Академический Документы
Профессиональный Документы
Культура Документы
Effect of Methanol Leaf Extract of Nauclea Latifolia On Albino Mice Infected With Plasmodium Berghei
Загружено:
David IsuОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Effect of Methanol Leaf Extract of Nauclea Latifolia On Albino Mice Infected With Plasmodium Berghei
Загружено:
David IsuАвторское право:
Доступные форматы
Udobre et al. Afr. J. Pharmacol. Ther. 2013.
2(3): 83-87
African Journal of Pharmacology and Therapeutics Vol. 2 No. 3 Pages 83-87, 2013
Open Access to full text available at http://www.uonbi.ac.ke/journals/kesobap/
Research Article
Effect of Methanol Leaf Extract of Nauclea latifolia
on Albino Mice Infected with Plasmodium berghei
berghei
Aniefiok S. Udobre a,*, John A. Udobang b, Anwanabasi E. Udoh b, Victor U. Anah a,
Akaninyene E. Akpan a, and Goodnews E Charles a
a Department
b Department
of Pharmaceutical and Medicinal Chemistry, Faculty of Pharmacy, University of Uyo, Nigeria
of Pharmacology and Toxicology, Faculty of Pharmacy, University of Uyo, Nigeria
_____________
* Corresponding author: Department of Pharmaceutical and Medicinal Chemistry, Faculty of Pharmacy, University of
Uyo, P.M.B. 1017 Uyo, Nigeria; Tel: +234-802-7672367; Email: aniefiokudobre@yahoo.com
Background: In Nigeria the leaf decoction of Nauclea latifolia is taken to treat malaria and sexually transmitted
diseases. This study intends to generate a scientific data in support of the traditional use of the leaves in malaria
treatment.
Objective: To investigate the antiplasmodial effect of the methanol extract of the leaves of Nauclea latifolia on
chloroquine sensitive Plasmodium berghei berghei in experimentally infected albino mice.
Materials and Methods: The fresh leaves of Nauclea latifolia were collected, dried under shade, ground into powder
and macerated in methanol for 72 hrs. The dried extract was stored at -4 C for use. Thirty (30) mice were divided
into five groups (A,B,C,D,E). Group A received 10 ml/kg/day of distilled water (negative control). Groups B, C and D
received 370, 740 and 1110 mg/kg/day of the extract respectively. Group E received 1.2 mg/kg/day of artesunate
(positive control). This experiment was repeated for suppressive, prophylactic and curative tests.
Results: The extract produced considerable antiplasmodial activity in all the three tests evaluated compared to the
standard drug (artesunate). The extract reduced parasitaemia significantly (p<0.05) in a dose dependent manner.
Bioactive constituents of the plant could be responsible for the antiplasmodial activity
Conclusion: The result of the study supports the need for continued search for components of traditional medicine as
potential antimalarial agents.
Keywords: Malaria, Nauclea latifolia, mice, Plasmodium berghei berghei
Received: April, 2013
Published: October, 2013
1. Introduction
There are about 380,000 species of plants in our world
of which 260,000 belong to the higher plants; only 10%
of the higher plants have been studied to a significant
extent (Sandberg, 1976).
Nauclea latifolia is a multi-stemmed tree of up to 12 m
tall. It has an open canopy. Flowers are joined by their
calyxes. The fruit is a syncarp.
A KeSoBAP Publication 2013. All rights reserved.
The young leaf contains mild alkaloids with analgesic
property. The leaf preparations are taken as a
vermifuge and diuretic, for amenorrhoea, antimalarial
and sterility. It is hypotensive and hypoglycemic. In
Corte de Voire, it is taken for jaundice and blood in
urine, intestinal troubles and incipient hernia . In Ghana,
it is taken for fever and jaundice. In Democratic
Republic of Congo, leaf preparations are used externally
on oedemas. The Igala of Northern Nigeria use a boiling
water infusion of the leaf on swellings and skin rashes.
The Tenda of South East Senegal crush and cook the
ISSN 2303-9841
83
Udobre et al. Afr. J. Pharmacol. Ther. 2013. 2(3): 83-87
leaves to make plasters for wound dressings. The leaves
are deemed to have haemostatic property and are put
on circumcision wounds and on haemorrhoids and
hernias. The leaf extract is taken with chewed alligator
pepper to relief malaria dysentery and diarrhoea. The
leaf decoction is taken to treat sexually transmitted
diseases (Burkill, 1997).
In a study, the aqueous extracts of Nauclea latifolia
leaves (0.25-2.0 mg/ml) paralyzed T. columbrifomis
larva in a concentration-dependent manner (Asuzu and
Njoku, 1996). Ethanol stem extracts of Nauclea latifolia
decreased the level of parasitaemia in a dose-dependent
manner in mice experimentally infected with
Trypanosome brucei (Madubunyi, 1995). In another
study Nauclea latifolia extract was effective against
nociception, inflammation and pyrexia in rats and mice
thus partially justifying its use traditionally in the
treatment of uncomplicated malaria and painful
condition (Abbah et al, 2010).
Malaria is a mosquito-borne infectious disease of
humans and other animals caused by protozoa of the
genus Plasmodium (WHO, 2011). At present, 40% of the
world population lives in malaria endemic regions
(Snow, 2005). In 2001 about 700,000 lives of children
below the age of five were lost to malaria in Africa. The
disease is responsible for many medical complications
like low birth weights in infants and increase in sudden
abortion and stillbirth in pregnant women (Joda et al,
2005). Malaria is responsible for about 66% of all clinic
visits in Nigeria. It causes the death of an estimated
250,000 children under the age of five every year.
According to UNICEF findings, about 60% of deaths
especially those of children in the Specialist Hospital in
Bauchi, Nigeria are caused by malaria (UNICEF, 2009).
There is increase in the resistance of P. falciparum to
antimalarial drugs. This development has compromised
the efficacy of the available antimalarial drugs such as
chloroquine, Fansidar and even artemisinin. Records
have shown that there are no drugs that can offer
protection against malaria in all the regions of the world
(WHO, 2011).
