Академический Документы
Профессиональный Документы
Культура Документы
$116 SMFM Abstracts
Загружено:
Sheila Regina Tiza0 оценок0% нашли этот документ полезным (0 голосов)
23 просмотров1 страницаThis document contains 4 summaries of medical journal articles on topics related to pregnancies and fetal outcomes:
1) The first article finds that pregnancies resulting from assisted reproduction techniques like IVF carry higher risks for adverse outcomes compared to pregnancies not using these techniques. These risks include early bleeding, hypertension, gestational diabetes, prematurity, and growth restriction.
2) The second article examines the relationship between maternal age and risk of fetal death in twin gestations. It finds young maternal age increases this risk similarly to other common conditions screened for like hypertension and diabetes.
3) The third article measures levels of the drug metoclopramide excreted in breastmilk of women delivering preterm infants. It
Исходное описание:
jurnal obstetri
Оригинальное название
American Journal of Obstetrics and Gynecology Volume 185 Issue 6-Supp-S 2001 [Doi 10.1016%2Fs0002-9378%2801%2980163-0] Ronit Beck-Fruchter; Yasser Hujeirat; Stavit Shalev; Zohar Nahum -- 128 Third-tri
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документThis document contains 4 summaries of medical journal articles on topics related to pregnancies and fetal outcomes:
1) The first article finds that pregnancies resulting from assisted reproduction techniques like IVF carry higher risks for adverse outcomes compared to pregnancies not using these techniques. These risks include early bleeding, hypertension, gestational diabetes, prematurity, and growth restriction.
2) The second article examines the relationship between maternal age and risk of fetal death in twin gestations. It finds young maternal age increases this risk similarly to other common conditions screened for like hypertension and diabetes.
3) The third article measures levels of the drug metoclopramide excreted in breastmilk of women delivering preterm infants. It
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
23 просмотров1 страница$116 SMFM Abstracts
Загружено:
Sheila Regina TizaThis document contains 4 summaries of medical journal articles on topics related to pregnancies and fetal outcomes:
1) The first article finds that pregnancies resulting from assisted reproduction techniques like IVF carry higher risks for adverse outcomes compared to pregnancies not using these techniques. These risks include early bleeding, hypertension, gestational diabetes, prematurity, and growth restriction.
2) The second article examines the relationship between maternal age and risk of fetal death in twin gestations. It finds young maternal age increases this risk similarly to other common conditions screened for like hypertension and diabetes.
3) The third article measures levels of the drug metoclopramide excreted in breastmilk of women delivering preterm infants. It
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 1
December 2001
A m J Obstet Gynecol
$116 SMFM Abstracts
125
PREGNANCIES AFI'ER ASSISTED REPRODUCTION--HIGHER RISK FOR
ADVERSE O U T C O M E UWE LANG t, J U L I O HERRERO ], A BECK l, T
STALF2, C MEHNERT 2, H GIPS2; lJus tus-Liebig-Univer sitar Giessen, Obstetrics
and Gynecology, Giessen, Hessen; 2Institute of Reproductive Medicine Giessen,
IVF, Giessen, Hessen
OBJECTIVE: Pregnancies after assisted r e p r o d u c t i o n (IVF/ICSI) are
considered to be risk pregnancies. The goal of our study was to assess whether
a n d in which aspects the course of these pregnancies a n d perinatal outcome
after [VF differ from pregnancies not conceived through assisted reproduction.
STUDY DESIGN: 406 pregnancies after IVF between 1994 a n d 1999 were
examined. Data were c o m p a r e d with those of 338,737 patients without any
form of sterility treatment from the statewide perinatal survey of the state of
Hesse/ Germany (HEPE) for the same period. Additionally, within the IYT
group, subgroups for PCO, hyperstimulation a n d other factors were formed
a n d evaluated.
