Академический Документы
Профессиональный Документы
Культура Документы
The Art of Motivating Behavior Change
Загружено:
Orban Csaba DanielИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
The Art of Motivating Behavior Change
Загружено:
Orban Csaba DanielАвторское право:
Доступные форматы
Public Health Nursing Vol. 18 No. 3, pp.
178185
0737-1209/01/$15.00
Blackwell Science, Inc.
The Art of Motivating Behavior
Change: The Use of
Motivational Interviewing to
Promote Health
Harold E. Shinitzky, Psy.D., and
Joan Kub, Ph.D., R.N., C.S.
Abstract Health promotion and disease prevention have always
been essential to public health nursing. With the changing health
care system and an increased emphasis on cost-containment, the
role of the nurse is expanding even more into this arena. A
challenge for public health nurses, then, is to motivate and facilitate health behavior change in working with individuals, families,
and communities and designing programs based on theory. Leading causes of death continue to relate to health behaviors that
require change. The purpose of this article is to integrate theory
with practice by describing the Transtheoretical Model of Change
as well as the principles of motivational interviewing that can
be used in motivating behavioral change. A case scenario is
presented to illustrate the use of the models with effective interviewing skills that can be used to enhance health. Implications for
practice with an emphasis on providing an individually tailored
matched intervention is stressed.
Key words: Transtheoretical Model, motivational interviewing, health promotion, health behavior.
Harold E. Shinitzky is an Instructor, Department of Pediatrics,
Johns Hopkins University, School of Medicine, Baltimore, Maryland. Joan Kub is an Assistant Professor, Johns Hopkins University School of Nursing, Baltimore, Maryland.
Address correspondence to Harold E. Shinitzky, 2531 Landmark Dr., Suite 203, Clearwater, FL 33761. E-mail: hshinitz@
jhmi.edu
178
INTRODUCTION
With the changing health care system and an increased
emphasis on cost-containment, the role of the nurse is
expanding more and more into the arena of health promotion. In 1986, the First International Conference on Health
Promotion was held in Ottawa, Canada. This conference
has served as a source of inspiration for health promotion
since that time. Five levels of action were outlined: (1)
building health public policy, (2) creating supportive environments, (3) strengthening community action, (4) developing personal skills, and (5) reorienting the health system
(World Health Organization [WHO], Health and Welfare
Canada, and the Canadian Public Health Association,
1986). It is increasingly recognized that action on all of
these levels is necessary for a comprehensive approach to
health. Influences on health occur at several levels including individual, interpersonal, community, environmental,
and health care system (Donatelle & Davis, 1998).
Health promotion strategies, which influence an individual or population, may be either active or passive. Passive
strategies involve the client as an inactive participant and
include approaches such as maintaining clean water. Active
strategies on the other hand, depend on the individual
becoming personally involved in adopting a proposed program of health promotion that might include exercise regimens or decreasing daily calories (Edelman & Mandle,
1998). Personal health behavior began to attract attention
in the 1960s, with the release of the First Surgeon Generals
Report on Smoking and Health. Since that time other areas
of human behavior, such as dietary patterns and physical
activity, have been subjects of major Surgeon Generals
Reports (Lee & Estes, 1997).
Shinitzky and Kub: Motivating Behavior Change 179
As outlined in the Ottawa Charter, we seek to explore
the role that nurses can play in promoting and developing
personal skills leading to healthier clinical outcomes. This
is not to negate the importance of the other skills, but it
is increasingly recognized that behavioral determinants of
health are contributing factors of premature death. These
leading causes of death in order of priority are tobacco,
diet and activity, alcohol, microbial agents, toxic agents,
firearms, sexual behavior, motor vehicles, and the illicit
use of drugs (McGinnis & Foege, 1993).
A challenge for public health nurses then, is to motivate
and facilitate health behavior change. Effective interpersonal skills are essential techniques that can be used to
accomplish this task. Enhancing the interpersonal communication skills of health providers results in increased levels
of satisfaction among clients and providers, greater adherence to treatment regimens, fewer lawsuits, continuity of
the same provider, and better follow-up on appointment
keeping (Hall, Roter, & Tand, 1988; Levinson, Roter, Mullooly, Dull, & Frankel, 1997; Wissow et al., 1998; Haynes,
1976).
Noneffective encounters often result in barriers to optimal care. Although most patients are able to identify approximately three to four issues that they would like to
address with their health care provider, one study revealed
that the average health care provider interrupts his or her
patients disclosures after 18 seconds (Beckman & Frankel,
1984). Post visit research has also revealed that 30 to
60% of medical information discussed in an encounter is
forgotten, and 50% of medical treatment regimens are not
followed to their fullest extent (Haynes, Taylor, & Sackett,
1981).
Our role as effective health care providers must include
then, an understanding of the interpersonal skills that can
be used to motivate individuals to move towards optimal
health. The purpose of this article is to integrate theory
with practice by describing one model, the Transtheoretical
Model of Change, that can guide nurses in facilitating
change and to further discuss principles of motivational
interviewing that can be used in facilitating this change.
Transtheoretical Model of Change
The Transtheoretical Model of Change, which consists of
five stages, has emerged from the research efforts of Carlo
DiClemente and James Prochaska over the past 18 years.
Most of the research has focused on smoking cessation,
but the model has also been applied to other addictive
behaviors including drug abuse, obesity, eating disorders,
gambling, exercise, and condom use (DiClemente & Prochaska, 1998). In the model, intentional behavior change
is emphasized as opposed to societal, developmental, or
imposed change (Prochaska, DiClemente, & Norcrass,
1992). The three organizing constructs of the model are
stages of change, processes of change, and levels of change
(DiClemente & Prochaska, 1998).
Stages of Change
The stages of change consist of five categories along a
continuum that reflect an individuals interest and motivation to alter a current behavior. It is through movement
along these stages that one is able to achieve successful
behavioral change (DiClemente & Prochaska, 1998). These
stages include precontemplation, contemplation, preparation, action, and maintenance. Each health care provider
must determine the readiness to change or the stage in
which each patient is in prior to developing a treatment
plan.
