Академический Документы
Профессиональный Документы
Культура Документы
DMD Verma2010md
Загружено:
Fajri MuhammadАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
DMD Verma2010md
Загружено:
Fajri MuhammadАвторское право:
Доступные форматы
Clinical
Pediatrics
http://cpj.sagepub.com/
Review of Duchenne Muscular Dystrophy (DMD) for the Pediatricians in the Community
Sumit Verma, Yaacov Anziska and Joan Cracco
CLIN PEDIATR 2010 49: 1011 originally published online 19 August 2010
DOI: 10.1177/0009922810378738
The online version of this article can be found at:
http://cpj.sagepub.com/content/49/11/1011
Published by:
http://www.sagepublications.com
Additional services and information for Clinical Pediatrics can be found at:
Email Alerts: http://cpj.sagepub.com/cgi/alerts
Subscriptions: http://cpj.sagepub.com/subscriptions
Reprints: http://www.sagepub.com/journalsReprints.nav
Permissions: http://www.sagepub.com/journalsPermissions.nav
Citations: http://cpj.sagepub.com/content/49/11/1011.refs.html
Downloaded from cpj.sagepub.com at UNIV CALGARY LIBRARY on April 7, 2011
Commentaries
Review of Duchenne Muscular
Dystrophy (DMD) for the
Pediatricians in the Community
Clinical Pediatrics
49(11) 10111017
The Author(s) 2010
Reprints and permission: http://www.
sagepub.com/journalsPermissions.nav
DOI: 10.1177/0009922810378738
http://clp.sagepub.com
Sumit Verma, MD1,Yaacov Anziska, MD1, and Joan Cracco, MD1
Introduction
Duchenne muscular dystrophy (DMD), an inherited
X-linked recessive disorder, is characterized by progressive symmetric muscle weakness and gait disturbance,
with onset in early childhood.1 DMD is the most common
muscular dystrophy in children, and incidence ranges
from 1 in 3600 to 4700 live male births.2 Early diagnosis (screening, confirmation, and genetic counseling),
treatment, and long-term follow-up of affected individuals in routine pediatric practice can be challenging and
are the focus of this review.
Natural History and
Clinical Features
Infant boys with DMD are often asymptomatic. Although
the clinical manifestations may be present by the end of
the first year, first symptoms are usually noted during
the toddler and preschool years (2-5 years). In spite of
increased awareness, there is an average delay of 2.5 years
from the onset of symptoms, and mean age of definitive
diagnosis is 5 years.3 Affected children usually present
with gait problems (waddling, toe walking, and lordotic
posture), calf hypertrophy, positive Gowers sign (difficulty arising from the floor, spreading their legs, and
using their hands to climb up their thighs to help them
to an upright position), and difficulty climbing stairs.
Pediatricians should be aware of the importance of having preschoolers get up from a sitting position on the floor,
walk, and run so as to detect early signs of muscle weakness. Motor status may appear to plateau between 3 and
6 years; deterioration begins between 6 to 8 years. Affected
children lose the ability to climb stairs and rise from the
floor and also develop Achilles tendon contractures. They
may be able to self-propel for some time and maintain
posture, but lordosis and scoliosis become obvious.
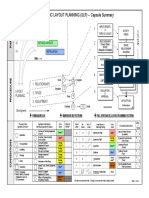
Between ages 9 and 12 years, the majority of DMD
patients become wheelchair bound (Figure 1). Upperlimb function is preserved until a later period. Decreased
pulmonary function as a result of respiratory muscle
weakness and chest deformity (kyphoscoliosis), along
with respiratory infections, predisposes to respiratory
failure. Cardiomyopathy and arrhythmia result in cardiac
failure. Cardiorespiratory complications appear during
the second decade and eventually lead to death.4
Screening With
Creatine Kinase (CK)
CK is a good screening test for muscle disease in clinical practice because levels rise in conditions with active
muscle fiber necrosis and injury.5 In DMD patients, CK
levels are usually very elevated and are between 5000 and
150000 IU/L (normal is less than 200 IU/L). Reversible
causes of elevated CK include drugs, trauma, crush injury,
recent bacterial/viral infections, and hypothyroidism.
