Академический Документы
Профессиональный Документы
Культура Документы
Prevention and Management of Infants With Suspected or Proven Neonatal Sepsis - AAP 2013
Загружено:
Juan Pablo Dianderas MarengoАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Prevention and Management of Infants With Suspected or Proven Neonatal Sepsis - AAP 2013
Загружено:
Juan Pablo Dianderas MarengoАвторское право:
Доступные форматы
Prevention and Management of Infants With
Suspected or Proven Neonatal Sepsis
In 2010, the Centers for Disease Control and Prevention in collaboration with the American Academy of Family Physicians, American
Academy of Pediatrics (AAP), American College of Nurse-Midwives,
American College of Obstetricians and Gynecologists, and American
Society for Microbiology published revised group B streptococcal
(GBS) guidelines entitled Prevention of perinatal group B streptococcal disease: revised guidelines from CDC 2010 in the Morbidity
and Mortality Weekly Report (MMWR).1 The recommendations were
endorsed by all the collaborating organizations including AAP after
review by the Committee on Infectious Diseases (COID) and the Committee on Fetus and Newborn (COFN) and after AAP Board approval. In
the report, a revised algorithm for Secondary prevention of earlyonset group B streptococcal disease was included. This algorithm
represented the expert opinions of the technical working group (based
on current literature available at that time). In 2011, the COID and the
COFN published a policy statement in Pediatrics that was in agreement
with the 2010 GBS guidelines and included the same algorithm.2
In the spring of 2012, the COFN published a clinical report containing
management guidelines entitled Management of neonates with suspected or proven early-onset neonatal sepsis.3 The 2012 COFN document includes guidance on laboratory evaluations and treatment
duration, which were not addressed in the 2010 GBS prevention
guidelines. The algorithms at the end of the COFN report differed from
those in the 2010 guidelines published in the MMWR.1 The discordance
in the algorithms prompted questions by the pediatric community as
to which recommendations to follow.
AUTHORS: Michael T. Brady, MD,a and Richard A. Polin, MDb
a
Nationwide Childrens Hospital, Columbus, Ohio; and bCollege of
Physicians and Surgeons, Columbia University, New York, New
York
KEY WORDS
neonatal sepsis, group B streptococcus, prevention, treatment
ABBREVIATIONS
AAPAmerican Academy of Pediatrics
CBCcomplete blood cell
COFNCommittee on Fetus and Newborn
COIDCommittee on Infectious Diseases
GBSgroup B streptococcal
MMWRMorbidity and Mortality Weekly Report
Opinions expressed in these commentaries are those of the
authors and not necessarily those of the American Academy of
Pediatrics or its Committees.
www.pediatrics.org/cgi/doi/10.1542/peds.2013-1310
doi:10.1542/peds.2013-1310
Accepted for publication Apr 24, 2013
Address correspondence to Michael T. Brady, MD, 700 Childrens
Dr, AB 7048, Columbus, OH 43205. E-mail: michael.brady@
nationwidechildrens.org
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275).
Copyright 2013 by the American Academy of Pediatrics
FINANCIAL DISCLOSURE: The authors have indicated they have
no nancial relationships relevant to this article to disclose.
FUNDING: No external funding.
The purpose of this commentary is to clarify AAP policy. Discordant
algorithms for secondary prevention of GBS were published in 2
separate policy statements.2,3 This commentary includes the algorithm that has been approved as current AAP policy. Providing a single algorithm will avoid confusion and ensure that the guidelines
achieve their desired effects.
The COFN and the COID strongly support the recommendations made in
the 2010 prevention guidelines approved by the AAP and the other
collaborating organizations (secondary prevention of GBS algorithm
representing current AAP policy is attached in Fig 1). However, the COFN
notes that in some situations, other approaches might be considered
that differ from guidance provided in the 2010 prevention guidelines.
The following recommendations include the recommendations from the
2010 MMWR publication and those made by the COFN:
1. Neonates who have signs of sepsis should receive broad-spectrum
antimicrobial agents.
2. Healthy-appearing preterm and term infants born to women with
suspected chorioamnionitis should receive a blood culture at
166
BRADY and POLIN
Downloaded from by guest on February 12, 2016
COMMENTARY
the 2010 GBS prevention guidelines recommend a limited evaluation (blood culture and complete
blood cell [CBC] count with differential at birth or 6 to 12 hours
of age) and hospital observation
for 48 hours. The COFN recommends hospital observation for
48 hours in this circumstance
(without further testing or cultures). However, when close observation is not possible, the
COFN recommends a laboratory
evaluation.
