Академический Документы
Профессиональный Документы
Культура Документы
DT Oct 13 NPR Milnar Fnl1
Загружено:
Kranti PrajapatiАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
DT Oct 13 NPR Milnar Fnl1
Загружено:
Kranti PrajapatiАвторское право:
Доступные форматы
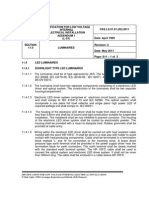
Continuing Education
Volume 32 No. 10 Page 100
Minimally Invasive Cure
for Life-Long Discoloration
Authored by Frank J. Milnar, DDS
Upon successful completion of this CE activity 2 CE credit hours will be awarded
Opinions expressed by CE authors are their own and may not reflect those of Dentistry Today. Mention of
specific product names does not infer endorsement by Dentistry Today. Information contained in CE articles and
courses is not a substitute for sound clinical judgment and accepted standards of care. Participants are urged to
contact their state dental boards for continuing education requirements.
Continuing Education
transmission properties of the tooth structure due to pulp
necrosis or variations in the dentin.2 As a result, the
permanent dentition is affected by turning a brown hue.3
Unfortunately, many more conditions that can create
permanent discoloration include dental fluorosis, plaque
calcifications, and the prenatal use of tetracycline.
Tooth discoloration can have psychological effects on
individuals. A study conducted by the US Air Force Dental
Corps identified what people thought characterized an
attractive smile. A total of 297 subjects viewed 8
photographs of female smiles, 8 photographs of male
smiles, and completed a questionnaire to rate the
attractiveness of each photograph. The study concluded that
in all cases, tooth shade was the most important factor in
determining an attractive smile. This is relevant because
science has already established that dentofacial
attractiveness greatly affects the psychosocial well-being of
an individual.4
Unfortunately, managing discolored teeth can be a
complex problem, and treatment usually requires a
combination of modalities for predictability. For cases in
which the discoloration is not extreme, dentist dispensed or
supervised at-home or in-office bleaching procedures may
be adequate to enhance tooth shade. Bleaching
procedures using hydrogen peroxide or carbamide
peroxide have been proven effective and safe, but there are
reports of adverse reactions such as cervical root
resorption5 and post-treatment sensitivity that can last from
a few hours up to several days.6 However, with brown
intrinsic staining, the discoloration is often more difficult to
address, and bleaching procedures alone will likely not be
sufficient to achieve the desired result.7
Porcelain veneers have been a preferred and effective
option for many patients to treat discolored teeth.8 The reasons
for this include the materials high strength, high aesthetics,
biocompatibility, and clinical longevity when proper adhesive
bonding protocol is followed.9 Some disadvantages of indirect
veneers are aggressive tooth preparation requirements and
technique-sensitive adhesive procedures that, if not performed
precisely, result in debonding or marginal leakage.9
All-ceramic crowns are another treatment option for
masking discolored teeth. These materials, such as lithium
Minimally Invasive Cure
for Life-Long Discoloration
Effective Date: 10/1/2013
Expiration Date: 10/1/2016
ABOUT THE AUTHOR
Dr. Milnar is a graduate from the
University of Minnesota, School of
Dentistry. He is an accredited member of
the American Academy of Cosmetic
Dentistry and a board examiner for
Accreditation. Dr. Milnar maintains a fulltime practice in St. Paul, Minn, emphasizing appearance
related dentistry. He has published numerous articles about
the direct placement of composites, shade selection, and
porcelain materials and is on editorial review boards for
dental journals. Dr. Milnar is cofounder of the Minnesota
Academy of Cosmetic Dentistry and has lectured
extensively within the US Armed Forces as well as
internationally on the subject of direct composite
restorations, shade selection and porcelain materials. He
has been voted Top Dentist for the last several years in the
Minneapolis/St. Paul Magazine. He has been named a
Leader in Continuing Education by Dentistry Today. He can
be reached at the Web site stpaulsmiles.com.
Disclosure: Dr. Milnar discloses that he received financial
support from Tokuyama Dental America.
INTRODUCTION
Often the first noticeable difference in varying dentition
between individuals is tooth color. Tooth discoloration is
caused in one of 2 ways.1 These causes can be extrinsic
when dietary colorants or other deposits attach to the tooth
surface or pellicle layer through tobacco use, coffee or tea
ingestion, poor oral hygiene, and use of chemical plaque
preventative agents.
The causes can also be intrinsic. The formation of
intrinsic discoloration occurs during tooth development (or
as a result of trauma) and produces altered light
Continuing Education
Minimally Invasive Cure for Life-Long Discoloration
disilicate and leucite-reinforced porcelains, exhibit
increased durability and aesthetics due to natural/high
translucency. This makes them an excellent option for
treating discoloration in the posterior region where high
strength is necessary and aesthetics are still a concern.