However, the CK elevation in these circumstances rarely
approaches that of DMD. Newborn screening using CK
levels is not done routinely, and such screening has been
restricted to research settings because of limited data on
the impact of early diagnosis and initiation of (steroid)
therapy in DMD.6
Disease Confirmation and
Genetic Counseling
Those with DMD are deficient in dystrophin, an important muscle structural protein. The gene that codes for
dystrophin is large, with 79 exons.7 Approximately onethird of new cases in children are the result of new mutations.8 Dystrophin gene mutation testing should be done
in all suspected cases. Large deletions or duplications on
1
State University of New York (SUNY) Downstate Medical Center,
Brooklyn, New York, NY, USA
Corresponding Author:
Yaacov Anziska, Department of Neurology, 450 Clarkson Avenue,
Box 1213, Brooklyn, NY 11023
Email: Yaacov.Anziska@downstate.edu
Downloaded from cpj.sagepub.com at UNIV CALGARY LIBRARY on April 7, 2011
1012
Clinical Pediatrics 49(11)
Ability to ambulate
EARLY AMBULATORY
STAGE (II)
LATE AMBULATORY
STAGE (III)
Labored gait
Gowers sign
Waddling gait
Toe walking
Difficulty climbing stairs
Achilles contractures
Calf hypertrophy
PRESYMPTOM
STAGE (I)
Dev. delay
Family history
Elevated CK
EARLY NONAMBULATORY
STAGE (IV)
PLATEAUS
Able to self propel
IMPROVING
Lordotic posture
DECLINE
Scoliosis
LATE NONAMBULATORY
STAGE (V)
Limited upper limb function
Wheel chair bound
Scoliosis worsens
10
12
14
Age in years
Figure 1. Musculoskeletal course in Duchenne muscular dystrophy
Xp21 locus account for 72% of the mutations among all
cases; another 20% are point mutations (amino acid
substitution, premature stop mutation, splice mutation),
and 7% are small insertions or deletions; entire gene deletions are very rare.9,10 Disruption or preservation of
the reading frame by deletion mutations accounts for the
phenotype severity. The mRNA formed by joining the
ends of exons has to be in phase to maintain the correct
translational open reading frame for the ribosome. Deletions that shift the translational reading frame (frameshift
deletion) result in severely truncated dystrophin molecules. In-frame deletions lead to production of semifunctional protein, which can persist in small quantities,
and this results in Becker Muscular Dystrophy (BMD),
a milder, later onset muscular dystrophy.11 EMG has no
role in the diagnosis of DMD. Muscle biopsy can be considered in suspected children with negative family history and inconclusive or nonavailable genetic testing.12 In
DMD, dystrophin is absent in the muscle on immunostaining. Clinically asymptomatic siblings and the mother
of the index case should be tested for disease and carrier
state. Most carrier females are asymptomatic; however,
up to 20% of carrier females may develop some degree
of muscle weakness or cardiomyopathy.13 A carrier mother
has a 50% risk of having a boy with DMD and a 50%
risk of her daughters being carriers. In sporadic cases,
with no known family history and negative DNA deletion testing in the mother, germ line mosaicism cannot
be excluded. These families have a 7% to 10% recurrence risk. Before planning the next pregnancy, mothers with a carrier state or sporadic germline mutations
with previously affected male babies must have genetic
counseling and prenatal testing (Southern blot or polymerase chain reaction with chorionic villus sampling or
amniocentesis).14
Differential Diagnosis
The majority of childhood and adult onset inherited muscular disorders involve defects in the dystrophin axis
(Figure 2). The axis comprises an actindystrophin
dystroglycansarcoglycanlaminin complex that connects
Downloaded from cpj.sagepub.com at UNIV CALGARY LIBRARY on April 7, 2011
1013
Verma et al.
the sarcolemma and extracellular basal lamina and provides
the mechanical stabilization of the sarcolemma during
contraction and relaxation of muscle fibers.15 Common
differential diagnosis for DMD include BMD, limb girdle
muscular dystrophies (subtypes 2D, 2E, 2C, 2F, 1C and 2B),
Emery-Dreifuss disease, congenital muscular dystrophies
with and without brain involvement, congenital myopathies, motor neuron disease (spinal muscular atrophy,
type III), dermatomyositis, and acid maltase deficiency
(Table 1). Most neuromuscular diseases occurring at similar ages as DMD do not have the striking increase in
CK levels. In BMD, CK levels are generally lower but at
times may approach those of DMD. CK levels may also
be significantly elevated in the autosomal recessive
sarcoglyconopathies. Therefore, patients presenting with
DMD but having normal dystrophin levels should be evaluated for sarcoglycans on the muscle biopsy. Pediatricians
should also consider DMD in children with persistently
elevated liver enzymes (aspartate aminotransferase/alanine
aminotransferase) with negative workup for liver disease.16
Dystrophinopathies should be considered in children with
unexplained dilated cardiomyopathy. In summary, diagnosis of muscular dystrophy can be made by taking a complete history and pedigree, determining CK levels, and
carrying out a thorough neuromuscular exam.
Treatment of DMD:
Role of Glucocorticoids
Glucocorticoids are the first line therapy in the treatment of DMD. Steroids decrease inflammation, prevent
fibrosis, improve muscle regeneration, improve mitochondrial function, decrease oxidative radicals, and stop
abnormal signaling of pathways and apoptosis. The 2
most commonly used corticosteroids are prednisone and
deflazocort. Oral prednisone 0.75 mg/kg/d (max 80 mg/d)
improved muscle strength and function for 6 months to
2 years as shown in Cochrane meta-analysis.17 Daily
scheduling is more effective than alternate-day or
intermittent dosing. In those with intolerable side
effects, the glucocorticoid dose should be decreased by
25% each month. The minimum effective dose is 0.3
mg/kg/d for prednisone.18 Deflazocort 0.9 mg/kg/d is
another alternative with fewer side effects (less weight
gain and behavior problems) but has limited availability.19 Age of initiation for corticosteroids is debatable.
Many experts advocate beginning between 2 and 5 years,
when gait difficulty develops. Bone density measurement and up-to-date immunization is a prerequisite for
steroid initiation. Children on corticosteroids need calcium and vitamin D supplementation. Vertebral fractures are a well-known complication associated with
steroid use and should be aggressively treated with
bisphosphonate therapy.20 Glucocorticoids should be
continued even in nonambulatory patients to prevent
scoliosis and heart and lung failure. Parents should be
informed about the side effects and limitations of steroid
therapy and made aware that this form of therapy is not
curative.
