsforearlyandlate
onsetpreeclampsiaincludedoldermaternalage,Hispanicrace,NativeAmerican
http://emedicine.medscape.com/article/1476919overview
8/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
race,smoking,unmarriedstatus,andmalefetus.Riskfactorsmorestrongly
associatedwithearlyonsetpreeclampsiathanlateonsetdiseaseincludedblack
race,chronichypertension,andcongenitalanomalies,whileyoungermaternalage,
nulliparity,anddiabetesmellitusweremorestronglyassociatedwithlateonset
preeclampsiathanwithearlyonsetdisease. [41,42]
Earlyonsetpreeclampsiawassignificantlyassociatedwithahighriskforfetaldeath
(adjustedoddsratio[AOR],5.8),butlateonsetpreeclampsiawasnot(AOR,1.3).
However,theAORforperinataldeath/severeneonatalmorbiditywassignificantfor
bothearlyonset(16.4)andlateonset(2.0)preeclampsia. [41,42]
Inaddition,theincidenceofpreeclampsiaincreasedsharplyasgestation
progressed:therateforearlyonsetpreeclampsiawas0.38%comparedwith2.72%
forlateonsetpreeclampsia. [41,42]
Table1liststheriskfactorsandtheiroddsratiosforpreeclampsia. [2]
Table1.RiskFactorsforPreeclampsia*(OpenTableinanewwindow)
Nulliparity
3:1
Age>40y
3:1
Blackrace
1.5:1
Familyhistory
5:1
Chronicrenaldisease
20:1
Chronichypertension
10:1
Antiphospholipidsyndrome
10:1
Diabetesmellitus
2:1
Twingestation(butunaffectedbyzygosity)
4:1
Highbodymassindex
3:1
AngiotensinogengeneT235
Homozygous
20:1
Heterozygous
4:1
*AdaptedfromACOGTechnicalBulletin219,Washington,DC1996. [1]
EvaluationofPreeclampsia
Becausetheclinicalmanifestationsofpreeclampsiacanbeheterogeneous,
diagnosingpreeclampsiamaynotbestraightforward.Inparticular,becausethefinal
diagnosisofgestationalhypertensioncanonlybemadeinretrospect,aclinician
maybeforcedtotreatsomewomenwithgestationalhypertensionasiftheyhave
preeclampsia.Inaddition,ifawomanhasunderlyingrenalorcardiovascular
disease,thediagnosisofpreeclampsiamaynotbecomeclearuntilthedisease
becomessevere.
Mildtomoderatepreeclampsiamaybeasymptomatic.Manycasesaredetected
throughroutineprenatalscreening.
Preeclampsiainapreviouspregnancyisstronglyassociatedwithrecurrencein
subsequentpregnancies.Ahistoryofgestationalhypertensionorpreeclampsia
shouldstronglyraiseclinicalsuspicion.
Physicalfindings
Patientswithpreeclampsiawithseverefeaturesdisplayendorganeffectsandmay
complainofthefollowing:
Headache
Visualdisturbances:Blurred,scintillatingscotomata
Alteredmentalstatus
Blindness:Maybecortical [3]orretinal
Dyspnea
Edema
Epigastricorrightupperquadrantabdominalpain
WeaknessormalaiseMaybeevidenceofhemolyticanemia
Edemaexistsinmanypregnantwomen,butasuddenincreaseinedemaorfacial
edemaissuggestiveofpreeclampsia.Theedemaofpreeclampsiaoccursbya
distinctmechanismthatissimilartothatofangioneuroticedema.
Hepaticinvolvementoccursin10%ofwomenwithseverepreeclampsia.The
resultingpain(epigastricorrightupperquadrantabdominalpain)isfrequently
accompaniedbyelevatedserumhepatictransaminaselevels.
Thepresenceofclonusmayindicateanincreasedriskofconvulsions.
AstudybyCoorayetalfoundthatthemostcommonsymptomsthatimmediately
precedeeclampticseizuresareneurologicsymptoms(ie,headache,withorwithout
visualdisturbance),regardlessofdegreeofhypertension.Thissuggeststhatclosely
monitoringpatientswiththesesymptomsmayprovideanearlywarningfor
eclampsia. [43]
http://emedicine.medscape.com/article/1476919overview
9/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
Recurrenceofpreeclampsia
Uncommonly,patientshaveantepartumpreeclampsiathatistreatedwithdelivery
butthatrecursinthepostpartumperiod. [44]Recurrentpreeclampsiashouldbe
consideredinpostpartumpatientswhopresentwithhypertensionandproteinuria.
(SeePrognosis.)
Inpatientswhoaresufferingarecurrenceofpreeclampsia,findingsonphysical
examinationmayincludethefollowing(seePrognosis):
Alteredmentalstatus
Decreasedvisionorscotomas
Papilledema
Epigastricorrightupperquadrantabdominaltenderness
PeripheraledemaHyperreflexiaorclonus:Althoughdeeptendonreflexesare
moreusefulinassessingmagnesiumtoxicity,thepresenceofclonusmay
indicateanincreasedriskofconvulsions.
Seizures
Focalneurologicdeficit
MeasurementofHypertension
HypertensionisdiagnosedwhentwoBPreadingsof140/90mmHgorgreaterare
noted4hoursapartwithina1weekperiod.MeasuringBPwithanappropriatesized
cuffplacedontherightarmatthesamelevelastheheartisimportant.Thepatient
mustbesittingand,ideally,havehadachancetorestforatleast10minutes
beforetheBPmeasurement.Sheshouldnotbelyingdowninalateraldecubitus
position,asthearmoftenusedtomeasurethepressureinthispositionwillbe
abovetherightatrium.
TheKorotkoffVsoundshouldbeusedforthediastolicpressure.Incasesinwhich
theKorotkoffVsoundisnotpresent,theKorotkoffIVsoundmaybeused,butit
shouldbenotedassuch.ThedifferencebetweentheKorotkoffIVandVsounds
maybeasmuchas10mmHg.Whenanautomatedcuffisused,itmustbeableto
recordtheKorotkoffVsound.Whenserialreadingsareobtainedduringan
observationalperiod,thehighervaluesshouldbeusedtomakethediagnosis.
Lackofhypertensiononexamination
Althoughhypertensionisanimportantcharacteristicofpreeclampsia,becausethe
underlyingpathophysiologyofpreeclampsiaisadiffuseendothelialcelldisorder
influencingmultipleorgans,hypertensiondoesnotnecessarilyneedtoprecede
otherpreeclampticsymptomsorlaboratoryabnormalities.Presentingsymptoms
otherthanhypertensionmayinclude,aspreviouslymentioned,edema,visual
disturbances,headache,andepigastricorrightupperquadranttenderness.
DiagnosticConsiderations
Gestationalhypertension
Duringdiagnosis,preeclampsiamustbedifferentiatedfromgestational
hypertensionalthoughgestationalhypertensionismorecommonandmaypresent
withsymptomssimilartothoseofpreeclampsia,includingepigastricdiscomfortor
thrombocytopenia,itiswhichisnotcharacterizedbyproteinuria.(SeeClassification
andCharacteristicsofHypertensiveDisorders.)
Placentalhypoperfusion
Placentalhypoperfusionorischemiainpreeclampsiahasmanycauses.Preexisting
vasculardisorders,suchashypertensionandconnectivetissuedisorders,canresult
inpoorplacentalcirculation.Incasesofmultiplegestationorincreasedplacental
mass,itisnotsurprisingfortheplacentatobecomeunderperfused.However,most
womenwhodeveloppreeclampsiaarehealthyanddonothaveunderlyingmedical
conditions.Inthisgroupofwomen,abnormallyshallowplacentationhasbeen
showntoberesponsibleforplacentalhypoperfusion.(SeePlacentationin
Preeclampsia.)
Differentialdiagnosis
AbdominalTrauma,Blunt
AbruptioPlacentae
Aneurysm,Abdominal
Appendicitis,Acute
CholecystitisandBiliaryColic
Cholelithiasis
CongestiveHeartFailureandPulmonaryEdema
DomesticViolence
EarlyPregnancyLoss
http://emedicine.medscape.com/article/1476919overview
10/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
Encephalitis
Headache,Tension
HypertensiveEmergencies
Hyperthyroidism,ThyroidStorm,andGravesDisease
MigraineHeadache
OvarianTorsion
Pregnancy,Eclampsia
StatusEpilepticus
Stroke,Hemorrhagic
Stroke,Ischemic
SubarachnoidHemorrhage
SubduralHematoma
ThromboticThrombocytopenicPurpura
Toxicity,Amphetamine
Toxicity,Sympathomimetic
Toxicity,ThyroidHormone
TransientIschemicAttack
UrinaryTractInfection,Female
WithdrawalSyndromes
Cerebrovascularaccidents
Seizuredisorders
Braintumors
Metabolicdiseases
Metastaticgestationaltrophoblasticdisease
Thromboticthrombocytopenicpurpura
RoutineStudies
Allwomenwhopresentwithnewonsethypertensionshouldhavethefollowing
laboratorytests:
Completebloodcell(CBC)count
Serumalanineaminotransferase(ALT)andaspartateaminotransferase
(AST)levels
Serumcreatinine
Uricacid
Inaddition,aperipheralsmearshouldbeperformed,serumlactatedehydrogenase
(LDH)levelsshouldbemeasured,andanindirectbilirubinshouldbecarriedoutif
HELLP(hemolysis,elevatedliverenzyme,lowplatelets)syndromeissuspected.
Althoughacoagulationprofile(prothrombintime[PT],activatedpartial[aPTT],and
fibrinogen)shouldalsobeevaluated,theclinicaluseofroutineevaluationisunclear
whentheplateletcountis100,000/mm3ormorewithnoevidenceofbleeding. [4]
LaboratoryvaluesforpreeclampsiaandHELLPsyndrome [13,45]
Renalvaluesareasfollows:
Proteinurialevelabove300mg/24hours
Urinedipstickover1+
Protein/creatinineratiogreaterthan0.3*
Serumuricacidlevelabove5.6mg/dL*
Serumcreatininelevelover1.1mg/dL
Platelet/coagulopathyrelatedresultsareasfollows:
Plateletcountbelow100,000/mm 3
ElevatedPToraPTT*
Decreasedfibrinogen*
Increasedddimerlevel*
Hemolysisrelatedresultsareasfollows:
Abnormalperipheralsmear*
Indirectbilirubinlevelover1.2mg/dL*
LDHlevelgreaterthan600U/L*
http://emedicine.medscape.com/article/1476919overview
11/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
Inaddition,elevatedliverenzymes(serumAST>70U/L)arefoundinpreeclampsia
andHELLPsyndrome. [24]
Urinetests
Todiagnoseproteinuria,a24hoururinecollectionforproteinandcreatinineshould
beobtainedwheneverpossible.Upto30%ofwomenwithgestationalhypertension
whohavetraceproteinnotedonrandomurinesamplesmayhave300mgofprotein
ina24hoururinecollection. [46]Thus,a24hoururineproteinanalysisremainsthe
criterionstandardforproteinuriadiagnosis.Alternatively,greaterthan1+proteinon
adipstickanalysisonarandomsampleissufficienttomakethediagnosisof
proteinuria.