RESULTS: 300 (73.9%) o f the p r e g n a n c i e s after 1VF were singleton
pregnancies, 97 (23.9%) twin p r e g n a n c i e s a n d 9 (2.2%) triplets. After
grouping HEPE data for age a n d parity to match the IVF group, in singleton
pregnancies we f o u n d a high late of early vaginal bleeding (1VF 15.7%; HEPE
2.5%; P < .05), PIH (IVF: 6.3 %; HEPE 2.1%; P < .05), gestational diabetes (IVF:
4.0%; HEPE 0.8%; P < .05), a n d premature labour (IVF: 25.7%; HEPE 7.3%; P
< .05) in the 1VF group. Consequently p r e g n a n c i e s after 1VF h a d a high
prematurity (IVF 20.3%; HEPE 6.7%; P < .05) a n d caesarean section late (IVF
35.7%; HEPE 19.9%; P < .05). Perinatal mortality in the IVF g r o u p was 1.0%
(HEPE 0.6%). Furthermore, 16.8% of the newborns after IVF were growth
restricted (HEPE 8.0%; P < .05); 4.4% were severely growth restricted (<3rd
Percentile). Similar results were observed c o m p a r i n g twin pregnancies.
Subgroups of IVF patients h a d even higher risks for e.g. gestational diabetes,
hypertension a n d prematurity. Interestingly, impaired sperm morphology was
associated with an increased IUGR late.
CONCLUSION: Pregnancies after 1VF therapy are high risk pregnancies
when c o m p a r e d to a s t a n d a r d collective (HEPE) m a t c h e d for n u m b e r of
fetuses, age a n d parity. Subgroups of IVF patients show even higher rates of
specific pregnancy risks, impaired sperm morphology seems to be linked to
IUGR.
126
MATERNAL AGE AND RISK O F FETAL DEATH IN TWIN GESTATIONS IN
T H E UNITED STATES JOSEPH CANTERINO t, CANDE ANANTH 2, J O H N
SMULIAN2, J O H N HARRIGAN 3, ANTHONY VINTZILEOS2; i UMDNJ-Rober t
Wood J o h n s o n Medical School/Saint Peter's University Hospital, Obstetrics,
Gynecology a n d Reproductive Sciences, New Brunswick, NJ; 2UMDNJRobert
Wood J o h n s o n Medical School/Saint Peter's University Hospital, Obstetrics,
Gynecology a n d Reproductive Sciences, New Brunswick, NJ; 3Jersey Shore
Medical Center, Maternal-Fetal Medicine, Neptune, NJ
OBJECTIVE: To evaluate the i n d e p e n d e n t contributions of y o u n g a n d
advanced naaternal age on fetal death in twin gestations a n d compare these
risk profiles with other c o m m o n indications for a n t e p a r t o m testing.
STUDY DESIGN: Retrospective c o h o r t analysis of twin gestataions
between 1995-97 in the United States using linked birth-infant death data was
p e r f o r m e d . Gestational age <20 weeks a n d fetuses with anomalies were
excluded. Fetal death rates with maternal ages 20-34 were c o m p a r e d with
y o u n g (<20 years) a n d advanced age (35-39 years a n d _>40 years). Fetal death
rates for c o m m o n indications for a n t e p a r t u m testing i n c l u d i n g c h r o n i c
h y p e r t e n s i o n (CHTN), p r e g n a n c y - i n d u c e d hypertension (PIH), diabetes
(DM), a n d small for gestational age (SGA) births were evaluated. I n d e p e n d e n t
contributions of young a n d advanced ages, CHTN, PIH, DM a n d SGA births
for the risk of fetal death were d e t e r m i n e d based on multivariable logistic
regression models. Relative risk (RR) a n d 95% confidence intervals (CI) were
derived f r o m these models after adjusting for b i r t h order, gravidity, race,
marital status, prenatal care, education a n d smoking.
RESULTS: A m o n g the 275,901 births, fetal d e a t h o c c u r r e d in 2,097
(0.8%). Fetal death rate a n d RR for maternal age categories, CHTN, PIH, DM
a n d SGA are shown in the Table. W h e n the analysis was restricted to delivery
_>32weeks similiar risk profiles were noted.
CONCLUSION: Young maternal age is independently associated with an
increased risk for fetal death. The magnitude of these risks is similiar to those
of other c o m m o n indications for a n t e p a r t u m testing. Advanced maternal age
appears to reduce the risk of fetal death.