Novel Therapies for DMD
Emerging treatment options for DMD include gene repair
or replacement. These therapies include the use of
recombinant adeno-associated viral vectors (rAAVs)
for dystrophin gene delivery.21 Studies in dystrophin doubleknock-out mice have shown that rAAV/ microdystrophin can be used to deliver dystrophin genes in adult
dystrophic mice. It is safe and effective for up to 2 years
with improvement in phenotype and 5-fold extension
in life span in these mice.22 Encouraging early data of
rAAV/microdystrophin delivery in dog models has been
reported.23 Another treatment modality is causing exon
skipping (avoiding deletions that disrupt the codon
reading frame) with antisense oligonucleotides.24 This
approach has shown promising results in both mice and
dog models of DMD and is currently under investigation in humans. A recent Phase 2b trial with overreading of premature stop codons in dystrophin transcription
did not achieve clinical significance (PTC Therapeutics). Other treatment strategies include upregulation
of compensatory proteins like utrophin, -dystrobrevin,
and 7integrin. Blocking the downstream effects of
muscle degeneration by the use of creatine, CoQ10,
MYO-029, IGF (insulin-like growth factor), glutamine,
arginine-like drugs, TNF (tumor necrosis factor)-
antagonists, and antifibrotics have been tried without
benefit.25
Comorbid Conditions and
Their Long-Term Management
DMD is a multisystem disease. Pediatricians caring for
these children need to coordinate with specialists in the
field of neurology, cardiology, pulmonology, orthopedics,
physical medicine, and rehabilitation. At each pediatric office visit, weight, height, and blood pressure (BP)
should be checked and plotted on age- and sex-appropriate anthropometric and BP percentile charts.26 Intellectual impairment with average intelligence quotient <1
standard deviation below the mean is common. Verbal
ability is more affected than performance skills.27 A
team approach with parents, school teachers, child psychologists, and speech and occupational therapists can
Downloaded from cpj.sagepub.com at UNIV CALGARY LIBRARY on April 7, 2011
1014
Clinical Pediatrics 49(11)
Table 1. Differential Diagnoses of Childhood-Onset Inherited Neuromuscular Disorders
Dystrophin Axis Level
Affected
Dystrophinopathies
Name of Disorder
Gene Location/Pattern
of Inheritance
Duchenne muscular Xp21/XR
dystrophy (DMD)
Becker muscular
dystrophy (BMD)
Xp21/XR
Sarcoglycanopathies
Limb girdle
muscular
dystrophy
(LGMD)
2D/C/E/F
Autosomal recessive:
2C13q12
2D17q21
2E4q12
2F5q33
Caveolin
LGMD1C
Autosomal dominant,
mutations in
caveolin-3
Laminin
Emery-Dreifuss
disease
Emerin xq28, x-linked:
laminin A/C 1q21.2,
autosomal dominant
or recessive
Extracellular
matrix defect:
congenital muscular
dystrophies
(CMDs) without
brain involvement
Merosin-positive
CMD
Merosin-negative
CMD
Dystroglyconopathies: Fukuyama-type
CMD with brain
CMD
involvement
Deletion or mutation
of LAMA2 (laminin)
gene on 6q22-q23
Autosomal recessive,
chromosome 9
Walker-Warburg
CMD
May be allelic with
Fukuyama
Clinical Features
CK Levels/Pathology
Onset 2 to 5 years,
CK level markedly elevated
calf hypertrophy,
(10-20), absent
cognitive dysfunction,
dystrophin in muscle on
wheel-chair bound
immunostaining
by 10 to 20 years;
cardiorespiratory
failure with death
in second to third
decade
Variable age of onset,
CK moderately elevated
benign course, wheel(5), reduced dystrophin
chair bound by end of
on muscle biopsy
second decade
immunostaining
Weakness first in hip
Very high CK (>10 normal),
and proximal leg
absent sarcoglycan
muscles, progressing
on staining of muscle
onto shoulder
biopsy, degeneration
and proximal arm
and regeneration of
weakness. No
muscle fibers, increased
cognitive impairment,
endomysial connective
rare cardiac disease
tissue
Absent caveolin-3 on
Western blot, muscle
biopsy degenerating and
regenerating fibers
Paravertebral rigidity;
Loss of emerin or laminin
tendon and joint
staining on muscle biopsy,
contractures,
mildly elevated CK, EKGincluding neck;
junctional escape rhythm,
conduction defects
absent P waves
and bradycardia;
humeroperoneal
weakness
Moderate severity,
CK level modestly
neonatal onset,
elevated, immunostaining
hypotonia, weakness,
for dystrophin helps
arthrogryposis, 90%
differentiate
ambulate by 4 years
Severe weakness,
MRI: extensive high-signalhypotonia, may have
intensity white matter
arthrogryposis,
respiratory failure
common
Moderate severity
CK levels, EMG, and muscle
(progressive)
biopsy finding similar
polymicrogyria,
to CMD without brain
lissencephaly,
involvement
neuronal heterotopia,
seizures
Moderate severity
CK levels, EMG, and muscle
polymicrogyria,
biopsy finding similar
lissencephaly,
to CMD without brain
neuronal heterotopia,
involvement
seizures
(continued)
Downloaded from cpj.sagepub.com at UNIV CALGARY LIBRARY on April 7, 2011
1015
Verma et al.
