Академический Документы
Профессиональный Документы
Культура Документы
Resume Ke 2 Mikrobio
Загружено:
DitaMenonАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Resume Ke 2 Mikrobio
Загружено:
DitaMenonАвторское право:
Доступные форматы
Name : Dita Paramytha A
NIM
: 140210103068
Class
:B
RESUME MICROBIOLOGY
STERILIZATION AND DISENFECTANT
Disinfection and sterilization are essential for ensuring that medical and surgical
instruments do not transmit infectious pathogens to patients. Because sterilization of all
patient-care items is not necessary, health-care policies must identify, primarily on the basis
of the items intended use, whether cleaning, disinfection or sterilization is indicated.
Sterilization describes a process that destroys or eliminates all forms of
microbial life and is carried out in health-care facilities by physical or
chemical methods. The various methods of sterilization are:
1. Physical Method
(a) Thermal (Heat) methods
(b) Radiation method
(c) Filtration method
2. Chemical Method
3. Gaseous Method
Thermal Physical method have two classifying for the heat. There
are heat sterilizaton and dry heat. One of physical method is heat
sterilization. It is the most widely used and reliable method of sterilization,
involving destruction of enzymes and other essential cell constituents. The
process is more effective in hydrated state where under conditions of high
humidity, hydrolysis and denaturation occur, thus lower heat input is
required. Under dry state, oxidative changes take place, and higher heat
input is required. This method of sterilization can be applied only to the
thermostable products, but it can be used for moisture-sensitive materials
for which dry heat (160-180C) sterilization, and for moisture-resistant
materials for which moist heat (121-134C) sterilization is used. Dry heat
sterilization are incineration, red heat, flaming and hot air oven. It
employs higher temperatures in the range of 160-180C and requires
exposures time up to 2 hours, depending upon the temperature
employed. The benefit of dry heat includes good penetrability and noncorrosive nature which makes it applicable for sterilizing glass-wares and
metal surgical instruments. It is also used for sterilizing non-aqueous
thermo-stable liquids and thermostable powders. Dry heat destroys
bacterial endotoxins (or pyrogens) which are difficult to eliminate by other
means and this property makes it applicable for sterilizing glass bottles
which are to be filled aseptically.
Many types of radiation are used for sterilization like
electromagnetic radiation (e.g. gamma rays and UV light), particulate
radiation (e.g. accelerated electrons). The major target for these radiation
is microbial DNA. Gamma rays and electrons cause ionization and free
radical production while UV light causes excitation. Radiation sterilization
with high energy gamma rays or accelerated electrons has proven to be a
useful method for the industrial sterilization of heat sensitive products.
But some undesirable changes occur in irradiated products, an example is
aqueous solution where radiolysis of water occurs. Radiation sterilization
is generally applied to articles in the dry state; including surgical
instruments, sutures, prostheses, unit dose ointments, plastic syringes
Filtration Sterilization process does not destroy but removes the
microorganisms. It is used for both the clarification and sterilization of
liquids and gases as it is capable of preventing the passage of both viable
and non viable particles. The major mechanisms of filtration are sieving,
adsorption and trapping within the matrix of the filter material. Sterilizing
grade filters are used in the treatment of heat sensitive injections and
ophthalmic solutions, biological products and air and other gases for
supply to aseptic areas. They are also used in industry as part of the
venting systems on fermentors, centrifuges, autoclaves and freeze driers.
Membrane filters are used for sterility testing.
Gaseous Sterilization had some indicator like physical Indicator: Gas
concentration is measured independently of pressure rise, often by
reference to weight of gas used, Chemical Indicator: The chemical
indicator used here are Royach Sacket, the indicator paper impregnated
with reactive chemical which undergoes a distinct colour change on
reaction. Chemical indicators are valuable monitors of the condition
prevailing at the coolest of most in accessible part of a sterilizer and
Biological Indicator: As with chemical indicator they are usually packed in
dummy packs located at strategic sites in the sterilizer. Alternatively for
gaseous sterilization, these may also be placed in tubular helix device.