1. Precontemplation is the stage in which there is an
unwillingness to change a problem behavior or there is
a lack of recognition of the problem. If a patient is not
thinking about any behavior change in the next 6
months, she or he is classified as a precontemplator.
2. Contemplation involves the stage in which there is a
consideration of change with a decision-making evaluation of the pros and cons of both the problem behavior
and the change. Individuals frequently begin to weigh
the consequences of action or inaction. At this point,
patients are able to discuss the negatives as well as the
benefits associated with the at-risk behavior. This opens
the door to a collaborative process. Usually, these patients discuss actually changing their current behavior
within a 6-month period.
3. Preparation represents the period when there is a commitment to change in the near future, usually 1-month.
Patients express a high degree of motivation towards
the desired behaviors and outcomes. Patients in the
preparation stage have determined that the adverse costs
of maintaining their current behavior exceed the benefits. Therefore, initiating a new behavior is more likely.
These patients have moved from thinking about the
issue to doing something about it.
4. The fourth stage, Action, is when change or modification of behavior actually takes place.
5. After 3 to 6 months of success, the last stage of Maintenance is begun. During this stage, there is a focus on
lifestyle modification in order to avoid relapse and to
stabilize the behavior change (Cassidy, 1997; DiClemente & Prochaska, 1998).
Processes of Change
The processes of change facilitate movement through the
stages of change. There are 10 processes that have been
identified that are responsible for movement (DiClemente & Prochaska, 1998). Five of these processes, which
include consciousness raising, dramatic relief, environ-
180 Public Health Nursing
Volume 18 Number 3 May/June 2001
mental reevaluation, social liberation, and self reevaluation,
are experiential or cognitive processes. These are internally
mediated factors that are associated with an individuals
emotions, values, and cognitions (Cassidy, 1997). Consciousness raising is described as encouraging individuals
to increase their level of awareness, seek new information,
or to gain an understanding about a problem. Dramatic
relief is experiencing and expressing feelings about ones
problems. Environmental reevaluation is assessing how
ones problem affects the physical environment. Social
liberation is increasing alternatives for nonproblem behaviors in society. Self reevaluation is assessing how one feels
and thinks about oneself in relationship to the problem
(Prochaska et al., 1992).
The five other processes (counter conditioning, helping
relationships, reinforcement management, stimulus control, and self-liberation) are behavioral processes (Prochaska et al., 1992; Cassidy, 1997). Counter conditioning
is substituting alternatives for problem behaviors. An example might be the use of meditation to cope with unpleasant emotions (Cassidy, 1997). Helping relationships are
defined as those that provide trust, acceptance, and support.
The provider that listens when there is a need to discuss
the problem is an example of this process. Reinforcement
management is the use of positive reinforcements and appropriate goal setting with the patient. Stimulus control is
helping the patient to restructure the environment so that
the stimuli or triggers for the undesired behavior are controlled. Self-liberation is when an individual believes in
him or herself and his or her ability to change.
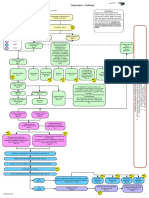
An integration of these processes with the stages can be
seen in Figure 1. In other words, there is a match between
the stage that the patient is in and the intervention that is
used. Individuals in the contemplation stage would be most
open to consciousness raising, the use of dramatic relief,
and an environmental reevaluation. In the action phase,
effective use of the behavioral processes is particularly
Figure 1. Stages of change in which processes are most emphasized. Reprinted with permission from Prochaska, Redding, &
Evers, 1997.
helpful (Prochaska et al., 1992); (Prochaska & DiClemente,
1983).
Levels of Change
Clinicians recognize that individuals have multiple problems that often overlap. Addiction, for example, may be associated with marital problems, financial problems,
personality disorders, depression, and violence. With this
recognition, the Transtheoretical Model of Change incorporates five levels of change for consideration. These include
changes that relate to the symptoms or situations, maladaptive cognitions, interpersonal problems, family/systems
problems, and intrapersonal conflicts. Treatment outcomes
are often better when a patients multiple problems are addressed (DiClemente & Scott, 1997). Understanding the life
context of our patients increases the probability that treatment plans will fit their overall needs and be individually
tailored. If we enter into this relationship with the belief
that we are to assess, diagnose, and treat only the most
obvious issue, we are likely to overlook other important
issues. If we remain open to the multiple factors impacting
our patients lives, however, we are apt to be inclusive
rather than exclusive of potential issues.
Research Findings
Support for the Transtheoretical Model of Change has been
accumulating over the past 15 years (DiClemente & Prochaska, 1998). Assessment of the stage of change that a
person is in is one of the most relevant findings for practice.
Previous research on estimating stage distribution has
found that typically 40% of a population with an unhealthy
behavior would be categorized in the precontemplation
stage, 40% would fall in the contemplation stage, and
20% would self-assess in the preparation stage (Dijkstra,
DeVries, & Bakker, 1996; Fava, Velicer, & Prochaska,
1995). Several studies have focused on creating assessment
tools to determine the level of motivation for change which
include the 12-item Readiness to Change measure (Rollnick, Heather, Gold, & Hall, 1992), the 20-item Alcohol
Abstinence Self-Efficacy Scale (DiClemente, Carbonari,
Montgomery, & Hughes, 1993), the University of Rhode
Island Change Assessment (URICA) (McConnaughy,
DiClemente, Prochaska, & Velicer, 1989), the Stages of
Change Readiness and Treatment Eagerness Scale (SOCRATES) (Miller & Tonigan, 1996), and the Readiness Ruler
(DNofrio, Bernstein, & Rollnick, 1996).