Table 1. (continued)
Dystrophin Axis Level
Affected
Congenital myopathy
Name of Disorder
Gene Location/Pattern
of Inheritance
Muscleeyebrain
disease
Links to 1p34-p32
Myotubular
myopathy
X-linked,Xq28, AD
11q22
Nemaline myopathy
NEB, ACTA1:
autosomal dominant
or recessive
SMN1 mutation,
phenotype depends
on number of SMN2
genes
Motor neuron disease Spinal muscular
atrophy (SMA)
Inflammatory
Dermatomyositis
Metabolic
Acid maltase
deficiency
AR (chromosome 17)
Clinical Features
CK Levels/Pathology
Developmental delay,
Ocular dysplasia, pyramidal
neuronal heterotopia,
tract dysplasia
hypomyelination,
optic nerve
hypoplasia
Ptosis, joint
Centrally placed large
contractures,
nuclei, immunochemical
micognathia
increased signal of
myofibers against desmin
Muscle wasting, rarely
Thread-like inclusions
cardiomyopathy
on Gomori trichrome
staining
Varies based on
Grouped muscle fiber
severity of disease,
atrophy, mainly type I
ranges from death
fibers
at 1 month from
respiratory weakness
to living >18 years
Proximal muscle
Vasculitis on biopsy,
weakness, helitrope
perifascicular, CK elevated
rash on upper eyelids,
Gottrons papules
Proximal muscle
CK not elevated, EMG is
weakness, childhood
characteristic
onset <5 years with
calf hypertrophy in
some cases
NOTE:AR = autosomal recessive.
address this problem. To monitor decline in ejection fraction and the onset of dilated cardiomyopathy, a baseline
echocardiogram should be performed at diagnosis or by
age 6; it should be repeated every 2 years up to the age
of 10 and annually thereafter.28 ACE (angiotensinconverting enzyme) inhibitors are the first line therapy
in DMD patients with cardiac failure to aid in cardiac
remodeling. -Blockers and diuretics are also used.
Pulmonary involvement from respiratory muscle weakness and chest wall deformity (kyphoscoliosis) needs
close monitoring.29 Annual forced vital capacity (FVC)
measurement at an age when the child can cooperate is
essential. During office visits, pulse oximetry and peak
flow should be documented. In the late nonambulatory
stage, end-tidal CO2 can be measured with a capnograph. Pulmonary insufficiency (FVC < 30% predicted,
SpO2 < 95%, end-tidal CO2 > 45 mm Hg) warrants volume recruitment and deep lung inflation (FVC < 40%
predicted) with noninvasive ventilation, including CPAP
(continuous positive airway pressure) or BiPAP (bilevel
positive airway pressure). This may begin with nighttime ventilation, with full-time ventilation if hypoventilation persists. Tracheostomy is required if noninvasive
ventilation cannot be done successfully or 3 extubation
failures are recorded. A cough assist device may be useful to prevent respiratory infections, which should be
treated aggressively. Orthopedic evaluation of the spine
and X rays every 6 months between 10 and 16 years
are advised. Although scoliosis incidence has decreased
with the use of glucocorticoids, spine stabilization surgery may be useful for curvature as little as 15 to 20 to
prolong ambulation. A physical medicine and rehabilitation specialist must be involved early in care to emphasize exercise and contracture prevention. Stretching and
positioning exercises at the hip, knee, and ankle should
be performed daily at home or at school. Aquatic therapy may also be helpful. Use of night ankle bracing has
been shown to prevent Achilles contractures. Children
on oral steroids also need screening for mood disorder
and reflux disease. Diet and swallowing evaluation is
Downloaded from cpj.sagepub.com at UNIV CALGARY LIBRARY on April 7, 2011
1016
Clinical Pediatrics 49(11)
Extra-cellular matrix
Defects in Extra-cellular matrix
2- chain/Merosin
Congenital Muscular Dystrophy (CMD)
Merosin Deficient CMD (MDC 1A)
Ullrich CMD
Bethlem myopathy
Laminin-2
Dystroglycan complex
Dystroglyconopathies
Spectrum: increasing order of
Caveolin
severity; brain/eye involvement
Sarcolgycan complex
Dysferlin
LGMD 2I
Extracellular
MDC 1C
Sarcolemma
MDC 1D
Cytoplasmic
Fukuyama CMD
Muscle-Eye-Brain (MEB)
CYS COOH
Sarcoglyconopathies
LGMD (Limb Girdle
Muscular Dystrophy)
LGMD 2D ()
LGMD 2E ()
LGMD 2C ()
LGMD 2F ()
Walker-Warburg (WWS)
NH2
Dystrophin
Dystrophinopathies
Duchenne Muscular Dystrophy (DMD)
Becker Muscular Dystrophy (BMD)
Figure 2. Dystrophin axis and its defects
helpful for those with rapid weight gain or weight loss
from swallowing difficulty. Gastrointestinal hypo motility secondary to smooth muscle involvement can be seen
as acute gastric distension, vomiting, abdominal pain,
and distension. The current management approach has
dramatically improved life expectancy, and patients
may now survive into their late 20s and 30s.30
Summary
DMD is a life-limiting disorder. Pediatricians can play
a vital role in screening, diagnosis, and management of
the affected children. Observing young children walk
and squat during well-child examination, CK level testing in suspicious cases, and referral to muscular dystrophy clinics, if available, can help decrease the delay in
diagnosis of DMD. Pediatricians can play an important
role in coordinating treatment and follow-up of affected
patients with a multidisciplinary team. Pediatricians can
also be a great resource in encouraging genetic testing
and counseling, prenatal diagnosis, and newborn screening for affected families.
Authors Note
SV conceived the idea and wrote the manuscript; YA and
JC reviewed the article and would act as guarantors.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest
with respect to the authorship and/or publication of this
article.
Funding
The author(s) received no financial support for the research
and/or authorship of this article.
References
1. Darras BT, Menache CC. Dystrophinopathies. In: Katriji B,
ed. Neuromuscular Disorders in Clinical Practice. 1st ed.
Newton, MA: Butterworth-Heinemann; 2002:1028-1048.
2. Dooley J, Gordon KE, Dodds L, MacSween J. Duchenne
muscular dystrophy: a 30-year population-based incidence
study. Clin Pediatr (Phila). 2010;49:177-179.