The species of bacteria generally used for gaseous sterilization are
B.subtilis var.niger and B.subtilis var.golbigii.
Gaseous Sterilization is the chemically reactive gases such as
formaldehyde, (methanol, H.CHO) and ethylene oxide (CH2)2O possess
biocidal activity. Ethylene oxide is a colorless, odorless, and flammable
gas. The mechanism of antimicrobial action of the two gases is assumed
to be through alkylations of sulphydryl, amino, hydroxyl and carboxyl
groups on proteins and amino groups of nucleic acids. The concentration
ranges (weight of gas per unit chamber volume) are usually in range of
800-1200 mg/L for ethylene oxide and 15-100 mg/L for formaldehyde with
operating temperatures of 45-63C and 70-75C respectively. Both of
these gases being alkylating agents are potentially mutagenic and
carcinogenic. They also produce acute toxicity including irritation of the
skin, conjunctiva and nasal mucosa.
Liquid Sterilization is one part of the chemical method. Liquid
sterilization are Peracetic Acid liquid sterilization: Peracetic acid was found
to be sporicidal at low concentrations. It was also found to be water
soluble, and left no residue after rinsing. It was also shown to have no
harmful health or environmental effects. It disrupts bonds in proteins and
enzymes and may also interfere with cell membrane transportation
through the rupture of cell walls and may oxidize essential enzymes and
impair vital biochemical pathways. Hydrogen Peroxide Sterilization: This
method disperses a hydrogen peroxide solution in a vacuum chamber,
creating a plasma cloud. This agent sterilizes by oxidizing key cellular
components, which inactivates the microorganisms. The plasma cloud
exists only while the energy source is turned on. When the energy source
is turned off, water vapor and oxygen are formed, resulting in no toxic
residues and harmful emissions. The temperature of this sterilization
method is maintained in the 40-50C range, which makes it particularly
well-suited for use with heat-sensitive and moisture-sensitive medical
devices. The instruments are wrapped prior to sterilization, and can either
be stored or used immediately. There are five phases of the hydrogen
peroxide.
Disinfection describes a process that eliminates many or all
pathogenic microorganisms, except bacterial spores, on inanimate
objects. Classification of disinfectants based on consistency; (a) Liquid
(E.g., Alcohols, Phenols); (b) Gaseous (Formaldehyde vapour) ,based on
spectrum of activity ; (a) High level;(b) Intermediate level; (c) Low level ,
based on mechanism of action; (a) Action on membrane (E.g., Alcohol,
detergent); (b) Denaturation of cellular proteins (E.g., Alcohol, Phenol); (c)
Oxidation
of
essential
sulphydryl
groups
of
enzymes
(E.g.,
H2O2,Halogens); (d) Alkylation of amino-, carboxyl- and hydroxyl group
(E.g.,Formaldehyde); (e) Damage to nucleic acids (Formaldehyde).
Question :
1. How to protect our body with the various sterilization process in
dangerous location and our body have alergy for some chemical
tools?
Answer :
1. Maybe we can used the radiation sterilization dor little
concentrations.