Action oriented interventions often target the 20% of
the individuals in the preparation stage while the remaining
needs of the entire population are not being met. It would
therefore be incumbent to develop programs and interventions that either match the needs of individuals who have
not yet made the conscious effort to change or for health
Shinitzky and Kub: Motivating Behavior Change 181
care providers to assist in moving those at-risk individuals
along the continuum from precontemplation to action. Prochaska and Velicer (1997) found that stage-matched programs can assist 80 to 90% of an at-risk population of
smokers. These authors also found that 40% of the individuals who prematurely terminated treatment were initially
assessed as falling into the precontemplation stage.
Another important finding is that extensive relapse and
recycling occurs in populations attempting to take action
to change behavior. This appears to be the norm and has
important implications for practice. Terms such as noncompliant and unmotivated are frequent labels applied
to patients who do not follow through on their treatment
plans. This may reflect the norm of relapse or may also
reflect a poorly created treatment plan that does not consider the stage of change the patient is in. In labeling
patients as such, the provider may be externalizing responsibility, placing blame rather than reflecting upon his or
her own skills. Therefore appreciating the stage of change
the patient is in is imperative before we can begin to
develop an optimal treatment plan. Assessing the patients
position facilitates the development of an individually tailored and matched protocol.
Though our review of the Transtheoretical Model of
Change has focused on its application to an individual
patient, in actuality we may apply the model to families,
populations, and organizations. Prior to implementing an
intervention, one must assess and determine the readiness
to change. After determining the stage of readiness for that
group or individual, the intervention may be tailored to
match their position. By doing so, we can increase the
impact and effectiveness of our intervention.
MOTIVATIONAL INTERVIEWING
Once a patients stage of change is identified, the health
care practitioner needs to implement clinical skills that
will help facilitate the patients progression and movement
along the continuum. Motivational interviewing is a framework developed by Miller and Rollnick (1991) that can
help to facilitate this movement. It builds on the foundation
of understanding that our role as the health care provider
is to assist our patients to move toward a state of action
that leads to improved health status outcomes. A mutually
agreed upon treatment plan that is acceptable to the patient
and fits within the medical parameters is more likely to
be attained. Motivational interviewing is comprised of two
equally important phases, which include: Phase I
building a therapeutic rapport and commitment, and Phase
IIfacilitating the movement through decisional analysis
and behavior change. Table 1 outlines the principles of
motivational interviewing.
Motivational interviewing is a process that is based on
TABLE 1. The Five General Principles of Motivational
Interviewing (Miller, 1983)
1. Express empathy
a. Acceptance and understanding facilitates change
b. Skillful reflective listening is fundamental
c. Ambivalence is normal
2. Develop discrepancies
a. Awareness of consequences is important
b. Engage in a discussion between present behavior and
valued goals
c. Client driven rational for change
3. Avoid argumentation
a. Arguments are counterproductive
b. Judging (why?) breeds defensiveness
c. Resistance is a signal to change therapeutic strategies
d. Labeling is unnecessary
4. Roll with resistance
a. New perceptions are invited but not imposed
b. Client is a valuable resource re: solutions
c. Collaboration is valued
d. Mutually negotiated solutions
5. Support self-efficacy
a. Hope is motivating
b. Patient is responsible for choosing and initiating
c. There is hope in the range of alternatives
d. Knowledge that certain behaviors lead to desired outcomes
e. Possession of those behavior
input by both parties. A starting point is to establish a safe
environment in which our patients and their families feel
as though they can reveal personal information.
The art of motivational interviewing is therefore a dance
between two individuals suspending judgment and avoiding
a confrontational style thereby minimizing defensive reactions by the patient. Providers need to challenge patients
without eliciting defensiveness. When a patient reacts defensively, many providers tend to negatively label the patient
and accuse him or her of being noncompliant and resistant.
We view this as a logical behavioral reaction on the part
of the patient who may not perceive the issues in the same
manner. Providers need to be cautioned then, about challenging a patient too early and creating a dynamic relationship
that requires a defensive posture. As all behaviors are purposeful, we must understand what it is that our patient values
by maintaining his or her current unhealthy lifestyle behavior (for example, smoking).
Acceptance of the person does not mean agreement with
his or her behavior, but rather an appreciation of his or
her perceived issues. We need to be more open to and
understanding of our patients life contexts. It is best to
start out with the patients agenda. No patient comes to us
without some emotional concern. The emotional concern
is frequently the motivating factor that prompted him or
182 Public Health Nursing
Volume 18 Number 3 May/June 2001
her to schedule an appointment and seek out an experts
opinion. A competent provider acknowledges the emotional components of the encounter. To avoid addressing
these issues is a sign that the providers agenda is controlling the encounter.
Another important role of the provider is to help our
patients see that they are in control of their lives. The sense
of an internal locus of control, self-efficacy, and personal
empowerment leads to taking a more active role in ones
life (Egan, 1998). The patient is ultimately the one responsible for making behavioral changes in his or her life.
When mutually discussing treatment options and alternatives, it is important to brainstorm. During the brainstorming phase, cast the net as wide as possible. Subsequent
to identifying the vast array of possibilities, we then narrow
our options to the most viable alternatives. A key concept
during the brainstorming phase is to suspend judging the
best therapeutic fit. Criticizing forestalls creativity and
identification of all possibilities. Patients moving along the
continuum of change, need their providers to amplify the
discrepancy between the pros and cons which make up
their decision-making equation. During the encounter it is
important to refrain from lecturing, for pontificating the
right way only alienates our patients.
As providers we need to weigh our words wisely. Every
question asked needs to have some underlying purpose.
We need to be reflective of our style and of the line of
questioning. Whenever possible, providers need to avoid
habitually asking the question, why? (Benjamin, 1987).
This connotes disapproval and forces the patient to respond
with excuses or alibis. Asking open-ended questions is a
technique that encourages the patient to elaborate while
habitually using closed-ended questions leads to brief responses (that is, Yes or No). By utilizing these techniques
and skills, the encounter can be more rewarding. Recall that
each session must address the needs, concerns, and opinions
of the patient. Lastly, emotional factors are dealt with and
problem solving is mutually managed. Common problems
that providers can encounter are seen in Table 2.