3. Ciafaloni E, Fox DJ, Pandya S, et al. Delayed diagnosis
in Duchenne muscular dystrophy: data from the Muscular
Downloaded from cpj.sagepub.com at UNIV CALGARY LIBRARY on April 7, 2011
1017
Verma et al.
Dystrophy Surveillance, Tracking, and Research Network
(MD STARnet). J Pediatr. 2009;155:380-385.
4. Bushby K, Finkel R, Birnkrant DJ, et al. Diagnosis and
management of Duchenne muscular dystrophy, part 1:
diagnosis, and pharmacological and psychosocial management. Lancet Neurol. 2010;9:77-93.
5. Brooke MH, Fenichel GM, Griggs RC, et al: Clinical
investigation in Duchenne dystrophy: 2. Determination of
the power of therapeutic trials based on the natural history. Muscle Nerve. 1983;6:91-103.
6. Kemper AR, Wake MA. Duchenne muscular dystrophy:
issues in expanding newborn screening. Curr Opin Pediatr.
2007;19:700-704.
7. Stockley TL, Akber S, Bulgin N, Ray PN. Strategy for
comprehensive molecular testing for Duchenne and Becker
muscular dystrophies. Genet Test. 2006;10:229-243.
8. Online Mendelian Inheritance in Man. Muscular dystrophy, Duchenne type; DMD. http://www.ncbi.nlm.nih.gov/
omim/310200. Accessed July 13, 2010.
9. Gillard EF, Chamberlain JS, Murphy EG, et al. Molecular
and phenotypic analysis of patients with deletions within
the deletion-rich region of the Duchenne muscular dystrophy (DMD) gene. Am J Hum Genet. 1989;45:507-520.
10. Bushby KM. Genetic and clinical correlations of Xp21
muscular dystrophy. J Inherit Metab Dis. 1992;15:551-564.
11. Monaco AP, Bertelson CJ, Liechti-Gallati S, et al. An
explanation for the phenotypic differences between patients
bearing partial deletions of the DMD locus. Genomics.
1988;2:90-95.
12. Darras BT, Jones HR. Diagnosis of pediatric neuromuscular disorders in the era of DNA analysis. Pediatr Neurol.
2000;23:289-300.
13. Hoogerwaard EM, Bakker E, Ippel PF, et al. Signs and
symptoms of Duchenne muscular dystrophy and Becker
muscular dystrophy among carriers in The Netherlands: a
cohort study. Lancet. 1999;353:2116-2119.
14. Abbs S. Prenatal diagnosis of Duchenne and Becker muscular dystrophy. Prenat Diagn. 1996;16:1187-1198.
15. Ozawa E, Yoshida M, Hagiwara Y, et al. Dystrophinassociated proteins in muscular dystrophy. Hum Mol Genet.
1990;4:11711-11716.
16. Morse RP, Rosman NP: Diagnosis of occult muscular dystrophy: importance of the chance finding of elevated
serum aminotransferase activities. J Pediatr. 1993;122:
254-256.
17. Manzur AY, Kuntzer T, Pike M, Swan A. Glucocorticoid corticosteroids for Duchenne muscular dystrophy.
Cochrane Database Syst Rev. 2008;(1):CD003725.
18. Moxley RT III, Ashwal S, Pandya S, et al. Practice parameter: corticosteroid treatment of Duchenne dystrophy: report
of the Quality Standards Subcommittee of the American
Academy of Neurology and the Practice Committee of the
Child Neurology Society. Neurology. 2005;64:13-20.
19. Biggar WD, Gingras M, Fehlings DL, Harris VA, Steele CA.
Deflazacort treatment of Duchenne muscular dystrophy.
J Pediatr. 2001;138:45-50.
20. Bothwell JE, Gordon KE, Dooley JM, MacSween J,
Cummings EA, Salisbury S. Vertebral fractures in boys
with Duchenne muscular dystrophy. Clin Pediatr (Phila).
2003;42:353-356.
21. Blankinship MJ, Gregorevic P, Chamberlain JS. Gene
therapy strategies for Duchenne muscular dystrophy utilizing recombinant adeno-associated virus vectors. Mol
Ther. 2006;13:241-249.
22. Arnett AL, Chamberlain JR, Chamberlain JS. Therapy for
neuromuscular disorders. Curr Opin Genet Dev. 2009;19:
290-297.
23. Gregorevic P, Schultz BR, Allen JM, et al. Evaluation
of vascular delivery methodologies to enhance rAAV6mediated gene transfer to canine striated musculature. Mol
Ther. 2009;17:1427-1433.
24. Yokota T, Duddy W, Partridge T. Optimizing exon skipping therapies for DMD. Acta Myol. 2007;26:179-184.
25. Nelson SF, Crosbie RH, Miceli MC, Spencer MJ. Emerging genetic therapies to treat Duchenne muscular dystrophy.
Curr Opin Neurol. 2009;22:532-538.
26. Rosner B, Prineas RJ, Loggie JM, Daniels SR. Blood pressure nomograms for children and adolescents, by height,
sex, and age, in the United States. J Pediatr. 1993;123:
871-886.
27. Cyrulnik SE, Fee RJ, De Vivo DC, Goldstein E,
Hinton VJ. Delayed developmental language milestones
in children with Duchennes muscular dystrophy. J Pediatr.
2007;150:474-478.
28. American Academy of Pediatrics Section on Cardiology
and Cardiac Surgery. Cardiovascular health supervision
for individuals affected by Duchenne or Becker muscular
dystrophy. Pediatrics. 2005;116:1569-1573.