This treatment option should only be considered for teeth
with significant loss of anatomy or severe discoloration, as
all-ceramic crowns generally require more tooth preparation
as compared to other full-coverage options.10
Despite the multitude of options available, there are
several reasons why patients may decline these
recommended aesthetic dental treatments for correcting tooth
discoloration. These may include time constraints or financial
considerations that restrict the methods or materials chosen
by the dentist.11 A patients fear/anxiety level pertaining to
certain procedures like aggressive tooth preparation must
also be considered as a possible reason for refusing
treatment.12
reserved only for the most skillful clinicians, because the
careful layering technique, sculpting, and artistic coloration
were best performed by dentists who had mastered the
material.19 The 1970s brought about light-cured composites
with smaller filler particles that were more color stable than their
predecessors and demonstrated enhanced wear characteristics. A few years later, filler particle size decreased, load
increased, and subsequently the material strengths became
significantly higher, allowing for clinical longevity in the
posterior region. The next material advancement was in using
nanoparticles. These particles are very small, ranging in size
from one nm to 100 nm, increasing filler loading and thusly
enhancing the physical and mechanical properties of the
material.20
Todays composites are available as microfilled,
microhybrid, nanohybrid, and most recently suprananohybrid
materials. These composites range in viscosity from
packables that have handling characteristics similar to
amalgam,21 to flowables that can be syringed directly into
preparations. These advanced materials are important to
clinicians because they provide the ability to deliver
restorations that are aesthetic due to their light reflecting/refracting properties, bond well to dentin and enamel,
and they attain and maintain a good polish and gloss. Among
the composites to date that have addressed these requisites
are Estelite Sigma Quick (Tokuyama Dental America), Filtek
Supreme Ultra (3M ESPE), Tetric EvoCeram and IPS
Empress Direct (Ivoclar Vivadent), Venus Diamond and Venus
Pearl (Heraeus Kulzer), and Renamel Microfill (Cosmedent),
to name just a few.
The newest version of direct composite, suprananohybrids
(Estelite Sigma Quick), demonstrates the combination of
characteristics that dentists have desired from composites for
30 years. Suprananohybrid composite features exceptional
strength while also displaying enhanced optical properties.
Suprananohybrids also demonstrate chameleon shades that
allow for easy matching to natural tooth structure. This enables
dentists to reduce overhead and inventory while still
maintaining their ability to create highly aesthetic restorations
in all regions of the mouth. Additionally, there is almost no
variation in color or volume before and after light-curing, so
there is greater predictability when placing restorations.22
Considering Minimally Invasive Options
When minimally invasive preparation is ideal, dentistmonitored in-office and at-home bleaching procedures,
followed by carefully planned and placed direct composite
restorations, are an option that yields favorable results to
satisfy both patient and dentist aesthetic goals.13,14 Direct
composite is considered among clinicians to be the least
invasive and most conservative method to restore
aesthetically displeasing or diseased teeth to stable color,
form, and function.15 When paired with bleaching, this
combination of procedures achieves the desired appearance
with minimal discomfort, low cost, predictability, and excellent
success rates.16 There is also a very high rate of patient
satisfaction associated with these treatment methods.17
The first generation of dental composites was chemically
polymerized, very brittle, and only suitable for restoring anterior
teeth. These composites were usually quartz-filled, required
hand mixing of self-curing pastes that only came in 4 shades,
and were difficult to work with. Wear and fracture resistance
were low, the materials did not meet compressive and tensile
force requirements, were difficult to polish, and exhibited high
surface roughness.18
Even as they evolved, direct composites were, at first,
Continuing Education
Minimally Invasive Cure for Life-Long Discoloration
In fact, several studies were
conducted to identify the amount
of volumetric shrinkage suprananohybrid composites undergo
due to polymerization, and the
results illustrate that the rate of
volumetric shrinkage is statistically low (ie, about 1.3% to
Figure 2. Close-up view, following in-office tooth
2%).23,24 These composites also Figure 1. Preoperative view exhibiting the severe
whitening.
tooth discoloration.
bond well to all tooth surfaces. In
a study testing microtensile bond
strength of an experimental
adhesive between dentin and
different restorative materials,
the suprananohybrid performed
well, demonstrating a good microtensile bond to dentin with
strength of 51.0 MPa.25
Figure 4. The proposed enamel composite shades
Aesthetically, due to the Figure 3. The proposed dentin composite shades
were previewed.
were previewed.
submicron particle size of the filler,
these composites can be polished very quickly to a high gloss
would have allowed for the subsequent opportunity to
that is maintained for years and enhanced using a systematic
consider prosthodontic treatments in the future. The patient
finishing and polishing kit (eg, Shofu Dental).
indicated that she wanted to pursue a minimally invasive
option and wanted to understand what could be possible.
CASE REPORT
During the aesthetic evaluation, it was noted that the
A female patient in her 40s presented for a consultation to
patient displayed a full smile. However, it was determined that
discuss treatment options for correcting the appearance of
her aesthetic concerns could be addressed with a
her severely discolored teeth (Figure 1). A comprehensive
combination of in-office whitening (eg, BriteSmile) and direct
examination was performed that included an aesthetic
composite restorations (Estelite Sigma Quick) in a minimally
evaluation.
invasive, reversible, and repairable way. Her dental condition
She had been afflicted with such discoloration and
was good, so she was scheduled for a hygiene appointment
aesthetic dilemma since age 13 years that affected her
and for tooth whitening.
psychologically. However, despite the social stigma she
endured due to the tooth discoloration, she was reluctant to
Clinical Treatment
undergo the more aggressive treatments (eg, all-ceramic
Fourteen days after completing the tooth whitening
crowns, veneers) that previous dentists had recommended.
procedure (Figure 2), the patients tooth color could be
As she described the prosthodontic solutions that had
managed in the labial enamel, with minimal tooth preparation
been suggested to her, it was clear that her previous
required. The composite selected for the case was a
consultations did not include discussion about tooth structure
suprananohybrid (Estelite Sigma Quick), since this material
removal or tooth shade. Additionally, it was apparent that there
would provide the simplified shade selection necessary to
was a lack of clarity within the profession regarding minimally
cover the tooth space using one or 2 shades, making it ideal
invasive alternatives for enhancing her smile at this time that
for this type of everyday dentistry.22 Yet, it would enable
Continuing Education
Minimally Invasive Cure for Life-Long Discoloration
Figure 5. Areas of color concerns and zones
of high chroma areas were outlined.