2.2 Extraction and Phytochemical Analysis
1.0 kg of the powdered leaves was macerated with
methanol for 72 hr at room temperature (27+2 C) with
agitation 3 times daily to enhance the extraction
process. The extracts were filtered out using filter
paper (Whatman No. 1). The filtrates were evaporated
to dryness using rotary evaporator and water bath at 40
C. The concentrated extracts were then transferred to
air-tight containers, corked and preserved in the
refrigerator until required.
The
methanol
extracts
were
screened
for
phytochemicals using the standard methods of analysis
by Trease and Evans (2009) and Sofowora (2008).
2.3 Breeding of Animals
Ninety (90) male albino mice weighing between 14-20 g
were collected from the Animal House, Department of
Pharmacology, University of Uyo, Nigeria. The mice
were bred, food and water provided ad libitum. The
animal house was cleaned and disinfected regularly and
the sawdust changed three times a week.
2.4 Parasite Inoculation
A chloroquine sensitive strain of P. berghei berghei
(ANKA) was obtained from the National Institute of
Medical Research (NIMER), Lagos and was maintained
by sub passage in mice (Basir et al, 2012).
Each mouse used in the experiment was inoculated
intraperitoneally with 0.3 ml of infected blood
containing about 1x107 Plasmodium berghei parasitized
erythrocytes. The inoculum consisted of 5x107
Plasmodium berghei parasitized erythrocytes per ml.
This was prepared by determining both the percentage
parasitaemia and the erythrocytes count of the donor
mouse and diluting the blood with isotonic (normal)
saline in proportions indicated by both determinations:
red blood counts and percentage parasitaemia (Odetola,
1980).
2.5 Evaluation of Antiplasmodial Activity
The research on Nauclea latifolia reported herein
therefore is a contribution to the research efforts
towards identifying new potential treatments for
malaria. Previous studies on Nauclea latifolia led to the
development of a tablet dosage form from the water
extract of this plant. The tablet produced had good
mechanical properties like hardness but poor friability
and disintegration (Emeje et al, 2005).
2. Materials and Methods
2.1 Collection of Plant Materials
The fresh leaves of Nauclea latifola were collected in
September, 2011 from Ikot Ide village, Nto Edino Clan,
in Obot Akara Local Government Area of Akwa Ibom
State, Nigeria. The leaves were thoroughly washed with
clean water and dried under shade for seven days to
reduce moisture content and prevent enzyme action.
The dry leaves were pulverized using mortar and pestle
into powdered form and then preserved in a black airtight polythene bag and stored away from light to
prevent it from photolysis until required.
A KeSoBAP Publication 2013. All rights reserved.
Evaluation of Prophylactic (Repository) Activities of
Extracts
The repository activity of the extract was assessed using
the method described by Peters (1965).
Thirty (30) mice were randomly divided into five
groups of six mice each. Group A mice received 10
ml/kg of distilled water (negative control). Mice in
groups B, C and D mice received 430, 860 and 1290
mg/kg body weight of the extract, respectively. Group E
mice received 1.2 mg/kg of Artesunate (positive
control). The treatment was carried out for three
consecutive days (Do D2) between 8 am and 9 am,
using oral route of administration.
On the fourth day (D3), the mice were inoculated with
Plasmodium berghei. The parasitaemia level was
assessed by blood smears seventy-two hours later.
ISSN 2303-9841
84
Udobre et al. Afr. J. Pharmacol. Ther. 2013. 2(3): 83-87
Evaluation of Suppressive Activity of the Methanol
Extracts (4-Day Test)
The schizontocidal activity of the extract, distilled water
and artesunate against early P. berghei infection in mice
was evaluated using the method described by Knight
and Peters (1980). Another thirty (30) mice were
randomly divided into five groups of six mice each. On
the first day, (Do), the mice were infected with the
parasite and randomly divided into various groups.
These animals were given the extracts, distilled water
and artesunate orally using oral carnula.
were fasted overnight and were grouped in threes. In
the initial phase, four groups of the mice were
administered with various doses of the crude methanol
extract at the dose of 1.0, 2, 3.0 and 4.0g/kg body
weight orally. The treated mice were monitored for
24hours for mortality and general behaviour. After
24hours, the remaining six groups of the mice were
treated with the dose of 4.5, 4.6, 4.7, 4.8, 4.9 and 5.0g/kg
body weight based on the findings of the phase 1 and
were monitored for another 24hours (Lorke, 1983 and
Bruce, 1985).
2.7 Ethical approval
Group A mice received 10 ml/kg of distilled water
(negative control); mice in groups B, C and D received
430, 860 and 1290 mg/kg body weight of the extract,
respectively. Group E mice received 1.2 mg/kg of
Artesunate (positive control). Dosing was done for four
consecutive days (Do D3) between 8 am and 9 am. On
the fifth day, thick blood films were made from tail
blood. The films were then stained with Leishmans
stain to reveal parasitized erythrocytes out of 500 in a
random field of the microscope. The average percentage
suppressive effect of parasitaemia was calculated in
comparison with the controls.
Evaluation of Curative Activities of Methanol
Extracts (Ranes test)
Ranes test was used to evaluate the schizonticidal
activity of the extract and artesunate in established
infection. This was done as described by Ryley and
Peters (1970). P. berghei berghei was injected
intraperitoneally into another 30 mice on the first day
(Do). Seventy-two hours later (D3), the mice were
divided randomly into five groups of six mice each and
administered orally.
Group A mice received 10ml/kg of distilled water
(negative control); mice in groups B, C and D received
430, 860 and 1290 mg/kg body weight of the extract,
respectively. Group E mice received 1.2mg/kg of
Artesunate (positive control). Dosing was done for four
consecutive days (Do D3) between 8am and 9am. On
the fifth day, thick blood film was made from tail blood.
The film was then stained with Leishmans stain to
reveal parasitized erythrocytes out of 500 in a random
field of the microscope. The average percentage
suppression of parasitaemia was calculated in
comparison with the control.