Randomurinesamplescanbeusedtocalculatetheproteincreatinineratio.
Thresholdsof0.140.3havebeenproposedfordiagnosingproteinuria. [47]However,
thereisnoagreementyetastothebestthresholdforidentifyingpregnantwomen
withsignificantproteinuria.Moreover,upto10%ofpatientswithpreeclampsiaand
20%ofpatientswitheclampsiamaynothaveproteinuria. [48,49](HELLPsyndrome
hasbeenknowntooccurwithouthypertensionorproteinuria.)
Hyperuricemiaisoneoftheearliestlaboratorymanifestationsofpreeclampsia.It
hasalowsensitivity,rangingfrom0%to55%,butarelativelyhighspecificityof77
95%. [50]Seriallevelsmaybeusefultoindicatediseaseprogression.
Bawejaetalsuggestthatwhenmeasuringurinaryalbuminusinghighperformance
liquidchromatographyinanearlyanduncomplicatedpregnancy,spoturinary
albumin:creatinineratio(ACR)valuesarehigher.Ifmeasuredearlyinthesecond
trimester,anACRof35.5mg/mmolorhighermaypredictpreeclampsiabefore
symptomsarise. [51]
Congoreddye
AstudyatYaleUniversityshowedpreliminaryresultssuggestingthatCongored
(CR),adyecurrentlyusedtolocateatypicalamyloidaggregatesinAlzheimer
disease,mayalsobeeffectiveintheearlydiagnosisofpreeclampsia. [50]Itwas
thoughtthatthisfindingmightleadtoaspoturinetestthatcouldbeusedin
emergencydepartmentsandinternationally,especiallyinresourcepoorcountries
wherepreeclampsiacontinuestobeunderdiagnosedandaccountsforalarge
percentageofmaternalandfetalmortality.
Inastudyof40pregnantwomenwithseverepreeclampsiaand40healthypregnant
controls,Buhimschietalfoundthattheurineandplacentasofwomenwith
preeclampsiacontainaggregatesofmisfoldedproteins. [52,53]Theysuggestedthat
urineCRspottingtests(CRbindstomisfoldedproteins)maybebetterthan
currentlyusedcurrentdipstickmethodsatdiagnosingpreeclampsiaandindicating
theneedformedicallyindicateddelivery. [52,53]
Inthisstudy,acutoffvalueofa15%measureofrednessontheCRspottingtest
had100%sensitivityand100%specificityfordistinguishingwomenwithsevere
preeclampsiafromcontrolsubjects. [53]Inaseparatevalidationcohortof563
pregnantwomen,thetesthadasensitivityof85.9%,aspecificityof85.0%,a
positivelikelihoodratioof5.7,andanegativelikelihoodratioof0.17.
Liverenzymes
Althoughcontroversyexistsoverthethresholdforelevatedliverenzyme,thevalues
proposedbySibaietal(ASTof>70U/LandLDHof>600U/L)appeartobethe
mostwidelyaccepted.Alternatively,valuesthatarethreestandarddeviationsaway
fromthemeanforeachlaboratoryvaluemaybeusedforAST. [45]
Histology
Thepresenceofschistocytes,burrcells,orechinocytesonperipheralsmears,or
elevatedindirectbilirubinandlowserumheptoglobinlevels,maybeusedas
evidenceofhemolysisindiagnosingHELLPsyndrome.Thedifferentialdiagnosisfor
HELLPsyndromemustincludevariouscausesforthrombocytopeniaandliverfailure
suchasacutefattyliverofpregnancy,hemolyticuremicsyndrome,acute
pancreatitis,fulminanthepatitis,systemiclupuserythematosus,cholecystitis,and
thromboticthrombocytopenicpurpura.
Additionallaboratorytests
Otherlaboratoryvaluessuggestiveofpreeclampsiaincludeanelevationin
hematocritandariseinserumcreatinineand/oruricacid.Adecreasedlevelof
placentalgrowthfactor(PlGF)inthebloodisalsosuggestiveofpreeclampsia. [54,
55]Althoughtheselaboratoryabnormalitiesincreasethesuspicionforpreeclampsia,
noneoftheselaboratorytestsshouldbeusedtodiagnosepreeclampsia.
Inastudyof540womenwithtype1diabetes,Holmesandcolleaguesfoundthat
thosewomenwhodevelopedpreeclampsiahadabnormalserumlevelsof
angiogenicandantiangiogeniccompoundsinthesecondtrimester.At26weeks
gestation,womenwholaterdevelopedpreeclampsiahadsignificantlylowerlevelsof
theangiogenicfactorPlGF,significantlyhigherlevelsoftheantiangiogenicfactors
solublefmsliketyrosinekinase1(sFlt1)andsolubleendoglin(sEng),aswellas
alterationintheratioofPlGFtosEngortheratioofsFlt1toPlGF. [56,57]
http://emedicine.medscape.com/article/1476919overview
12/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
AtestthatmeasuresthePIGFlevelintheblood(Triage)accuratelyidentified
preeclampsiarequiringdeliveryinaprospectivestudyof625pregnantwomen
presentingbefore35weeks'gestationwithsuspectedpreeclampsia.Ofthe625
subjects,346(55%)developedconfirmedpreeclampsia. [54,55]
Between20and34weeks'gestation,thesensitivityoftheTriagetestinpredicting
theneedfordeliverywithin14dayswas0.96(95%confidenceinterval[CI],0.89
0.99),andthenegativepredictivevaluewas0.98(95%CI0.930.995). [54,55]
Between35and36weeks'gestation,thesensitivitywas0.70(95%CI,0.580.81),
andthenegativepredictivevaluewas0.69(95%CI0.570.80).At37weeks'
gestationormore,thesensitivitywas0.57(95%CI,0.460.68),andthenegative
predictivevaluewas0.70(95%CI,0.620.78). [54,55]
APlGFlevelbelow100pg/mLwasjustasgoodasaPlGFlevelbelowthefifth
centileforgestationalageatpredictingpreeclampsiarequiringdeliverywithin14
days.PIGFlevelslowerthan12pg/mLindicatedanaveragetimetodeliveryofjust
9days.Usedaloneorincombination,thePlGFtestwassignificantly(P<0.001)
betterthanothercommonlyusedtests,includingsystolicanddiastolicblood
pressure,uricacid,alaninetransaminase,andproteinuria,inpredicting
preeclampsiarequiringdeliverywithin14days. [54,55]
Amulticenter,prospectiveobservationalstudyoftheratioofsFlt1toPlGFin
womenwithaclinicalsuspicionofpreeclampsiaorHELLPsyndrome,whowere
between24and37weeks'gestationalage,hasdemonstratedthatansFlt1to
PlGFratioof38orlowertohaveimportantpredictivevalue[58]:AnsFlt1:PlGF
ratioof38orlowerhadanegativepredictivevalueof99.3%(95%confidence
interval[CI],97.9to99.9),suggestinganextremelyunlikelydevelopmentof
preeclampsiaorHELLPwithin1week.However,thepositivepredictivevalueofan
sFlt1:PlGFratioabove38foradiagnosisofpreeclampsiawithin4weekswas
36.7%(95%CI,28.4to45.7).TheauthorsconcludedthatansFlt1:PlGFratioof
38orlowercanbeusedtopredicttheshorttermabsenceofpreeclampsiain
womeninwhomthesyndromeissuspectedclinically. [58]
CTScanningandMRI
Computedtomography(CT)scanningandmagneticresonanceimaging(MRI)scans
haverevealednumerousabnormalitiesinpatientswitheclampsia,suchascerebral
edema,focalinfarction,intracranialhemorrhage,andposterior
leukoencephalopathy. [59]
Currently,however,thereisnopathognomonicCTscanorMRIfindingfor
eclampsia.Furthermore,cerebralimagingisnotnecessaryfortheconditions
diagnosisandmanagement.However,headCTscanningisusedtodetect
intracranialhemorrhageinselectedpatientswithsuddensevereheadaches,focal
neurologicdeficits,seizureswithaprolongedpostictalstate,oratypicalpresentation
foreclampsia.
Ultrasonography
Ultrasonographyisusedtoassessthestatusofthefetusaswellastoevaluatefor
growthrestriction(typicallyasymmetricaluseabdominalcircumference). [60]Aside
fromtransabdominalultrasonography,umbilicalarteryDopplerultrasonography
shouldbeperformedtoassessbloodflow.ThevalueofDopplerultrasonographyin
otherfetalvesselshasnotbeendemonstrated.
Cardiotocography
Cardiotocographyisthestandardfetalnonstresstestandthemainstayoffetal
monitoring.Althoughitgivescontinuinginformationaboutfetalwellbeing,ithas
littlepredictivevalue.
ManagementofPreeclampsia
Theoptimalmanagementofawomanwithpreeclampsiadependsongestational
ageanddiseaseseverity.Becausedeliveryistheonlycureforpreeclampsia,
cliniciansmusttrytominimizematernalriskwhilemaximizingfetalmaturity.The
primaryobjectiveisthesafetyofthemotherandthenthedeliveryofahealthy
newborn.Obstetricconsultationshouldbesoughtearlytocoordinatetransfertoan
obstetricfloor,asappropriate. [61]
Patientswithpreeclampsiawithoutseverefeaturesareofteninducedafter37
weeks'gestation.Beforethis,theimmaturefetusistreatedwithexpectant
managementwithcorticosteroidstoacceleratelungmaturityinpreparationforearly
delivery.
Inpatientswithpreeclampsiawithseverefeatures,inductionofdeliveryshouldbe
consideredafter34weeks'gestation.Inthesecases,theseverityofdiseasemust
beweighedagainsttherisksofinfantprematurity.Intheemergencysetting,control
ofBPandseizuresshouldbepriorities.Ingeneral,thefurtherthepregnancyisfrom
term,thegreatertheimpetustomanagethepatientmedically.
PrehospitalTreatment
http://emedicine.medscape.com/article/1476919overview
13/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
Prehospitalcareforpregnantpatientswithsuspectedpreeclampsiaincludesthe
following:
Oxygenviafacemask
Intravenousaccess
Cardiacmonitoring
Transportationofpatientinleftlateraldecubitusposition
Seizureprecautions
CareinPreeclampsiaWithoutSevereFeatures
Before37weeks,expectantmanagementisappropriate.Inmostcases,patients
shouldbehospitalizedandmonitoredcarefullyforthedevelopmentofworsening
preeclampsiaorcomplicationsofpreeclampsia.Althoughrandomizedtrialsin
womenwithgestationalhypertensionandpreeclampsiademonstratethesafetyof
outpatientmanagementwithfrequentmaternalandfetalevaluations,mostofthe
patientsinthesestudieshadmildgestationalhypertension. [62]Therefore,thesafety
ofmanagingawomanwithpreeclampsiawithoutseverefeaturesasanoutpatient
stillneedstobeinvestigated.
Althoughbedresthasbeenrecommendedinwomenwithpreeclampsia,little
evidencesupportsitsbenefit.Infact,prolongedbedrestduringpregnancyincreases
theriskofthromboembolism.