Figure 6. A minimally invasive preparation
was undertaken using a No. 331-0913
diamond (Shofu Dental).
Figure 7. Bevels were placed using a No.
7903-0939 diamond (Shofu Dental).
Figure 8. A selective-etch technique was
used.
Figure 9. A dentin bonding agent was
placed according to the manufacturers
instructions (Bond Force [Tokuyama Dental
America]).
Figure 10. The initial dentin composite layer
in shade A1 was applied and sculpted onto
tooth No. 8 (Estelite Sigma Quick [Tokuyama
Dental America]).
Figure 11. The A1 dentin composite was
then placed on tooth No. 9.
Figure 12. The final shade CE composite
enamel layer was placed on tooth No. 8.
Figure 13. Pencil lines were drawn to
identify necessary line angles.
effective shade matching with the adjacent natural dentition,
maximization of the selected shades for recreating the tooths
inherent hue, chroma and value, and therefore realization of
aesthetic principles.
During the restorative appointment, the proposed dentin
composite shades (eg, B1 on the left, A1 on the right) were
previewed on the unprepared teeth (Figure 3). Shade A1
was selected. Then proposed enamel composite shades
(eg, WE on the left, CE on right) were previewed (Figure 4),
and shade CE was selected.
Teeth Nos. 8 and 9 were evaluated to outline areas of
concern regarding color and zones of high chroma areas
(Figure 5), after which a minimally invasive preparation was
begun using a No. 331-0913 diamond (Shofu Dental)
(Figure 6). Initially, the preparation demonstrated areas of
high chroma. Bevels were placed using a No. 7903-0939
diamond (Shofu Dental) to complete the preparation
(Figure 7).
Because a small area of the preparation extended into
dentin, a selective-etch technique was used (Figure 8). The
etchant was then rinsed thoroughly, and the teeth were dried.
Next, a dentin bonding agent (Bond Force [Tokuyama Dental
America]) was placed according to the manufacturers
instructions (Figure 9) and light-cured.
Using freehand direct composite artistry, the initial
dentin composite layer (Estelite Sigma Quick) in shade A1
Continuing Education
Minimally Invasive Cure for Life-Long Discoloration
Figure 14. The line angles were modified
with a disc.
Figure 15. A CTF yellow Robot carbide
finisher (Shofu Dental) was used to create
the secondary anatomy.
Figure 16. To create the tertiary anatomy, a
Dura-Green Stone No. 1211252 (Shofu
Dental) was used.
Figure 17. An initial polish was applied to
the restorations using One Gloss (Shofu
Dental).
Figure 18. A buffing disc (Super Snap
Buff Disc [Shofu Dental]) moistened with
water was used to continue polishing the
restorations.
Figure 19. The restorations achieved their
final luster using a buffing disc and polishing
paste (Direct Dia [Shofu Dental]).
was applied and sculpted onto tooth No. 8, then light-cured
(Figure 10). The A1 dentin composite was then placed on
tooth No. 9 (Figure 11) in a similar manner and light-cured. A
matrix (Omni Band [Ultradent Products]) was placed, after
which the final CE shade composite enamel layer was placed
on tooth No. 8 and light-cured (Figure 12). The CE composite
enamel layer was then applied to tooth No. 9 and light-cured.
Pencil lines were drawn to identify necessary line angles
and facilitate construction of primary anatomy (Figure 13).
These line angles were then modified in the restorations using
a disc (Super Snap [Shofu Dental]) (Figure 14). Next, a CTF
yellow Robot carbide finisher (Shofu Dental) was used to
create the secondary anatomy (Figure 15). Subsequently, a
Dura-Green Stone No. 1211252 (Shofu Dental) was used to
create the tertiary anatomy (Figure 16).
The restorations were initially polished using One Gloss
(Shofu Dental) (Figure 17). A buffing disc (Super Snap Buff
Disc [Shofu Dental]) moistened with water continued the
polishing sequence to create a prelustered surface (Figure 18).
The restorations achieved their final luster through the use
of a buffing disc (Super Snap Buff Disc) and polishing paste
(Direct Dia [Shofu Dental]) (Figure 19).
Figure 20. Final close-up
postoperative view of the
patients direct composite
restorations. Note the
dramatically enhanced
appearance of her smile,
accomplished with a
minimally invasive
protocol.
The handling, physical, and visual properties
demonstrated in the selected composite (Estelite Sigma
Quick) represent the evolution of direct composites to their
currently advanced state, which enabled the use of only 2
ideal dentin and enamel shades for creating the chameleon
effect necessary for the restorations to appear naturally
aesthetic (Figure 20).
IN SUMMARY
The in-office whitening and suprananohybrid composite,
combined with the dentists full understanding of the
transformational possibilities of responsible aesthetics,
essentially cured this patients discolored smile, with
which she had been afflicted all her life.
Continuing Education
Minimally Invasive Cure for Life-Long Discoloration
14. LeSage BP. Are you treating planned cases or treating
teeth to stay busy? Dent Today. 2012;31:76-78.
15. LeSage BP. Aesthetic anterior composite restorations:
a guide to direct placement. Dent Clin North Am.
2007;51:359-378, viii.
16. Dietschi D. Optimizing smile composition and esthetics
with resin composites and other conservative esthetic
procedures. Eur J Esthet Dent. 2008;3:14-29.
17. Kelleher MG, Djemal S, Al-Khayatt AS, et al. Bleaching
and bonding for the older patient. Dent Update.
