Академический Документы
Профессиональный Документы
Культура Документы
tmp2CFB TMP
Загружено:
FrontiersОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
tmp2CFB TMP
Загружено:
FrontiersАвторское право:
Доступные форматы
SHOCK, Vol. 33, No. 3, pp.
258Y262, 2010
GENDER DIFFERENCES IN INFLAMMATORY MARKERS IN CHILDREN
Georges J. A. Casimir,* Sandra Mulier,* Laurence Hanssens,* Kathya Zylberberg,*
and Jean Duchateau
*Department of Pulmonology and Allergology, University Childrens Hospital Queen Fabiola, and
Laboratory of Paediatrics, Free University of Brussels (ULB), Brussels, Belgium
Received 3 May 2009; first review completed 20 May 2009; accepted in final form 10 Jun 2009
ABSTRACTNo clear explanation exists to understand how sex hormones and/or chromosomes affect the immune
system. In vitro studies of human lymphoid cells also show sex differences in immune function. To evaluate these
differences in frequent pediatric emergencies, we analyze the expression of inflammatory markers (C-reactive protein,
erythrocyte sedimentation rate, and neutrophil count) underlying inflammatory processes in children: 482 children
(241 girls and 241 boys) hospitalized for pneumonia (n = 384), pyelonephritis (n = 39), or bronchiolitis (n = 59) matched for
age and sex. All patients were younger than 10 years. A control population of 97 children (50 girls and 47 boys) admitted
for day surgery (tonsillectomy, circumcision, or strabismus) was included. We observed highly significant differences
between girls and boys: median C-reactive protein concentration of 5.45 mg/dL (range, 0.2Y36.0 mg/dL) for girls and
2.6 mg/dL (range, 0.3Y37.3 mg/dL) for boys (P G 0.0001), and median erythrocyte sedimentation rate of 39.5 mm/h
(range, 2Y104 mm/h) for girls and 24 mm/h (range, 4Y140 mm/h) for boys (P G 0.005). Neutrophil counts were also
significantly different: a median of 8,796 cells/2L (range, 328Y27,645 cells/2L) for girls and 6,774 cells/2L (range,
600Y38,668 cells/2L) for boys (P G 0.02). The duration of fever after initiating antibiotic therapy was longer in girls
than in boys, but there was no difference (Fisher exact test, P G 0.06). The present study documents a relationship
between sex and both the production of inflammatory markers and neutrophil recruitment. Sex difference also showed
more direct clinical relevance with associations seen between sex and both duration of fever and duration of disease
(bronchiolitis P G 0.0007).
KEYWORDSInflammation, sex differences, CRP, ESR, neutrophil count, children
INTRODUCTION
inflammation is chronic, such as when caused by cystic
fibrosis, severe asthma, or sickle cell disease, the prognosis
for females is worse than males. In these situations, female
morbidity and complications are greater than in males. This is
particularly the case in cystic fibrosis where there is a sex gap
in mortality, even if it tends to be reduced today because of
the quality of care from which these patients benefit. This
difference is not explained by the disease characteristics that
are associated with the frequency of Pseudomonas infection,
nutritional state, or lung function. We postulate that in normal
females, the inflammatory response is greater than in males.
This is an advantage to females in cases of acute stress but
detrimental in cases of chronic inflammation. Few clinical
data on sex influences are available in prepubescent patients,
with discrepancies between clinical outcomes: female sex
seems to protect against the deleterious effects of cardiac
operations (9) or postinjury pneumonia (10), but on the
contrary, female sex is associated with a poor prognosis in
cystic fibrosis (11). To evaluate sex differences in frequent
pediatric emergencies, we analyzed the expression of inflammatory markers underlying the inflammatory process (Creactive protein [CRP], erythrocyte sedimentation rate [ESR],
and neutrophil count) in children during common infectious
diseases (pneumonia, pyelonephritis, and bronchiolitis due to
respiratory syncytial virus).
Inflammation plays a major role in life, allowing the
organism to restore homeostatic balance in the case of
infection and traumatic or ischemic tissue damage (1). In
human adults and in animals, females express enhanced levels
of immunoreactivity with increased resistance to infections,
but also higher susceptibility to autoimmune diseases (1Y7).