CASE SCENARIO
The following case scenario depicts a patient in the different phases of the Transtheoretical Model of Change. Different motivational interviewing approaches, some less
effective and colleagues more effective, are presented to
illustrate the value of applying appropriately matched techniques to help patients progress towards change. It is your
task to determine the stage of change that this patient
currently fits and assess the encounter. The case scenario
that we present is based on a synthesis of actual patient
encounters.
Mr. Smith is a 46-year-old, African American male.
TABLE 2. Common Problems That Providers Display
1. Asking closed-ended questions. These do not foster an open
dialogue between the patient and the provider. They usually
limit the discussion to a yes or a no response.
2. Double options. Providers frequently assert an either-or
scenario. This implies that there are only two options and that
the provider is the one who knows which options are best.
This style does not empower the patient to take an active role
in problem solving.
3. Not responding to the emotional needs of a patient. Many
providers feel comfortable focusing on the bio-medical needs.
If a therapeutic rapport is not established, however, the patient
is likely to remain focused on their underlying emotional
issues that interfere with the effective flow of information
and negotiation.
4. Using cliches to respond to patient disclosures. If used too
often, they are perceived as trite and minimizing to the
patients.
He presents with an upper respiratory infection (that is,
wheezing, cough, and expectorant for 4 weeks). He has
smoked for 25 years. He is 5 8, 185 pounds, and has an
unremarkable medical history. He has a positive family
history for lung cancer in father and paternal grandfather.
He requested some prescribed antibiotics to resolve his
infection.
Nurse M: Mr. Smith, from what you have told me about your
symptoms, what do think might have contributed to your
infection?
Rationale: Respecting and valuing the patient as the
expert in his own life is an important skill. This question
is posed as an open-ended question, which allows the patient to elaborate from his perspective. This question also
assesses the level of knowledge and insight the patient
has regarding his current condition as well as initiates an
evaluation of his location regarding potential behavioral
changes.
Mr. S: I really dont know. I just need an order for some meds.
Rationale: Patient appears to be unaware or potentially
resistant and therefore, Precontemplative.
Nurse M: Based on the length of time of your symptoms, I
believe that your smoking cigarettes adds to your condition. You
should stop smoking.
Rationale: The provider has made a summarizing comment, however, this comment is latent with judgment and
confrontation. In essence, the provider is attempting to
force the patient from precontemplation into the action
stage. This provider was talking at, rather than with the
patient. The statement of obviously is filled with
judgment. The provider asserts the Gold Standards, yet
Shinitzky and Kub: Motivating Behavior Change 183
does not engage this patient in the problem-solving
opportunities.
Mr. S: Well, you know, I guess there wouldnt be any harm in
that.
Mr. S: No, I dont think so. I have been smoking cigarettes for
several decades and I have never had this before.
Rationale: By not directly challenging, the patient is
more accepting along the continuum. The patient is willing
to be reflective and accept educational information. We see
the movement from precontemplation to contemplation.
To further illustrate the movement along the continuum,
we shall continue with this patient encounter. Once a patient
is in the contemplative stage, our goal is to assist his
or her positive, healthy progression towards behavioral
change.
Rationale: The patient responds with resistance to the
confrontation. Denial is not a symptom of the addiction,
rather it is a defensive response to the providers accusation.
From the responses of this patient (that is, lack of insight or awareness of behavior problem and resistance)
we can determine that he falls within the category,
precontemplation.
Encounter Analysis: If this provider dictates the medical
treatment requirements without understanding and appreciating his or her patients life context, the patient will likely
fail and be labeled as noncompliant. Now that the provider
knows that once you have determined the correct stage of
change, however, the goal is to facilitate movement to the
next stage (Precontemplative to Contemplative). This is
best accomplished by matching motivational interviewing
techniques. Let us continue with Mr. Smith.
Nurse M: Mr. Smith, from the symptoms that you have expressed
and your history, I wonder if your smoking adds to this condition?
You might want to think about the potential impact of smoking
cigarettes has on your overall health.
Rationale: Again, using the history that the patient has
provided, active listening, and summarizing key points
back to the patient, the nurse displays genuine interest in
what has been said. This response also displays an active
listening style and the use of an indirect question. This
free-floating style continues the assessment of motivation
and insight into the patients condition. By offering numerous suggestions without any declarative accusations, the
provider is using the process of consciousness raising.
Mr. S: I never gave much thought to that. I know my family and
home has been affected by cigarette smoking and perhaps I have
too.
Rationale: Patient is willing to consider this as a point
of reflection due to the nonjudgmental style of the provider.
The patient also reveals a potential consequence associated
with the at-risk behaviors. Therefore, this patient has
shifted to the contemplation stage. The nurse has helped
the patient to use the processes of environmental reevaluation and self-liberation.
Nurse M: Would you care if I provided you with some information
for you to look over?
Rationale: Here the provider is establishing a partnership with this patient. Based on what he has said before,
we know that he had not considered this as contributing
to the problem. Engaging in option development without
imposing a judgment is vital.
Nurse M: Mr. S, from what you have told me about your symptoms, what do you think might have contributed to your infection?
Rationale: Asking an open-ended question facilitates
the encounter. This question elicits the patients opinions.
Again, we present this in a respectful manner that values
the patients observations and is therefore inclusive for
solutions.
Mr. S: Well, we have talked about how my smoking may be
making my infection worse and maybe even affecting my general
health.
Rationale: The patient used the word we, indicating
a mutual discussion rather than lecture from the provider.
Additionally, the patient states the possible connection between this behavior and adverse consequences. This individual appears to be in the contemplation stage.
Nurse M: Youve smoked for a couple of decades, what do you
find that you get from smoking?
Rationale: Since all behavior is purposeful, we need
to understand the reinforcing factors associated with this
behavior in order to adequately address this patients needs.
This is helping the patient to do a self-reevaluation.
Mr. S: I smoke when I am with my friends and it helps me to
relax.
Rationale: The patient openly discusses the rewards for
his current unhealthy behavior. These are needed when
seeking leverage and when increasing the discrepancy between the pros and cons.