Apregnancycomplicatedbypreeclampsiawithoutseverefeaturesatorbeyond37
weeksshouldbedelivered.Althoughthepregnancyoutcomeissimilarinthese
womenasitisinwomenwithanormotensivepregnancy,theriskofplacental
abruptionandprogressiontoseverediseaseisslightlyincreased. [63,64]Thus,
regardlessofcervicalstatus,inductionoflaborshouldberecommended.Cesarean
sectionmaybeperformedbasedonstandardobstetriccriteria.
Antepartumtestingisgenerallyindicatedduringexpectantmanagementofpatients
withpreeclampsiawithoutseverefeatures.However,thereislittleconsensus
regardingthetypesofteststobeusedandthefrequencyoftesting.Mostclinicians
offeranonstresstest(NST)andabiophysicalprofile(BPP)atthetimeofthe
diagnosisandusuallytwiceperweekuntildelivery. [2,1]
Ifapatientisat34weeks'gestationormoreandhasrupturedmembranes,
abnormalfetaltesting,orprogressivelaborinthesettingofpreeclampsia,delivery
isrecommended.
CarePreeclampsiaWithSevereFeatures
Whenpreeclampsiawithseverefeaturesisdiagnosedafter34weeksgestation,
deliveryismostappropriate.Themodeofdeliveryshoulddependontheseverityof
thediseaseandthelikelihoodofasuccessfulinduction.Wheneverpossible,
however,vaginaldeliveryshouldbeattemptedandcesareansectionshouldbe
reservedforroutineobstetricindications.
Womenwithpreeclampsiawithseverefeatureswhohavenonreassuringfetal
status,rupturedmembranes,labor,ormaternaldistressshouldbedelivered
regardlessofgestationalage.Ifawomanwithpreeclampsiawithseverefeaturesis
at32weeks'gestationormoreandhasreceivedacourseofsteroids,sheshouldbe
deliveredaswell.
Patientspresentingwithsevere,unremittingheadache,visualdisturbance,andright
upperquadranttendernessinthepresenceofhypertensionand/orproteinuria
shouldbetreatedwithutmostcaution.
Expectantmanagementofpreeclampsiawithseverefeatures
Ifapatientpresentswithpreeclampsiawithseverefeaturesbefore34weeks'
gestationbutappearstobestable,andifthefetalconditionisreassuring,expectant
managementmaybeconsidered,providedthatthepatientmeetsthestrictcriteria
setbySibaietal(seeLaboratoryvaluesforpreeclampsiaandHELLPsyndrome).
[65]Thistypeofmanagementshouldbeconsideredonlyinatertiarycenter.In
addition,becausedeliveryisalwaysappropriateforthemother,someauthorities
considerdeliveryasthedefinitivetreatmentregardlessofgestationalage.However,
deliverymaynotbeoptimalforafetusthatisextremelypremature.Therefore,ina
carefullychosenpopulation,expectantmanagementmaybenefitthefetuswithout
greatlycompromisingmaternalhealth.
Allofthesepatientsmustbeevaluatedinalaboranddeliveryunitfor24hours
beforeadecisionforexpectantmanagementcanbemade.Duringthisperiod,
maternalandfetalevaluationmustshowthatthefetusdoesnothaveseveregrowth
restrictionorfetaldistress.Inaddition,maternalurineoutputmustbeadequate.
Thewomanmusthaveessentiallynormallaboratoryvalues(withtheexclusive
exceptionofmildlyelevatedliverfunctiontestresultsthatarelessthantwicethe
normalvalue)andhypertensionthatcanbecontrolled.
Fetalmonitoringshouldincludedailynonstresstestingandultrasonography
performedtomonitorforthedevelopmentofoligohydramniosanddecreasedfetal
movement.Inaddition,fetalgrowthdeterminationat2weekintervalsmustbe
performedtodocumentadequatefetalgrowth.A24hoururinecollectionforprotein
mayberepeated.Corticosteroidsforfetallungmaturityshouldbeadministered
priorto34weeks.
http://emedicine.medscape.com/article/1476919overview
14/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
Dailybloodtestsshouldbeperformedforliverfunctiontests(LFTs),CBCcount,
uricacid,andLDH.Patientsshouldbeinstructedtoreportanyheadache,visual
changes,epigastricpain,ordecreasedfetalmovement.
Criteriafordelivery
Womenwithseverepreeclampsiawhoaremanagedexpectantlymustbedelivered
underthefollowingcircumstances:
Nonreassuringfetaltestingincludingnonreassuringnonstresstest,
biophysicalprofilescore,and/orpersistentabsentorreverseddiastolicflow
onumbilicalarteryDopplervelocimetry
Rupturedmembranes
UncontrollableBP(unresponsivetomedicaltherapy)
Oligohydramnios,withamnioticfluidindex(AFI)oflessthan5cm
Severeintrauterinegrowthrestrictioninwhichtheestimatedfetalweightis
lessthan5%
Oliguria(<500mL/24hours)
Serumcreatininelevelofatleast1.5mg/dL
Pulmonaryedema
Shortnessofbreathorchestpainwithpulseoximetryof<94%onroomair
Headachethatispersistentandsevere
Rightupperquadranttenderness
DevelopmentofHELLP(hemolysis,elevatedliverenzyme,low
platelets)syndrome
Eclampsia
Plateletcountlessthan100,000/L
Placentalabruption
Unexplainedcoagulopathy
SeizureTreatmentandProphylaxisWithMagnesium
Sulfate
Thebasicprinciplesofairway,breathing,andcirculation(ABC)shouldalwaysbe
followedasageneralprincipleofseizuremanagement.
Magnesiumsulfateisthefirstlinetreatmentforthepreventionofprimaryand
recurrenteclampticseizures.Foreclampticseizuresthatarerefractoryto
magnesiumsulfate,lorazepamandphenytoinmaybeusedassecondlineagents.
TheAmericanCollegeofObstetriciansandGynecologists(ACOG)andtheSociety
forMaternalFetalMedicine(SMFM)continuetosupporttheshortterm(usually<48
hours)useofmagnesiumsulfateinobstetriccareforconditionsandtreatment
durationsthatincludethefollowing[66]:
Forpreventionandtreatmentofseizuresinwomenwithpreeclampsia
oreclampsia
Forfetalneuroprotectionbeforeanticipatedearlypreterm(<32weeksof
gestation)delivery
Forshorttermprolongationofpregnancy(48hours)toallowforthe
administrationofantenatalcorticosteroidsinpregnantwomenwhoareatrisk
ofpretermdeliverywithin7days
Activeseizuresshouldbetreatedwithintravenousmagnesiumsulfateasafirstline
agent. [5]Aloadingdoseof4gshouldbegivenbyaninfusionpumpover510
minutes,followedbyaninfusionof1g/hmaintainedfor24hoursafterthelast
seizure.Recurrentseizuresshouldbetreatedwithanadditionalbolusof2goran
increaseintheinfusionrateto1.5gor2gperhour.
Prophylactictreatmentwithmagnesiumsulfateisindicatedforallpatientswith
severepreeclampsia.However,noconsensusexistsastowhetherpatientswith
mildpreeclampsianeedmagnesiumseizureprophylaxis.AlthoughACOG
recommendsmagnesiumsulfateinseverepreeclampsia,ithasnotrecommended
thistherapyinallcasesofmildpreeclampsia.
SomepractitionerswithholdmagnesiumsulfateifBPisstableand/ormildly
elevatedandifthelaboratoryvaluesforLFTsandplateletsaremildlyabnormal
and/orstable.Otherphysiciansfeelthatevenpatientswithgestationalhypertension
shouldreceivemagnesium,asasmallpercentageofthesepatientsmayeitherhave
preeclampsiaormaydevelopit.Theultimatedecisionshoulddependonthe
comfortlevelofthelaboranddeliverystaffinadministeringintravenous(IV)
magnesiumsulfate.Anestimated100patientsneedtobetreatedwithmagnesium
sulfatetherapytoprevent1caseofeclampsia. [5,67,68]
AcuteTreatmentofSevereHypertensionin
Pregnancy
Inthesettingofseverehypertension(SBP>160mmHgDBP>110mmHg),
antihypertensivetreatmentisrecommended.Thegoalofhypertensiontreatmentis
tolowerBPtopreventcerebrovascularandcardiaccomplicationswhilemaintaining
uteroplacentalbloodflow(ie,maintainBParound140/90mmHg).However,
althoughantihypertensivetreatmentdecreasestheincidenceofcerebrovascular
problems,itdoesnotaltertheprogressionofpreeclampsia.Controlofmildly
increasedBPdoesnotappeartoimproveperinatalmorbidityormortality,andit
may,infact,reducebirthweight.
http://emedicine.medscape.com/article/1476919overview
15/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
Hydralazine
Hydralazineisadirectperipheralarteriolarvasodilatorand,inthepast,waswidely
usedasthefirstlinetreatmentforacutehypertensioninpregnancy. [69,70]This
agenthasaslowonsetofaction(1020min)andpeaksapproximately20minutes
afteradministration.HydralazineshouldbegivenasanIVbolusatadoseof510
mg,dependingontheseverityofhypertension,andmaybeadministeredevery20
minutesuptoamaximumdoseof30mg.
Thesideeffectsofhydralazineareheadache,nausea,andvomiting.Importantly,
hydralazinemayresultinmaternalhypotension,whichcansubsequentlyresultina
nonreassuringfetalheartratetracinginthefetus. [13]
Inametaanalysis,Mageeetalpointedoutthathydralazinewasassociatedwith
worsematernalandperinataloutcomesthanwerelabetalolandnifedipine.
Furthermore,hydralazinewasassociatedwithmorematernalsideeffectsthanwere
labetalolandnifedipine. [69]
Labetalol
Labetalolisaselectivealphablockerandanonselectivebetablockerthatproduces
vasodilatationandresultsinadecreaseinsystemicvascularresistance.Thedosage
forlabetalolis20mgIVwithrepeatdoses(40,80,80,and80mg)every10
minutesuptoamaximumdoseof300mg.DecreasesinBPareobservedafter5
minutes(incontrasttothesloweronsetofactionofhydralazine),andthedrug
resultsinlessovershoothypertensionthandoeshydralazine.
Labetaloldecreasessupraventricularrhythmandslowstheheartrate,reducing
myocardialoxygenconsumption.Nochangeinafterloadisobservedaftertreatment
withlabetalol.Thesideeffectsoflabetalolaredizziness,nausea,andheadaches.
AftersatisfactorycontrolwithIVadministrationhasbeenachieved,anoral
maintenancedosecanbestarted. [13,69]
Nifedipine
Calciumchannelblockersactonarteriolarsmoothmuscleandinducevasodilatation
byblockingcalciumentryintothecells.Nifedipineistheoralcalciumchannel
blockerthatisusedinthemanagementofhypertensioninpregnancy.Thedosage
ofnifedipineis10mgPOevery1530minutes,withamaximumof3doses.The
sideeffectsofcalciumchannelblockersincludetachycardia,palpitations,and
headaches.Concomitantuseofcalciumchannelblockersandmagnesiumsulfateis
tobeavoided.Nifedipineiscommonlyusedpostpartuminpatientswith
preeclampsia,forBPcontrol. [13,69]
Sodiumnitroprusside
Inaseverehypertensiveemergency,whentheabovementionedmedicationshave
failedtolowerBP,sodiumnitroprussidemaybegiven.Nitroprussideresultsinthe
releaseofnitricoxide,whichinturncausessignificantvasodilation.Preloadand
afterloadarethengreatlydecreased.Theonsetofactionisrapid,andsevere
reboundhypertensionmayresult.Cyanidepoisoningmayoccursubsequenttoits
useinthefetus.Therefore,sodiumnitroprussideshouldbereservedforusein
postpartumcareorforadministrationjustbeforethedeliveryofthefetus. [13]
FluidManagement
Littleclinicalevidenceexistsinthepublishedliteratureonwhichtobasedecisions
regardingthemanagementoffluidsduringpreeclampsia.Currently,noprospective
studiesonthistopicareavailable,andguidelinesarelargelybasedonconsensus
andretrospectivereview.