In vitro studies of human lymphoid cells also show sex
differences in immune function. These differences (although
not explained) are usually accounted for by hormonal status
and usually become apparent after puberty. No clear and
unifying explanation exists to understand how sex and/or
hypothalamic-pituitary hormones affect the development and
function of the immune system. The medical literature shows
that the prognosis of an infection or a severe inflammation is
better for a woman than a man (8). This observation is also
true of children. The exact causes of this phenomenon remain
elusive. However, it could be explained by the strong
mobilization of immune and inflammatory responses during
acute stress; this inflammatory process would thus be
influenced by sex. Neutrophils play a major role during
sepsis, major burns, or surgical operations, as do proteins
produced during the acute inflammatory phase. When severe
Address reprint requests to Georges J. A. Casimir, MD, PhD, Pulmonology and
Allergology and Cystic Fibrosis Department, Free University of Brussels (ULB),
Hopital Universitaire des Enfants Reine Fabiola, Avenue Crocq, 15, 1020 Brussels,
Belgium. E-mail: gcasim@ulb.ac.be.
DOI: 10.1097/SHK.0b013e3181b2b36b
Copyright ! 2010 by the Shock Society
SUBJECTS AND METHODS
The study included 384 children (192 girls and 192 boys) hospitalized for
pneumonia at the University Childrens Hospital Queen Fabiola between
258
Copyright @ 2010 by the Shock Society. Unauthorized reproduction of this article is prohibited.
SHOCK MARCH 2010
GENDER DIFFERENCES
IN INFLAMMATORY
MARKERS
IN
CHILDREN
259
TABLE 1. Characteristics of the cohort of 482 children studied
Girls, median (range)
Age, mo
33.5 (1Y96)
Boys, median (range)
32.5 (1Y95)
P (Mann-Whitney)
0.53
ESR, mm/h
39.5 (2Y104)
24 (1Y104)
0.005
CRP, mg/dL
5.45 (0.2Y36)
2.6 (0.3Y37.3)
0.0001
Body temperature, -C
38.3 (35.5Y40.8)
38.3 (35.6Y40.8)
0.98
1 (0Y240)*
1 (0Y80)*
0.06
Duration of fever after antibiotics, h
WBC, cells/2L
Neutrophils, cells/2L
Lymphocytes, cells/2L
14,040 (2,940Y35,210)
13,110 (2,820Y43,470)
0.73
8,796 (328Y27,647)
6,774 (600Y38,688)
0.02
3,100 (511Y12,758)
Platelets, cells/2L
334,000 (32,000Y952,000)
No. subjects
241
3,072 (563Y12,728)
316,500 (32,000Y833,000)
0.56
0.66
241
*Results of 192 subjects.
WBC indicates white blood cells.
January 2000 and March 2001, as well as 39 children admitted for
pyelonephritis (20 girls and 19 boys) and 59 for bronchiolitis (29 girls and
30 boys). All these patients were successfully matched for age and sex and
then recorded for study purposes according to the date of admittance. All
patients were younger than 10 years (1Y119 months), and data were available
for each on temperature at admittance, isolated pathogen, white blood cell
count, and formula. Diagnosis of pneumonia was established by chest
radiograph, and pyelonephritis by radioactive renal scanning and three positive
urine cultures.
A control population of prepubescent children, consisting of 97 healthy
children (50 girls and 47 boys) admitted for day surgery (tonsillectomy, circumcision, or strabismus), was included in the study to exclude the influence of sex
differences in basal body temperature. The study was approved by the Ethical
Committee of the University Childrens Hospital Queen Fabiola.
For these children (Table 1; Fig. 1), we observed highly
significant differences between girls and boys in CRP
concentrations and ESR, with a median CRP concentration
C-reactive protein and erythrocyte sedimentation rate
Data were collected from routine screening tests at admission. C-reactive
protein was measured by turbidimetric immunoassay using the kit from
APTEC Diagnostic (Hamme, Belgium), calibrated according to IFCC recommendations (ref. CRM 470). Erythrocyte sedimentation rate was estimated
over 1 h using the ESR reader from Menarini Diagnostic (Paris, France).