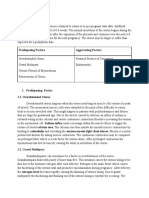
FIGURE 1
Secondary prevention of GBS disease.1,2 Algorithm for the prevention of early-onset GBS infection in
the newborn. (Adapted with permission from Centers for Disease Control and Prevention. Prevention
of perinatal group B streptococcal disease: prevention of perinatal group B streptococcal disease
from CDC, 2010. MMWR Recomm Rep. 2010;59 [RR-10]:132.) IV, intravenously. aFull diagnostic
evaluation includes a blood culture; CBC count, including white blood cell differential and platelet
counts; chest radiograph (if respiratory abnormalities are present); and lumbar puncture (if the
patient is stable enough to tolerate procedure and sepsis is suspected). bAntibiotic therapy should
be directed toward the most common causes of neonatal sepsis, including intravenous ampicillin for
GBS and coverage for other organisms (including Escherichia coli and other gram-negative
pathogens) and should take into account local antibiotic-resistance patterns. cConsultation with
obstetric providers is important in determining the level of clinical suspicion for chorioamnionitis.
Chorioamnionitis is diagnosed clinically, and some of the signs are nonspecic. dLimited evaluation
includes blood culture (at birth) and CBC count with differential and platelets (at birth and/or at
612 hours after birth). eGBS prophylaxis is indicated if 1 or more of the following is true: (1) mother
is GBS-positive late in gestation and is not undergoing cesarean delivery before labor onset with intact
amniotic membranes; (2) GBS status is unknown and there are 1 or more intrapartum risk factors,
including ,37 weeks gestation, rupture of membranes for $18 hours, or temperature of $100.4F
(38.0C); (3) GBS bacteriuria during current pregnancy; or (4) history of a previous infant with GBS
disease. fIf signs of sepsis develop, a full diagnostic evaluation should be performed, and antibiotic
therapy should be initiated. gIf $37 weeks gestation, observation may occur at home after 24 hours
if other discharge criteria have been met, there is ready access to medical care, and a person who
is able to comply fully with instructions for home observation will be present. If any of these
conditions is not met, the infant should be observed in the hospital for at least 48 hours and until
discharge criteria have been achieved. hSome experts recommend a CBC count with differential and
platelets at 6 to 12 hours of age.
birth, a complete blood count with
differential 1/2 C-reactive protein
at age 6 to 12 hours. These infants
should be treated with broadspectrum antimicrobial agents.
3. For well-appearing infants $37
weeks gestation whose mother did
not have suspected chorioamnionitis,
but who did have an indication for
intrapartum antibiotic prophylaxis
and did not receive at least 4 hours
of intrapartum penicillin, ampicillin
or cefazolin:
a. The 2010 GBS prevention guidelines and the 2012 COFN statement agree that infants who are
well appearing can be observed
without additional testing if duration of rupture of membranes
is ,18 hours. The COFN believes
that infants at 35 to 36 weeks
gestation can be treated similarly if the physical examination
is normal.
b. If duration of membrane rupture is
$18 hours and IAP is inadequate,
PEDIATRICS Volume 132, Number 1, July 2013
Downloaded from by guest on February 12, 2016
4. For well-appearing infants ,37
weeks gestation whose mother did
not have suspected chorioamnionitis,
but who did have an indication for
IAP and did not receive adequate
prophylaxis, the 2010 GBS prevention guidelines recommend a limited evaluation (blood culture and
CBC count) and hospital observation for 48 hours. The COFN also
recommends a limited evaluation,
but no blood culture unless antibiotics are started because of abnormal laboratory data.
5. The 2010 GBS prevention guidelines
do not address the duration of antibiotic therapy. The COFN makes
recommendations for the duration
of antimicrobial therapy based on
the results of laboratory testing.
Healthy-appearing infants without
evidence of bacterial infection should
receive broad-spectrum antimicrobial
agents for no more than 48 hours.
In small preterm infants, some
may continue antibiotics for up
to 72 hours while awaiting bacterial culture results.
Published data to support recommendations for prevention and management of newborn sepsis are limited.