Despitethepresenceofperipheraledema,patientswithpreeclampsiaare
intravascularlyvolumedepleted,withhighperipheralvascularresistance.Diuretics
shouldbeavoided.
Aggressivevolumeresuscitationmayleadtopulmonaryedema,whichisacommon
causeofmaternalmorbidityandmortality.Pulmonaryedemaoccursmost
frequently4872hourspostpartum,probablyduetomobilizationofextravascular
fluid.Becausevolumeexpansionhasnodemonstratedbenefit,patientsshouldbe
fluidrestrictedwhenpossible,atleastuntiltheperiodofpostpartumdiuresis.
Volumeexpansionhasnotbeenshowntoreducetheincidenceoffetaldistressand
shouldbeusedjudiciously.
Centralvenousorpulmonaryarterypressuremonitoringmaybeindicatedincritical
cases.Acentralvenouspressure(CVP)of5mmHginwomenwithnoheart
diseaseindicatessufficientintravascularvolume,andmaintenancefluidsaloneare
sufficient.Totalfluidsshouldgenerallybelimitedto80mL/hor1mL/kg/h.
Carefulmeasurementoffluidinputandoutputisadvisable,particularlyinthe
immediatepostpartumperiod.Manypatientswillhaveabrief(upto6h)periodof
oliguriafollowingdeliverythisshouldbeanticipatedandnotovercorrected.
PostpartumManagement
http://emedicine.medscape.com/article/1476919overview
16/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
Preeclampsiaresolvesafterdelivery.However,patientsmaystillhaveanelevated
BPpostpartum.Liverfunctiontestsandplateletcountsmustbeperformedto
documentdecreasingvaluespriortohospitaldischarge.Inaddition,onethirdof
seizuresoccurinthepostpartumperiod,mostwithin24hoursofdelivery,and
almostallwithin48hours. [71]Therefore,magnesiumsulfateseizureprophylaxisis
continuedfor24hourspostpartum.(SeeSeizureTreatmentandProphylaxisWith
MagnesiumSulfate.)
Rarely,apatientmayhaveelevatedliverenzymes,thrombocytopenia,andrenal
insufficiencymorethan72hoursafterdelivery.Inthesecases,thepossibilityof
hemolyticuremicsyndrome(HUS)orthromboticthrombocytopenicpurpura(TTP)
mustbeconsidered.Insuchsituations,plasmapheresis,alongwithcorticosteroid
therapy,maybeofsomebenefittosuchpatientsandmustbediscussedwithrenal
andhematologyconsultants.
Inaddition,theuseofdexamethasone(10mgIVq612hfor2dosesfollowedby5
mgIVq612hfor2doses)hasbeenproposedinthepostpartumperiodtorestore
plateletcounttonormalrangeinpatientswithpersistentthrombocytopenia. [72,73]
Theeffectivenessofthistherapyinpreventingseverehemorrhageorameliorating
thediseasecourseneedsfurtherinvestigation.
ElevatedBPmaybecontrolledwithnifedipineorlabetalolpostpartum.Ifapatient
isdischargedwithBPmedication,reassessmentandaBPcheckshouldbe
performed,atthelatest,1weekafterdischarge.Unlessawomanhasundiagnosed
chronichypertension,inmostcasesofpreeclampsia,theBPreturnstobaselineby
12weekspostpartum.
Eclampsiaiscommonafterdeliveryandhasoccurredupto6weeksafterdelivery.
AlSafietalsuggestthatthefirstweekafterdischargeisthemostcriticalperiodfor
thedevelopmentofpostpartumeclampsia.Discussingtherisksandeducating
patientsaboutthepossibilityofdelayedpostpartumpreeclampsiaisimportant,
regardlessofwhethertheydevelophypertensivediseasepriortodischarge. [74]
Patientsatriskforeclampsiashouldbecarefullymonitoredpostpartum. [75]
Additionally,patientswithpreeclampsiawhoweresuccessfullytreatedwithdelivery
maypresentwithrecurrentpreeclampsiaupto4weekspostpartum.
PreventionandPredictionofPreeclampsia
Effortstopreventpreeclampsiahavebeendisappointing. [76]
Aspirin
Asystematicreviewof14trialsusinglowdoseaspirin(60150mg/d)inwomenwith
riskfactorsforpreeclampsiaconcludedthataspirinreducedtheriskofpreeclampsia
andperinataldeath,althoughitdidnotsignificantlyaffectbirthweightortheriskof
abruption. [77]Lowdoseaspirininunselectednulliparouswomenseemstoreduce
theincidenceofpreeclampsiaonlyslightly. [78]Forwomenwithriskfactorsfor
preeclampsia,startinglowdoseaspirin(commonly,1tabletofbabyaspirinperday),
beginningat1214weeks'gestation,isreasonable.Thesafetyoflowdoseaspirin
useinthesecondandthirdtrimestersiswellestablished. [77,79]
Onthebasisoflimitedevidencefromasystematicreviewandmetaanalysis,the
additionoflowmolecularweightheparinorunfractionatedheparintolowdose
aspirinhasthepotentialtoreducetheprevalenceofpreeclampsiaandbirthof
smallforgestationalageneonatesinwomenwithahistoryofpreeclampsia. [80]
Heparin
Theuseoflowmolecularweightheparininwomenwiththrombophiliawhohavea
historyofadverseoutcomehasbeeninvestigated.Todate,however,nodata
suggestthattheuseofheparinprophylaxislowerstheincidenceofpreeclampsia.
Calciumandvitaminsupplements
ResearchintotheuseofcalciumandvitaminCandEsupplementationsinlowrisk
populationsdidnotfindareductionintheincidenceofpreeclampsia. [81,82,83]Ina
multicenter,randomized,controlledtrial,Villaretalfoundthatatthedosesusedfor
supplementation,vitaminsCandEwerenotassociatedwithareductionof
preeclampsia,eclampsia,gestationalhypertension,oranyothermaternaloutcome.
Lowbirthweight,smallforgestationalage,andperinataldeathswerealso
unaffected. [84]
AstudybyVadilloOrtegaetalsuggeststhatinahighriskpopulation,
supplementationduringpregnancywithaspecialfood(eg,bars)containingL
arginineandantioxidantvitaminsmayreducetheriskofpreeclampsia.However,
antioxidantvitaminsalonedonotprotectagainstpreeclampsia.Morestudies
performedonlowriskpopulationsareneeded. [85]
ResultsfromtheNorwegianMotherandChildCohortStudysuggestthat
supplementationofmilkbasedprobioticsmayreducetheriskofpreeclampsiain
primiparouswomen.Aprospectiverandomizedtrialhasnotyetbeendoneto
evaluatethisintervention. [86]
ScreeningTests
http://emedicine.medscape.com/article/1476919overview
17/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
Preeclampsiaisanappropriatediseasetoscreen,asitiscommon,important,and
increasesmaternalandperinatalmortality.However,althoughnumerousscreening
testsforpreeclampsiahavebeenproposedoverthepastfewdecades,notesthas
sofarbeenshowntoappropriatelyscreenforthedisease. [87](Measurementof
urinarykallikreinwasshowntohaveahighpredictivevalue,butitwasnot
reproducible. [88,89])
Morerecently,aprospectivestudydemonstratedthatansFlt1:PlGFratioof38or
lowerhadanegativepredictivevalueof99.3%(95%confidenceinterval[CI],97.9
to99.9),suggestinganextremelyunlikelydevelopmentofpreeclampsiaorHELLP
(hemolysis,elevatedliverenzyme,lowplatelets)syndromewithin1week,inwomen
withaclinicalsuspicionofpreeclampsiaorHELLPsyndrome. [58]Therefore,ansFlt
1:PlGFratioof38orlowermayhaveapotentialroleinpredictingtheshortterm
absenceofpreeclampsiainwomeninwhomthesyndromeissuspectedclinically.
[58]Arandomizedtrialisnecessarytodeterminetheintervalofsuchtestingin
womensuspectedonhavingpreeclampsiaorHELLPsyndrome,aswellasthe
effectofthisscreeningtestonmaternalandfetaloutcomes.
Currently,theclinicalvalueofanaccuratepredictivetestforpreeclampsiaisnot
clear,aseffectivepreventionisstilllacking.Intensivemonitoringinwomenwhoare
atincreasedriskfordevelopingpreeclampsia,whenidentifiedbyapredictivetest,
maylowertheincidenceofadverseoutcomeforthemotherandtheneonate.
However,theeffectivenessofsuchastrategymustberigorouslyinvestigated.
Prognosis
Morbidityandmortality
Worldwide,preeclampsiaandeclampsiaareestimatedtoberesponsiblefor
approximately14%ofmaternaldeathsperyear(50,00075,000). [21]Morbidityand
mortalityinpreeclampsiaandeclampsiaarerelatedtothefollowingconditions:
Systemicendothelialdysfunction
Vasospasmandsmallvesselthrombosisleadingtotissueandorgan
ischemia
Centralnervoussystem(CNS)events,suchasseizures,strokes,and
hemorrhage
Acutetubularnecrosis
Coagulopathies
Placentalabruptioninthemother
Fetalexposuretopreeclampsiamaybelinkedtoautismanddevelopmentaldelay
(DD). [90,91]Inapopulationbasedstudyof1061childrenfromsingleton
pregnanciesincluding517withautismspectrumdisorder(ASD),194withDD,
and350whoweretypicallydeveloping(TD)fetalexposuretopreeclampsiawas
associatedwithagreaterthantwofoldincreaseintheriskofASDandagreater
thanfivefoldincreaseintheriskofDD. [90,91]
OfthechildrenwithASD,7.7%hadbeenexposedtopreeclampsiainutero,
comparedwith5.1%ofthosewithDDand3.7%ofthosewithTD. [91]After
adjustmentforparity,maternaleducation,andprepregnancyobesity,theadjusted
oddsratio(aOR)forASDwithexposuretopreeclampsiawas2.36(95%confidence
interval[CI],1.184.68).Inanalyseslimitedtowomenwhohadhadsevere
preeclampsia,theaORforASDwas2.29(95%CI,0.975.43),andtheaORforDD
was5.49(95%CI,2.0614.64).