2.6 Acute toxicity studies
Experimental Animals
Albino mice (30) of either sex weighing 16-23 g were
obtained from the animal house of biological Science
Department, University of Calabar and were housed in
cages under standard condition (12 hours light and 12
hours dark), humidity and temperature in the
University of Uyo animal house, Department of
Pharmacology and Toxicology. They were fed on
growers palletized feed and water.
Lethal dose Determination (LD50)
The up and down method (Bruce, 1985) was used to
determine the toxicity level of the extract. The mice
A KeSoBAP Publication 2013. All rights reserved.
Permission and approval for animal studies were
obtained from the College of Health sciences animal
ethics committee, University of Uyo.
3. Results
1.0 kg of the powdered leaves of Nauclea latifolia
yielded 74 g (7.4%) of the methanol dried extract.
Phytochemical screening revealed that the methanol
extract of the leaf of Nauclea latifolia contained
alkaloids, cardiac glycosides, terpenes, polyphenols,
saponins, tannins and flavonoids in high concentration,
carbohydrates in moderate concentration and
anthraquinones in low concentration. Cyanogenic
glycosides, phlobatanins, balsams and resins were
absent (Table 1).
Table 1: Phytochemical analysis of the methanol
extract of Nauclea latifolia leaves
Constituent
Concentration in Leaf
Alkaloids
+++
Cardiac glycosisides
+++
Terpenes
+++
Cyanogenic glycosides
Carbohydrates
Anthraquinones
++
+
Polyphenols
+++
Saponins
+++
Tannins
+++
Flavonids
+++
Phlobatanins
Balsams
Resins
Key : +++ = present in high concentration
++ = present in moderate concentration
+ = present in low concentration
- = absent
The prophylactic / repository activity of methanol leaf
extract of Nauclea Latifolia showed a dosedependent
reduction in parasitaemia in the extract treated groups
(Table 2). These reductions were statistically
significant relative to control (p < 0.05) but not as much
ISSN 2303-9841
85
Udobre et al. Afr. J. Pharmacol. Ther. 2013. 2(3): 83-87
as that exhibited by the standard drug artesunate at 1.2
mg/kg.
0.05) but not as much as that of the standard drug artesunate
The chemosuppressive activity of methanol leaf extract
of Nauclea latrofolia on parasitaemia increased as the
dose of the extract increased (Table 3). These effects
were statistically significant relative to control (p <
The mean survival time of mice receiving methanol leaf
extract of Nauclea latifolia increased as the dose of the
extract increased. The increases were statistically
significant (p < 0.05) compared to control but not as
much as that of the standard drug, artesunate (Table 4).
Table 2: Prophylactic/repository activity of methanol leaf extract of Nauclea Latifolia on Plasmodium berghei berghei
infection in mice
Treatments
Group
Doses (mg/kg)
Parasitaemia
% chemosuppression
Distilled water
(Negative control)
10 ml/kg
17.430.34
Extract
430
10.520.24
40.1
860
8.240.28
53.0
1290
6.210.44
64.4
1.2
3.010.06
85.2
Artesunate
Values are expressed as mean SEM significance relative to control *p<0.05, (n=6)
Table 3: Suppressive activity of methanol leaf extract of Nauclea latrofolia on Plasmodium bergehei berghei infection
in mice 4 (day test)
Treatments
Distilled water
(Negative control)
Extract
Artesunate
(Positive control)
Group
Doses
Parasitameia
% Chemosuppression
10 ml/kg
22.021.05
430
11.98 0.35
46.6
860
10.500.46
56.0
1290
7.20 0.90
66.7
1.2
3.700.65
83.5
Values are expressed as mean SEM significance relative to control * P<0.05, (n=6)
Table 4: Mean survival time of mice receiving methanol leaf extract of Nauclea latifolia during established P. berghei
berghei infection in mice
Treatments
Doses (mg/kg)
Mean survival time (days)
Normal saline
10 ml/ kg
10.36 0.37
430
16.63 0.74
860
17.70 0.35
1290
22.33 0.86
1.2
26.28 0.51
Extract
Artesunate (positive control)
Values are expressed as mean SEM. Significance relative to control: P < 0.05
The maximum dose producing 0% mortality was 4.0
and the minimum dose producing 100% mortality was
4.7g/kg body weight. The LD50 was calculated to be 4.3
g/kg. The physical signs of toxicity observed included
excitation, paw licking, increased respiratory rate,
decreased motor activity, gasping, coma and death.
A KeSoBAP Publication 2013. All rights reserved.
4 . Discussion
In traditional medicine the leaf of Nauclea latifolia has
been used in the treatment of malaria, skin rashes,
jaundice, fever, oedema, haemolysis, dysentery, hernias,
diarrhoea and sexually transmitted diseases (Burkill,
1977). The folkloric use of this plant prompted the need
ISSN 2303-9841
86
Udobre et al. Afr. J. Pharmacol. Ther. 2013. 2(3): 83-87
to evaluate the in vivo antiplasmodial activity of its
methanol leaf extract to provide some support for its
ethnobotanical uses.
Burkill HM. (1997). Medicinal Importance of Nauclea latifolia.
The useful plants of West Tropical Africa. Vol. 4, Families M-R,
Kew: Royal Botanic Gardens. pp. 614-621.
The extract reduced the parasitaemia in suppressive,
prophylactic and curative models in a dose-dependent
manner. These results may support the reported
activity of the plant against norciception, inflammation,
pyrexia which are symptoms uncomplicated malaria
(Abbah et al, 2010)
Christensen SB and Kharazmi A (2001). Antimalarial Natural
Products. Isolation, Characterization and Biological
Properties. In: Bioactive Compounds from natural sources. .
Isolation, Characterization and Biological Properties. Tringali
C., editor, London: Taylor and Francis, pp.379-432
Joda AE, Kola-Mustapha AT, Folawewo I, Fetto BE and Quadric
UF. (2004). A review of malaria in Nigeria. Nigerian J. Pharm.
37: 45-54.