However, success of the GBS prevention
guidelines provides evidence that reductions in early-onset GBS disease
have been possible by the development
of consensus guidelines with consistent
167
implementation.1 The COFNs 2012 recommendations complement the 2010
GBS prevention guidelines by providing
additional treatment information that is
not addressed in the 2010 prevention
guidelines. These should provide clinicians with guidance for optimal duration
of antimicrobial therapy and reduce
excess exposure to broad-spectrum antimicrobial therapy in healthy-appearing
uninfected infants who had empirical
antimicrobial therapy initiated.
2. Committee on Infectious Diseases; Committee on
Fetus and Newborn, Baker CJ, Byington CL, Polin
RA. Policy statementRecommendations for
prevention of perinatal group B streptococcal
(GBS) disease. Pediatrics. 2011;128(3):611616
3. Polin RA; Committee on Fetus and Newborn. Management of neonates with
suspected or proven early-onset neonatal sepsis. Pediatrics. 2012;129(5):1006
1015
REFERENCES
1. Centers for Disease Control and Prevention.
Prevention of perinatal group B streptococcal diseaserevised guidelines from CDC,
2010. MMWR Recomm Rep. 2010;59(RR-10):
136
CANINE LICKS OF LOVE SHAPE HUMAN BIOME: Theres nothing like coming home
at the end of the day to nd mans best friend there to greet you. Dogs provide
unconditional love and affection, and it appears that their welcoming kisses
may do more than just strengthen the relationship between human and animal.
As reported on an NPR health news blog (Shots: April 18, 2013), a recent study
indicates that dog owners share a common bond the bacteria on their skin.
In their investigation of 159 individuals living in 17 households, researchers
found that dog owners living in separate households share a common bacterial linkage through their canine companions. Actinobacteria and Betaproteobacteria found in soil and on dogs tongues, respectively, were present on
dog owners skin in greater amounts than in those who did not own dogs.
Unsurprisingly, the type and amount of bacteria on an owners skin were most
closely related to that of their own pooch. This effect was only observed in the
adult dog owner population (18-59 years of age); the presence of other
household pets, including cats, had no signicant effect on owner microbiota.
While our canine furry friends may shape our skin environment, additional
research is necessary to better dene how these bacteria inuence our health.
Noted by Leah H. Carr, BS, MS-IV
168
BRADY and POLIN
Downloaded from by guest on February 12, 2016
Prevention and Management of Infants With Suspected or Proven Neonatal
Sepsis
Michael T. Brady and Richard A. Polin
Pediatrics 2013;132;166; originally published online June 10, 2013;
DOI: 10.1542/peds.2013-1310
Updated Information &
Services
including high resolution figures, can be found at:
/content/132/1/166.full.html
References
This article cites 3 articles, 2 of which can be accessed free
at:
/content/132/1/166.full.html#ref-list-1
Citations
This article has been cited by 6 HighWire-hosted articles:
/content/132/1/166.full.html#related-urls
Post-Publication
Peer Reviews (P3Rs)
2 P3Rs have been posted to this article /cgi/eletters/132/1/166
Subspecialty Collections
This article, along with others on similar topics, appears in
the following collection(s):
Fetus/Newborn Infant
/cgi/collection/fetus:newborn_infant_sub
Neonatology
/cgi/collection/neonatology_sub
Permissions & Licensing
Information about reproducing this article in parts (figures,
tables) or in its entirety can be found online at:
/site/misc/Permissions.xhtml
Reprints
Information about ordering reprints can be found online:
/site/misc/reprints.xhtml
PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly
publication, it has been published continuously since 1948. PEDIATRICS is owned, published,
and trademarked by the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk
Grove Village, Illinois, 60007. Copyright 2013 by the American Academy of Pediatrics. All
rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275.
Downloaded from by guest on February 12, 2016
Prevention and Management of Infants With Suspected or Proven Neonatal
Sepsis
Michael T. Brady and Richard A. Polin
Pediatrics 2013;132;166; originally published online June 10, 2013;
DOI: 10.1542/peds.2013-1310
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
/content/132/1/166.full.html
PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly
publication, it has been published continuously since 1948. PEDIATRICS is owned,
published, and trademarked by the American Academy of Pediatrics, 141 Northwest Point
Boulevard, Elk Grove Village, Illinois, 60007. Copyright 2013 by the American Academy
of Pediatrics. All rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275.