29. Finder JD, Birnkrant D, Carl J, et al. Respiratory care of
the patient with Duchenne muscular dystrophy: an official
ATS consensus statement. Am J Respir Crit Care Med.
2004;170:456-465.
30. Bushby K, Finkel R, Birnkrant DJ, et al. Diagnosis and
management of Duchenne muscular dystrophy, part 2:
implementation of multidisciplinary care. Lancet Neurol.
2010;9:177-189.
Downloaded from cpj.sagepub.com at UNIV CALGARY LIBRARY on April 7, 2011
Вам также может понравиться
- CAP214 Web Devlopment PDFДокумент9 страницCAP214 Web Devlopment PDFAlisha AgarwalОценок пока нет
- BP TB A2PlusДокумент209 страницBP TB A2PlusTAMER KIRKAYA100% (1)
- Becker Muscular DystrophyДокумент9 страницBecker Muscular DystrophyManusama HasanОценок пока нет
- Dismorfología GeneralidadesДокумент6 страницDismorfología GeneralidadesLesley GalindoОценок пока нет
- Venous Thrombosis,: Atopic Dermatitis (AD)Документ5 страницVenous Thrombosis,: Atopic Dermatitis (AD)Kenneth DomirezОценок пока нет
- CaseДокумент7 страницCaseEka NurjannahОценок пока нет
- Oncogenic Osteomalacia - A Complex Dance of Factors: Thomas O. Carpenter, M.DДокумент4 страницыOncogenic Osteomalacia - A Complex Dance of Factors: Thomas O. Carpenter, M.DAsticha Erlianing SariОценок пока нет
- Cerebral PalsyДокумент10 страницCerebral PalsytipharethtОценок пока нет
- Congenitalmyopathies Andmusculardystrophies: Heather R. Gilbreath,, Diana Castro,, Susan T. IannacconeДокумент15 страницCongenitalmyopathies Andmusculardystrophies: Heather R. Gilbreath,, Diana Castro,, Susan T. IannacconeRizki Nandasari SulbahriОценок пока нет
- Mitochondrial MyopathiesДокумент20 страницMitochondrial MyopathiescristobalchsОценок пока нет
- Tumores CerebralesДокумент24 страницыTumores CerebralesRocio LedesmaОценок пока нет
- Myopathies: DMD, BMD, FSHДокумент15 страницMyopathies: DMD, BMD, FSHLeica Mae CalooyОценок пока нет
- Pathophysiology: Duchenne Muscular DystrophyДокумент10 страницPathophysiology: Duchenne Muscular DystrophyMukesh YadavОценок пока нет
- Patho Physio 51 To 100qДокумент67 страницPatho Physio 51 To 100qRaquel BencosmeОценок пока нет
- Muscular DystrophyДокумент4 страницыMuscular DystrophyEnachi OlgaОценок пока нет
- 60 Rathod EtalДокумент3 страницы60 Rathod EtaleditorijmrhsОценок пока нет
- Multiple Sclerosis Research Paper ConclusionДокумент9 страницMultiple Sclerosis Research Paper Conclusiongz91rnat100% (1)
- The Multidisciplinary Management of Duchenne Muscular DystrophyДокумент22 страницыThe Multidisciplinary Management of Duchenne Muscular DystrophyranihentynovitaОценок пока нет
- CPДокумент10 страницCPAnonymous vnv6QFОценок пока нет
- Achondroplasia Natural History Study (CLARITY)Документ7 страницAchondroplasia Natural History Study (CLARITY)jakelinelagoadvОценок пока нет
- Clinical-Diagnostic Features of Duchenne Muscular Dystrophy in ChildrenДокумент3 страницыClinical-Diagnostic Features of Duchenne Muscular Dystrophy in ChildrenFajri MuhammadОценок пока нет
- New Developments in Diagnosis, Treatment, and Management of Duchenne Muscular DystrophyДокумент14 страницNew Developments in Diagnosis, Treatment, and Management of Duchenne Muscular DystrophyRooh UllahОценок пока нет
- LGMDДокумент10 страницLGMDidno1008Оценок пока нет
- Myotonic Dystrophy 2017Документ8 страницMyotonic Dystrophy 2017Ully BatubaraОценок пока нет
- Congenital Myopathies: BackgroundДокумент34 страницыCongenital Myopathies: BackgroundHerry GunawanОценок пока нет
- Myelomeningocele - StatPearls - NCBI BookshelfДокумент13 страницMyelomeningocele - StatPearls - NCBI BookshelfEmmanuel Andrew Dela CruzОценок пока нет
- Special Needs PopulationДокумент13 страницSpecial Needs PopulationVina EmpialesОценок пока нет
- Mitochondrial DisorderДокумент3 страницыMitochondrial DisorderRoxie May Theresse AbagatnanОценок пока нет
- Severe Sickle Cell Disease-Pathophysiology and Therapy 2010Документ4 страницыSevere Sickle Cell Disease-Pathophysiology and Therapy 2010Shoua XiongОценок пока нет
- Agingwithmuscular Dystrophy: Pathophysiologyand ClinicalmanagementДокумент22 страницыAgingwithmuscular Dystrophy: Pathophysiologyand ClinicalmanagementDeborah SalinasОценок пока нет
- Chitty SkeletalДокумент34 страницыChitty SkeletalAhmed H. Ali ElbestaweyОценок пока нет
- Cushing Niños 2016Документ18 страницCushing Niños 2016sheyla alegreОценок пока нет
- Disruptions Result From Destruction of A NorДокумент6 страницDisruptions Result From Destruction of A NorAsri RachmawatiОценок пока нет