2011;38:294-303.
18. Small BW. Direct resin composites for 2002 and
beyond. Gen Dent. 2002;50:30-33.
19. Milnar FJ. The evolution of direct composites.
Compendium. 2011;32:79-81.
20. Margeas R. Composite materials: advances lead to
ease of use, better performance. Compendium.
2013;34:370.
21. Suzuki S. Does the wear resistance of packable
composite equal that of dental amalgam? J Esthet
Restor Dent. 2004;16:355-365.
22. Tokuyama Estelite Sigma Quick.
www.dentalaegis.com/id/2012/08/tokuyama-estelitesigma-quick. Accessed July 12, 2013.
23. Kaga S, Fusejima F, Kumagai T, et al. Polymerization
shrinkage ratio of various resin composites. J Dent
Res. 2009;88(special issue A). Abstract 2441.
24. Beck P, Lindsey M, Michelson C, et al. Polymerization
shrinkage of nine highly-filled composite materials. J
Dent Res. 2011;90(special issue A). Abstract 606.
25. Hirata K, Armstrong S, Qian F. Material compatibility of
self-etching self-cure 1-step adhesive when dentin
bonding. J Dent Res. 2012;91(special issue A).
Abstract 225.
REFERENCES
1. Hattab FN, Qudeimat MA, al-Rimawi HS. Dental
discoloration: an overview. J Esthet Dent.
1999;11:291-310.
2. Sulieman M. An overview of tooth discoloration:
extrinsic, intrinsic and internalized stains. Dent Update.
2005;32:463-471.
3. Watts A, Addy M. Tooth discolouration and staining: a
review of the literature. Br Dent J. 2001;190:309-316.
4. Dunn WJ, Murchison DF, Broome JC. Esthetics:
patients perceptions of dental attractiveness. J
Prosthodont. 1996;5:166-171.
5. Friedman S, Rotstein I, Libfeld H, et al. Incidence of
external root resorption and esthetic results in 58
bleached pulpless teeth. Endod Dent Traumatol.
1988;4:23-26.
6. Tam L. The safety of home bleaching techniques. J
Can Dent Assoc. 1999;65:453-455.
7. Setien VJ, Roshan S, Nelson PW. Clinical
management of discolored teeth. Gen Dent.
2008;56:294-300.
8. Taleghani M, Wathen WF. Porcelain laminate veneers
in the adult dentition. Tex Dent J. 2006;123:928-936.
9. Ibarra G, Johnson GH, Geurtsen W, et al. Microleakage
of porcelain veneer restorations bonded to enamel and
dentin with a new self-adhesive resin-based dental
cement. Dent Mater. 2007;23:218-225.
10. Sadowsky SJ. An overview of treatment considerations
for esthetic restorations: a review of the literature. J
Prosthet Dent. 2006;96:433-442.
11. Feigenbaum N. The challenge of cost restrictions in
smile design. Pract Periodontics Aesthet Dent.
1991;3:41-44.
12. Cohen SM, Fiske J, Newton JT. The impact of dental
anxiety on daily living. Br Dent J. 2000;189:385-390.
13. Milnar FJ. Incorporating flowable composites into the
minimally invasive treatment sequence for aesthetic
enhancement. Pract Proced Aesthet Dent. 2006;18:65-70.
Continuing Education
Minimally Invasive Cure for Life-Long Discoloration
POST EXAMINATION INFORMATION
POST EXAMINATION QUESTIONS
To receive continuing education credit for participation in
this educational activity you must complete the program
post examination and answer 6 out of 8 questions correctly.
1. Conditions that can often cause permanent
discoloration include dental fluorosis, plaque
calcifications, and the prenatal use of tetracycline.
a. True
Traditional Completion Option:
You may fax or mail your answers with payment to Dentistry
Today (see Traditional Completion Information on following
page). All information requested must be provided in order
to process the program for credit. Be sure to complete your
Payment, Personal Certification Information, Answers,
and Evaluation forms. Your exam will be graded within 72
hours of receipt. Upon successful completion of the postexam (answer 6 out of 8 questions correctly), a letter of
completion will be mailed to the address provided.
b. False
2. Science has already established that dentofacial
attractiveness rarely affects the psychosocial well
being of an individual.
a. True
b. False
3. Bleaching procedures using hydrogen peroxide or
carbamide peroxide have been proven effective and
safe, but there are reports of adverse reactions such
as cervical root resorption and post-treatment
sensitivity that can last from a few hours up to
several days.
Online Completion Option:
Use this page to review the questions and mark your
answers. Return to dentalcetoday.com and sign in. If you
have not previously purchased the program, select it from
the Online Courses listing and complete the online
purchase process. Once purchased the program will be
added to your User History page where a Take Exam link
will be provided directly across from the program title.
Select the Take Exam link, complete all the program
questions and Submit your answers. An immediate grade
report will be provided. Upon receiving a passing grade,
complete the online evaluation form. Upon submitting
the form, your Letter Of Completion will be provided
immediately for printing.
a. True
b. False
4. Porcelain veneers have been a preferred and
effective option for many patients to treat discolored
teeth.
a. True
b. False
5. All-ceramic crowns are another treatment option for
masking discolored teeth.
a. True
b. False
6. A patients fear/anxiety level pertaining to certain
procedures like aggressive tooth preparation should
not be considered as a reason for refusing treatment.
General Program Information:
Online users may log in to dentalcetoday.com any time in
the future to access previously purchased programs and
view or print letters of completion and results.
a. True
b. False
7. Direct composite is considered among clinicians to
be the least invasive and most conservative method
to restore aesthetically displeasing or diseased teeth
to stable color, form, and function.