Downloaded from by guest on February 12, 2016
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- SCI - Learning Packet - Biology Week 5Документ13 страницSCI - Learning Packet - Biology Week 5Pal, Julia HanneОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Original Prevention of Sickness PamphletДокумент88 страницThe Original Prevention of Sickness PamphletGeorge Singleton100% (4)
- Womens Fitness UK 08.2021Документ92 страницыWomens Fitness UK 08.2021Diseño ArtisОценок пока нет
- Fdar Samples PresentationДокумент29 страницFdar Samples PresentationKewkew Azilear92% (37)
- Diabetic Ketoacidosis Case StudyДокумент5 страницDiabetic Ketoacidosis Case Studyjc_albano29100% (7)
- Family DeclarationДокумент5 страницFamily DeclarationVanlal MuanpuiaОценок пока нет
- Guided Home Module: Psychosocial Support Activities For Elementary Learners Cordillera Administrative Region (CAR)Документ36 страницGuided Home Module: Psychosocial Support Activities For Elementary Learners Cordillera Administrative Region (CAR)Jennyhyn cruz75% (4)
- Essential Care of Newborn at BirthДокумент32 страницыEssential Care of Newborn at Birthastha singh100% (1)
- Reaching OutДокумент353 страницыReaching OutDebayan NandaОценок пока нет
- Bacterial Vaginosis Treatment - UpToDateДокумент12 страницBacterial Vaginosis Treatment - UpToDateAlex Esteban Espinoza CevallosОценок пока нет
- Lab 7 HIV Detection Using ELISAДокумент24 страницыLab 7 HIV Detection Using ELISAAhmed AbedoОценок пока нет
- Queenie Rose Domingo - Drug Study (Silver Sulfadiazine)Документ1 страницаQueenie Rose Domingo - Drug Study (Silver Sulfadiazine)Sheryl Ann Barit PedinesОценок пока нет
- Assessment of Knowledge Attitude and Perception of Dental Students Towards Obesity in Kanpur CityДокумент6 страницAssessment of Knowledge Attitude and Perception of Dental Students Towards Obesity in Kanpur CityAdvanced Research PublicationsОценок пока нет
- Chapter 10Документ10 страницChapter 10The makas AbababaОценок пока нет
- Epoch Elder Care Provides High Quality Assisted Living HomesДокумент17 страницEpoch Elder Care Provides High Quality Assisted Living HomesMahesh MahtoliaОценок пока нет
- Product Brochure 2023-2024 en LRДокумент23 страницыProduct Brochure 2023-2024 en LRaf8009035Оценок пока нет
- 4.ethico - Legal in Older AdultДокумент46 страниц4.ethico - Legal in Older AdultShazich Keith LacbayОценок пока нет
- Detection of NoncomplianceДокумент12 страницDetection of Noncompliancesomayya waliОценок пока нет
- Difhtheria in ChildrenДокумент9 страницDifhtheria in ChildrenFahmi IdrisОценок пока нет
- Ethical Considerations in Transcultural Nursing.Документ1 страницаEthical Considerations in Transcultural Nursing.Maddy LaraОценок пока нет
- EO-GA-32 Continued Response To COVID-19 IMAGE 10-07-2020Документ7 страницEO-GA-32 Continued Response To COVID-19 IMAGE 10-07-2020Jakob RodriguezОценок пока нет
- Format Nutritional StatusДокумент43 страницыFormat Nutritional StatusDirkie Meteoro Rufin83% (6)
- Discharge PlanДокумент2 страницыDischarge Plan2G Balatayo Joshua LeoОценок пока нет
- Cupuncture: Victor S. SierpinaДокумент6 страницCupuncture: Victor S. SierpinaSgantzos MarkosОценок пока нет
- Fecal Occult BloodДокумент9 страницFecal Occult BloodRipu DamanОценок пока нет
- FNCPДокумент5 страницFNCPGwen De CastroОценок пока нет
- Startup StoryДокумент1 страницаStartup StorybmeghabОценок пока нет
- List of Private Hospitals and Diagnostic Centers Approved by INSAДокумент16 страницList of Private Hospitals and Diagnostic Centers Approved by INSAvijay sainiОценок пока нет
- FoodДокумент3 страницыFoodDiego EscobarОценок пока нет
- What Is Subinvolution?Документ5 страницWhat Is Subinvolution?Xierl BarreraОценок пока нет