Neutrophil counts
Neutrophil counts were estimated using the reader from Bayer, Technicon
H2 (Dublin, Ireland) and Advia 120 hematology analyzer (Siemens Healthcare Diagnostic, Brussels, Belgium).
Virus cultures, Mycoplasma culture, and bacterial
antigen in urine
Cultures of viruses were done for influenza virus, respiratory syncytial
virus, parainfluenza virus, and adenovirus on nasal or tracheobronchial
specimens, which contain many epithelial cells that can be used to isolate
these common viruses. Culture of nasopharyngeal aspirates was done for
Mycoplasma pneumoniae (Mycoalert; Lonza, Drogenbos, Belgium). Urine
antigen detection (Binax Now; Iverness Medical, Gent, Belgium) was
performed for Streptococcus pneumoniae and Haemophilus influenzae.
Body temperature
To establish central body temperatures, intrarectal measurements were
made using a mercury thermometer. Fever was defined for central body
temperature values greater than 37.5-C.
Statistical analysis
For discrete variable, Fisher exact test was used, and for nonparametric
variables, Mann-Whitney test. Multiple regression analysis was used to
determine related variables, and the Kruskal-Wallis test to analyze relationship
between multiple nonparametric variables.
RESULTS
The study population comprised 482 children, age- and
sex-matched, who had had different infectious conditions.
FIG. 1. A, C-reactive protein and sex (P G 0.0001). B, Erythrocyte
sedimentation rate and sex (P G0.0009). C, Neutrophils and sex (P G 0.02).
Copyright @ 2010 by the Shock Society. Unauthorized reproduction of this article is prohibited.
260
SHOCK VOL. 33, NO. 3
of 5.45 mg/dL (range, 0.2Y36.0 mg/dL) for girls and 2.6
mg/dL (range, 0.3Y37.3 mg/dL) for boys (P G 0.0001) and a
median ESR of 39.5 mm/h (range, 2Y104 mm/h) for girls
and 24 mm/h (range, 4Y140 mm/h) for boys (P G 0.005).
Neutrophil counts were also significantly different, with a
median value of 8,796 cells/2L (range, 328Y27,645 cells/2L)
for girls and 6,774 cells/2L (range, 600Y38,668 cells/2L)
for boys (P G 0.02). In all cases, values tended to be higher
in girls. Duration of fever (temperature 938-C) after initiation
of antibiotic therapy was recorded for only 384 patients with
pneumonia. The duration was longer in girls than in boys,
but there was no statistically significant difference (Fisher
exact test, P G 0.06). Also, the proportion of girls (n = 27)
presenting fever after 24 h of antibiotic therapy was higher
than that of boys (n = 16), although most patients were
afebrile after 24 h (110 girls and 122 boys). Body temperature at admittance was not statistically significantly different
(P G 0.98).
CASIMIR
ET AL.
FIG. 3. Erythrocyte sedimentation rate in 480 male and female
children. Erythrocyte sedimentation rates were statistically significantly
different between girls and boys: P G 0.0009 (Mann-Whitney).
Percentile plots of CRP concentrations, ESR, and neutrophil counts (Figs. 2Y4) clearly showed separate distributions
for boys (below) and girls (above). Figures 2 and 3 show separate curves above a threshold of CRP 2.5 mg/dL and ESR 20
mm/h up to CRP 25 mg/dL and ESR 80 mm/h. The same was
true for neutrophil count (Fig. 4), with two distinct distributions observed for values between 7,500 and 20,000 cells/2L.
The trend was the same when patients were classified according to their specific infectious condition (results not shown). In
the case of bronchiolitis, separate curves were already visible
for neutrophil counts greater than 2,000 cells/2L. Further
analyses were made with respect to the specific infectious
disease.
PyelonephritisBody temperature at admission was not
significantly different for both sexes. However, significant
differences were observed between girls and boys with respect
to CRP concentration (P = 0.02) and both white blood cell and
neutrophil counts (P = 0.04 and 0.03, respectively) (Table 2).