This CE activity was not developed in accordance with
AGD PACE or ADA CERP Standards.
CEUs for this activity will not be accepted by the AGD
for MAGD/FAGD credit.
a. True
b. False
8. The newest version of direct composite, suprananohybrids demonstrate the combination of
characteristics that dentists have desired from
composites for 30 years.
a. True
b. False
Continuing Education
Minimally Invasive Cure for Life-Long Discoloration
PROGRAM COMPLETION INFORMATION
PERSONAL CERTIFICATION INFORMATION:
If you wish to purchase and complete this activity
traditionally (mail or fax) rather than online, you must
provide the information requested below. Please be sure to
select your answers carefully and complete the evaluation
information. To receive credit you must answer 6 of the 8
questions correctly.
Last Name
First Name
Profession / Credentials
Suite or Apartment Number
TRADITIONAL COMPLETION INFORMATION:
Mail or fax this completed form with payment to:
City
Dentistry Today
State
Zip Code
Daytime Telephone Number With Area Code
Department of Continuing Education
100 Passaic Avenue
Fairfield, NJ 07004
Fax Number With Area Code
Fax: 973-882-3622
E-mail Address
PAYMENT & CREDIT INFORMATION:
ANSWER FORM: VOLUME 32 NO. 10 PAGE 100
Examination Fee: $40.00 Credit Hours: 2
Please check the correct box for each question below.
1. o a. True
o b. False
5. o a. True
o b. False
2. o a. True
o b. False
6. o a. True
o b. False
I have enclosed a check or money order.
3. o a. True
o b. False
7. o a. True
o b. False
I am using a credit card.
4. o a. True
o b. False
8. o a. True
o b. False
Note: There is a $10 surcharge to process a check drawn on
any bank other than a US bank. Should you have additional
questions, please contact us at (973) 882-4700.
License Number
Street Address
Complete online at: dentalcetoday.com
(PLEASE PRINT CLEARLY OR TYPE)
My Credit Card information is provided below.
o American Express o Visa o MC o Discover
Please provide the following
PROGRAM EVAUATION FORM
Please complete the following activity evaluation questions.
(please print clearly):
Rating Scale: Excellent = 5 and Poor = 0
Course objectives were achieved.
Exact Name on Credit Card
Content was useful and benefited your clinical practice.
Review questions were clear and relevant to the editorial.
/
Credit Card #
Illustrations and photographs were clear and relevant.
Expiration Date
Written presentation was informative and concise.
How much time did you spend reading the activity and
completing the test?
Signature
What aspect of this course was most helpful and why?
This CE activity was not developed in accordance with
AGD PACE or ADA CERP Standards.
CEUs for this activity will not be accepted by the AGD
for MAGD/FAGD credit.
What topics interest you for future Dentistry Today CE courses?
Вам также может понравиться
- Esthetic Management of Anterior Teeth with GiomerДокумент7 страницEsthetic Management of Anterior Teeth with GiomerFoysal Sirazee100% (1)
- Policy On The Use of Dental Bleaching For Child and Adolescent PatientsДокумент4 страницыPolicy On The Use of Dental Bleaching For Child and Adolescent PatientsFebriani SerojaОценок пока нет
- Restoring Endodontically Treated TeethДокумент20 страницRestoring Endodontically Treated Teethlishenwong100% (1)
- Dental Bleaching - A Review of The LiteratureДокумент6 страницDental Bleaching - A Review of The LiteratureMissyОценок пока нет
- Recommended Pediatric Dental RestorationsДокумент9 страницRecommended Pediatric Dental RestorationsentistdeОценок пока нет
- P BleachingДокумент4 страницыP Bleachingpooja singhОценок пока нет
- The Esthetic Option of Veneers: Section 9Документ21 страницаThe Esthetic Option of Veneers: Section 9mandakinimohanОценок пока нет
- PEAK Restoration of The Endodontically Treated Tooth PDFДокумент20 страницPEAK Restoration of The Endodontically Treated Tooth PDFana9025100% (1)
- Guideline On Pediatric Restorative Dentistry: Originating Committee Review Council Adopted RevisedДокумент7 страницGuideline On Pediatric Restorative Dentistry: Originating Committee Review Council Adopted RevisedEduardo SánchezОценок пока нет
- Vital Tooth Bleaching An Update by StrasslerДокумент12 страницVital Tooth Bleaching An Update by StrassleranjozzОценок пока нет
- Restorative Dentistry for ChildrenДокумент62 страницыRestorative Dentistry for Childrensamar yousif mohamedОценок пока нет
- Minimumthickness Anteriorporcelain Restorations: Gary M. RadzДокумент18 страницMinimumthickness Anteriorporcelain Restorations: Gary M. RadzElize MachadoОценок пока нет
- Re-Establishing Esthetics of Uorosis-Stained Teeth Using Enamel Microabrasion and Dental Bleaching TechniquesДокумент10 страницRe-Establishing Esthetics of Uorosis-Stained Teeth Using Enamel Microabrasion and Dental Bleaching TechniquesCeida Lopez CastillaОценок пока нет