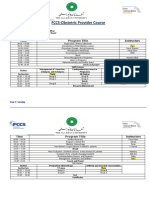
Table
Fetal death rate in twin gestations
GROUP
<20
20-34
35-39
>_40
CHTN
PIH
DM
SGA
TOTAL BIRTHS
D E A T H S (N)
RATE
19,997
207,456
40,743
7,705
2,462
23,234
9,156
25,050
260
1,546
239
52
22
115
57
620
13.0
7.5
5.9
6.7
8.9
4.9
6.2
24.8
R R (95% CI)
1.8
1.0
0.8
0.9
1.2
0.6
0.8
4.3
(1.5-2.0)
(Referent)
(0.7-0.9)
(0.7-1.2)
(0.8-1.8)
(0.5-0.8)
(0.6-1.1)
(3.9-4.7)
127
METOCLOPRAMIDE CONCENTRATION IN BREAST MILK O F WOMEN
DELIVERING BETWEEN 23-34 WEEKS GESTATION WENDY HANSEN I,
STEPHEN H U N T E R 1, STEPHANIE MCANDREW ~, KATHLEEN HARRIS 3,
BRIDGET ZIMMERMAN4; University of Iowa Hospitals a n d Clinics,
Obstetrics a n d Gynecology, Iowa City, IA; 2University of Iowa Hospitals a n d
Clinics, Iowa City, IA; 3University of Wisconsin Medical School, Madison, WI;
4University of Iowa College of Public Health, Biostatistics, Iowa City, IA
OBJECTIVE: Metoclopramide (MC) is generally accepted to be a n
effective lactagogne. We determined the concentration of MC in the breast
milk of women with preterm infants (23-34 weeks gestation).
STUDY DESIGN: Breast milk samples were obtained from 14 mothers
taking MC who delivered p r e t e r m infants. Subjects were chosen r a n d o m l y
from the experimental g r o u p (n = 34) of a larger randomized, double blind,
placebo-controlled study (n = 69). Within 96 hours after birth, women took 10
m g of MC three times a day for 10 days. Breast milk samples were taken on day
10 -+ 2 a n d sent to National Medical Services (Willow Grove, PA) for a highpressure liquid c h r o m a t o g r a p h y assay of the MC levels in the milk. All samples
except one were extracted from a 24-hour collection of expressed breast milk.
Breast milk samples f r o m two m o t h e r s taking placebo were analyzed as
controls.
RESULTS: Breast milk assays of the two women in the placebo g r o u p did
not detect MC. The mean level of MC excreted into the breast milk of the 14
subjects was 44.8 + 20.4 n g / m L . The median (25th-75th percentile) level of
MC in breast milk was 45 (28-56) n g / m L .
CONCLUSION: Mean levels of metocloplamide in preterm breast milk
are similar to levels f o u n d in studies of term subjects. Breast milk levels are
similar to the reported therapeutic range of 40-80 n g / m L in the plasma of
adults taking 10 mg TID. We calculated the m a x i m u m possible exposure to
infants in our study to be 0.011 m g / k g / d a y . This is about 3% of the recomm e n d e d daily dosage (0.5 m g / k g / d a y ) for children. This is similar to findings
on term infants.
128
THIRD-TRIMESTER UNEXPLAINED INTRAUTERINE FETAL DEATH IS
N O T ASSOCIATED WITH THROMBOPI-UI.I& RONIT BECK-FRUCHTER t,
YASSER HUJEIRAT 2, STAVIT SHALEV"2, ZOHAR NAHUM 1, AMIR WEISS 1,
ZEEV WEINER t, ELIEZER SHALEV'3; t H a ' E m e k Medical Center, Obstetrics
a n d Gynecology, Afnla; 2 H a ' E m e k Medical Center, H u m a n Genetic Unit,
Afula; 3Technion-Israel Institute of Technology, R a p p a p o r t Faculty of Medicine, Haifa
OBJECTIVE: To d e t e r m i n e the frequency of i n h e r i t e d a n d a c q u i r e d
thrombophilia a m o n g women with third-trimester unexplained intrauterine
fetal death (IUFD).
STUDY DESIGN: All women with IUFD after 24 weeks gestation in a 3-year
period were initially assessed. Cases with congenital anomalies, intrauterine
infection, feto-maternal bleeding or diabetes mellitus were excluded. The
remaining 53 women were matched for ethnicity with 53 healthy women with a
n o r m a l obstetrical history. All women, in b o t h groups were tested for
mutations of factor V Leiden, p r o t h r o m b i n gene, MTHFR, for the deficiencies
of protein S, protein C, anti t h r o m b i n III a n d for lupus anticoagulant a n d
anticardiolipin antibodies.