Recurrence
Ingeneral,therecurrenceriskofpreeclampsiainawomanwhoseprevious
pregnancywascomplicatedbypreeclampsianeartermisapproximately10%. [48]If
awomanhaspreviouslysufferedfrompreeclampsiawithseverefeatures(including
HELLP[hemolysis,elevatedliverenzyme,lowplatelets]syndromeand/or
eclampsia),shehasa20%riskofdevelopingpreeclampsiasometimeinher
subsequentpregnancy. [92,93,94,95,96,97]
IfawomanhashadHELLPsyndromeoreclampsia,therecurrenceriskofHELLP
syndromeis5%[93]andofeclampsiaitis2%. [95,96,97]Theearlierthedisease
manifestsduringtheindexpregnancy,thehigherthechanceofrecurrencerises.If
preeclampsiapresentedclinicallybefore30weeks'gestation,thechanceof
recurrencemaybeashighas40%. [98]
ThefullPIERSmodelhasbeenvalidatedandwassuccessfulinpredictingadverse
outcomesinadvancetherefore,itispotentiallyabletoinfluencetreatmentchoices
beforecomplicationsarise. [99]
ContributorInformationandDisclosures
Author
KeeHakLim,MDClinicalAssociateProfessor,DepartmentofObstetricsandGynecology,HarvardMedical
SchoolPhysicianinMaternalFetalMedicine,BethIsraelDeaconessMedicalCenter
KeeHakLim,MDisamemberofthefollowingmedicalsocieties:AmericanCollegeofObstetriciansand
Gynecologists,AmericanInstituteofUltrasoundinMedicine,SocietyforMaternalFetalMedicine,JohnsHopkins
MedicalandSurgicalAssociation
http://emedicine.medscape.com/article/1476919overview
18/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
Disclosure:Nothingtodisclose.
Coauthor(s)
GuySteinberg,MD,MPH,MScFellowinMaternalFetalMedicine,BethIsraelDeaconessMedical
Center/HarvardMedicalSchool
Disclosure:Nothingtodisclose.
ChiefEditor
RonaldMRamus,MDProfessorofObstetricsandGynecology,Director,DivisionofMaternalFetalMedicine,
VirginiaCommonwealthUniversitySchoolofMedicine
RonaldMRamus,MDisamemberofthefollowingmedicalsocieties:AmericanCollegeofObstetriciansand
Gynecologists,AmericanInstituteofUltrasoundinMedicine,MedicalSocietyofVirginia,SocietyforMaternal
FetalMedicine
Disclosure:Nothingtodisclose.
Acknowledgements
ADavidBarnes,MD,PhD,MPH,FACOGConsultingStaff,DepartmentofObstetricsandGynecology,
MammothHospital(MammothLakes,California),PioneerValleyHospital(SaltLakeCity,Utah),WarrenGeneral
Hospital(Warren,Pennsylvania),andMountainWestHospital(Tooele,Utah)
ADavidBarnes,MD,PhD,MPH,FACOGisamemberofthefollowingmedicalsocieties:AmericanCollegeof
ForensicExaminers,AmericanCollegeofObstetriciansandGynecologists,AmericanMedicalAssociation,
AssociationofMilitarySurgeonsoftheUS,andUtahMedicalAssociation
Disclosure:Nothingtodisclose.
PamelaLDyne,MDProfessorofClinicalMedicine/EmergencyMedicine,UniversityofCalifornia,LosAngeles,
DavidGeffenSchoolofMedicineAttendingPhysician,DepartmentofEmergencyMedicine,OliveViewUCLA
MedicalCenter
PamelaLDyne,MDisamemberofthefollowingmedicalsocieties:AmericanAcademyofEmergencyMedicine,
AmericanCollegeofEmergencyPhysicians,andSocietyforAcademicEmergencyMedicine
Disclosure:Nothingtodisclose.
MertErogul,MDAssistantProfessorofEmergencyMedicine,UniversityHospitalofBrooklyn:ConsultingStaff,
DepartmentofEmergencyMedicine,KingsCountyHospitalCenter
MertErogul,MDisamemberofthefollowingmedicalsocieties:AmericanCollegeofEmergencyPhysicians,
AmericanMedicalAssociation,andSocietyforAcademicEmergencyMedicine
Disclosure:Nothingtodisclose.
JohnJKavanaghJrMD,Chief,Professor,DepartmentofInternalMedicine,SectionofGynecologicaland
MedicalTherapeutics,MDAndersonCancerCenter,UniversityofTexasMedicalSchoolatHouston
JohnJKavanaghJrisamemberofthefollowingmedicalsocieties:AmericanAssociationforCancerResearch,
AmericanAssociationfortheAdvancementofScience,AmericanAssociationfortheHistoryofMedicine,
AmericanCollegeofPhysicians,AmericanFederationforMedicalResearch,AmericanMedicalAssociation,
SocietyofGynecologistOncologists,SouthernMedicalAssociation,andTexasMedicalAssociation
Disclosure:Nothingtodisclose.
AssaadJSayah,MDChief,DepartmentofEmergencyMedicine,CambridgeHealthAlliance
AssaadJSayah,MDisamemberofthefollowingmedicalsocieties:NationalAssociationofEMSPhysicians
Disclosure:Nothingtodisclose.
ZinaSemenovskaya,MDResidentPhysician,DepartmentofEmergencyMedicine,KingsCountyHospital,
StateUniversityofNewYorkDownstateMedicalCenterCollegeofMedicine
Disclosure:Nothingtodisclose.
AashitKShah,MD,FAAN,FANAProfessorofNeurology,Director,ComprehensiveEpilepsyProgram,Program
Director,ClinicalNeurophysiologyFellowship,DetroitMedicalCenter,WayneStateUniversitySchoolofMedicine
AashitKShah,MD,FAAN,FANAisamemberofthefollowingmedicalsocieties:AmericanAcademyof
Neurology,AmericanClinicalNeurophysiologySociety,AmericanEpilepsySociety,andAmericanNeurological
Assocation
Disclosure:UCBPharma,Consultingfee,SpeakingandteachingCyberonics,Consultingfee,ConsultingUCB
Pharma,Grant/researchfunds,Other
GuySteinberg,MD,MPH,MScFellowinMaternalFetalMedicine,BethIsraelDeaconessMedical
Center/HarvardMedicalSchool
Disclosure:Nothingtodisclose.
FranciscoTalavera,PharmD,PhDAdjunctAssistantProfessor,UniversityofNebraskaMedicalCenterCollege
ofPharmacyEditorinChief,MedscapeDrugReference
Disclosure:MedscapeSalaryEmployment
MarkZwanger,MD,MBAAssistantProfessor,DepartmentofEmergencyMedicine,JeffersonMedicalCollege
ofThomasJeffersonUniversity
http://emedicine.medscape.com/article/1476919overview
19/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
MarkZwanger,MD,MBAisamemberofthefollowingmedicalsocieties:AmericanAcademyofEmergency
Medicine,AmericanCollegeofEmergencyPhysicians,andAmericanMedicalAssociation
Disclosure:Nothingtodisclose.
References
1.[Guideline]AmericanCollegeofObstetriciansandGynecologists,TaskForceonHypertensionin
Pregnancy.Hypertensioninpregnancy.ReportoftheAmericanCollegeofObstetriciansandGynecologists
TaskForceonHypertensioninPregnancy.ObstetGynecol.2013Nov.122(5):112231.[Medline].[Full
Text].
2.AmericanCollegeofObstetriciansandGynecologists.Hypertensioninpregnancy.ACOGTechnicalBulletin
No.219.WashingtonDC:1996.
3.TaylorRN,deGrootCJ,ChoYK,etal.Circulatingfactorsasmarkersandmediatorsofendothelialcell
dysfunctioninpreeclampsia.SeminReprodEndocrinol.1998.16(1):1731.[Medline].
4.BarronWM,HeckerlingP,HibbardJU,etal.Reducingunnecessarycoagulationtestinginhypertensive
disordersofpregnancy.ObstetGynecol.1999Sep.94(3):36470.[Medline].
5.SibaiBM.Magnesiumsulfateprophylaxisinpreeclampsia:Lessonslearnedfromrecenttrials.AmJObstet
Gynecol.2004Jun.190(6):15206.[Medline].
6.LaganaAS,FavilliA,TrioloO,GraneseR,GerliS.Earlyserummarkersofpreeclampsia:arewestepping
forward?.JMaternFetalNeonatalMed.2015Nov23.15.[Medline].
7.SibaiBM.Diagnosisandmanagementofgestationalhypertensionandpreeclampsia.ObstetGynecol.
2003Jul.102(1):18192.[Medline].
8.NessRB,RobertsJM.Heterogeneouscausesconstitutingthesinglesyndromeofpreeclampsia:a
hypothesisanditsimplications.AmJObstetGynecol.1996Nov.175(5):136570.[Medline].
9.VattenLJ,SkjaervenR.Ispreeclampsiamorethanonedisease?.BJOG.2004Apr.111(4):298302.
[Medline].
10.VillarJ,BetranAP,GulmezogluM.Epidemiologicalbasisfortheplanningofmaternalhealthservices.
WHO/RHR.2001.
11.KhedunSM,MoodleyJ,NaickerT,etal.Drugmanagementofhypertensivedisordersofpregnancy.
PharmacolTher.1997.74(2):22158.[Medline].
12.NgocNT,MerialdiM,AbdelAleemH,CarroliG,PurwarM,ZavaletaN,etal.Causesofstillbirthsand
earlyneonataldeaths:datafrom7993pregnanciesinsixdevelopingcountries.BullWorldHealthOrgan.
2006Sep.84(9):699705.[Medline].[FullText].
13.ReportoftheNationalHighBloodPressureEducationProgramWorkingGrouponHighBloodPressurein
Pregnancy.AmJObstetGynecol.2000Jul.183(1):S1S22.[Medline].
14.RodriguezThompsonD,LiebermanES.Useofarandomurinaryproteintocreatinineratioforthe
diagnosisofsignificantproteinuriaduringpregnancy.AmJObstetGynecol.2001Oct.185(4):80811.
[Medline].
15.MackillopL.Preeclampsia:reducingtheriskwithcalciumsupplements.BMJClinEvid.2015Dec7.2015:
[Medline].
16.WitlinAG,FriedmanSA,SibaiBM.Theeffectofmagnesiumsulfatetherapyonthedurationoflaborin
womenwithmildpreeclampsiaatterm:arandomized,doubleblind,placebocontrolledtrial.AmJObstet
Gynecol.1997Mar.176(3):6237.[Medline].
17.LivingstonJC,LivingstonLW,RamseyR,etal.Magnesiumsulfateinwomenwithmildpreeclampsia:a
randomizedcontrolledtrial.ObstetGynecol.2003Feb.101(2):21720.[Medline].
18.BellamyL,CasasJP,HingoraniAD,etal.Preeclampsiaandriskofcardiovasculardiseaseandcancerin
laterlife:systematicreviewandmetaanalysis.BMJ.2007Nov10.335(7627):974.[Medline].
19.HarskampRE,ZeemanGG.Preeclampsia:atriskforremotecardiovasculardisease.AmJMedSci.2007
Oct.334(4):2915.[Medline].
20.CunninghamFG,VenoKJ,BloomSL,etal.PregnancyHypertension.In:WilliamsObstetrics.23e.2010.
21.WHO,2004.Bethesda,MD.GlobalBurdenofDiseasefortheYear2001byWorldBankRegion,forUsein
DiseaseControlPrioritiesinDevelopingCountries,NationalInstitutesofHealth:WHO.Makeeverymother
andchildcount.WorldHealthReport,2005,Geneva:WorldHealthOrga...2nded.