Of the 39 children with pyelonephritis, the disease was shown
to be caused by Escherichia coli in 28 cases (72%), Proteus
mirabilis in six cases (15%), Pseudomonas aeruginosa in
five cases (2%), and Staphylococcus sp or Enterococcus sp in
the remaining patients.
PneumoniaAs above, basal body temperature was not
different in the two sexes. Whereas differences in CRP
concentrations and ESR levels between girls and boys were
statistically significant (P = 0.001 and 0.01, respectively)
(Table 3), there was no significant difference in neutrophil
counts. In the 384 children with pneumonia included in this
study, infectious parameters including presence of bacterial
antigen in urine, positive viral culture, or identification of a
Mycoplasma were found to be similar in both boys and girls.
BronchiolitisIn this group of very young children, both
concentrations of CRP and ESR measurements were low, with
no significant differences between girls and boys. However,
neutrophil counts were significantly higher (P = 0.02) in girls
than in boys (Table 4). Antibiotics were not administered in
these cases, but the duration of hospitalization in girls was
longer in boys (P = 0.0007).
FIG. 2. C-reactive protein in 480 male and female children. C-reactive
protein concentrations were statistically significantly different between girls
and boys (Mann-Whitney).
FIG. 4. Neutrophil counts in 480 male and female children. Neutrophil
counts were statistically significantly different between girls and boys: P G
0.02 (Mann-Whitney).
Distributions of CRP concentrations, ESR values, and
neutrophil counts
Copyright @ 2010 by the Shock Society. Unauthorized reproduction of this article is prohibited.
SHOCK MARCH 2010
GENDER DIFFERENCES
IN INFLAMMATORY
MARKERS
IN
CHILDREN
261
TABLE 2. Characteristics of the patients with pyelonephritis
Girls, median (range)
Age, mo
Boys, median (range)
26.5 (2Y104)
ESR, mm/h
19 (1Y116)
53 (13Y75)
CRP, mg/dL
36.5 (3Y82)
9.8 (1.7Y34.9)
Body temperature, -C
39 (36.7Y40.5)
35 (1Y96)
0.47
0.14
7.5 (0.5Y20.4)
Duration of fever after antibiotics, h
P (Mann-Whitney)
38.2 (36.9Y40.5)
24 (1Y80)
0.02
0.2
0.27
WBC, cells/2L
18,490 (5,440Y30,780)
13,700 (5,800Y28,489)
0.04
Neutrophils, cells/2L
11,440 (2,263Y23,055)
7,700 (600Y17,608)
0.03
Lymphocytes, cells/2L
3,898 (1,008Y10,680)
Platelets, cells/2L
3,024 (1,127Y7,955)
289,500 (208,000Y606,000)
303,000 (172,000Y525,000)
20
19
No. subjects
Basal body temperature in 97 healthy children
(50 girls and 47 boys)
There were no significant differences between the sexes in
age (P 9 0.33) and for basal body temperature (P 9 0.22)
measured using a mercury thermometer.
DISCUSSION
Our retrospective study presents some weaknesses, because
it focused only on three markers of the inflammatory response
while key cytokines or other upstream mediators (e.g., IL-6,
IL-2, IL-12, TNF, and NO) were not measured. However,
using usual biological markers (CRP, ESR, and neutrophil
count), these data show that marked differences exist between
boys and girls younger than 10 years. Possible differences in
immune reactivity due to age were excluded because male and
female subjects were age matched. Longer periods of hospitalization in girls, for example, with bronchiolitis, and
longer duration of fever after antibiotic therapy, also in girls,
generally suggest that sex can modulate the clinical expression of certain symptoms and perhaps the severity of disease.
However, new prospective studies are needed to evaluate
whether sexual differences in inflammatory markers are
associated with clear quantitative and/or qualitative clinical
0.46
0.59
differences. In this case, the treatment of choice in the future
and the doses of anti-inflammatory drugs could be sex related.
Previous studies on recorded CRP levels have shown no
sex-associated differences in healthy adult blood donors (12).