- Zirconia Crowns Improve Patient SmileДокумент4 страницыZirconia Crowns Improve Patient SmileWiwin Nuril FalahОценок пока нет
- Choosing between bonded composite or amalgam for Class II cavityДокумент7 страницChoosing between bonded composite or amalgam for Class II cavityMedoxОценок пока нет
- Minimal Invasive Microscopic Tooth Preparation in Esthetic Restoration, A Specialist Consensus PDFДокумент11 страницMinimal Invasive Microscopic Tooth Preparation in Esthetic Restoration, A Specialist Consensus PDFBelen AntoniaОценок пока нет
- Pin-Retained Restoration With Resin Bonded Composite of A Badly Broken ToothДокумент3 страницыPin-Retained Restoration With Resin Bonded Composite of A Badly Broken ToothIOSRjournalОценок пока нет
- Direct Laminate Veneers With Resin Composites: Two Case Reports With Five-Year Follow-UpsДокумент7 страницDirect Laminate Veneers With Resin Composites: Two Case Reports With Five-Year Follow-UpsBarbulescu Anca DianaОценок пока нет
- Non Preparation VeneersДокумент24 страницыNon Preparation VeneersastinejenniferОценок пока нет
- Aapd EnameloplastyДокумент9 страницAapd EnameloplastydrkameshОценок пока нет
- PEMOLISAN KOMPOSIT MENURUNKAN DISKOLORASI NANOFILLERДокумент6 страницPEMOLISAN KOMPOSIT MENURUNKAN DISKOLORASI NANOFILLERFransisca FeliciaОценок пока нет
- Principles of Composite Restoration GuideДокумент9 страницPrinciples of Composite Restoration GuideBari AakashОценок пока нет
- Ceramic Veneers Treatment PlanningДокумент11 страницCeramic Veneers Treatment PlanningheycoolalexОценок пока нет
- Class Four from Cavity to SmileДокумент18 страницClass Four from Cavity to SmileAbdullah HassanienОценок пока нет
- Enamel Hypoplasia or AAДокумент4 страницыEnamel Hypoplasia or AArahul sharmaОценок пока нет
- Esthetic Inlays and Onlays: A Conservative Alternative for Posterior TeethДокумент13 страницEsthetic Inlays and Onlays: A Conservative Alternative for Posterior TeethrahmaОценок пока нет
- G RestorativeДокумент8 страницG RestorativeEllizabeth LilantiОценок пока нет
- Aapd Guidelines - Restorative Dentistry PDFДокумент8 страницAapd Guidelines - Restorative Dentistry PDFMaqbul AlamОценок пока нет
- FAQ-Bleaching Van HaywoodДокумент14 страницFAQ-Bleaching Van HaywoodBasil AlОценок пока нет
- Ultradent Catalogue ANZ 2013Документ134 страницыUltradent Catalogue ANZ 2013Dorin PupezОценок пока нет
- PS9 Restorative Materials - PS9.19.0Документ6 страницPS9 Restorative Materials - PS9.19.0Ana María ReyesОценок пока нет
- Restoring Endodontically Treated TeethДокумент31 страницаRestoring Endodontically Treated TeethLuis Alberto Carpio MorenoОценок пока нет
- Format JurnalДокумент14 страницFormat JurnalAnonymous HtTD0BОценок пока нет
- 322 1403 1 PB PDFДокумент2 страницы322 1403 1 PB PDFAdityaОценок пока нет
- Pit and Fissure Sealants in Pediatric Dentistry: April 2019Документ8 страницPit and Fissure Sealants in Pediatric Dentistry: April 2019pdg 2020Оценок пока нет
- Restoration of The Endodontically Treated Posterior ToothДокумент16 страницRestoration of The Endodontically Treated Posterior ToothGraciela BarrОценок пока нет
- Tooth Whitening Research UpdateДокумент7 страницTooth Whitening Research UpdateDaniel VelezОценок пока нет
- Longevity of RestorationsДокумент12 страницLongevity of RestorationsmusaabsiddiquiОценок пока нет
- Aapd Guidelines - Restorative DentistryДокумент8 страницAapd Guidelines - Restorative DentistrymahmoudОценок пока нет
- Teori Pembersihan Gigi Tiruan - EngДокумент5 страницTeori Pembersihan Gigi Tiruan - EngZuhra An Nisa SamudraОценок пока нет
- Direct Laminate Veneers With Resin Composites: Two Case Reports With Five-Year Follow-UpsДокумент3 страницыDirect Laminate Veneers With Resin Composites: Two Case Reports With Five-Year Follow-UpsBarbulescu Anca DianaОценок пока нет
- Droplet DesignДокумент72 страницыDroplet DesignArvindОценок пока нет
- Adhesivos UniversalesДокумент9 страницAdhesivos Universalesmaria posadaОценок пока нет
- Acondicionamiento, Adhesión y Cementado de Aparatología Ortodóncica en Dientes Con Alteraciones Del Esmalte. Revisión de LiteraturaДокумент10 страницAcondicionamiento, Adhesión y Cementado de Aparatología Ortodóncica en Dientes Con Alteraciones Del Esmalte. Revisión de Literaturaruqoyah022Оценок пока нет
- Veneer Series PT 1Документ6 страницVeneer Series PT 1Cornelia Gabriela OnuțОценок пока нет
- Tooth Whitening: Efficacy, Effects and Biological SafetyДокумент6 страницTooth Whitening: Efficacy, Effects and Biological SafetyAndykaYayanSetiawanОценок пока нет