22.RedmanCW,SargentIL.Latestadvancesinunderstandingpreeclampsia.Science.2005Jun10.
308(5728):15924.[Medline].
23.ZhouY,DamskyCH,FisherSJ.Preeclampsiaisassociatedwithfailureofhumancytotrophoblaststo
mimicavascularadhesionphenotype.Onecauseofdefectiveendovascularinvasioninthissyndrome?.J
ClinInvest.1997May1.99(9):215264.[Medline].[FullText].
24.ZhouY,DamskyCH,FisherSJ.Preeclampsiaisassociatedwithfailureofhumancytotrophoblaststo
mimicavascularadhesionphenotype.Onecauseofdefectiveendovascularinvasioninthissyndrome?.J
ClinInvest.1997May1.99(9):215264.[Medline].
25.ZhouY,DamskyCH,ChiuK,etal.Preeclampsiaisassociatedwithabnormalexpressionofadhesion
moleculesbyinvasivecytotrophoblasts.JClinInvest.1993Mar.91(3):95060.[Medline].
http://emedicine.medscape.com/article/1476919overview
20/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
26.LimKH,ZhouY,JanatpourM,etal.Humancytotrophoblastdifferentiation/invasionisabnormalinpre
eclampsia.AmJPathol.1997Dec.151(6):180918.[Medline].
27.FriedmanSA,SchiffE,EmeisJJ,etal.Biochemicalcorroborationofendothelialinvolvementinsevere
preeclampsia.AmJObstetGynecol.1995Jan.172(1Pt1):2023.[Medline].
28.TaylorRN,GrimwoodJ,TaylorRS,etal.Longitudinalserumconcentrationsofplacentalgrowthfactor:
evidenceforabnormalplacentalangiogenesisinpathologicpregnancies.AmJObstetGynecol.2003Jan.
188(1):17782.[Medline].
29.MaynardSE,MinJY,MerchanJ,etal.Excessplacentalsolublefmsliketyrosinekinase1(sFlt1)may
contributetoendothelialdysfunction,hypertension,andproteinuriainpreeclampsia.JClinInvest.2003
Mar.111(5):64958.[Medline].
30.LevineRJ,MaynardSE,QianC,etal.Circulatingangiogenicfactorsandtheriskofpreeclampsia.NEngl
JMed.2004Feb12.350(7):67283.[Medline].
31.ThadhaniR,MutterWP,WolfM,etal.Firsttrimesterplacentalgrowthfactorandsolublefmsliketyrosine
kinase1andriskforpreeclampsia.JClinEndocrinolMetab.2004Feb.89(2):7705.[Medline].
32.BillsV,SalmonA,HarperS,etal.ImpairedvascularpermeabilityregulationcausedbytheVEGF(165)b
splicevariantinpreeclampsia.BJOG.2011Sep.118(10):12531261.[Medline].
33.LevineRJ,LamC,QianC,etal.Solubleendoglinandothercirculatingantiangiogenicfactorsin
preeclampsia.NEnglJMed.2006Sep7.355(10):9921005.[Medline].
34.VenkateshaS,ToporsianM,LamC,etal.Solubleendoglincontributestothepathogenesisof
preeclampsia.NatMed.2006Jun.12(6):6429.[Medline].
35.GermainSJ,SacksGP,SoorannaSR,etal.Systemicinflammatorypriminginnormalpregnancyand
preeclampsia:theroleofcirculatingsyncytiotrophoblastmicroparticles.JImmunol.2007May1.
178(9):594956.[Medline].
36.LykkeJA,PaidasMJ,LanghoffRoosJ.Recurringcomplicationsinsecondpregnancy.ObstetGynecol.
2009Jun.113(6):121724.[Medline].
37.SweetingAN,RossGP,HyettJ,etal.Gestationaldiabetesmellitusinearlypregnancy:evidenceforpoor
pregnancyoutcomesdespitetreatment.DiabetesCare.2016Jan.39(1):7581.[Medline].
38.CondeAgudeloA,VillarJ,LindheimerM.Maternalinfectionandriskofpreeclampsia:systematicreview
andmetaanalysis.AmJObstetGynecol.2008Jan.198(1):722.[Medline].
39.ShandA,NassarN,VonDadelszenP,InnisS,GreenT.MaternalvitaminDstatusinpregnancyand
adversepregnancyoutcomesinagroupathighriskforpreeclampsia.BJOG.2010Dec.117(13):15938.
[Medline].
40.KnightM,KurinczukJJ,SparkP,BrocklehurstP.ExtremeobesityinpregnancyintheUnitedKingdom.
ObstetGynecol.2010May.115(5):98997.[Medline].
41.FoxS.EarlyandLateOnsetPreeclampsia:2DifferentEntities?.MedscapeMedicalNews.Availableat
http://www.medscape.com/viewarticle/810245.Accessed:September6,2013.
42.LisonkovaS,JosephKS.Incidenceofpreeclampsia:riskfactorsandoutcomesassociatedwithearly
versuslateonsetdisease.AmJObstetGynecol.2013Aug22.[Medline].
43.CooraySD,EdmondsSM,TongS,SamarasekeraSP,WhiteheadCL.Characterizationofsymptoms
immediatelyprecedingeclampsia.ObstetGynecol.2011Nov.118(5):9959.[Medline].
44.AndrusSS,WolfsonAB.Postpartumpreeclampsiaoccurringafterresolutionofantepartumpreeclampsia.
JEmergMed.2010Feb.38(2):16870.[Medline].
45.SibaiBM.Diagnosis,controversies,andmanagementofthesyndromeofhemolysis,elevatedliver
enzymes,andlowplateletcount.ObstetGynecol.2004May.103(5Pt1):98191.[Medline].
46.WaughJJ,ClarkTJ,DivakaranTG,etal.Accuracyofurinalysisdipsticktechniquesinpredictingsignificant
proteinuriainpregnancy.ObstetGynecol.2004Apr.103(4):76977.[Medline].
47.DurnwaldC,MercerB.Aprospectivecomparisonoftotalprotein/creatinineratioversus24hoururine
proteininwomenwithsuspectedpreeclampsia.AmJObstetGynecol.2003Sep.189(3):84852.[Medline].
48.ChesleyLC.Hypertensivedisordersofpregnancy.NewYork:AppletonCenturyCrofts1978.p42143.
49.FisherKA,LugerA,SpargoBH,etal.Hypertensioninpregnancy:clinicalpathologicalcorrelationsand
remoteprognosis.Medicine(Baltimore).1981Jul.60(4):26776.[Medline].
50.Larson,NF.CongoRedDotUrineTestCanPredict,DiagnosePreeclampsia.MedscapeMedicalNews.
Availableathttp://www.medscape.com/viewarticle/716741?src=rss\t_blank.
51.BawejaS,KentA,MastersonR,RobertsS,McMahonL.Predictionofpreeclampsiainearlypregnancyby
estimatingthespoturinaryalbumin:creatinineratiousinghighperformanceliquidchromatography.BJOG.
2011Aug.118(9):112632.[Medline].
52.HandL.UrineTestforMisfoldedProteinsMayDiagnosePreeclampsia.MedscapeMedicalNews.
Availableathttp://www.medscape.com/viewarticle/828545.Accessed:July28,2014.
53.BuhimschiIA,NayeriUA,ZhaoG,ShookLL,PensalfiniA,FunaiEF,etal.Proteinmisfolding,
congophilia,oligomerization,anddefectiveamyloidprocessinginpreeclampsia.SciTranslMed.2014Jul
16.6(245):245ra92.[Medline].
54.ChappellLC,DuckworthS,SeedPT,GriffinM,MyersJ,MackillopL,etal.Diagnosticaccuracyof
placentalgrowthfactorinwomenwithsuspectedpreeclampsia:aprospectivemulticenterstudy.
Circulation.2013Nov5.128(19):212131.[Medline].
http://emedicine.medscape.com/article/1476919overview
21/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
55.LowryF.NewTestIdentifiesPreeclampsiaRequiringDelivery.Medscape[serialonline].Availableat
http://www.medscape.com/viewarticle/813764.Accessed:November11,2013.
56.MacReadyN.AStepClosertoPredictingPreeclampsiaRiskinDiabetes.Availableat
http://www.medscape.com/viewarticle/809509.Accessed:August20,2013.
57.HolmesVA,YoungIS,PattersonCC,MareshMJ,PearsonDW,WalkerJD,etal.TheRoleofAngiogenic
andAntiangiogenicFactorsintheSecondTrimesterinthePredictionofPreeclampsiainPregnantWomen
WithType1Diabetes.DiabetesCare.2013Aug6.[Medline].
58.ZeislerH,LlurbaE,ChantraineF,etal.PredictivevalueofthesFlt1:PlGFratioinwomenwithsuspected
preeclampsia.NEnglJMed.2016Jan7.374(1):1322.[Medline].
59.KaneSC,DennisAT.Dopplerassessmentofuterinebloodflowinpreeclampsia:areview.Hypertens
Pregnancy.2015Nov.34(4):400421.[Medline].
60.WagnerLK.Diagnosisandmanagementofpreeclampsia.AmFamPhysician.2004Dec15.70(12):2317
24.[Medline].
61.BartonJR,WitlinAG,SibaiBM.Managementofmildpreeclampsia.ClinObstetGynecol.1999Sep.
42(3):45569.[Medline].
62.HauthJC,EwellMG,LevineRJ,etal.Pregnancyoutcomesinhealthynulliparaswhodeveloped
hypertension.CalciumforPreeclampsiaPreventionStudyGroup.ObstetGynecol.2000Jan.95(1):248.
[Medline].
63.BuchbinderA,SibaiBM,CaritisS,etal.Adverseperinataloutcomesaresignificantlyhigherinsevere
gestationalhypertensionthaninmildpreeclampsia.AmJObstetGynecol.2002Jan.186(1):6671.
[Medline].
64.SibaiBM,BartonJR.Expectantmanagementofseverepreeclampsiaremotefromterm:patientselection,
treatment,anddeliveryindications.AmJObstetGynecol.2007Jun.196(6):514.e19.[Medline].
65.Committeeopinionno652:magnesiumsulfateuseinobstetrics.ObstetGynecol.2016Jan.127(1):e523.
[Medline].
66.Whichanticonvulsantforwomenwitheclampsia?EvidencefromtheCollaborativeEclampsiaTrial.Lancet.
1995Jun10.345(8963):145563.[Medline].
67.WitlinAG,SibaiBM.Magnesiumsulfatetherapyinpreeclampsiaandeclampsia.ObstetGynecol.1998
Nov.92(5):8839.[Medline].
68.MageeLA,ChamC,WatermanEJ,etal.Hydralazinefortreatmentofseverehypertensioninpregnancy:
metaanalysis.BMJ.2003Oct25.327(7421):95560.[Medline].
69.NadenRP,RedmanCW.Antihypertensivedrugsinpregnancy.ClinPerinatol.1985Oct.12(3):52138.
[Medline].
70.CreasyRK,ResnikR,IamsJD.MaternalFetalMedicine:PrinciplesandPractice.5thed.2004.859899.