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- 07 - Nutrition - Health Dairy PDFДокумент14 страниц07 - Nutrition - Health Dairy PDFladirОценок пока нет
- Manual Transaxle: Group 22AДокумент18 страницManual Transaxle: Group 22AToponari MedveОценок пока нет
- Figure 2-6 Block Diagram of An Industrial Control System, Which Consists of An Automatic Controller, AnДокумент6 страницFigure 2-6 Block Diagram of An Industrial Control System, Which Consists of An Automatic Controller, AnTaufiq RizkiОценок пока нет
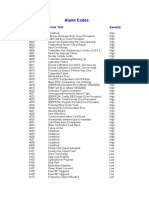
- Alarm Codes: Alarm Code Alarm Text SeverityДокумент2 страницыAlarm Codes: Alarm Code Alarm Text SeverityЕТМОценок пока нет
- Experiment No. 3: To Perform Turning Operation On LatheДокумент3 страницыExperiment No. 3: To Perform Turning Operation On LatheHasnain AshrafОценок пока нет
- CBSE Class-12 Chemistry Quick Revision Notes on Haloalkanes and HaloarenesДокумент6 страницCBSE Class-12 Chemistry Quick Revision Notes on Haloalkanes and HaloarenesKunal ShahОценок пока нет
- Lithium-Ion Vs AGM BatteriesДокумент20 страницLithium-Ion Vs AGM BatteriesCentaur ArcherОценок пока нет
- Vietnam-Korea Friendship IT College Module 4: Principles of DesignДокумент13 страницVietnam-Korea Friendship IT College Module 4: Principles of DesignPhạm Trần Mộc MiêngОценок пока нет
- Configurations & Parts Identification: Trailer Suspension SeriesДокумент26 страницConfigurations & Parts Identification: Trailer Suspension SeriesleosignareОценок пока нет
- UM1M830BNA Rev M NCU Controller (6150) PDFДокумент268 страницUM1M830BNA Rev M NCU Controller (6150) PDFanon_760637530Оценок пока нет
- EEMB 2 Study Sheet Midterm 1 W14Документ2 страницыEEMB 2 Study Sheet Midterm 1 W14Paola KallОценок пока нет
- Bacal Typed QuestionsДокумент6 страницBacal Typed QuestionsAdrian Palanio DayonОценок пока нет
- Work Experience Education: Software Engineer InternДокумент1 страницаWork Experience Education: Software Engineer InternBob JonesОценок пока нет
- Design of Irrigation CanalsДокумент6 страницDesign of Irrigation CanalsSaad ShauketОценок пока нет
- (Don Noble (Editor) ) John Steinbeck (Critical Insights)Документ439 страниц(Don Noble (Editor) ) John Steinbeck (Critical Insights)jnoubiyeОценок пока нет
- Cavity Wall Insulation Inspection ReportДокумент100 страницCavity Wall Insulation Inspection ReportAbbas LadonniОценок пока нет
- Sample CollectionДокумент41 страницаSample Collectionsoumen100% (1)
- PROTEIN AND WATER (Updated)Документ17 страницPROTEIN AND WATER (Updated)abahojomacynthiaОценок пока нет
- Absorption Tower For CO2Документ11 страницAbsorption Tower For CO2ankitsamriaОценок пока нет
- Jansen ASM Chapte TMG2011 PDFДокумент23 страницыJansen ASM Chapte TMG2011 PDFeitan-dalia4971Оценок пока нет
- SBCI State of Play IndiaДокумент46 страницSBCI State of Play IndiaUnited Nations Environment ProgrammeОценок пока нет
- TOBUL OandMsheet052909v2Документ5 страницTOBUL OandMsheet052909v2Walter JosephОценок пока нет
- PHYSICAL SCIENCE - Lesson Plan On Solubility and MiscibilityДокумент7 страницPHYSICAL SCIENCE - Lesson Plan On Solubility and MiscibilityBarbeicaht Sallin100% (1)
- LZ457A New Three StepДокумент2 страницыLZ457A New Three StepAndre Medeiros AlmeidaОценок пока нет
- 1.5 Total Maintenance Cost As A Percent of Replacement Asset Value (Rav)Документ4 страницы1.5 Total Maintenance Cost As A Percent of Replacement Asset Value (Rav)cksОценок пока нет
- Primark Metal Policy Ensures Customer SafetyДокумент27 страницPrimark Metal Policy Ensures Customer SafetyalamtareqОценок пока нет
- About Harappan Town PlanningДокумент7 страницAbout Harappan Town PlanningAnonymous tQgCnSBKmOОценок пока нет
- Reasons For Developing Food ProductsДокумент5 страницReasons For Developing Food Productssheela baralОценок пока нет
- Critical Analysis of The Great Belt East Bridge PDFДокумент10 страницCritical Analysis of The Great Belt East Bridge PDFMahmoud Moustafa ElnegihiОценок пока нет
- Bronchitis ReportДокумент34 страницыBronchitis ReportRolinette DaneОценок пока нет