A large cohort of children with various infectious conditions
was studied, and results showed that sex-related differences in
response were dependent on the magnitude (and/or kinetics)
of the inflammatory response, influenced by the organ
infected. Biological parameters increase at the beginning of
the inflammatory process. Over time, CRP levels, ESR values,
and neutrophil counts reached threshold levels above which
values in girls were systematically higher than those observed
in boys. At the peak of the inflammatory response, parameters
become similar.
The phenomenon is similar in the three diseases, even if the
importance of the inflammatory process might modulate the
response of each marker according to its variability in each
sick population.
In cases of pneumonia, whereas CRP concentrations and
ESR levels were higher in girls than in boys between the
lower and upper thresholds, neutrophil counts were not
distinct. In this case, sex differences may have been masked
by differences caused by the diversity of pathogens involved.
Neutrophils could also have been largely trapped in infected
lungs.
TABLE 3. Sex-related inflammatory differences in 384 children with pneumonia
Girls, median (range)
Age, mo
38 (1Y121)
CRP, mg/dL
5.5 (0.2Y36)
ESR, mm/h
44.5 (2Y104)
WBC, cells/2L
Boys, median (range)
41 (1Y119)
3.3 (0.3Y37.3)
28 (3Y140)
P Mann-Whitney
0.27
0.001
0.01
13,730 (2,940Y35,210)
12,925 (2,820Y43,470)
0.83
Neutrophils, cells/2L
8,794 (328Y27,645)
7,785 (875Y38,688)
0.77
Lymphocytes, cells/2L
3,052 (511Y12,758)
3,097 (563Y12,728)
Duration of fever after antibiotics, h
1 (0Y240)
1 (0Y64)
No. cases with bacterial antigens in urine
78
72
No. cases with Mycoplasma-positive culture
19
15
No. cases with virus-positive culture
Body temperature, -C
No. subjects
33
39 (36.2Y40.8)
192
0.81
0.11
29
39 (36Y40)
192
Copyright @ 2010 by the Shock Society. Unauthorized reproduction of this article is prohibited.
0.74
262
SHOCK VOL. 33, NO. 3
CASIMIR
ET AL.
TABLE 4. Sex-related inflammatory differences in 59 children with bronchiolitis
Girls, median (range)
Age, mo
5 (1Y12)
Boys, median (range)
4 (1Y18)
P (Mann-Whitney)
0.20
CRP, mg/dL
0.5 (0.5Y8.1)
0.55 (0.5Y8)
0.61
ESR, mm/h
8.5 (2Y67)
10.5 (1Y60)
0.84
WBC, cells/2L
Neutrophils, cells/2L
Hospitalization, d
No. subjects
14,000 (4,890Y23,760)
5,267 (1,433Y14,921)
15 (9Y42)
29
Sexual differences in adults are usually related to sexual
hormone production, but in prepubescent children, levels of
sex hormones are very low. However, some studies have
shown that even in very young children, mean estrogen levels
could be seven times higher in girls than in boys (13).
Therefore, even in prepubescent children, hormonal differences might influence inflammatory response, modifying the
level of response in girls: the potential roles of estrogens,
testosterone, prolactin, and glucocorticosteroids need to be
evaluated. The role of steroid sex hormones, especially
estrogens, on the synthesis of acute-phase response proteins
is well established. Indeed, high levels of fibrinogen production during oral contraceptive therapy are responsible for the
increased risk of thrombosis, strokes, and pulmonary emboli.
Furthermore, during pregnancy, concentrations of ceruloplasmin, !1-protease inhibitor, fibrinogen, C3, and C4 are
elevated (6). Before puberty, prepubertal gonads are already
producing sex hormones, which might play a role, not only in
the control of growth hormone synthesis in early childhood,
but also in the management of acute inflammation (7).
Alternatively, our observations could be explained by differences in the expression of certain genes that depend on the
balance between X and Y chromosomes. Ellis (14) showed
that the second X chromosome might be only partially
inactivated in girls allowing the two X chromosomes to
express certain genes, as well documented by Spolarics (15).