Nurse M: I see. And what are the drawbacks?
Rationale: Determining the patients level of insight
and now assessing the negatives that will facilitate the
decision-making process.
Mr. S: Well, we both know that its not doing me any good
healthwise and it costs a lot.
Rationale: Mr. S is able to discuss both sides of the
equation. He openly discusses the negative consequences
associated with the at-risk behaviors. Again, these shall be
184 Public Health Nursing
Volume 18 Number 3 May/June 2001
used to accentuate the discrepancy between reinforcing
agents and contraindicators from the patients point of view.
Nurse M: It sounds like there are a few reasons that keep you
smoking and a few on the downside. There is a lot of evidence
that indicates cigarette smoking contributes to upper respiratory
problems and knowing your family history places you at further
risk for problems. If you were to see yourself in 6 months, what
would you be doing differently and how would you go about
getting there?
Rationale: This provider paraphrases the relevant history using the patients words. An indicator of the contemplation stage is the motivation to change behavior over the
next 6 months.
Mr. S: Well, I have tried to quit in the past. I guess I could try
to cut back. I would hopefully feel better than I do now.
Rationale: This patient affirms his willingness to problem solve by altering his at-risk behavior. This patient is
expressing the emotional struggle associated with changing
behaviors. Knowing that 50% of all medical treatment
plans are not followed through to their fullest extent, this
provider expresses an appreciation for the patients identified issue and attempts to partner with the patient to develop
a mutually agreed option.
Nurse M: That certainly sounds reasonable. Why dont you give
that a try. What do you think you could change over the next
month?
Rationale: Empathy and support. Rather than focusing
on the negatives, this provider has chosen to begin by
establishing a therapeutic rapport through reinforcing a
positive. The provider is determining if this patient is in
the preparation stage by inquiring if the behavior change
will occur within 1 month.
Mr. S: I can think about what we have talked about and start
making a game plan for changing my behavior. I guess I could
have fewer cigarettes.
Rationale: This patient has progressed to the preparation
stage by displaying motivation and a plan to alter his
behavior within the coming month.
Nurse M: Is there anything I can do to help you reach this goal?
Rationale: Always survey for more information or concerns. This displays your level of commitment and involvement and prevents those dreaded, Oh, by the way
comments as you and your patient are leaving the office.
Mr. S: Well besides standing next to me every moment, can you
tell me about some of those new treatment programs that I have
heard about?
Rationale: This response displays an active listening
style to the patient. As this patient has already declared a
potential contributing behavior, we then pose an indirect
question. We have moved this patient further along the
continuum through empathetic listening, enhancing the discrepancies, nonjudgmental problem solving, and empowering the patient. This free-floating style continues the
assessment of motivation and insight into his condition.
The provider refrained from labeling or presenting this
in an accusatory manner. The provider is now using the
behavioral processes in the Transtheoretical Model of
Change. In particular, reinforcement management is being
used with the helping relationship.
SUMMARY
This scenario provides us with examples of a patient in
different stages of the change process. This scenario also
provides us with examples of motivational interviewing
techniques that can be used to help our patients progress
through each stage. Therapeutic movement is one stage at
a time. Assessing the patients readiness to change is the
first task for the provider. Once we have determined where
our patients are along the continuum, our task is to facilitate
movement from their current position to the next stage.
An individually tailored, matched service is recommended.
The health care encounter consists of two parties, in
which both play a significant role in the dynamic process.
A provider who chooses not to utilize communication skills
that have been shown to improve the visit and the clinical
outcomes is doing a disservice to his or her patient. We
have the capabilities to positively affect the medical visit
and to influence health. Using specific communication
skills that enlist the patients active involvement in the
encounter, developing the discrepancies between the pros
and the cons of change, and mutually negotiating viable
options can shift a patient further toward adaptive healthy
behavior. Health promotion has been defined as the science and art of helping people change their lifestyle to
move toward a state of optimal health (ODonnell, 1987,
p. 4). The integration of Prochaska and DiClementes
Transtheoretical Model of Change and Miller and Rollnicks Motivational Interviewing techniques seamlessly
merge together to create an optimal patient encounter.
This article has discussed the importance of using a
model of change and motivational interviewing to improve
health. Health promotion into the 21st century demands
an approach that improves the ability of individuals to take
action. Taking action involves at least two of the levels of
action outlined in the Ottawa Charter (WHO, Health and
Welfare Canada, and the Canadian Public Health Association, 1986). It includes creating supportive environments
where clinicians take into consideration the life context of
their patients. In addition, it involves the development of
personal skills to promote health. The Jakarta Fourth Inter-
Shinitzky and Kub: Motivating Behavior Change 185
national Conference on Health Promotion has stressed that
one priority is that of empowering individuals (WHO,
1997). This entails reliable access to the decision-making
process and skills and knowledge essential to effect change.
Through the art of motivating, health care providers can
influence and empower individuals to positively influence
their level of health.
REFERENCES
Beckman, H. B., & Frankel, R. M. (1984). The effect of the
physician behavior on the collection of data. Annals of Internal
Medicine, 101, 692696.
Benjamin, A. (1987). The helping interview: With case illustrations. Boston: Houghton Mifflin.
Cassidy, C. A. (1997). Facilitating Behavior Change. American
Association of Occupational Health Nurses, 45(5), 239246.
DNofrio, G., Bernstein, E., & Rollnick, S. (1996). Motivating
patients for change: A brief strategy for negotiation. In E.
Bernstein & J. Bernstein (Eds.), Case studies in emergency
medicine and the health of the public (pp. 295303). Sudbury,
MA: Jones and Bartlett Publishers.
DiClemente, C. C., Carbonari, J. P., Montgomery, R. P. G., &
Hughes, S. O. (1993). The alcohol abstinence self-efficacy
scale. Journal of Studies on Alcohol, 55, 141148.
DiClemente, C., & Prochaska, J. (1998). Toward a comprehensive
transtheoretical model of change. In W. R. Miller & N.