- Ayad ResincompositepolyethylenefiberreinforcementДокумент5 страницAyad ResincompositepolyethylenefiberreinforcementPaulette Sarmiento RosalesОценок пока нет
- Coelho de Souza2015Документ20 страницCoelho de Souza2015kelly johanna quintero arevaloОценок пока нет
- Dr. Shoeb MujawarДокумент4 страницыDr. Shoeb Mujawarmeena syedОценок пока нет
- Conservative ZirconiaДокумент10 страницConservative ZirconiaTareq Al-sayedОценок пока нет
- Biomimetic AllemanДокумент6 страницBiomimetic AllemanAlireza RaieОценок пока нет
- The Biomimetic Concept (8 Online Lessons)Документ14 страницThe Biomimetic Concept (8 Online Lessons)Francesca MocanuОценок пока нет
- Conservative Esthetic Procedures: Part 2Документ9 страницConservative Esthetic Procedures: Part 2Dt omarОценок пока нет
- Esthetic Oral Rehabilitation with Veneers: A Guide to Treatment Preparation and Clinical ConceptsОт EverandEsthetic Oral Rehabilitation with Veneers: A Guide to Treatment Preparation and Clinical ConceptsRichard D. TrushkowskyОценок пока нет
- DtceДокумент10 страницDtceKranti PrajapatiОценок пока нет
- YTC Initial ChecklistДокумент3 страницыYTC Initial ChecklistBrian KohlerОценок пока нет
- (Ebook - Psychology) The World of Subconscious MindДокумент315 страниц(Ebook - Psychology) The World of Subconscious MindKranti PrajapatiОценок пока нет
- CBCT Imaging's Insight Into Endodontic Retreatment Success - Dentistry TodayДокумент7 страницCBCT Imaging's Insight Into Endodontic Retreatment Success - Dentistry TodayKranti PrajapatiОценок пока нет
- Advances in Biomechanical Preparation - Dentistry TodayДокумент5 страницAdvances in Biomechanical Preparation - Dentistry TodayKranti PrajapatiОценок пока нет
- Combine Each Pair of Sentences With The Conjunction in Parenthesis To Make A New SentenceДокумент3 страницыCombine Each Pair of Sentences With The Conjunction in Parenthesis To Make A New SentenceKranti PrajapatiОценок пока нет
- Past TenseДокумент6 страницPast TenseKranti PrajapatiОценок пока нет
- Clinical Applications - Apical Negative Pressure Irrigation - Dentistry TodayДокумент7 страницClinical Applications - Apical Negative Pressure Irrigation - Dentistry TodayKranti PrajapatiОценок пока нет
- AB Amaris DR Marques Australasian Dentist June 2011Документ3 страницыAB Amaris DR Marques Australasian Dentist June 2011Kranti PrajapatiОценок пока нет
- DTCE Weeks Oct 214 FNLДокумент8 страницDTCE Weeks Oct 214 FNLKranti PrajapatiОценок пока нет
- Creating Well-Obturated Canals - The Use of Warm Vertical Condensation Techniques - Dentistry TodayДокумент9 страницCreating Well-Obturated Canals - The Use of Warm Vertical Condensation Techniques - Dentistry TodayKranti PrajapatiОценок пока нет
- An Improved Quadrant Class II Composite Technique - Dentistry TodayДокумент6 страницAn Improved Quadrant Class II Composite Technique - Dentistry TodayKranti PrajapatiОценок пока нет
- Dental Clinics of North America Appendix 485 486Документ2 страницыDental Clinics of North America Appendix 485 486Kranti PrajapatiОценок пока нет
- Monetary Policy Securities Market 2074Документ2 страницыMonetary Policy Securities Market 2074Kranti PrajapatiОценок пока нет
- An Improved Glass Ionomer Restorative System for Class I and II RestorationsДокумент7 страницAn Improved Glass Ionomer Restorative System for Class I and II RestorationsKranti PrajapatiОценок пока нет
- Erratum IxДокумент3 страницыErratum IxKranti PrajapatiОценок пока нет
- Monetary Policy Securities Market 2074Документ2 страницыMonetary Policy Securities Market 2074Kranti PrajapatiОценок пока нет
- Dental Clinics of North America Sleep Medicine in Dentistry Xi XiiiДокумент3 страницыDental Clinics of North America Sleep Medicine in Dentistry Xi XiiiKranti PrajapatiОценок пока нет
- 1 s2.0 S0011853213000438 MainДокумент2 страницы1 s2.0 S0011853213000438 MainKranti PrajapatiОценок пока нет
- Dental Clinics of North America Medical Disorders Impacted by Obstructive Sleep Apnea 373 386Документ14 страницDental Clinics of North America Medical Disorders Impacted by Obstructive Sleep Apnea 373 386Kranti PrajapatiОценок пока нет
- Diagnostic Imaging For Temporomandibular Disorders and Orofacial Pain 2013 Dental Clinics of North AmericaДокумент14 страницDiagnostic Imaging For Temporomandibular Disorders and Orofacial Pain 2013 Dental Clinics of North AmericaazizОценок пока нет
- Dental Clinics of North America Use of Portable Monitoring For Sleep Disordered Breathing Treated With An Oral Appliance 445 452Документ8 страницDental Clinics of North America Use of Portable Monitoring For Sleep Disordered Breathing Treated With An Oral Appliance 445 452Kranti PrajapatiОценок пока нет
- 1 s2.0 S0011853213000347 MainДокумент15 страниц1 s2.0 S0011853213000347 MainKranti PrajapatiОценок пока нет