RESULTS: The prevalence of any t h r o m b o p h i l i a was 40% in the study
g r o u p c o m p a r e d to 32% in the control g r o u p (P = .54). Inherited thrombophilia was f o u n d in 32% of the study c o m p a r e d to 21% of controls (P= .27).
The late of acquired thrombophilia did not differ between the groups (20% vs.
19%, respectively). The rate of combined thrombophilias was 15% vs. 7.5% (P
= .36).
CONCLUSION: Third-trimester unexplained IUFD is not associated with
thrombophilia.
Вам также может понравиться
- Pregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsОт EverandPregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsОценок пока нет
- Am J Perinatol. 2007 Jun24 (6) 373-6Документ4 страницыAm J Perinatol. 2007 Jun24 (6) 373-6Ivan Osorio RuizОценок пока нет
- DownloadДокумент6 страницDownloadKai GgОценок пока нет
- Early Prediction of Preterm Birth For Singleton, Twin, and Triplet PregnanciesДокумент6 страницEarly Prediction of Preterm Birth For Singleton, Twin, and Triplet PregnanciesNi Wayan Ana PsОценок пока нет
- Original ArticleДокумент4 страницыOriginal ArticlefeyzarezarОценок пока нет
- PIIS0002937821019992Документ2 страницыPIIS0002937821019992made dharmaОценок пока нет
- A Prospective Cohort Study of Pregnancy Risk Factors and Birth Outcomes in Aboriginal WomenДокумент5 страницA Prospective Cohort Study of Pregnancy Risk Factors and Birth Outcomes in Aboriginal WomenFirman DariyansyahОценок пока нет
- The NeoUpdates - DecДокумент7 страницThe NeoUpdates - DecDr Satish MishraОценок пока нет
- Fracture of The Clavicle in The Newborn Following Normal Labor and DeliveryДокумент6 страницFracture of The Clavicle in The Newborn Following Normal Labor and DeliveryAlberto OrtizОценок пока нет
- Predictive Factors For Preeclampsia in Pregnant Women: A Unvariate and Multivariate Logistic Regression AnalysisДокумент5 страницPredictive Factors For Preeclampsia in Pregnant Women: A Unvariate and Multivariate Logistic Regression AnalysisTiti Afrida SariОценок пока нет
- Zhang 2019Документ9 страницZhang 2019Maria José MendiolaОценок пока нет
- 1 s2.0 S0002937804009159 MainДокумент6 страниц1 s2.0 S0002937804009159 MainNi Wayan Ana PsОценок пока нет
- Leitich, 2003 Antibiotico No Tratamento de VB Meta AnaliseДокумент7 страницLeitich, 2003 Antibiotico No Tratamento de VB Meta AnaliseEdgar SimmonsОценок пока нет
- Gong Fei (Orcid ID: 0000-0003-3699-8776) Li Xihong (Orcid ID: 0000-0002-0986-760X)Документ21 страницаGong Fei (Orcid ID: 0000-0003-3699-8776) Li Xihong (Orcid ID: 0000-0002-0986-760X)Clarithq LengguОценок пока нет
- EUROMEDLAB 2013 PostersДокумент101 страницаEUROMEDLAB 2013 PostersidownloadbooksforstuОценок пока нет
- Singleton Term Breech Deliveries in Nulliparous and Multiparous Women: A 5-Year Experience at The University of Miami/Jackson Memorial HospitalДокумент6 страницSingleton Term Breech Deliveries in Nulliparous and Multiparous Women: A 5-Year Experience at The University of Miami/Jackson Memorial HospitalSarah SilaenОценок пока нет
- Natural History of Fetal Position During Pregnancy.11Документ6 страницNatural History of Fetal Position During Pregnancy.11PutriОценок пока нет
- Obstetric Complications in Women With Polycystic Ovary Syndrome: A Systematic Review and Meta-AnalysisДокумент26 страницObstetric Complications in Women With Polycystic Ovary Syndrome: A Systematic Review and Meta-AnalysisPany Chandra LestariОценок пока нет