Healther (Eds.), Treating addictive behaviors (pp. 324). New
York: Plenum Press.
DiClemente, C. C., & Scott, C. W. (1997). Stages of change:
Interactions with treatment compliance and involvement. In
L. S. Onken, J. D. Blaine, & J. J. Boren (Eds.), Beyond the
therapeutic alliance: Keeping the drug-dependent individual
in treatment (NIDA Research Monograph 165). Washington,
DC: U.S. Department of Health and Human Services.
Dijkstra, A., DeVries, H., & Bakker, M. (1996). Pros and cons
of quitting, self-efficacy, and the stages of change in smoking
cessation. Journal of Consulting and Clinical Psychology, 64,
758763.
Donatelle, R., & Davis, L. G. (1998). Access to health. Needham
Heights, MA: Allyn and Bacon.
Edelman, C. L., & Mandle, C. L. (1998). Health promotion
throughout the lifespan. St. Louis, MO: Mosby Co.
Egan, G. (1998). The skilled helper: A problem-management
approach to helping (6th ed.). Pacific Grove, CA: Brooks/
Cole Publishing Company.
Fava, J. L., Velicer, W. F., & Prochaska, J. O. (1995). Applying the
transtheoretical model to a representative sample of smokers.
Addictive Behaviors, 20, 189203.
Hall, J. A., Roter, D. L., & Tand, C. S. (1988). Meta-analysis of
correlates of provider behavior in medical encounters. Medical
Care, 26, 657675.
Haynes, R. B. (1976). A critical review of the determinants
of patient compliance with therapeutic regimens. In D. L.
Sackett & R. B. Haynes, (Eds.), Compliance with therapeutic
regimens. Baltimore, MD: Johns Hopkins University Press.
Haynes, R. B., Taylor, D. W., & Sackett, D. L. (1981). Compliance
in health care (2nd ed.). Baltimore, MD: Johns Hopkins University Press.
Lee, P. R., & Estes, C. L. (1997). The nations health. Boston:
Jones and Bartlett Publishers.
Levinson, W., Roter, D. L., Mullooly, J. P., Dull, V. T., & Frankel,
R. M. (1997). Physician-patient communication: The relationship with malpractice claims among primary care physicians
and surgeons. Journal of American Medical Association, 277,
553559.
McConnaughy, E. A., DiClemente, C. C., Prochaska, J. O., &
Velicer, W. F. (1989). Stages of change in psychotherapy:
A follow-up report. Psychotherapy: Theory, Research, and
Practice, 4, 494503.
McGinnis, J. M., & Foege, W. H. (1993). Actual causes of death in
the United States. Journal of American Medical Association,
270(18), 22072212.
Miller, W. R., & Rollnick, S. (1991). Motivational interviewing:
Preparing people for change. New York: Guilford Press.
Miller, W. R., & Tonigan, J. S. (1996). Assessing drinkers motivation for change: The stages of change readiness and treatment eagerness scale (SOCRATES). Psychology of Addictive
Behaviors, 10, 8189.
ODonnell, M. (1986). Definition of health promotion. Journal
of Health Promotion, 1(1), 45.
Prochaska, J. O., & DiClemente, C. C. (1983). Stages and processes of self-change of smoking: Toward an integrative model
of change. Journal of Consulting and Clinical Psychology,
51(3), 390395.
Prochaska, J. M., & Velicer, W. F. (1997). The transtheoretical
model of health behavior. American Journal of Health Promotion, 12(1), 3848.
Prochaska, J., DiClemente, C., & Norcross, J. (1992). In search
of how people change. American Psychologist, 47(9),
11021114.
Rollnick, S., Heather, N., Gold, R., & Hall, W. (1992). Development of a short readiness to change questionnaire for use
in brief, opportunistic interventions among excessive drinkers.
British Journal of Addiction, 87(5), 743754.
Wissow, L. S., Roter, D., Bauman, L. J., Crain, E., Kercsmar, C.,
Weiss, K., Mitchell, H., & Mohr, B. (1998). Patient-provider
communication during the emergency department care and
children with asthma. Medical Care, 36(10), 14391448.
World Health Organization, Health and Welfare Canada, and the
Canadian Public Health Association. (1986). Ottawa charter
for health promotion. Copenhagen, Denmark: FADL
Publishers.
World Health Organization. (1997). The Jakarta declaration of
leading health promotion into the 21st century [On-line].
Available: http//www.who.int/hpr/docs/jakarta/english.html.