Some secondary metabolites of plants such as alkaloids
and terpenes have been associated with antiplasmodial
activity (Ponarulselvam et al, 2012, Christensen and
Kharazmi, 2001). In this study alkaloids and terpenes
were present in abundance. Monoterpene indolealkaloids have been implicated in endoperoxidation by
generating reactive oxygen species which in turn may
alkylate with heme protein resulting in the death of the
parasite (Robert, 1998; Shigemori et al, 2003).
Madubunyi I. (1995). Antihepatoxic and Trypanocidal
Activities of the Ethanolic Extract of Nauclea latifolia Root
Bark. J. Herbs, Species and Med. Plants. 3: 23-35.
5. Conclusion
Odetola A, Basir O. (1980). Evaluation of Antimalarial
properties of some Nigerian Medicinal Plants. In: Safowora, A.,
Editor, 275-283.
The Annang people in Akwa Ibom State, Nigeria drink
the leaf decoction of Nauclea latifolia for prevention and
cure of malaria. The result of this study has provided
some scientific basis for its ethnomedical use and also
supports the need for continued search for the active
principle responsible for the antimalarial property for
possible characterization.
Lorke D (1983). A new Approach to Practical Acute Toxicity
Testing. Arch. Toxicol. 53:275-287
Peters W. (1965). Drug resistance in Plasmodia berghi, Exp.
Parasitol. 17: 80-89.
Roberts F, Robert C and Johnson (1998). Evidence for
Shikimate Pathway of apicomplexan parasites. Nature, 393:
219-220
Ryley JF, Peter W. (1970). The antimalarial activity of some
quinolone esters. Annals Trop. Med. Parasitol. 84: 209-222.
Conflict of Interest declaration
The authors declare no conflict of interest
Sandberg, F and Bruhm, J.G. (1976). Screening of Plants for
Biologically Active Substances. African Med. Plants, Ife:
Obafemi Awolowo University Press, p. 119.
References
Shigemori H, Kagata T, Ishiyama H, Morah F, Ohsaki A and
Kobayashi J. (2003). New Monoterpene Alkaloids from
Nauclea latifolia. Chem. Pharmaceut. Bulletin 51: 58-61.
Abbah J, Amos S, Chindo B, Nqazal I, Vonqtau HO, Adzu B,
Farida T, Odutola A, Wambebe C and Gamaniiel KS (2010).
Pharmacological Evidence Favouring the use Nauclea latifolia
in Malaria Ethnopharmacy: Effect against nociception,
inflammation and pyrexia in rats and mice. J. Ethnopharmacol.
127: 85-90.
Asuzu, IU and Njoku CJ. (1996). The Anthelmintic Effect of
Alstonia Boonei Bark and Nauclea latifolia Leaf Aqueous
Extracts on Triichostrongylus Infective Larvae. Fitoterapia.
67: 220-222.
Basir R, Fazalul Rahiman SS, Hashaballa K, Yam MF,
Jabbarzare M, Tie TH, Othman F, Moklas AM, Abdullahi WO
and Ahmad Z (2012). Plasmodium berghei ANKA infection In
ICR mice as a model of cerebral malaria. Iranian J. Parasitol. 7:
62-74.
Snow, R W, Guerna, A, Noor, A M, Mvint HY and Hay SI. (2005).
The global distribution of clinical episodes of Plasmodium
falciparum mature. Nature 434: 214-217.
Sofowora A. (2008). Medicinal Plant and Traditional Medicine
in Africa 3rd Ed. Spectrum Books Limited Ibadan, 182: 199208.
Trease A and Evans WC. (2009). Pharmacognosy.
Edition. Bailiere Tindall, London: 685-690.
New
UNICEF (2009). Partnering to Roll Back Malaria in Nigerias
Bauchi State
W.H.O. (2011). World Malaria Report.
Bruce RD (1985). An Up and Down Procedure of Acute
Toxicity Testing. Fund. Appl. Toxicol. 5:151-157
A KeSoBAP Publication 2013. All rights reserved.
ISSN 2303-9841
87
Вам также может понравиться
- Plant Disease Management Strategies for Sustainable Agriculture through Traditional and Modern ApproachesОт EverandPlant Disease Management Strategies for Sustainable Agriculture through Traditional and Modern ApproachesImran Ul HaqОценок пока нет
- Hepato Protective Assessment of Pawpaw Leaves, Neem, Lemon Grass and Acts On Plasmodium Berghei Parasitized Wistar RatsДокумент7 страницHepato Protective Assessment of Pawpaw Leaves, Neem, Lemon Grass and Acts On Plasmodium Berghei Parasitized Wistar RatsEditor IJTSRDОценок пока нет
- In Vivo Antimalarial Activities of Extracts From Amaranthus Spinosus L. andДокумент5 страницIn Vivo Antimalarial Activities of Extracts From Amaranthus Spinosus L. andfitriana ibrahimОценок пока нет
- Magifera PDFДокумент5 страницMagifera PDFNguyen Thi Ai LanОценок пока нет
- Antiplasmodial Activity of Ethanol Extract of Vernonia StudyДокумент6 страницAntiplasmodial Activity of Ethanol Extract of Vernonia StudyIOSRjournalОценок пока нет
- 1 PB PDFДокумент5 страниц1 PB PDFApt Fitri RosdianaОценок пока нет
- Preliminary Study of The Antibacterial and Analgesic Effect of The Leaf Extract of Pterocarpus Santalinoides L'Hér. Ex DCДокумент6 страницPreliminary Study of The Antibacterial and Analgesic Effect of The Leaf Extract of Pterocarpus Santalinoides L'Hér. Ex DCinventionjournalsОценок пока нет
- Antidepressant Potentials of Aqueous Extract of Voacanga Africana Stept. Ex Eliot (Apocynaceae) Stem BarkДокумент7 страницAntidepressant Potentials of Aqueous Extract of Voacanga Africana Stept. Ex Eliot (Apocynaceae) Stem BarkT. A OwolabiОценок пока нет
- Accepted Manuscript: Euphorbia HirtaДокумент20 страницAccepted Manuscript: Euphorbia HirtaLina PuspitaОценок пока нет