- P ('t':'3', 'I':'3053721863') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Документ3 страницыP ('t':'3', 'I':'3053721863') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Ni Wayan Ana PsОценок пока нет
- Fibroid TumorsДокумент5 страницFibroid TumorscacingpandoraОценок пока нет
- Intrauterine Fetal Demise-A Tragic Event: A Study of Its Epidemiology, Causes and Methods of InductionДокумент6 страницIntrauterine Fetal Demise-A Tragic Event: A Study of Its Epidemiology, Causes and Methods of InductionSuyati KomalОценок пока нет
- Morbilidad Y Mortalidad Materna Y Perinatal de La Diabetes Gestacional en Una Población MexicanaДокумент11 страницMorbilidad Y Mortalidad Materna Y Perinatal de La Diabetes Gestacional en Una Población MexicanaEnith Perez RangelОценок пока нет
- Lactation and Maternal Risk of Type 2 Diabetes: A Population-Based StudyДокумент6 страницLactation and Maternal Risk of Type 2 Diabetes: A Population-Based StudyMoni SantamariaОценок пока нет
- Nidhi Thesis PresentationДокумент25 страницNidhi Thesis Presentationujjwal souravОценок пока нет
- Jurnal Placenta PreviaДокумент9 страницJurnal Placenta Previasheva25Оценок пока нет
- Preterm Parturition and Pre-Eclampsia: The Confluence of Two Great Gestational SyndromesДокумент7 страницPreterm Parturition and Pre-Eclampsia: The Confluence of Two Great Gestational SyndromesmarinanananaОценок пока нет
- Impact of Oligohydramnios On Maternal and PerinataДокумент6 страницImpact of Oligohydramnios On Maternal and PerinataDiana SchlittlerОценок пока нет
- Relationship Between Serum Vitamin D Level and Ectopic Pregnancy: A Case-Control StudyДокумент6 страницRelationship Between Serum Vitamin D Level and Ectopic Pregnancy: A Case-Control StudyMatias Alarcon ValdesОценок пока нет
- Wolf Et Al MultivitaminsДокумент30 страницWolf Et Al MultivitaminsAnonymous 2GBzrE3XОценок пока нет
- RokokpromДокумент9 страницRokokpromyoga_kusmawanОценок пока нет
- Frequency of Preterm Labor and Its Factors in Patients Presenting To Secondary Care HospitalДокумент6 страницFrequency of Preterm Labor and Its Factors in Patients Presenting To Secondary Care HospitalJohn WickОценок пока нет
- Minimal Stimulation IVF Vs Conventional IVFДокумент8 страницMinimal Stimulation IVF Vs Conventional IVFpolygoneОценок пока нет
- 140 140 1 PBДокумент4 страницы140 140 1 PBMina LelymanОценок пока нет
- Vitamins and Perinatal Outcomes Among HIV-Negative Women in TanzaniaДокумент9 страницVitamins and Perinatal Outcomes Among HIV-Negative Women in TanzaniaEmma KomalasariОценок пока нет
- Bjo12636 PDFДокумент9 страницBjo12636 PDFLuphly TaluvtaОценок пока нет
- Placental Abruption in Term and Preterm.8 PDFДокумент8 страницPlacental Abruption in Term and Preterm.8 PDFMuhammad Riza FahlawiОценок пока нет
- CDC 84627 DS1Документ15 страницCDC 84627 DS1Thu HoaiОценок пока нет
- Vol9 Issue1 06Документ4 страницыVol9 Issue1 06annisaОценок пока нет
- High-Grade Cervical Squamous Intraepithelial LesioДокумент6 страницHigh-Grade Cervical Squamous Intraepithelial LesiodiazdianadpОценок пока нет
- Faktor Risiko 3 Dan PemeriksaanДокумент19 страницFaktor Risiko 3 Dan PemeriksaanNidhaSavitriОценок пока нет
- Women With Preterm Birth Have A Distinct Cervicovaginal MetabolomeДокумент21 страницаWomen With Preterm Birth Have A Distinct Cervicovaginal MetabolomeFatha RaniОценок пока нет
- Nej Mo A 1509819Документ10 страницNej Mo A 1509819Fhirastika AnnishaОценок пока нет
- Can Fundal Height Predict Weight or Twins?: SommaireДокумент4 страницыCan Fundal Height Predict Weight or Twins?: SommairePandawa ObgynОценок пока нет
- Del 153Документ6 страницDel 153Fan AccountОценок пока нет