These data are very important from the clinical point of
view, when we observe that approximately five times more
girls have severe asthma than boys, that many autoimmune
diseases appear more frequently in girls than in boys, and that
some diseases, such as cystic fibrosis, characterized by local
inflammatory destruction of tissues, have a more severe
prognosis in the female population. In a recent study, Aoyama
et al. (16) showed that male wild-type (WT) mice were more
susceptible to endotoxin than female WT mice (survival rate,
25% in male WT and 82% in female WT), and this
phenomenon seems to be under the influence of IL-18
production that decreases survival only in boys. On the other
hand, increased inflammatory response may be beneficial in
some pathological conditions where acute inflammatory
response may aid complete recovery and perhaps improve
11,900 (3,300Y23,260)
0.35
3,385 (921Y14,002)
0.02
0.0007
10 (3Y24)
30
longevity. In addition, inflammatory markers are often
substances with antiprotease activity, and it may be that
increased antiprotease activity is in some way advantageous to
the female population.
ACKNOWLEDGMENTS
The authors thank Prof. A. Kahn for his grant support.
REFERENCES
1. Lahita RG: Sex hormones and the immune system-part 1. Human data.
Baillieres Clin Rheumatol 4:1Y12, 1990.
2. Ahmed SA, Talal N: Sex hormones and the immune system-part 2. Human
data. Baillieres Clin Rheumatol 4:13Y31, 1990.
3. Cannon JG, St Pierre B: Gender differences in host defense mechanisms.
J Psychiatr Res 31:99Y113, 1997.
4. Hansen BL: Why do some individuals produce autoreactive antibodies against
receptors and/or their ligands? A possible answer to the question. Scand J
Immunol 24:363Y370, 1986.
5. Buckingham JC, Cowell AM, Gillies GE, Herbison AE, Steel JH: Neuroendocrine response to stress. In: Buckingham JC, Gillies GE, Cowell AM
(eds.): Stress, Stress Hormones and the Immune System. New York, NY:
Wiley, pp 9Y47, 1997.
6. Sigal LH: The acute phase response to inflammation. In: Sigal LH, Ron Y,
(eds.): Immunology and Inflammation. Basic Mechanisms and Clinical
Consequences. New York: McGraw-Hill, pp 287Y301, 1994.
7. Shames RS: Gender differences in the development and function of the
immune system. J Adolesc Health 30(4 suppl 1):59Y70, 2002
8. Sperry JL, Nathens AB, Frankel HL, Vanek SL, Moore EE, Maier RV, Minei
JP: Characterization of the gender dimorphism after injury and hemorrhagic
shock: are hormonal differences responsible? Crit Care Med 36(6):1838Y1845,
2008.
9. Seghaye MC, Qing M, von Bernuth G: Systemic inflammatory response to
cardiac surgery: does female sex really protect? Crit Care 5(6):343Y348, 2001.
10. Gannon CJ, Pasquale M, Tracy JK, McCarter RJ, Napolitano LM: Male gender
is associated risk for postinjury pneumonia. Shock 21(5):410Y414, 2004.
11. Rosenfeld M, Davis R, FitzSimmons S, Pepe M, Ramsey B: Gender gap in
cystic fibrosis mortality. Am J Epidemiol 145(9):794Y803, 1997.
12. Macy EM, Hayes TE, Tracy RP: Variability in the measurement of C reactive
protein in healthy subjects: implication for reference intervals and epidemiological applications. Clin Chem 43:52Y58, 1997.
13. Oerter Klein K, Baron J, Colli MJ, Mc Donnel DP, Cutler GB: Estrogen levels
in childhood determined by an ultrasensitive recombinant cell bioassay. J Clin
Invest 94(6):2475Y2480, 1994.
14. Ellis N: The war of sex chromosomes. Nature Genetics 20:9Y10, 1998.
15. Spolarics Z: The X-files of inflammation: cellular mosaicism of X-linked
polymorphic genes and the female advantage in the host response to injury and
infection. Shock 27(6):597Y604, 2007.
16. Aoyama M, Kotani J, Usami M: Gender difference in granulocyte dynamics
and apoptosis and the role of IL-18 during endotoxin-induced systemic
inflammation. Shock 32(4):401Y409, 2009.