- Evaluation of The Antimalarial Activity of The Aqueous Leaf Extract of Gossypium Barbadense (Malvaeceae) in MiceДокумент3 страницыEvaluation of The Antimalarial Activity of The Aqueous Leaf Extract of Gossypium Barbadense (Malvaeceae) in MiceDrugs & Therapy StudiesОценок пока нет
- In Vitro Antimalarial and Cytotoxic Activities of Leaf Extracts of Vernonia Amygdalina (Del.)Документ6 страницIn Vitro Antimalarial and Cytotoxic Activities of Leaf Extracts of Vernonia Amygdalina (Del.)Haile KassaОценок пока нет
- Taleb 2015Документ5 страницTaleb 2015skkbd415Оценок пока нет
- A Comparative Study of The Antibacterial Activity of PiliostigmaДокумент8 страницA Comparative Study of The Antibacterial Activity of PiliostigmaglornumrОценок пока нет
- Antimalaria Activity of Ethanolic Extract of Tetrapleura Tetraptera Fruit PDFДокумент4 страницыAntimalaria Activity of Ethanolic Extract of Tetrapleura Tetraptera Fruit PDFvivitri.dewiОценок пока нет
- tmpCA8E TMPДокумент7 страницtmpCA8E TMPFrontiersОценок пока нет
- Anthelmintic Efficacy of The Aqueous Crude Extract of Euphorbia Hirta Linn in Nigerian DogsДокумент9 страницAnthelmintic Efficacy of The Aqueous Crude Extract of Euphorbia Hirta Linn in Nigerian DogsparavelloОценок пока нет
- Membrane Stabilizing EffectsДокумент5 страницMembrane Stabilizing Effectssulthana HОценок пока нет
- Cerbera Seeds - OpemДокумент6 страницCerbera Seeds - OpemMuhammad NaseerОценок пока нет
- Onyeto Et Al 5Документ8 страницOnyeto Et Al 5Collins onyetoОценок пока нет
- Salawu 2011Документ7 страницSalawu 2011Eti ApriyantiОценок пока нет
- Anti-Trypanosomal Activities and Effect Garcinia Kola Aqueous Seed Extract in Trypanosomiaisis Induced Wister RatДокумент10 страницAnti-Trypanosomal Activities and Effect Garcinia Kola Aqueous Seed Extract in Trypanosomiaisis Induced Wister RatInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- Sida Acuta Burm. F. A Medicinal Plant With Numerous PotenciesДокумент7 страницSida Acuta Burm. F. A Medicinal Plant With Numerous PotenciesyigalbyОценок пока нет
- Evaluation of The Antimicrobial, Antioxidant and Phytochemical Activities of Methanolic and Aqueous Extract of Cissus Aralioides Leaves On Some Selected Pathogenic MicroorganismsДокумент5 страницEvaluation of The Antimicrobial, Antioxidant and Phytochemical Activities of Methanolic and Aqueous Extract of Cissus Aralioides Leaves On Some Selected Pathogenic MicroorganismsIOSRjournalОценок пока нет
- Potensi Antimalaria Pepaya Carica Dan Vernonia Amygdalina Pada Tikus Terinfeksi Plasmodium BergheiДокумент7 страницPotensi Antimalaria Pepaya Carica Dan Vernonia Amygdalina Pada Tikus Terinfeksi Plasmodium Bergheibu ventiОценок пока нет
- N-Vivo Anti-Inflammatory and Anti-Pyretic Activities of Anilkara Zapota Leaves in Albino Istar RatsДокумент7 страницN-Vivo Anti-Inflammatory and Anti-Pyretic Activities of Anilkara Zapota Leaves in Albino Istar Ratszebchemistyahoo.comОценок пока нет
- Antiplasmodial and Analgesic Activities of Clausena Anisata: Asian Pacific Journal of Tropical MedicineДокумент6 страницAntiplasmodial and Analgesic Activities of Clausena Anisata: Asian Pacific Journal of Tropical MedicineNur Hayati IshОценок пока нет
- Immunomodulatory Activities of Methanol Extract of The Whole Aerial Part of Phyllantus Niruri L2014Journal of Pharmacognosy and PhytotherapyДокумент6 страницImmunomodulatory Activities of Methanol Extract of The Whole Aerial Part of Phyllantus Niruri L2014Journal of Pharmacognosy and PhytotherapyAkifОценок пока нет
- Olea EuropaeaДокумент7 страницOlea EuropaeaOlayiwola OmiyefaОценок пока нет
- Antimalarial Activity and Cytotoxicity Study of Ethanol Extract and Fraction From Alectryon Serratus LeavesДокумент4 страницыAntimalarial Activity and Cytotoxicity Study of Ethanol Extract and Fraction From Alectryon Serratus LeavesdinaОценок пока нет
- Psidium Guajava: Genotoxic and Antimicrobial Studies of The Leaves ofДокумент9 страницPsidium Guajava: Genotoxic and Antimicrobial Studies of The Leaves ofjabbamikeОценок пока нет
- Tougoma Et Al.Документ8 страницTougoma Et Al.Stanislas ZahouiОценок пока нет
- Sample Thesis 2009-04-16-160109 - 4672Документ4 страницыSample Thesis 2009-04-16-160109 - 4672Hajar IsahОценок пока нет
- Anti Inflammatory Ola Dejo 2021Документ7 страницAnti Inflammatory Ola Dejo 2021AdebayoОценок пока нет
- Anti-In Ammatory Effect of Ampelocissus Indica (L.) Planch (Chembravalli) in Wistar RatsДокумент19 страницAnti-In Ammatory Effect of Ampelocissus Indica (L.) Planch (Chembravalli) in Wistar RatsAnil DasОценок пока нет
- Anticonvulsant and Antioxidant Activity ofДокумент7 страницAnticonvulsant and Antioxidant Activity ofIkla CavalcanteОценок пока нет
- In Vitro Antibacterial Prospective of Crude Leaf Extracts of MeliДокумент6 страницIn Vitro Antibacterial Prospective of Crude Leaf Extracts of MeliMuhammad sherazОценок пока нет
- Antibacterial Activity of Azadirachita Indica and Psidium Guajava Extracts Against Three Bacterial Strains PDFДокумент6 страницAntibacterial Activity of Azadirachita Indica and Psidium Guajava Extracts Against Three Bacterial Strains PDFAlexander DeckerОценок пока нет