- Duchenne Muscular Dystrophy: Benedict J.A. Lankester, Michael R. Whitehouse, Martin F. GarganДокумент3 страницыDuchenne Muscular Dystrophy: Benedict J.A. Lankester, Michael R. Whitehouse, Martin F. GarganAntonio SimoncelliОценок пока нет
- Abstract BookДокумент90 страницAbstract BookPopescu RoxanaОценок пока нет
- Reyes - Unit 2 (Part 2)Документ4 страницыReyes - Unit 2 (Part 2)Justine Ericca ReyesОценок пока нет
- COMPLICAÇÕES LESÃO CEREBRAL 1-S2.0-S1047965114001065-MainДокумент8 страницCOMPLICAÇÕES LESÃO CEREBRAL 1-S2.0-S1047965114001065-MainYury FelicianoОценок пока нет
- Espina Bifida 2022Документ7 страницEspina Bifida 2022Edwin Fabian Paz UrbanoОценок пока нет
- Brain TumorsДокумент12 страницBrain Tumors36Kushal saNdHuОценок пока нет
- A Sonographic Approach To The Prenatal Diagnosis of Skeletal DysplasiasДокумент19 страницA Sonographic Approach To The Prenatal Diagnosis of Skeletal DysplasiasminhhaiОценок пока нет
- Cerebral Palsy: Comprehensive Review and Update: Annals of Saudi Medicine March 2006Документ11 страницCerebral Palsy: Comprehensive Review and Update: Annals of Saudi Medicine March 2006andreas kevinОценок пока нет
- Cerebral Palsy: Comprehensive Review and Update: Annals of Saudi Medicine March 2006Документ11 страницCerebral Palsy: Comprehensive Review and Update: Annals of Saudi Medicine March 2006andreas kevinОценок пока нет
- DYSTROPHYДокумент15 страницDYSTROPHYleeyan2wenty6Оценок пока нет
- Postsurgical Physical Therapy Management of.16OledzkaSuhr2017Документ8 страницPostsurgical Physical Therapy Management of.16OledzkaSuhr2017naeemullahОценок пока нет
- Cancer-5 (HSS 2305) - F2022Документ10 страницCancer-5 (HSS 2305) - F2022zahra.lalani14Оценок пока нет
- Review: Irina Bancos, Stefanie Hahner, Jeremy Tomlinson, Wiebke ArltДокумент11 страницReview: Irina Bancos, Stefanie Hahner, Jeremy Tomlinson, Wiebke Arltinterna MANADOОценок пока нет
- Multiple Sclerosis Thesis PDFДокумент6 страницMultiple Sclerosis Thesis PDFKarla Long100% (2)
- Willmann Mammalian Animal Models For Duchenne Muscular Dystrophy 2009Документ9 страницWillmann Mammalian Animal Models For Duchenne Muscular Dystrophy 2009vidyasagarsОценок пока нет
- Duchenne Muscular Dystrophy: June 2014Документ6 страницDuchenne Muscular Dystrophy: June 2014Beta Yunita PОценок пока нет
- Down's Syndrome and Spina BifidaДокумент23 страницыDown's Syndrome and Spina BifidaKajal KaliaОценок пока нет
- Preterm Infants: Effect Modification by Risk For Chronic Lung Disease Impact of Postnatal Systemic Corticosteroids On Mortality and Cerebral Palsy inДокумент9 страницPreterm Infants: Effect Modification by Risk For Chronic Lung Disease Impact of Postnatal Systemic Corticosteroids On Mortality and Cerebral Palsy inschizodhiОценок пока нет
- Duchenne Muscular Dystrophy (DMD)Документ9 страницDuchenne Muscular Dystrophy (DMD)rutwickОценок пока нет
- Research Paper Topics On Multiple SclerosisДокумент6 страницResearch Paper Topics On Multiple Sclerosisc9s9h7r7100% (1)
- Duchenne Muscular DystrophyДокумент2 страницыDuchenne Muscular DystrophyEmilia GunawanОценок пока нет
- Congenital Muscular Dystrophies and Congenital.8 PDFДокумент26 страницCongenital Muscular Dystrophies and Congenital.8 PDFlithium2203Оценок пока нет
- MedulloblastomaДокумент17 страницMedulloblastomabrown_chocolate87643Оценок пока нет
- Cervical Spondylotic Myelopathy: A Guide To Diagnosis and ManagementДокумент11 страницCervical Spondylotic Myelopathy: A Guide To Diagnosis and ManagementSurya PangeranОценок пока нет
- Pediatric Acute Transverse Myelitis Overview and Differential DiagnosisДокумент12 страницPediatric Acute Transverse Myelitis Overview and Differential Diagnosismmoraes0709Оценок пока нет
- Research Paper On Multiple Sclerosis FreeДокумент4 страницыResearch Paper On Multiple Sclerosis Freeutwvgkxgf100% (1)
- Neuroendocrine Tumors: Surgical Evaluation and ManagementОт EverandNeuroendocrine Tumors: Surgical Evaluation and ManagementJordan M. CloydОценок пока нет
- SLP Capsule SummaryДокумент1 страницаSLP Capsule SummaryFajri MuhammadОценок пока нет
- 5SLP - Day 5Документ3 страницы5SLP - Day 5Fajri MuhammadОценок пока нет
- Kematian Akibat Pembunuhan Di Kota Manado Yang Masuk Bagian Forensik RSUP Prof. Dr. R. D. Kandou Manado Tahun 2014Документ6 страницKematian Akibat Pembunuhan Di Kota Manado Yang Masuk Bagian Forensik RSUP Prof. Dr. R. D. Kandou Manado Tahun 2014Fajri MuhammadОценок пока нет