- 1 s2.0 S001185321300030X MainДокумент27 страниц1 s2.0 S001185321300030X MainKranti PrajapatiОценок пока нет
- Preface: Scott S. de Rossi, DMD David A. Sirois, DMD, PHD EditorsДокумент2 страницыPreface: Scott S. de Rossi, DMD David A. Sirois, DMD, PHD EditorsKranti PrajapatiОценок пока нет
- Bonnick - 2011 - Dental Clinics of North America PDFДокумент14 страницBonnick - 2011 - Dental Clinics of North America PDFKranti PrajapatiОценок пока нет
- 1 s2.0 S0011853213000438 MainДокумент2 страницы1 s2.0 S0011853213000438 MainKranti PrajapatiОценок пока нет
- Preface Oralandcraniofacialimplant Reconstructionasfoundation ForrestorativedentistryДокумент1 страницаPreface Oralandcraniofacialimplant Reconstructionasfoundation ForrestorativedentistryKranti PrajapatiОценок пока нет
- Trushkowsky - 2011 - Dental Clinics of North America PDFДокумент10 страницTrushkowsky - 2011 - Dental Clinics of North America PDFKranti PrajapatiОценок пока нет
- 2011 4 PDFДокумент23 страницы2011 4 PDFKranti PrajapatiОценок пока нет
- CH 22 Solutions ManualДокумент22 страницыCH 22 Solutions Manuallmbrn0415Оценок пока нет
- Morpho Full Fix 2Документ9 страницMorpho Full Fix 2Dayu AnaОценок пока нет
- Anticipate Problems Before They Emerge: White PaperДокумент7 страницAnticipate Problems Before They Emerge: White PaperYotsapol KantaratОценок пока нет
- MEC332-MA 3rd Sem - Development EconomicsДокумент9 страницMEC332-MA 3rd Sem - Development EconomicsRITUPARNA KASHYAP 2239239Оценок пока нет
- Internal auditing multiple choice questionsДокумент4 страницыInternal auditing multiple choice questionsSantos Gigantoca Jr.Оценок пока нет
- Resistance and ResisivityДокумент2 страницыResistance and ResisivityDeddy KismanaОценок пока нет
- Polymer Science: Thermal Transitions in PolymersДокумент20 страницPolymer Science: Thermal Transitions in Polymerstanveer054Оценок пока нет
- Technical Bro A4 UK LR NEW v2Документ45 страницTechnical Bro A4 UK LR NEW v2Roxana NegoitaОценок пока нет
- LP IV Lab Zdvzmanual Sem II fbsccAY 2019-20z 20-ConvxvzzertedДокумент96 страницLP IV Lab Zdvzmanual Sem II fbsccAY 2019-20z 20-ConvxvzzertedVikas GuptaОценок пока нет
- LTC2410 Datasheet and Product Info - Analog DevicesДокумент6 страницLTC2410 Datasheet and Product Info - Analog DevicesdonatoОценок пока нет
- Applied Physics Mini Launcher Lab ReportДокумент12 страницApplied Physics Mini Launcher Lab ReportTalharashid RamzanОценок пока нет
- ECE 4400 Performance Analysis Local Computer Networks HomeworkДокумент2 страницыECE 4400 Performance Analysis Local Computer Networks HomeworkNguyen Phi HungОценок пока нет
- Nelson Sanchez GE Module October 2020Документ92 страницыNelson Sanchez GE Module October 2020Nneg Gray0% (1)
- Pankaj Screener 10 Oct 2014Документ127 страницPankaj Screener 10 Oct 2014Sadul Singh Naruka100% (1)
- EOD Stanags Overview April 2021Документ12 страницEOD Stanags Overview April 2021den mas paratate leo egoОценок пока нет
- Solution Aid-Chapter 01Документ21 страницаSolution Aid-Chapter 01Vishal ChintapalliОценок пока нет
- Fire Pump System Test ReportДокумент12 страницFire Pump System Test Reportcoolsummer1112143100% (2)
- ccpc15 Supportive and Preventive WorkbookДокумент30 страницccpc15 Supportive and Preventive WorkbookJeremy HamptonОценок пока нет
- Operation Manual 11-3000psi Shear Ram BopДокумент30 страницOperation Manual 11-3000psi Shear Ram BopBoedi SyafiqОценок пока нет
- IJRP 2018 Issue 8 Final REVISED 2 PDFДокумент25 страницIJRP 2018 Issue 8 Final REVISED 2 PDFCarlos VegaОценок пока нет
- A Laboratory Experiment in Crystals and Crystal Model Building ObjectivesДокумент7 страницA Laboratory Experiment in Crystals and Crystal Model Building ObjectivesrajaaОценок пока нет
- Informed Consent: Ghaiath M. A. HusseinДокумент26 страницInformed Consent: Ghaiath M. A. HusseinDocAxi Maximo Jr AxibalОценок пока нет
- Open MPДокумент30 страницOpen MPmacngocthanОценок пока нет
- 4MB0 02R Que 20160609 PDFДокумент32 страницы4MB0 02R Que 20160609 PDFakashОценок пока нет
- JKR Specs L-S1 Addendum No 1 LED Luminaires - May 2011Документ3 страницыJKR Specs L-S1 Addendum No 1 LED Luminaires - May 2011Leong KmОценок пока нет
- Explore Spanish Lesson Plan - AnimalsДокумент8 страницExplore Spanish Lesson Plan - Animalsapi-257582917Оценок пока нет
- Makerwys - Exe Version 4.891: by Pete Dowson © 2019 InstructionsДокумент11 страницMakerwys - Exe Version 4.891: by Pete Dowson © 2019 InstructionsRafrol RamonОценок пока нет
- Brochure HorticultureДокумент46 страницBrochure HorticulturezulfiqaralimalikОценок пока нет
- LAU Paleoart Workbook - 2023Документ16 страницLAU Paleoart Workbook - 2023samuelaguilar990Оценок пока нет
- WP1019 CharterДокумент5 страницWP1019 CharternocnexОценок пока нет