- Research Journal of Pharmaceutical, Biological and Chemical SciencesДокумент10 страницResearch Journal of Pharmaceutical, Biological and Chemical SciencesKehinde AlagbeОценок пока нет
- N Vitro Evaluation of Antimicrobial and Antioxidant Activity of Ragon 'S Blood Tree Racaena Cinnabari Alf.f. of Ocotra Sland EmenДокумент7 страницN Vitro Evaluation of Antimicrobial and Antioxidant Activity of Ragon 'S Blood Tree Racaena Cinnabari Alf.f. of Ocotra Sland EmensugianliОценок пока нет
- Analgesik OnДокумент7 страницAnalgesik OnChichi2406Оценок пока нет
- Balanites Aegyptiaca L. Drel. Moringa Oleifera Lam. On Salmonella TyphiДокумент4 страницыBalanites Aegyptiaca L. Drel. Moringa Oleifera Lam. On Salmonella Typhishishir badveОценок пока нет
- Eugenia Uniflora3Документ6 страницEugenia Uniflora3amensetОценок пока нет
- Anti InflammatoryДокумент7 страницAnti InflammatoryJeylan simboОценок пока нет
- In Vitro Studies of Antibacterial Activities of Nauclea Latifolia Root Extracts Using Micro Dilution Indicator TechniqueДокумент6 страницIn Vitro Studies of Antibacterial Activities of Nauclea Latifolia Root Extracts Using Micro Dilution Indicator TechniqueIOSRjournalОценок пока нет
- 167190-Article Text-430515-1-10-20180221Документ7 страниц167190-Article Text-430515-1-10-20180221RichardОценок пока нет
- Effects of The Aqueous Extract of Persea Americana Mill (Lauraceae) Leaves On The Rat Isolated Aorta: Evaluation of Vasomotility and Acute ToxicityДокумент9 страницEffects of The Aqueous Extract of Persea Americana Mill (Lauraceae) Leaves On The Rat Isolated Aorta: Evaluation of Vasomotility and Acute ToxicityOpenaccess Research paperОценок пока нет
- Antiplasmodial Potency of Ethanolic Leaf Extract of Infected Swiss Albino MiceДокумент8 страницAntiplasmodial Potency of Ethanolic Leaf Extract of Infected Swiss Albino MiceAl Bukhari SubulussalamОценок пока нет
- PR 14255Документ9 страницPR 14255Devi Dwi AmaliaОценок пока нет
- Tugas Kelompok 5 - Anti Diarrhea Psidium Guajava in VivoДокумент7 страницTugas Kelompok 5 - Anti Diarrhea Psidium Guajava in VivoNanda Felisha PutriОценок пока нет
- tmp31C6 TMPДокумент9 страницtmp31C6 TMPFrontiersОценок пока нет
- Phytochemical Screening and in Vitro Antimicrobial Activity of Typha Angustifolia Linn Leaves Extract Against Pathogenic Gram Negative Micro OrganismsДокумент4 страницыPhytochemical Screening and in Vitro Antimicrobial Activity of Typha Angustifolia Linn Leaves Extract Against Pathogenic Gram Negative Micro Organismsumeshbt720Оценок пока нет
- 2 51 1582878335 2ijmpsapr20202Документ10 страниц2 51 1582878335 2ijmpsapr20202TJPRC PublicationsОценок пока нет
- Journal Homepage: - : IntroductionДокумент11 страницJournal Homepage: - : IntroductionIJAR JOURNALОценок пока нет
- Phytochemical Screening and in Vitro AntimicrobialДокумент4 страницыPhytochemical Screening and in Vitro AntimicrobialArmel Géraldo HOUNDETONОценок пока нет
- Evaluation of The Prophylactic Activity of Ethanolic Extract of Ricinus Communis L. Against Plasmodium Berghei in MiceДокумент11 страницEvaluation of The Prophylactic Activity of Ethanolic Extract of Ricinus Communis L. Against Plasmodium Berghei in MiceUMYU Journal of Microbiology Research (UJMR)Оценок пока нет
- Immunocytotoxic Effect of Aqueous Leaf Extract of Cassia Occidentalis On Human Peripheral Blood Mononuclear Cells and NeutrophilsДокумент7 страницImmunocytotoxic Effect of Aqueous Leaf Extract of Cassia Occidentalis On Human Peripheral Blood Mononuclear Cells and NeutrophilsUMYU Journal of Microbiology Research (UJMR)Оценок пока нет
- Antipyretic Ectraction From PlantДокумент5 страницAntipyretic Ectraction From PlantTaufiksyaefulmalikОценок пока нет
- Ologundudu Article EditedДокумент17 страницOlogundudu Article Editedkolawole robert ogunmakinОценок пока нет
- 450-Article Text-535-1-10-20200330Документ13 страниц450-Article Text-535-1-10-20200330Nguyễn Sĩ Giáng VânОценок пока нет
- Antitumor Activity of An Ethanol Extract of Nigella Sativa SeedsДокумент6 страницAntitumor Activity of An Ethanol Extract of Nigella Sativa SeedsRaden WisnugrohoОценок пока нет
- Formulation of Water-Based Drilling Fluid Using Local MaterialsДокумент8 страницFormulation of Water-Based Drilling Fluid Using Local MaterialsDavid IsuОценок пока нет
- Issues in The Translation of An In-Text Igbo Expression in Achebe's There Was A CountryДокумент11 страницIssues in The Translation of An In-Text Igbo Expression in Achebe's There Was A CountryDavid IsuОценок пока нет
- Syllable Structure Types in UkwuaniДокумент7 страницSyllable Structure Types in UkwuaniDavid IsuОценок пока нет
- Periodization of Igbo Written Literature: Problems and ProspectsДокумент11 страницPeriodization of Igbo Written Literature: Problems and ProspectsDavid IsuОценок пока нет
- Presupposition and Entailment in Ammadarko's FacelessДокумент12 страницPresupposition and Entailment in Ammadarko's FacelessDavid IsuОценок пока нет