Вам также может понравиться
- Solution Focused Harm Reduction: Working effectively with people who misuse substancesОт EverandSolution Focused Harm Reduction: Working effectively with people who misuse substancesОценок пока нет
- Changing Trends in Mental Health Care and Research in GhanaОт EverandChanging Trends in Mental Health Care and Research in GhanaОценок пока нет
- The Role of Emergency Room Social Worker - An Exploratory StudyДокумент45 страницThe Role of Emergency Room Social Worker - An Exploratory StudyjHen LunasОценок пока нет
- Spices PDFДокумент2 страницыSpices PDFAnonymous S5UkdjJWAОценок пока нет
- Carl Rogers 1Документ10 страницCarl Rogers 1Monica S. SantiagoОценок пока нет
- A Cognitive Information Process Approach To Career Counseling The Many Major Changes of A College StudentДокумент13 страницA Cognitive Information Process Approach To Career Counseling The Many Major Changes of A College Studentapi-307225631Оценок пока нет
- Chronic Pain ACTДокумент8 страницChronic Pain ACTRan AlmogОценок пока нет
- Chapter 23 - Medication Interest ModelДокумент83 страницыChapter 23 - Medication Interest ModelNaomi LiangОценок пока нет
- Resident e Progress NotesДокумент2 страницыResident e Progress Notesapi-273537080Оценок пока нет
- Case-Anheuser Busch UpdatedДокумент12 страницCase-Anheuser Busch UpdatedJennifer Bello Araquel100% (1)
- Depression Care PathwayДокумент267 страницDepression Care PathwaydwiОценок пока нет
- Biopsychosocial ModelДокумент1 страницаBiopsychosocial ModelJames SkinnerОценок пока нет
- Depression Children PDFДокумент2 страницыDepression Children PDFConstanzaОценок пока нет
- SOAP Notes: HistoryДокумент5 страницSOAP Notes: HistoryRajveerОценок пока нет
- Assertive Community Treatment TreatmentOptions 2018Документ2 страницыAssertive Community Treatment TreatmentOptions 2018titik dyahОценок пока нет
- Motivational Interviewing: Application in Clinical PracticesДокумент24 страницыMotivational Interviewing: Application in Clinical PracticesElizabeth HoОценок пока нет
- Making ReferralsДокумент9 страницMaking Referralsglenn johnstonОценок пока нет
- Prochaska JO Velicer The Transtheoretical Model of Health Behavior PDFДокумент11 страницProchaska JO Velicer The Transtheoretical Model of Health Behavior PDFClaudio M. Cruz-FierroОценок пока нет
- P R O D U T I V I T Y: Absenteeism Turnover DisciplineДокумент30 страницP R O D U T I V I T Y: Absenteeism Turnover DisciplineShahzad NazirОценок пока нет
- Occupational Identity Disruption After Traumatic Brain Injury - An Approach To Occupational Therapy Evaluation and TreatmentДокумент13 страницOccupational Identity Disruption After Traumatic Brain Injury - An Approach To Occupational Therapy Evaluation and Treatmentapi-234120429Оценок пока нет
- Post Stroke Psychiatric DisordersДокумент52 страницыPost Stroke Psychiatric Disordersdrkadiyala2Оценок пока нет
- 2015 Final Case Studies Asam Fundamentals Final UpdatedДокумент68 страниц2015 Final Case Studies Asam Fundamentals Final UpdatedTrampa AdelinaОценок пока нет
- Assignment 3Документ12 страницAssignment 3Syed Muhammad Moin Ud Din SajjadОценок пока нет
- Assignment 1Документ4 страницыAssignment 1api-581780198Оценок пока нет
- Cns 780 Know The LawДокумент7 страницCns 780 Know The Lawapi-582911813Оценок пока нет
- Running Head: Writing A Treatment Plan 1Документ6 страницRunning Head: Writing A Treatment Plan 1Angy ShoogzОценок пока нет
- Extended Case Formulation WorksheetДокумент3 страницыExtended Case Formulation Worksheetbakkiya lakshmiОценок пока нет
- Grop No 1counseling ProcessДокумент23 страницыGrop No 1counseling ProcessHina Kaynat100% (1)
- Template For Clinical Progress Note June 2009Документ3 страницыTemplate For Clinical Progress Note June 2009Buthaina AltenaijiОценок пока нет
- Mock First Soap NoteДокумент7 страницMock First Soap Noteapi-372150835Оценок пока нет
- Older Adults and Integrated Health Settings: Opportunities and Challenges For Mental Health CounselorsДокумент15 страницOlder Adults and Integrated Health Settings: Opportunities and Challenges For Mental Health CounselorsGabriela SanchezОценок пока нет
- Writing Project - Soap Note MemorandumДокумент2 страницыWriting Project - Soap Note Memorandumapi-340006591Оценок пока нет
- My Safety Plan: You Deserve To Be Safe and HappyДокумент2 страницыMy Safety Plan: You Deserve To Be Safe and HappySaundra NguyenОценок пока нет
- RUNNING HEAD: The SoloistДокумент7 страницRUNNING HEAD: The SoloistMary Winston DozierОценок пока нет
- Behavioral InterviewingДокумент3 страницыBehavioral InterviewingMarsden RockyОценок пока нет
- Case Management Using CBTДокумент2 страницыCase Management Using CBTalessarpon7557Оценок пока нет
- Soap Note - ExampleДокумент1 страницаSoap Note - ExamplearchanabrianОценок пока нет
- Macro - CommunityДокумент2 страницыMacro - CommunityFaranОценок пока нет
- 10 Introductory Questions Therapists Commonly Ask PDFДокумент4 страницы10 Introductory Questions Therapists Commonly Ask PDFsamir shah100% (1)
- Case Note Excellent2 AnnotatedДокумент8 страницCase Note Excellent2 AnnotatedShubham Jain Modi100% (1)
- Electronic CigarettesДокумент2 страницыElectronic CigarettesLeixa Escala100% (1)
- Cognitive TherapyДокумент18 страницCognitive TherapyHaysheryl Vallejo SalamancaОценок пока нет
- Working With Older AdultsДокумент84 страницыWorking With Older AdultsdarketaОценок пока нет
- Motivational Interviewing Theoretical EssayДокумент6 страницMotivational Interviewing Theoretical EssayDanelleHollenbeckОценок пока нет
- Chapter 5 AnxietyДокумент16 страницChapter 5 AnxietyMark Jayson JuevesОценок пока нет
- Thesis Presentation 2Документ13 страницThesis Presentation 2api-457509028Оценок пока нет