71.MartinJNJr,PerryKGJr,BlakePG,etal.Bettermaternaloutcomesareachievedwithdexamethasone
therapyforpostpartumHELLP(hemolysis,elevatedliverenzymes,andthrombocytopenia)syndrome.AmJ
ObstetGynecol.1997Nov.177(5):10117.[Medline].
72.MartinJNJr,ThigpenBD,RoseCH,etal.Maternalbenefitofhighdoseintravenouscorticosteroidtherapy
forHELLPsyndrome.AmJObstetGynecol.2003Sep.189(3):8304.[Medline].
73.AlSafiZ,ImudiaAN,FilettiLC,etal.Delayedpostpartumpreeclampsiaandeclampsia:demographics,
clinicalcourse,andcomplications.ObstetGynecol.2011Nov.118(5):11027.[Medline].
74.YanceyLM,WithersE,BakesK,AbbottJ.Postpartumpreeclampsia:Emergencydepartmentpresentation
andmanagement.JEmergMed.2008Sep22.[Medline].
75.SibaiBM.Preventionofpreeclampsia:abigdisappointment.AmJObstetGynecol.1998Nov.
179(5):12758.[Medline].
76.CoomarasamyA,HonestH,PapaioannouS,etal.Aspirinforpreventionofpreeclampsiainwomenwith
historicalriskfactors:asystematicreview.ObstetGynecol.2003Jun.101(6):131932.[Medline].
77.SibaiBM,CaritisSN,ThomE,etal.Preventionofpreeclampsiawithlowdoseaspirininhealthy,
nulliparouspregnantwomen.TheNationalInstituteofChildHealthandHumanDevelopmentNetworkof
MaternalFetalMedicineUnits.NEnglJMed.1993Oct21.329(17):12138.[Medline].
78.KozerE,CosteiAM,BoskovicR,etal.Effectsofaspirinconsumptionduringpregnancyonpregnancy
outcomes:metaanalysis.BirthDefectsResBDevReprodToxicol.2003Feb.68(1):7084.[Medline].
79.RobergeS,DemersS,NicolaidesKH,BureauM,CoteS,BujoldE.Preventionofpreeclampsiabylow
molecularweightheparininadditiontoaspirin:ametaanalysis.UltrasoundObstetGynecol.2015Oct20.
[Medline].
80.VillarJ,AbdelAleemH,MerialdiM,etal.WorldHealthOrganizationrandomizedtrialofcalcium
supplementationamonglowcalciumintakepregnantwomen.AmJObstetGynecol.2006Mar.194(3):639
49.[Medline].
81.PostonL,BrileyAL,SeedPT,etal.VitaminCandvitaminEinpregnantwomenatriskforpreeclampsia
(VIPtrial):randomisedplacebocontrolledtrial.Lancet.2006Apr8.367(9517):114554.[Medline].
82.RumboldAR,CrowtherCA,HaslamRR,etal.VitaminsCandEandtherisksofpreeclampsiaand
perinatalcomplications.NEnglJMed.2006Apr27.354(17):1796806.[Medline].
83.VillarJ,PurwarM,MerialdiM,ZavaletaN,ThiNhuNgocN,AnthonyJ,etal.WorldHealthOrganisation
multicentrerandomisedtrialofsupplementationwithvitaminsCandEamongpregnantwomenathighrisk
http://emedicine.medscape.com/article/1476919overview
22/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
forpreeclampsiainpopulationsoflownutritionalstatusfromdevelopingcountries.BJOG.2009May.
116(6):7808.[Medline].
84.VadilloOrtegaF,PerichartPereraO,EspinoS,etal.EffectofsupplementationduringpregnancywithL
arginineandantioxidantvitaminsinmedicalfoodonpreeclampsiainhighriskpopulation:randomised
controlledtrial.BMJ.2011May19.342:d2901.[Medline].[FullText].
85.BrantsterAL,MyhreR,HaugenM,etal.Intakeofprobioticfoodandriskofpreeclampsiainprimiparous
women:thenorwegianmotherandchildcohortstudy.AmJEpidemiol.2011Oct1.174(7):80715.
[Medline].
86.FriedmanSA,LubarskySL,LimKH.MildGestationalHypertensionandPreeclampsia.InHypertensive
DisordersinWomen.SibaiBM,ed.HypertensiveDisordersinWomen.Philadelphia:W.B.Saunders
2001.923.
87.MillarJGB,CampbellSK,AlbanoJDM,etal.Earlypredictionofpreeclampsiabymeasurementof
kallikreinandcreatinineonarandomurinesample.BrJObstetGynaecol.1996.103:421426.
88.KyleP,RedmanC,deSwietM,MillarG.Acomparisonoftheinactiveurinarykallikrein:creatinineratioand
theangiotensinsensitivitytestforthepredictionofpreeclampsia[letterreply].BrJObstetGynaecol.1997.
104:969974.
89.BrooksM.Preeclampsialinkedtoautism,developmentaldelay.MedscapeMedicalNews.December12,
2014.[FullText].
90.WalkerCK,KrakowiakP,BakerA,HansenRL,OzonoffS,HertzPicciottoI.Preeclampsia,placental
insufficiency,andautismspectrumdisorderordevelopmentaldelay.JAMAPediatr.2015Feb.169(2):154
62.[Medline].
91.SullivanCA,MagannEF,PerryKGJr,etal.Therecurrenceriskofthesyndromeofhemolysis,elevated
liverenzymes,andlowplatelets(HELLP)insubsequentgestations.AmJObstetGynecol.1994Oct.
171(4):9403.[Medline].
92.SibaiBM,RamadanMK,ChariRS,etal.PregnanciescomplicatedbyHELLPsyndrome(hemolysis,
elevatedliverenzymes,andlowplatelets):subsequentpregnancyoutcomeandlongtermprognosis.AmJ
ObstetGynecol.1995Jan.172(1Pt1):1259.[Medline].
93.ChamesMC,HaddadB,BartonJR,etal.Subsequentpregnancyoutcomeinwomenwithahistoryof
HELLPsyndromeat<or=28weeksofgestation.AmJObstetGynecol.2003Jun.188(6):15047
discussion15078.[Medline].
94.SibaiBM,SarinogluC,MercerBM.Eclampsia.VII.Pregnancyoutcomeaftereclampsiaandlongterm
prognosis.AmJObstetGynecol.1992Jun.166(6Pt1):175761discussion17613.[Medline].
95.LopezLleraM,HernandezHortaJL.Pregnancyaftereclampsia.AmJObstetGynecol.1974May15.
119(2):1938.[Medline].
96.AdelusiB,OjengbedeOA.Reproductiveperformanceaftereclampsia.IntJGynaecolObstet.1986Jun.
24(3):1839.[Medline].
97.SibaiBM,MercerB,SarinogluC.Severepreeclampsiainthesecondtrimester:recurrenceriskandlong
termprognosis.AmJObstetGynecol.1991Nov.165(5Pt1):140812.[Medline].
98.vonDadelszenP,PayneB,LiJ,AnserminoJM,BroughtonPipkinF,CtAM,etal.Predictionofadverse
maternaloutcomesinpreeclampsia:developmentandvalidationofthefullPIERSmodel.Lancet.2011
Jan15.377(9761):21927.[Medline].
99.BlockAbrahamDM,TuranOM,DoyleLE,etal.Firsttrimesterriskfactorsforpreeclampsiadevelopment
inwomeninitiatingaspirinby16weeksofgestation.ObstetGynecol.2014Feb7.[Medline].
100.SibaiBM.Diagnosis,prevention,andmanagementofeclampsia.ObstetGynecol.2005Feb.105(2):402
10.[Medline].
101.GarciaJ.HigherBPinfirsttrimestermayincreasepreeclampsiarisk.MedscapeMedicalNews.February
10,2014.[FullText].
102.MostelloD,JenChangJ,AllenJ,LuehrL,ShykenJ,LeetT.Recurrentpreeclampsia:theeffectofweight
changebetweenpregnancies.ObstetGynecol.2010Sep.116(3):66772.[Medline].
103.SibaiBM.Magnesiumsulfateprophylaxisinpreeclampsia:Lessonslearnedfromrecenttrials.AmJObstet
Gynecol.2004Jun.190(6):15206.[Medline].
104.[Guideline]TuffnellDJ,ShennanAH,WaughJJ,WalkerJJ.RoyalCollegeofObstetriciansand
Gynaecologists.Themanagementofseverepreeclampsia/eclampsia.2006.[FullText].
105.OkusanyaBO,OladapoOT,LongQ,etal.Clinicalpharmacokineticpropertiesofmagnesiumsulphatein
womenwithpreeclampsiaandeclampsia:asystematicreview.BJOG.2015Nov24.[Medline].
106.NandiP,SiddiquiMF,LalaPK.Restraintoftrophoblastinvasionoftheuterusbydecorin:roleinpre
eclampsia.AmJReprodImmunol.2015Nov11.[Medline].
107.KandasamyY,WatsonD,RuddD.Biomarkerofearlyglomerularinjuryinpreeclampsia.Hypertens
Pregnancy.2015Nov.34(4):3919.[Medline].