- 247-Article Text-1425-1-10-20200122Документ11 страниц247-Article Text-1425-1-10-20200122Gisela M SilvaОценок пока нет
- Weight: Maternal Body and Pregnancy Outcomel'2Документ1 страницаWeight: Maternal Body and Pregnancy Outcomel'2Sary ArisazОценок пока нет
- Herrera 2017Документ9 страницHerrera 2017Bianca Maria PricopОценок пока нет
- Original Article: Comparison of Vitamin D Levels in Cases With Preeclampsia, Eclampsia and Healthy Pregnant WomenДокумент7 страницOriginal Article: Comparison of Vitamin D Levels in Cases With Preeclampsia, Eclampsia and Healthy Pregnant WomenSarlitaIndahPermatasariОценок пока нет
- Demographic, Lifestyle, and Reproductive Risk Factors For EctopicДокумент17 страницDemographic, Lifestyle, and Reproductive Risk Factors For EctopicJustin IqbalОценок пока нет
- Unintended Pregnancy, Prenatal Care, Newborn Outcomes, and Breastfeeding in Women With EpilepsyДокумент10 страницUnintended Pregnancy, Prenatal Care, Newborn Outcomes, and Breastfeeding in Women With EpilepsyasfwegereОценок пока нет
- App Acog 2012Документ10 страницApp Acog 2012jimedureyОценок пока нет
- Predictive value of maternal s erum β-hCG concentration in the ruptured tubal ectopic pregnancyДокумент7 страницPredictive value of maternal s erum β-hCG concentration in the ruptured tubal ectopic pregnancyyayayaОценок пока нет
- Sibai PDFДокумент2 страницыSibai PDFAdriana PajueloОценок пока нет
- Pregnancy Complications and Outcomes in Women With Epilepsy: Mirzaei Fatemeh, Ebrahimi B. NazaninДокумент5 страницPregnancy Complications and Outcomes in Women With Epilepsy: Mirzaei Fatemeh, Ebrahimi B. NazaninMentari SetiawatiОценок пока нет
- Prediction of Recurrent Preeclampsia Using First-Trimester Uterine Artery DopplerДокумент6 страницPrediction of Recurrent Preeclampsia Using First-Trimester Uterine Artery Dopplerganesh reddyОценок пока нет
- Jurnal Plasenta PreviaaДокумент41 страницаJurnal Plasenta PreviaacimyОценок пока нет
- Articulos Sepsis Neonatal TempranaДокумент29 страницArticulos Sepsis Neonatal Tempranaverock88Оценок пока нет
- Analytical Study of Intrauterine Fetal Death Cases and Associated Maternal ConditionsДокумент5 страницAnalytical Study of Intrauterine Fetal Death Cases and Associated Maternal ConditionsNurvita WidyastutiОценок пока нет
- Maternal Insulin Resistance and Preeclampsia: ObstetricsДокумент6 страницMaternal Insulin Resistance and Preeclampsia: ObstetricsDiajeng Marta TriajiОценок пока нет
- 33873-Article Text-121761-1-10-20170831Документ6 страниц33873-Article Text-121761-1-10-20170831AnggaОценок пока нет
- Kahn 1998Документ3 страницыKahn 1998Sheila Regina TizaОценок пока нет
- Sulfated Glycosaminoglycans of Periurethral Tissue in Pre-And Postmenopausal WomenДокумент4 страницыSulfated Glycosaminoglycans of Periurethral Tissue in Pre-And Postmenopausal WomenSheila Regina TizaОценок пока нет
- C-Section + Total Abdominal Hysterectomy ReportДокумент3 страницыC-Section + Total Abdominal Hysterectomy ReportSheila Regina TizaОценок пока нет
- Liver Cirrhosis LectureДокумент83 страницыLiver Cirrhosis LectureSheila Regina Tiza100% (1)
- GERD Pariet OkДокумент53 страницыGERD Pariet OkSheila Regina TizaОценок пока нет
- Referat: Oleh: Sheila Regina Tiza 1102008332Документ1 страницаReferat: Oleh: Sheila Regina Tiza 1102008332Sheila Regina TizaОценок пока нет
- Assessment & Procedure For Performing A Vaginal Examination 3.0Документ10 страницAssessment & Procedure For Performing A Vaginal Examination 3.0jomarie gamiaoОценок пока нет