Copyright @ 2010 by the Shock Society. Unauthorized reproduction of this article is prohibited.
Вам также может понравиться
- tmp3CAB TMPДокумент16 страницtmp3CAB TMPFrontiersОценок пока нет
- tmpCE8C TMPДокумент19 страницtmpCE8C TMPFrontiersОценок пока нет
- tmp80F6 TMPДокумент24 страницыtmp80F6 TMPFrontiersОценок пока нет
- tmpF3B5 TMPДокумент15 страницtmpF3B5 TMPFrontiersОценок пока нет
- tmpE3C0 TMPДокумент17 страницtmpE3C0 TMPFrontiersОценок пока нет
- tmpEFCC TMPДокумент6 страницtmpEFCC TMPFrontiersОценок пока нет
- tmp6F0E TMPДокумент12 страницtmp6F0E TMPFrontiersОценок пока нет
- Tmpa077 TMPДокумент15 страницTmpa077 TMPFrontiersОценок пока нет
- tmpF178 TMPДокумент15 страницtmpF178 TMPFrontiersОценок пока нет
- Tmp1a96 TMPДокумент80 страницTmp1a96 TMPFrontiersОценок пока нет
- tmpFFE0 TMPДокумент6 страницtmpFFE0 TMPFrontiersОценок пока нет
- tmpE7E9 TMPДокумент14 страницtmpE7E9 TMPFrontiersОценок пока нет
- tmp998 TMPДокумент9 страницtmp998 TMPFrontiersОценок пока нет
- tmp6382 TMPДокумент8 страницtmp6382 TMPFrontiersОценок пока нет
- tmpF407 TMPДокумент17 страницtmpF407 TMPFrontiersОценок пока нет
- Tmp75a7 TMPДокумент8 страницTmp75a7 TMPFrontiersОценок пока нет
- tmp72FE TMPДокумент8 страницtmp72FE TMPFrontiersОценок пока нет
- tmp60EF TMPДокумент20 страницtmp60EF TMPFrontiersОценок пока нет
- tmp9D75 TMPДокумент9 страницtmp9D75 TMPFrontiersОценок пока нет
- tmp8B94 TMPДокумент9 страницtmp8B94 TMPFrontiersОценок пока нет
- tmp4B57 TMPДокумент9 страницtmp4B57 TMPFrontiersОценок пока нет
- tmpC0A TMPДокумент9 страницtmpC0A TMPFrontiersОценок пока нет
- tmp37B8 TMPДокумент9 страницtmp37B8 TMPFrontiersОценок пока нет
- tmpB1BE TMPДокумент9 страницtmpB1BE TMPFrontiersОценок пока нет
- tmpD1FE TMPДокумент6 страницtmpD1FE TMPFrontiersОценок пока нет
- tmp27C1 TMPДокумент5 страницtmp27C1 TMPFrontiersОценок пока нет
- tmpA0D TMPДокумент9 страницtmpA0D TMPFrontiersОценок пока нет
- tmp2F3F TMPДокумент10 страницtmp2F3F TMPFrontiersОценок пока нет
- tmpC30A TMPДокумент10 страницtmpC30A TMPFrontiersОценок пока нет
- tmp3656 TMPДокумент14 страницtmp3656 TMPFrontiersОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Dengue Shock Syndrome: Dr. Elsye Souvriyanti, SpaДокумент18 страницDengue Shock Syndrome: Dr. Elsye Souvriyanti, SpaYesi Maulani NovitasariОценок пока нет
- Gapuz Communicable Disease NursingДокумент46 страницGapuz Communicable Disease NursingBJ DUQUESAОценок пока нет
- Hav Igm CTKДокумент2 страницыHav Igm CTKGu AleXanderОценок пока нет
- 2018 - 07-TTI-Quarterly-Report-Form - 2nd QuarterДокумент2 страницы2018 - 07-TTI-Quarterly-Report-Form - 2nd QuarterRoy PasadillaОценок пока нет
- Pediatric Vaccine Àd Vaccination PDFДокумент257 страницPediatric Vaccine Àd Vaccination PDFntnquynhpro100% (1)
- Etiopathogenesis and Natural History of Carcinoma Cervix: Human Papilloma Virus High Risk FactorsДокумент33 страницыEtiopathogenesis and Natural History of Carcinoma Cervix: Human Papilloma Virus High Risk FactorsNatasya Ayusandra MahersaputriОценок пока нет