- Family Members: Means The Spouse of The Principal/undersigned The Grandparents, Parents, Siblings, Children, Nieces, Nephews, Grandchildren, AuntsДокумент2 страницыFamily Members: Means The Spouse of The Principal/undersigned The Grandparents, Parents, Siblings, Children, Nieces, Nephews, Grandchildren, AuntsDavid IsuОценок пока нет
- Visiting The UK To StudyДокумент1 страницаVisiting The UK To StudyDavid IsuОценок пока нет
- Application For Permission To Use The Hall of Mercy For Our SeminarДокумент1 страницаApplication For Permission To Use The Hall of Mercy For Our SeminarDavid IsuОценок пока нет
- 2 Corinthians - Hard Knocks, Unbreakable Faith (4 Session Study)Документ31 страница2 Corinthians - Hard Knocks, Unbreakable Faith (4 Session Study)David IsuОценок пока нет
- Standard Chartered Branches in NigeriaДокумент6 страницStandard Chartered Branches in NigeriaDavid IsuОценок пока нет
- ScriptДокумент1 страницаScriptDavid Isu75% (4)
- UploadscriptДокумент2 страницыUploadscriptDavid IsuОценок пока нет
- Custard ItДокумент16 страницCustard ItDavid Isu100% (2)
- Remita RRRДокумент1 страницаRemita RRRDavid IsuОценок пока нет
- Facebook Commerce Product Merchant Agreement: Last Updated: October 5, 2015Документ6 страницFacebook Commerce Product Merchant Agreement: Last Updated: October 5, 2015David IsuОценок пока нет
- Untitled 1Документ1 страницаUntitled 1David IsuОценок пока нет
- Remita RRRДокумент1 страницаRemita RRRDavid IsuОценок пока нет
- Federal University of Technology, P.M.B. 1526, Owerri, Imo StateДокумент24 страницыFederal University of Technology, P.M.B. 1526, Owerri, Imo StateDavid IsuОценок пока нет
- Application For The Post of Assistance Executive OfficerДокумент1 страницаApplication For The Post of Assistance Executive OfficerDavid IsuОценок пока нет
- Nuclie PDFДокумент34 страницыNuclie PDFlvnarsingaraoОценок пока нет
- (Intelligent Systems, Control and Automation_ Science and Engineering 72) B. S. Goh, W. J. Leong, K. L. Teo (Auth.), Honglei Xu, Xiangyu Wang (Eds.)-Optimization and Control Methods in Industrial EngiДокумент300 страниц(Intelligent Systems, Control and Automation_ Science and Engineering 72) B. S. Goh, W. J. Leong, K. L. Teo (Auth.), Honglei Xu, Xiangyu Wang (Eds.)-Optimization and Control Methods in Industrial EngiVu Duc TruongОценок пока нет
- Lessons Electric Circuits 1 PDFДокумент530 страницLessons Electric Circuits 1 PDFStefano SintoniОценок пока нет
- Polynomial Functions 1Документ19 страницPolynomial Functions 1Arafath Basheer100% (1)
- Victor Vroom PresentaciónДокумент7 страницVictor Vroom Presentaciónapi-3831590100% (1)
- $RKNVNODДокумент8 страниц$RKNVNODhoangleeicftОценок пока нет
- Class IfДокумент9 страницClass IfDavidRavenMoonОценок пока нет
- Guide SauvegardeДокумент688 страницGuide SauvegardemitrailleОценок пока нет
- Eju Maths Samp PaperДокумент29 страницEju Maths Samp PapersravanarajОценок пока нет
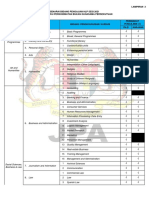
- Bidang Pengajian HLP 2021 - Perkhidmatan Bukan Gunasama PersekutuanДокумент4 страницыBidang Pengajian HLP 2021 - Perkhidmatan Bukan Gunasama PersekutuanMasnah Insyirah AnneskiОценок пока нет
- 169-Article Text-987-1-10-20220530Документ8 страниц169-Article Text-987-1-10-20220530Ika PratiwiОценок пока нет
- Schopenhauer S LebenДокумент345 страницSchopenhauer S LebenVeRa100% (1)
- Aavit 5 AДокумент113 страницAavit 5 AAnonymous ok5UankОценок пока нет
- Control System QBДокумент29 страницControl System QBPrabhavathi AadhiОценок пока нет
- My Black BookДокумент5 страницMy Black BookRiSHI KeSH GawaIОценок пока нет
- 4.NBT.1 Task 2Документ2 страницы4.NBT.1 Task 2Nur NadzirahОценок пока нет
- Memory Management and LatchingДокумент34 страницыMemory Management and Latchingrockerabc123Оценок пока нет
- My Dream Job Essay WritingДокумент3 страницыMy Dream Job Essay WritingAnne NgОценок пока нет
- Weather Phenomena MatrixДокумент4 страницыWeather Phenomena MatrixsetolazarОценок пока нет
- Samsung CL21K3W PDFДокумент4 страницыSamsung CL21K3W PDFNelson Muñoz BautistaОценок пока нет
- Carol Jones: Res Publica 8: 295-299, 2002Документ6 страницCarol Jones: Res Publica 8: 295-299, 2002Colton McKeeОценок пока нет
- Week 9-1 - H0 and H1 (Updated)Документ11 страницWeek 9-1 - H0 and H1 (Updated)Phan Hung SonОценок пока нет
- Literacy Lesson PlanДокумент5 страницLiteracy Lesson Planapi-437974951Оценок пока нет
- Sample TestДокумент2 страницыSample TestSarah Guimary PelarisОценок пока нет
- Ethical Issues in SupervisionДокумент10 страницEthical Issues in SupervisionBiona FranciscoОценок пока нет
- Wahs 1 PDFДокумент12 страницWahs 1 PDFKadek Deddy TaraОценок пока нет
- Vxworks Kernel Programmers Guide 6.8Документ802 страницыVxworks Kernel Programmers Guide 6.8hisahinОценок пока нет
- IBM Security Access Manager PDFДокумент708 страницIBM Security Access Manager PDFHenri ErasОценок пока нет
- SSRN Id3126098Документ3 страницыSSRN Id3126098Aditya kompalliОценок пока нет
- Alfred Nobel and The Nobel PrizesДокумент17 страницAlfred Nobel and The Nobel PrizesElizabethDarcyОценок пока нет