- FCCS-Obstetric Provider Course: Time Program Title InstructorsДокумент2 страницыFCCS-Obstetric Provider Course: Time Program Title InstructorsSamina AyazОценок пока нет
- Every Drop Is PreciousДокумент18 страницEvery Drop Is Preciousvikas rattanОценок пока нет
- Multiple PregnancyДокумент32 страницыMultiple Pregnancyneenuj_5100% (2)
- Hpe Year 9 Lifestyle Diseases Oral Presentation AssessmentДокумент1 страницаHpe Year 9 Lifestyle Diseases Oral Presentation Assessmentapi-247292404Оценок пока нет
- SHN Learning Resource - Puberty and Menstrual HealthДокумент6 страницSHN Learning Resource - Puberty and Menstrual HealthWENNY LYN BEREDOОценок пока нет
- DR - Novan-Preterm Birth Awam 2Документ31 страницаDR - Novan-Preterm Birth Awam 2Mamik ShofiaОценок пока нет
- DiarrheaДокумент28 страницDiarrheakalpesh parvatОценок пока нет
- 02 - Waste Water Treatment - Disposal For Building PremisesДокумент10 страниц02 - Waste Water Treatment - Disposal For Building PremisesGlyra RosalemОценок пока нет
- Notice: Committees Establishment, Renewal, Termination, Etc.: Physical Activity Guidelines Advisory CommitteeДокумент2 страницыNotice: Committees Establishment, Renewal, Termination, Etc.: Physical Activity Guidelines Advisory CommitteeJustia.comОценок пока нет
- Ecological and Longitudinal StudyДокумент44 страницыEcological and Longitudinal Studyabdikani hassanОценок пока нет
- Planning For Healthy PregnancyДокумент31 страницаPlanning For Healthy Pregnancyafiani qonitaОценок пока нет
- Rapha Exam (35 MKS)Документ2 страницыRapha Exam (35 MKS)TumabangОценок пока нет
- Reaction PaperДокумент2 страницыReaction PaperYahBoiMaykelОценок пока нет
- Preprint 29733 AcceptedДокумент21 страницаPreprint 29733 AcceptedUcu Virna RianiОценок пока нет
- The Importance of Walking To Public Health.2Документ7 страницThe Importance of Walking To Public Health.2DorjeОценок пока нет
- Artikel Bahasa Inggris Tentang Kesehatan Artinya TerbaruДокумент5 страницArtikel Bahasa Inggris Tentang Kesehatan Artinya Terbaruahwandi riswantoОценок пока нет
- Global AIDS Strategy 2021 2026 enДокумент100 страницGlobal AIDS Strategy 2021 2026 enmohammedОценок пока нет
- EBOOK Proceedings C516 PDFДокумент765 страницEBOOK Proceedings C516 PDFCristinaCaprosОценок пока нет
- IMAM Guidelines For Uganda Jan2016 PDFДокумент204 страницыIMAM Guidelines For Uganda Jan2016 PDFkamakyageofrey100% (3)
- Installation of Earthing SystemДокумент9 страницInstallation of Earthing SystemamalОценок пока нет
- Calawis Water Treatment PlantДокумент4 страницыCalawis Water Treatment PlantSakura ShigaОценок пока нет
- Maternal Mortality in India-NewДокумент17 страницMaternal Mortality in India-NewMaitreyi MenonОценок пока нет
- Epidemiology of Sarcopenia Prevalence, Risk FactoДокумент9 страницEpidemiology of Sarcopenia Prevalence, Risk FactoW Antonio Rivera MartínezОценок пока нет
- Disinfection: Universidad APEC Prof. Yessica Castro, PH.DДокумент31 страницаDisinfection: Universidad APEC Prof. Yessica Castro, PH.DAsistencia YCEОценок пока нет
- Communiqué de La MfaДокумент4 страницыCommuniqué de La MfaL'express MauriceОценок пока нет
- RESEARCH AlponsДокумент102 страницыRESEARCH Alponsrmconvidhya sri2015Оценок пока нет
- 08 PrakasamДокумент113 страниц08 PrakasamRajeev SagiОценок пока нет
- Immunization Schedule, Japan Vaccination JaponДокумент1 страницаImmunization Schedule, Japan Vaccination JaponBouissac100% (2)
- Job Description of Staff Working in BHU PDFДокумент10 страницJob Description of Staff Working in BHU PDFJamshaidzubairee100% (7)