- Coal MineДокумент6 страницCoal MineFajri MuhammadОценок пока нет
- Duchenne Muscular Dystrophy: A Cerebellar Disorder?: Shana E. Cyrulnik, Veronica J. HintonДокумент11 страницDuchenne Muscular Dystrophy: A Cerebellar Disorder?: Shana E. Cyrulnik, Veronica J. HintonFajri MuhammadОценок пока нет
- Medicolegal Issues Leveled Against Forensic Physicians in Prescreeningof Detainees Gnfs 1000e103Документ3 страницыMedicolegal Issues Leveled Against Forensic Physicians in Prescreeningof Detainees Gnfs 1000e103Fajri MuhammadОценок пока нет
- Clinical-Diagnostic Features of Duchenne Muscular Dystrophy in ChildrenДокумент3 страницыClinical-Diagnostic Features of Duchenne Muscular Dystrophy in ChildrenFajri MuhammadОценок пока нет
- Family Guide PDFДокумент36 страницFamily Guide PDFFajri MuhammadОценок пока нет
- Manejo Anestesico de Paciente Con Sepsis Severa PDFДокумент10 страницManejo Anestesico de Paciente Con Sepsis Severa PDFFajri MuhammadОценок пока нет
- Duchenne Muscular Dystrophy: Current Cell Therapies: Therapeutic Advances in Neurological Disorders ReviewДокумент12 страницDuchenne Muscular Dystrophy: Current Cell Therapies: Therapeutic Advances in Neurological Disorders ReviewFajri MuhammadОценок пока нет
- Duchenne and Becker Muscular DystrophyДокумент7 страницDuchenne and Becker Muscular DystrophyFajri MuhammadОценок пока нет
- Tour Guiding and Escort Services - 301Документ95 страницTour Guiding and Escort Services - 301Zane 19531Оценок пока нет
- Tangazo La Kazi October 29, 2013 PDFДокумент32 страницыTangazo La Kazi October 29, 2013 PDFRashid BumarwaОценок пока нет
- CGP Module 1 FinalДокумент19 страницCGP Module 1 Finaljohn lexter emberadorОценок пока нет
- Kofax Cross Product Compatibility MatrixДокумент93 страницыKofax Cross Product Compatibility MatrixArsh RashaОценок пока нет
- Syllabus Biomekanika Kerja 2012 1Документ2 страницыSyllabus Biomekanika Kerja 2012 1Lukman HakimОценок пока нет
- Custom Belt Buckles: Custom Brass Belt Buckles - Hand Made in The USA - Lifetime Guarantee of QualityДокумент1 страницаCustom Belt Buckles: Custom Brass Belt Buckles - Hand Made in The USA - Lifetime Guarantee of QualityAndrew HunterОценок пока нет
- RESO NO. 4 - LANYARD FinalДокумент1 страницаRESO NO. 4 - LANYARD FinalsharonleefulloОценок пока нет
- Flabbergasted! - Core RulebookДокумент160 страницFlabbergasted! - Core RulebookRobert RichesonОценок пока нет
- Army Public School Recruitment 2017Документ9 страницArmy Public School Recruitment 2017Hiten BansalОценок пока нет
- Outline - Criminal Law - RamirezДокумент28 страницOutline - Criminal Law - RamirezgiannaОценок пока нет
- Conceptual Diagram of Ways To Increase SalesДокумент1 страницаConceptual Diagram of Ways To Increase SalesO6U Pharmacy RecordingsОценок пока нет
- China Daily 20181031Документ24 страницыChina Daily 20181031JackZhangОценок пока нет
- Information Security Policies & Procedures: Slide 4Документ33 страницыInformation Security Policies & Procedures: Slide 4jeypopОценок пока нет
- Contoh RPH Ts 25 Engish (Ppki)Документ1 страницаContoh RPH Ts 25 Engish (Ppki)muhariz78Оценок пока нет
- Morocco Top ScientistsДокумент358 страницMorocco Top Scientistsa.drioicheОценок пока нет
- Applied Thermodynamics - DraughtДокумент22 страницыApplied Thermodynamics - Draughtpiyush palОценок пока нет
- Claim &: Change ProposalДокумент45 страницClaim &: Change ProposalInaam Ullah MughalОценок пока нет
- Harbin Institute of TechnologyДокумент7 страницHarbin Institute of TechnologyWei LeeОценок пока нет
- FIREXДокумент2 страницыFIREXPausОценок пока нет
- Physiology PharmacologyДокумент126 страницPhysiology PharmacologyuneedlesОценок пока нет
- Bootstrap DatepickerДокумент31 страницаBootstrap DatepickerdandczdczОценок пока нет
- Speaking Test FeedbackДокумент12 страницSpeaking Test FeedbackKhong TrangОценок пока нет
- Athena 60 Installation Manual EN 2022.07.03Документ30 страницAthena 60 Installation Manual EN 2022.07.03joaquin.cadondonОценок пока нет
- Irregular Verbs-1Документ1 страницаIrregular Verbs-1timas2Оценок пока нет
- Present Continuous WorkshopДокумент5 страницPresent Continuous WorkshopPaula Camila Castelblanco (Jenni y Paula)Оценок пока нет
- Intro To EthicsДокумент4 страницыIntro To EthicsChris Jay RamosОценок пока нет
- Echeverria Motion For Proof of AuthorityДокумент13 страницEcheverria Motion For Proof of AuthorityIsabel SantamariaОценок пока нет
- Conrad John's ResumeДокумент1 страницаConrad John's ResumeTraining & OD HRODОценок пока нет