MedscapeReference2011WebMD,LLC
http://emedicine.medscape.com/article/1476919overview
23/24
21/8/2016
Preeclampsia:PracticeEssentials,Overview,Pathophysiology
http://emedicine.medscape.com/article/1476919overview
24/24
Вам также может понравиться
- 14 Speaking Roleplays - OET-00003Документ83 страницы14 Speaking Roleplays - OET-00003jijo kurian mathew80% (5)
- Diagnosis & Management of Preeclampsia & Eclampsia PDFДокумент9 страницDiagnosis & Management of Preeclampsia & Eclampsia PDFBerri RahmadhoniОценок пока нет
- Orthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingОт EverandOrthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingОценок пока нет
- Case Study On Stroke PatientДокумент2 страницыCase Study On Stroke PatientsparrowcrowОценок пока нет
- First AidДокумент1 202 страницыFirst AidAnonymous QVovunM100% (17)
- Preeclampsia: Practice EssentialsДокумент17 страницPreeclampsia: Practice EssentialsjmlffelixОценок пока нет
- Preeclampsia and EclampsiaДокумент32 страницыPreeclampsia and EclampsiaJuan Carlos Camacho PastranaОценок пока нет
- Classification and Diagnosis of Hypertensive Disorders of PregnancyДокумент6 страницClassification and Diagnosis of Hypertensive Disorders of PregnancyZAHID AHMED KHANОценок пока нет
- 3 EclampsiaДокумент1 страница3 EclampsiaBolos, Kate Hampshire L.Оценок пока нет
- Practice Essentials: DefinitionsДокумент5 страницPractice Essentials: DefinitionsNovita sariОценок пока нет
- Practice Essentials: Essential Update: Preeclampsia Requiring Delivery Identified by Placental Growth Factor TestДокумент21 страницаPractice Essentials: Essential Update: Preeclampsia Requiring Delivery Identified by Placental Growth Factor TestFirstyaprilly WahyuningtyasОценок пока нет
- EklamsiaДокумент2 страницыEklamsiaPrayoga SiraitОценок пока нет
- Chronic Hypertension in Pregnancy ACOGДокумент25 страницChronic Hypertension in Pregnancy ACOGJulienni ArvelosОценок пока нет
- Preeclampsia and Eclampsia: Preeclampsia Is New-Onset Hypertension and Proteinuria After 20 WK Gestation. Eclampsia IsДокумент6 страницPreeclampsia and Eclampsia: Preeclampsia Is New-Onset Hypertension and Proteinuria After 20 WK Gestation. Eclampsia IsYusi RizkyОценок пока нет
- APEC Guidelines Preeclampsia: DefinitionsДокумент9 страницAPEC Guidelines Preeclampsia: DefinitionsPatrick BayuОценок пока нет
- Management of Severe Pre and EclampsiaДокумент14 страницManagement of Severe Pre and EclampsiaElton NyengoОценок пока нет
- Recent Trends in PIHДокумент21 страницаRecent Trends in PIHShashank VsОценок пока нет
- 194hypertens PregPCДокумент6 страниц194hypertens PregPCdr.putra888Оценок пока нет
- Pre EclampsiaДокумент27 страницPre EclampsiasynОценок пока нет
- Pre EclampsiaДокумент9 страницPre EclampsiaAnixa GutiérrezОценок пока нет
- Hypertensive Disorders of PregnancyДокумент70 страницHypertensive Disorders of PregnancyYibelu BazezewОценок пока нет
- H. Hypertensive Disorders in PregnancyДокумент50 страницH. Hypertensive Disorders in PregnancyRadha ChiombonОценок пока нет
- MK Hypertensive Disorders of Pregnancy (OBGY)Документ35 страницMK Hypertensive Disorders of Pregnancy (OBGY)Moses Jr Kazevu100% (1)
- APEC Guidelines Preeclampsia: DefinitionsДокумент9 страницAPEC Guidelines Preeclampsia: DefinitionsoscarОценок пока нет
- Pre Eclampsia Management 280720Документ9 страницPre Eclampsia Management 280720justisia padmiyatiОценок пока нет
- Hypertensive Disorder in Pregnancy: DR Melat AsratДокумент35 страницHypertensive Disorder in Pregnancy: DR Melat AsratKIYAОценок пока нет
- Preeclampsia: An Update: Acta Anaesthesiologica Belgica January 2014Документ14 страницPreeclampsia: An Update: Acta Anaesthesiologica Belgica January 2014Irma YunizaОценок пока нет
- Hypertensive in Pregnancy NewДокумент29 страницHypertensive in Pregnancy NewNuha AbdullahОценок пока нет
- Hypertensive Disorders Complicating Pregnancy: Beijing Obstetrics & Gynecology Hospital Hou LeiДокумент43 страницыHypertensive Disorders Complicating Pregnancy: Beijing Obstetrics & Gynecology Hospital Hou LeiAhmed TarigОценок пока нет
- Clincal Management of Hypertensive in PregnancyДокумент18 страницClincal Management of Hypertensive in PregnancyDr-Saja O. DmourОценок пока нет
- Gestational Hypertension and Preeclampsia ACOG Practice Bulletin, Number 222 1605448006Документ24 страницыGestational Hypertension and Preeclampsia ACOG Practice Bulletin, Number 222 1605448006xibalba.edОценок пока нет
- Hypertension in PregnancyДокумент18 страницHypertension in Pregnancyshubham kumarОценок пока нет
- HT KehamilanДокумент17 страницHT KehamilanAfraDewitaОценок пока нет
- Hypertensive Disorder in PregnancyДокумент56 страницHypertensive Disorder in PregnancyESCA GabrielОценок пока нет
- Mid EvalДокумент21 страницаMid EvalRaissaОценок пока нет
- PIH InvestigationsДокумент29 страницPIH InvestigationsPrasanna Kumaravel100% (1)
- Preeclampsia and Hypertensive Disease in PregnancyДокумент28 страницPreeclampsia and Hypertensive Disease in PregnancyBelajar PintarОценок пока нет
- Hypertension With Pregnanacy M AbusayedДокумент66 страницHypertension With Pregnanacy M AbusayedHadeer AlshekhОценок пока нет
- Hypertensive DisordersДокумент25 страницHypertensive DisordersCHRISTIAN SIDAYAОценок пока нет
- Air PIHДокумент43 страницыAir PIHSubhada GosaviОценок пока нет
- Pre Eclampsia ManagementДокумент8 страницPre Eclampsia Managementmayerling perdomoОценок пока нет
- Pregnancy InducedДокумент36 страницPregnancy InducedaьdulZдєЯiєQОценок пока нет
- 2019 Hypertensive Disorders of PregnancyДокумент16 страниц2019 Hypertensive Disorders of PregnancyMaria del Pilar Devis MoralesОценок пока нет
- Hypertensive Disorder in Pregnancy ObgynДокумент46 страницHypertensive Disorder in Pregnancy ObgynRachata PiriyamanunОценок пока нет
- Hypertensive Disorders in PregnancyДокумент7 страницHypertensive Disorders in PregnancyCaleb biiОценок пока нет
- Acog 2019 Preeclampsia PDFДокумент25 страницAcog 2019 Preeclampsia PDFJhoel Zuñiga LunaОценок пока нет
- EclampsiaДокумент56 страницEclampsiagalihtrimuninggarОценок пока нет
- NCP PrenatalДокумент20 страницNCP PrenatalemeyyОценок пока нет
- Hypertension ACOGДокумент3 страницыHypertension ACOGSupriatna TenОценок пока нет
- OB Hypertension in PregnancyДокумент5 страницOB Hypertension in PregnancyIsabel CastilloОценок пока нет
- Jurnal Hipertesi Dalam KehamilanДокумент6 страницJurnal Hipertesi Dalam KehamilanAnonymous FSI5VChDОценок пока нет
- PpqpsapdxzczxДокумент24 страницыPpqpsapdxzczxAriff RosliОценок пока нет
- EklamsiДокумент26 страницEklamsiRifaldiОценок пока нет
- Hypertension Disorder in PregnancyДокумент42 страницыHypertension Disorder in Pregnancyholly girlchy JastinОценок пока нет
- Gestational HypertensionДокумент13 страницGestational HypertensionHamza AhmedОценок пока нет
- Case StudyДокумент46 страницCase StudyChatwaz ManeerОценок пока нет
- Patho Ob Chronic Hypertension in PregnancyДокумент3 страницыPatho Ob Chronic Hypertension in PregnancyicОценок пока нет
- Hypertensive Disorder in Pregnancy-2Документ42 страницыHypertensive Disorder in Pregnancy-2CAC KK DABONGОценок пока нет
- PQCNC CMOP March 2014 WebinarДокумент23 страницыPQCNC CMOP March 2014 WebinarkcochranОценок пока нет
- Portal Hypertension, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandPortal Hypertension, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- High Blood Pressure: Natural Self-help for Hypertension, including 60 recipesОт EverandHigh Blood Pressure: Natural Self-help for Hypertension, including 60 recipesОценок пока нет
- Perioperative Cardiovascular Risk Assessment and Management For Noncardiac Surgery A ReviewДокумент12 страницPerioperative Cardiovascular Risk Assessment and Management For Noncardiac Surgery A Reviewyuyoide6857Оценок пока нет
- Basic Life Support PamphletДокумент26 страницBasic Life Support PamphletRex Loren de Leon0% (1)
- Sample Questions For HAAD Prometric and DHA For NursesДокумент46 страницSample Questions For HAAD Prometric and DHA For NursesJaezelle Ella Sabale100% (4)
- First Aid & CPR Manual: Brought To You byДокумент51 страницаFirst Aid & CPR Manual: Brought To You byAbbas AidinОценок пока нет
- Whitman Express 02 - 03 - 2011Документ24 страницыWhitman Express 02 - 03 - 2011Express EditorОценок пока нет
- Stroke Physician: Clinical Decision FormДокумент6 страницStroke Physician: Clinical Decision FormBaiq PritaОценок пока нет
- Effectiveness and Neural Mechanisms of Home-BasedДокумент5 страницEffectiveness and Neural Mechanisms of Home-BasedMuhammad ImronОценок пока нет
- Comparison of Dabigatran Versus Warfarin TreatmentДокумент7 страницComparison of Dabigatran Versus Warfarin TreatmentDivyesh AmarsedaОценок пока нет
- 1228 HFStroke Altered Neuro 2011Документ74 страницы1228 HFStroke Altered Neuro 2011Cyndy EnterlineОценок пока нет
- A Detailed Lesson Plan in Living ThingsДокумент23 страницыA Detailed Lesson Plan in Living ThingsclarisseОценок пока нет
- Ed Safety Checklist ToolkitДокумент20 страницEd Safety Checklist ToolkitRyeowook RyeОценок пока нет
- The Aspirin Story - From Willow To Wonder DrugДокумент10 страницThe Aspirin Story - From Willow To Wonder DrugbeirutjenОценок пока нет
- AJH - Winter 2015Документ52 страницыAJH - Winter 2015Sunand UnniОценок пока нет
- ESC Guidelines On The Diagnosis and Treatment of Peripheral Artery DiseasesДокумент56 страницESC Guidelines On The Diagnosis and Treatment of Peripheral Artery DiseasesJuan José Ruiz CastilloОценок пока нет
- Strokeaha 116 011309Документ7 страницStrokeaha 116 011309Anvesh JallapallyОценок пока нет
- Medical Surgical Nursing Nclex Questions Neuro2Документ12 страницMedical Surgical Nursing Nclex Questions Neuro2dee_day_8Оценок пока нет
- Stroke Assessment ToolsДокумент21 страницаStroke Assessment Toolsatti174Оценок пока нет
- Immunology Lippincotts Illustrated Reviews Paperback by Deborah LebmanДокумент22 страницыImmunology Lippincotts Illustrated Reviews Paperback by Deborah LebmanElanghovan ArumugamОценок пока нет
- Questionnares NeuroДокумент29 страницQuestionnares NeuroKirk Patrick MojicaОценок пока нет
- Year 3 Medicine Posting G-1, R-5b, August, 2021Документ23 страницыYear 3 Medicine Posting G-1, R-5b, August, 2021BABU BRAMANAPALLE JAGADEESHОценок пока нет
- Case Study 1Документ49 страницCase Study 1Yoan Eka Putra PalilingОценок пока нет
- Science4 - Q2 - Mod2 - Causes and Treatment of Diseases of The Major Organs - Version3Документ51 страницаScience4 - Q2 - Mod2 - Causes and Treatment of Diseases of The Major Organs - Version3Mean De Castro ArcenasОценок пока нет
- Siriraj Stroke ScoreДокумент3 страницыSiriraj Stroke ScoreHendy SetiawanОценок пока нет
- 2018 Book IntracerebralHemorrhageTherape PDFДокумент210 страниц2018 Book IntracerebralHemorrhageTherape PDFLinaSuarezОценок пока нет
- Stroke: Lynn Wittwer, MD, MPD Clark County EMSДокумент35 страницStroke: Lynn Wittwer, MD, MPD Clark County EMSvorez100% (1)
- Protocols and Pathways: Ischemic and Hemorrhagic StrokeДокумент38 страницProtocols and Pathways: Ischemic and Hemorrhagic StrokeDayana FiaОценок пока нет
- Quackery, The 20 Million Dollar DuckДокумент20 страницQuackery, The 20 Million Dollar DuckAustin Macauley Publishers Ltd.Оценок пока нет