- Peer SupportДокумент5 страницPeer SupportGillian FleuryОценок пока нет
- Clinical Social Work: Privilege FormДокумент1 страницаClinical Social Work: Privilege FormjirehcounselingОценок пока нет
- Perinatal Mood and Anxiety DisДокумент186 страницPerinatal Mood and Anxiety Disandifa aziz satriawan100% (1)
- Suicide Risk Assessment Guide NSWДокумент1 страницаSuicide Risk Assessment Guide NSWapi-254209971Оценок пока нет
- Mental Status ExamДокумент24 страницыMental Status ExamRemedios BandongОценок пока нет
- Pre Post TestДокумент4 страницыPre Post TestRainОценок пока нет
- What Is Problem Solving Therapy?Документ2 страницыWhat Is Problem Solving Therapy?Divaviya100% (1)
- C4C Upload of The U.S. EEOC Management Directive 110Документ358 страницC4C Upload of The U.S. EEOC Management Directive 110C4CОценок пока нет
- 3-3 - MasterTreatment Plan Update4-9-18newestGD7-9Документ1 страница3-3 - MasterTreatment Plan Update4-9-18newestGD7-9Rudy KolderОценок пока нет
- Postconcussive Syndrome (PCS) Clinical Practice Guideline: Occupational TherapyДокумент7 страницPostconcussive Syndrome (PCS) Clinical Practice Guideline: Occupational TherapyNicoleta Stoica100% (1)
- No Evidence of DependenceДокумент2 страницыNo Evidence of Dependencemago1961Оценок пока нет
- Adolescent Problem - DepressionДокумент27 страницAdolescent Problem - DepressionMeera AnnОценок пока нет
- NCE Study GuideДокумент62 страницыNCE Study GuideSusana MunozОценок пока нет
- Who Conselling For Maternal and Newborn Health CareДокумент18 страницWho Conselling For Maternal and Newborn Health CareDouglas Magagna MagagnaОценок пока нет
- Interrwerwevettia TaserapsfeuticaДокумент1 страницаInterrwerwevettia TaserapsfeuticaOrban Csaba DanielОценок пока нет
- RezultateДокумент3 страницыRezultateOrban Csaba DanielОценок пока нет
- Why Does Handedness Exist?Документ2 страницыWhy Does Handedness Exist?Orban Csaba DanielОценок пока нет
- Facultatea De: Psihologie Si Stiinte Ale Educatiei Sectia: Psihologie, Anul 3 (2014)Документ4 страницыFacultatea De: Psihologie Si Stiinte Ale Educatiei Sectia: Psihologie, Anul 3 (2014)Orban Csaba DanielОценок пока нет
- Family Guy S13e02Документ43 страницыFamily Guy S13e02Orban Csaba DanielОценок пока нет
- The Planning, Attention-Arousal, Simultaneous and Successive (PASS) Theory of IntelligenceДокумент1 страницаThe Planning, Attention-Arousal, Simultaneous and Successive (PASS) Theory of IntelligenceOrban Csaba DanielОценок пока нет
- Self ConfidenceДокумент56 страницSelf Confidenceaecelcas pelagio100% (5)
- HRM3704 Tut101 17Документ44 страницыHRM3704 Tut101 17MichaelОценок пока нет
- Ej976654 PDFДокумент8 страницEj976654 PDFRaniena ChokyuhyunОценок пока нет
- AppreciationДокумент7 страницAppreciationRalph Samuel VillarealОценок пока нет
- Organizational Behaviour Chapter II AДокумент78 страницOrganizational Behaviour Chapter II AAwol TunaОценок пока нет
- Stress AssignmentДокумент7 страницStress AssignmentMartin MbaoОценок пока нет
- The Essential Motivation Handbook - Leo Babauta PDFДокумент112 страницThe Essential Motivation Handbook - Leo Babauta PDFdidiertwОценок пока нет
- MGT502 Organizational Behavior All Midterm Solved Paper in One FileДокумент162 страницыMGT502 Organizational Behavior All Midterm Solved Paper in One FileMalikusmanОценок пока нет
- Writing A Statement of Teaching Philosophy - 1Документ8 страницWriting A Statement of Teaching Philosophy - 1Michelle Zelinski100% (1)
- 12324890001Документ416 страниц12324890001دنيا سلومОценок пока нет
- Marketing MNG NotesДокумент119 страницMarketing MNG NotesShipra AggarwalОценок пока нет
- VALS-2 Segment CharacteristicsДокумент1 страницаVALS-2 Segment CharacteristicsThaoОценок пока нет
- Self-Assessment 8Документ4 страницыSelf-Assessment 8api-720382735Оценок пока нет
- Change Management ToolkitДокумент84 страницыChange Management Toolkitgabocobain100% (4)
- Intership Report Meer-Ehsan-BillahДокумент21 страницаIntership Report Meer-Ehsan-BillahZahir Mohammad BabarОценок пока нет
- Customer Service ExcellenceДокумент6 страницCustomer Service Excellenceazlipaat50% (2)
- Character Formation With Leadership Decision MakingДокумент13 страницCharacter Formation With Leadership Decision MakingShaine Frugalidad II100% (4)
- Ashwini Chavan HR ProjectДокумент67 страницAshwini Chavan HR ProjectDivyesh100% (1)
- SSP 111 Material SelfДокумент22 страницыSSP 111 Material SelfKesia Joy EspañolaОценок пока нет
- Teaching SkillДокумент35 страницTeaching SkillGex AmyCha TtuChicОценок пока нет
- Sexual Health Education in Quebec Schools: A Critique and Call For ChangeДокумент9 страницSexual Health Education in Quebec Schools: A Critique and Call For ChangesyaОценок пока нет
- Intro To CS With MakeCode For MicrobitДокумент7 страницIntro To CS With MakeCode For MicrobitJerome CastañedaОценок пока нет
- Pendidikan Fisika, 5 (6) ,: Daftar PustakaДокумент7 страницPendidikan Fisika, 5 (6) ,: Daftar PustakaHerma SafitriОценок пока нет
- Esip Final Revision 2020-2-1Документ31 страницаEsip Final Revision 2020-2-1Divh Boquecoz100% (1)
- Unit 1 Understanding Teaching and Learning: StructureДокумент24 страницыUnit 1 Understanding Teaching and Learning: StructureSatyam KumarОценок пока нет
- HopeДокумент26 страницHopeRadhaОценок пока нет
- Consumer Buying BehaviorДокумент71 страницаConsumer Buying BehaviorSiva Ramakrishna0% (1)
- Posdcorb: Explain Planning Process / Steps in Planning ProcessДокумент7 страницPosdcorb: Explain Planning Process / Steps in Planning Processnishutha3340Оценок пока нет
- HR ContentsДокумент10 страницHR Contentsआशिष प्रकाश बागुलОценок пока нет
- Meditation, Restoration, and The Management of Mental FatigueДокумент27 страницMeditation, Restoration, and The Management of Mental FatigueBetzi RuizОценок пока нет