- The Bridesmaid: The addictive psychological thriller that everyone is talking aboutОт EverandThe Bridesmaid: The addictive psychological thriller that everyone is talking aboutРейтинг: 4 из 5 звезд4/5 (132)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDОт EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDРейтинг: 5 из 5 звезд5/5 (3)
- The Obesity Code: Unlocking the Secrets of Weight LossОт EverandThe Obesity Code: Unlocking the Secrets of Weight LossРейтинг: 4 из 5 звезд4/5 (6)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)От EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Рейтинг: 3 из 5 звезд3/5 (1)
- Briefly Perfectly Human: Making an Authentic Life by Getting Real About the EndОт EverandBriefly Perfectly Human: Making an Authentic Life by Getting Real About the EndОценок пока нет
- Neville Goddard Master Course to Manifest Your Desires Into Reality Using The Law of Attraction: Learn the Secret to Overcoming Your Current Problems and Limitations, Attaining Your Goals, and Achieving Health, Wealth, Happiness and Success!От EverandNeville Goddard Master Course to Manifest Your Desires Into Reality Using The Law of Attraction: Learn the Secret to Overcoming Your Current Problems and Limitations, Attaining Your Goals, and Achieving Health, Wealth, Happiness and Success!Рейтинг: 5 из 5 звезд5/5 (285)
- How to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipОт EverandHow to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipРейтинг: 4.5 из 5 звезд4.5/5 (1135)
- The Guilty Wife: A gripping addictive psychological suspense thriller with a twist you won’t see comingОт EverandThe Guilty Wife: A gripping addictive psychological suspense thriller with a twist you won’t see comingРейтинг: 4 из 5 звезд4/5 (72)
- Deep Sleep Hypnosis: Guided Meditation For Sleep & HealingОт EverandDeep Sleep Hypnosis: Guided Meditation For Sleep & HealingРейтинг: 4.5 из 5 звезд4.5/5 (104)
- The Energy Codes: The 7-Step System to Awaken Your Spirit, Heal Your Body, and Live Your Best LifeОт EverandThe Energy Codes: The 7-Step System to Awaken Your Spirit, Heal Your Body, and Live Your Best LifeРейтинг: 4.5 из 5 звезд4.5/5 (159)
- No Mud, No Lotus: The Art of Transforming SufferingОт EverandNo Mud, No Lotus: The Art of Transforming SufferingРейтинг: 5 из 5 звезд5/5 (175)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesОт EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesРейтинг: 4.5 из 5 звезд4.5/5 (1412)
- Follow your interests: This will make you feel better about yourself and what you can do.: inspiration and wisdom for achieving a fulfilling life.От EverandFollow your interests: This will make you feel better about yourself and what you can do.: inspiration and wisdom for achieving a fulfilling life.Оценок пока нет
- Prisoners of Geography: Ten Maps That Explain Everything About the WorldОт EverandPrisoners of Geography: Ten Maps That Explain Everything About the WorldРейтинг: 4.5 из 5 звезд4.5/5 (1145)
- Raising Grateful Kids in an Entitled World: How One Family Learned That Saying No Can Lead to Life's Biggest YesОт EverandRaising Grateful Kids in an Entitled World: How One Family Learned That Saying No Can Lead to Life's Biggest YesРейтинг: 4.5 из 5 звезд4.5/5 (108)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsОт EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsРейтинг: 4.5 из 5 звезд4.5/5 (170)
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyОт EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyРейтинг: 4.5 из 5 звезд4.5/5 (4)
- My Little Brother: The unputdownable, page-turning psychological thriller from Diane SaxonОт EverandMy Little Brother: The unputdownable, page-turning psychological thriller from Diane SaxonРейтинг: 4.5 из 5 звезд4.5/5 (39)
- His Needs, Her Needs: Building a Marriage That LastsОт EverandHis Needs, Her Needs: Building a Marriage That LastsРейтинг: 4.5 из 5 звезд4.5/5 (100)
- The Waitress: The gripping, edge-of-your-seat psychological thriller from the bestselling author of The BridesmaidОт EverandThe Waitress: The gripping, edge-of-your-seat psychological thriller from the bestselling author of The BridesmaidРейтинг: 4 из 5 звезд4/5 (65)
- Summary of The Art of Seduction by Robert GreeneОт EverandSummary of The Art of Seduction by Robert GreeneРейтинг: 4 из 5 звезд4/5 (46)
- Love Yourself, Heal Your Life Workbook (Insight Guide)От EverandLove Yourself, Heal Your Life Workbook (Insight Guide)Рейтинг: 5 из 5 звезд5/5 (40)
- The Secret Teachings Of All Ages: AN ENCYCLOPEDIC OUTLINE OF MASONIC, HERMETIC, QABBALISTIC AND ROSICRUCIAN SYMBOLICAL PHILOSOPHYОт EverandThe Secret Teachings Of All Ages: AN ENCYCLOPEDIC OUTLINE OF MASONIC, HERMETIC, QABBALISTIC AND ROSICRUCIAN SYMBOLICAL PHILOSOPHYРейтинг: 4.5 из 5 звезд4.5/5 (4)
- Summary of The 4-Hour Body: An Uncommon Guide to Rapid Fat-Loss, Incredible Sex, and Becoming Superhuman by Timothy FerrissОт EverandSummary of The 4-Hour Body: An Uncommon Guide to Rapid Fat-Loss, Incredible Sex, and Becoming Superhuman by Timothy FerrissРейтинг: 4.5 из 5 звезд4.5/5 (82)