- Rheumatic FeverДокумент16 страницRheumatic Feversteve benОценок пока нет
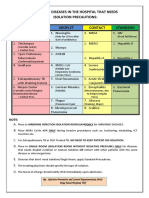
- Common Hospital Diseases Requiring Isolation PrecautionsДокумент1 страницаCommon Hospital Diseases Requiring Isolation Precautionsjerimiah_manzonОценок пока нет
- Anaphy Lec Sas-17Документ4 страницыAnaphy Lec Sas-17Francis Steve RipdosОценок пока нет
- What's The Best Antibiotic For A Staph Infection - Treatments and RisksДокумент3 страницыWhat's The Best Antibiotic For A Staph Infection - Treatments and RisksSundaramoorthy SelvanathanОценок пока нет
- Soi 2016-17Документ280 страницSoi 2016-17venkat_nsnОценок пока нет
- Blood Infusion Warmer DeviceДокумент16 страницBlood Infusion Warmer DeviceSRL MECHОценок пока нет
- URTICARIAДокумент2 страницыURTICARIAChandra Kefi AmtiranОценок пока нет
- AO RabiesДокумент21 страницаAO RabiesChristopher Owen T. JOCSONОценок пока нет
- Covid-19 SOP Flow Chart for Manufacturing CompanyДокумент6 страницCovid-19 SOP Flow Chart for Manufacturing CompanynorfilzahОценок пока нет
- Per-Pl 206Документ266 страницPer-Pl 206Wan YusufОценок пока нет
- Introduction To Serology - Immunology, HSV & H.pyloriДокумент37 страницIntroduction To Serology - Immunology, HSV & H.pyloritriaclaresiaОценок пока нет
- Tetanus ToxoidДокумент2 страницыTetanus Toxoidunkown userОценок пока нет
- Stress and Immune SystemДокумент15 страницStress and Immune SystemRhishabhОценок пока нет
- Treatment of Rheumatoid Arthritis in Patients With Concomitant Chronic Hepatitis C InfectionДокумент24 страницыTreatment of Rheumatoid Arthritis in Patients With Concomitant Chronic Hepatitis C InfectionMuhammad Farras Razin PerdanaОценок пока нет
- Bioterroris M: DR - Sakshi Mishra Mph-SemiДокумент26 страницBioterroris M: DR - Sakshi Mishra Mph-SemiSakshi MishraОценок пока нет
- Annotated BibliographyДокумент7 страницAnnotated Bibliographyapi-202202577Оценок пока нет
- 9 Th. Lec. Lewis Blood Group SystemДокумент11 страниц9 Th. Lec. Lewis Blood Group Systemda202263357026Оценок пока нет
- Common Childhood Diseases and Healthy HabitsДокумент6 страницCommon Childhood Diseases and Healthy HabitsHF ManigbasОценок пока нет
- Untitled21 PDFДокумент18 страницUntitled21 PDFElizabeth LeonОценок пока нет
- E-Poster Enterics For Global Health Shigella Surveillance StudyДокумент1 страницаE-Poster Enterics For Global Health Shigella Surveillance StudyNeyama AlladinОценок пока нет
- EpiДокумент3 страницыEpiNiño PaoloОценок пока нет
- Avian Influenza Case StudyДокумент8 страницAvian Influenza Case StudyAatif HussainОценок пока нет
- CDC Guidelines on Standard and Transmission-Based PrecautionsДокумент6 страницCDC Guidelines on Standard and Transmission-Based PrecautionsKomite PPI RSUDPCОценок пока нет
- Pathophysiology of Leptospirosis and Dengue FeverДокумент5 страницPathophysiology of Leptospirosis and Dengue FeverKenneth Lagman100% (1)